Abstract
Objectives.
Using the life course guidance, the goal of this study was to examine the degree to which previously experienced adversity and trauma was associated with subjective well-being among older adults.
Methods.
Data from the Health and Retirement Study (1992–2012) was used to examine these trends over time. We used multilevel models to test for specific individual change across time. The study sample included older community dwellers aged 55 and over (N = 5,649).
Results.
In terms of early childhood adversities, 77% experienced at least one trauma and 72% experienced at least one trauma in adulthood. Adverse childhood experiences and adulthood trauma were predictors of depressive symptoms, poorer self-rated health, and worse life satisfaction. Older black, other race, and Hispanic groups have poorer subjective well-being overtime compared to whites.
Conclusion.
Findings suggested exposure to childhood adversities and adulthood trauma increases depressive symptoms, poor self-rated health, and low satisfaction of life over time. Findings from this study provide insight into how life course exposure of adversity and trauma among older adults showed a negative trend over time.
Keywords: Adversity, Trauma, Social Support, Parental Support, Subjective Well-being
The world is aging faster than ever, and members of some groups fare better than others with respect to overall well-being. Although research on the aging minority population is growing, there are still gaps that need to be examined (Kuo et al., 2008; Mui & Kang, 2006; Mutchler et al., 2007; Wilmoth & Chen, 2003). A key gap is the impact of adversity experienced throughout the life course on later-life outcomes for minority populations. From the literature on childhood trauma and adjustment in early adulthood, we know that individuals who experienced trauma and adversity, such as growing up in a family with low socioeconomic status, having only one parent, growing up in less than favorable settings, are more likely to be at risk for maladjustment, poor health behaviors, risky life choices, and overall poorer mental and physical health outcomes (Dube et al., 2001; Horwitz et al., 2001). We do not know how racial minority older adults are faring, and their experience with these compounded traumas and adversity is not well documented (Pumariega et al., 2005).
The purpose of this research study is to examine how early-life events and adversity are associated with subjective well-being (e.g., depressive symptoms, self-rated health, and life satisfaction) in later life among vulnerable populations using data from the Health and Retirement Study (HRS). Self-rated health is part of a larger subjective component of overall well-being (Montross et al., 2006). Subjective well-being is assessed through various self-reported measures of well-being. Some of these measurements includes life satisfaction, aspects of life, quality of relationships, community, employment, and health (Proctor, 2014; National Research Council, 2013). Specifically, subjective health is viewed as part of an important component subjective well-being (Monden, 2014; National Research Council, 2013; Yang & Burr, 2015). For this study we include self-rated health as element of subjective well-being. By focusing on multiple dimensions of health, social relations, and life experiences, this study captured an expansive perspective on how older racial minorities are aging overall. The role of social support during childhood and later life are also explored to see if poor subjective well-being was reduced over time. In addition, this study examined whether race moderated the relationship between adversity and trauma and subjective well-being in later-life.
Adverse Experiences
Cumulative Advantage Theory (O’Rand, 1996), based on the life course perspective of health and well-being, specifically argues that childhood is critical to later-life well-being (Ben-Shlomo & Kuh, 2002). Adults who experienced childhood trauma and adversity were more likely to experience difficulty adjusting during adulthood, since they are at increased risk for poor health behaviors, lifestyle choices, and mental and physical health outcomes (Dube et al., 2001; Horwitz et al., 2001; Mullen et al., 1996). These traumas and adversities also influence well-being in later life, including mental (Barnes et al, 2012; Horowitz et al., 2001; Palgi et al., 2012) and physical health (Blackwell et al., 2001), life expectancy (Montez & Hayward, 2013), and mortality (Hayward & Gorman, 2004).
Adverse childhood experiences and later-life subjective well-being
The link between adverse childhood experiences to middle adulthood is well established and studied. Substantial research shows that childhood exposure to adverse events (e.g., physical abuse, mental abuse, neglect, family disruption(s), life-threatening illness, natural disasters) is negatively associated with middle and later-life well-being (Corso, et al., 2007; Schilling, Aseltine, & Gore, 2008; Springer, 2009). Negative outcomes included difficulty finding and maintaining meaningful relationships, employment, and poor health status (Amato, 2000; Benjet et al., 2010; Yang & Burr, 2015). Research specific to the Veteran population found that Veterans who experienced adverse childhood events reported lower levels of subjective well-being in later life (Bareis & Mezuk, 2016; Chapman et al., 2004: Park, et al., 2015). A study examining Jewish and Arab retirees found other-oriented adversity (witnessing harm done to another person) impacted Arabs’ mental and physical health more strongly than Jewish retirees’. Their finding showed the accumulation of adverse events negatively impacting health with respect to collective focused culture compared to individualist focused culture (Palgi & Shrira, 2016). However, little is known of the relationship of added experience of additional adverse experiences (e.g., combat trauma, survived an attack, or ever robbed) and the role of race and subjective well-being over time in American older adults.
Adverse adulthood experiences and later-life subjective well-being
The impact of adverse experiences in adulthood is also well documented. Adverse and traumatic adulthood experiences include death of one’s child, physical assault, life-threating illness or accident, or military combat exposure may all affect subjective well-being in later life. Empirical research has demonstrated that adults who experienced adversities were more likely to report lower life satisfaction, poorer health, and more depressive symptoms (Benjet, et al., 2010; Sachs-Ericsson, et al., 2015; Williams, et al., 2010). Older male Veterans who experienced military combat trauma during service reported poorer emotional control, psychological trauma, and lower subjective well-being compared to older Veterans who did not suffer from military combat trauma (Renshaw, et al., 2009; Sachs-Ericsson, et al., 2015; Williams, et al., 2010). These life course span adverse events during childhood and middle adulthood have yet to be examined together for their impacts on later-life subjective well-being among older adults.
Social Support: parent-child relationships and later-life relationships
There is a plethora of scientific literature that demonstrates social support as a protective factor from poor outcomes (Holt-Lunstad, Robles, & Sbarra, 2017; House, Landis, & Umberson, 1988). Early-childhood support from at least one parent or an adult figure have been shown to serve as a protective factor between early-life adversity and trauma on mental and physical health during early adulthood (Agaibi & Wilson, 2005; Lipschitz-Elhawi & Itzhaky, 2005). Specifically, children who experienced adversity developed functional relationships in early adulthood if they had a positive relationship with their parents or parents who provided them with support on how to navigate interpersonal relationships. The protective effect of a positive parent-child relationship into later life is still relatively unknown in general. However, the protective benefit of parent-child relationship may also extend into later life.
Social support in later life is particularly an important protective factor in subjective well-being. Health stressors in later life compounded with early and mid-adulthood adversity could lead to poorer health outcomes. Late-life social support have been shown to reduced poor outcomes including health conditions, mental health problems, and the risk of early mortality (Holt-Lunstad, Robles, & Sbarra, 2017; House, Landis, & Umberson, 1988). Krause (2004; 2005) demonstrated that the relationship between lifetime traumas and life satisfaction and meaning in life are buffered by social support, especially emotional support. Both of these support systems (parent-child relations and later life support) were examined as key protective factors in our study.
Race groups and later life subjective well-being
Studies have found older adults of racial minorities reported lower quality of subjective well-being than did white older adults. Cho et al. (2004) found Puerto Ricans have more activities of daily living limitations and spent more days in bed due to an illness compared to white older adults. In the same study, they also found that those who self-reported to be from a Hispanic subgroup (regardless of nativity status) or black self-rated their health lower compared to whites (Cho et al., 2004). Another study focused on older black and white community dwellers, using the Health and Retirement Study’s Assets and Health Dynamics data, found that at baseline the older black adults had lower self-rated health and more depressive symptoms compared to whites (Han, 2001). However, at follow up assessment (two years later) blacks self-reported improvement on health and depression even though there was no change in health function disability among both groups (Han, 2001). Subjective well-being in later-life is a complex concept to study and more research is needed to document life course approach to aging and change, especially with respect to race groups and adversity.
