Abstract
Low vaccination rates among health care providers (HCPs) pose a risk to themselves, their colleagues, their patients, and the general public. This paper seeks to frame the issues surrounding health care provider vaccine hesitancy and vaccination rates, as well as explore factors influencing respective decision-making, including health care occupation and demographic characteristics. This paper will then propose the use of the Preferred Cognitive Style and Decision-Making (PCSDM) Model and the Empathy Tool to increase health care provider vaccination rates, and will end by discussing several recommendations. It is important while discussing HCP vaccination rates to not view them as a monolithic group or apply “one-size-fits-all” approaches, and thus it is essential to present information and engage in conversations in ways that align with how the HCP takes in and processes information and decisions. Furthermore, it is vital to increase health literacy across the spectrum of HCP programs and professions. To this end, it is important to teach and incorporate the PCSDM Model and Empathy Tool, along with information about how individuals think and make decisions, into vaccine education programs and training sessions.
Keywords: Vaccine hesitancy, Health care providers, Immunization, Immunization rate, Health decision-making
Introduction
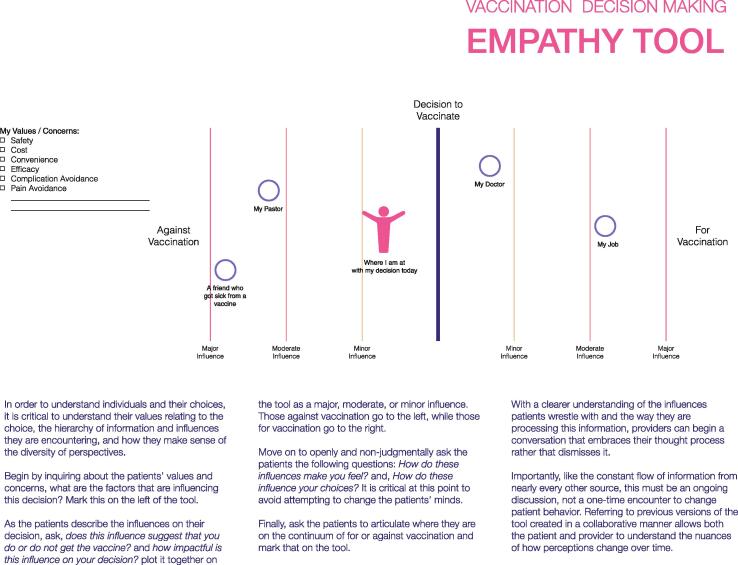
Vaccines have been instrumental in preventing illness, disability, and death – and resulted in the eradication of a major human scourge - smallpox. Perhaps surprisingly, multiple studies have demonstrated issues of vaccine hesitancy and even rejection among health care providers (HCPs) [1], [2], [3], [4], [5], [6]. These issues have been brought to the forefront during the COVID-19 pandemic. Mitigating the health effects of the pandemic required high levels of vaccine acceptance, both for health care providers (HCPs) and the general public [7], [8], [9] As health care providers provide face-to-face services to patients, often in high-risk encounters, it is of critical importance that HCPs protect themselves as well as the patients they serve by the use of safe and effective vaccines as well as other non-pharmaceutical means [10], [11] The knowledge, attitudes, and beliefs of health care providers in regards to vaccines and vaccine acceptance are a critical factor in accepting and delivering vaccines, in protecting themselves, and in being advocates for patient immunization. Yet, issues of vaccine misinformation, hesitancy, and rejection remains an ongoing issue across both developed and developing countries [12]. Exemplars of the issues surrounding vaccine acceptance includes annual influenza immunization and COVID-19 vaccines in HCPs (see Fig. 1).
Fig. 1.
The Empathy Tool. Adapted from Poland et al. [14]; with permission from Vaccine.
This paper will seek to explore the topic of health care provider vaccine hesitancy and acceptance through the lens of applying an understanding of the Preferred Cognitive Styles and Decision-Making Model (PCSDM model) [13] and the use of the Empathy Tool [14] to this important subject.
Health care provider vaccination rates
The problem of low vaccine uptake and significant vaccine hesitancy among HCPs has been evident in the context of seasonal influenza vaccination and other vaccines. Influenza immunization is now universally recommended in the US and other countries and, in many institutions, required for health personnel [6]. Despite the evidence for influenza vaccine in protecting recipients and reducing absenteeism, presenteeism, and transmission of disease to vulnerable patients, some HCPs resisted influenza vaccine requirements. For example, during the 2019–2020 influenza season, overall vaccination coverage among US health care providers was 80.6%, with rates ranging from 77.3% to 81.1% over the past six years [15], [16]. Despite a 15% to 18% increase from the 2010–2011 flu season rates [17], influenza vaccine coverage remains suboptimal [18], [19], [20], and generally stagnant.
Influenza vaccination rates among HCPs in the EU region and, with several exceptions, across all regions worldwide are even more concerning, with no EU countries meeting the target coverage of 75%, and many falling short of 40% [21], [22]. These low rates are despite the general incremental trend which is often related to implementation of influenza vaccination policies and other strategies across healthcare institutions following coverage decline in post-2009 pandemic seasons [21], [22], [23], [24]. While suboptimal influenza vaccine uptake has demonstrated that health care providers are not immune to vaccine hesitancy, the notion gained even more attention and perhaps immediate impact during the COVID-19 pandemic. Prior to the institution of COVID-19 vaccine mandates HCP-specific data related to COVID-19 vaccination rates demonstrated wide discrepancies [25]. Although mandates have led to increased vaccination coverage, significant numbers of HCPs, including frontline workers involved in direct patient care, remain unvaccinated and even vaccine resistant [26], [27]. Notable disparities are observed based on job category, healthcare setting, geographic location, sex and race (females and HCPs from ethnic/racial minorities have higher rates of vaccine hesitancy), and these apply to both vaccine uptake and vaccine hesitancy in a number of countries worldwide [28], [29], [30], [31], [32], [33], [34], [35], [36]. With several exceptions reported, COVID-19 vaccination rates tend to be significantly higher in physicians (approaching > 95% in several surveys and reports, but notably lower than 80% in some settings in the US) than among nursing and allied health staff who generally have higher rates of vaccine hesitancy (uptake dropping to 55% and less in some reports) [26], [37]],[38], [39],[40].
