Abstract
Background
Depression is a common mental disorder in family practice with an impact on global health. The aim of this study is to provide insight in the trends of epidemiological measures as well as pharmacological treatments and comorbidities of depression.
Methods
A study using data from INTEGO, a family practice registration network in Flanders, Belgium. Trends in age-standardized prevalence and incidence of depression from 2000 to 2019 as well as antidepressant prescriptions in prevalent depression cases were analyzed with join point regression. Comorbidity profiles were explored using the Cochran-Armitage test and the Jonckheere-Terpstra test.
Results
We identified 538 299 patients older than 15 years during the study period. We found an increasing trend in the age-standardized prevalence of depression from 6.73 % in 2000 to 9.20 % in 2019. For the incidence of depression, a decreasing trend was observed from 2000 to 2015 with an incidence of 9.42/1000 in 2000 and 6.89/1000 in 2015, followed by an increasing trend from 2015 to 2019 (incidence of 13.64/1000 in 2019). The average number of chronic diseases per patient with depression increased significantly during the study period (from 1.2 to 1.8), and the proportion of patients relative to the whole study population that received at least one antidepressant prescription per year increased between 2000 and 2019 from 26.44% to 40.16%.
Conclusions
The prevalence of depression increases while the incidence sharply rises, but only in recent years. Patients with depression tend to have more comorbidities, making a multi-faceted approach to these patients more important.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12875-022-01769-w.
Keywords: Epidemiology, Depression, Flanders, Belgium
Introduction
Depression is a mental disorder with an important impact on global health [1]. It is the third leading cause of non-fatal health loss according to the World Health Organization (WHO). In 2019, globally more than 279 million people were affected by depression [1]. The 2018 Belgian health survey, using self-reported questionnaire data, showed an estimated prevalence of depression of 9.4% for people aged 15 years and older [2]. According to the Global Burden of Disease Study in 2019 (using Diagnostic and Statistical Manual of Mental Disorders and International Classification of Diseases 10 criteria), depression prevalence in Belgium was 4.36%, comparable with the surrounding countries, with France having the highest prevalence (4.74%) [1]. This contrasts with the global prevalence of depression, which was estimated to be 3.76%. With regard to time trends, the majority of studies reported an increase from the early 2000s till recent years [3–9].
However, there are inconsistencies across age groups. Some studies show increasing trends in prevalence in young adults and no change or even a decline in older adults [4, 7, 8], while others also found an increase in the middle-aged or elderly population [6, 9].
The use of mental health services and the prescription of antidepressants seem to have consistently increased in the last two decades [6, 10–16]. The type of antidepressant prescribed changed, with a decline in the use of tricyclic antidepressants (TCAs) and a rise of selective serotonin and noradrenalin reuptake inhibitors (SNRIs) and selective serotonin reuptake inhibitors (SSRIs) [10, 16].
There is also a rising problem of depression associated with multimorbidity [6, 17–19]. Individuals with depression are more likely than individuals without depression to have comorbid physical conditions [17, 20]. Moreover, depression is two to three times more likely in patients with multimorbidity compared to patients without [18].
While many studies have covered these topics, an analysis of data across age categories in family practice, with its unique patient population, is missing in literature. In order to have an accurate idea of how depression is represented in this context, we focused on tangible data, such as diagnoses made by the physicians or prescriptions given out, something which has already been done before in different settings [21, 22].
In this study we provide a comprehensive overview of the trends in the epidemiology of depression in family practice, its drug treatment and comorbidities in patients with depression between 2000 and 2019 in Flanders, Belgium.
Methods
Study design and data collection
Data for this study were obtained from INTEGO, a Belgian family practice morbidity registration network managed at the Department of General Practice of the University of Leuven [23]. The registry started in 1994 and was founded to inform public health on the incidence and prevalence of disease in family practice.
In 2019, over 300 family physicians (FPs) evenly spread throughout Flanders, Belgium, were participating in the INTEGO project, which now provides data from over 400 000 patients. Family practices apply for inclusion in the registry. Before acceptance of their data, registration performance is audited using algorithms to compare their results with those of all other applicants. Only data from practices with optimal registration performance are included in the database. Additionally, INTEGO data are externally validated by means of national and international comparisons [23]. INTEGO FPs prospectively and routinely register all new diagnoses and new drug prescriptions using computer-generated keywords internally linked to codes.
