Abstract
Primary sclerosing cholangitis is a disease affecting around 0.006–0.016% of the population. Of these, around 75% have concomitant inflammatory bowel disease (IBD) according to the most recent epidemiological studies. Several theories have been proposed regarding the pathogenesis of primary sclerosing cholangitis (PSC). These include changes in the function of cholangiocytes, effects of the gut microbiome, association with specific human leukocyte antigen haplotypes and dysregulation of the immune system. However, these do not explain the observed association with IBD. Moreover, there are considerable differences in the frequency and outcomes between patients with PSC and ulcerative colitis compared with PSC and Crohn’s disease. The aim of this review is to appraise the most recent studies that have contributed to the epidemiology, advances in the pathophysiology, and characterization of important clinical aspects of the association of PSC and IBD.
Keywords: Primary sclerosing cholangitis, Cholangitis, Inflammatory bowel disease, Ulcerative colitis, Crohn’s disease
Introduction
Primary sclerosing cholangitis (PSC) is a rare disease that has a strong association with inflammatory bowel disease (IBD). However, the exact mechanisms that give rise to this association are not known. Several theories have proposed pathophysiological commonalities, but the data are conflicting. In the 20th century, a substantial number of studies identified the relationship between several human leukocyte antigen (HLA) loci and PSC. Recent advances in understanding the genetic risks have been achieved through large genome-wide association studies (GWAS), which provide a better understanding on the complex pathways involved in PSC. Important clinical associations and divergences among patients with PSC and IBD (PSC-IBD) and those without IBD have helped to differentiate the clinical course of the two groups and to provide important information that can guide further comprehension of the etiology of this pathology. Moreover, several clinical and pathological differences are seen between PSC-IBD patients and those with IBD only, raising the possibility of a different subset of IBD in patients with PSC. The aim of this review is to present the most current data on the different pathophysiological mechanisms that are believed to contribute to the development of PSC in the setting of IBD.
Epidemiology
PSC and IBD
The overall incidence of PSC alone varies geographically, but men are more affected than women. There is a higher incidence and prevalence in northern compared with southern regions. The estimated incidence in North America is 1.25 per 100,000 person-years in men and lower in women, at 0.54 per 100,000 person-years.1 In the UK, the combined incidence in men and women was 0.68 per 100,000 person-years, and the prevalence was 5.58 per 100,000 person-years. On the other hand, Southeast Asian countries like Singapore only reported 10 cases of PSC over 10 years and a male to female ratio of 9:1.2 In Spain for instance, the overall incidence has been increasing, and over the course of 3 years it went from 0.16 to 0.58 cases/million persons, of whom 60.5% were males.3 The median age at diagnosis was around 40 years in Australia, 42.3 years in Spain, 50.9 in Singapore and 54 in the UK.3–6
Bambha et al.1 reported that 73% of the patients diagnosed with PSC in North America had IBD. Similarly, in a large multicenter study in Europe, North America, and Australia including 7,121 patients with PSC, 70% also had IBD.7 In the UK, this association was slightly lower, from 250 patients with the diagnosis of PSC, 54% had concomitant IBD as opposed to 2% of the 1,250 healthy controls (HCs).5 It is estimated that the prevalence of PSC among patients with IBD is around 2%. Some studies compared the rates of PSC associated with ulcerative colitis (UC) and PSC associated with Crohn’s disease (CD).8,9 Escorsell et al.3 observed that 44.2% of 43 patients with PSC also had UC (PSC-UC), and of those, only one patient had PSC and CD (PSC-CD). A larger study by Fraga et al.8 studied 2,744 patients with IBD, of which 1,188 had UC and 1,556 had CD. Conversely, 4% of the UC patients had PSC compared with only 0.58% of the CD group. Ye et al.10 investigated the probability of PSC after diagnosis of IBD in 1,849 Korean patients and reported that there was a cumulative increased association among these pathologies with time. They concluded that in the first 5 years, the probability of PSC-UC was around 0.71% (significantly lower compared with Western countries), 2.59% after 15 years, and 3.35% after 20–25 years. The data are likely to be underestimated given the insidious nature of the disease, which can take several years until the symptoms arise. In addition, many patients were actively screened for PSC following a diagnosis of IBD. However, that was rarely done the other way around. This possibly reflects a statistically significant difference in the age of diagnosis of PSC-IBD and PSC-only patients. In a study of Navaneethan et al.,11 the mean age of diagnosis of PSC in the PSC-IBD group was 37 years compared with 48 years in the PSC-only group.
Proposed Pathogenetic Theories
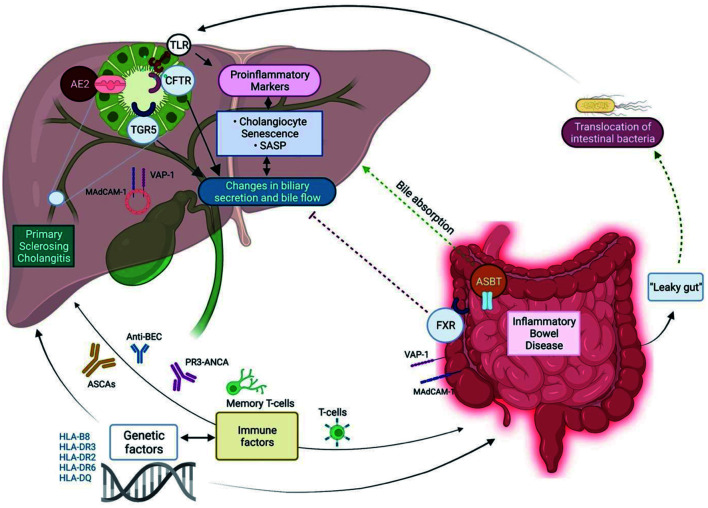
Several theories describing complex mechanisms that together lead to progressive inflammatory and scarring changes of the bile ducts have been proposed. Immune-mediated pathways play a major role in the disease. Defects in the mechanisms of protection against bile duct toxicity have been proposed. Several GWASs continue to provide a better understanding of the important genetic processes that are implicated in the development of this disease. More precisely, advances in the recognition of several specific HLA alleles are now widely accepted. In addition, other recently studied non-HLA risk loci are thought to be involved in the pathogenesis of PSC. The close association of IBD and PSC has given rise to the implication of the gut microbiome as one of the contributing factors. Several studies indicate that the inflammatory changes that occur in the gut of IBD of patients lead to subsequent bacterial translocation. Figure 1 outlines the main suggested pathogenic factors in the association of PSC and IBD.
Fig. 1. Illustration of potential pathogenic factors of PSC-IBD.
AE2, Cl−/HCO3− anion exchanger; TLR, Toll-like receptor; CFTR, cystic fibrosis transmembrane conductance regulator; TGR5, G protein-coupled bile acid receptor 1; VAP-1, vascular adhesion protein 1; MadCAM-1, Mucosal addressin cell adhesion molecule; ASCAs, Anti-Saccharomyces cerevisiae antibodies; Anti-BEC, anti- biliary epithelial cell antibody; PR3-ANCA, Proteinase 3 anti-neutrophil cytoplasmic antibody; FXR, nuclear farnesoid X receptor; ASBT, apical sodium-bile acid transporter; HLA, human leukocyte antigen.
Premature Cholangiocyte Senescence
Normal cholangiocytes can be activated by lipopolysaccharides (LPS) through Toll-like receptor (TLR) pathways leading to secretion of proinflammatory cytokines. Activation of TLRs in the plasma membrane of cholangiocytes strongly activates N-ras, which can induce cellular senescence characterized by irreversible cellular arrest during the G1 phase of the cell cycle and inability of further cell replication.12 Tabibian et al.13 evaluated liver-tissue specimens from PSC, PBC, and hepatitis C patients. They observed that PSC cholangiocytes had higher expression of senescence markers and profibro-inflammatory senescence-associated secretory phenotype (SASP) components such as interleukin (IL)-6, IL8, C-C motif chemokine ligand 2, and plasminogen activator inhibitor-1 (PAI-1), compared with patients with PBC and hepatitis C. The study included a thorough experimental analysis of human cholangiocytes obtained from the livers of patients with various liver diseases as well as control healthy livers, which allowed for a good comparison of cholangiocyte function in different environments. However, it was limited by lack of subgroup analysis.
Role of Cholangiocytes and Enterohepatic Bile Flow
Human biliary epithelial cells are continuously exposed to high concentrations of bile acids. Interestingly, most cells including hepatocytes show signs of cytotoxicity when exposed to low concentrations of bile acid. However, cholangiocytes are highly resistant to the toxic effects of bile acids. Human bile is composed of 25–40% of HCO3−. The morphology and function of cholangiocytes changes with the size of the bile ducts. Larger cholangiocytes are fully differentiated cells that line the medium and large bile ducts. They express receptors for secretin and somatostatin (CFTR, Cl−, Cl−/HCO3− exchanger). On the other hand, the small ducts are lined by small cholangiocytes that do not have the same secretion capacity or ability to respond to the above hormones and are thought to be primordial cells. However, they are more resistant to hepatic injury and toxins and express the antiapoptotic protein bcl-2.14 Hohenester et al.15 hypothesized that the HCO3− might serve as a protective umbrella in the apical part of the cholangiocyte, as alterations in important modulators of the HCO3− umbrella are associated with cholangiopathies. As an example, genetic changes in G protein-coupled bile acid receptor 1 (TGR5), which is a key modulator of the HCO3− umbrella, has been associated with PSC.