Health care provider vaccination coverage is generally lower in rural healthcare settings [27], [41]. However, some large urban hospitals in several US states also faced alarmingly low vaccine uptake among their staff, particularly during the initial vaccine rollouts [27]. Despite having access to COVID-19 vaccines at the time, as many as 43.2% of all health care providers (24.9% physicians and advanced practice providers, 43.3% nurses and 54.4% aides) in facilities of long-term care in the United States were unvaccinated in April of 2021 [38] putting high-risk patients who suffer the worst consequences of the pandemic at continuous imminent risk.
Several large systematic reviews of existing literature regarding COVID-19 vaccine hesitancy among health care providers published at different stages of vaccine rollout conclude that there is only a moderate level of vaccine acceptance worldwide, with a very wide range (5.2–77.3%) of acceptance [42], [43], [27]. Across a multitude of surveys conducted among HCPs around the globe, the major reasons for vaccine hesitancy/uncertainty or refusal are similar for influenza and COVID-19 vaccines and include concerns about safety, possible side-effects, fast-track approvals by national regulatory authorities, unknown long-term risks of getting the vaccine, lack of knowledge about available vaccines, assumed low risk of getting the disease, minimization of actual threats imposed by the virus, and low levels of trust in government and health authorities, to list a few [26], [37], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53],[[54], [28], [29] On the other hand, high perception of risks to oneself, family, and patients, direct care of infected patients (however, at least one report identifies this as an insignificant variable [55], general knowledge about and confidence in vaccine efficacy/safety, prior influenza vaccination, male sex, and vaccine mandates are associated with higher vaccine acceptance among HCPs [26], [47], [48], [42], [34], [56], [22], [57][[3], [58], [59].
Over the years, various strategies ranging from facilitating easy access on-site vaccination to educational activities to vaccination requirements have been implemented with varying success in improving vaccination rates among HCPs. [6], [60], [61], [62], [63]. Even though the reports on the success of similar interventions are conflicting at times, overall, easy access, free vaccination, educational campaigns, peer-based interventions and social norming [64], decision aids, various incentives, requirements for vaccine declination forms and, critically, vaccine mandates have been associated with increases in immunization rates in diverse healthcare settings [59], [65], [66], [67], [68]. Importantly, combinations of these different strategies and multifaceted approaches are likely to be more successful than any individual strategy alone [69]. Expert reviews on the extensive topic of vaccination-promoting methods and studies of their effectiveness have been published elsewhere [65], [69], [70], [71].
While the importance of high vaccination coverage among health care providers in reducing morbidity and mortality caused by vaccine-preventable infectious agents cannot be overstated, the role of vaccines in preventing communicable diseases should transcend one’s own health behaviors. Even in today’s era of expanding influences, unlimited web access to both accurate and unreliable medical information, and overwhelming social media discussion of often suspicious or misinformation in regard to vaccines, healthcare personnel remain one of the most trusted sources of knowledge and advice about immunization for diverse communities worldwide [12], [6], [50]. It has been repeatedly demonstrated that vaccinated and vaccine confident HCPs are more likely to recommend vaccination to their patients [6], [72], [51], [57], [73]. Thus, health personnel play a unique and pivotal role in discussions about immunization. Such advocacy can lead to increased vaccination coverage, and this is an important strategy in defeating this pandemic and vaccine preventable diseases in general.
The preferred cognitive styles and decision-making model
In order to increase HCP vaccination rates across the spectrum of the health care professions, it is important to understand how individuals take in information, process that information, and make decisions about their health. The Preferred Cognitive Style and Decision-Making Model [13] seeks to understand the ways in which individuals, including HCPs, make decisions about a variety of health behaviors, including vaccine acceptance. This model seeks to understand the preferred cognitive style(s) that an individual employs in making decisions and looks at how this impacts the choices they make. The underlying premise of the model is “the idea that an individual’s preferred cognitive style, emotional baseline, and subsequent behavior, are all intertwined.” [13] This model emphasizes the fact that humans do not make decisions in a singular way, but instead employ a variety of different styles when making decisions. Thus, to discuss health decisions in one formulaic way i.e., a “one size fits all”, leads to missing how individuals (patients and providers) take in and process information in different ways. Thus, it is important for the HCP, and the medical community as a whole, to be flexible in their presentation of vaccine information, along with how they engage in conversation about vaccine fears and hesitancy, in order to present information in such a way that aligns with the preferred cognitive style of the listener (i.e. a patient or a HCP). If the HCP is not trained in this skill, they will likely miss key opportunities to move the decision-making conversation forward by presenting information that the patient can best understand and process. It is important to note that HCPs are also patients, and thus information regarding how HCPs communicate with their patients also applies to HCPs in general. And while this is true of the HCP to patient conversation (and HCP to HCP as the patient conversation), it is also true in the ways that education programs communicate with HCPs, of how HCPs are professionalized, and the peer-to-peer conversations across the health care profession as well.
Table 1 outlines several of these common cognitive styles, their verbal expressions/phenotypes, and communication strategies that might be helpful for that style. It is critical to remember that an individual’s cognitive style impacts how information is taken in and processed, and how and whether they move forward in decision-making. For the HCP, their preferred cognitive style can impact how they take in information and data through their educational process (i.e. nursing school, medical school, others), how they interact with research, study design and data, and ultimately how they communicate with their patients.
Table 1.
Table adapted from Poland CM, Poland GA. Vaccine education spectrum disorder: the importance of incorporating psychological and cognitive models into vaccine education. Vaccine. 2011 Aug 26;29[37]:6145–8 with permission from Vaccine.