New data are encrypted and collected from the FPs’ personal computers and entered in a central database on a weekly basis. We excluded data from 2020 as the currently ongoing COVID pandemic might change epidemiologic trends outside the scope of this paper.
New diagnoses are classified according to the International Classification of Primary Care 2 (ICPC-2) and International Statistical Classification of Diseases and Related Health Problems, 10th Revision. Drugs are classified according to the WHO’s Anatomical Therapeutic Chemical (ATC) classification system. The denominator is the yearly contact group (YCG). These are the patients who visit a certain practice at least once in a given year [23, 24]. They have a unique pseudonymized patient ID (based on their national social security number), which remains the same across practices. Data from family practices outside the INTEGO network are not included in the database.
Depression, comorbidities and antidepressive treatment
Patients with depression were identified based on the ICPC-2 coded diagnosis P76 “Depression” in their Electronic Medical Record (EMR). Cases were considered prevalent if a P76 diagnosis was ever registered without considering if the patient had an active depressive episode or whether the patient had been free of depressive episodes for years. In other words, we considered depression as a chronic disease. Patients were no longer considered prevalent if they stopped being included in the YCG (i.e. deceased, moved to practice outside of the INTEGO network). No distinction could be made between mild, moderate and severe depression. Cases were considered incident if a first diagnosis was made the same year.
A disease count was calculated for all incident depression cases for which a list of chronic diseases was used (Table A1, Appendix). For the presence of chronic kidney disease, the glomerular filtration rate was estimated based on the closest creatinine measurement in the 2 years before or after the date of diagnosis of depression.
Medication for patients with depression was recorded for all prevalent cases each year between 2000 and 2019. Medication use in a specific year was considered positive when at least one prescription had been made in that year (Table A2, Appendix).
Data analysis
Prevalence (/100 patients) and incidence (/1000 patients) were calculated for patients with depression by gender.
The rates were age-standardized by taking the Flemish population in Belgium as the standard population (reference year 2000). Age groups were formed starting from 15-29 years, 30-44 years, 45-59 years, 60-74 years, with 75 years and older being the last group for standardization. Additionally, the trend in age-standardized rates between 2000 and 2019 was analyzed. For that purpose, a join point regression analysis was performed [25]. From the join point regression model, the annual percentage change (APC) and the average annual percentage change (AAPC) were extracted. The APC is calculated for each significant trend from a piecewise log-linear model on the logarithm of the age-standardized rate versus the year. The AAPC represents the average of APC estimates per significant trend weighted by the corresponding trend length (number of years in the trend). The points between each trend period are called join points, which represent a significant change in the calculated trend (either upwards or downwards) and can be different across strata. This implies that the number and length of trend periods can vary between strata as well.
The trend analysis using the join point regression model was performed using the SEER*Stat software [Join Point Trend Analysis software from the Surveillance Research Program of the US National Cancer Institute (available at http://surveillance.cancer.gov/joinpoint)]. Trends in comorbidity profiles were explored in incident depression cases with the Cochran-Armitage test and the Jonckheere-Terpstra test over the following intervals: 2000–2003, 2004-2007, 2008-2011, 2012-2016 and 2017-2019. Trends in prescription of antidepressants over the years 2000–2019 were analyzed using a join point regression analysis, as described above. A two-sided P value <0.05 was considered to be statistically significant. These analyses were performed using R Software V.4.8.0.1 (Free Software Foundation, Boston, Massachusetts, USA) (DescTools and clinfun packages).
Results
Trends in age-standardized prevalence and incidence of depression (2000-2019)
There were 538 299 unique patients older than 15 during the study period. The age-standardized prevalence of depression increased over time.