Recently, the TGR5 receptor has been identified as the first plasma membrane-bound bile acid receptor. Its role includes homeostasis and metabolic regulation of bile and inhibition of release of inflammatory cytokines.16 Studies in humans identified the TGR5 receptor in the gallbladder, colocalized with the cystic fibrosis transmembrane conductance regulator (CFTR) raising the possibility that both receptors interact in the secretory activity of cholangiocytes. The TGR5 gene is located in a chromosomal area close to the single nucleotide polymorphism (SNP) rs12612347, which has been associated both with UC and PSC.17 Hov et al.18 extensively studied the resequencing of TGR5 and found statistically significant associations of the TGR5 SNP common to both UC and PSC. However, the authors could not find a direct linkage between TGR5 and those diseases. Moreover, all the study subjects were from northern Europe, which could impact the reproducibility of the results.
CFTR has also been studied as a factor in the development of PSC. This transmembrane regulator is present in the apical membrane of cholangiocytes, where it has an important function in biliary secretion and bile flow. The cholangiographic hallmarks of both diseases are very similar.19 Previous studies that tried to identify the genetic commonalities of these clinical identities, found an increased frequency of CFTR mutations in patients with PSC (10.6%), but it was not statistically significant.20 Sheth et al.21 performed a prospective study in 19 patients with PSC, 17 with primary biliary cirrhosis (PBC), 18 with IBD but no liver disease, 81 with CF, and 51 healthy patients, and evaluated and compared their CFTR genotype and phenotype. They observed a significantly higher frequency of mutations and variations of the CFTR gene in the PSC group compared to the disease control group. The rate of CFTR mutations/variations in the PSC group was 37% compared with 8.6% in controls (p=0.02), and all seven PSC patients with CFTR variations had IBD. Moreover, they identified CFTR variants in the IBD group, but none in the PBC group, which could indicate that the CFTR gene might be one of the causes of strong association between PSC and IBD. However, the statistical power of this study was low. Additionally, there was a significant sex difference (74% of the PSC group were men and 88% of the PBC group were women). No subgroup analyses were performed, and selection bias cannot be ruled out. Alterations of other important transporters have been implicated in the contribution to cholangiocyte senescence and biliary disease. Cl−/HCO3− anion exchanger 2 (AE2) located in the cell membrane of normal human cholangiocytes, has been associated with PBC, and bile acid toxicity has been shown to be increased when AE2 was inhibited.22,23 Moreover, downregulation of AE2 has been observed in PSC-UC patients.23
Given the close association of PSC and IBD, the enterohepatic circulation of bile is of major interest, and recent studies have suggested new therapeutic strategies for the treatment of cholestatic diseases based on these observations. Bile acids in the intestine bind the nuclear farnesoid X receptor (FXR) which is present on the enterocytes throughout the small intestine and colon. Subsequently, fibroblast growth factor (FGF)15/19 is activated and binds the FGF receptor 4 which in turn inhibits bile acid synthesis in the liver.24 Although there are no studies demonstrating a direct relationship between FXR/FGF19/FGFR4 changes and PSC, activation of that pathway has been shown to improve cholestasis in PSC patients.25 Interestingly, Vavassori et al.26 provided good evidence that FXR works as a modulator of intestinal innate immunity in IBD. They observed that FXR-depleted mice had an uncontrolled immune response upon active intestinal inflammation, and upon introduction of a synthetic FXR, they observed counter-regulatory effects on innate immunity and attenuation of organ injury. Lastly, the apical sodium dependent transporter is located in the membrane of the enterocytes of the terminal ileum and is responsible for the absorption of conjugated bile. It is an evolving target in the therapy of PSC. However, data on its role in the pathophysiology of PSC are scarce and conflicting.27,28 Table 1 outlines the main findings of different studies of important cell receptors and transporters in the pathogenesis of PSC-IBD.16–21,23,25–27
Table 1. Overview of the main findings of studies of cell receptors and transporters in the pathogenesis of PSC-IBD.
| Receptor/transporter in cholangiocytes and enterocytes | ||||
|---|---|---|---|---|
| Receptor/transporter | Function | Study | Findings/association with PSC-IBD | Weakness (−)/Strength (+) |
| TGR5 receptor | a G protein-coupled bile acid receptor 1, which is a key modulator of the cholangiocyte HCO3− umbrella | Kawamata et al.16 | TGR5 identified as the first plasma membrane-bound bile acid receptor. Its role includes homeostasis and metabolic regulation of bile, and inhibition of release of inflammatory cytokines | |
| Karlsen et al.17 | TGR5 in the gallbladder co-localized with the CFTR raising the possibility that both receptors interact in the secretory activity of cholangiocytes. TGR5 gene is located in a chromosomal area close to the SNP rs12612347 which has been associated both with UC and PSC | |||
| Hov et al.18 | Significant associations of the TGR5 SNP common to UC and PSC; No direct linkage between PSC and IBD was found | (−) All study subjects were from Northern Europe | ||
| CFTR | Present in the apical membrane of most epithelia, including cholangiocytes. Functions in biliary secretion and bile flow | McGill et al.20 | No statistical significance in the frequency of CFTR mutations in patients with PSC | (−) Small number of mutations were genotyped |
| Sheth et al.21 | Significantly higher frequency of mutations and variations of CFTR gene in the PSC group compared to the disease control group. | (−) Small sample size. | ||
| Durieu et al.19 | Similar liver findings on magnetic resonance cholangiography between patients with CF and liver disease and those with PSC. | (−) Lack of control group. | ||
| AE2 | Cl−/HCO3− anion exchanger | Kempinska-Podhorodecka et al.23 | Downregulation of AE2 has been observed in PSC-UC patients; Suppression of AE2 is associated with higher bile acid toxicity | (−) Small sample size |
| FXR | Nuclear receptor Farnesoid X receptor; present in the enterocytes throughout the small intestine and colon; inhibits bile acid synthesis through negative feedback | Trauner et al.25 | Activation of this pathway has been shown to improve cholestasis in PSC patients | |
| Vavassori et al.26 | FXR works as a modulator of intestinal innate immunity in IBD | |||
| ASBT | Apical sodium dependent transporter is located in the membrane of enterocytes of the terminal ileum and responsible for the absorption of conjugated bile | Hegade et al.27 | Evolving target in the therapy of PSC however the data of its role in the pathophysiology of PSC is scarce | |
PSC-IBD, primary sclerosing cholangitis-inflammatory bowel disease; TGR5, G protein-coupled bile acid receptor 1; SNP, single nucleotide polymorphism; CFTR, cystic fibrosis transmembrane conductance regulator; AE2, Cl−/HCO3− anion exchanger; FXR, nuclear farnesoid X receptor; UC, ulcerative colitis; ASBT, apical sodium dependent bile acid transporter.
Immunopathogenic Factors
Adaptive immunity
The inflammatory infiltrate of the liver of PSC patients has been reported to contain a large proportion of memory T cells.29 Furthermore, other extra-intestinal manifestations of IBD, including erythema nodosum and ankylosing spondylitis are characterized by the presence of lymphocytes on tissue examination. Although there is a strong association between IBD and PSC, PSC in IBD patients can develop independently from active colitis, and can persist after colectomy.30 That conclusion was reported in a recent meta-analysis. However, the studies were not of high quality, mainly because of a small sample size and high variability observed in the results. Nonetheless, the findings challenge the hypothesis that bacterial translocation and intestinal toxins are the sole or main cause of PSC. Moreover, PSC post-liver transplant patients have been found to still develop IBD, but with a milder course.31 Importantly, the patients were started on immunosuppressive therapy after liver transplantation, which could have affected the severity of IBD.
The liver and the gastrointestinal tract share two endothelial molecules, vascular adhesion protein 1 and mucosal addressin cell adhesion molecule 1, which allow for lymphocyte adhesion.32 This study effectively provided the evidence in two independent analyses through immunohistochemistry using monoclonal antibodies. Grant et al.33 proposed that effector T cells develop in the intestinal lymphoid tissues during active inflammation, and that they persist as memory cells and reach the liver through the portal vein. It is likely that the process requires initial antigen migration through the enterohepatic circulation to the liver and subsequent presentation to lymphocytes. The liver also plays a role in downregulating immune responses to food antigens. The effects are possible because of recirculation of lymphocytes between the gut and the liver. The authors also hypothesized that T cells are activated during IBD flares and have the capacity to originate memory T cells that in turn adhere to the intestinal mucosa and hepatic endothelium.33 One drawback of the theory is that it fails to explain the difference in frequency of PSC between UC and CD. Kekilli et al.34 further studied the role of adaptive immunity in the pathophysiology of PSC, using flow cytometry to assay levels of CD4+CD5+ T cells in patients with PSC-UC, and UC but not PSC. There was a significantly higher level of CD4+CD5+ T cells in patients with PSC-UC. Although the study sample was relatively small, selection bias was low, as both groups were matched by demographic characteristics. However, applicability to non-Turkish populations may be an issue. There were no statistically significant differences in smoking status and disease duration, and all patients were taking mesalamine.
