Abstract
Background
Post-traumatic kyphosis of the thoracic and lumbar spine can lead to pain and decreased function. MRI has been advocated to assess ligament integrity and risk of kyphosis.
Methods
All thoracic and lumbar spine MRI performed for evaluation of trauma over a 3-year period at a single institution were reviewed. Patients were included if there was an MRI showing a vertebral body fracture and follow-up radiographs. Two observers retrospectively reviewed all radiographs, CT and MRI scans, and classified injuries based on the Denis, TLICS, AO and load sharing classification systems. Change in kyphosis between injury and follow-up studies was measured. The initial radiology reports made at time of patient injury were compared to the retrospective interpretations.
Results
There were 67 separate injuries in 62 patients. Kyphosis measuring ≥ 10° developed despite an intact PLC in 6/14 nonoperative cases, and 3/7 surgically treated cases; when PLC was partially injured, it developed in 6/10 cases (8 treated nonoperatively, 2 treated operatively. Thirty injuries had complete disruption of PLC by MRI, 24 treated with fusion. Kyphosis ≥ 10° developed in 3/6 treated nonoperatively, and 8/24 treated with fusion. Development of kyphosis was independent of degree of vertebral body comminution. It developed equally in patients with Grade 2 and Grade 3 Denis injuries. It developed in patients with intact PLC when multiple vertebrae were involved and/or there was compressive injury to anterior longitudinal ligament (ALL). There was high interobserver variability in assessment of severity of ligamentous injury on MRI.
Conclusions
Classification systems of thoracic and lumbar spine injury and integrity of the PLC failed to predict the risk of development of post-traumatic kyphotic deformity.
Keywords: Posterior ligamentous complex (PLC), Thoracolumbar spine trauma, Post-traumatic kyphosis, MRI of spine trauma, Denis classification, AO classification spine trauma, Load-sharing classification, TLICS classification, Anterior longitudinal ligament
Abbreviations: AO, Arbeitsgemeinschaft für Osteosynthesefragen; TLICS, Thoraco-Lumbar injury Classification and severity scale; PLC, posterior ligamentous complex, anterior longitudinal ligament-ALL; PLL, posterior longitudinal ligament
Introduction
The classification of thoracic and lumbar spine fractures is a subject of ongoing debate. Many classification schemes have been proposed. Each system's goal is to improve uniformity of description of injury, direct treatment and predict patient outcomes. The Denis system [1] was published in 1983 and has had the longest utilization. The Thoraco-Lumbar Injury Classification and Severity scale (TLICS) [2,3] was developed in 2006. The AO classification [4] was first proposed by Magerl [5] in 1994, and subsequently modified. The load sharing system was proposed in 1994 to focus attention on the anterior column of the spine in axial load injuries [6,7].
The Denis, TLICS and AO classify fractures based on the forces acting on the spine, vertebral body fracture morphology, and distraction injury to the posterior ligamentous complex (PLC) or anterior longitudinal ligament (ALL). AO system divides fractures into 3 main groups, of which type A are compression (axial load), type B are tension band (either injury to the PLC or osseous posterior column), and type C are displacement injuries, including hyperextension, translation and separation. The load-sharing system was developed for evaluation of burst fractures, and classifies vertebral body fractures based on the amount of comminution and displacement in the sagittal and axial planes.
We studied the ability of classification systems to predict a single outcome measure, development of progressive kyphotic deformity, which is often associated with back pain, decreased daily function and adjacent segment degeneration [8], [9], [10].
