Abstract
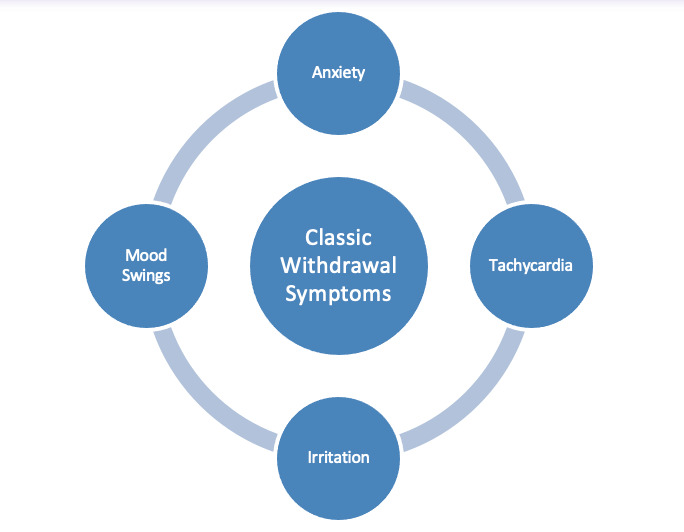
A 44-year-old male with no known past medical history but a known history of daily synthetic marijuana use presented to the emergency department after two witnessed seizures. The patient was admitted to the neurology service, where he was worked up with an MRI with epilepsy protocol and an EEG. During admission, the patient was admitted to daily synthetic marijuana use. He did note that he had started to decrease the amount of mojo he used daily in an attempt to stop. His last use was at 9 am the day of his admission. He was trying to decrease his use; his girlfriend of difficulty word-finding noted periods. Synthetic marijuana (SM) or “mojo” use has been increasing in the past decade for two reasons; It is considered an herbal product and has been legal. A withdrawal syndrome of SM use has been characterized chiefly as tachycardia, irritation, anxiety, and mood swings. These withdrawal symptoms are usually seen with chronic use. Some early results in the literature also show that SM use can lead to functional and structural neuronal changes. This manuscript discusses a case of a first on-set seizure as a possible withdrawal symptom in chronic SM use.
Keywords: Synthetic Marijuana, Mojo, Withdrawal, seizures, first onset seizures, Spice
Introduction
Synthetic marijuana (SM) or “mojo” use has been increasing in the past decade for two reasons; It is considered an herbal product and has been legal. Two, it is not detected on most standard urine drug screens.1 Since 2012, many compounds that can be found in synthetic marijuana have been banned in the United States and made a scheduled I substance; however, that has not stopped brick and mortar shops and internet stores from selling SM as “incense” and “herbs” making sure to label it as “not for human consumption.”2 SM is a popular drug of choice among the youth and those who are drug tested often as it does not show up on most standard drug tests.
A withdrawal syndrome of SM use has been characterized chiefly as tachycardia, irritation, anxiety, and mood swings.2,3 These withdrawal symptoms are usually seen with chronic use. Some early results in the literature also show that SM use can lead to functional and structural neuronal changes.3 Zorlu et al. found that there was a reduction in white matter volumes in several brain regions. These regions include the left temporal lobe and subcortical structures.4 Another case report looked at a chronic user’s brain after voluntary abstinence. The researchers found decreased dopamine D2/3 receptor availability in the striatum and extra-striatal regions than healthy controls.5 The availability of these receptors returned to normal levels after treatment.
Seizures have been associated with SM use; however, in a literature search, this was seemingly more connected to its use as seizures occurred in the context of intoxication. In this manuscript, we present a case of a chronic user who presented with the first onset of seizures and other subtle neurological changes in the context of decreased use of SM.
