Abstract
Purpose:
To evaluate the causes of acute acquired comitant esotropia (AACE) in young adults and children in the setting of COVID-19-induced home confinement.
Methods:
A retrospective, clinical study of all patients, who presented to the Pediatric Ophthalmology and Strabismus services of a tertiary eye care center in South India from August 2020 to January 2021 during the COVID-19 pandemic, with acute-onset, comitant esotropia.
Results:
11 (73.3%) of the total 15 patients were students, above 10 years and with a mean age of 16.8 years. 12 patients (80%) had more than 8 hours of near activity a day with a mean duration of 8.6 hours per day. The most common near activity was online classes, followed by job-related work and mobile games, and 86.7% used smartphones for near work. The average esotropia was 22.73 prism diopter (PD) for distance and 18.73 PD for near. Majority (66.6%) had hyperopia with basic or divergence insufficiency esotropia, and the remaining 33.3% had myopia and fitted in to the Bielschowsky type AACE. There was no precipitating event other than sustained near work in all, except in one patient who also had fever prior to the onset of esotropia
Conclusion:
The habit of long-time and sustained near work, especially on smartphones, may increase the risk of inducement of AACE.
Keywords: AACE, COVID-19, excess near work
The COVID-19 pandemic, caused by the novel coronavirus SARS-CoV2, has changed life dramatically for everyone at work and home. The global number of workers working from home is now estimated to be 558 million, corresponding to 17.4% of global employment (Berg et al. 2020, ILO 2020).[1] Schools and colleges across the country started to shut down temporarily by the second week of March 2020 to contain the spread of the novel coronavirus.[2] Around 320 million learners have transitioned to e-learning since then. The increasing use of gadgets for studies, work, and leisure prompted by the pandemic has led to cropping up of many health problems in the students, including weight gain, sleep disruption, and psychosocial stress.[3] The worsening dependence on digital devices during the COVID-19 pandemic and its negative impact on students’ eye health, including that of computer vision syndrome and increased risk of myopia, has raised some serious concerns.[4]
Ever since the countrywide lockdown due to COVID-19 began and with the new norm of “work, study and play from home”, we saw a substantial number of children and young adults with complaints of recent onset of squinting and diplopia coming to the Pediatric Ophthalmology and Strabismus services of our hospital. This prompted us to devise this study.
Acquired nonaccommodative esotropia (ANAET) is a relatively rare and distinct subtype of esotropia characterized by a nonaccommodative esodeviation which can occur in older children, adults, and even the elderly.[5,6] It can result from deterioration of existing, previously controlled, esophoria, or can present acutely with diplopia when it is called acute acquired comitant esotropia (AACE).[7,8] AACE contributes to about 0.3% of childhood strabismus. AACE can be divided into five different subtypes.[9,10,11,12,13] The Swan type (type I) occurs after a period of interrupted binocularity.[10] Type II AACE, known as Burian-Franceschetti, has minimal hypermetropia and diplopia that are often associated with physical or psychological stress.[11] The Bielschowsky type (type III) is associated with patients with myopia, convergence spasm, and divergence paralysis.[12] Type IV, called refractive-accommodative type, is characterized by high hypermetropia that can be adequately controlled with the refractive correction alone.[13] Type V, a lesser common entity, is associated with intracranial pathology, most commonly a posterior fossa lesion.[14] In a small retrospective noncomparative study of 10 adult patients with acute-onset concomitant esotropia, Spierer[15] found that almost all were myopic, all regained normal stereopsis after surgery and suggested that they be classified as a distinct subgroup of acute-onset esotropia.
The purpose of this study was to examine the causes of acute acquired comitant esotropia (AACE) in young adults and children in the setting of COVID-19-induced home confinement.
Methods
This was a retrospective, clinical study of all patients who presented to the Pediatric Ophthalmology and Strabismus Services of a tertiary eye care center in South India from August 2020 to January 2021 during the COVID-19 pandemic, with acute-onset comitant esotropia.
The diagnosis of AACE was made based on the following criteria:
Acute onset of esotropia within hours/days/weeks, with photographic evidence of previously aligned eyes.