| Preferred Cognitive Styles Communication and Approaches | |||
|---|---|---|---|
| Cognitive style | Main effect | Verbal expression | Approach |
| Denialist | Disbelieves accepted scientific facts, despite overwhelming evidence. Prone to believe conspiracy theories | “I don’t care what the data show, I don’t believe the vaccine is safe” | Provide consistent messaging repeatedly over time from trustworthy sources, provide educational materials, solicit questions, avoid “hard sell” approach, use motivational interviewing approaches |
| Innumerate | Cannot understand or has difficulty manipulating numbers, probabilities, or risks | “One in a million risk sounds high, for sure I’ll be the 1 in a million that has a side effect, I’ll avoid the vaccine” | Provide nonmathematical information, analogies, or comparators using a more holistic “right brain” or emotive approach |
| Fear-based | Decision making based on fears | “I heard vaccines are harmful and I’m not going to get them” | Understand source of fear, provide consistent positive approach, show risks in comparison to other daily risks, demonstrate risks of not receiving vaccines, use social norming approaches |
| Heuristic | Often appeals to availability heuristic (what I can recall equates with how commonly it occurs | “I remember GBS happened in 1977 after flu vaccines, that must be common, and therefore I’m not getting a flu vaccine” | Point out inconsistencies and fallacy of heuristic thinking, provide educational materials, appeal to other heuristics |
| Bandwagoning | Primarily influenced by what others are doing or saying | “If others are refusing the vaccine there must be something to it. I’m going to skip getting the vaccine” | Understand primary influencers, point out logical inconsistencies, use social norming and self-efficacy approaches |
| Analytical | Left brain thinking, facts are paramount | “I want to see the data so I can make a decision” | Provide data requested, review analytically with patient |
As an example, we can examine a HCP who is more emotion-driven in their decision-making, perhaps making decisions based on fear (the fear-based cognitive style). This provider might hear and even be able to repeat back the data applicable to a vaccine, but based on their own fears, and perhaps the personal anecdotes that they have read about online (i.e. comments on social media platforms), they struggle with their own fears and worries outweighing the facts they have been taught and that research has demonstrated. In this case, continuing to push the data and facts is simply unhelpful, as the individual already knows the data and facts. Instead, it is important to listen to understand the source of their fear, utilize the empathy tool (discussed later in this article), help the individual engage in a self-led risk: benefit analysis, and perhaps engage in social norming, among other strategies.
As noted above, the attitudes of the HCP toward vaccination, and their own confidence levels in discussing vaccination and vaccine efficacy, matter significantly in their own vaccine acceptance as well as their patient’s vaccine acceptance. In a study completed with internal medicine residents at the Mayo Clinic, residents were randomized into two groups: one was a fact-based curriculum and the other a PCSDM-based curriculum. At the end of the study, researchers concluded that “The intervention group (the PCSDM-based curriculum group) had significant improvements in multiple domains that assessed confidence in counseling patients on immunizations.” [74]. This increased confidence in communicating about vaccine hesitancy and decision-making is critical, whether the HCP is processing the data themselves, or in communication with their patients.
To add another layer to this discussion, it is important to mention Michael Shermer’s thoughts on belief-dependent realism. He says: “We form our beliefs for a variety of subjective, emotional and psychological reasons in the context of environments created by family, friends, colleagues, culture and society at large. After forming our beliefs, we then defend, justify and rationalize them with a host of intellectual reasons, cogent arguments and rational explanations. Beliefs come first; explanations for beliefs follow.” [75]. Once beliefs have been established, a framework has been created to easily accept or reject certain data. If, for example, a belief exists that the COVID-19 vaccine isn’t safe (the formation of a belief), this belief will be defended and justified, and data that goes against this belief will likely be rejected. The critical point is that explanations for beliefs often come after the belief has been formed instead of the explanations (i.e. the data) informing the creation of beliefs. Understanding the process of belief-dependent realism in decision-making is important, especially as HCPs arrive at their undergraduate and graduate education with beliefs already in place about certain aspects of health, including vaccine acceptance and hesitancy. Exploring these beliefs and engaging in a process of how to think (critical discernment, not just what to think, and the scientific method) through their educational process is important, as this begins to challenge belief-dependent realism.
Thus, it is important at this point that vaccine educators stop continuing to pursue only the well-worn and generally low-yield routes that we have pursued in the past regarding HCP knowledge, attitudes, and beliefs about vaccines (primarily utilizing the analytical style and relying on data). In an article written by one of the authors (CMP), the authors explored cognitive styles from another angle, focusing on the influences in others’ lives (often under the “bandwagoning” style where an individual is influenced by what others are thinking, saying, and doing). We believe this concept should also be taken in vaccination education efforts directed at HCPs. Likewise, instead of continuing to give information and data to patients when they reject previously given data, HCPs would be best served by “getting above the scene” to get a wider picture of the patient, their fears, where they are getting information they trust, and what their preferred cognitive style is. By doing this, HCPs are better able to develop a respectful and trusting relationship with their patient.
The empathy tool
In a prior publication, one of us (CMP), outlined the use of a unique empathy tool, geared at helping HCPs explore influences on health-decision making. The empathy tool can be utilized by the HCP to better understand an individual’s influences on their behavior (i.e. doctor, religious institution/pastor, friends, a blogger), and how these influences impact their decision-making. This tool also helps the HCP to explore an individual’s values, concerns, and motivations within the decision-making process. Underlying the creation of the empathy tool is human centered design, which aims to address a particular need through a systems-based approach [76]. Human centered design takes a “listening to understand” approach to a problem (in this case, vaccine hesitancy), and looks systemically at the problem, taking the systems that an individual is a part of into account while creating tools and communicating with that individual. To that end, the empathy tool was developed with a variety of different individual contexts and systems in mind.
Conversely, the empathy tool can also be applied to the exploration of the influences on HCP’s beliefs and decision-making in regard to vaccines, as HCPs have the opportunity to explore who or what influences them, how strongly that influence is, and how they feel about this influence on their life. The HCP would then have the opportunity to overlap these influences with their reported values and engage in decision-making conversations from this point. Overlapping the Empathy Tool with the PCSDM model allows for robust conversations about beliefs surrounding vaccine acceptance and hesitancy, as well as engaging in decision-making conversations in a manner and strategy that the HCP most resonates with and understands.
The empathy tool and PCSDM model can be utilized in tandem to heighten a HCPs understanding of how their patient thinks and feels about vaccines, as well as how best to process health information. This can lead to further trust within the patient-provider relationship. An example of these being used together might be utilizing the empathy tool in conversation with a patient (having them identify their values, fears, motivations, and concerns, as well as to identify who their primary influencers are, as identified by the empathy tool). Throughout this conversation, the HCP can be listening for particular statements that identify the preferred cognitive style utilized by the patient as identified in the PCSDM table, allowing the HCP to more quickly identify primary and secondary cognitive styles. Using this understanding that the HCP has gathered regarding the cognitive styles utilized by their patient, the HCP can have a more robust conversation about patient concerns, fears, and values regarding health and vaccine decisions through the lens and cognitive style that the patient most prefers and understands. Thus, the empathy tool and PCSDM model functions as a feedback loop for one another and helps to inform the HCP how to best address patient concerns and fears surrounding vaccination.
It should be noted that a number of different strategies of patient-provider communication have been devised, applied, and studied both historically and currently. Several of these, such as motivational interviewing, presumptive communication, gain vs loss-based framing, the Health Belief Model and others have been used to promote vaccination through effective communication [77], [78], [79], [80], [81], [82], [83] While the review of these strategies and their utility is beyond the scope of this manuscript, different combinations of these strategies can potentially be applied in conjunction with PCSDM and the empathy tool both for HCP vaccine education or to provider-patient vaccine conversations to optimize the efforts directed at increasing vaccine confidence.