Innate immunity
Pattern recognition receptors (PRRs), including TLRs, have the ability to detect intestinal pathogen-associated molecular patterns (PAMPs). When activated, PRRs trigger an innate immune response leading to a poorly organized inflammatory reaction. Human cholangiocytes constantly interact with PAMPs that travel from the intestine. Common intestinal PAMPs include LPS, which is an endotoxin derived from Gram-negative bacteria and lipoteichoic acid from Gram-positive bacteria. Repeated exposure to PAMPs leads to a tolerant state in healthy bile epithelial cells which is a protective mechanism and precludes a persistent inflammatory environment.35,36 Several studies provide evidence that the tolerance to PAMPs is suppressed in several cholangiopathies, including PSC. The main pathogenesis is thought to occur through variations in TLR which subsequently lead to an aberrant innate immune response with continuous production of cytokines and chronic inflammation.12,35
Mueller et al.12 analyzed innate immune responses mediated by PRRs and endotoxin tolerance in biliary endothelial cells from PSC patients, alcoholic liver disease, and healthy livers. In end-stage PSC livers, they detected increased TLR protein expression and MyD88/IRAK signaling complex activation in biliary endothelial cells, with consequent abnormal innate immune activation on exposure to endotoxins together with lack of protective endotoxin tolerance. Moreover, there were increased levels of interferon gamma and tumor necrosis factor alpha (TNF-α), which magnify TLR expression and TLR-mediated signaling. Similar findings were observed in patients with end-stage alcoholic liver disease. However, in the livers of early PSC patients, the finding was not as evident, as it was marked with low levels of pro-inflammatory markers. The results suggested that the poorly regulated overactive innate immune response in PSC has a higher impact in later stages of the disease rather than acting as an initial contributor. In addition, the abnormal innate immune response was not limited to PSC. The fact that PSC is highly associated with IBD might increase the levels of endotoxin exposure and explain the enhanced TLR-mediated signaling. However, it cannot be assumed that these results are restricted to PSC.
Autoantibodies
Detection of autoantibodies in patients with PSC is not uncommon. However, their specificity is very low, and there are no strong data that support autoantibodies as a main cause of PSC. Furthermore, immunosuppressants do not lead to disease improvement of PSC.37 Among the autoantibodies detected in PSC patients, increased frequencies of anti-biliary epithelial cell (BEC), phosphorylated antineutrophil cytoplasmic antibodies (pANCA), antinuclear antibody (ANA), smooth muscle actin, and anticardiolipin have been reported. Yet, the ranges of incidence are wide and not consistent.38 Moreover, the reported frequencies of pANCA in PSC-UC have a high variability of 33–83%.39,40 Those of PSC-CD are significantly lower and range from 0–27%.40,41
Xu et al.42 investigated the presence of antibodies to BEC in PSC, PBC, autoimmune hepatitis (AIH), and controls, and found a significantly more patients with PSC had anti-BEC antibodies. In their study, anti-BEC antibodies were present in 63% of PSC patients, 37% with PBC, 16% with AIH, and in only 8% of controls. It is important to note, however, that the control group consisted of only 12 patients, and that the PSC group had the most patients (n=30). A study of the effect of anti-BEC antibodies in liver transplantation by Ge et al.43 reported different results. In their patient sample, anti-BEC antibodies were positive in 31.8% of patients with hepatitis C cirrhosis, 55.6% with PSC, 75% with PBC, 57.1% with AIH, 57.1% with hepatitis B cirrhosis, and 71.4% with alcoholic cirrhosis. The fact that all the patients had end-stage liver disease could either represent a risk for development of these antibodies or, from another perspective, that patients with anti-BEC antibodies might have a higher chance of progressing to end-stage liver disease.
ANCA and pANCA antibodies are present in many autoimmune and immune-mediated diseases. The prevalence of ANCA antibodies has been reported to range from 42–93% and that of pANCA from 26–94% in PSC, so they are not specific for PSC.38,40,44–46 Importantly, PR3-ANCA, an atypical ANCA antibody, has been associated with PSC, and it may also a marker that differentiates UC from CD. For instance, Mahler et al.47 assayed PR3-ANCA in 283 UC and 208 CD patients with a chemiluminescent immunoassay, and detected it in 31.1% of UC vs. 1.9% of CD sera. Stinton et al.48 evaluated 244 PSC and 254 HC, by PR3-ANCA chemiluminescent immunoassay; and reported that it was present in 38.5% (94/244) of PSC patients compared with 10.6% (27/254) of controls (p <0.0001). However, the authors did not find any association with the presence or type of IBD.
Anti-Saccharomyces cerevisiae antibodies (ASCAs) are associated with CD, with a prevalence of 60–70%, compared with 10–15% in UC.49 Muratori et al.50 reported that ASCA was positive in 70% (16/23) of CD patients and in 44% (11/25) of PSC patients compared with 5% of HC patients. The presence of ASCA in PSC patients did not predict the occurrence of or type IBD. However, the number of patients in this study was small. Further studies are warranted.
The prevalence of ANA in PSC has been reported to have a wide range (8–77%).38 Moreover, Angulo et al.51 observed a predominance of speckled and homogenous patterns of ANA. However, we could not find any studies that investigated the association of ANA with PSC-IBD. Furthermore, ANA is not a common marker in IBD.52 The presence of autoantibodies in PSC is more likely a reflection of abnormal immune response rather than a pathogenetic factor. Table 2 summarizes the main findings of studies of important immune factors in the pathogenesis of PSC-IBD.12,29-31,34,42-44,47,48,50
Table 2. Overview of the main findings of studies of immune factors in the pathogenesis of PSC-IBD.
| Immunopathogenic factors | |||
|---|---|---|---|
| Study | Findings/associations with PSC-IBD | Weakness (−)/Strength (+) | |
| Adaptive immunity | |||
| Ponsioen et al.29 | The inflammatory infiltrate of the liver of PSC patients contains a large proportion of memory T cells | ||
| Ong et al.30 | PSC in IBD patients can develop independently from active colitis, and activity can continue after colectomy | (−) Although the results are from a meta-analysis, independent studies had small sample sizes | |
| Befeler et al.31 | PSC post-liver transplant patients have been found to still develop IBD, but with a milder course | (−) These patients were started on immunosuppressive therapy after liver transplant which could have affected the severity of IBD | |
| Kekilli et al.34 | Higher level of CD4+CD5+ T cells in patients with UC-PSC compared to patients with UC and no PSC | (−) Small sample size | |
| Innate immunity | |||
| TLR changes | Mueller et al.12 | End stage PSC livers have higher TLR protein expression and MyD88/IRAK signaling complex activation in the biliary endothelial cells, with consequent abnormal innate immune activation; In the livers of early PSC, this finding was not as evident as it was marked with low levels of pro-inflammatory markers | |
| Auto-antibodies | |||
| Anti-BEC | Xu et al.42 | Higher number of patients with PSC having anti-BEC antibodies compared to PBC, autoimmune hepatitis, and controls | (−) Control group had a significant lower number of patients |
| Ge et al.43 | No significant differences in frequency of anti-BEC among patients with PSC, AIH, HBV cirrhosis. | ||
| Roozendaal et al.44 | Anti-BEC IgG from PSC patients induced the expression of TLR4 and TLR9 in BEC which together with exposure to LPS lead to the secretion of cytokines | ||
| PR3-ANCA | Mahler et al.47 | Higher prevalence in UC vs. CD (31.1% UC vs. 1.9% CD sera) | (+) Good study power |
| Stinton et al.48 | Detected in 38.5% (94/244) of PSC patients compared to 10.6% (27/254) controls; No association with the presence or type of IBD | (+) Good study power | |
| ASCA | Muratori et al.50 | ASCA was positive in 70% (16/23) of CD patients and in 44% (11/25) of PSC patients compared to 5% of HC | (−) Small sample size |
PSC-IBD, primary sclerosing cholangitis-inflammatory bowel disease; TLR, Toll-like receptor; ASCAs, Anti-Saccharomyces cerevisiae antibodies; AIH, autoimmune hepatitis; HBV, hepatitis B virus; LPS, lipopolysaccharide; CD, Crohn’s disease; HC, healthy controls.
