Abstract
Background and Aims
Alcohol-associated liver disease (ALD) is the most common cause of advanced liver disease worldwide, including in the USA. Alcohol use and cirrhosis mortality is higher in American Indian/Alaska Native (AI/AN) compared to Whites. Data are scanty on ALD as a liver disease etiology in AI/AN compared to other races and ethnicities.
Methods
The National Inpatient Sample on 199,748 cirrhosis-related hospitalizations, 14,241 (2,893 AI/AN, 2,893 Whites, 2,882 Blacks, 2,879 Hispanics, and 2,694 Asians or other races) matched 1:1 for race/ethnicity on demographics, insurance, and income quartile of the residence zip code analyzed.
Results
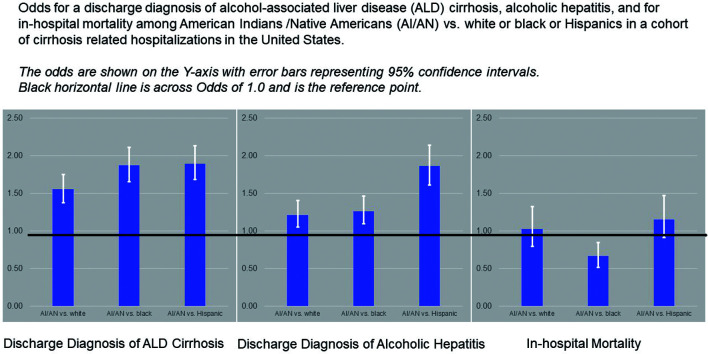
After controlling for geographic location and hospital type, odds ratio (OR) and 95% confidence interval (CI) for ALD as cirrhosis etiology was higher among admissions in AI/AN vs. Whites [1.55 (1.37–1.75)], vs. Blacks [1.87 (1.65–2.11)], vs. Hispanic [1.89 (1.68–2.13)] and Asians/other races [2.24 (1.98–2.53)]. OR was also higher for AI/AN vs. all other races for alcohol-associated hepatitis (AH) as one of the discharge diagnoses. The findings were similar in a subgroup of 4,649 admissions with decompensated cirrhosis and in a cohort of 350 admissions with acute-on-chronic liver failure as defined by EASL-CLIF criteria. Alcohol use disorder diagnosis was present in 38% of admissions in AI/AN vs. 24–30% in other races, p<0.001. A total of 838 (5.9%) admissions were associated with in-hospital mortality. OR (95% CI) for in-hospital mortality in AI/AN individuals was 34% reduced vs. Blacks [0.66 (0.51–0.84)], but no difference was observed on comparison with other races.
Conclusions
ALD, including AH, is the most common etiology among cirrhosis-related hospitalizations in the USA among AI/AN individuals. In-hospital mortality was observed in about 6% of admissions, which was higher for Blacks and similar in other races compared to admissions for AI/AN. Public health policies should be implemented to reduce the burden of advanced ALD among AI/AN individuals.
Keywords: American Indians, Alaska Natives, Native Americans, Healthcare burden, Epidemiology, Magnitude, Transplant
Graphical abstract
Introduction
Alcohol-associated liver disease (ALD) is one of the most common liver diseases worldwide, leading to advanced fibrosis and alcohol-associated cirrhosis (AC) in 10–20% of cases.1 Further, advanced fibrosis among individuals at risk for ALD is increasing in the USA, from 2.2% in 2001 to 6.6% in 2016.2 In 2017, a total of 123 million people worldwide and about 2.2 million in the USA had AC.3 Currently, ALD is the leading indication for liver transplantation (LT), with over 40% of LTs in the USA performed in 2018 for this indication.4 AC contributes to about 27% of all cirrhosis-related deaths, with a total of 332,268 deaths due to AC in 2017 in the USA.3
Patients with ALD are often hospitalized for complications of cirrhosis or for more severe forms of the disease with alcohol-associated hepatitis (AH) or acute-on-chronic liver failure (ACLF). The proportion of all chronic liver disease hospitalizations in the USA due to ALD is increasing, having risen from 19.4% in 2012 to 37.7% in 2016, with an estimated direct cost of hospitalizations of $22.7 billion during that period.5 Patient mortality during ALD-related hospitalization is about 12%5 and can be up to approximately 40% for those with ACLF.6
American Indian/Alaska Native (AI/AN) contribute to about 1.7% of the USA population, with a total of about 5.2 million AI/AN individuals according to the 2010 census.7 Mortality among AI/AN individuals has been shown to be disproportionately higher compared to Whites for many diseases, including chronic liver disease and cirrhosis.8–10 Increased use of alcohol and other recreational drugs in the AI/AN population is likely contributing to the high rates of cirrhosis-related mortality. For example, AC-related mortality in the 45–64 years-old age group was 75 per 100,000 individuals with AI/AN race but was only 15 per 100,000 in White individuals.8 However, data are scanty in cirrhosis patients comparing ALD as cirrhosis etiology in AI/AN vs. other races and ethnicities. In a cohort of hospitalized patients with cirrhosis in the USA, we compared AI/AN to matched cohorts of other races for ALD as cause of liver disease, AH as discharge diagnosis, and in-hospital mortality. We also examined subgroup cohorts with decompensated cirrhosis or with ACLF.