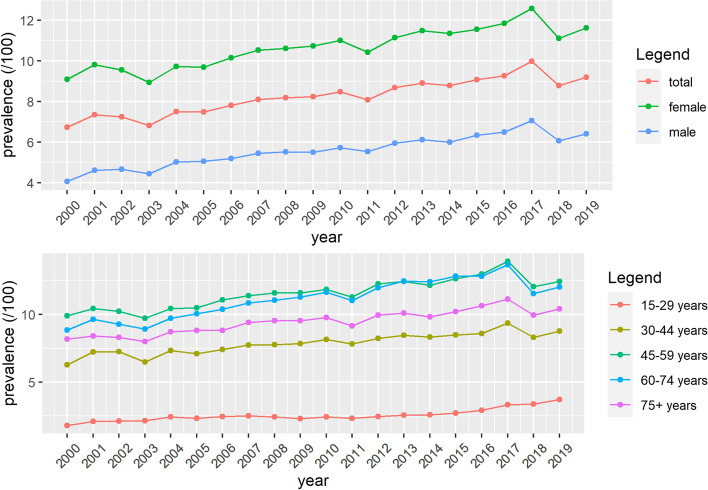
A different trend in women and men was noted. Although women had a higher prevalence of depression during the whole study period, the AAPC for men was higher (Table 1, Fig. 1). The prevalence of depression differed in different age groups. The highest prevalence was found in patients aged 45-59. A significant rise in prevalence was observed in all age groups. The highest AAPC was found in the youngest group, with the steepest rise between 2013-2019 (Table 1, Fig. 1).
Table 1.
Trends in the prevalence and incidence of depression in Flanders, Belgium (2000-2019)
| Summary | Trend 1 | Trend 2 | Trend 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Year 2000 | Year 2019 | AAPC (95% CI) | Years | APC (95% CI) | Years | APC (95% CI) | Years | APC (95% CI) | |
| Prevalence (/100) | |||||||||
| Total | 6.73 | 9.20 | 1.6 (1.2;1.9) | 2000-2019 | 1.6 (1.2;1.9) | ||||
| Women | 9.10 | 11.63 | 1.3 (1.0;1.6) | 2000-2019 | 1.3 (1.0;1.6) | ||||
| Men | 4.05 | 6.40 | 2.0 (1.6;2.5) | 2000-2019 | 2.0 (1.6;2.5) | ||||
| 15-29 | 1.80 | 3.72 | 3.6 (2.7;4.6) | 2000-2004 | 6.4 (2.4;10.7) | 2004-2013 | 0.2 (-0.9;1.3) | 2013-2019 | 7.2 (5.7;8.6) |
| 30-44 | 6.30 | 8.77 | 1.4 (1.1;1.8) | 2000-2019 | 1.4 (1.1;1.8) | ||||
| 45-59 | 9.90 | 12.44 | 1.1 (0.5;1.7) | 2000-2017 | 1.7 (1.4;2.0) | 2017-2019 | -3.8 (-9.3;2.1) | ||
| 60-74 | 8.86 | 12.04 | 1.5 (0.6;2.3) | 2000-2016 | 2.4 (1.9;3.0) | 2016-2019 | -3.6 (-8.3;1.4) | ||
| 75+ | 8.17 | 10.40 | 1.3 (1.0:1.6) | 2000-2019 | 1.3 (1.0:1.6) | ||||
| Incidence (/1000) | |||||||||
| Total | 9.42 | 13.64 | 1.9 (0.4;3.3) | 2000-2015 | -2.3 (-3.3;-1.3) | 2015-2019 | 19.1 (11.8;26.9) | ||
| Women | 11.62 | 16.68 | 1.7 (0.0;3.5) | 2000-2015 | -2.5 (-3.7;-1.2) | 2015-2019 | 19.2 (10.3;28.7) | ||
| Men | 7.14 | 10.27 | 1.6 (0.4;2.9) | 2000-2014 | -2.5 (-3.5;-1.5) | 2014-2019 | 14.2 (9.6;19.0) | ||
| 15-29 | 7.37 | 13.62 | 3.3 (1.1;5.5) | 2000-2015 | -1.0 (-2.5;0.6) | 2015-2019 | 20.9 (10.4;32.4) | ||
| 30-44 | 10.66 | 16.66 | 1.7 (0.0;3.5) | 2000-2015 | -1.8 (-3.0;-0.6) | 2015-2019 | 16.2 (7.8;25.3) | ||
| 45-59 | 11.94 | 14.89 | 1.4 (-0.5;3.3) | 2000-2015 | -2.7 (-3.9;-1.4) | 2015-2019 | 18.1 (8.9;28.1) | ||
| 60-74 | 7.67 | 9.29 | 0.8 (-1.7;3.2) | 2000-2015 | -4.5 (-6.0;-2.9) | 2015-2019 | 23.0 (10.2;37.2) | ||
| 75+ | 7.72 | 9.80 | 1.9 (-1.1;4.9) | 2000-2014 | -3.7 (-6.3;-1.1) | 2014-2019 | 19.5 (8.6;31.6) | ||
Abbreviations: AAPC average annual percent change, APC annual percent change
Fig. 1.