Recommendations
We must begin with agreement that vaccines are critically important factors in preventing vaccine-preventable illness, disability, and death. Further, HCPs have a moral duty to be vaccinated in order to not transmit vaccine-preventable diseases to their highly vulnerable patients. Additionally, we must acknowledge the critical role that HCPs play in vaccine acceptance and coverage in the population. To this end, we propose a number of recommendations in moving forward with the important task of increasing vaccine acceptance across the health care profession from an integrative approach. These approaches layer together an understanding of how individuals think and process information (cognitive styles), the influences and values held by the individual, and the systems that one may have been raised and educated in throughout their lives. Creativity will be needed to move beyond the way that things have been done in the past (primarily continuing to utilize the analytical approach of data and facts), and instead developing new innovative ways of communicating these facts within approaches that address how the individual best takes in and processes information. In this regard, we suggest the following:
First, vaccine education needs to be interwoven into the educational programming that students receive while in pre-college, undergraduate, graduate, and health professions schools. By incorporating education that teaches a variety of cognitive styles, HCP students may receive information in the style that they most easily process. By teaching the PCSDM model in educational programs, HCPs will not only learn more about their own style of decision-making and information-processing, but will also learn the key skill of how to best meet the educational needs of their patient. Teaching and using the empathy tool can also aid HCPs in not only understanding themselves better, but it also serves to give them a better way of understanding their patients, emphasizing that these are not “one and done” conversations, but instead the start of a journey. Hospitals and medical settings would best be served by continuing to integrate a variety of such models into continuing education, training sessions, or Grand Rounds in order to reinforce these skills, and to continue to challenge HCPs. Vaccine education should be made a priority in HCP education, continuing education, and in licensure examination. As this should be a long-term, continuous effort, a potential limitation in implementation is the time that it takes to train health care students and HCPs.
Second, there needs to be intentional, proactive work to increase health literacy by incorporating programming into middle and high school education, prior to exposure to anti-vaccinationist misinformation and rhetoric. Health literacy is defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information needed to make appropriate health decisions” [84]. It’s important to note that health literacy does not simply encompass an individual’s access or ability to understand health-related information, but also their ability to then utilize this information in decision-making. Health care providers are subject to biases in health decision-making in similar ways to the general population as a whole. A protective buffer to these biases and errors in decision-making involves training in how to separate their scientific knowledge from cognitive biases, being equipped to identify their own biases, as well as to also be educated in such a way as to increase their own health literacy. Increasing health literacy at an early age (thus impacting the individual throughout the lifespan) is an important part of increasing vaccine acceptance across the population, including increasing vaccine rates amongst HCPs. We also believe that the implementation of teaching basic principles of discernment, the scientific method, and fact-checking is crucial at all levels of education. Examples of this include building skills necessary to differentiate between trusted and untrustworthy sources of information and between misinformation and evidence-based science. It is critical that students learn to distinguish credible sources from self-announced experts, as well as be able to identify and counter propaganda. This approach involves starting at the very root to address the concern. By increasing health literacy, a domino effect will follow health care professionals into their continuing education, personal decisions regarding their health, and their engagement in the health profession as a whole.
Third, research funding needs to be devoted to further development and testing of new and existing models, as well as integration of the models currently available. This includes evaluating the usage of both the PCSDM and Empathy Tool across a variety of populations and settings. The authors suggest a call for funding of practical clinical studies demonstrating the utility and outcomes across a variety of settings and medical subspecialties using these tools.
Fourth, it is important for vaccine requirements for HCPs to be designed and implemented. This could include differential reimbursement rates for health care institutions based on vaccination coverage rates in staff. Measuring metrics relevant to vaccine rates among HCP job categories would allow for transparency, with reporting of those rates publicly. Designing vaccine requirements, and measuring metrics of implementation and success, will further inform improved models of compliance. Additionally, such requirements will drive innovations in vaccine education.
Conclusions
Despite many programs and much effort over the last decades, vaccine hesitancy and low immunization rates among healthcare personnel worldwide remain alarming, threatening the health of both caregivers and care recipients, especially in the context of the COVID-19 pandemic. Moreover, health care providers’ attitude toward vaccination directly affects public opinion and thus, impacts the success of mass immunization efforts vital for defeating this pandemic. Approvals by regulating authorities and implementation of staff vaccine mandates is likely to improve vaccination rates among HCPs. However, care must be taken to not further aggravate mistrust in already vaccine hesitant individuals or to deepen the existing problem of staff shortages across healthcare settings if providers choose to opt out, posing an even greater risk to strained health systems. Thus, while acknowledging the importance and necessity of strict vaccination policies and proactive fact-based educational activities for healthcare personnel, we believe that synergistic implementation of individualized approaches including the PCSDM is crucial for decreasing vaccine hesitancy among HCPs.
Data statement
This article does not include raw data that has been generated or analyzed, and thus does not apply to this article.
CRediT authorship contribution statement
Caroline M. Poland: Conceptualization, Writing – original draft, Writing – review & editing. Tamar Ratishvili: Conceptualization, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Caroline Poland provides consultative advice to Sanofi Pasteur. Tamar Ratishvili is the president of a Georgian non-governmental organization Association of Immunization and Vaccinology. The association currently conducts a UNICEF-funded project Young Doctors Against the Pandemic of which TR is a consultant.