Methods
Study population
The National Inpatient Sample (NIS) database was used for the study. Using the Healthcare Cost and Utilization Project, the NIS database was developed and is maintained by the Agency for Healthcare Research and Quality, and is the largest inpatient database in the USA, representing hospital discharges from 46 states (approximately 97% of the USA’s population). It contains data from over 7 million hospital discharges annually, yielding national estimates of hospital inpatient stays. The NIS includes up to 25 discharge diagnoses using the International Classification of Diseases (ICD) codes. The clinical discharge records also include patient demographics, payer status, procedure codes, hospital costs, comorbidities, inpatient mortality, and hospital characteristics, such as region and teaching status. As the ICD code changed from ICD-09 to ICD-10 from 10/01/2015, cirrhosis-related hospitalizations in the NIS database (10/01/2015–12/31/2016) were identified using one of the discharge diagnosis ICD-10 codes (Supplementary Table 1).11
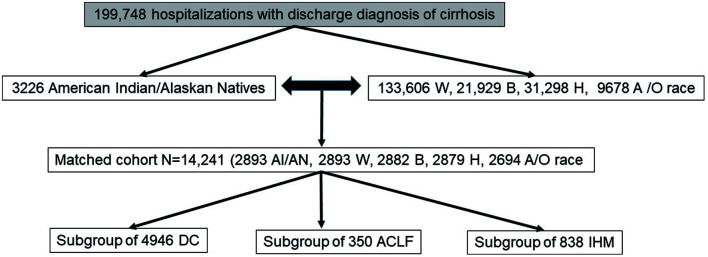
Hospitalizations with AI/AN race identification were matched 1:1 on demographics (age and sex) and the socio-economic status [insurance and income quartile of the residence zip code] to each of the other race and ethnicity groups. As 71% of AI/AN people according to the 2010 census have migrated to urban cities for better education, housing, and employment, matching was also done for the type of hospital (urban vs. rural and teaching vs. non-teaching). From this matched cohort, subgroups of hospitalizations with decompensated cirrhosis, with ACLF, or with in-hospital mortality were extracted (Fig. 1). The whole and subgroup cohorts were examined for primary and secondary outcomes. As the cirrhosis-related disparities in AI/AN individuals may be related to their socioeconomic status,12 the analyses were controlled for this potential confounder. The denominator for all the analyses is the number of admissions and not the number of patients, as the database does not allow linking an admission to a patient identifier.
Fig. 1. Flow diagram of study population cohort matched for AI/AN with other races or ethnicities.
W, Whites; B, Blacks; H, Hispanics; A/O, Asian or other races; DC, decompensated cirrhosis; ACLF, acute-on-chronic liver failure; IHM, In-hospital mortality.
Outcomes
Primary outcome was ALD as cause for hospitalization, identified using the ICD-10 codes (K70.30 and K70.31 for AC, K70.10 and K70.11 for AH) (Supplementary Table 1).6,13 Secondary outcome was hospitalization with one of the discharge diagnoses of AH.
Definitions
AI/AN
The NIS database captures the information on self-reported race of the patient and is stratified in the database to White, Black, Hispanic, AI/AN, Asian or other race.
Socioeconomic status
Insurance status (Medicare, Medicaid, Private or other) and quartile distribution on the median household income of the residents zip code (first quartile as poorest and fourth quartile as the wealthiest population) were used to define the socioeconomic status.14
Decompensated cirrhosis
This was defined by the presence of either of complications of ascites, hepatic encephalopathy, or variceal bleeding. ICD-10 codes used for these are presented in Supplementary Table 1.
ACLF
As the NIS database does not provide laboratory values, ACLF among ALD-related admissions was defined using the North American Consortium for the Study of End-Stage Liver Disease definition, with presence of two or more extrahepatic organ failures.6,15 Those with three and four organ failures defined ACLF-2 and ACLF-3 grades respectively. ICD-10 codes were used to define cardiovascular failure (central venous pressure, arterial line, pulmonary wedge pressure, septic shock), pulmonary failure (mechanical ventilation), brain failure (hepatic encephalopathy), and renal failure (dialysis or hepatorenal syndrome), as shown in Supplementary Tables 1 and 2.6,16 Brain failure stratification was modified to include anyone with a discharge ICD-10 diagnosis code of hepatic encephalopathy, and not limiting to those with grade 3–4 encephalopathy.
Statistical analyses
Baseline characteristics of cirrhosis-related hospitalizations were compared when stratified by race of AI/AN against the other races. Chi-square test was used for comparing categorical variables. For the continuous variables, analysis of variance test was used for comparing means and non-parametric test for comparing medians. Multivariate logistic regression analysis models were built to determine independent association of AI/AN race with the primary outcome of ALD etiology and the secondary outcome of AH. We also performed a similar model with in-hospital mortality as the outcome. Variables significantly different at baseline and other clinically relevant ones were included in the models. A p-value of <0.05 was considered significant. SAS version 9.4 (SAS Institute, Cary, NC, USA) was used for statistical analyses.