Prevalence of depression in Flanders, Belgium from 2000 to 2019, age-standardized (A) and per age group (B)
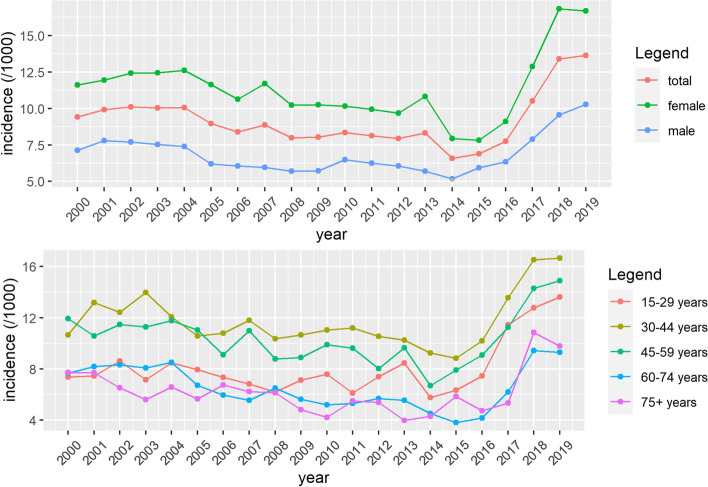
The total incidence of depression decreased from 2000 to 2015, after which a steep increase was noted. The incidence also increased steeply and significantly for all age groups, mostly so in age groups 15-29 and 60-74. (Table 1, Fig. 2) The mean age at depression diagnosis did not change significantly during the study period.
Fig. 2.
Incidence of depression in Flanders, Belgium from 2000 to 2019, age-standardized (A) and per age group (B)
Trends in comorbidities at diagnosis (2000-2019)
The average number of chronic diseases per patient with depression increased significantly over the study period. (Table 2) The leading psychiatric comorbidity was alcohol abuse. In the somatic comorbidities, the strongest rising trend was observed for diabetes mellitus, hypothyroidism, asthma and malignant diseases. The three leading somatic comorbidities for patients with depression in 2017 to 2019 were hypertension, malignancy and asthma, all of which increased significantly during the study period (Table 2).
Table 2.
Trends in comorbidities in patients with depression in Flanders, Belgium (2000-2019)
| Variables | 2000-2003 | 2004-2007 | 2008-2011 | 2012-2016 | 2017-2019 | Trend test | ||
|---|---|---|---|---|---|---|---|---|
| STUDY POPULATION | ||||||||
| Patients with depression (n) | 3268 | 3650 | 3535 | 3545 | 5732 | 0 | ||
| Mean age (standard deviation) | 45.2(17) | 45.4(17.1) | 44.9(17) | 44.3(17.5) | 44.5(18.6) | 1 | ||
| Number of women (%) | 2054(62.9) | 2392(65.5) | 2244(63.5) | 2189(61.7) | 3720(64.9) | 0.6175 | ||
| PREVALENCE OF COMORBIDITIES, n (%) | ICPC code | |||||||
| Mean chronic disease count per patient (SD) | 1.2(1.6) | 1.3(1.8) | 1.5(2) | 1.6(2) | 1.8(2.1) | 0.0002 | ||
| Anxiety disorder | P74 | 15(0.5) | 26(0.7) | 28(0.8) | 31(0.9) | 167(2.9) | <0.0001 | |
| Alcohol abuse | P15-16 | 60(1.8) | 98(2.7) | 98(2.8) | 163(4.6) | 208(3.6) | <0.0001 | |
| Dementia | P70 | 15(0.5) | 15(0.4) | 30(0.8) | 41(1.2) | 63(1.1) | <0.0001 | |
| Schizophrenia | P72 | 13(0.4) | 15(0.4) | 13(0.4) | 16(0.5) | 28(0.5) | 0.4464 | |
| Suicide/suicide attempt | P77 | 3(0.1) | 6(0.2) | 7(0.2) | 9(0.3) | 34(0.6) | <0.0001 | |