Age of onset after 1 year of age.
Comitant esodeviation with normal ocular movements.
Apart from demographic parameters like age, sex, occupation or class of study, visual acuity for distance and near, binocular status for distance and near, amount and type of deviation were studied. A careful history including duration of presenting complaint, any precipitating event, previous use of glasses, nature, duration and medium of near work were taken. All patients underwent a meticulous ocular examination including a dilated fundus examination. Cycloplegic refraction was done with atropine in all to detect true refractive status and to rule out accommodative esotropia. A detailed orthoptic evaluation was also performed. Occlusion therapy was started in all children detected to have amblyopia or at risk of amblyopia. All patients underwent magnetic resonance imaging (MRI) of the brain and orbits to rule out intracranial pathology as well as a neurology evaluation. The minimum follow-up period was six months. The study was conducted in accordance with the Declaration of Helsinki, and was approved by the appropriate Institutional Review Board and Ethics Committee.
We found four categories of patients with AACE in our study:
Those with myopia (SE ≥ -0.5DS) and divergence insufficiency (distance esotropia > near esotropia), and occasionally equal deviation for distance and near as described by Bielschowsky.[12]
Those with low hyperopia (SE ≤2 DS) and divergence insufficiency esotropia
Those with low hyperopia (SE ≤2 DS) and basic type esotropia (difference between distance and near esotropia not more than 5 PD)
Those with moderate hyperopia (SE = 2.25–5 DS), with basic type esotropia.
The only common factor in all these patients with esotropia was excessive near work either on the smartphone, laptop, or books, except in one patient with low hyperopia and divergence insufficiency esotropia who denied any overuse of near work.
Results
We had a total of 15 cases of AACE in our study: 11 males and 4 females. The age ranged from 5 years to 24 years with majority above 10 years and with a mean age of 16.8 years (SD = 5.659). Majority (11, 73.3%) were students and the rest (4, 26.7%) were employed. Most patients (73.3%) presented with diplopia and squint, whereas 6 (40.0%) had only diplopia, and 2 (13.3%) presented with only squint. The mean duration of presentation was 2.98 months (SD = 4.790) and ranged from 15 days to 6 months. There was no precipitating event other than excessive near work in the majority, except in one patient who had fever prior to the onset of esotropia. MRI brain was done in all and were unremarkable. Duration of near work ranged from 3–12 hours a day with a mean duration of 8.6 hours/day. 12 patients (80%) had more than 8 hours of near activity. The near activity was related to online classes in 8 (53.3%), official work in 3 (20%), mobile games in 3 (20%), and religious text reading in 1 (6.7%). The medium of near work was mainly smartphone alone in 13 patients (86.7%), smartphone and laptop in 1 patient (6.7%), and books in 1 patient (6.7%). Nine patients (60%) in our study had low hyperopia (SE ≤2 DS), 1 (6.6%) had moderate hyperopia (2.25–5 DS SE) and the remaining 5 (33.3%) had myopia (SE ≥-0.5 DS). Seven patients (46.7%) were using glasses at the time of presentation, of which five (33.3%) had myopia. Three (60.0%) out of the five with myopia admitted to doing near work without glasses. 