Results
Study population
Between 10/01/2015 and 12/31/2016, there were 199,748 hospitalizations with discharge diagnosis of cirrhosis. Among them, 3,226 (1.6%) hospitalizations were for AI/AN compared to those for other races (133,306 Whites, 21,929 Blacks, 31,298 Hispanics, and 9,678 Asian or other race/ethnicity). AI/AN individuals were more likely to be younger, female, clustered in mountain and west north central divisions, below-median income, insured with Medicaid pay source, ALD etiology, and disease status of decompensated (Supplementary Table 3). A matched cohort of 14,241 hospitalizations (2,893 AI/AN, 2,893 Whites, 2,882 Blacks, 2,879 Hispanics, and 2,694 Asian or other race) was examined for further analyses.
Comparison of hospitalizations in AI/AN vs. other races
Analysis of the entire cohort
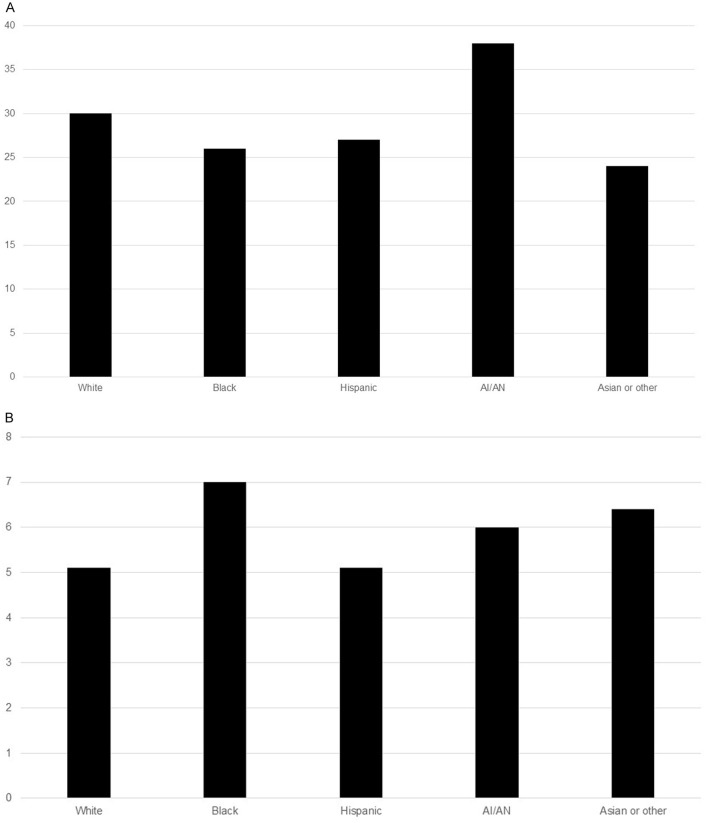
After matching for age, sex, type of hospital (urban vs. rural and teaching vs. non-teaching), and the socioeconomic status, hospitalizations in AI/AN individuals compared to all other races were more likely to have decompensated disease and discharged with a diagnosis of ALD or AH (Table 1). Admissions in AI/AN individuals compared to other races had higher frequency of alcohol use disorder (AUD) (38 vs. 24–30%, p<0.001) (Fig. 2A). In a logistic regression model controlling for demographics (age, sex, and race), payer source, zip code income quartile, and hospital type, hospitalization with AI/AN compared to White race was 55% [1.55 (1.37–1.75)] and 21% [1.21 (1.05–1.40)] were more likely to be discharged with a diagnosis of ALD and AH respectively. We also performed univariate association between each covariate and discharge diagnosis of ALD or of AH (Supplementary Table 4). Odds of ALD and of AH as cause of admission were also higher in AI/AN by, respectively, 1.87 and 1.26 compared with Black, 1.89 and 1.86 compared with Hispanic, and 2.24 and 1.72 compared with Asian or other races. Other predictors of ALD or AH etiology were young age, male sex, Medicaid or private insurance, and admission in a rural or urban non-teaching hospital (Table 2).
Table 1. Baseline characteristics of hospitalizations in the USA with discharge diagnosis of cirrhosis.