Materials and methods
Patient cohort
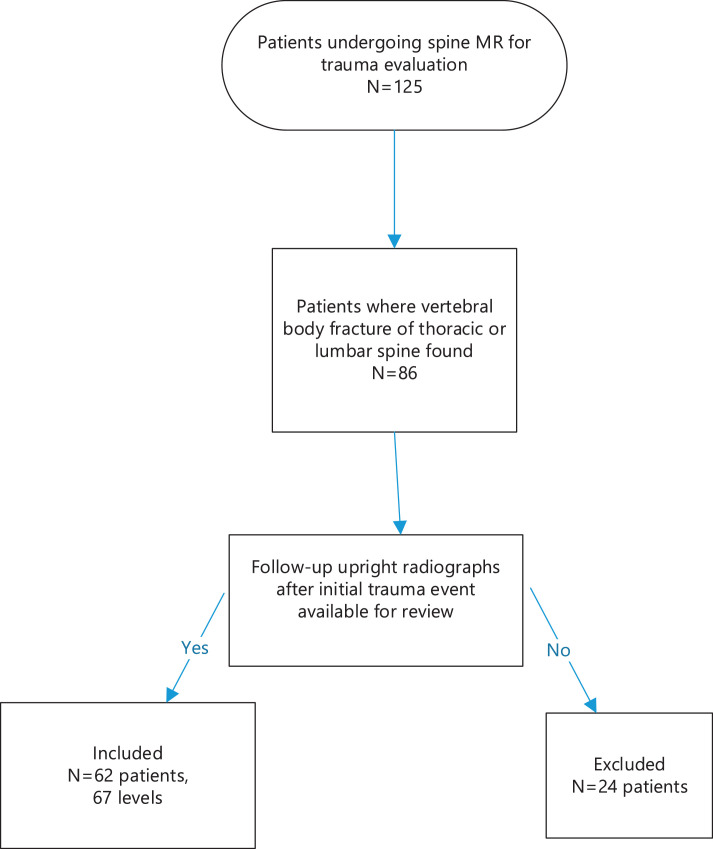
Institutional review board approval was obtained prior to beginning the study, and the study was Health Insurance Portability and Accountability Act compliant. Informed consent was waived. Radiology records were retrospectively reviewed for all patients who underwent MRI for acute thoracic and lumbar spinal trauma at a single level 1 trauma hospital between January 2014 and December 2017, excluding patients in whom vertebral body fracture was related to neoplasm or infection. Patients were included in the study if imaging demonstrated traumatic thoracic or lumbar vertebral body fractures, and follow-up upright radiographs were available. Sixty-two patients (67 separate injury levels) met criteria. Fig. 1 shows flowchart of patient selection. All MRI scans were at 1.5 Tesla, and included sagittal T1-weighted, T2-weighted and STIR sequences as well as axial T2-weighted images.
Fig. 1.
Flowchart showing patient selection for the study.
Imaging evaluation
The initial and follow-up imaging studies were retrospectively reviewed by two radiologists by consensus, without knowledge of the initial interpretations of the studies which were made at time of presentation and treatment. Fractures were classified based on published criteria for Denis [1], TLICS [2,3,[11], [12], [13]], AO [4] and load-sharing [7,6] classifications. Published literature was used as the guide for assessment of MRI findings of ligament disruption [14], [15], [16]. The first observer is a fellowship-trained musculoskeletal radiologist with 30 years’ experience in trauma spine MRI interpretation, and the second is an interventional radiology fellow. The spinal level, number of involved vertebrae, vertebral body fracture morphology, status of ligaments, posterior element fractures, and alignment on initial MRI and follow-up imaging were recorded. Upright radiographs were obtained, usually after the initial CT scan, in all patients, and all but 10 patients also were examined with CT scan in addition to the injury MRI at the time of injury; these were also reviewed.
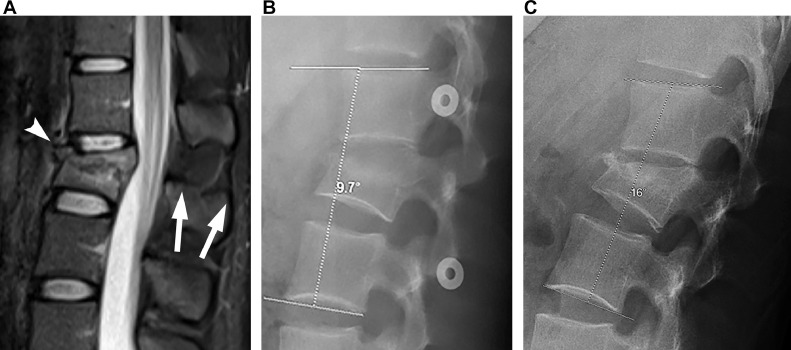
Measurement of kyphosis in the trauma setting has been previously shown to have high interobserver and intraobserver reliability [17], and for that reason variability was not measured for this study. Utilizing the method of Cobb, the change in kyphosis was calculated between MRI (performed supine) and initial pretreatment upright radiographs, as well as between MRI and final upright radiographs (Fig. 2). Sagittal plane alignment was measured on supine MRI scans as a surrogate for supine radiographs. The change in focal sagittal plane alignment from supine to upright, measured from 1 level above to 1 level below the fracture, was used to assess axial mechanical instability of the fracture at time of injury: i.e., the development of focal, acute kyphosis indicated loss of vertebral body height under the stress of weight-bearing. This comparison is analogous to the standard comparison of supine to upright images for evaluation of scoliosis, or supine to gravity stress views of the ankle for ankle stability.