References
- 1.Grochowska M, Ratajczak A, Zdunek G, Adamiec A, Waszkiewicz P, Feleszko W. A Comparison of the Level of Acceptance and Hesitancy towards the Influenza Vaccine and the Forthcoming COVID-19 Vaccine in the Medical Community. Vaccines (Basel). 2021;9(5). Epub 2021/06/03. 10.3390/vaccines9050475. PubMed PMID: 34066790; PubMed Central PMCID: PMCPMC8150871. [DOI] [PMC free article] [PubMed]
- 2.Karafillakis E., Dinca I., Apfel F., Cecconi S., Wűrz A., Takacs J., et al. Vaccine hesitancy among healthcare workers in Europe: A qualitative study. Vaccine. 2016;34(41):5013–5020. doi: 10.1016/j.vaccine.2016.08.029. [DOI] [PubMed] [Google Scholar]
- 3.Lin C, Mullen J, Smith D, Kotarba M, Kaplan SJ, Tu P. Healthcare Providers' Vaccine Perceptions, Hesitancy, and Recommendation to Patients: A Systematic Review. Vaccines (Basel). 2021;9(7). Epub 2021/08/07. 10.3390/vaccines9070713. PubMed PMID: 34358132; PubMed Central PMCID: PMCPMC8310254. [DOI] [PMC free article] [PubMed]
- 4.MacDonald N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 5.Haviari S., Bénet T., Saadatian-Elahi M., André P., Loulergue P., Vanhems P. Vaccination of healthcare workers: A review. Hum Vacc Immunotherap. 2015;11(11):2522–2537. doi: 10.1080/21645515.2015.1082014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paterson P., Meurice F., Stanberry L.R., Glismann S., Rosenthal S.L., Larson H.J. Vaccine hesitancy and healthcare providers. Vaccine. 2016;34(52):6700–6706. doi: 10.1016/j.vaccine.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 7.Khubchandani J., Sharma S., Price J.H., Wiblishauser M.J., Sharma M., Webb F.J. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J Community Health. 2021;46(2):270–277. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Albuquerque Veloso Machado M, Roberts B, Wong BLH, van Kessel R, Mossialos E. The Relationship Between the COVID-19 Pandemic and Vaccine Hesitancy: A Scoping Review of Literature Until August 2021. Front Public Health. 2021;9:747787. Epub 2021/10/16. 10.3389/fpubh.2021.747787. PubMed PMID: 34650953; PubMed Central PMCID: PMCPMC8505886. [DOI] [PMC free article] [PubMed]
- 9.Lindholt M.F., Jørgensen F., Bor A., Petersen M.B. Public acceptance of COVID-19 vaccines: cross-national evidence on levels and individual-level predictors using observational data. BMJ Open. 2021;11(6):e048172. doi: 10.1136/bmjopen-2020-048172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Richterman A, Meyerowitz EA, Cevik M. Indirect Protection by Reducing Transmission: Ending the Pandemic With Severe Acute Respiratory Syndrome Coronavirus 2 Vaccination. Open Forum Infect Dis. 2022;9(2):ofab259. Epub 2022/01/25. 10.1093/ofid/ofab259. PubMed PMID: 35071679; PubMed Central PMCID: PMCPMC8194790. [DOI] [PMC free article] [PubMed]
- 11.Doroshenko A. The Combined Effect of Vaccination and Nonpharmaceutical Public Health Interventions—Ending the COVID-19 Pandemic. JAMA Netw Open. 2021;4(6):e2111675. doi: 10.1001/jamanetworkopen.2021.11675. [DOI] [PubMed] [Google Scholar]
- 12.Solis Arce JS, Warren SS, Meriggi NF, Scacco A, McMurry N, Voors M, et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med. 2021;27(8):1385-94. Epub 2021/07/18. 10.1038/s41591-021-01454-y. PubMed PMID: 34272499; PubMed Central PMCID: PMCPMC8363502. [DOI] [PMC free article] [PubMed]
- 13.Poland C.M., Poland G.A. Vaccine education spectrum disorder: the importance of incorporating psychological and cognitive models into vaccine education. Vaccine. 2011;29(37):6145–6148. doi: 10.1016/j.vaccine.2011.07.131. [DOI] [PubMed] [Google Scholar]
- 14.Poland C.M., Matthews A.K.S., Poland G.A. Improving COVID-19 vaccine acceptance: Including insights from human decision-making under conditions of uncertainty and human-centered design. Vaccine. 2021;39(11):1547–1550. doi: 10.1016/j.vaccine.2021.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.CDC. October 2020 [Google Scholar]
- 16.CDC. Influenza Vaccination Coverage Among Health Care Personnel - United States, 2019-20 Influenza Season | Atlanta, GA: US Department of Health and Human Services, CDC; 2021 [10/22/2021]. Available from: https://www.cdc.gov/flu/fluvaxview/hcp-coverage_1920estimates.htm.
- 17.Black C.L., Yue X., Ball S.W., Fink R.V., de Perio M.A., Laney A.S., et al. Influenza Vaccination Coverage Among Health Care Personnel — United States, 2017–18 Influenza Season. MMWR Morb Mortal Wkly Rep. 2018;67(38):1050–1054. doi: 10.15585/mmwr.mm6738a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Poland G., Tosh P., Jacobson R. Requiring influenza vaccination for health care workers: seven truths we must accept. Vaccine. 2005;23(17-18):2251–2255. doi: 10.1016/j.vaccine.2005.01.043. [DOI] [PubMed] [Google Scholar]
- 19.Influenza vaccination coverage among health-care personnel --- United States, 2010-11 influenza season. MMWR Morb Mortal Wkly Rep. 2011;60(32):1073-7. Epub 2011/08/19. PubMed PMID: 21849963. [PubMed]
- 20.Orenstein W.A., Gellin B.G., Buck T., Jackson L.A., LaRussa P.S., Mason J.O., et al. Strategies to Achieve the Healthy People 2020 Annual Influenza Vaccine Coverage Goal for Health-Care Personnel: Recommendations from the National Vaccine Advisory Committee. Public Health Rep. 2013;128(1):7–25. [PMC free article] [PubMed] [Google Scholar]
- 21.Control ECfDPa. Seasonal influenza vaccination and antiviral use in EU/EEA Member States. Stockholm: ECDC: 2018.
- 22.Dini G., Toletone A., Sticchi L., Orsi A., Bragazzi N.L., Durando P. Influenza vaccination in healthcare workers: A comprehensive critical appraisal of the literature. Human Vacc Immunotherap. 2018;14(3):772–789. doi: 10.1080/21645515.2017.1348442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.England PH. Seasonal influenza vaccine uptake in healthcare workers (HCWs) in England: winter season 2020 to 2021. 2021.
- 24.Maltezou H.C., Theodoridou K., Poland G. Influenza immunization and COVID-19. Vaccine. 2020;38(39):6078–6079. doi: 10.1016/j.vaccine.2020.07.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shaw J, Stewart T, Anderson KB, Hanley S, Thomas SJ, Salmon DA, et al. Assessment of US Healthcare Personnel Attitudes Towards Coronavirus Disease 2019 (COVID-19) Vaccination in a Large University Healthcare System. Clin Infect Dis. 2021;73(10):1776-83. Epub 2021/01/26. 10.1093/cid/ciab054. PubMed PMID: 33491049; PubMed Central PMCID: PMCPMC7929026. [DOI] [PMC free article] [PubMed]
- 26.Lazer D QH, Ognyanova K, Baum M, Perlis RH, Druckman J, Uslu A, Lin J, Santillana M, Green J, Simonson MD. The COVID States Project #62: COVID-19 vaccine attitudes among healthcare workers. 2021 08/18. Report No.