| White (n=2,893) | Black (n=2,882) | Hispanic (n=2,879) | Asian or other (n=2,694) | AI/NA (n=2,893) | p | |
|---|---|---|---|---|---|---|
| Age in years (mean, SD) | 52, 13 | 52, 14 | 51, 15 | 52, 15 | 52, 13 | 0.087 |
| % Females | 44 | 44 | 43 | 42 | 45 | 0.72 |
| % Elective admissions | 8.2 | 8.4 | 7.3 | 7.4 | 8.5 | 0.84 |
| % Pay source (MC, MD, Pvt.) | 29, 49, 22 | 30, 49, 21 | 29, 51, 20 | 31, 48, 21 | 29, 49, 22 | 0.98 |
| % Hospital type (R, U non-teaching, U teaching) | 15, 17, 68 | 14, 16, 70 | 14, 16, 70 | 7, 19, 74 | 15, 17, 68 | 0.044 |
| % Zip code income quartile (Q1–Q4) | 55, 24, 15, 6 | 55, 24, 15, 6 | 53, 26, 15, 6 | 52, 26, 16, 6 | 54, 25, 15, 6 | 0.26 |
| % Alcohol-associated cirrhosis | 38 | 31 | 40 | 33 | 50 | <0.001 |
| % Alcohol-associated hepatitis | 24 | 22 | 18 | 19 | 28 | 0.038 |
| % Alcohol-associated liver disease | 53 | 47 | 49 | 44 | 64 | <0.001 |
| % HCV cirrhosis | 10.3 | 12 | 11.5 | 10.4 | 9.1 | 0.029 |
| % NASH cirrhosis | 8.8 | 5.3 | 9.7 | 6.1 | 8.2 | 0.75 |
| % Decompensated cirrhosis | 35 | 28 | 37 | 33 | 40 | <0.001 |
SD: Standard deviation; MC, Medicare; MD, Medicaid; NASH, nonalcoholic steatohepatitis; Q, quartile; Pvt., private; R, rural; U, urban.
Fig. 2. Proportion of admissions for different races associated with AUD, p<0.001 (A) and in-hospital mortality, p=0.36 (B).
Table 2. Logistic regression multivariable analyses on the matched cohort of hospitalizations with cirrhosis for predictors of ALD or of AH as etiology of liver disease.
| Predictors of discharge diagnosis of ALD |
Predictors of discharge diagnosis of AH |
|||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Age in years | 0.977 (0.974–0.980) | <0.001 | 0.959 (0.956–0.962) | <0.001 |
| Female vs. Male | 0.50 (0.46–0.53) | <0.001 | 0.67 (0.62–0.73) | <0.001 |
| Medicaid vs. Medicare | 2.22 (2.0–2.4) | <0.001 | 2.03 (1.79–2.32) | <0.001 |
| Pvt. vs. Medicare | 1.87 (1.68–2.08) | <0.001 | 2.13 (1.85–2.46) | <0.001 |
| AI/AN vs. White | 1.55 (1.37–1.75) | <0.001 | 1.21 (1.05–1.40) | <0.001 |
| AI/AN vs. Black | 1.87 (1.65–2.11) | <0.001 | 1.26 (1.09–1.46) | <0.001 |
| AI/AN vs. Hispanic | 1.89 (1.68–2.13) | <0.001 | 1.86 (1.61–2.14) | <0.001 |
| AI/AN vs. Asian or other | 2.24 (1.98–2.53) | <0.001 | 1.72 (1.48–2.00) | <0.001 |
| Rural vs. Urban teaching hospital | 1.11 (0.99–1.24) | 0.94 | 1.30 (1.14–1.48) | 0.027 |
| Urban non-teaching vs. Urban teaching hospital | 1.23 (1.11–1.35) | <0.004 | 1.12 (0.99–1.26) | 0.73 |
| Zip income Quartile 1 vs. 4 | 0.90 (0.77–1.05) | 0.086 | 0.63 (0.53–0.76) | <0.001 |
| Zip income Quartile 2 vs. 4 | 0.94 (0.80–1.09) | 0.77 | 0.71 (0.59–0.86) | 0.03 |
| Zip income Quartile 3 vs. 4 | 0.95 (0.80–1.13) | 0.87 | 0.82 (0.68–0.997) | 0.28 |
OR, Odds ratio; CI, Confidence interval; AI/AN, American Indian/Alaska Native.
Subgroup of hospitalizations with decompensated cirrhosis
Among the 4,649 hospitalizations with decompensated cirrhosis within the matched cohort, hospitalizations for AI/AN individuals compared to all other races were more likely to be due to ALD, including AH (Table 3). There was no difference on proportion of hospitalizations on cirrhosis-related complications (Supplementary Fig. 1). In an adjusted logistic regression model, hospitalization with AI/AN compared to White race was 30% [1.30 (1.04–1.63)] and 38% [1.38 (1.10–1.74)] were more likely to be due to ALD and AH, respectively. Admission in AI/AN compared to other races was also associated with increased odds of ALD or AH as discharge diagnosis. Other predictors of ALD or AH etiology were young age, male sex, and Medicaid or private insurance (Supplementary Table 5).
Table 3. Baseline characteristics of hospitalizations in the US with decompensated cirrhosis.