The evidences of racial minorities suffering from adversity or traumatic events and developing post-traumatic stress disorder are higher compared to whites is well established (Pieterse, et al., 2010; Roberts et al., 2011). Blacks and Hispanics were more likely to have higher risk of child maltreatment, witnessing domestic violence. And War-related traumas were more likely to be experienced by Asians, black men, and Hispanic women compared to whites (Roberts et al., 2011). However, we do not have information how these adversity and trauma impact racial minorities when they are older. A goal of this study is to see if there were interactions between the two indexes (ACE, ATI) and race groups.
This study employs the life course theory to provide a theoretical framework for exploring and interpreting how experiences with adversity and trauma throughout a lifespan relate to subjective well-being among older minority adults (Pearlin, 2010; Pearlin et al., 1990). We examine both adverse childhood experience and adult trauma together to provide a better understand of how these two effect subjective well-being in the same model since little is known how these two indexes impact later life subjective well-being. Thus, we sought to explore whether there were race groups difference in the relationship between changes in subjective well-being. This study focused on three hypothesis:
We expect those with exposure to adversity and trauma during childhood and mid-adulthood and later life to report lower subjective well-being over time.
Those who have social support during childhood and/or late adulthood will report favorable subjective well-being on average over time.
We anticipate a negative association between racial minority groups and subjective well-being in later life. And over time racial minority groups who experienced adversity and trauma at the two time points will report lower subjective well-being in later life.
Methods
Data source and study sample
The Health and Retirement Study (HRS) was used to address our research questions. The HRS is a panel study of a nationally representative sample of community-dwelling adults 51 years of age or older, with its first wave of data collection in 1992 (Servais, 2010). The HRS oversampled blacks and Hispanics. We examined group differences based on race (e.g., non-Hispanic blacks, non-Hispanic others, Hispanics, and non-Hispanic whites) for those who are 55 years or older. According to the literature young-old starts at age 55, thus we used the cut off of 55 years or older for this study (Hummert, 1993; Jeuring, et al., 2019; Klokgieters, van Tilburg, Huisman, 2018; Neugarten, 1974; Suanet, Broese van Groenou, & Braam, 2009). We used core data from the HRS from 1992–2012. Between 2008–2012 the Leave Behind Questionnaire (LBQ) portion of the HRS collected retrospective information from respondents that dated from childhood to the last five years (Smith et al., 2013). Data from the LBQ was also utilized in this study. Information on health conditions and limitations with activities of daily living were taken from a special data file constructed by the RAND Corporation.
Our outcome variables were self-rated health, depressive symptoms, and life satisfaction. The HRS began collecting data on each variable at different waves: self-rated health in 1992, depressive symptoms in 1998, and life-satisfaction in 2008. Therefore, there are 11 time points for self-rated health, 8 time points for depressive symptoms, and 3 time points for life-satisfaction. Each of the participants had to have answered all three of the outcome variables at least once to be retained in this study. The sample size for this study started at 16,298 (after deleting proxy, nursing home respondents, and not having at least one observation for all subjective well-being measures). An additional 10,649 respondents were deleted due to missing one or more of the independent variables or covariates.
The total sample for this study was 5,649 community dwellers. To examine differences between those who were deleted (N = 10,649) compared to those who were used for the analytical sample (N = 5,649) we conducted t-tests of mean differences for the predictors (i.e., Adverse Childhood Experiences Index, Adulthood Trauma Index, Parent-Child Relation Index, and Social Relationship Index) and control variables (i.e., age, gender, education, race categories, income, health conditions, and activities of daily living). Given the large sample size, many of the comparisons were statistically significant. However, in terms of meaningful differences, Cohen (1988) suggests effect sizes as follows: less than .2 of a standard deviation as a small effect size, between .2 - .5 as small to moderate, and .8 or higher as large. Most of the differences were in the low range, however the following variables had effect sizes larger than .2: Hispanic (.21), black (.27), age (.34), white (.38), and ADLs (.44). One could suggest that from these effect sizes those who remained in the analytic sample were healthier, white, and younger respondents. However, the t-test of mean differences suggest that those who were deleted compared to the analyzed respondents were not very different from each other.
Measures
Subjective well-being variables.
The dependent variables for this study were depressive symptoms, self-reported health, and life satisfaction. Depressive symptoms were measured by the short version of the Center for Epidemiologic Studies Depression Scale (CESD – 8), containing 8 questions: Much of the time during the past week “you felt depressed”, “you felt that everything you did was an effort”, “your sleep was restless”, “you were happy”, “you felt lonely”, “you enjoyed life”, “you felt sad”, and “you could not get going” (1=yes and 0 = no). The depression scale may range from 0 – 8 (two positive items were reverse coded). Self-reported health was based on the question: “Would you say your health is excellent, very good, good, fair, or poor?” (1 = excellent to 5 = poor). Life satisfaction was based on the following question: “Please think about your life-as-a-whole. How satisfied are you with it?” (1 = completely satisfied to 5 = not at all satisfied).
Trauma and adversity variables.
Two indices capture the experience of trauma and adversity: Adverse Childhood Experience Index (ACE) and Adulthood Traumas Index (ATI). The ACE consists of the following 6 questions (range 0 – 6): “Before you were 18 years old, did you have to do a year of school over again?”, “Before you were 18 years old, were you ever in trouble with the police?”, “Now think about your family when you were growing up, from birth to age 16. Would you say your family during that time was pretty well off financially, about average, or poor?”, “While you were growing up, before age 16, did financial difficulties ever cause you or your family to move to a different place?”, “Before you were 18 years old, did either of your parents drink or use drugs so often that it caused problems in the family?”, “Before you were 18 years old, were you ever physically abused by either of your parents?” The ATI was based on the following questions (range 0 – 7): “Has a child of yours ever died?”, “Have you ever been in a major fire, flood, earthquake, or other natural disaster?”, “Have you ever fired a weapon in combat or been fired upon in combat?”, “Has your spouse, partner, or child ever been addicted to drugs or alcohol?”, “Were you the victim of a serious physical attack or assault in your life?”, “Did you ever have a life-threatening illness or accident?”, “Did your spouse or a child of yours ever have a life-threatening illness or accident?”
Parent-child relationship index.
The Parent-Child Relationship Index (PCRI) was based on the following questions (range 0 – 5): “How much time and attention did your mother give you when you needed it?”, “How much effort did your mother put into watching over you and making sure you had a good upbringing?”, “How much did your mother teach you about life?”, “I had a good relationship with my mother before age 18”, “I had a good relationship with my father before age 18.” Higher score indicated more support from parents.
Social relationship index.
A Social Relationship Index (SRI) was a summation of the presence of the following social characteristics (range 0 – 7): married (1 = yes), child geographic proximity (1 = within 10 miles), self-report of good friends living in the neighborhood (1 = yes), self-report of relatives living the neighborhood (1 = yes), volunteered for a formal organization in the previous year (1 = yes), attended religious services one or more times a week in the previous year (1 = yes), and perceived social support available for help with basic personal care activities from relatives or friends (1 = yes).
Covariates.
Age is a continuous variable in years. A disability index is the sum of five self-reported Activities of Daily Living (ADLs) limitations (Does anyone ever help you dress, get across a room, bathe, etc.? Does anyone ever help you eat? Does anyone ever help you get in or out of bed?). A variable on health conditions is a count of eight self-reported physician diagnosed health conditions (heart disease, stroke, hypertension, cancer, diabetes, lung disease, arthritis and psychiatric condition, range = 0 – 8). Two socioeconomic status measures were annual household income (transformed by natural log) and years of formal education. Gender was coded as 1 = female, 0 = male.