Genetic Risk
HLA and PSC
Prior studies have shown an increased association of PSC and specific HLA haplotypes, raising the possibility of a genetic risk in the development of this disease. Both HLA histocompatibility complex class I and class II have been described in the setting of PSC. Susceptibility to PSC has been associated with HLA-B8, -DR3, -DR2, -DR6, and -DQ. Schrumpf et al.53 evaluated 20 patients with UC and hepatobiliary disease and 34 UC patients without hepatobiliary disease, and found that 80% of patients with combined disease had HLA-B8 compared with 32% in those with only UC. HLA-DR3 was also positive in 70% of patients with combined disease and in only 35% of those with only UC. Similar findings were observed by Chapman et al.54 Donaldson et al.55 further analyzed the frequency of HLA-DR3 in PSC patients. Of 81 with PSC, 40% had positive HLA-DR3 vs. 12% of controls. The authors then eliminated the HLA-DR3 positive patients from the PSC and control groups, including heterozygous patients, and tested for HLA-DR2. They found that 69% of the HKA-DR3-negative PSC patients were positive for HLA-DR2 compared with 34% of the HLA-DR3 negative control patients. Noguchi et al.56 evaluated several HLA haplotypes in a population with PSC. The highest frequencies in the PSC group compared with the control group over the course of 7 years were HLA-A1 42.3% vs. 25.7%, HLA-B8 43.6% vs. 17.1%, HLA-DR3 40% vs. 22.2%, and HLA-DR6 40% vs. 7.2%. In a study of 130 Norwegian patients with PSC and 306 healthy patients, Wiencke et al.57 reported a significantly higher proportion of PSC patients carrying all four alleles of HLA-B8, HLA-DR3, MICA5.1, and MICB24 compared with controls (49% vs. 18%; OR: 4.5; Pc<1×10−7). The study lacked demographic characterization of the study subjects. Nonetheless, despite the initial results of increased frequencies of MICA5.1 and MICB24 markers in PSC cases, regrouping of the cases according to the DR3 status (positive vs. negative) allowed for completely different results and reduced bias.
Inheritance risk
Bergquist et al.58 investigated the frequency of autoimmune diseases in 145 patients with PSC. They divided the patients into groups with PSC only (n=19) and with PSC and IBD (n=126). For every patient with PSC and IBD there was a control patient with IBD only. There were five cases of PSC among first-degree relatives. This represents a prevalence of 0.7% and around 100-fold higher risk of first-degree relatives to develop PSC. In the group of patients with only PSC (n=19), the frequency of a first-degree relative with IBD was higher than that in the group of PSC and IBD (26% vs. 9%, p<0.05). This retrospective case-control study had a large sample size. In addition, the authors confirmed the diagnosis of PSC with magnetic resonance cholangiopancreatography or endoscopic retrograde cholangiopancreatography in the patient’s first-degree relatives without relying on questionnaires. However, all patients were Swedish so the results might not be reproducible worldwide. Also, the initial information was provided through a questionnaire that was sent to all patients. Only the first-degree relatives with reported liver disease, IBD, diabetes, rheumatoid arthritis, thyroid disease, or other autoimmune disease by the patients were evaluated.
GWAS
New information has been obtained from GWAS by identifying important loci associated with PSC using SNP markers. The vast majority of the studies had a large patient sample, providing a good statistical power. Srivastava et al.59 evaluated 992 PSC, and 5,162 HC patients, and found a strong association between PSC and 3p21 macrophage stimulating-1, 10p15 (IL2RA) and 4q27 (IL-2/IL-21). The results showed that the IL-2/IL2RA pathway plays a significant role in PSC. IL-2 acts as a T cell growth factor and increases the cytolytic activity of natural killer cells. Moreover, it is involved in T cell tolerance. IL-21 stimulates B cell differentiation to plasma cells that then leads to the expansion of CD8+ T cells.60 Additional genetic loci have been detected, including 1p36, harbors the MNEL1 and TNFRSF1 genes, and 19q13 responsible for the FUT2 gene. The latter is known for its involvement in host-microbe interactions and altered susceptibility to infectious agents such as the microbiome.61 Other identified gene loci are 2q37 (GPR35), 18Q21 (TCF4), and 2q13 (BCL2L11).61,62 The BCL2L11 gene encodes the Bcl-2 interacting protein that has a critical function in the induction of apoptosis of autoreactive T cells and deletion of activated T cells after an immune response, thus conferring and maintaining immunological tolerance.63 A large northern European GWAS involving 1,186 UC-PSC patients and 1,748 controls found two additional non-HLA UC susceptibility loci associated with PSC, 2p16 (REL) and 9q34 (CARD9). The REL gene is a mediator of the NF-kB inflammatory signaling and CARD9 has a key function in triggering innate immune signaling.64 Table 3 outlines the main findings of studies of genetic factors in the pathogenesis of PSC-IBD.53,55,56,58,59,61,64
Table 3. Overview of the main findings of studies of genetic factors in the pathogenesis of PSC-IBD.
| Genetic risk | |||
|---|---|---|---|
| HLA associations | |||
| HLA subtypes | Study | Findings/associations with PSC-IBD | Weaknesses (−)/Strengths (+) |
| HLA-B8 | Schrumpf et al.53 | 20 patients with UC and hepatobiliary disease and 34 UC patients without hepatobiliary disease and found that 80% of patients with combined disease had HLA-B8 compared to 32% in the UC only group | (−) Small sample size |
| HLA-DR3 | Schrumpf et al.53 | Positive in 70% of patients with combined PSC-UC and in only 35% of the UC only patients | (−) Small sample size |
| HLA-DR2 | Donaldson et al.55 | 69% of the 49 HLA-DR3 negative PSC patients were positive for HLA-DR2 compared to 34% of the -DR3 negative control group | |
| HLA-A1, HLA-B8, HLA-DR3, HLADR6 | Noguchi et al.56 | Frequency of different HLA subtypes between PSC and controls: -A1 42.3% vs. 25.7%, -B8 43.6% vs. 17.1%, -DR3 40% vs. 22.2%, -DR6 40% vs. 7.2% | |
| Inheritance risk | ||
|---|---|---|
| Study | Findings/associations with PSC-IBD | |
| Bergquist et al.58 | Prevalence of 0.7% and around 100-fold higher risk of first-degree relatives to develop PSC | (+) The authors confirmed the diagnosis of PSC with MRCP or ERCP in the patient’s first-degree relatives without relying on questionnaires. (−) all patients were Swedish |
| In the group of patients with PSC only (n=19), the frequency of a first-degree relative with IBD was higher than that in the group of PSC and IBD (26% vs. 9%, p <0.05). | ||
| Genome-wide association studies | ||
|---|---|---|
| Study | Findings/associations with PSC-IBD | |
| Srivastava et al.59 | Strong association between PSC and 3p21 (MST1 which encodes for the macrophage stimulating protein), 10p15 (IL2RA) and 4q27 (IL-2/IL-21) | (+) Good study power |
| Folseraas et al.61 | Associations of PSC with 1p36 that harbors MNEL1 and TNFRSF1 genes and 19q13 responsible for FUT2 gene (important in host-microbe interactions) | (+) Good study power |
| Janse et al.64 | Strong associations of PSC with 2p16 (REL), 9q34 (CARD9). The REL gene is a mediator of the NF-kB inflammatory signaling and CARD9 has a key function in triggering innate immune signaling | (+) Good study power |
PSC-IBD, primary sclerosing cholangitis-inflammatory bowel disease; UC, ulcerative colitis; CD, Crohn’s disease; HLA, human leukocyte antigen.
Impact of Intestinal Microbiota
The fact that gut inflammation might result in “leaky gut” and translocation of bacteria to the portal system and the liver has raised the possibility that bacteria potentially contribute to PSC. To evaluate the hypothesis, Schrumpf et al.65 studied the NOD.c3c4 mouse model which is known to develop spontaneous inflammation of the intrahepatic and extra-hepatic bile ducts as well as NOD control mice. The authors found that the germ-free raised NOD.c3c4 mice had less severe biliary disease compared with conventionally raised NOD.c3c4 mice. In contrast, Tabibian et al.66 compared germ-free multidrug resistance in knockout mdr2(−/−) mice to conventionally housed mdr2(−/−) mice, and found more severe histopathological findings of bile duct fibrosis, ductular reaction, and ductopenia in the germ-free mdr2(−/−) mice.
Bajer et al.67 investigated stool samples and found that differences in the gut microbiota of in PSC-IBD and in IBD only were not significant. It should be noted that the PSC only, PSC-IBD, and UC groups all had high-frequency exposure to ursodeoxycholic acid, 5-aminosalicylic acid, corticosteroids, azathioprine, anti-TNF alpha, and more importantly probiotics. The HC patients did not have any exposure to those medications, which may have affected the results. Kummen et al.68 collected and analyzed stool samples from 85 patients with PSC (50 PSC-UC and 11 PSC-CD), 263 with HC, and 36 with UC and without liver disease. They found a lower bacterial biodiversity in the whole population of PSC patients compared with HC and a distinct microbial composition compared with both HC and UC patients. Genus Veillonella was more frequent in the PSC population than in the HC group. Veillonella is a commensal microbe that has been associated with inflammatory diseases such as periodontitis and spondylodiscitis.69,70 Adding to previous findings, Quraishi et al.71 performed 16-rRNA analysis of colonic tissue from patients with IBD only, with PSC-IBD, and with HC. They detected increased Escherichia, Lachnospiraceae, and Megasphera populations in patients with PSC-IBD compared with HC. The PSC-IBD patients also had fewer Prevotella and Roseburia (butyrate producers) species and a near absence of Bacteroides. Unfortunately, the authors did not report whether the IBD or PSC-IBD patients were taking any medications. Liwinski et al.72 found a more Enterococcus faecalis in ductal bile fluid of 43 PSC patients compared with 22 HC patients. Furthermore, the large proportion of Enterococcus faecalis was positively correlated to the concentration of the noxious taurolithocholic acid. The results suggest that the bile-duct damage was potentiated by bacteria, but not a direct cause. The authors obtained samples from other areas of the proximal digestive tract that allowed for control of the effect of possible contamination from endoscopic retrograde cholangiography. Importantly, as the authors mentioned, most patients with PSC were taking ursodeoxycholic acid, which might have affected the results. However, a study of Pereira et al.73 comprised a larger sample, 80 patients with PSC, and 46 controls. There was no significant difference in the bile microbiome in the two groups, but streptococcus abundance was correlated with increased disease severity. The control subjects had abnormal liver enzymes, and the final diagnoses were not stated. Moreover, the indications for endoscopic retrograde cholangiography were not clearly described. Also, patients who had recently received antibiotics were only excluded if the therapy was given within 1 month, which might have impacted the microbiome. Table 4 shows the main findings of studies on the role of the microbiome in the pathogenesis of PSC-IBD.53,67,68,71,73
Table 4. Overview of the main findings of studies of the role of the microbiome in the pathogenesis of PSC-IBD.