Fig. 2.
Twenty-three-year-old male who fell from a height. A. Sagittal STIR image in midline shows burst morphology of L2 fracture, with retropulsion of the posterior vertebral body cortex. Loss of vertebral body height is <50%. Kyphosis measured 5° using the method of Cobb, from 1 level above the injury to 1 level below. All radiology readers agreed that the posterior ligamentous complex is intact (arrows). There is increased signal intensity of the anterior longitudinal ligament (arrowhead) consistent with sprain due to compression, but there is no fluid signal to indicate ligament discontinuity. There was no neurologic deficit. TLICS score is 2. Denis grading is 2 column injury. AO grading is A3. Load sharing classification based on CT (not shown) is mild comminution (score of 1), and minimal axial spreading (score of 1), total score 2. B. Initial upright lateral radiograph shows the kyphosis has increased to 10° compared to 5° on supine MRI. C. Final lateral radiograph, obtained 3 months after injury, shows kyphosis has increased to 16°, for an overall increase in kyphosis of 11° compared to the initial supine MRI.
Each level of injury was classified using the TLICS, AO, Denis, and load-sharing classification systems. The original radiologist's MRI interpretation made at the time that the patient presented was also reviewed, at a separate time subsequent to the independent review of the images; the original MRI interpretations were made by fellowship-trained neuroradiologists and musculoskeletal radiologists at the same Level 1 Trauma Center. The original and retrospective radiologic interpretations were compared. Data were analyzed for patients of all ages, as well as separate analyses to assess the potential impact of osteoporosis. Patients were placed in the category of higher likelihood of osteoporosis when they were males >age 60 and females > age55 [15]. Progressive kyphosis at the injured level was recorded, and subdivided into 2 groups: 10–19°, and 20° or more.
Statistical analysis
Statistical analysis was performed using SAS 9.4 version using PROC FREQ procedure. Odds ratios were calculated for relative risk of developing kyphosis for differing grades of injury. Cohen's Kappa coefficient (κ) was used to measure the interobserver agreement for MRI diagnosis of PLC injury. The categorization of κ value follows the guidelines proposed by Landis and Koch [18]. Treatment and outcomes were recorded from the electronic medical record.
Theory
Classification systems are useful when they are unambiguous, have high interobserver consistency, and predict outcomes. There is a paucity of literature on the ability of spine trauma classifications to predict patient outcomes. This paper evaluates how different classifications predict a single outcome measure.
Results
Patient cohort
There were 25 female and 37 male patients, ages 15 to 77 years (mean 40.8). Seventeen patients were classified as potentially osteoporotic based on age. There were 67 separate injuries, because 5 patients had 2 noncontiguous levels of injury. There were 14 thoracic, 11 lumbar, and 42 thoracolumbar junction (T11-L2) levels. Percutaneous posterior fixation surgery was performed for 37 injuries, and 30 were conservatively managed. The average time of clinical follow up was 11.1 months with an average time of imaging follow up of 6.2 months. For operatively treated patients, follow-up averaged 4 months. For nonoperatively treated patients, follow-up averaged 8 months. Mechanisms of injury as determined by review of imaging and medical records were axial load (36), flexion-distraction (18), translation (10) and extension (3).
Fracture classification
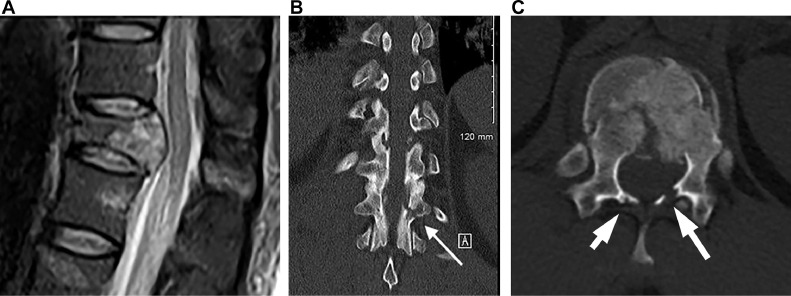
Table 1 shows fractures and outcomes as categorized by the different systems. One Denis 2 column injury was due to a flexion-distraction mechanism, with disruption of PLC. Following the guidelines in Denis’ original paper, this was included with the Denis 3 column fractures as an unstable injury. One fracture could not be classified in the TLICS system because the patient had neurologic deficits from a concomitant cervical spine injury. There were no injuries classified as TLICS 3. The assessment of injury severity by the different classification systems was variable: several TLICS 1–2 met Denis 3 criteria (Fig. 3).