11 patients (73.3%) had diplopia, 1 had fusion, and the rest 3 were suppressed on Worth Four Dot Test (WFDT) for distance. The mean stereopsis for near was 112.307 and ranged from 40 to 400 arc seconds using the Randot® Stereotest. The average esotropia for distance was 22.73 PD and ranged from 10 to 40 PD; whereas for near, it was 18.73 PD and ranged from 2 to 45 PD. Orthoptic evaluation revealed average near point of accommodation (NPA) of 6 (SD = 1.664), average near point of convergence (NPC) of 5.36 (SD = 1.689), average negative relative accommodation (NRA) of 3.33 (SD = 1.033), average monocular estimation method (MEM) of 0.76 (SD = 0.305) and an average accommodative convergence/accommodation (AC/A) ratio of 5.40 (SD = 3.638). There was high positive relative accommodation (PRA > -3.5) in 8 (53.3%), and the rest had normal (PRA ≤ 3.5) values. Reduced or poor negative fusional vergence (NFV) for distance was seen in 40% of patients. On accommodative facility testing, 26.66% complained of difficulty in clearing plus lenses, 13.33% had difficulty clearing minus lenses, 46.66% had reduced binocular accommodative facility, and only two (13.33%) had normal facility. Most of those with myopia (three out of five) had high AC/A ratio, accommodative lag (four out of five) on MEM, but had esodeviation more for distance than near, contrary to expectation. All five (33.33%) of those with myopia fitted in to the Bielschowsky type of AACE with four of them having divergence insufficiency and the remaining one having basic type AACE. One patient with moderate hypermetropia and diplopia, who had fever preceding the onset of esotropia, was prescribed plus lenses and could be classified as Burian-Franceschetti type of AACE. The remaining nine (60%) had low hyperopia with either basic type AACE (33.3%) or divergence insufficiency type AACE (26.7%). All were advised to restrict and reduce their near work; those with glasses were advised constant use and those with divergence insufficiency were prescribed divergence exercises or prisms. Reduction of near work with divergence exercises (eccentric circles card and divergence training) was helpful in five patients in our study. Those with basic type of AACE, who did not improve, were advised squint surgery. Ground prisms in glasses were prescribed for two patients, both with myopia and divergence insufficiency type AACE (3 PD BO OU and 6 PD BO OD respectively). Four patients; three with low hyperopia and basic type AACE, and one with Burian-Franceschetti type of AACE underwent squint surgery and regained binocular vision [Figs. 1(a, b), 2(a, b), 3(a, b), 4(a, b)] and Tables [(1a, b), 2 and 3].
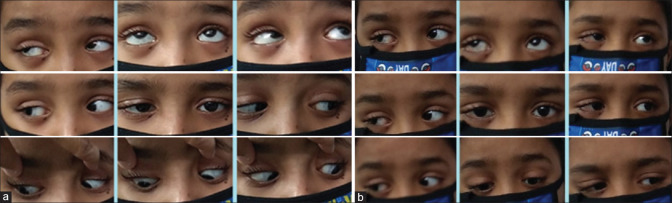
Figure 1.

(a) Patient A at 1.5 years. (b) Patient A (an avid PUBG video game player) before and after surgery
Figure 2.

(a) Patient B 6 months before with straight eyes (b) Patient B (Class X student with 8 hours/day of online classes on smartphone) with basic type esotropia (left eye) before and after surgery
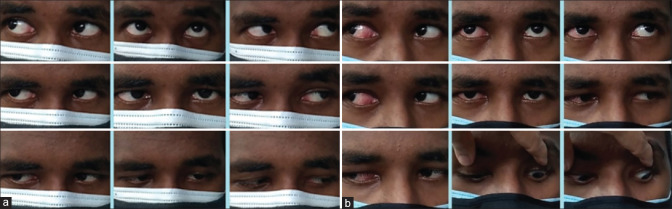
Figure 3.
(a) Patient C (using smartphone for online classes and games more than 8 hours/day) showing basic type esotropia (right eye), (b) Patient C showing straight eyes post right eye surgery (medial rectus recession + lateral rectus resection)
Figure 4.
(a) Patient D before: 17 years old, college student who developed AACE with more than 8 hours of near work on smartphone; (b) Patient D after surgery (medial rectus recession + lateral rectus resection)
Table 1a.
Profile of patients with acute acquired comitant esotropia
| Age (years) | Sex | Presenting Complaints | Hours of near work/day |
|---|---|---|---|
| 24 | M | Diplopia | 6 |
| 17 | M | Diplopia and Squint | 8 |
| 8 | M | Squint | 8 |
| 15 | F | Diplopia and Squint | >8 |
| 15 | M | Diplopia | 6 |
| 20 | M | Diplopia | >8 |
| 16 | M | Diplopia | >8 |
| 20 | M | Diplopia and Squint | 12 |
| 24 | M | Diplopia | > 8 |
| 5 | M | Squint | >10 |
| 16 | F | Diplopia | 12 |
| 20 | F | Diplopia and Squint | >12 |
| 23 | M | Diplopia and Squint | >12 |
| 19 | F | Diplopia And Squint | 3 |
| 10 | M | Diplopia and Squint | 8 |
M: Male, F: Female
Table 1b.