| Impact of intestinal microbiota | ||
|---|---|---|
| Study | Findings/associations with PSC-IBD | Weaknesses (−)/Strengths (+) |
| Schrumpf et al.53 | Germ-free raised NOD.c3c4 mice had less severe biliary disease compared to conventionally raised NOD.c3c4 | |
| Bajer et al.67 | Investigated stool samples and found that the gut microbiota was not significantly different between the PSC-IBD and IBD only groups which differ from HC | (−) Study groups had exposure to UDCA, 5-ASA, corticosteroids, azathioprine, anti-TNF alpha, and more importantly probiotics, whereas the HC did not have any exposure to these medications |
| Kummen et al.68 | Lower bacterial biodiversity in the whole group of PSC compared to HC and a distinct microbial composition compared to both HC and UC groups. The Veillonella genus was more frequent in the PSC population | |
| Quraishi et al.71 | Increased amount of Escherichia, Lachnospiraceae, and Megasphera in the patients with PSC-IBD compared with HC. The PSC-IBD group also had lower levels of Prevotella and Roseburia (butyrate producer) and a near absence of Bacteroides | (−) Authors did not mention if the study group was taking any medications |
| Pereira et al.73 | No significant difference in the bile microbiome among PSC and HC groups, but streptococcus abundance was correlated with higher disease severity | (−) Patients that had recent antibiotics were only excluded if the therapy was given within one month. This could still have impacted the microbiome. |
PSC-IBD, primary sclerosing cholangitis-inflammatory bowel disease; UC, ulcerative colitis; UDCA, ursodeoxycholic acid; 5-ASA, 5-aminosalicylic acid; HC, healthy controls.
Overview of the Clinical Aspects of PSC and IBD
Studies have shown that the intestinal involvement of PSC-IBD patients has specific differences when compared to IBD without hepatic involvement. Moreover, the strong association of PSC and UC compared with CD is well established. A retrospective study investigated 71 PSC-IBD cases and matched them to 142 UC patients with no PSC. Of the 71 cases, 86% had UC, 7% had CD, and 7% had indeterminate colitis.74 There was a high prevalence of pancolitis and evident rectal sparing and backwash ileitis in all three study groups of PSC patients compared with the UC controls. Isolated ileal involvement was rare in the PSC-IBD group. Pancolitis was seen in 87% of PSC-IBD, 92% of PSC-UC, 40% of PSC-CD, and 80% of PSC-indeterminate colitis vs. 54% of UC controls. Fifty-two percent of PSC-IBD patients had rectal sparing compared with only 6% of UC controls. The results showed that PSC-CD patients might be at higher risk for pancolitis than those with CD alone. There were no clinically significance differences of the other variables including sex and age between the two groups in the study. Other studies have shown a higher incidence of PSC-IBD in men, 66% in CD and 76% in UC patients.75 Likely because of the weaker association of PSC with CD compared with UC, there are only few studies attempting to better understand the disease course and characteristics of PSC-CD.
Halliday et al.76 conducted a retrospective study using an Oxford database and investigated the characteristics of PSC-CD, evaluating 32 PSC-CD cases and 64 CD controls. Similar to the prior study, there was a lower rate of isolated ileal disease in the PSC-CD group (6% vs. 31%), a higher rate of ileocolonic involvement in PSC-CD patients than in the control group (44% vs. 24%). There were no significant differences of sex and age at diagnosis between the two groups. The authors also compared the 32 PSC-CD cases with 64 PSC-UC cases. There was a lower frequency of large-duct involvement (78% vs. 94%) and higher rates of small-duct disease in PSC-CD compared with PSC-UC (22% vs. 6%). The PSC-UC group had the worst outcome, with a significantly higher rate of combined cancer, liver transplant, and death.
Small-duct PSC includes a subset of patients with PSC on liver biopsy, but completely normal cholangiograms showing that the large ducts are spared. Progression to classic PSC occurs in a small percentage of those patients.3 When comparing the outcomes of PSC-CD and PSC-UC, there was an association with the type of bile duct involvement. There also was a negative association between UC and small-duct disease. In a large study including 240 PSC cases (105 UC, 32 CD, 14 unclassified IBD, and 89 without IBD), 28% (n=6) of PSC-CD and 3% (n=3) of PSC-UC patients had small-duct involvement compared with 24% (n=21) of PSC and no IBD cases.75 The diagnosis of IBD prior to PSC was made in 61% of PSC-CD cases and 45% of UC ones. The disease severity at the time of PSC diagnosis was similar in the small- and large-duct groups. However, liver disease progression was lower and the survival was remarkably better in the small-duct disease patients. Overall, none of the PSC patients with small-duct disease died of liver disease or colorectal cancer in contrast to 6% and 9%, respectively, of the PSC patients with large-duct disease. Furthermore, colorectal cancer was diagnosed in three of 34 small-duct PSC patients (10%) in contrast to 11 of 206 large-duct PSC patients (5%). Among the large-duct disease patients, those with PSC-CD had far better outcomes. Only one of the 23 patients had liver transplantation, and no patient died from a liver-related cause. The large-duct PSC-UC, PSC-CD, and PSC without IBD patients had a 7% combined mortality from liver disease (n=8, n=1, and n=9 of a total of 102, 23, and 68, respectively) and a 28% rate of liver transplantation. Large-duct PSC-UC and large-duct PSC without IBD groups also had significantly higher rates of cholangiocarcinoma.75 The results are in line with the Oxford study. Aranake-Chrisinger et al.77 also showed an overall better outcome in the PSC-CD group although their study lacked statistical power. Of six PSC-CD cases, none required liver transplantation, but 38% of the 26 PSC-UC patients met the requirements.
It is generally accepted that more extensive colitis including pancolitis occurs in PSC-UC compared with UC without PSC. Furthermore, rectal sparing, and backwash ileitis have been reported as a unique feature of PSC-UC. However, the findings are not specific. Joo et al.78 investigated 40 PSC-UC cases and matched them with 40 UC controls. Although rectal sparing was slightly higher in the PSC-UC group, the difference was not statistically significant. Similarly, there were no statistically significant differences in the presence of backwash ileitis. Because of the high incidence of IBD in patients with PSC, there are limited data comparing the severity of PSC in PSC-IBD patients with that in PSC without IBD. Aranake-Chrisinger et al.77 did not find any statistical difference between the two groups. However, the sample size was very small. A study by Fevery et al.75 showed an overall better outcome in patients with PSC-CD compared with those with PSC-UC and PSC but no IBD. There was a slightly higher rate of liver transplantation in the PSC-UC group compared with PSC and no IBD. However, it was not statistically significant.
Discussion
There is a well-established association between PSC and IBD, with a much higher frequency of PSC-UC compared with PSC-CD. Moreover, the prevalence of PSC and IBD has been increasing worldwide. The three large studies of the epidemiology of PSC done in the UK, USA, and Sweden reported crude prevalences of 6.12, 13.6, and 16.2 per 100,000 persons, respectively. In the same countries, the corresponding crude prevalences of PSC-IBD were 3.3, 9.8 and 12.4 cases per 100,000, all much higher than would be expected by chance for independent events. Furthermore, the majority of the PSC-IBD cases in the studies had a UC diagnosis (61%, 75%, and 84%, respectively). The results from three different populations around the globe support an association of PSC and IBD that is especially strong for PSC and UC.