Table 1.
. Grade of injury in TLICS, Denis, and AO systems, correlated to nonsurgical or surgical treatment and development of progressive kyphosis. Classifications are based on retrospective readings. Δ=delta or change in kyphosis.
| Patients treated without surgery | Patients with surgical fixation | |||||
|---|---|---|---|---|---|---|
| Grade of injury | Total | Kyphosis Δ10–19º | KyphosisΔ> 20 º | Total | KyphosisΔ10-19º | KyphosisΔ> 20 º |
| TLICS 1-2 (n = 23) | 18 (78%) | 6 (33%) | 0 (0%) | 5 (22%) | 1 (20%) | 0 (0%) |
| TLICS 4 (n = 10) | 7 (70%) | 4 (57%) | 1 (14%) | 3 (30%) | 2 (67%) | 0 (0%) |
| TLICS 5+ (n = 33) | 4 (12%) | 0 (0%) | 2 (50%) | 29 (88%) | 6 (21%) | 4 (14%) |
| TLICS Indeterminate (n = 1) | 1 (100%) | 1 (100%) | 0 (0%) | 0 | na | na |
| Denis 1 (n = 5) | 5 (100%) | 1 (20%) | 0 (0%) | 0 | na | na |
| Stable Denis 2 (n = 24) | 17 (71%) | 9 (53%) | 1 (6%) | 7 (29%) | 2 (29%) | 0 (0%) |
|
Denis 3 (n = 37) + Unstable Denis 2 (n = 1) |
8 (21%) | 1 (13%) | 2 (25%) | 30 (79%) | 7 (23%) | 4 (13%) |
| AO A only (n = 32) | 23 (72%) | 10 (39%) | 0 (0%) | 9 (28%) | 4 (44%) | 0 (0%) |
| AO B1-2: all A, C = 0 (n = 21) | 6 (29%) | 1 (17%) | 3 (50%) | 15 (71%) | 2 (13%) | 3 (20%) |
| AO B3: all A, C = 0 (n = 2) | 0 | 0 | 0 | 2 | 1 (50%) | 0 |
| AO C: All A, all B (n = 12) | 1 (8%) | 0 | 0 | 11 (92%) | 2 (18%) | 1 (9%) |
Fig. 3.
Twenty-seven-year-old male who fell from a height, showing discordance of surgical recommendations from TLICS, Denis and load sharing classifications. The patient underwent surgical fixation one level above and one level below the fracture, and had no increased kyphosis on follow up imaging. A. Sagittal STIR shows burst morphology of T12 fracture, with intact PLC. Neurologic status was normal, and this injury has a TLICS score of 2, indicating nonsurgical management is recommended. The load sharing score based on CT is 4, and nonoperative management would be recommended. B. Coronal CT shows fracture of the left pars interarticularis (arrow) indicating 3-column fracture in Denis classification. This is an A4B2 injury in AO classification. C. Axial CT shows that bilateral laminar fractures (arrows) are also present.
The load-sharing system is limited to axial load injuries, and was therefore not compared to the more inclusive classifications. The degree of vertebral body comminution was diagnosed as none in 3 patients (4.48%), mild in 38 (56.72%), moderate in 21 (31.34%) and severe in 5 (7.46%). Axial (transverse plane) displacement of vertebral body fragments was none in 2 (2.99%), mild in 22 (32.84%), moderate in 28 (41.79%), and severe in 15 (22.39%). None of the surgeons formally employed a classification system.
Outcomes and treatment
Overall, 12 injuries developed post-traumatic kyphosis of 10–19°, and 4 developed kyphosis of >20°, with the largest post-traumatic kyphosis measuring 26°. Kyphosis occurred with injuries at all levels, but injuries to the thoracic spine above T11 resulted in kyphosis of 10° or greater only when 2 or more vertebral bodies were fractured.