| White (n=1,006) | Black (n=819) | Hispanic (n=1,066) | Asian or other (n=890) | AI/NA (n=1,165) | p | |
|---|---|---|---|---|---|---|
| Age in years (mean, SD) | 51, 12 | 52, 14 | 51, 13 | 52, 14 | 52, 12 | 0.55 |
| % Females | 41 | 46 | 44 | 40 | 45 | 0.7 |
| % Elective admissions | 5.6 | 7.2 | 5.4 | 5.1 | 6.8 | 0.72 |
| % Pay source (MC, MD, Pvt.) | 25, 53, 22 | 29, 48, 23 | 27, 54, 19 | 28, 50, 22 | 29, 51, 20 | 0.77 |
| % Hospital type (R, U non-teaching, U teaching) | 12, 16, 72 | 15, 17, 68 | 14, 17, 69 | 6, 20, 74 | 13, 16, 71 | 0.32 |
| % Zip code income quartile (Q1–4) | 53, 24, 17, 6 | 57, 23, 14, 6 | 53, 28, 14, 5 | 52, 26, 16, 6 | 56, 23, 15, 6 | 0.91 |
| % Alcohol-associated cirrhosis | 65 | 59 | 62 | 56 | 71 | 0.016 |
| % Alcohol-associated hepatitis | 23 | 16 | 18 | 17 | 28 | 0.002 |
| % Alcohol-associated liver disease | 70 | 63 | 65 | 60 | 76 | 0.003 |
| % HCV cirrhosis | 11.4 | 10.7 | 9.9 | 8.7 | 8.5 | 0.11 |
| % NASH cirrhosis | 11.1 | 4.8 | 9.6 | 6.4 | 7.9 | 0.051 |
SD, Standard deviation; MC, Medicare; MD, Medicaid; R, Rural; U, Urban.
Subgroup of hospitalizations with ACLF at or during admission
Among the 350 hospitalizations with ACLF within the matched cohort, hospitalizations for AI/AN individuals compared to all other races were more likely to be due to ALD (Supplementary Table 6). In an adjusted logistic regression model, there was no difference based on race for a discharge diagnosis of ALD or AH, except for about five- and four-fold higher risk of ALD as discharge diagnosis among admissions for AI/AN compared to Hispanics and Asians or other races, respectively. Predictors of ALD or AH etiology were young age, male sex, and Medicaid or private insurance (Supplementary Table 7).
In-hospital mortality in hospitalizations due to cirrhosis
After excluding 97 admissions associated with receiving LT, 836 of 14,144 (5.9%) hospitalizations were associated with in-hospital mortality, 7% in Blacks followed by 6.4% in Asians or other races, 6% in AI/AN, and 5.1% in Hispanics and Whites (p=0.36) (Fig. 2B). In a logistic regression model controlling for demographics (age, sex, and race), payer source, zip code income quartile, and hospital type, admission in an AI/AN individual was less likely to be associated with in-hospital mortality compared to Black race [0.66 (0.51–0.84)]. We also performed univariate association between each covariate and the in-hospital mortality (Supplementary Table 8). Comparison with other races showed statistical insignificance (Table 4). Diagnosis of AH and of decompensated cirrhosis were associated with higher odds of in-hospital mortality, and a diagnosis of ALD without AH were associated with a lower odds of in-hospital mortality (Table 4). Other predictors were age and private or other mode of insurance. Race was not associated with in-hospital mortality in subgroup analyses of 7,354 hospitalizations with discharge diagnosis of ALD or 3,128 hospitalizations with discharge diagnosis of AH (data not shown).
Table 4. Logistic regression multivariable analyses on the matched cohort of hospitalizations with cirrhosis for predictors of in-hospital mortality*.
| OR (95% CI) | p | |
|---|---|---|
| Age in years | 1.02 (1.01–1.03) | <0.001 |
| Female vs. Male | 0.84 (0.73–0.98) | 0.024 |
| AI/AN vs. White | 1.02 (0.79–1.32) | 0.20 |
| AI/AN vs. Black | 0.66 (0.51–0.84) | 0.015 |
| AI/AN vs. Hispanic | 1.15 (0.91–1.47) | 0.19 |
| AI/AN vs. Asian or other | 0.84 (0.66–1.07) | 0.50 |
| Medicaid vs. Medicare insurance | 1.16 (0.95–1.41) | 0.16 |
| Pvt. or other vs. Medicare insurance | 1.57 (1.27–1.93) | <0.001 |
| Rural vs. urban teaching hospital | 0.78 (0.62–0.98) | 0.04 |
| Urban non-teaching vs. urban teaching hospital | 0.77 (0.63–0.95) | 0.032 |
| Zip income Quartile 1 vs. 4 | 1.16 (0.84–1.60) | 0.36 |
| Zip income Quartile 2 vs. 4 | 1.21 (0.87–1.69) | 0.26 |
| Zip income Quartile 3 vs. 4 | 0.9 (0.63–1.29) | 0.58 |
| Alcohol-associated hepatitis | 1.41 (1.14–1.74) | 0.025 |
| Alcohol-associated liver disease | 0.67 (0.55–0.79) | <0.001 |
| Decompensated cirrhosis | 3.2 (2.8–3.7) | <0.001 |
*Analysis for ALD etiology did not show any differences on race with OR (95% CI) for AI/AAN vs. Black race 0.79 (0.56–1.14). Other predictors being patient’s age, private or other insurance, decompensated ALD, and presence of AH. OR, Odds ratio; CI, Confidence interval; AI/AN, American Indian/Alaska Native.
Discussion
The main finding of our study is that ALD, including AH, is the most common etiology of cirrhosis-related admissions for AI/AN individuals compared to other races and ethnicities in the USA. A total of 6% of admissions result in in-hospital mortality, which is increased among Blacks compared to AI/AN but is similar to admissions for non-Black races or ethnicities.