Profile of patients with acute acquired comitant esotropia
| Type and medium of near work | BCVA RE (SNELLEN) | BCVA LE (SNELLEN) | Cycloplegic refraction RE | Cycloplegic refraction LE |
|---|---|---|---|---|
| Job Related, Smartphone | 6/6 N6 | 6/6 N6 | -2.25 DS | -1.25 DS/-1.25 DC@80 |
| Religious Text Reading, Books + Smartphone | 6/6 N6 | 6/6 N6 | +0.50 DS/+0.50 DC@35 | +0.50DS/+0.50DC @135 |
| Mobile Games, You Tube, Smartphone | 6/6 N6 | 6/6 N6 | +0.75 DS/+1.00 DC@90 | +1.25DS/+0.75DC@90 |
| Online Classes, Smartphone | 6/6 N6 | 6/6 N6 | +1.25 DS/+0.25 DC @75 | +1.00 DS/+0.50 DC@80 |
| Online Classes, Smartphone | 6/6 N6 | 6/6 N6 | +0.75 DS | +1.25 DS |
| Online Classes, Smartphone | 6/6 N6 | 6/6 N6 | +0.50 DS/-0.75 DC@100 | +1.00 DS/-0.75 DC@100 |
| Online Classes, Smartphone | 6/6 N6 | 6/6 N6 | +0.75 DS | +0.75 DS |
| Mobile Games, You Tube, Smartphone | 6/6 N6 | 6/6 N6 | -4.00 DS/-1.00 DC @180 | -4.00/-1.00 DC @170 |
| Job Related, Smartphone | 6/6 N6 | 6/6 N6 | -4.00 DS/-1.75 DC@ 90 | -4.00 DS/-1.00 DC @ 90 |
| PUBG Game, Smartphone | 6/6 N6 | 6/6 N6 | +2.50 DS | +2.50 DS |
| Online Classes, Smartphone | 6/6 N6 | 6/6 N6 | -4.00 DS | -3.25 DS |
| Online Classes, Social Media, Smartphone | 6/6 N6 | 6/6 N6 | +0.75 DS/+0.75 DC @90 | +0.75 DS/+0.50 DC @85 |
| Job Related, Smartphone + Laptop | 6/9 N6 | 6/6 N6 | -4.75 DS/+0.75 DC @90 | -4.00 DS/-0.50 DC@ 20 |
| Online Classes, Smartphone | 6/6 N6 | 6/6 N6 | +1.00 DS | +1.00 DS |
| Online Classes, Smartphone | 6/6 N6 | 6/6 N6 | +1.25 DS/+0.50 DC@175 | +1.50 DS/+0.25 DC @15 |
BCVA: Best Corrected Visual Acuity, RE: Right Eye, LE: Left Eye
Table 2.
Clinical features of esotropia
| ET (D) in PD | ET (N) in PD | Type of ET | WFDT (D) | Stereopsis (N) (arc seconds) |
|---|---|---|---|---|
| 12 | 5 | ET D > N | Diplopia | 60 |
| 40 | 45 | Basic | Diplopia | 140 |
| 30 | 30 | Basic | Right Suppression | 400 |
| 35 | 30 | Basic | Diplopia | Could not Comprehend |
| 16 | 9 | ET D > N | Alternate Suppression | 40 |
| 10 | 2 | ET D > N | Diplopia | 60 |
| 30 | 30 | Basic | Diplopia | 140 |
| 25 | 30 | Basic | Diplopia | 100 |
| 12 | 2 | ET D > N | Diplopia | 100 |
| 35 | 40 | Basic | Alternate Suppression | Could not Comprehend |
| 10 | 5 | ET D > N | Diplopia | 100 |
| 25 | 14 | ET D > N | Diplopia | 100 |
| 16 | 6 | ET D > N | Fusion | 60 |
| 20 | 8 | ET D > N | Diplopia | 100 |
| 25 | 25 | Basic | Diplopia | 100 |
ET: Esotropia, D: Distance, N: Near, PD: Prism Diopter, WFDT: Worth Four Dot Test
Table 3.