Injury to the PLC as documented on MRI did not correlate to development of kyphosis (P = 0.86); the odds ratio of development of kyphosis with PLC injury was 0.91 (95% CI = 0.32–2.6). There was no significant difference in development of kyphosis between Denis Grade 2 and Grade 3 injuries (P = 0.35). Utilizing the load sharing classification, axial (transverse) spread of fracture fragments did not correlate to development of kyphosis (P = 0.41), and neither did degree of fracture comminution (P = 0.85).
Potential contribution of compressive anterior longitudinal ligament (ALL) and posterior longitudinal ligament (PLL) injury
A compressive, incomplete injury to the ALL was seen in 21 patients who developed a kyphotic deformity. This represents an odds ratio of 1.625 (95% CI 0.558–4.73) for the development of kyphosis, compared to patient with intact ALL. Seven patients who developed kyphosis had injury to the ALL but an intact PLC. Injury to the PLL did not contribute to the development of kyphosis. Twenty-three patients had PLL injury; odds ratio of developing kyphosis due to PLL injury was 0.643 (95% CI 0.2268–1.822).
Involvement of multiple contiguous spinal levels
Thirteen patients (4 axial load, 7 flexion distraction and 2 translation) had injuries involving at least 3 contiguous levels. Seven of them underwent surgery; four out of the 6 who were treated nonsurgically developed significant kyphosis. One patient with multilevel injury in the potentially osteoporotic group developed kyphosis despite surgical fixation.
Potential contribution of osteoporosis
Seventeen injuries were in the potentially osteoporotic age group. Seven of these (41%) developed kyphotic deformity. Two of these were 2 column Denis and 2 points TLICS, while 5 were 3 column Denis and 4–7 points TLICS. In comparison, 17/50 (34%) of younger patients developed a kyphotic deformity.
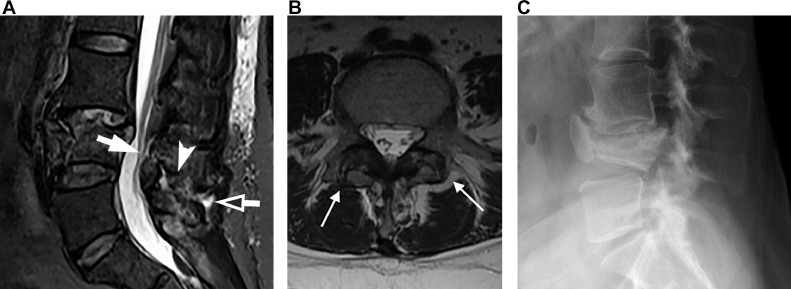
Interobserver variability
Interobserver variability in assessment of PLC integrity is summarized in Table 2. The greatest area of disagreement was in the diagnosis of an injured but not definitely disrupted PLC. There were 18 cases where the PLC was prospectively called injured but not definitively disrupted, and the retrospective reading agreed with this assessment in only 2 cases. This disagreement in PLC status led to changes in the TLICS scores of multiple patients. Two injuries were changed from TLICS category 1–3 on prospective radiology reading to category 4 on retrospective reading, and 5 injuries were changed from prospective TLICS category 4 to category 5 or above on retrospective review (Fig. 4).
Table 2.
Correlation of prospective (at time that study was performed and retrospective (review by independent reader without knowledge of initial reading or patient history) assessment of the PLC out of 42 patients in whom the integrity of the PLC was prospectively assessed. Kappa = 0.3162 (95% confidence interval 0.1302–0.5022).
| Prospective assessment of PLC | Retrospective assessment of PLC | |||
|---|---|---|---|---|
| normal | Partially injured | Completely torn | Total | |
| Normal | 6 (14.29%) |
3 (7.14%) |
0 (0.00%) |
9 (21.43%) |
| Partially injured | 2 (4.76%) |
2 (4.76%) |
14 (33.33%) |
18 (42.86%) |
| Completely torn | 0 (0.00%) |
0 (0.00%) |
15 (35.71%) |
15 (35.71%) |
| Total | 8 (19.05%) |
5 (11.90%) |
29 (69.05%) |
42 (100.00%) |
Fig. 4.