Analytic Strategy
We employed multilevel models (i.e., hierarchical linear) to investigate the relationships among older adults’ experiences with adversity and traumas, social relationships, and subjective well-being. Multilevel models allow for each subject to have his/her own “personal” intercept and time trend deviating from the population average intercept and time trend, thus allowing heterogeneity in the subject trends across time (Hedeker & Gibbons, 2006). The model specification for each subjective well-being variable (depressive symptoms, self-rated health, and life satisfaction) included these predictors: time, ACE, ATI, PCRI, SRI in later life, and race categories (non-Hispanic white as reference group). Both depressive symptoms and self-rated health models allowed for linear and quadratic time trends. Since life satisfaction was assessed at three time points, only linear time trends were considered. We conducted three sets of interaction terms (race groups by ACE, race groups by ATI, and race groups by time) for all subjective well-being variables. Further interaction models between time and each of the adversity indexes (time*ACE, time*ATI) were ran however we did not find any support for each of the interactions (information on additional interaction models ran is available upon request). All models were adjusted for social demographic variables, health conditions, and ADLs.
Results
Figure 1 shows the means of each of the subjective well-being outcomes plotted over time. Over time self-rated health worsened, lower life satisfaction levels rose, and depressive symptoms decreased modestly. Table 1 lists descriptive characteristics of the sample. The average age of the sample was 70.9 years (SD = 8.8), with the majority of respondents identifying as non-Hispanic white (77.6%). Of the sample 11.6% self-reported as non-Hispanic black, 8.5% Hispanic, and 2.2% non-Hispanic other. 49.4% of the sample had completed at least one year of college. The median income for this sample was $42,904 (M = $ 66,516, SD = 94,657). This sample self-reported an average of 2.3 health conditions (SD = 1.40) and an average of 0.10 ADLs limitations (SD = .40). The mean ACE was .88 (SD = 1.03), and the mean ATI was 1.03 (SD = 1.11). The mean score for PCRI was 4.35 (SD = 1.20), and the mean later-life SRI was 3.62 (SD = 1.52). Table 1a describes the frequency of the ACE and ATI indexes items. In terms of the adverse childhood experiences index the most reported adversities were family not being financially well off (n = 1,589), followed by family having to move due to financial hardship (n = 930), next was having at least one parent had substance abuse problems (n = 924), and having to repeat a school year (n = 837). For the adulthood trauma index the most experienced traumas were experiencing a family member’s life-threatening illness or accident (n = 1,436), surviving a life-threatening illness or accident (n = 1,241), suffering through a death of a child (n = 828), surviving a natural disaster (n = 799), and having a family member addicted to drugs or alcohol (n = 789).
Figure 1. Means of Subjective Well-Being Variables overtime.
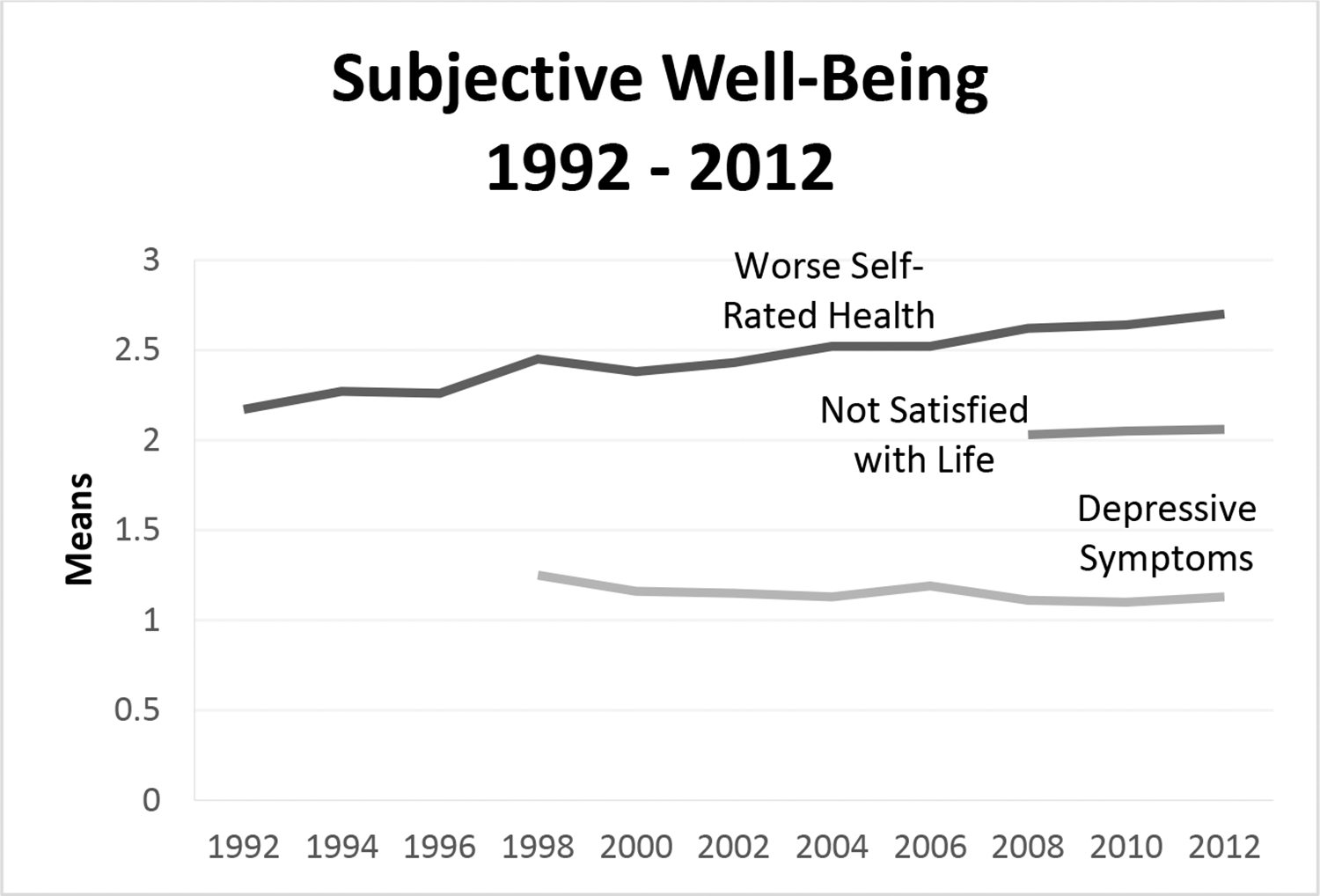
Note: N=5,649, Data from the Health and Retirement Study
Table 1.
Sample Characteristics for Community Dwellers in the Health and Retirement Study
| Mean/% | (SD) | Range | |
|---|---|---|---|
|
| |||
| Adversity | |||
| Adverse childhood experiences index | 0.88 | (1.03) | 0–6 |
| Adulthood trauma experiences index | 1.03 | (1.11) | 0–7 |
| Social Support | |||
| Early-life parent-child relationship index | 4.35 | (1.20) | 0–5 |
| Later-life social relationships index | 3.62 | (1.52) | 0–7 |
| Demographic characteristics | |||
| Race-ethnic status | |||
| Non-Hispanic Black, % | 11.60 | ||
| Non-Hispanic other race, % | 2.24 | ||
| Hispanic, % | 8.53 | ||
| Non-Hispanic White, % | 77.61 | ||
| Age | 70.91 | (8.81) | 55–100 |
| Female, % | 59.11 | ||
| Socioeconomic status | |||
| Education (in years) | 13.00 | (2.88) | 0–17 |
| Household income ($) | 66,516 | (94,657) | |
| Health characteristics | |||
| Number of health conditions | 2.30 | (1.40) | 0–8 |
| Number of ADL limitations | 0.10 | (0.40) | 0–5 |
Notes: N = 5,649. ADL = activities of daily living, a sum score of five items.