Several previous studies have shown that AI/AN individuals have high prevalence of cirrhosis compared to other races.8–10 For example, mortality from any cause between 1999 and 2009 in AI/AN located in contract health services delivery area counties was 46% greater than among non-Hispanic Whites. Further, ALD was the leading cause of cirrhosis-related mortality for AI/AN as well as non-Hispanic Whites.17–19 Healthcare burden from ALD is also increasing among individuals aged 25–44 years, a population at their prime of productivity and contribution to national growth.3,6,8–10,19,20 Our study on hospitalized patients with cirrhosis including subgroups of decompensated cirrhosis or those with ACLF showed a novel finding that admissions for AI/AN individuals were more likely to have diagnosis of ALD, including AH.
The higher prevalence of AUD in AI/AN, as observed in this and earlier studies, may likely explain this finding. AUD is known to be associated with geographic location, socioeconomic status, and education of the individual.21,22 The higher prevalence observed in this study was observed in AI/AN individuals after controlling for these potential confounders. Patients with ALD compared to other liver diseases are known to often present at an advances stage of cirrhosis and/or complications.23,24 Several factors, including sex, alcohol use patterns (binge use, drinking outside of meals, type of alcohol, and severity of AUD), socioeconomic status, having insurance, receipt of treatment for risk factors of AUD, and specialty care for liver disease determine receipt of treatment of any liver disease, including ALD.25–31 Further, genetic polymorphisms of alcohol metabolizing enzymes may predispose an individual to AUD, and polymorphisms of PNPLA3, TMSF62, and MBOAT7 genes have been shown to predispose an individual with AUD to the development and severity of ALD.32,33 Although, we were able to account for socioeconomic and insurance status, lack of available data on other clinical variables in the NIS database and blood samples for genetic analyses limited assessment on association of other variables with predisposition of AUD and ALD in AI/AN individuals.
About 6% of admissions with discharge diagnosis of cirrhosis were associated with in-hospital mortality. These data are similar to in-hospital mortality observed in other studies using the NIS database on admissions with cirrhosis. The in-hospital mortality was higher for Blacks compared to AI/AN but similar to that for other races. In another study using death certificate data (1999–2016) from the Center for Disease Control, the overall mortality was projected to increase by 10.1% between 2017 and 2030 for AI/AN and for White men, contributing to 239,700 excess deaths.34 In the same study, mortality from chronic liver disease/cirrhosis was projected to increase for all races, except for Black men, similar to what we observed in the current study.34
The large sample size obtained by means of a national (USA) database of a homogeneous population of admissions with cirrhosis is a potential strength of our study. Further, using a cohort of AI/AN individuals matched for other races and analysis controlled for some of the potential confounders, like geographic location, socioeconomic status, and insurance payer, is another strength. However, a cautious approach is suggested on the interpretation of our observations, as the authors also recognize some limitations of this study. For example, ALD may have been over reported due to potential coding error in adjudicating the discharge diagnosis, as the study population was identified using the ICD codes. Further, admissions were not linkable to patient identifier, which limited evaluation of readmissions. Unavailability of laboratory values during the hospitalization and post-discharge follow-up, and lack of data from Veteran hospitals are some other limitations of this study. It may also be difficult to conclude whether the survival difference seen in our study is a real finding or not. Clearly, studies are needed to examine other host factors, such as drinking patterns and educational background of the individual, genetic polymorphisms, and access to care, to seek deeper explanations for the ethnic differences on in-hospital mortality.
In summary, this study on hospitalized patients with cirrhosis in the USA shows that ALD and/or AH is the most common cirrhosis etiology in AI/AN individuals compared to other races. The in-hospital mortality among cirrhosis-related hospitalizations is increased in Blacks compared to AI/AN, while this is similar to non-Black races. Large multicenter studies are needed to examine other factors, such as alcohol use patterns, receipt and type of provider care for AUD and for liver disease, and genetic polymorphisms, to further study mechanisms of our findings. Furthermore, these studies would also provide useful data to derive public health policies like prevention or treatment of AUD, early detection of silent advanced fibrosis, and increased access to healthcare, and to reduce the ALD-related healthcare burden,26,35,36 especially in AI/AN populations.
Supporting information
Abbreviations
- AC
alcohol-associated cirrhosis
- ACLF
acute on chronic liver failure
- AH
alcohol-associated hepatitis
- AI/AN
American Indian/Alaska Native
- ALD
alcohol associated liver disease
- NIS
National Inpatient Sample
Data sharing statement
The data used to support findings of the study are available in the publicly available National Inpatient Sample database.