Fifty-year-old woman with flexion-distraction injury at L4 due to motor vehicle collision. Injury was 3-column by Denis classification, with posterior element fractures present in addition to burst morphology, and A4B2 in AO classification. There was mild comminution and moderate spreading of the fragments (3 points in the load sharing classification). Initial MRI interpretation at time of injury was partial injury of PLC (TLICS 4) but retrospective interpretation was complete PLC injury (TLICS 5). Neurologic status was normal. A. Sagittal STIR MRI Initial MRI was interpreted at time of injury as partial PLC injury. On retrospective review, it was felt to be completely disrupted. Solid arrow points to ligamentum flavum, arrowhead to interspinous ligament, and open arrow to supraspinous ligament. The patient did not undergo surgical fixation. Lordosis from L3 to L5 measured 36°.B. Axial T2 WI 13 months after injury shows widened facet joints (arrows), which were not present on initial MRI. C. Lateral radiographs 13 months after injury show healed fracture, with loss of vertebral body height. Lordosis measured 10°, representing a 25° decrease from the original MRI. The patient complained of chronic back pain.
Discussion
We studied a single outcome measure of thoracic and lumbar spine trauma, post-traumatic kyphosis in thoracic and lumbar spine. Kyphosis can lead to pain, postural imbalance, and adjacent segment degeneration. It is our hope that our data might raise awareness of limitations in current classification systems, and consideration of additional factors which may lead to development of kyphosis.
By providing a posterior tether, the PLC restrains the spine against the development of kyphotic deformity. Previous reports [19] have found high interobserver variability in the MRI assessment of PLC injury, and this was confirmed in our series. The place of MRI in the management of thoracic and lumbar trauma is debated. A recent series of patients without neurologic injury found that MRI changed management in 15% of cases [20]. A consensus paper from the Congress of Neurologic Surgeons found that MRI can change management by evaluation of PLC [21]. A recent literature review found that MRI shows high positive predictive value and low negative predictive value for injury to the PLC, but also that there is little information about the prognostic value of PLC injury [22].
Without anterior column support, an intact PLC will not prevent kyphosis, as shown in a study which found that loss of vertebral body height >50% and local kyphosis of 20° on the initial trauma evaluation did not correlate to PLC injury [23]. The load sharing classification provides the most extensive evaluation of the integrity of the anterior column, although it is limited to the evaluation of axial load injuries. It has not been found to correlate to PLC injury or empiric decision making [24]. Our study did not find that the load sharing system correlated to development of kyphosis. Data on intra and interobserver consistency utilizing the load sharing classification is mixed, with an earlier study finding excellent reliability [25], but a later study finding only fair reliability [26].
One study compared operative to nonoperative treatment of injuries with a TLICS score of 4, where there is incomplete or inconclusive injury to the PLC [22]. They found that patients treated surgically had less pain, less development of kyphosis, and earlier return to work. Ten patients in our cohort were retrospectively assessed as TLICS 4. Kyphotic deformity developed in 5/7 TLICS: 4 patients treated nonoperatively, and 2/3 treated with surgical fixation. The degree of kyphosis was less in the surgical group, but numbers are not sufficient to be statistically significant. This is consistent with a previous long-term follow-up of thoracolumbar burst fractures which found that kyphosis was similar in operatively and nonoperatively managed patients [27].
One case report called the development of kyphotic deformity the “Achilles heel” of TLICS [28]. We believe it is the Achilles heel of other classifications as well. Additional factors which might be addressed in future classification systems are the number of adjacent injured levels, and compressive injury to the anterior longitudinal ligament, both of which appeared in our study to contribute to risk of kyphotic deformity.
Study limitations
The study was retrospective. We were unable to compare MRI assessment of ligament integrity to surgical assessment, because surgery was percutaneous. Overall sagittal alignment of the spine was not evaluated because full standing radiographs were not obtained. We cannot say what degree of progressive kyphosis correlates to pain.
Study strengths
All images were high-resolution and performed at a single institution. Review of images was unbiased by clinical examination. We compared the radiologists’ interpretations at time of the injury to a separate interpretation based on in-depth literature review of classification systems and imaging findings.
Summary
The prevalent thoracolumbar spine trauma classification systems and MRI demonstration of injury to the PLC are not predictive of development of kyphosis. Interobserver variability in assessing injury to PLC on MRI is high. The number of adjacent injured levels and the presence of compressive injury to the ALL are risk factors for development of kyphosis.