| Phobia/compulsive disorder | P79 | 29(0.9) | 25(0.7) | 23(0.7) | 46(1.3) | 76(1.3) | 0.0012 | |
| Personality disorder | P80 | 10(0.3) | 26(0.7) | 30(0.8) | 52(1.5) | 194(3.4) | <0.0001 | |
| Anorexia nervosa/bulimia | P86 | 5(0.2) | 1(0) | 3(0.1) | 5(0.1) | 12(0.2) | 0 | |
| Substance abuse | P18-19 | 7(0.2) | 10(0.3) | 17(0.5) | 16(0.5) | 65(1.1) | <0.0001 | |
| Atrial fibrillation/flutter | K78 | 47(1.4) | 50(1.4) | 54(1.5) | 69(1.9) | 128(2.2) | 0.0004 | |
| Hypertension | K86-87 | 392(12) | 486(13.3) | 492(13.9) | 429(12.1) | 836(14.6) | 0.0074 | |
| Heart failure | K77 | 23(0.7) | 35(1) | 30(0.8) | 32(0.9) | 46(0.8) | 0.8971 | |
| Atherosclerosis | K92 | 59(1.8) | 82(2.2) | 62(1.8) | 61(1.7) | 88(1.5) | 0.0707 | |
| Ischemic heart disease | K74-75-76 | 95(2.9) | 126(3.5) | 98(2.8) | 103(2.9) | 140(2.4) | 0.039 | |
| Diabetes Mellitus | T89-90 | 114(3.5) | 167(4.6) | 231(6.5) | 320(9) | 382(6.7) | <0.0001 | |
| Hypothyroidism | T86 | 50(1.5) | 47(1.3) | 49(1.4) | 57(1.6) | 162(2.8) | <0.0001 | |
| Hyperthyroidism | T85 | 6(0.2) | 12(0.3) | 6(0.2) | 7(0.2) | 31(0.5) | 0.0093 | |
| Irritable bowel syndrome | D01-D93 | 296(9.1) | 363(9.9) | 378(10.7) | 363(10.2) | 549(9.6) | 0.6288 | |
| Asthma | R96 | 194(5.9) | 277(7.6) | 321(9.1) | 348(9.8) | 603(10.5) | <0.0001 | |
| COPD | R95 | 83(2.5) | 110(3) | 104(2.9) | 94(2.7) | 214(3.7) | 0.0055 | |
| Osteoarthritis | L89-90-91 | 314(9.6) | 384(10.5) | 434(12.3) | 356(10) | 528(9.2) | 0.1349 | |
| Cerebrovascular disease | K90-91 | 60(1.8) | 68(1.9) | 72(2) | 78(2.2) | 153(2.7) | 0.0025 | |
| Malignancy | A79-Y78-N74-Y77-U76-T71-D76-D74-U77-U75-D75-R84-B74-S77-R85-D77-X76-W72-X75-X77 | 97(3) | 139(3.8) | 194(5.5) | 259(7.3) | 696(12.1) | <0.0001 | |
| Chronic Kidney Disease | 44(1.3) | 35(1) | 36(1) | 36(1) | 66(1.2) | 0.7067 | ||
Trends in antidepressant prescriptions (2000-2019)
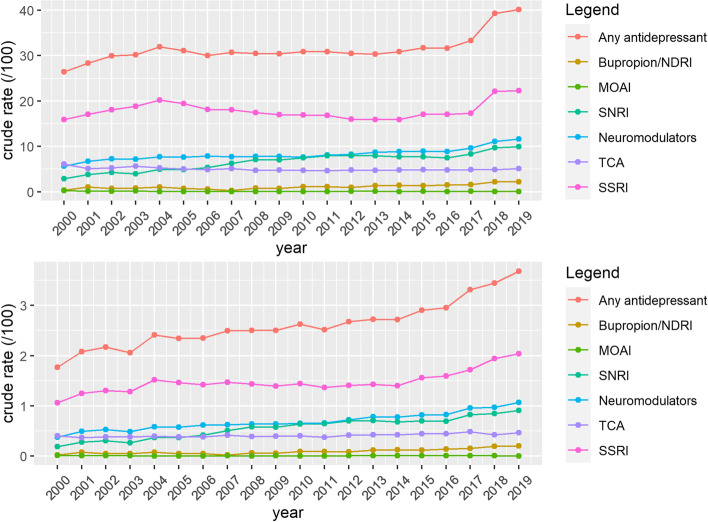
Among prevalent cases with depression, the proportion of patients that received drug treatment increased with one third from 2000 to 2019 (Table 3, Fig. 3). Likewise, the proportion of treated patients who received more than one prescription of an antidepressant per year increased from 63.4% in 2000 to 92.1% in 2019. For the whole population of prevalent cases, the proportion of patients with more than one prescription per year increased from 18% in 2000 to 37% in 2019 (Table 4).