Management of patients with acute acquired comitant esotropia
| Refractive Error | Impression from Orthoptic Evaluation | MRI Brain and Orbits | Improvement with reduction of Near Work | Other Treatment Given |
|---|---|---|---|---|
| Myopia | High AC/A, Accommodative Lag, Reduced Fusional Divergence, ET D > N | Normal | Yes | Prism glasses (3 PD BO both eyes) |
| Low Hyperopia | Normal AC/A, Normal MEM, High PRA, Basic ET | Normal | No | Right eye MR recession 6mm + LR resection 8mm |
| Low Hyperopia | High AC/A, Accommodative Lag, Basic ET | Normal | No | Right eye MR recession 5mm + LR resection 5mm |
| Low Hyperopia | High AC/A, Normal MEM, High PRA, Basic ET | Normal | No | Left eye MR Recession 6 mm + LR resection 7.5mm |
| Low Hyperopia | Normal AC/A, High NRA, Normal MEM, Reduced Fusional Divergence, ET D > N | Normal | No | Divergence exercises |
| Low Hyperopia | Low AC/A, High PRA, Accommodative Lag, Reduced Fusional Divergence, ET D > N | Normal | No | Glasses + Divergence exercises |
| Low Hyperopia | Low AC/A, Low NRA, Accommodative Lag, Basic ET | No | Glasses + Divergence Exercises, Advised Squint Surgery | |
| Myopia | High AC/A, High PRA, Accommodative Lag, Basic ET | Normal | No | Glasses, advised Squint surgery |
| Myopia | Normal AC/A, High NRA, High PRA, Accommodative Lag Reduced Fusional Divergence, ET D > N | Normal | Yes | Prism glasses (6 PD BO Right eye) |
| Moderate Hyperopia | High AC/A, High NRA, High PRA, Accommodative Lag, Basic ET | Normal | No | OU MR Recession 6mm |
| Myopia | Normal AC/A, High NRA, Low PRA, Normal MEM, Reduced Fusional Divergence, ET D > N | Normal | Yes | Glasses + Divergence Exercises |
| Low Hyperopia | Low AC/A, High NRA, Normal MEM, ET D > N | Normal | No | Glasses + Divergence Exercises |
| Myopia | High AC/A, High NRA, Accommodative Lag, ET D > N | Normal | Yes | Glasses + Divergence Exercises |
| Low Hyperopia | Low AC/A, High NRA, High PRA. Accommodative Lag, ET D > N | Normal | No | Glasses + Divergence Exercises |
| Low Hyperopia | Normal AC/A, Normal MEM, Basic ET | Normal | No | Squint Surgery Advised |
BO: Base Out, AC/A: Accommodative Convergence/Accommodation, MEM: Monocular Estimation Method, PRA: Positive Relative Accommodation, NRA: Negative Relative Accommodation, MR: Medial Rectus, LR: Lateral Rectus
Discussion
Continuing school closure, home confinement, and work from home policies during the current COVID-19 lockdown have ushered in important lifestyle behavioral changes in the young population, including a significant increase in screen time,[16] digital eye strain, and raised serious concerns of worsening the global burden of myopia.[4] Apart from these, the excessive application of near vision might have other undesirable effects, including development of acute acquired concomitant esotropia (AACE). Lee et al.[17] documented a series of 12 teenagers with AACE who used smartphones more than four hours a day. Interestingly, the esodeviation improved in all patients after refraining from smartphone use for 1 month. Nevertheless, strabismus surgery was required in five patients with good postoperative outcomes in terms of ocular alignment and stereo acuity. The average duration of smartphone use in their study was 6.08 ± 1.78 hours/day, which was similar to 8.6 hours/day of near work in our study. In a retrospective study of 26 cases with AACE over 20 months, Yan Wu et al.[18] deduced that AACE could be caused by excessive near work regardless of whether or not one wears glasses regularly, especially for individuals with myopic refractive error. The only common factor that contributed to the development of AACE in their study was also the excessive near visual activities, especially the use of smartphones.