Table 1a.
Frequencies of Adverse Childhood Experience Index and Adulthood Trauma Index items
| Index | n |
|---|---|
| Adverse Childhood Experiences Index | |
| Repeat a year of school | 837 |
| Trouble with the police | 276 |
| Family not financially well off | 1,589 |
| Had to move due to financial hardship | 930 |
| Parent(s) had substance abuse problem | 924 |
| Physically abused by either of his or her parents | 408 |
| Adulthood Trauma Index | |
| A death of a child | 828 |
| Experienced a natural disaster | 799 |
| Experienced military combat | 240 |
| A family member addicted to drugs or alcohol | 789 |
| Experienced a serious physical attack or assault | 249 |
| Experienced a robbery | 217 |
| Experienced a life-threatening illness or accident | 1,241 |
| A family member experienced a life-threatening illness or accident | 1,436 |
| Total | 5,649 |
Depressive symptoms and adversity
Table 2 presents the results of the multilevel models for each subjective well-being outcome (depressive symptoms, self-rated health, and life satisfaction). Direct effects are shown, as interaction terms were non-significant. For depressive symptoms (Model 1), the linear time effect was statistically significant, indicating that symptoms decrease on average over time (B = − 0.04, 95% CI = −0.07, −0.02). ACE was positively related to depressive symptoms (B = 0.09, 95% CI = 0.07, 0.13). ATI was positively related to depressive symptoms over time in later life (B = 0.04, 95% CI =0 .01, 0.06). PCRI on average was negatively associated with depressive symptoms over time on average (B = −0.08, 95% CI = −0.10, −0.05). Further, SRI relationships in later-life was associated with fewer symptoms (B = −0.12, 95% CI = −0.14, −0.10). Blacks (B = 0.15, 95% CI = 0.05, 0.24), others (B = 0.69, 95% CI = 0.49, .89), and Hispanics (B = 0.37, 95% CI = 0.25, 0.48) groups were associated with overall more depressive symptoms compared to non-Hispanic whites over time. Table 3 presents results for the change across time between race groups and depressive symptoms (left columns). The results indicate that older blacks (B = 0.36, 95% CI = 0.23, 0.49), others (B = 0.70, 95% CI = 0.43, 0.98), and Hispanics (B = 0.58, 95% CI = 0.42, 0.74) compared to whites the differences were more pronounced at time zero (1998) and then the racial differences diminished over time for older blacks (B = −0.05, 95% CI = −0.07, − 0.03) and Hispanics (B = −0.05, 95% CI = −0.08, − 0.03). The findings provided support for our first and second questions, exposure to adversity and trauma during childhood, middle-aged and/or later life were all related to higher levels of depressive symptoms; having early and later life social support lowered depressive symptoms. There were race groups difference over time with reports of higher depressive symptoms. We found no support for any of the interaction terms, thus we found partial support for our third question. Please see the supplemental material section to review additional information on the interaction terms between race groups and each of the adversity indexes (Table 4a–c), and the variance-covariance estimates for the time trends (Table 5).
Table 2.
Mixed-Effect Regression Results for Adverse Childhood Experiences, Adulthood Trauma Experiences and Subjective Well-Being among Older Community Dwellers
| Depressive Symptoms | Worse Self-Rated Health | Lower Life Satisfaction | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| B | SE | 95% CI | B | SE | 95% CI | B | SE | 95% CI | |
| Adverse Childhood Experiences Index | 0.09 | 0.02 | (0.07, 0.13) | 0.04 | 0.01 | (0.02, 0.05) | 0.03 | 0.01 | (0.01, 0.05) |
| Adulthood Trauma Experiences Index | 0.04 | 0.01 | (0.01, 0.06) | 0.02 | 0.01 | (0.01, 0.04) | 0.05 | 0.01 | (0.03, 0.06) |
| Parent-Child Relationship Index | −0.08 | 0.01 | (−0.10, −0.05) | −0.01 | 0.01 | (−0.02, 0.01) | −0.04 | 0.01 | (−0.06, −0.03) |
| Later-Life Social Relationship Index | −0.12 | 0.01 | (−0.14, −0.10) | −0.04 | 0.01 | (−0.05, −0.03) | −0.09 | 0.01 | (−0.10, −0.08) |
| Race | |||||||||
| Non-Hispanic black | 0.15 | 0.05 | (0.05, 0.24) | 0.22 | 0.03 | (0.17, 0.27) | 0.01 | 0.03 | (−0.05, 0.06) |
| Non-Hispanic other | 0.69 | 0.10 | (0.49, 0.89) | 0.35 | 0.06 | (0.24, 0.46) | 0.11 | 0.06 | (0.001, 0.22) |
| Hispanic | 0.37 | 0.06 | (0.25, 0.48) | 0.32 | 0.03 | (0.26, 0.38) | 0.05 | 0.03 | (−0.02, 0.11) |
| Non-Hispanic white (ref) | |||||||||
| Time | −0.04 | 0.01 | (−0.07, −0.02) | 0.07 | 0.01 | (0.06, 0.08) | 0.01 | 0.01 | (−0.001, 0.02) |
| Time^2 | 0.003 | 0.002 | (−0.0003, 0.01) | −0.002 | 0.0003 | (−.003, −.001) | |||
Notes: B = unstandardized coefficients, SE = standard error of coefficients; ref = reference group; N = 5,649.
All models controlled for: age, gender, education, income, health condition counts, and activities of daily living
Table 3.
Mixed-effect regression results for adverse childhood experiences adulthood trauma experiences, moderated by race groups and time, and subjective well-being among older community dwellers
| Depressive Symptoms | Worse Self-Rated Health | Lower Life Satisfaction | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| B (SE) | 95% CI | B (SE) | 95% CI | B (SE) | 95% CI | |
| Adverse Childhood Experiences Index (ACE) | 0.10 (0.02) | (0.07, 0.13) | 0.04 (0.01) | (0.02, 0.05) | 0.03 (0.01) | (0.01, 0.05) |
| Adulthood Trauma Experiences Index (ATI) | 0.04 (0.01) | (0.01, 0.06) | 0.02 (0.01) | (0.01, 0.04) | 0.04 (0.01) | (0.03, 0.06) |
| Parent-Child Relationship Index | −0.08 (0.01) | (−0.10, −0.05) | −0.01 (0.01) | (−0.02, 0.01) | −0.04 (0.01) | (−0.06, −0.03) |
| Later-Life Social Relationship Index | −0.12 (0.01) | (−0.14, −0.10) | −0.04 (0.01) | (−0.05, −0.03) | −0.09 (0.01) | (−0.10, −0.07) |
| Race | ||||||
| Non-Hispanic black (Blk) | 0.36 (0.07) | (0.23, 0.49) | 0.38 (0.04) | (0.30, 0.46) | 0.003 (0.03) | (−0.06, 0.07) |
| Non-Hispanic other (Other) | 0.70 (0.14) | (0.43, 0.98) | 0.29 (0.09) | (0.11, 0.47) | 0.15 (0.07) | (0.12, 0.29) |
| Hispanic (Hisp) | 0.58 (0.08) | (0.42, 0.74) | 0.42 (0.05) | (0.32, 0.52) | 0.13 (0.04) | (0.06, 0.21) |
| Non-Hispanic white (ref) | ||||||
| Time | −0.03 (0.01) | (−0.06, −0.01) | 0.07 (0.01) | (0.06, 0.08) | 0.02 (0.01) | (−0.01, 0.03) |
| Time^2 | 0.003 (0.002) | (−0.0001, 0.01) | −0.002 (0.0004) | (−0.003, −.001) | ||
| Interactions | ||||||
| Blk*Time | −0.05 (0.01) | (−0.07, −0.30) | −0.02 (0.01) | (−0.03, −0.02) | 0.003 (0.02) | (−0.03, 0.04) |
| Other*Time | −0.01 (0.02) | (−0.05, 0.04) | 0.01 (0.01) | (−0.01, 0.03) | −0.04 (0.04) | (−0.12, 0.04) |
| Hisp*Time | −0.05 (0.01) | (−0.08, −0.03) | −0.02 (0.01) | (−0.03, −0.004) | −0.09 (0.02) | (−0.13, 0.04) |
Notes: B=unstandardized coefficients, SE=standard error of coefficients; ref=reference group.