Declarations
Funding
No funding was received.
Ethics approval
Study was IRB approved and HIPAA compliant.
Consent to participate
Consent was waived.
Consent for publication
Consent was waived.
Availability of data and material
Data is maintained securely at institution where performed.
Code availability
None.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. The authors report no conflict of interest.
Footnotes
Short sentence: Post-traumatic kyphotic deformity in the thoracic and lumbar spine may develop in the presence of an intact PLC, and depends in part on number of contiguous involved vertebrae and compressive injury to the ALL.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.xnsj.2022.100134.
Appendix. Supplementary materials
References
- 1.Denis F. Spinal instability as defined by the three-column spine concept in acute spinal trauma. Clin Orthop Relat Res. 1984;(189):65–76. [PubMed] [Google Scholar]
- 2.Bono C.M., Vaccaro A.R., Hurlbert R.J., et al. Validating a newly proposed classification system for thoracolumbar spine trauma: looking to the future of the thoracolumbar injury classification and severity score. J Orthop Trauma. 2006;20(8):567–572. doi: 10.1097/01.bot.0000244999.90868.52. [DOI] [PubMed] [Google Scholar]
- 3.Lee J.Y., Vaccaro A.R., Lim M.R., et al. Thoracolumbar injury classification and severity score: a new paradigm for the treatment of thoracolumbar spine trauma. J Orthop Sci. 2005;10(6):671–675. doi: 10.1007/s00776-005-0956-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schnake K.J., Schroeder G.D., Vaccaro A.R., Oner C. AOSpine classification systems (subaxial, thoracolumbar) J Orthop Trauma. 2017;31(Suppl 4):S14–S23. doi: 10.1097/BOT.0000000000000947. [DOI] [PubMed] [Google Scholar]
- 5.Magerl F., Aebi M., Gertzbein S.D., Harms J., Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3(4):184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 6.Dai L.Y., Jiang L.S., Jiang S.D. Conservative treatment of thoracolumbar burst fractures: a long-term follow-up results with special reference to the load sharing classification. Spine. 2008;33(23):2536–2544. doi: 10.1097/BRS.0b013e3181851bc2. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]
- 7.McCormack T., Karaikovic E., Gaines R.W. The load sharing classification of spine fractures. Spine. 1994;19(15):1741–1744. doi: 10.1097/00007632-199408000-00014. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]
- 8.Buchowski J.M., Kuhns C.A., Bridwell K.H., Lenke L.G. Surgical management of posttraumatic thoracolumbar kyphosis. Spine J. 2008;8(4):666–677. doi: 10.1016/j.spinee.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 9.Vaccaro A.R., Silber J.S. Post-traumatic spinal deformity. Spine. 2001;26(24 Suppl):S111–S118. doi: 10.1097/00007632-200112151-00019. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]
- 10.Been H.D., Poolman R.W., Ubags L.H. Clinical outcome and radiographic results after surgical treatment of post-traumatic thoracolumbar kyphosis following simple type A fractures. Eur Spine J. 2004;13(2):101–107. doi: 10.1007/s00586-003-0576-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vaccaro A.R., Baron E.M., Sanfilippo J., et al. Reliability of a novel classification system for thoracolumbar injuries: the thoracolumbar injury severity score. Spine. 2006;31(11 Suppl):S62–S69. doi: 10.1097/01.brs.0000218072.25964.a9. (Phila Pa 1976)discussion S104. [DOI] [PubMed] [Google Scholar]
- 12.Vaccaro A.R., Lehman R.A., Hurlbert R.J., et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine. 2005;30(20):2325–2333. doi: 10.1097/01.brs.0000182986.43345.cb. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]
- 13.Vaccaro A.R., Rihn J.A., Saravanja D., et al. Injury of the posterior ligamentous complex of the thoracolumbar spine: a prospective evaluation of the diagnostic accuracy of magnetic resonance imaging. Spine. 2009;34(23):E841–E847. doi: 10.1097/BRS.0b013e3181bd11be. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]
