Dear Editor,
The purpose of this manuscript is to emphasize the importance and methods to fortify mixed handedness in a variety of ophthalmologic subspecialties. Ambidexterity is a necessity for anterior segment procedures such as phacoemulsification, where right-handed surgeons must use their left hand or the non-dominant hand (NDH) to operate a chopper.[1] Mixed handedness is more critical than ever, extending its utility in pediatric ophthalmology, oculoplasty, and vitreoretinal surgery. It is also required for holding slit-lamp biomicroscopic lenses [Fig. 1a and b], gonio lenses, and laser contact lenses. Utilizing the second foot is also crucial where control of the foot pedal is essential in phacoemulsification. Surgeons who drive automobiles will have adequate foot command and face fewer difficulties while using the non-dominant foot [Fig. 2].
Figure 1.
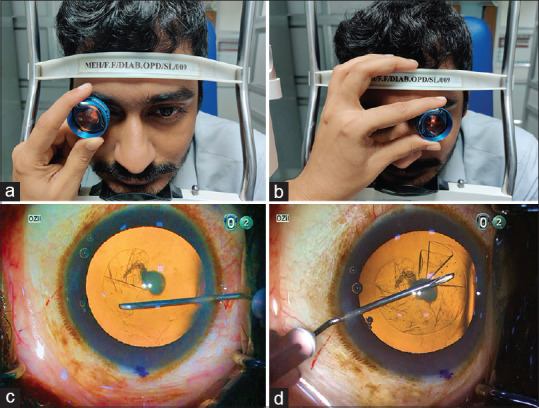
(a) Image showing the 90D lens held in the clinician’s left hand while performing fundus examination of the patient’s right eye. (b) Image showing the 90D lens held in the clinician’s left hand while performing fundus examination on the patient’s left eye, which involves touching the patient’s face, causing patient discomfort. (c) Image showing the rhexis initiated with the cystitome in the right hand, which is interchanged to the left hand (d) to complete it in the area which is sub-incisional for the right hand, for better circularity
Figure 2.
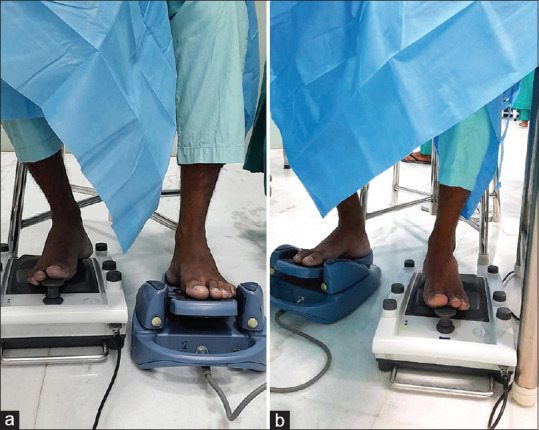
(a and b) Image showing the surgeon’s dominant and non-dominant foot interchanging while accessing and pressing the microscope pedal and phaco machine foot pedal between different right eye and left eye surgeries, respectively (which involves different surgeon positions)
There are numerous strategies to increase dexterity through the conscious practice of using both hands while performing ordinary tasks. Residents have traditionally been adviced to employ their NDH when performing routine activities such as eating, brushing their teeth, and combing. Another helpful technique is to flip the computer’s mouse to the opposite side. Strengthening the NDH by using grip tools also improves muscular control. Hobbies such as knitting, video gaming, and playing musical instruments help to reinforce the use of the NDH. In Palazzolo’s research, medical students with sketching experience did better on capsulorhexis [Fig. 1c and d].[2]
The importance of surgical simulators and routine wet lab practice in the development of dexterity cannot be overstated in clinical settings.[3,4] Surgical simulation is one modality that can assist young surgeons in developing their ambidexterity in a controlled and safe environment. Even in the absence of simulators, suturing practice on porcine or goat eyeballs can aid in the process. Residents may choose to experiment with NDH while administering eye drops.
At the outset of residency training, ambidexterity should be emphasized as it is an important trait for neophyte ophthalmologists to develop and continually hone, as they advance in their careers. It is crucial in anterior segment surgeries, where anterior chambers shrink by the day. Consistent deliberate practice can aid in the reinforcement of NDH use. Finally, handedness occurs in the brain, not the hands. If the brain establishes the barrier, it can also dissolve it.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ramesh PV, Balasubramaniam P, Devadas AK, Ray P, Ramesh SV, Ramesh MK, et al. Venturing into the third dimension of cataract surgery/observations with digital heads-up display –A personal take on NGENUITY for anterior segment surgeries. Indian J Ophthalmol. 2022;70:694–5. doi: 10.4103/ijo.IJO_3008_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Palazzolo L, Kozlova A, Laudi JJ, Rizzuti AE. Predictors of manual dexterity in simulation-based cataract surgery. J Acad Ophthalmol. 2020;12:e239–43. [Google Scholar]
- 3.Khalifa YM, Bogorad D, Gibson V, Peifer J, Nussbaum J. Virtual reality in ophthalmology training. Surv Ophthalmol. 2006;51:259–73. doi: 10.1016/j.survophthal.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 4.Ramesh PV, Aji K, Joshua T, Ramesh SV, Ray P, Raj PM, et al. Immersive photoreal new-age innovative gameful pedagogy for e-ophthalmology with 3D augmented reality. Indian J Ophthalmol. 2022;70:275–80. doi: 10.4103/ijo.IJO_2133_21. [DOI] [PMC free article] [PubMed] [Google Scholar]