References
- 1.Singal AK, Mathurin P. Diagnosis and Treatment of Alcohol-Associated Liver Disease: A Review. JAMA. 2021;326(2):165–176. doi: 10.1001/jama.2021.7683. [DOI] [PubMed] [Google Scholar]
- 2.Wong T, Dang K, Ladhani S, Singal AK, Wong RJ. Prevalence of Alcoholic Fatty Liver Disease Among Adults in the United States, 2001-2016. JAMA. 2019;321(17):1723–1725. doi: 10.1001/jama.2019.2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2017 Cirrhosis Collaborators The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5(3):245–266. doi: 10.1016/s2468-1253(19)30349-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong RJ, Singal AK. Trends in Liver Disease Etiology Among Adults Awaiting Liver Transplantation in the United States, 2014-2019. JAMA Netw Open. 2020;3(2):e1920294. doi: 10.1001/jamanetworkopen.2019.20294. [DOI] [PubMed] [Google Scholar]
- 5.Hirode G, Saab S, Wong RJ. Trends in the Burden of Chronic Liver Disease Among Hospitalized US Adults. JAMA Netw Open. 2020;3(4):e201997. doi: 10.1001/jamanetworkopen.2020.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singal AK, Arora S, Wong RJ, Satapathy SK, Shah VH, Kuo YF, et al. Increasing Burden of Acute-On-Chronic Liver Failure Among Alcohol-Associated Liver Disease in the Young Population in the United States. Am J Gastroenterol. 2020;115(1):88–95. doi: 10.14309/ajg.0000000000000411. [DOI] [PubMed] [Google Scholar]
- 7. 2010 Census urban and rural classification and urban area criteria. 2014.
- 8.Sancar F, Abbasi J, Bucher K. Mortality Among American Indians and Alaska Natives. JAMA. 2018;319(2):112. doi: 10.1001/jama.2017.20760. [DOI] [PubMed] [Google Scholar]
- 9.Jacobs-Wingo JL, Espey DK, Groom AV, Phillips LE, Haverkamp DS, Stanley SL. Causes and Disparities in Death Rates Among Urban American Indian and Alaska Native Populations, 1999-2009. Am J Public Health. 2016;106(5):906–914. doi: 10.2105/AJPH.2015.303033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Suryaprasad A, Byrd KK, Redd JT, Perdue DG, Manos MM, McMahon BJ. Mortality caused by chronic liver disease among American Indians and Alaska Natives in the United States, 1999-2009. Am J Public Health. 2014;104(Suppl 3):S350–358. doi: 10.2105/AJPH.2013.301645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singal AK, Ahmed Z, Axley P, Arora S, Arab JP, Haas A, et al. Hospitalizations for Acute on Chronic Liver Failure at Academic Compared to Non-academic Centers Have Higher Mortality. Dig Dis Sci. 2021;66(4):1306–1314. doi: 10.1007/s10620-020-06263-w. [DOI] [PubMed] [Google Scholar]
- 12.Ponicki WR, Henderson JA, Gaidus A, Gruenewald PJ, Lee JP, Moore RS, et al. Spatial Epidemiology of Alcohol- and Drug-Related Health Problems Among Northern Plains American Indians: Nebraska and South Dakota, 2007 to 2012. Alcohol Clin Exp Res. 2018;42(3):578–588. doi: 10.1111/acer.13580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ladhani S, Hirode G, Singal AK, Wong RJ. Impact of Safety-Net Burden on In-Hospital Mortality and Hospitalization Costs Among Patients with Alcoholic Hepatitis and Alcoholic Cirrhosis. Alcohol Alcohol. 2021;56(3):368–375. doi: 10.1093/alcalc/agaa081. [DOI] [PubMed] [Google Scholar]
- 14.Lieber AM, Boniello AJ, Kerbel YE, Petrucelli P, Kavuri V, Jakoi A, et al. Low Socioeconomic Status Is Associated With Increased Complication Rates: Are Risk Adjustment Models Necessary in Cervical Spine Surgery? Global Spine J. 2020;10(6):748–753. doi: 10.1177/2192568219874763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bajaj JS. Defining acute-on-chronic liver failure: will East and West ever meet? Gastroenterology. 2013;144(7):1337–1339. doi: 10.1053/j.gastro.2013.04.024. [DOI] [PubMed] [Google Scholar]
- 16.Waleed M, Abdallah MA, Kuo YF, Arab JP, Wong R, Singal AK. Higher Frequency of Hospital-Acquired Infections but Similar In-Hospital Mortality Among Admissions With Alcoholic Hepatitis at Academic vs. Non-academic Centers. Front Physiol. 2020;11:594138. doi: 10.3389/fphys.2020.594138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Espey DK, Jim MA, Cobb N, Bartholomew M, Becker T, Haverkamp D, et al. Leading causes of death and all-cause mortality in American Indians and Alaska Natives. Am J Public Health. 2014;104(Suppl 3):S303–311. doi: 10.2105/AJPH.2013.301798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shirazi F, Singal AK, Wong RJ. Alcohol-associated Cirrhosis and Alcoholic Hepatitis Hospitalization Trends in the United States. J Clin Gastroenterol. 2021;55(2):174–179. doi: 10.1097/MCG.0000000000001378. [DOI] [PubMed] [Google Scholar]