All models controlled for: age, gender, education, income, health condition counts, and activities of daily living
Table 4a.
Mixed-effect regression results for adverse childhood experiences adulthood trauma experiences, moderated by race groups and adverse indexes, and depressive symptoms among older community dwellers
| Depressive Symptoms | ||||
|---|---|---|---|---|
|
| ||||
| B (SE) | 95% CI | B (SE) | 95% CI | |
| Adverse Childhood Experiences Index (ACE) | 0.10 (0.02) | (0.06, 0.13) | 0.10 (0.02) | (0.07, 0.13) |
| Adulthood Trauma Experiences Index (ATI) | 0.04 (0.01) | (0.01, 0.06) | 0.03 (0.02) | (0.004, 0.06) |
| Parent-Child Relationship Index | −0.08 (0.01) | (−0.10, −0.05) | −0.08 (0.01) | (−0.10, −0.05) |
| Later-Life Social Relationship Index | −0.12 (0.01) | (−0.14, −0.10) | −0.12 (0.01) | (−0.14, −0.10) |
| Race | ||||
| Non-Hispanic black (Blk) | 0.13 (0.07) | (−0.002, 0.26) | 0.15 (0.10) | (0.02, 0.28) |
| Non-Hispanic other (Other) | 0.83 (0.14) | (0.55, 1.11) | 0.76 (0.14) | (0.49, 1.04) |
| Hispanic (Hisp) | 0.34 (0.08) | (0.18, 0.50) | 0.32 (0.07) | (0.18, 0.47) |
| Non-Hispanic white (ref) | ||||
| Time | −0.04 (0.01) | (−0.06, −0.02) | −0.04 (0.01) | (−0.06, −0.02) |
| Time^2 | 0.003 (0.002) | (−0.0004, 0.01) | 0.003 (0.002) | (−0.0004, 0.01) |
| Interactions | ||||
| Blk*ACE | 0.02 (0.04) | (−0.07, 0.10) | ||
| Other*ACE | −0.13 (0.09) | (−0.31, 0.05) | ||
| Hisp*ACE | 0.02 (0.05) | (−0.08, 0.13) | ||
| Blk*ATI | −0.002 (0.04) | −0.09, 0.08 | ||
| Other*ATI | −0.07 (0.09) | −0.26, 0.11 | ||
| Hisp*ATI | 0.04 (0.05) | −0.05, 0.13 | ||
Notes: B=unstandardized coefficients, SE=standard error of coefficients; ref=reference group.
All models controlled for: age, gender, education, income, health condition counts, and activities of daily living
Table 5.
Variance − covariance estimates and 95% CI (for Table 2 models)
| Depressive Symptoms |
Self-Rated Health |
Life Satisfaction |
||||
|---|---|---|---|---|---|---|
| Random-effects | Estimate (SE) | 95% CI | Estimate (SE) | 95% CI | Estimate (SE) | 95% CI |
|
| ||||||
| Int var | 0.51 (0.02) | (0.47, 0.55) | 0.51 (0.02) | (0.47, 0.55) | 0.26 (0.01) | (0.24, 0.28) |
| Int, Time covar | −0.04 (0.01) | (−0.05, −0.03) | −0.04 (0.01) | (−0.05, −0.03) | −0.01 (0.01) | (−0.02, 0.001) |
| Time var | 0.03 (0.002) | (0.02, 0.03) | 0.03 (0.002) | (0.02, 0.03) | 0.02 (.01) | (0.10, 0.03) |
| Int, Time^2 covar | 0.001 (0.004) | (0.0003, 0.002) | 0.001 (0.0004) | (0.0004, 0.002) | ||
| Time, Time^2 covar | −0.002 (0.0002) | (−0.002, −0.001) | −0.002 (0.0002) | (−0.002, −0.001) | ||
| Time^2 var | 0.0002 (0.00002) | (0.0001, 0.0002) | 0.0002 (0.00002) | (0.0001, 0.0002) | ||
| Residual var | 0.36 (0.003) | (0.35, 0.36) | 0.36 (0.003) | (0.35, 0.36) | 0.33 (.01) | (0.32, .34) |
Self-rated health and adversity
Likelihood test between the direct model (without interaction terms) and a moderated model (including interaction terms) and found the model with moderators did not provide a better fit. Thus, we report the results from the direct effect model. Over time, self-rated health worsened (B = 0.07, 95% CI = 0.06, 0.08). There was a quadratic effect of time on self-rated health, indicating that the linear trend diminished as time increased, however, this effect is relatively small (B = −0.002, 95% CI = −0.003, −0.001). ACE was positively related to higher levels of poor health status (B = 0.04, 95% CI = 0.02, 0.05). ATI was positively associated to worse self-rated health (B = 0.02, 95% CI = 0.01, 0.04). The later-life SRI was negatively associated with worse self-rated health in later life (B = −0.04, 95% CI = −0.05, −0.03). Black (B = 0.22, 95% CI = 0.17, 0.27), other (B = 0.35, 95% CI = 0.24, 0.46), and Hispanic (B = 0.32, 95% CI = 0.26, 0.38) groups all were positively associated with higher poor self-rated health compared to non-Hispanic whites. Table 3 presents the change over time between race groups and self-rated health (middle columns). The results indicate that compared to whites older blacks (B = 0.38, 95% CI = 0.30, 0.46), others (B = 0.29, 95% CI = 0.11, 0.47), and Hispanics (B = 0.42, 95% CI = 0.32, 0.52) the differences were more pronounced at time zero (1992). However, over time the racial differences diminished for the older black (B = −0.02, 95% CI = −0.03, − 0.02) and Hispanic groups (B = −0.02, 95% CI = −0.03, − 0.004). There was partial support for our third question, race groups predicted poor self-rated health in later-life across time.
Life satisfaction and adversity
A likelihood test between the direct model and the model with interaction terms and indicated that there was no difference between the two models. Therefore, we presented the direct effect model here. ACE was positively associated with lower life satisfaction (B = 0.03, 95% CI = 0.01, 0.05). ATI was positively associated with lower life satisfaction (B = 0.05, 95% CI = 0.03, 0.06). PCRI was negatively associated with not satisfied with life (B = −0.04, 95% CI = −0.06, −0.03). In other words those with PCRI were more satisfied with their life. SRI in later-life was also negatively related to not satisfied with life over time (B = −0.09, 95% CI = −0.10, −0.08). Thus those with later life social support reported having higher life satisfaction. For those who self-reported other race they on average had lower life satisfaction (B = 0.11, 95% CI = 0.001, 0.22) compared to whites over time. Table 3, right columns, presents the change across time between race groups and life satisfaction. The results indicate that older others (B = 0.15, 95% CI = 0.12, 0.29) and Hispanics (B = 0.13, 95% CI = 0.06, 0.21) compared to whites the differences were more pronounced at time zero (2008). Over time the racial differences diminished for the older Hispanic group (B = −0.09, 95% CI = −0.13, − 0.04). There were support for the first and second hypothesis that older adults who were exposed to adverse childhood experiences and/or adulthood trauma reported higher level of not being satisfied with later-life; and early and later-life social support served as protective factors against reporting worse life satisfaction. Again, we found only partial support for our third question, those who self-identified as other rated their life satisfaction worse overtime compared to whites. There were no interactions between any of the adversity indexes and race groups.