Table 3.
Trends in first-line treatment in patients with depression in Flanders, Belgium (2000-2019)
| SUMMARY | Trend 1 | Trend 2 | Trend 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Medication (%) | Year 2000 | Year 2019 | AAPC (95% CI) | Years | APC (95% CI) | Years | APC (95% CI) | Years | APC (95% CI) |
| Total | 26.42 | 40.16 | 2.4 (1.0;3.7) | 2000-2002 | 7.1 (-5.4;21.3) | 2002-2016 | 0.2 (-0.3;0.7) | 2016-2019 | 9.6 (5.7;13.6) |
| Women | 26.75 | 41.92 | 2.4(1.3;3.6) | 2000-2002 | 8.3 (-2.6;20.5) | 2002-2016 | 0.4 (-0.1;0.8) | 2016-2019 | 8.6 (5.2;12) |
| Men | 25.58 | 36.51 | 1.8 (0.9;2.7) | 2000-2016 | 0.1 (-0.5;0.6) | 2016-2019 | 11.6 (6.0;17.5) | ||
| ANTIDEPRESSANTS | |||||||||
| SSRI | 15.89 | 22.28 | 1.8 (0.4;3.1) | 2000-2004 | 5.0 (-0.5;10.8) | 2004-2014 | -2.4 (-3.6;-1.2) | 2014-2019 | 8.0 (5.3;10.7) |
| SNRI | 2.87 | 9.95 | 6.1 (4.6;7.6) | 2000-2010 | 9.1 (7.4;10.8) | 2010-2016 | -0.4 (-3.4;2.7) | 2016-2019 | 9.7 (3.8; 16.1) |
| TCA | 6.09 | 5.07 | -0.7 (-1.2;-0.1) | 2000-2010 | -2.0 (-2.8;-1.1) | 2010-2019 | 0.7 (0.0;1.5) | ||
| Neuromodulators | 5.62 | 11.65 | 3.9 (2.2;5.5) | 2000-2002 | 11.9 (-3.7;30.2) | 2002-2016 | 1.5 (1.0;2.1) | 2016-2019 | 10.0 (5.8;14.3) |
| MAOI | 0.29 | 0.06 | -6.1 (-10.1;-1.9) | 2000-2005 | -22.8 (-33.6;-10.1) | 2005-2019 | 0,7 (-2.8;4.3) | ||
| Bupropion | 0.36 | 2.19 | 7.4(5.4;9.5) | 2000-2019 | 7.4(5.4;9.5) | ||||
| OTHER | |||||||||
| Antipsychotics | 7.28 | 8.29 | 0.3 (-0.2;0.8) | 2000-2019 | 0.3 (-0.2;0.8) | ||||
| Anxiolytics | 19.52 | 18.09 | -0.7 (-1.1;-0.2) | 2000-2013 | -1.2(-1.7;-0.8) | 2013-2019 | 0.5 (-0.7;-1.6) | ||
| Hypnotics and sedatives | 11.27 | 14.77 | 1.3 (0.8;1.7) | 2000-2009 | 2.0 (1.5;2.5) | 2009-2017 | -0.1 (-0.7;0.5) | 2017-2019 | 3.5 (0.3;6.8) |
Fig. 3.
