Abstract
A 73-year-old lady presented with a white spot and redness in the left eye for 1 month and had been treated elsewhere as a case of fungal keratitis. She had severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) viral infection 2 months before. Her past ocular history and examination gave a probable diagnosis of herpetic stromal and endothelial keratitis. She responded to oral acyclovir and topical steroid, leading to resolution of stromal edema and inflammation. Anterior chamber fluid polymerase chain reaction (PCR) confirmed pathogen herpes simplex virus (HSV)-1. HSV ocular reactivation after coronavirus disease 2019 (COVID-19) has been reported currently. The present report will add knowledge about this potential opportunistic ophthalmic infection during the recovery phase of COVID-19 disease.
Keywords: COVID-19, reactivation of HSV keratitis, stromal and endothelial herpetic keratitis
In late 2019, coronavirus disease 2019 (COVID-19) originated in the Wuhan province of China and it immediately turned into a pandemic.[1] The disease is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which primarily affects the respiratory system with its diverse sequels including acute respiratory distress syndrome (ARDS) with subsequent multi-organ involvement.[2] Patients with comorbidities (older age, obesity, immunocompromised states, malignancy, diabetes mellitus, chronic respiratory and cardiovascular disease) are at higher risk of COVID-19–associated complications, intensive care unit (ICU) admissions, and fatal outcomes. During the course of SARS-CoV-2 infection, several cases of opportunistic infections including bacterial, fungal, protozoal, and viral infections have been reported mostly with those on systemic immune-suppressive therapy for cytokine storm related to COVID-19.[3] Both systemic and ocular herpes zoster and herpes simplex viral activation in COVID-19–affected patients have occurred and have been documented in literature.[4,5,6] In this case report, we try to add another evidence of the possible etiopathogenic role of COVID-19, where immunodeficiencies are generated favoring other viral infections, such as herpes virus infections.
Case Report
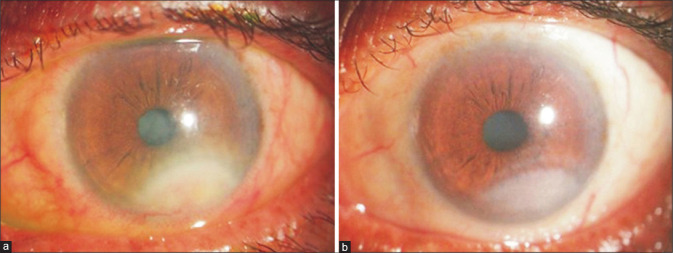
A 73-year-old woman presented at the cornea clinic with chief complaints of dense white spot, photophobia, and slightly worsened vision in her left eye for 1 month. She was getting treatment elsewhere with topical and systemic antifungal drugs without any improvement. The ophthalmological exam revealed a visual acuity of 20/30 in the left eye and 20/80 in the right eye. Intraocular pressure values were 6 mmHg in the right eye and 17 mmHg in the left eye. At slit-lamp examination, the left eye had conjunctival and limbal hyperemia and inferior corneal (extending two clock hours) dense stromal edema with active deep and superficial neovascularization [Fig. 1a]. Overlying epithelium was intact with mild anterior chamber (AC) inflammation and few keratic precipitates (KP) on the endothelium near the edema, and there was Nuclear Sclerosis (NS) grade 2 cataract. Corneal sensation was moderately reduced in the left eye, but normal in the right eye. The right eye had pseudophakia with advanced glaucomatous cupping and functional trabeculectomy bleb. On further enquiry, she revealed past history of corneal ulcer with a small white spot in her left eye several years ago. She also gave history of moderate COVID-19 infection in May 2021 (second wave of the epidemic in India), 1 month before she developed symptoms in her left eye. She was treated for COVID-19 illness with systemic steroid and noninvasive ventilation.
Figure 1.
Diffuse slit-lamp photograph of the left eye: (a) conjunctival hyperemia, dense semilunar corneal stromal edema, and vascularization near inferior limbus with associated KP on the surrounding endothelium; (b) posttreatment photograph shows resolved stromal edema and thinned out blood vessels with remaining faint corneal scar. KP = keratic precipitates
So, according to history and examination, a possible diagnosis of recurrent herpes simplex keratitis with stromal involvement and AC inflammatory activity in the left eye was made, which was confirmed by positive reverse transcription-polymerase chain reaction (RT-PCR) testing from AC tap fluid. Topical therapy was started with fluorometholone 0.1% (six times/day) eye drop in weekly tapering doses, homatropine drop (three times/day), and oral acyclovir tablet 400 mg (five times/day for 2 weeks, then two times/day for 6 months.
The patient was evaluated after 2 weeks. The conjunctival and limbal hyperemia improved with resolved KP and thinning of vascularization. Stromal edema was significantly reduced both in area and density with quiet AC [Fig. 1b]. The patient’s visual acuity and photophobia in the left eye had improved. On follow-up after 2 months, she maintained the stable condition with no recurrence of the infection in her left eye.