Discussion
This study examined the lasting effects of childhood adversity and adulthood trauma in later life among community-dwelling adults in the U.S. The results showed adverse childhood experiences had a long-lasting negative impact on subjective well-being among older adults, supporting our study’s first question. Specifically, individuals who reported exposure to adverse childhood experiences had higher depressive symptoms, worse self-rated health, and less satisfied with life in later life. Exposure to adulthood trauma also had a negative impact on later-life subjective well-being. As expected, social support during childhood (e.g., early-life parent-child relationship and in later life) contributed to subjective well-being in later life, supporting for our second question. These findings align with previous studies that suggest social support served as a protective factor from depressive symptoms, worse self-rated health, and life satisfaction in later adulthood.
For the third question in this study we looked at the direct and moderating effects of race on subjective well-being. In the direct effect models we found black, other, and Hispanic groups compared to the white group in later-life reported more depressive symptoms and worse self-rated health over time. Respondents who self-reported as other reported less life satisfaction compared to whites over time. We found partial support for our third question.
Adversity and trauma observed at various stages of the life-course had long-term association with subjective well-being in this sample. The direct effects between adversity and trauma and depressive symptoms support the findings from previous research (Barnes et al, 2012; Horwitz et al., 2001; Palgi et al., 2012). Families and social support were important factors for mental health in later life (Golden et al., 2009). The findings demonstrated that resilience in later adulthood were in the form of parent-child relationships and later-life social relationships. We should note that the protective effect of parent-child relationship was not present with respect to self-rated health, thus suggesting that late life social support may be more impactful for later life health status.
Previous studies that examined race and subjective well-being in later life among U.S based community dwellers were primarily cross-sectional studies (Cho et al., 2004; Han, 2001; Roberts et al., 2011). Our study used longitudinal data among middle-aged and older community dwellers of the U.S. to examine the relationship between race and subjective well-being. Our study did not replicate previous findings like Palgi and Shrira’s (2016) study where other-oriented adversity impacted Arab respondents’ mental and physical health compared to Jewish respondents’ health. Our null finding could be attributed to the limitations of the types of adversity and trauma questions that were available in the HRS. The questions did not fully reflect any dialogistic inventory and were general. In addition, we may need to examine our null finding further by examining the role of social support and race, and resiliency and race in later life in future studies.
This study adds to current literature on the impact of life-span exposure to adversity and trauma on later-life subjective well-being. Previous studies have examined the role of adverse childhood experiences up to mid-adulthood (Dube et al., 2001; Horwitz et al., 2001; Irving & Ferraro, 2006; Noll, et al., 2009). These studies found adults who were exposed to adversities (e.g., physical abuse, sexual abuse, neglected) were more likely to report poor quality of relationships in adulthood, poor mental health status, and poor life choices. Our study’s findings further this field by using longitudinal data, the effect of cumulated adversity and trauma, and the life course approach to examine the long-term effect of adverse childhood experiences on later-life subjective well-being. In addition, we found changes across time between race groups and subjective well-being in later life.
Limitations
There were a few limitations in this study. Although we were able to use longitudinal data to examine our research questions the measurement of childhood adversity relies on participants’ ability to recall events that occurred decades ago. A study by Andrews, Brewin, & Gotlib (1993) discussed how recalled memories maybe exaggerated and there may be a retrospective recall bias for early trauma experiences. Thus the first limitation could be there was some bias from the reliance on the respondents’ retrospective recall of adversity and parent-child support. A second limitation is that our sample may have been biased towards those who either experienced intensely positive or negative experiences, as these may be individuals more likely to report experiencing adversity and traumatic events and childhood support. Thirdly, the HRS does not have information on the exact timing of the childhood events. In addition, the frequency of childhood adversities was not collected. Thus, we do not know if certain adversities were experienced more than once and its full impact on subjective well-being in later-life. Another limitation is the fact that the measured ACE items do not correspond to the Diagnostic and Statistical Manual of Mental Disorder-5 (DSM-5) Criterion A for traumatic events (American Psychiatric Association, 2013). The DSM-5’s Criterion A events may exert greater effect on subjective well-being than what was measured by ACE in this study. Thus, this study may have not been able to capture the full effect of adversity and trauma in early-life on later life well-being. Finally, certain types of adversity and trauma were not asked in the HRS. For example, adversity and trauma related to historical events, e.g., Civil Rights movement, may have influenced later-life subjective well-being.
Conclusion and contributions
Although this study is not without its limitations we contributed to the literature on the impact of adverse childhood experiences and adulthood trauma on later-life subjective well-being using the life course perspective. This study was able to employ longitudinal data to capture how adversity and trauma impact subjective well-being among community dwellers in later life. A vast majority of studies focuses on the association between adverse childhood exposure and mid-adulthood. Along with a few other studies focusing on adversity and later-life well-being we advanced this field by adding mid-adulthood trauma and extending the impact of these adversities into later life using longitudinal data. This approach allowed us to begin to understand the roles of adversity and trauma and demographic characteristics (race groups) on well-being in later-life among older community dwellers. Finally, the findings from this study suggest that professional care givers and healthcare provides should ask, recognize, and understand older adults’ exposure to adversity and trauma from a lifespan perspective to better provide services for mental and physical health concerns.
Table 4b.
Mixed-effect regression results for adverse childhood experiences adulthood trauma experiences, moderated by race groups and adverse indexes, and self-rated health among older community dwellers
| Worse Self-Rated Health | ||||
|---|---|---|---|---|
|
| ||||
| B (SE) | 95% CI | B (SE) | 95% CI | |
| Adverse Childhood Experiences Index (ACE) | 0.05 (0.01) | (0.03, 0.06) | 0.04 (0.01) | (0.02, 0.05) |
| Adulthood Trauma Experiences Index (ATI) | 0.02 (0.01) | (0.01, 0.04) | 0.02 (0.01) | (0.01, 0.04) |
| Parent-Child Relationship Index | −0.01 (0.01) | (−0.02, 0.01) | −0.01 (0.01) | (−0.02, 0.01) |
| Later-Life Social Relationship Index | −0.04 (0.01) | (−0.05, −0.03) | −0.04 (0.01) | (−0.05, −0.03) |
| Race | ||||
| Non-Hispanic black (Blk) | 0.23 (0.04) | (0.16, 0.31) | 0.20 (0.04) | (0.13, 0.27) |
| Non-Hispanic other (Other) | 0.38 (0.08) | (0.22, 0.53) | 0.41 (0.08) | (0.26, 0.57) |
| Hispanic (Hisp) | 0.40 (0.04) | (0.31, 0.49) | 0.35 (0.04) | (0.27, 0.43) |
| Non-Hispanic white (ref) | ||||
| Time | 0.07 (0.01) | (0.06, 0.08) | 0.07 (0.01) | (0.06, 0.08) |
| Time^2 | −0.002 (0.0004) | (−0.003, −.001) | −0.002 (0.0004) | (−0.003, −0.001) |
| Interactions | ||||
| Blk*ACE | −0.02 (0.02) | (−0.06, 0.03) | ||
| Other*ACE | −0.03 (0.05) | (−0.13, 0.08) | ||
| Hisp*ACE | −0.08 (0.03) | (−0.14, −0.02) | ||
| Blk*ATI | 0.02 (0.02) | −0.03, 0.06 | ||
| Other*ATI | −0.06 (0.05) | −0.16, 0.04 | ||
| Hisp*ATI | −0.03 (0.03) | −0.08, 0.02 | ||
Notes: B=unstandardized coefficients, SE=standard error of coefficients; ref=reference group.
All models controlled for: age, gender, education, income, health condition counts, and activities of daily living
Table 4c.