Recent advances in our understanding of the pathophysiology of these diseases include key genetic characteristics associated with PSC ranging from HLA subtypes to alterations in essential cholangiocyte functions. GWAS results have provided more understanding that genes implicated in innate and adaptive immune responses are associated with this disease. The association of PSC is much stronger for UC than CD, with a different frequency of large versus small bile-duct involvement in PSC-UC versus PSC-CD. The differences suggest that the pathogenesis of cholangiopathy in combined diseases may differ, as do the inflammatory processes in intestinal diseases. The presence of inflammation, and autoantibodies in both UC and PSC raises questions of whether the diseases have a common autoimmune etiology, or whether UC is involved in the autoimmune development of PSC. So far, the data indicate a high variability in the frequency of autoantibodies in PSC. Some studies show rates of ANCA and pANCA as high as 93 and 94%, while others reported rates as low as 42% and 26%. Similarly, in IBD, and in particular UC, high titers of pANCA are common. However, the specificity is low and the frequency of pANCA in PSC-IBD varies considerably among studies. The serological evidence of autoimmune dysregulation in PSC is inconsistent. Nonetheless, P3ANCA has a strong association with both UC and PSC, but larger studies are needed. The fact that, in contrast to acute cases of IBD, treatment of PSC with corticosteroids has been largely unsuccessful makes a high degree of similarity of the autoimmune dysregulation between the diseases less likely. The occurrence of PSC after colectomy in some patients with UC argues against the possibility that UC is involved in the development of PSC, although triggering of an irrevocable autoimmune process by UC resulting in PSC cannot be excluded. As advances in our understanding of the pathophysiology of PSC-IBD continue to grow, manipulation of the mechanisms by which these abnormal immune responses occur, the functional responses of cholangiocytes, and enterohepatic bile flow circulation are likely to lead to the development of new and effective targeted therapies.
Acknowledgments
This work was made possible by the Herman Lopata Chair in Hepatitis Research.
Abbreviations
- AE2
Cl−/HCO3− anion exchanger 2
- AIH
autoimmune hepatitis
- ASBT
sodium dependent transporter
- ASCA
anti-Saccharomyces cerevisiae antibody
- ANA
antinuclear antibody
- ANCA
antineutrophil cytoplasmic antibody
- CD
Crohn’s disease
- CIA
chemiluminescent immunoassay
- CF
cystic fibrosis
- CFTR
cystic fibrosis transmembrane conductance regulator
- FGF
fibroblast growth factor
- FXR
Farnesoid X receptor
- GWAS
genome-wide association studies
- HC
healthy controls
- HLA
human leukocyte antigen
- IBD
inflammatory bowel disease
- LPS
lipopolysaccharide
- MRC
magnetic resonance cholangiography
- PAMPs
pathogen-associated molecular patterns
- PBC
primary biliary cirrhosis
- PRR
pattern recognition receptor
- PSC-CD
primary sclerosing cholangitis and Crohn’s disease
- PSC-IBD
primary sclerosing cholangitis and inflammatory bowel disease
- PSC-UC
primary sclerosing cholangitis and ulcerative colitis
- PSC
primary sclerosing cholangitis
- SASP
senescence-associated secretory phenotype
- SNP
single nucleotide polymorphism
- TGR5
G protein-coupled bile acid receptor 1
- TLR
Toll-like receptor
- UC
ulcerative colitis
- UDCA
ursodeoxycholic acid
References
- 1.Bambha K, Kim WR, Talwalkar J, Torgerson H, Benson J, Therneau T, et al. Incidence, clinical spectrum, and outcomes of primary sclerosing cholangitis in a United States community. Gastroenterol. 2003;125(5):1364–1369. doi: 10.1016/j.gastro.2003.07.011. [DOI] [PubMed] [Google Scholar]
- 2.Ang TL, Fock KM, Ng TM, Teo EK, Chua TS, Tan JYL. Clinical profile of primary sclerosing cholangitis in Singapore. J Gastroenterol Hepatol (Australia) 2002;17(8):908–913. doi: 10.1046/j.1440-1746.2002.02835.x. [DOI] [PubMed] [Google Scholar]
- 3.Escorsell A, Parés A, Rodés J, Solís-Herruzo JA, Miras M, Morena E, et al. Epidemiology of primary sclerosing cholangitis in Spain. J Hepatol. 1994;21(5):787–791. doi: 10.1016/S0168-8278(94)80240-8. [DOI] [PubMed] [Google Scholar]
- 4.Liu K, Wang R, Kariyawasam V, Wells M, Strasser S, McCaughan G, et al. Epidemiology and outcomes of primary sclerosing cholangitis with and without inflammatory bowel disease in an Australian cohort. Liver Int. 2017;37(3):442–448. doi: 10.1111/liv.13328. [DOI] [PubMed] [Google Scholar]
- 5.Liang H, Manne S, Shick J, Lissoos T, Dolin P. Incidence, prevalence, and natural history of primary sclerosing cholangitis in the United Kingdom. Med (United States) 2017;96(24):e7116. doi: 10.1097/MD.0000000000007116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Angulo P, Maor-Kendler Y, Lindor KD. Small-duct primary sclerosing cholangitis: A long-term follow-up study. Hepatology. 2002;35(6):1494–1500. doi: 10.1053/jhep.2002.33202. [DOI] [PubMed] [Google Scholar]
- 7.Weismüller TJ, Trivedi PJ, Bergquist A, Imam M, Lenzel H, Ponsioen CY, et al. Patient age, sex, and inflammatory bowel disease phenotype associate with course of primary sclerosing cholangitis. Gastroenterology. 2017;152(8):1975–1984.e8. doi: 10.1053/j.gastro.2017.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fraga M, Fournier N, Safroneeva E, Pittet V, Sebastien G, Straumann A, et al. Primary sclerosing cholangitis in the Swiss inflammatory bowel disease cohort study: prevalence, risk factors, and long-term follow-up. Eu J Gastroenterol Hepatol. 2017;29(1):91–97. doi: 10.1097/MEG.0000000000000747. [DOI] [PubMed] [Google Scholar]
- 9.O’toole A, Alakkari A, Keegan D, Doherty G, Mulcahy H, O’donoghue D. Primary sclerosing cholangitis and disease distribution in inflammatory bowel disease. YJCGH. 2012;10:439–441. doi: 10.1016/j.cgh.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 10.Ye BD, Yang SK, Boo SJ, Cho YK, Yang DH, Yoon SM, et al. Clinical characteristics of ulcerative colitis associated with primary sclerosing cholangitis in Korea. Inflamm Bowel Dis. 2011;17(9):1901–1906. doi: 10.1002/ibd.21569. [DOI] [PubMed] [Google Scholar]
- 11.Navaneethan U, Venkatesh PGK, Lashner BA, Shen B, Kiran RP. The impact of ulcerative colitis on the long-term outcome of patients with primary sclerosing cholangitis. Aliment Pharmacol Ther. 2012;35(9):1045–1053. doi: 10.1111/j.1365-2036.2012.05063.x. [DOI] [PubMed] [Google Scholar]
- 12.Mueller T, Beutler C, Picó AH, Oren S, Pratt DS, Pascher A, et al. Enhanced innate immune responsiveness and intolerance to intestinal endotoxins in human biliary epithelial cells contributes to chronic cholangitis. Liver Int. 2011;31(10):1574–1588. doi: 10.1111/j.1478-3231.2011.02635.x. [DOI] [PubMed] [Google Scholar]
- 13.Tabibian JH, O’Hara SP, Splinter PL, Trussoni CE, Larusso NF. Cholangiocyte senescence by way of N-Ras activation is a characteristic of primary sclerosing cholangitis. Hepatology. 2014;59(6):2263–2275. doi: 10.1002/hep.26993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marzioni M, Glaser S, Francis H, Phinizy J, LeSage G, Alpini G. Functional heterogeneity of cholangiocytes. Semin Liver Dis. 2002;22(3):227–240. doi: 10.1055/S-2002-34501. [DOI] [PubMed] [Google Scholar]
- 15.Hohenester S, Maillette de Buy Wenniger M, Paulusma CC, van Vliet SJ, Jefferson DM, Oude Elferink RP, et al. A biliary HCO umbrella constitutes a protective mechanism against bile acid-induced injury in human cholangiocytes. Hepatology. 2012;55(1):173–183. doi: 10.1002/hep.24691. [DOI] [PubMed] [Google Scholar]
- 16.Kawamata Y, Fujii R, Hosoya M, Harada M, Yoshida H, Miwa M, et al. A G protein-coupled receptor responsive to bile acids. J Biol Chem. 2003;278(11):9435–9440. doi: 10.1074/jbc.M209706200. [DOI] [PubMed] [Google Scholar]
- 17.Karlsen TH, Franke A, Melum E, Kaser A, Hov JR, Balschun T, et al. Genome-wide association analysis in primary sclerosing cholangitis. Gastroenterology. 2010;138(3):1102–1111. doi: 10.1053/j.gastro.2009.11.046. [DOI] [PubMed] [Google Scholar]