- 27.Reses H.E., Jones E.S., Richardson D.B., Cate K.M., Walker D.W., Shapiro C.N. COVID-19 vaccination coverage among hospital-based healthcare personnel reported through the Department of Health and Human Services Unified Hospital Data Surveillance System, United States, January 20, 2021-September 15, 2021. Am J Infect Control. 2021;49(12):1554–1557. doi: 10.1016/j.ajic.2021.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Green-McKenzie J., Shofer F.S., Momplaisir F., Kuter B.J., Kruse G., Bilal U., et al. Factors Associated With COVID-19 Vaccine Receipt by Health Care Personnel at a Major Academic Hospital During the First Months of Vaccine Availability. JAMA Netw Open. 2021;4(12):e2136582. doi: 10.1001/jamanetworkopen.2021.36582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Woolf K., McManus I.C., Martin C.A., Nellums L.B., Guyatt A.L., Melbourne C., et al. Ethnic differences in SARS-CoV-2 vaccine hesitancy in United Kingdom healthcare workers: Results from the UK-REACH prospective nationwide cohort study. Lancet Reg Health - Europe. 2021;9:100180. doi: 10.1016/j.lanepe.2021.100180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Holt E. COVID-19 vaccination in Ukraine. Lancet Infect Dis. 2021;21(4):462. Epub 2021/03/28. 10.1016/S1473-3099(21)00156-0. PubMed PMID: 33773128; PubMed Central PMCID: PMCPMC7990473. [DOI] [PMC free article] [PubMed]
- 31.Rosental H, Shmueli L. Integrating Health Behavior Theories to Predict COVID-19 Vaccine Acceptance: Differences between Medical Students and Nursing Students. Vaccines (Basel). 2021;9(7). Epub 2021/08/07. 10.3390/vaccines9070783. PubMed PMID: 34358199; PubMed Central PMCID: PMCPMC8310115. [DOI] [PMC free article] [PubMed]
- 32.Rong H, Lai X, Ma X, Hou Z, Li S, Jing R, et al. Seasonal Influenza Vaccination and Recommendation: The Difference between General Practitioners and Public Health Workers in China. Vaccines (Basel). 2020;8(2). Epub 2020/06/04. 10.3390/vaccines8020265. PubMed PMID: 32486350; PubMed Central PMCID: PMCPMC7350002. [DOI] [PMC free article] [PubMed]
- 33.Awaidy STA, Z KAM, Kaddoura M, Mahomed O, Lahoud N, Abubakar A, et al. Influenza Vaccination Hesitancy among Healthcare Workers in South Al Batinah Governorate in Oman: A Cross-Sectional Study. Vaccines (Basel). 2020;8(4). Epub 2020/11/12. 10.3390/vaccines8040661. PubMed PMID: 33172064; PubMed Central PMCID: PMCPMC7712351. [DOI] [PMC free article] [PubMed]
- 34.Paris C., Bénézit F., Geslin M., Polard E., Baldeyrou M., Turmel V., et al. COVID-19 vaccine hesitancy among healthcare workers. Infectious Diseases Now. 2021;51(5):484–487. doi: 10.1016/j.idnow.2021.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.KFF. KFF/The Washington Post frontline health care workers survey. 2021 April 6, 2021. Report No.
- 36.Dror A.A., Eisenbach N., Taiber S., Morozov N.G., Mizrachi M., Zigron A., et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.AMA. Physician COVID-19 Vaccination Study (Final Report). 2021.
- 38.Lee J.T., Althomsons S.P., Wu H., Budnitz D.S., Kalayil E.J., Lindley M.C., et al. Disparities in COVID-19 Vaccination Coverage Among Health Care Personnel Working in Long-Term Care Facilities, by Job Category, National Healthcare Safety Network — United States, March 2021. MMWR Morb Mortal Wkly Rep. 2021;70(30):1036–1039. doi: 10.15585/mmwr.mm7030a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gilboa M, Tal I, Levin EG, Segal S, Belkin A, Zilberman-Daniels T, et al. Coronavirus disease 2019 (COVID-19) vaccination uptake among healthcare workers. Infect Control Hosp Epidemiol. 2021:1-6. Epub 2021/09/24. 10.1017/ice.2021.421. PubMed PMID: 34551833; PubMed Central PMCID: PMCPMC8503070. [DOI] [PMC free article] [PubMed]
- 40.Browne SK, Feemster KA, Shen AK, Green-McKenzie J, Momplaisir FM, Faig W, et al. Coronavirus disease 2019 (COVID-19) vaccine hesitancy among physicians, physician assistants, nurse practitioners, and nurses in two academic hospitals in Philadelphia. Infect Control Hosp Epidemiol. 2021:1-9. Epub 2021/09/21. 10.1017/ice.2021.410. PubMed PMID: 34538290; PubMed Central PMCID: PMCPMC8503076. [DOI] [PMC free article] [PubMed]
- 41.Group TC. Vaccine Hesitancy Among Rural Hospitals. 2021.
- 42.Luo C., Yang Y., Liu Y., Zheng D., Shao L., Jin J., et al. Intention to COVID-19 vaccination and associated factors among health care workers: A systematic review and meta-analysis of cross-sectional studies. Am J Infect Control. 2021;49(10):1295–1304. doi: 10.1016/j.ajic.2021.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Biswas N, Mustapha T, Khubchandani J, Price JH. The Nature and Extent of COVID-19 Vaccination Hesitancy in Healthcare Workers. J Community Health. 2021. Epub 2021/04/21. 10.1007/s10900-021-00984-3. PubMed PMID: 33877534; PubMed Central PMCID: PMCPMC8056370. [DOI] [PMC free article] [PubMed]
- 44.D. H. The 2009 influenza pandemic—an independent review of the UK response to the 2009 influenza pandemic. Cabinet Office, London: 2010.