Mixed-effect regression results for adverse childhood experiences adulthood trauma experiences, moderated by race groups and adverse indexes, and life satisfaction among older community dwellers
| Lower Life Satisfaction | ||||
|---|---|---|---|---|
|
| ||||
| B (SE) | 95% CI | B (SE) | 95% CI | |
| Adverse Childhood Experiences Index (ACE) | 0.03 (0.01) | (0.01, 0.05) | 0.04 (0.01) | (0.02, 0.05) |
| Adulthood Trauma Experiences Index (ATI) | 0.04 (0.01) | (0.03, 0.06) | 0.04 (0.01) | (0.03, 0.06) |
| Parent-Child Relationship Index | −0.04 (0.01) | (−0.06, −0.03) | −0.05 (0.01) | (−0.07, −0.04) |
| Later-Life Social Relationship Index | −0.09 (0.01) | (−0.10, −0.07) | −0.09 (0.01) | (−0.10, −0.08) |
| Race | ||||
| Non-Hispanic black (Blk) | −0.10 (0.04) | (−0.80, −0.06) | 0.04 (0.04) | (−0.03, 0.12) |
| Non-Hispanic other (Other) | 0.17 (0.08) | (0.02, 0.03) | 0.25 (0.08) | (0.10, 0.41) |
| Hispanic (Hisp) | 0.05 (0.04) | (−0.04, 0.13) | 0.15 (0.04) | (0.07, 0.23) |
| Non-Hispanic white (ref) | ||||
| Time | 0.01 (0.01) | (−0.001, 0.02) | 0.01 (0.05) | (−0.0001, 0.02) |
| Time^2 | ||||
| Interactions | ||||
| Blk*ACE | 0.01 (0.02) | (−0.03, 0.06) | ||
| Other*ACE | −0.05 (0.05) | (−0.15, 0.05) | ||
| Hisp*ACE | −0.001 (0.03) | (−0.06, 0.06) | ||
| Blk*ATI | 0.01 (0.02) | (−0.03, 0.06) | ||
| Other*ATI | −0.10 (0.05) | (−0.20, 0.004) | ||
| Hisp*ATI | −0.02 (0.03) | (−0.07, 0.03) | ||
Notes: B=unstandardized coefficients, SE=standard error of coefficients; ref=reference group.
All models controlled for: age, gender, education, income, health condition counts, and activities of daily living
Contributor Information
Mai See Yang, Center on Demography and Economics of Aging, University of Chicago.
Donald Hedeker, Department of Public Health Sciences, University of Chicago.
References
- Agaibi CE, & Wilson JP (2005). Trauma, PTSD, and resilience: A review of the literature. Trauma, Violence, & Abuse, 6, 195–216. doi: 10.1177/1524838005277438. [DOI] [PubMed] [Google Scholar]
- Amato PR (2000). The consequences of divorce for adults and children. Journal of Marriage and Family, 62, 1269–1287. doi: 10.1111/j.1741-3737.2000.01269.x. [DOI] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5 ed.). Arlington, VA. [DOI] [PubMed] [Google Scholar]
- Antonucci TC, Birditt KS, & Akiyama H (2009). Convoys of social relations: An interdisciplinary approach. In Bengston VL, Gangs D, Pulney NM, & Silverstein M (Eds.), Handbook of theories of aging (pp. 247–260). New York, NY, US: Springer Publishing Co. [Google Scholar]
- Bareis N, & Mezuk B (2016). The relationship between childhood poverty, military service, and later life depression among men: Evidence from the Health and Retirement Study. Journal of Affective Disorders, 206, 1–7. doi: 10.1016/j.jad.2016.07.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes LL, Wilson RS, Everson-Rose SA, et al. , (2012). Effects of early-life adversity on cognitive decline in older African Americans and Whites. Neurology 79(24), 2321–2327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Shlomo Y & Kuh D (2002). A life course approach to chronic disease epidemiology: Conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology, 31(2), 285–293. doi: 10.1093/ije/31.2.285. [DOI] [PubMed] [Google Scholar]
- Benjet C, Borges G, & Medina-Mora M a. E. (2010). Chronic childhood adversity and onset of psychopathology during three life stages: childhood, adolescence and adulthood. Journal of Psychiatric Research, 44(11), 732–740. doi: 10.1016/j.jpsychires.2010.01.004. [DOI] [PubMed] [Google Scholar]
- Blackwell DL, Hayward MD, & Crimmins EM (2001). Does childhood health affect chronic morbidity in later life? Social Science and Medicine 52(8), 1269–1284. [DOI] [PubMed] [Google Scholar]
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, & Anda RF (2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders, 82(2), 217–225. doi: 10.1016/j.jad.2003.12.013. [DOI] [PubMed] [Google Scholar]
- Cho Y, Frisbie WP, Hummer RA, & Rogers RG (2004). Nativity, duration of residence, and the health of Hispanic adults in the United States. International Migration Review, 38(1), 184–211. [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioural sciences. PUBLISHER [Google Scholar]
- Corso PS, Edwards VJ, Fang X, & Mercy JA (2008). Health-related quality of life among adults who experienced maltreatment during childhood. American Journal of Public Health, 98(6), 1094–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depp CA, & Jeste DV (2006). Definitions and predictors of successful aging: a comprehensive review of larger quantitative studies. The American Journal of Geriatric Psychiatry, 14(1), 6–20. [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, & Giles WH (2001). Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span. JAMA, 286(24), 3089–3096. [DOI] [PubMed] [Google Scholar]
- Golden J, Conroy RM, & Lawlor BA (2009). Social support network structure in older people: underlying dimensions and association with psychological and physical health. Psychology, Health & Medicine, 14(3), 280–290. [DOI] [PubMed] [Google Scholar]
- Han B (2001). The impact of age, gender, and race on the relationship between depression and self-rated health in community-dwelling older adults: a longitudinal study. Home health care services quarterly, 20(3), 27–43. [DOI] [PubMed] [Google Scholar]
- Hayward MD, & Gorman BK, (2004). The long are of childhood: the influence of early-life social conditions on men’s mortality. Demography, 41(1), 87–107. [DOI] [PubMed] [Google Scholar]
- Hedeker D, & Gibbons RD (2006). Longitudinal Data Analysis (Vol. 451). John Wiley & Sons. [Google Scholar]
- Holt-Lunstad J, Robles TF, & Sbarra DA (2017). Advancing social connection as a public health priority in the United States. The American Psychologist, 72(6), 517–530. doi: 10.1037/amp0000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz AV, Widom CS, McLaughlin J, & White HR (2001). The impact of childhood abuse and neglect on adult mental health: a prospective study. Journal of Health and Social Behavior, 42(2), 184–201. [PubMed] [Google Scholar]
- House JS, Landis KR, & Umberson D (1988). Social relationships and health. Science, 241(4865), 540. [DOI] [PubMed] [Google Scholar]
- Hummert ML (1993). Age and Typicality Judgments of Stereotypes of the Elderly: Perceptions of Elderly vs. Young Adults. The International Journal of Aging and Human Development, 37(3), 217–226. 10.2190/L01P-V960-8P17-PL56 [DOI] [PubMed] [Google Scholar]
- Irving SM, & Ferraro KF (2006). Reports of abusive experiences during childhood adult health ratings: Personal control as a pathway? Journal of Aging and Health, 18(3), 458–485. doi: org/ 10.1177/0898264305280994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeuring HW, Hoogendijk EO, Comijs HC, Deeg DJH, Beekman ATF, Huisman M, Stek ML (2019). The tide has turned: incidence of depression declined in community living young-old adults over one decade. Epidemiology and Psychiatric Sciences 1–8. 10.1017/S204579601800081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klokgieters S, van Tilburg T, Deeg D, & Huisman M (2018, May). Do religious activities among young-old immigrants (aged 55–66) living in the Netherlands act as a buffer against the effect of a lack of resources on well-being? In European Journal Of Public Health (Vol. 28, pp. 185–185). Great Clarendon St, Oxford Ox2 6dp, England: Oxford Univ Press. [Google Scholar]