- 19.Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999-2016: observational study. BMJ. 2018;362:k2817. doi: 10.1136/bmj.k2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shiels MS, Chernyavskiy P, Anderson WF, Best AF, Haozous EA, Hartge P, et al. Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: an analysis of death certificate data. Lancet. 2017;389(10073):1043–1054. doi: 10.1016/S0140-6736(17)30187-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kranzler HR, Soyka M. Diagnosis and Pharmacotherapy of Alcohol Use Disorder: A Review. JAMA. 2018;320(8):815–824. doi: 10.1001/jama.2018.11406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Caputo F, Domenicali M, Bernardi M. Diagnosis and Treatment of Alcohol Use Disorder in Patients With End-Stage Alcoholic Liver Disease. Hepatology. 2019;70(1):410–417. doi: 10.1002/hep.30358. [DOI] [PubMed] [Google Scholar]
- 23.Shoreibah M, Raff E, Bloomer J, Kakati D, Rasheed K, Kuo YF, et al. Alcoholic liver disease presents at advanced stage and progresses faster compared to non-alcoholic fatty liver diseas. Ann Hepatol. 2016;15(2):183–189. doi: 10.5604/16652681.1193707. [DOI] [PubMed] [Google Scholar]
- 24.Shah ND, Ventura-Cots M, Abraldes JG, Alboraie M, Alfadhli A, Argemi J, et al. Alcohol-Related Liver Disease Is Rarely Detected at Early Stages Compared With Liver Diseases of Other Etiologies Worldwide. Clin Gastroenterol Hepatol. 2019;17(11):2320–2329.e2312. doi: 10.1016/j.cgh.2019.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Axley PD, Richardson CT, Singal AK. Epidemiology of Alcohol Consumption and Societal Burden of Alcoholism and Alcoholic Liver Disease. Clin Liver Dis. 2019;23(1):39–50. doi: 10.1016/j.cld.2018.09.011. [DOI] [PubMed] [Google Scholar]
- 26.Asrani SK, Mellinger J, Arab JP, Shah VH. Reducing the Global Burden of Alcohol-Associated Liver Disease: A Blueprint for Action. Hepatology. 2021;73(5):2039–2050. doi: 10.1002/hep.31583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li W, Kemos P, Salciccioli JD, Marshall DC, Shalhoub J, Alazawi W. Socioeconomic Factors Associated With Liver-Related Mortality From 1985 to 2015 in 36 Developed Countries. Clin Gastroenterol Hepatol. 2021;19(8):1698–1707.e13. doi: 10.1016/j.cgh.2020.08.047. [DOI] [PubMed] [Google Scholar]
- 28.Rogal S, Youk A, Zhang H, Gellad WF, Fine MJ, Good CB, et al. Impact of Alcohol Use Disorder Treatment on Clinical Outcomes among Patients with Cirrhosis. Hepatology. 2020;71(6):2080–2092. doi: 10.1002/hep.31042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lucey MR, Singal AK. Integrated Treatment of Alcohol Use Disorder in Patients with Alcohol-associated Liver Disease: An evolving story. Hepatology. 2020;71(6):1891–1893. doi: 10.1002/hep.31235. [DOI] [PubMed] [Google Scholar]
- 30.Bajaj JS, O’Leary JG, Tandon P, Wong F, Kamath PS, Biggins SW, et al. Insurance Status But Not Race and Ethnicity Are Associated With Outcomes in a Large Hospitalized Cohort of Patients With Cirrhosis. Clin Gastroenterol Hepatol. 2021;19(3):565–572.e5. doi: 10.1016/j.cgh.2020.04.081. [DOI] [PubMed] [Google Scholar]
- 31.Askgaard G, Leon DA, Kjaer MS, Deleuran T, Gerds TA, Tolstrup JS. Risk for alcoholic liver cirrhosis after an initial hospital contact with alcohol problems: A nationwide prospective cohort study. Hepatology. 2017;65(3):929–937. doi: 10.1002/hep.28943. [DOI] [PubMed] [Google Scholar]
- 32.Louvet A, Mathurin P. Alcoholic liver disease: mechanisms of injury and targeted treatment. Nat Rev Gastroenterol Hepatol. 2015;12(4):231–242. doi: 10.1038/nrgastro.2015.35. [DOI] [PubMed] [Google Scholar]
- 33.Salameh H, Raff E, Erwin A, Seth D, Nischalke HD, Falleti E, et al. PNPLA3 Gene Polymorphism Is Associated With Predisposition to and Severity of Alcoholic Liver Disease. Am J Gastroenterol. 2015;110(6):846–856. doi: 10.1038/ajg.2015.137. [DOI] [PubMed] [Google Scholar]
- 34.Best AF, Haozous EA, de Gonzalez AB, Chernyavskiy P, Freedman ND, Hartge P, et al. Premature mortality projections in the USA through 2030: a modelling study. Lancet Public Health. 2018;3(8):e374–e384. doi: 10.1016/S2468-2667(18)30114-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hadland SE, Xuan Z, Blanchette JG, Heeren TC, Swahn MH, Naimi TS. Alcohol Policies and Alcoholic Cirrhosis Mortality in the United States. Prev Chronic Dis. 2015;12:E177. doi: 10.5888/pcd12.150200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Diaz LA, Idalsoaga F, Fuentes-Lopez E, Marquez-Lomas A, Ramirez CA, Roblero JP, et al. Impact of public health policies on alcohol-associated liver disease in Latin America: An ecological multi-national study. Hepatology. 2021;74(5):2478–2490. doi: 10.1002/hep.32016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.