- 45.Rachiotis G., Mouchtouri V.A., Kremastinou J., Gourgoulianis K., Hadjichristodoulou C. Low acceptance of vaccination against the 2009 pandemic influenza A(H1N1) among healthcare workers in Greece. Euro Surveill. 2010;15(6) Epub 2010/02/18. PubMed PMID: 20158980. [PubMed] [Google Scholar]
- 46.Shekhar R, Sheikh AB, Upadhyay S, Singh M, Kottewar S, Mir H, et al. COVID-19 Vaccine Acceptance among Health Care Workers in the United States. Vaccines (Basel). 2021;9(2). Epub 2021/02/07. 10.3390/vaccines9020119. PubMed PMID: 33546165; PubMed Central PMCID: PMCPMC7913135. [DOI] [PMC free article] [PubMed]
- 47.Baniak LM, Luyster FS, Raible CA, McCray EE, Strollo PJ. COVID-19 Vaccine Hesitancy and Uptake among Nursing Staff during an Active Vaccine Rollout. Vaccines (Basel). 2021;9(8). Epub 2021/08/29. 10.3390/vaccines9080858. PubMed PMID: 34451983; PubMed Central PMCID: PMCPMC8402347. [DOI] [PMC free article] [PubMed]
- 48.Scardina G, Ceccarelli L, Casigliani V, Mazzilli S, Napoletano M, Padovan M, et al. Evaluation of Flu Vaccination Coverage among Healthcare Workers during a 3 Years' Study Period and Attitude towards Influenza and Potential COVID-19 Vaccination in the Context of the Pandemic. Vaccines (Basel). 2021;9(7). Epub 2021/08/07. 10.3390/vaccines9070769. PubMed PMID: 34358185; PubMed Central PMCID: PMCPMC8310181. [DOI] [PMC free article] [PubMed]
- 49.Verger P., Fressard L., Collange F., Gautier A., Jestin C., Launay O., et al. Vaccine Hesitancy Among General Practitioners and Its Determinants During Controversies: A National Cross-sectional Survey in France. EBioMedicine. 2015;2(8):891–897. doi: 10.1016/j.ebiom.2015.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bish A., Yardley L., Nicoll A., Michie S. Factors associated with uptake of vaccination against pandemic influenza: A systematic review. Vaccine. 2011;29(38):6472–6484. doi: 10.1016/j.vaccine.2011.06.107. [DOI] [PubMed] [Google Scholar]
- 51.Marcu A., Rubinstein H., Michie S., Yardley L. Accounting for personal and professional choices for pandemic influenza vaccination amongst English healthcare workers. Vaccine. 2015;33(19):2267–2272. doi: 10.1016/j.vaccine.2015.03.028. [DOI] [PubMed] [Google Scholar]
- 52.Parry H.M., Damery S., Fergusson A., Draper H., Bion J., Low A.E. Pandemic influenza A (H1N1) 2009 in a critical care and theatre setting: beliefs and attitudes towards staff vaccination. J Hosp Infect. 2011;78(4):302–307. doi: 10.1016/j.jhin.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 53.Torun S.D., Torun F. Vaccination against pandemic influenza A/H1N1 among healthcare workers and reasons for refusing vaccination in Istanbul in last pandemic alert phase. Vaccine. 2010;28(35):5703–5710. doi: 10.1016/j.vaccine.2010.06.049. [DOI] [PubMed] [Google Scholar]
- 54.Zhang J., While A.E., Norman I.J. Nurses’ knowledge and risk perception towards seasonal influenza and vaccination and their vaccination behaviours: A cross-sectional survey. Int J Nurs Stud. 2011;48(10):1281–1289. doi: 10.1016/j.ijnurstu.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 55.Kuter B.J., Browne S., Momplaisir F.M., Feemster K.A., Shen A.K., Green-McKenzie J., et al. Perspectives on the receipt of a COVID-19 vaccine: A survey of employees in two large hospitals in Philadelphia. Vaccine. 2021;39(12):1693–1700. doi: 10.1016/j.vaccine.2021.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bonaccorsi G., Lorini C., Santomauro F., Guarducci S., Pellegrino E., Puggelli F., et al. Predictive factors associated with the acceptance of pandemic and seasonal influenza vaccination in health care workers and students in Tuscany, Central Italy. vaccines. 2013;9(12):2603–2612. doi: 10.4161/hv.26036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Alame M, Kaddoura M, Kharroubi S, Ezzeddine F, Hassan G, Diab El-Harakeh M, et al. Uptake rates, knowledge, attitudes, and practices toward seasonal influenza vaccination among healthcare workers in Lebanon. Hum Vaccin Immunother. 2021:1-9. Epub 2021/07/23. 10.1080/21645515.2021.1948783. PubMed PMID: 34292126. [DOI] [PMC free article] [PubMed]
- 58.Gadoth A., Halbrook M., Martin-Blais R., Gray A., Tobin N.H., Ferbas K.G., et al. Cross-sectional Assessment of COVID-19 Vaccine Acceptance Among Health Care Workers in Los Angeles. Ann Intern Med. 2021;174(6):882–885. doi: 10.7326/M20-7580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kaplan R.M., Milstein A. Influence of a COVID-19 vaccine’s effectiveness and safety profile on vaccination acceptance. Proc Natl Acad Sci USA. 2021;118(10) doi: 10.1073/pnas.2021726118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mitchell G, Leonard L, Carter G, Santin O, Brown Wilson C. Evaluation of a 'serious game' on nursing student knowledge and uptake of influenza vaccination. PLoS One. 2021;16(1):e0245389. Epub 2021/01/15. 10.1371/journal.pone.0245389. PubMed PMID: 33444348; PubMed Central PMCID: PMCPMC7808644. [DOI] [PMC free article] [PubMed]
- 61.Berry S.D., Goldfeld K.S., McConeghy K., Gifford D., Davidson H.E., Han L., et al. Evaluating the Findings of the IMPACT-C Randomized Clinical Trial to Improve COVID-19 Vaccine Coverage in Skilled Nursing Facilities. JAMA Intern Med. 2022;182(3):324. doi: 10.1001/jamainternmed.2021.8067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Honda H., Sato Y., Yamazaki A., Padival S., Kumagai A., Babcock H. A Successful Strategy for Increasing the Influenza Vaccination Rate of Healthcare Workers without a Mandatory Policy Outside of the United States: A Multifaceted Intervention in a Japanese Tertiary Care Center. Infect Control Hosp Epidemiol. 2013;34(11):1194–1200. doi: 10.1086/673452. [DOI] [PubMed] [Google Scholar]