- Krause N (2004). Lifetime trauma, emotional support, and life satisfaction among older adults. The Gerontologist, 44(5), 615–623. doi: 10.1093/geront/44.5.615. [DOI] [PubMed] [Google Scholar]
- Krause N (2005). Traumatic events and meaning in life: Exploring variations in three age cohorts. Ageing & Society, 25(4), 501–524. doi: 10.1017/S0144686X0500382X. [DOI] [Google Scholar]
- Kuo BC, Chong V, & Joseph J (2008). Depression and Its Psychosocial Correlates Among Older Asian Immigrants in North America A Critical Review of Two Decades’ Research. Journal of Aging and Health, 20(6), 615–652. [DOI] [PubMed] [Google Scholar]
- Lipschitz-Elhawi R, & Itzhaky H (2005, October). Social support, mastery, self-esteem and individual adjustment among at-risk youth. In Child and Youth Care Forum (Vol. 34, No. 5, pp. 329–346). Kluwer Academic Publishers-Human Sciences Press. [Google Scholar]
- Monden C (2014). Subjective Health and Subjective Well-Being. Encyclopedia of Quality of Life and Well-Being Research, 6423–6426. [Google Scholar]
- Montez JK, & Hayward MD (2014). Cumulative childhood adversity, educational attainment, and active life expectancy among US adults. Demography, 51(2), 413–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montross LP, Depp C, Daly J, Reichstadt J, Golshan S, Moore D, … & Jeste DV (2006). Correlates of self-rated successful aging among community-dwelling older adults. The American Journal of Geriatric Psychiatry, 14(1), 43–51. [DOI] [PubMed] [Google Scholar]
- Mui AC, & Kang S-Y (2006). Acculturation stress and depression among Asian immigrant elders. Social Work, 51(3), 243–255. [DOI] [PubMed] [Google Scholar]
- Mullen PE, Martin JL, Anderson JC, Romans SE, & Herbison GP (1996). The long-term impact of the physical, emotional, and sexual abuse of children: a community study. Child Abuse & Neglect, 20(1), 7–21. [DOI] [PubMed] [Google Scholar]
- Mutchler JE, Prakash A, & Burr JA (2007). The demography of disability and the effects of immigrant history: Older Asians in the United States. Demography, 44(2), 251–263.Treas & Mazumdar, 2002. [DOI] [PubMed] [Google Scholar]
- National Research Council. (2013). Subjective Well-Being: Measuring Happiness, Suffering, and Other Dimensions of Experience. Panel on Measuring Subjective Well-Being in a Policy-Relevant Framework. Stone AA and Mackie C, Editors. Committee on National Statistics, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Neugarten BL (1974). Age groups in American society and the rise of the young-old. The annals of the American academy of political and social science, 415(1), 187–198. [Google Scholar]
- Noll JG, Shenk CE, & Putnam KT (2009). Childhood sexual abuse and adolescent pregnancy: A meta-analytic update. Journal of Pediatric Psychology, 34(4), 366–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Rand AM (1996). The precious and the precocious: understanding cumulative disadvantage and cumulative advantage over the life course. The Gerontologist, 36, 230–238. [DOI] [PubMed] [Google Scholar]
- Palgi Y, & Shrira A (2016). A cross-cultural longitudinal examination of the effect of cumulative adversity on the mental and physical health of older adults. Psychological Trauma: Theory, Research, Practice, and Policy, 8(2), 172–179. 10.1037/tra0000056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palgi Y, Shrira A, Ben-Ezra M, Shiovitz-Ezra S, & Ayalon L (2012). Self-and other-oriented potential lifetime traumatic events as predictors of loneliness in the second half of life. Aging & Mental Health, 16(4), 423–430. [DOI] [PubMed] [Google Scholar]
- Park CL, Wachen JS, Pless Kaiser A, & Mager Stellman J (2015). Cumulative trauma and midlife well-being in American women who served in Vietnam: Effects of combat exposure and postdeployment social support. Anxiety, Stress, & Coping, 28(2), 144–161. doi: 10.1080/10615806.2014.944905. [DOI] [PubMed] [Google Scholar]
- Pearlin LI (2010). The life course and the stress process: Some conceptual comparisons. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 65(2), 207–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, & Skaff MM (1990). Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist, 30(5), 583–594. [DOI] [PubMed] [Google Scholar]
- Pieterse AL, Carter RT, Evans SA, & Walter RA (2010). An exploratory examination of the associations among racial and ethnic discrimination, racial climate, and trauma-related symptoms in a college student population. Journal of Counseling Psychology, 57(3), 255. [DOI] [PubMed] [Google Scholar]
- Proctor C (2014) Subjective Well-Being (SWB). In: Michalos AC (eds) Encyclopedia of Quality of Life and Well-Being Research. Springer, Dordrecht. [Google Scholar]
- Pumariega AJ, Rothe E, & Pumariega JB (2005). Mental health of immigrants and refugees. Community Mental Health Journal, 41(5), 581–597. [DOI] [PubMed] [Google Scholar]
- Renshaw KD, Rodrigues CS, & Jones DH (2009). Combat exposure, psychological symptoms, and marital satisfaction in National Guard soldiers who served in Operation Iraqi Freedom from 2005 to 2006. Anxiety, Stress, & Coping, 22(1), 101–115. doi: 10.1080/10615800802354000. [DOI] [PubMed] [Google Scholar]
- Roberts AL, Gilman SE, Breslau J, Breslau N, & Koenen KC (2011). Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological medicine, 41(1), 71–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachs-Ericsson N, Joiner TE, Cougle JR, Stanley IH, & Sheffler JL (2015). Combat exposure in early adulthood interacts with recent stressors to predict PTSD in aging male veterans. The Gerontologist, 56(1), 82–91. doi: 10.1093/geront/gnv036. [DOI] [PubMed] [Google Scholar]
- Schilling EA, Aseltine RH, & Gore S (2008). The impact of cumulative childhood adversity on young adult mental health: measures, models, and interpretations. Social Science & Medicine, 66(5), 1140–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Servais MA (2010). Overview of HRS Public Data Files for Cross-sectional and Longitudinal Analysis. Institute for Social Research: University of Michigan. [Google Scholar]
- Smith J, Fisher G, Ryan L, Clarke P, House J, & Weir D (2013). HRS psychosocial and lifestyle questionnaire 2006–2010: Documentation report. Ann Arbor, MI: Institute for Social Research, University of Michigan. Retrieved from http://hrsonline.isr.umich.edu/sitedocs/userg/HRS2006-2010SAQdoc.pdf. [Google Scholar]
- Springer KW (2009). Childhood physical abuse and midlife physical health: Testing a multi-pathway life course model. Social Science & Medicine, 69(1), 138–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suanet B, Broese van Groenou M & Braam AW Eur J Ageing (2009) 6: 157. 10.1007/s10433-009-0119-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JE, Johnson AM, Heiss G, & Rose KM (2010). Association between exposure to combat-related stress and psychological health in aging men: The Atherosclerosis Risk in Communities (ARIC) Study. Journal of Traumatic Stress, 23(3), 358–366. doi: 10.1002/jts.20533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilmoth JM, & Chen PC (2003). Immigrant status, living arrangements, and depressive symptoms among middle-aged and older adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 58(5), S305–S313. [DOI] [PubMed] [Google Scholar]
- Yang MS, & Burr JA (2016). Combat exposure, social relationships, and subjective well-being among middle-aged and older veterans. Aging and Mental Health, 20, 637–646. doi: 10.1080/13607863.2015.1033679 [DOI] [PubMed] [Google Scholar]