Case
A 44-year-old male with no known past medical history but a known history of daily synthetic marijuana use presented to the emergency department after two witnessed seizures. Seizure semiology was described as the patient feeling dizzy before the two episodes then tensing up, leaning to his left side, and having entire body jerking motions last about 1-2 minutes. He was noted to be confused and somnolent right after the episodes. His girlfriend witnessed both. The patient was admitted to the neurology service, where he was worked up with an MRI with epilepsy protocol and an EEG. During admission, the patient was admitted to daily synthetic marijuana use. When asked how much he used daily, he stated, “all day every day.” He did note that he had started to decrease the amount of mojo he used daily in an attempt to stop. His last use was at 9 am the day of his admission. He was trying to decrease his use; his girlfriend of difficulty word-finding noted periods. He states that he had been using it for about 24 years. MRI showed no abnormalities, and routine EEG was negative. The patient had no further seizures during admission but was started on Keppra for seizure prevention since he had two unprovoked seizures.
Discussion
Cannabis has been associated in the literature with adverse events and trips to the emergency room. THC, one of the psychoactive molecules in cannabis, works on cannabinoid receptors known as CB1 and CB2.6 THC exerts significant effects on the body, often manifested as substantial increases in heart rate and cardiac output, which are of particular concern in the novice or occasional user. Five cases in a case report on the adverse effects of marijuana highlighted presentations to the emergency department of possible cardiac events.6 Two had a mild narrowing of a coronary artery, one had histological evidence of cellular necrosis, and another had mild to moderate evidence of a fatty liver with an organizing thrombus that might have been secondary to cannabis-associated toxicity. Another collapsed while smoking a joint, and a cardiac arrhythmia was the suspected cause.6 Activation of the CB1 receptor is thought to increase sympathetic tone and decrease parasympathetic activity leading to these events.
SM is more potent than natural cannabis in activating CB1 and CB2 receptors, accounting for its increased incidence of adverse events.1 SM is a full agonist with a binding affinity five times higher than natural cannabis, which is just a partial agonist.1 This full agonist ability was thought to be why SM use could be associated with seizures. CB1 has associated seizure activity as antagonist pretreatments in one study prevented this from occurring.7 Serotonin syndrome has also been attributed to SM consumption, where excessive serotonin leads to the overactivity of nerve cells, which could cause migraines, myoclonus, agitation, confusion, seizures, coma, hyperthermia, etc. cardiovascular collapse, permanent hyperthermic brain damage, and death.8
During the literature review for this case, there were cases found where seizures were associated with SM use. One was a case of a 19-year-old male who had a generalized seizure while smoking a product called “happy tiger.”9 Four synthetic cannabinoids were found in his system. Another case was a 24-year-old male who had a witnessed generalized tonic-clonic seizure after smoking “funky monkey,” a known SM brand.10 Another case of a 48-year-old man who tried SM for the first time after buying it from an internet shop. This was the first time he had tried SM and had a generalized tonic-clonic seizure witnessed by his wife.11
Withdrawal of SM by chronic users was not associated with seizures in the literature search. Case reports that looked at cessation by regular users showed a case of a 20-year-old male who suffered chest pain six days after the termination of the use of SM.2 A second case discussed in the aforementioned case report was that of a 20-year-old woman who experienced sweats and chills along with cravings, headaches, insomnia, and vivid dreams, anorexia with a 20-lb weight loss, and severe anxiety after abrupt cessation of the use of SM.2 Neither of the cases found in the literature was associated with seizure-like the case discussed in this manuscript. Figure 1 shows the cluster of symptoms associated with chronic synthetic marijuana use withdrawal.
Figure 1. Cluster of symptoms that are linked to synthetic marijuana withdrawal in the literature.
Conclusion
Although seizures are associated with SM use, it seems to be more associated with the occasional use of SM or with the use of specific brands of SM which may affect an individual’s threshold differently. None of the cases of withdrawal seen in the literature was associated with the onset of seizures. The instances of withdrawal seen in the literature were also the complete cessation of SM use, wherein the case discussed here, the patient just had a decrease in his use without complete cessation. He also had associated difficulty with word-finding in the days leading up to the seizure, and this was not seen in any of the cases in the literature. This case highlights the importance of recognizing a possible withdrawal syndrome that could include seizures in chronic daily SM users. The limitations were that the patient could not recall what SM he used, and there was no testing for SM compounds in the hospital. Understanding this as a possible withdrawal symptom and the importance of taking a detailed substance abuse history is also highlighted in this case. Proper counseling was given to anti-epileptic drugs (AEDs) as the patient had two possibly provoked seizures. Since withdrawal seizures could not be ruled out, he was started on AEDs with the plan to taper off in six months.