- 18.Hov JR, Keitel V, Laerdahl JK, Spomer L, Ellinghaus E, ElSharawy A, et al. Mutational characterization of the bile acid receptor TGR5 in primary sclerosing cholangitis. PLoS One. 2010;5(8):e12403. doi: 10.1371/journal.pone.0012403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Durieu I, Pellet O, Simonot L, Durupt S, Bellon G, Durand DV, et al. Sclerosing cholangitis in adults with cystic fibrosis: A magnetic resonance cholangiographic prospective study. J Hepatol. 1999;30(6):1052–1056. doi: 10.1016/S0168-8278(99)80259-1. [DOI] [PubMed] [Google Scholar]
- 20.McGill JM, Williams DM, Hunt CM. Survey of cystic fibrosis transmembrane conductance regulator genotypes in primary sclerosing cholangitis. Dig Dis and Sci. 1996;41(3):540–542. doi: 10.1007/BF02282335. [DOI] [PubMed] [Google Scholar]
- 21.Sheth S, Shea JC, Bishop MD, Chopra S, Regan MM, Malmberg E, et al. Increased prevalence of CFTR mutations and variants and decreased chloride secretion in primary sclerosing cholangitis. Hum Genet. 2003;113(3):286–292. doi: 10.1007/s00439-003-0963-z. [DOI] [PubMed] [Google Scholar]
- 22.Sasaki M, Sato Y, Nakanuma Y. An impaired biliary bicarbonate umbrella may be involved in dysregulated autophagy in primary biliary cholangitis. Lab Invest. 2018;98(6):745–754. doi: 10.1038/s41374-018-0045-4. [DOI] [PubMed] [Google Scholar]
- 23.Kempinska-Podhorodecka A, Adamowicz M, Ostrycharz E, Chmielarz M, Wojcicki M, Milkiewicz P, et al. Role of miR-506 in ulcerative colitis associated with primary sclerosing cholangitis. Sci Rep. 2021;11(1):1–13. doi: 10.1038/s41598-021-89631-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kliewer S, Mangelsdorf D. Bile Acids as Hormones: The FXR-FGF15/19 pathway. Dig Dis (Basel, Switzerland) 2015;33(3):327–331. doi: 10.1159/000371670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Trauner M, Gulamhusein A, Hameed B, Caldwell S, Shiffman M, Landis C, et al. The Nonsteroidal Farnesoid X Receptor Agonist Cilofexor (GS-9674) Improves Markers of Cholestasis and Liver Injury in Patients With Primary Sclerosing Cholangitis. Hepatology (Baltimore, Md) 2019;70(3):788–801. doi: 10.1002/HEP.30509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vavassori P, Mencarelli A, Renga B, Distrutti E, Fiorucci S. The bile acid receptor FXR is a modulator of intestinal innate immunity. J Immunol. 2009;183(10):6251–6261. doi: 10.4049/JIMMUNOL.0803978. [DOI] [PubMed] [Google Scholar]
- 27.Hegade VS, Jones DEJ, Hirschfield GM. Apical sodium-dependent transporter inhibitors in primary biliary cholangitis and primary sclerosing cholangitis. Dig Dis. 2017;35(3):267–274. doi: 10.1159/000450988. [DOI] [PubMed] [Google Scholar]
- 28.Milkiewicz M, Klak M, Kempinska-Podhorodecka A, Wiechowska-Kozlowska A, Urasinska E, Blatkiewicz M, et al. Impaired hepatic adaptation to chronic cholestasis induced by primary sclerosing cholangitis. Sci Rep. 2016;6(1):1–12. doi: 10.1038/srep39573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ponsioen CY, Kuiper H, Ten Kate FJ, van Milligen De Wit M, van Deventer SJ, Tytgat GN. Immunohistochemical analysis of inflammation in primary sclerosing cholangitis. Eur J Gastroenterol Hepatol. 1999;11(7):769–774. doi: 10.1097/00042737-199907000-00015. [DOI] [PubMed] [Google Scholar]
- 30.Ong J, Bath MF, Swift C, Al-Naeeb Y. Does colectomy affect the progression of primary sclerosing cholangitis? A systematic review and meta-analysis. Gastroenterol Hepatol Bed Bench. 2018;11(4):277–283. doi: 10.22037/ghfbb.v11i4.1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Befeler AS, Lissoos TW, Schiano TD, Conjeevaram H, Dasgupta KA, Millis JM, et al. Clinical course and management of inflammatory bowel disease after liver transplantation. Transplantation. 1998;65(3):393–396. doi: 10.1097/00007890-199802150-00017. [DOI] [PubMed] [Google Scholar]
- 32.McNab G, Reeves J, Salmi M, Hubscher S, Jalkanen S, Adams D. Vascular adhesion protein 1 mediates binding of T cells to human hepatic endothelium. Gastroenterology. 1996;110(2):522–528. doi: 10.1053/GAST.1996.V110.PM8566600. [DOI] [PubMed] [Google Scholar]
- 33.Grant AJ, Lalor PF, Salmi M, Jalkanen S, Adams DH. Homing of mucosal lymphocytes to the liver in the pathogenesis of hepatic complications of inflammatory bowel disease. Lancet. 2002;359(9301):150–157. doi: 10.1016/S0140-6736(02)07374-9. [DOI] [PubMed] [Google Scholar]
- 34.Kekilli M, Tunc B, Beyazit Y, Kurt M, Koral Onal I, Ulker A, et al. Circulating CD4+CD25+ regulatory t cells in the pathobiology of ulcerative colitis and concurrent primary sclerosing cholangitis. Dig Dis Sci. 2013;58(5):1250–1255. doi: 10.1007/s10620-012-2511-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harada K, Nakanuma Y. Biliary innate immunity: function and modulation. Mediators Inflamm. 2010;2010:373878. doi: 10.1155/2010/373878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Medvedev AE, Sabroe I, Hasday JD, Vogel SN. Tolerance to microbial TLR ligands: Molecular mechanisms and relevance to disease. J Endotoxin Res. 2006;12(3):133–150. doi: 10.1179/096805106X102255. [DOI] [PubMed] [Google Scholar]
- 37.Cullen SW, Chapman RW. The medical management of primary sclerosing cholangitis. Semin Liver Dis. 2006;26(1):52–61. doi: 10.1055/s-2006-933563. [DOI] [PubMed] [Google Scholar]
- 38.Hov JR, Boberg KM, Karlsen TH. Autoantibodies in primary sclerosing cholangitis. World J Gastroenterol. 2008;14(24):3781–3791. doi: 10.3748/wjg.14.3781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Seibold F, Weber P, Klein R, Berg P, Wiedmann K. Clinical significance of antibodies against neutrophils in patients with inflammatory bowel disease and primary sclerosing cholangitis. Gut. 1992;33(5):657–662. doi: 10.1136/GUT.33.5.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lo S, Fleming K, Chapman R. Prevalence of anti-neutrophil antibody in primary sclerosing cholangitis and ulcerative colitis using an alkaline phosphatase technique. Gut. 1992;33(10):1370–1375. doi: 10.1136/GUT.33.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Seibold F, Weber P, Klein R, Berg PA, Wiedmann KH. Clinical significance of antibodies against neutrophils in patients with inflammatory bowel disease and primary sclerosing cholangitis. Gut. 1992;33(5):657–662. doi: 10.1136/GUT.33.5.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xu B, Broome U, Ericzon BG, Sumitran-Holgersson S. High frequency of autoantibodies in patients with primary sclerosing cholangitis that bind biliary epithelial cells and induce expression of CD44 and production of interleukin 6. Gut. 2002;51(1):120–127. doi: 10.1136/gut.51.1.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ge X, Ericzon B, Nowak G, öHrström H, Broomé U, Sumitran-Holgersson S. Are preformed antibodies to biliary epithelial cells of clinical importance in liver transplantation? Liver Transpl. 2003;9(11):1191–1198. doi: 10.1053/JLTS.2003.50236. [DOI] [PubMed] [Google Scholar]
- 44.Roozendaal C, de Jong MA, van den Berg AP, van Wijk RT, Limburg PC, Kallenberg CGM. Clinical significance of anti-neutrophil cytoplasmic antibodies (ANCA) in autoimmune liver diseases. J Hepatol. 2000;32(5):734–741. doi: 10.1016/S0168-8278(00)80241-X. [DOI] [PubMed] [Google Scholar]
- 45.Seibold F, Weber P, Klein R, Berg PA, Wiedmann KH. Clinical significance of antibodies against neutrophils in patients with inflammatory bowel disease and primary sclerosing cholangitis. Gut. 1992;33(5):657–662. doi: 10.1136/gut.33.5.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pokorny CS, Norton ID, McCaughan GW, Selby WS. Anti-neutrophil cytoplasmic antibody: A prognostic indicator in primary sclerosing cholangitis. J Gastroenterol Hepatol. 1994;9(1):40–44. doi: 10.1111/j.1440-1746.1994.tb01214.x. [DOI] [PubMed] [Google Scholar]