- 63.Barbara A, La Milia DI, Di Pumpo M, Tognetto A, Tamburrano A, Vallone D, et al. Strategies to Increase Flu Vaccination Coverage among Healthcare Workers: A 4 Years Study in a Large Italian Teaching Hospital. Vaccines (Basel). 2020;8(1). Epub 2020/02/20. 10.3390/vaccines8010085. PubMed PMID: 32069869; PubMed Central PMCID: PMCPMC7157643. [DOI] [PMC free article] [PubMed]
- 64.Dempsey RC, McAlaney J, Bewick BM. A Critical Appraisal of the Social Norms Approach as an Interventional Strategy for Health-Related Behavior and Attitude Change. Front Psychol. 2018;9:2180. Epub 2018/11/22. 10.3389/fpsyg.2018.02180. PubMed PMID: 30459694; PubMed Central PMCID: PMCPMC6232455. [DOI] [PMC free article] [PubMed]
- 65.Hollmeyer H, Hayden F, Mounts A, Buchholz U. Review: interventions to increase influenza vaccination among healthcare workers in hospitals. Influenza Other Respir Viruses. 2013;7(4):604-21. Epub 2012/09/19. 10.1111/irv.12002. PubMed PMID: 22984794; PubMed Central PMCID: PMCPMC5781006. [DOI] [PMC free article] [PubMed]
- 66.Saunier F., Berthelot P., Mottet-Auselo B., Pelissier C., Fontana L., Botelho-Nevers E., et al. Impact of a decision-aid tool on influenza vaccine coverage among HCW in two French hospitals: A cluster-randomized trial. Vaccine. 2020;38(36):5759–5763. doi: 10.1016/j.vaccine.2020.07.011. [DOI] [PubMed] [Google Scholar]
- 67.Campos-Mercade P, Meier AN, Schneider FH, Meier S, Pope D, Wengstrom E. Monetary incentives increase COVID-19 vaccinations. Science. 2021;374(6569):879-82. Epub 2021/10/08. 10.1126/science.abm0475. PubMed PMID: 34618594. [DOI] [PMC free article] [PubMed]
- 68.Mills M.C., Rüttenauer T. The effect of mandatory COVID-19 certificates on vaccine uptake: synthetic-control modelling of six countries. The Lancet Public Health. 2022;7(1):e15–e22. doi: 10.1016/S2468-2667(21)00273-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rashid H., Yin J.K., Ward K., King C., Seale H., Booy R. Assessing Interventions To Improve Influenza Vaccine Uptake Among Health Care Workers. Health Aff. 2016;35(2):284–292. doi: 10.1377/hlthaff.2015.1087. [DOI] [PubMed] [Google Scholar]
- 70.Ozisik L., Tanriover M.D., Altınel S., Unal S. Vaccinating healthcare workers: Level of implementation, barriers and proposal for evidence-based policies in Turkey. Human Vacc Immunotherap. 2017;13(5):1198–1206. doi: 10.1080/21645515.2016.1269992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Schumacher S., Salmanton-García J., Cornely O.A., Mellinghoff S.C. Increasing influenza vaccination coverage in healthcare workers: a review on campaign strategies and their effect. Infection. 2021;49(3):387–399. doi: 10.1007/s15010-020-01555-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.LaVela S.L., Smith B., Weaver F.M., Legro M.W., Goldstein B., Nichol K. Attitudes and Practices Regarding Influenza Vaccination Among Healthcare Workers Providing Services to Individuals With Spinal Cord Injuries and Disorders. Infect Control Hosp Epidemiol. 2004;25(11):933–940. doi: 10.1086/502323. [DOI] [PubMed] [Google Scholar]
- 73.Zhang J., While A.E., Norman I.J. Nurses’ vaccination against pandemic H1N1 influenza and their knowledge and other factors. Vaccine. 2012;30(32):4813–4819. doi: 10.1016/j.vaccine.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 74.Whitaker J.A., Poland C.M., Beckman T.J., Bundrick J.B., Chaudhry R., Grill D.E., et al. Immunization education for internal medicine residents: A cluster-randomized controlled trial. Vaccine. 2018;36(14):1823–1829. doi: 10.1016/j.vaccine.2018.02.082. [DOI] [PubMed] [Google Scholar]
- 75.Shermer M. The Believing Brain: From Ghosts and Gods to Politics and Conspiracies-How We Construct Beliefs and Reinforce Them As Truths: St. Martin's Griffin; 2011.
- 76.Melles M, Albayrak A, Goossens R. Innovating health care: key characteristics of human-centered design. Int J Qual Health Care. 2021;33(Supplement_1):37-44. Epub 2020/10/18. 10.1093/intqhc/mzaa127. PubMed PMID: 33068104; PubMed Central PMCID: PMCPMC7802070. [DOI] [PMC free article] [PubMed]
- 77.Godin G., Vézina-Im L.-A., Naccache H. Determinants of Influenza Vaccination among Healthcare Workers. Infect Control Hosp Epidemiol. 2010;31(7):689–693. doi: 10.1086/653614. [DOI] [PubMed] [Google Scholar]
- 78.Yu Y., Lau J.T.F., She R., Chen X.i., Li L., Li L., et al. Prevalence and associated factors of intention of COVID-19 vaccination among healthcare workers in China: application of the Health Belief Model. Hum Vacc Immunotherap. 2021;17(9):2894–2902. doi: 10.1080/21645515.2021.1909327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Opel D.J., Omer S.B. Measles, Mandates, and Making Vaccination the Default Option. JAMA Pediatr. 2015;169(4):303. doi: 10.1001/jamapediatrics.2015.0291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jacobson R.M., St. Sauver J.L., Griffin J.M., MacLaughlin K.L., Finney Rutten L.J. How health care providers should address vaccine hesitancy in the clinical setting: Evidence for presumptive language in making a strong recommendation. Human Vacc Immunotherap. 2020;16(9):2131–2135. doi: 10.1080/21645515.2020.1735226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Omer S.B.P.C., Chamberlain A.C. Elsevier; Louis, Missouri: 2019. Interpersonal Communication Approaches to Increase Adult Vaccine Acceptance' in Poland GA and Whitaker JA (ed): St. [Google Scholar]
- 82.Motta M., Sylvester S., Callaghan T., Lunz-Trujillo K. Encouraging COVID-19 vaccine uptake through effective health communication. Frontiers. Political Sci. 2021;3 doi: 10.3389/fpos.2021.630133. [DOI] [Google Scholar]
- 83.Karras J., Dubé E., Danchin M., Kaufman J., Seale H. A scoping review examining the availability of dialogue-based resources to support healthcare providers engagement with vaccine hesitant individuals. Vaccine. 2019;37(44):6594–6600. doi: 10.1016/j.vaccine.2019.09.039. [DOI] [PubMed] [Google Scholar]
- 84.Equity HRSAOoH. Health Literacy [May 6, 2022]. Available from: https://www.hrsa.gov/about/organization/bureaus/ohe/health-literacy/index.html.