Ethics approval and consent to participate
Ethics approval was not applicable since no new or off label medications or other treatments were used. The participant did give permission for his case with de-identification of his information to be used.
Consent for publication
All authors consent to the publication of this manuscript
Competing interests
All of the authors have no competing interests to disclose.
Authors’ contributions
A.E and P.D participated in the care of this patient. A.E was responsible for the writing of the manuscript and literature review. A.E, P.D., and J.F. was responsible for the editing of the manuscripts
Data Availability
All data used in the evaluation of this case can be publicly found in PubMed.
Acknowledgments
Acknowledgements
The authors would like to acknowledge and thank the patient for their participation in his care and the use of his case for the advancement of medical knowledge.
Funding Statement
No funding was used in the construction of this manuscript
References
- 1. Vera L, Bernstein K, Lee S. Historical and Current Perspectives of Synthetic Marijuana: Critical Review. J Addict Nurs. 2020;31(2):85-91. doi:10.1097/JAN.0000000000000333 [DOI] [PubMed]
- 2. Nacca N, Vatti D, Sullivan R, Sud P, Su M, Marraffa J. The synthetic cannabinoid withdrawal syndrome. J Addict Med. 2013;7(4):296-298. doi:10.1097/ADM.0b013e31828e1881 [DOI] [PubMed]
- 3. Cohen K, Weinstein AM. Synthetic and Non-synthetic Cannabinoid Drugs and Their Adverse Effects-A Review From Public Health Prospective. Front Public Health. 2018;6. doi:10.3389/fpubh.2018.00162 [DOI] [PMC free article] [PubMed]
- 4. Zorlu N, Angelique Di Biase M, Kalaycı ÇÇ, et al. Abnormal white matter integrity in synthetic cannabinoid users. Eur Neuropsychopharmacol. 2016;26(11):1818-1825. doi:10.1016/j.euroneuro.2016.08.015 [DOI] [PubMed]
- 5. Rominger A, Cumming P, Xiong G, et al. Effects of acute detoxification of the herbal blend “Spice Gold” on dopamine D2/3 receptor availability: a [18F]fallypride PET study. Eur Neuropsychopharmacol. 2013;23(11):1606-1610. doi:10.1016/j.euroneuro.2013.01.009 [DOI] [PubMed]
- 6. Drummer OH, Gerostamoulos D, Woodford NW. Cannabis as a cause of death: A review. Forensic Sci Int. 2019;298:298-306. doi:10.1016/j.forsciint.2019.03.007 [DOI] [PubMed]
- 7. Breivogel CS, Wells JR, Jonas A, et al. Comparison of the Neurotoxic and Seizure-Inducing Effects of Synthetic and Endogenous Cannabinoids with Δ9-Tetrahydrocannabinol. Cannabis Cannabinoid Res. 2020;5(1):32-41. doi:10.1089/can.2019.0003 [DOI] [PMC free article] [PubMed]
- 8. Schifano F, Orsolini L, Duccio Papanti G, Corkery JM. Novel psychoactive substances of interest for psychiatry. World Psychiatry. 2015;14(1):15-26. doi:10.1002/wps.20174 [DOI] [PMC free article] [PubMed]
- 9. Schneir AB, Baumbacher T. Convulsions Associated with the Use of a Synthetic Cannabinoid Product. doi:10.1007/s13181-011-0182-2 [DOI] [PMC free article] [PubMed]
- 10. Havenon A de, Chin B, Thomas KC, Afra P. The Secret “Spice”: An Undetectable Toxic Cause of Seizure. Neurohospitalist. 2011;1(4):182-186. doi:10.1177/1941874411417977 [DOI] [PMC free article] [PubMed]
- 11. Tofighi B, Lee JD. Internet highs-seizures after consumption of synthetic cannabinoids purchased online. J Addict Med. 2012;6(3):240-241. doi:10.1097/ADM.0b013e3182619004 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used in the evaluation of this case can be publicly found in PubMed.