- 14.Pizones J., Izquierdo E., Alvarez P., et al. Impact of magnetic resonance imaging on decision making for thoracolumbar traumatic fracture diagnosis and treatment. Eur Spine J. 2011;20(Suppl 3):390–396. doi: 10.1007/s00586-011-1913-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pizones J., Sanchez-Mariscal F., Zuniga L., Alvarez P., Izquierdo E. Prospective analysis of magnetic resonance imaging accuracy in diagnosing traumatic injuries of the posterior ligamentous complex of the thoracolumbar spine. Spine. 2013;38(9):745–751. doi: 10.1097/BRS.0b013e31827934e4. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]
- 16.Smith H., Rihn J.A., Radcliff K.E., Vaccaro A.R. Imaging in the setting of thoracolumbartrauma: the use of magnetic resonance imagin to diagnose injury to the posterior ligamentous complex. Semin Spine Surg. 2012;24:216–220. [Google Scholar]
- 17.Ulmar B., Brunner A., Guhring M., Schmalzle T., Weise K., Badke A. Inter- and intraobserver reliability of the vertebral, local and segmental kyphosis in 120 traumatic lumbar and thoracic burst fractures: evaluation in lateral X-rays and sagittal computed tomographies. Eur Spine J. 2010;19(4):558–566. doi: 10.1007/s00586-009-1231-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Landis J.R., Koch G.G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 19.Lee G.Y., Lee J.W., Choi S.W., et al. MRI inter-reader and intra-reader reliabilities for assessing injury morphology and posterior ligamentous complex integrity of the spine according to the thoracolumbar injury classification system and severity score. Korean J Radiol. 2015;16(4):889–898. doi: 10.3348/kjr.2015.16.4.889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khoury L., Chang E., Hill D., et al. Management of thoracic and lumbar spine fractures: is MRI necessary in patients without neurological deficits? Am Surg. 2019;85(3):306–311. doi: 10.1177/000313481908500338. [DOI] [PubMed] [Google Scholar]
- 21.Qureshi S., Dhall S.S., Anderson P.A., et al. Congress of neurological surgeons systematic review and evidence-based guidelines on the evaluation and treatment of patients with thoracolumbar spine trauma: radiological evaluation. Neurosurgery. 2019;84(1):E28–E31. doi: 10.1093/neuros/nyy373. [DOI] [PubMed] [Google Scholar]
- 22.van Middendorp J.J., Patel A.A., Schuetz M., Joaquim A.F. The precision, accuracy and validity of detecting posterior ligamentous complex injuries of the thoracic and lumbar spine: a critical appraisal of the literature. Eur Spine J. 2013;22(3):461–474. doi: 10.1007/s00586-012-2602-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Radcliff K., Su B.W., Kepler C.K., et al. Correlation of posterior ligamentous complex injury and neurological injury to loss of vertebral body height, kyphosis, and canal compromise. Spine. 2012;37(13):1142–1150. doi: 10.1097/BRS.0b013e318240fcd3. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]
- 24.Radcliff K., Kepler C.K., Rubin T.A., et al. Does the load-sharing classification predict ligamentous injury, neurological injury, and the need for surgery in patients with thoracolumbar burst fractures? Clinical article. J Neurosurg Spine. 2012;16(6):534–538. doi: 10.3171/2012.3.SPINE11570. [DOI] [PubMed] [Google Scholar]
- 25.Dai L.Y., Jin W.J. Interobserver and intraobserver reliability in the load sharing classification of the assessment of thoracolumbar burst fractures. Spine. 2005;30(3):354–358. doi: 10.1097/01.brs.0000152095.85927.24. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]
- 26.Elzinga M., Segers M., Siebenga J., Heilbron E., de Lange-de Klerk E.S., Bakker F. Inter- and intraobserver agreement on the load sharing classification of thoracolumbar spine fractures. Injury. 2012;43(4):416–422. doi: 10.1016/j.injury.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 27.Wood K.B., Buttermann G.R., Phukan R., et al. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit: a prospective randomized study with follow-up at sixteen to twenty-two years. J Bone Jt Surg Am. 2015;97(1):3–9. doi: 10.2106/JBJS.N.00226. [DOI] [PubMed] [Google Scholar]
- 28.Mattei T.A., Hanovnikian J., D H.D. Progressive kyphotic deformity in comminuted burst fractures treated non-operatively: the achilles tendon of the thoracolumbar injury classification and severity score (TLICS) Eur Spine J. 2014;23(11):2255–2262. doi: 10.1007/s00586-014-3312-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data is maintained securely at institution where performed.