In our study, majority (66.6%) had low hyperopia with basic or divergence insufficiency esotropia and the remaining 33.3% had myopia which fitted in to Bielschowsky type AACE. Excessive near work and a naturally stronger convergence in the young could have led to an imbalance between accommodation and vergences, thereby resulting in dynamic activation of the medial rectus muscles and a manifest esodeviation. This effect is greater in those with hyperopia due to their greater accommodative demand, as also seen in our study with 66.7% having hyperopia. Conventionally, it is thought that the presence of myopia is associated with a decreased demand for accommodation, and hence lower convergence and a predisposition for developing exotropia. However, those with myopia, can also develop esotropia due to the excessive application of near work, resulting in increased tone of medial rectus muscles, and coupled with the lack of distant stimuli during the home confinement, leading to divergence weakness as was also seen in our study. Bielschowsky[12] claimed that uncorrected myopia led to the development of increased tonus of the medial rectus muscles and suggested that the increase in tonus can be explained by the tendency of individuals with uncorrected myopia to hold print or sewing excessively close to the eyes, resulting in the development of esotropia. 60% of those with myopia in our study also admitted to doing near work without glasses as they felt they could see clearly. In a well-defined study of adult patients with acute-onset concomitant esotropia by Spierer et al.,[15] almost all were myopic, and all regained normal stereopsis after surgery. In a retrospective clinical study of all patients under the age of 18 years with acute-onset non-accommodative comitant esotropia, we[19] had earlier reported that prompt amblyopia therapy and timely surgery can result in a satisfactory outcome in those without systemic involvement. In our present study also, reduction of near work with divergence exercises was helpful in five patients. Two patients were prescribed prism glasses, four underwent squint surgery, three were advised glasses and squint correction, and one was awaiting squint surgery. All who underwent squint surgery regained binocularity and were diplopia free. Aldo Vagge et al.[20] described four cases of AACE that occurred during the COVID-19 lockdown in Italy in 2020, wherein all patients spent 8 to 10 hours a day using computers, tablets, and smartphones to play, access school lessons, and navigate social networks. In a similar case setting of COVID-19-induced home confinement, we are reporting a case series of 15 patients with AACE.
Although the etiology of AACE is still debated, it has been associated with sustained near point demands due to the excessive use of computers, tablets, and smartphones. With the increasing use of smartphones and tablets in modern life, more and more work is being done through small screens at a close distance. We feel that this excessive near work, a naturally stronger convergence, and lack of distance stimuli could have led to an imbalance between accommodation and vergences, thereby resulting in dynamic activation of the medial rectus muscles with or without divergence weakness, and thus producing a manifest esotropia in our patients. We feel that sustained near work played a pivotal role in the development of esotropia in our patients and hope that authorities would take serious note of this undesirable effect. Regulating the duration of e- learning, reducing the number of total hours of screen time, shifting to widescreen visual display devices like television, taking breaks, promoting healthy lifestyle habits, like increasing outdoor play, should be recommended to improve the eye health of the young population.
Conclusion
The habit of long-time and sustained near work, especially on smartphones, may increase the risk of inducement of AACE. Parents and public health authorities should take serious note of this negative impact on the eye health of the young population and should bring about suitable recommendations and regulations to mitigate this undesirable effect.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Berg J, Bonnet F, Soares S. Working from Home,Estimating the Worldwide Potential. VoxEU.org. 11 May. 2020 [Google Scholar]
- 2. Available from: https://government.economictimes.indiatimes.com/news/education/covid-19-pandemic-impact-and-strategies -foreducation-sector -in-india/75173099 .