Discussion
Herpes simplex virus (HSV)-1 belongs to the human herpes virus (HHV) alpha subfamily, which is a neurotrophic virus and establishes latency in the neural ganglion after primary infection in the body. Ocular infection is the second most common localization of symptomatic HSV-1 after oral involvement. The most frequent ophthalmic manifestation of HSV is keratitis, but it may also cause conjunctivitis, uveitis, or acute retinal necrosis. Triggering factors for HSV-1 reactivation are supposed to be psychological stress, fever, weakening of the immune system, and the presence of inflammatory mediators such as cytokines.[7]
There have been several case reports of reactivation of latent viral infections, including HSV infections, among COVID-19 patients.[8] In a study by Seeßle et al.,[9] a high rate of HSV-1 reactivation (83.3%, 15 out of 18 patients) was found in COVID-19 patients on invasive ventilation, after median 9 days of ventilation. Bilateral conjunctivitis, an ophthalmic HSV infection, was reported in a 69-year-old Caucasian male with moderate COVID-19 disease.[6] In a case series described by Majtanova et al.,[10] five cases (two of them bilateral) of keratitis were found among COVID-19–positive patients during the SARS-CoV-2 pandemic in Slovakia, where they also found 2–2.5 times higher incidence of HSV keratitis in that period and suspected COVID-19 as a potential activator of these five cases. All of their cases had associated epithelial keratitis, whereas our case presented with no epithelial ulcer. Most of their cases presented in 1–3 weeks of COVID-19 infection, but our patient had the eye infection 1 month after recovery from COVID-19 illness.
The possible reason of increased susceptibility of COVID-19 patients for herpetic reactivation may be the immune dysregulation that mainly occurs after prolonged illness and mechanical ventilation.[9] In COVID-19 patients, there is a significant decrease in number and also functional exhaustion of natural killer (NK) cells and cytotoxic T-lym phocytes, which are crucial for the control of viral infections in our body, due to increased expression of an inhibitory receptor (NKG2A).[11] There is also fall in the level of mediators activating NK and CD8+ cells (interferon-gamma [IFN-g]+ NK, interleukin [IL]-2+ NK, CD107a+ NK, tumor necrosis factor-alpha [TNF-a]+ NK cells, IL-2+ CD8+, IFN-g+ CD8+, CD107a+ CD8+ T cells), indicating that SARS-CoV-2 may suppress antiviral immunity.[11] COVID-19–re lated psychological stress, higher level of inflammatory and pyrogenic mediators, and IL-6– related cytokine storm may also have a direct role in reactivation of the herpes virus.[7] Immunosuppression to combat the cytokine storm by administration of higher dose of the systemic drug tocilizumab[3] and corticosteroid may lead to HSV-1 reactivation.
Latency of HSV-1 in trigeminal ganglion is mediated by specific CD8+ T cells. The exhaustion of these T cells along with COVID-19 may potentiate reactivation of herpes in these patients, which necessitates recommending acyclovir as an add-on treatment in COVID-19 treatment regime.[10]
One of the important things to remember is that as majority of the critical care patients will not be able to communicate their visual problems, ICU caregivers should be vigilant in identifying patients with evolving ophthalmic signs for further assessment and should promptly refer them to an ophthalmologist, as this keratitis may be blinding if not addressed timely and properly.
Conclusion
In conclusion, SARS-CoV-2 infection may be a potential risk factor for developing HSV-1 keratitis, and the ophthalmologist should have a knowledge of this ocular complication in COVID-19–infected cases, which may present either during acute or recovery phase of the illness; it mostly occurs in severely infected patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
Mr Tuhin Nandy is acknowledged for figure editing.
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. Anovel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–33. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Falahi S, Kenarkoohi A. Sex and gender differences in the outcome of patients with COVID-19. J Med Virol. 2021;93:151–2. doi: 10.1002/jmv.26243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guaraldi G, Meschiari M, Cozzi-Lepri A, Milic J, Tonelli R, Menozzi M. Tocilizumab in patients with severe COVID-19: A retrospective cohort study. Lancet Rheumatol. 2020;2:e474–84. doi: 10.1016/S2665-9913(20)30173-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elsaie ML, Youssef EA, Nada HA. Herpes zoster might be an indicator for latent COVID 19 infection. Dermatol Ther. 2020;33:e13666. doi: 10.1111/dth.13666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xu R, Zhou Y, Cai L, Wang L, Han J, Yang X, et al. Co-reactivation of the human herpesvirus alpha subfamily (herpes simplex virus-1 and varicella zoster virus) in a critically ill patient with COVID-19. Br J Dermatol. 2020;183:1145–7. doi: 10.1111/bjd.19484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hernandez JM, Singam H, Babu A, Aslam S, Lakshmi S. SARS-CoV-2 infection (COVID-19) and herpes simplex virus-1 conjunctivitis: Concurrent viral infections or a cause-effect result? Cureus. 2021;13:e12592. doi: 10.7759/cureus.12592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li H, Zhang J, Kumar A, Zheng M, Atherton SS, Yu FS. Herpes simplex virus 1 infection induces the expression of proinflammatory cytokines, interferons and TLR7 in human corneal epithelial cells. Immunology. 2006;117:167–76. doi: 10.1111/j.1365-2567.2005.02275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Le Balc'h P, Pinceaux K, Pronier C, Seguin P, Tadie J-M, Reizine F. Herpes simplex virus and cytomegalovirus reactivations among severe COVID-19 patients. Crit Care. 2020;24:530. doi: 10.1186/s13054-020-03252-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seeßle J, Hippchen T, Schnitzler P, Gsenger J, Giese T, Merle U. High rate of HSV-1 reactivation in invasively ventilated COVID- 19 patients: Immunological findings. PLoS One. 2021;16:e0254129. doi: 10.1371/journal.pone.0254129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Majtanova N, Kriskova P, Keri P, Fellner Z, Majtan J, Kolar P. Herpes simplex keratitis in patients with SARS-CoV-2 infection: A series of five cases. Medicina. 2021;57:412. doi: 10.3390/medicina57050412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zheng M, Gao Y, Wang G, Song G, Liu S, Sun D, et al. Functional exhaustion of antiviral lymphocytes in COVID-19 patients. Cell Mol Immunol. 2020;17:533–5. doi: 10.1038/s41423-020-0402-2. [DOI] [PMC free article] [PubMed] [Google Scholar]