- 47.Mahler M, Bogdanos DP, Pavlidis P, Fritzler MJ, Csernok E, Damoiseaux J, et al. PR3-ANCA: a promising biomarker for ulcerative colitis with extensive disease. Clin Chim Acta. 2013;424:267–273. doi: 10.1016/j.cca.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 48.Stinton LM, Bentow C, Mahler M, Norman GL, Eksteen B, Mason AL, et al. PR3-ANCA: A Promising Biomarker in Primary Sclerosing Cholangitis (PSC) PLoS One. 2014;9(11):e112877. doi: 10.1371/journal.pone.0112877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Walker LJ, Aldhous MC, Drummond HE, Smith BRK, Nimmo ER, Arnott IDR, et al. Anti-Saccharomyces cerevisiae antibodies (ASCA) in Crohn’s disease are associated with disease severity but not NOD2/CARD15 mutations. Clin Exp Immunol. 2004;135(3):490. doi: 10.1111/J.1365-2249.2003.02392.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Muratori P, Muratori L, Guidi M, Maccariello S, Pappas G, Ferrari R, et al. Anti-Saccharomyces cerevisiae antibodies (ASCA) and autoimmune liver diseases. Clin Exp Immunol. 2003;132(3):473. doi: 10.1046/J.1365-2249.2003.02166.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Angulo P, Peter JB, Gershwin ME, DeSotel CK, Shoenfeld Y, Ahmed AE, et al. Serum autoantibodies in patients with primary sclerosing cholangitis. J Hepatol. 2000;32(2):182–187. doi: 10.1016/S0168-8278(00)80061-6. [DOI] [PubMed] [Google Scholar]
- 52.Chen P, Zhou G, Lin J, Li L, Zeng Z, Chen M, et al. Serum biomarkers for inflammatory bowel disease. Front Med (Lausanne) 2020;7:123. doi: 10.3389/FMED.2020.00123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schrumpf E, Fausa O, Førre, Dobloug JH, Ritland S, Thorsby E. HLA antigens and immunoregulatory t cells in ulcerative colitis associated with hepatobiliary disease. Scand J Gastroenterol. 1982;17(2):187–191. doi: 10.3109/00365528209182038. [DOI] [PubMed] [Google Scholar]
- 54.Chapman RW, Varghese Z, Gaul R, Patel G, Kokinon N, Sherlock S. Association of primary sclerosing cholangitis with HLA-B8. Gut. 1983;24(1):38–41. doi: 10.1136/gut.24.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Donaldson PT, Farrant JM, Wilkinson ML, Hayllar K, Portmann BC, Williams R. Dual association of HLA DR2 and DR3 with primary sclerosing cholangitis. Hepatology. 1991;13(1):129–133. doi: 10.1002/hep.1840130119. [DOI] [PubMed] [Google Scholar]
- 56.Noguchi K, Kobayashi M, Yagihashi A, Yoshida Y, Terasawa K, Konno A, et al. HLA antigens in primary sclerosing cholangitis. Transplant Proc. 1992;24(6):2775–2776. [PMC free article] [PubMed] [Google Scholar]
- 57.Wiencke K, Spurkland A, Schrumpf E, Boberg KM. Primary sclerosing cholangitis is associated to an extended B8-DR3 haplotype including particular MICA and MICB alleles. Hepatology. 2001;34(4):625–630. doi: 10.1053/jhep.2001.27543. [DOI] [PubMed] [Google Scholar]
- 58.Bergquist A, Lindberg G, Saarinen S, Broomé U. Increased prevalence of primary sclerosing cholangitis among first-degree relatives. J Hepatol. 2005;42(2):252–256. doi: 10.1016/j.jhep.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 59.Srivastava B, Mells GF, Cordell HJ, Muriithi A, Brown M, Ellianghaus E, et al. Fine mapping and replication of genetic risk loci in primary sclerosing cholangitis. Scand J Gastroenterol. 2012;47(7):820–826. doi: 10.3109/00365521.2012.682090. [DOI] [PubMed] [Google Scholar]
- 60.Rochman Y, Spolski R, Leonard W. New insights into the regulation of T cells by gamma(c) family cytokines. Nat Rev Immunol. 2009;9(7):480–490. doi: 10.1038/NRI2580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Folseraas T, Melum E, Rausch P, Juran BD, Ellinghaus E, Shiryaev A, et al. Extended analysis of a genome-wide association study in primary sclerosing cholangitis detects multiple novel risk loci. J Hepatol. 2012;57(2):366–375. doi: 10.1016/j.jhep.2012.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ellinghaus D, Folseraas T, Holm K, Ellinghaus E, Melum E, Balschun T, et al. Genome-wide association analysis in primary sclerosing cholangitis and ulcerative colitis identifies risk loci at GPR35 and TCF4. Hepatology. 2013;58(3):1074–1083. doi: 10.1002/hep.25977. [DOI] [PubMed] [Google Scholar]
- 63.Melum E, Franke A, Schramm C, Weismuller T, Gotthardt DN, Offner FA, et al. Genome-wide association analysis in primary sclerosing cholangitis identifies two non-HLA susceptibility loci. Nat Genet. 2011;43(1):17–19. doi: 10.1038/ng.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Janse M, Lamberts L, Franke L, Raychaudhuri S, Ellinghaus E, Muri Boberg K, et al. Three ulcerative colitis susceptibility loci are associated with primary sclerosing cholangitis and indicate a role for IL2, REL, and CARD9. Hepatology. 2011;53(6):1977–1985. doi: 10.1002/HEP.24307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schrumpf E, Kummen M, Valestrand L, Greiner TU, Holm K, Arulampalam V, et al. The gut microbiota contributes to a mouse model of spontaneous bile duct inflammation. J Hepatol. 2017;66(2):382–389. doi: 10.1016/J.JHEP.2016.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tabibian J, O’Hara S, Trussoni C, Tietz PS, Splinter PL, Mounajjed T, et al. Absence of the intestinal microbiota exacerbates hepatobiliary disease in a murine model of primary sclerosing cholangitis. Hepatology. 2016;63(1):185–196. doi: 10.1002/HEP.27927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bajer L, Kverka M, Kostovcik M, Macinga P, Dvorak J, Stehlikova Z, et al. Distinct gut microbiota profiles in patients with primary sclerosing cholangitis and ulcerative colitis. World J Gastroenterol. 2017;23(25):4548. doi: 10.3748/WJG.V23.I25.4548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kummen M, Holm K, Anmarkrud JA, Nygard S, Vesterhus M, Høivik ML, et al. The gut microbial profile in patients with primary sclerosing cholangitis is distinct from patients with ulcerative colitis without biliary disease and healthy controls. Gut. 2017;66(4):611–619. doi: 10.1136/gutjnl-2015-310500. [DOI] [PubMed] [Google Scholar]
- 69.Gouze H, Noussair L, Padovano I, Salomon E, de Laroche M, Duran C, et al. Veillonella parvula spondylodiscitis. Med Mal Infect. 2019;49(1):54–58. doi: 10.1016/J.MEDMAL.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 70.Yamashita Y, Takeshita T. The oral microbiome and human health. J Oral Sci. 2017;59(2):201–206. doi: 10.2334/JOSNUSD.16-0856. [DOI] [PubMed] [Google Scholar]
- 71.Quraishi M, Sergeant M, Kay G, Tariq I, Jacqueline C, Constantinidou C, et al. The gut-adherent microbiota of PSC-IBD is distinct to that of IBD. Gut. 2017;66(2):386–388. doi: 10.1136/GUTJNL-2016-311915. [DOI] [PubMed] [Google Scholar]
- 72.Liwinski T, Zenouzi R, John C, Ehlken H, Rühlemann M, Bang C, et al. Alterations of the bile microbiome in primary sclerosing cholangitis. Gut. 2020;69(4):665–672. doi: 10.1136/GUTJNL-2019-318416. [DOI] [PubMed] [Google Scholar]
- 73.Pereira P, Aho V, Arola J, Boyd S, Jokelainen K, Paulin L, et al. Bile microbiota in primary sclerosing cholangitis: Impact on disease progression and development of biliary dysplasia. PloS One. 2017;12(8):e0182924. doi: 10.1371/JOURNAL.PONE.0182924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Loftus EV, Jr, Harewood GC, Loftus CG, Tremaine WJ, Harmsen WS, Zinsmeister AR, et al. PSC-IBD: a unique form of inflammatory bowel disease associated with primary sclerosing cholangitis. Gut. 2005;54(1):91–96. doi: 10.1136/GUT.2004.046615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fevery J, van Steenbergen W, van Pelt J, Laleman W, Hoffman I, Geboes K, et al. Patients with large-duct primary sclerosing cholangitis and Crohn’s disease have a better outcome than those with ulcerative colitis, or without IBD. Aliment Pharmacol Ther. 2016;43(5):612–620. doi: 10.1111/apt.13516. [DOI] [PubMed] [Google Scholar]
- 76.Halliday JS, Djordjevic J, Lust M, Culver EL, Braden B, Travis SPL, et al. A unique clinical phenotype of primary sclerosing cholangitis associated with Crohn’s disease. J Crohns Colitis. 2012;6(2):174–181. doi: 10.1016/j.crohns.2011.07.015. [DOI] [PubMed] [Google Scholar]
- 77.Aranake-Chrisinger J, Dassopoulos T, Yan Y, Nalbantoglu I. Primary sclerosing cholangitis associated colitis: Characterization of clinical, histologic features, and their associations with liver transplantation. World J Gastroenterol. 2020;26(28):4126–4139. doi: 10.3748/wjg.v26.i28.4126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Joo M, Abreu-E-Lima P, Farraye F, Smith T, Swaroop P, Gardner L, et al. Pathologic features of ulcerative colitis in patients with primary sclerosing cholangitis: A case-control study. Am J Surg Pathol. 2009;33(6):854–862. doi: 10.1097/PAS.0b013e318196d018. [DOI] [PubMed] [Google Scholar]