- 3.Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395:945–7. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pellegrini M, Bernabei F, Scorcia V, Giannaccare G. May home confinement during the COVID-19 outbreak worsen the global burden of myopia? Graefes Arch Clin Exp Ophthalmol. 2020;258:2069–70. doi: 10.1007/s00417-020-04728-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Legmann Simon A, Borchert M. Etiology and prognosis of acute, lateonset esotropia. Ophthalmology. 1997;104:134852. doi: 10.1016/s0161-6420(97)30136-5. [DOI] [PubMed] [Google Scholar]
- 6.Clark AC, Nelson LB, Simon JW, Wagner R, Rubin SE. Acute acquired comitant esotropia. Br J Ophthalmol. 1989;73:6368. doi: 10.1136/bjo.73.8.636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lyons CJ, Tiffin PA, Oystreck D. Acute acquired comitant esotropia: A prospective study. Eye (Lond) 1999;13:61720. doi: 10.1038/eye.1999.169. [DOI] [PubMed] [Google Scholar]
- 8.Sturm V, Menke MN, Töteberg M, Jaggi GP, Schoeffler C. Early onset of acquired comitant nonaccommodative esotropia in childhood. Klin Monbl Augenheilkd. 2012;229:35761. doi: 10.1055/s-0031-1299237. [DOI] [PubMed] [Google Scholar]
- 9.Burian HM, Miller JE. Comitant convergent strabismus with acute onset. Am J Ophthalmol. 1958;45:5564. doi: 10.1016/0002-9394(58)90223-x. [DOI] [PubMed] [Google Scholar]
- 10.Swan KC. Esotropia following occlusion. Arch Ophthalmol. 1947;37:44451. doi: 10.1001/archopht.1947.00890220457004. [DOI] [PubMed] [Google Scholar]
- 11.Franceschetti A. Acute concomitant strabismus. Ophthalmologica. 1952;123:21926. doi: 10.1159/000301172. [DOI] [PubMed] [Google Scholar]
- 12.Bielschowsky A. Das einwärtsschielen der myopen [Convergent strabismus of myopes] Ber Dtsch Ophthalmol Ges. 1922;43:245–59. [Google Scholar]
- 13.VonNoorden GK. Esodeviations. In: von Noorden GK, Campos E, editors. Theory and Management of Strabismus in Binocular Vision and Ocular Motility. 5th ed. USA: The C. V. Mosby Company; 1990. p. 309. [Google Scholar]
- 14.Astle WF, Miller SJ. Acute comitant esotropia: A sign of intracranial disease. Can J Ophthalmol. 1994;29:1514. [PubMed] [Google Scholar]
- 15.Spierer A. Acute concomitant esotropia of adulthood. Ophthalmology. 2003;110:1053–6. doi: 10.1016/S0161-6420(03)00102-7. [DOI] [PubMed] [Google Scholar]
- 16.Bahkir FA, Grandee SS. Impact of the COVID-19 lockdown on digital device-related ocular health. Indian J Ophthalmol. 2020;68:2378–83. doi: 10.4103/ijo.IJO_2306_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee HS, Park SW, Heo H. Acute acquired comitant esotropia related to excessive Smartphone use. BMC Ophthalmol. 2016;16:37. doi: 10.1186/s12886-016-0213-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu Y, Dai S, Feng XL, Sun B. Excessive smartphone use may cause acute acquired comitant esotropia. J Ophthalmol Vis Res. 2020;2(1) [Google Scholar]
- 19.Neena R, Giridhar A. Acute acquired comitant esotropia in children: A benign entity or an ominous sign? Kerala J Ophthalmol. 2019;31:33–8. [Google Scholar]
- 20.Vagge A, Giannaccare G, Scarinci F, Cacciamani A, Pellegrini M, Bernabei F, et al. Acute acquired concomitant esotropia from excessive application of near vision during the covid-19 lockdown. J Pediatr Ophthalmol Strabismus. 2020;57:e88–e91. doi: 10.3928/01913913-20200828-01. doi: 10.3928/01913913-20200828-01. [DOI] [PubMed] [Google Scholar]