Trends in prescriptions of antidepressants in Flanders, Belgium from 2000 to 2019, in patients with depression (A) and relative to the total yearly patient population (B). Abbreviations: NDRI = norepinephrine–dopamine reuptake inhibitor, MAOI = monoamine oxidase inhibitors, SNRI = serotonin–norepinephrine reuptake inhibitors, TCA = tricyclic antidepressants, SSRI = selective serotonin reuptake inhibitors
Table 4.
Evolution of antidepressant prescriptions in Flanders, Belgium (2000-2019), using the whole yearly study population as the denominator
| Year | One antidepressant prescription (%) | Two or more prescriptions (%) |
|---|---|---|
| 2000 | 8.68 | 17.77 |
| 2001 | 8.39 | 19.97 |
| 2002 | 8.62 | 21.31 |
| 2003 | 8.15 | 22.04 |
| 2004 | 7.68 | 24.29 |
| 2005 | 7.34 | 23.75 |
| 2006 | 6.6 | 23.46 |
| 2007 | 6.77 | 23.95 |
| 2008 | 6.28 | 24.23 |
| 2009 | 6.44 | 23.99 |
| 2010 | 6.94 | 23.92 |
| 2011 | 6.59 | 24.31 |
| 2012 | 6.31 | 24.16 |
| 2013 | 6.28 | 24.06 |
| 2014 | 6.78 | 24.07 |
| 2015 | 6.5 | 25.21 |
| 2016 | 6.74 | 24.87 |
| 2017 | 6.39 | 20.48 |
| 2018 | 2.4 | 36.91 |
| 2019 | 2.83 | 37.33 |
In women as well as in men, a significant increase in prescriptions was observed, with a steep rise from 2016 to 2019 (Table 3; Figure A1, Appendix). Regarding the different subclasses of antidepressants, we observed an increase in prescriptions of SNRIs, neuromodulators and bupropion. During the whole study period, SSRIs were the most prescribed antidepressants. For example, in 2019, 22.28% of patients with depression had a prescription for an SSRI. (Table 3) Over the whole study period, prescription rates of antipsychotics remained stable. Prescriptions for anxiolytics showed a slight significant decrease, while those for hypnotics and sedatives showed a small significant increase. Data on those psychopharmaceuticals can be found in Table 3 and in Figure A2, Appendix.
Discussion
We found an increasing trend in age-standardized prevalence and a first decreasing, then increasing trend in the incidence of depression from 2000 to 2019 in Flanders, Belgium. Among patients diagnosed with depression, the average disease count went from 1.2 to 1.8 comorbidities per patient. The prescription of antidepressive medication among depression-diagnosed patients almost doubled over the study period. SSRIs were prescribed the most, and while there was a significant decrease from 2004 to 2014, afterwards their use increased significantly.
Trends in the prevalence and incidence of depression
This study showed an increase in age-adjusted prevalence of depression and a decreasing incidence from 2000 to 2015. For the calculation of the prevalence, we have assumed depression to be a chronic condition. While not strictly defined as such, some authors do consider it so [26, 27]. Based on earlier observations of symptom chronicity in depression [28], and the fact that relapse and recurrence are common [29, 30], we have adopted this viewpoint as well.
The trend in prevalence found in this study is consistent with the bulk of existing literature as recently evaluated in a meta-analysis by Moreno-Agostino et al. [31] However, there are not many studies discussing trends in the incidence of depression. Rait et al. found a decrease in the incidence of depression diagnoses in UK primary care from 1996 to 2006 and an increase in depressive symptoms [21], something this study did not research. This phenomenon could be explained by medical professionals being more careful with the medicalization of grief and non-pathological feelings of sadness [21, 32]. However, this does not explain the increase in incidence after 2015 that we found.
In light of interpreting our results, it is important to note that the INTEGO database underwent a change in 2017, with the participating practices switching medical software, updating the medical files from one system to another. Conceivably, this might have facilitated coding practice in general, stimulating physicians to code more frequently and diligently. Bearing this in mind, the increase in incidence could also be at least partly explained by a registration effect. In essence, this is a sort of registration bias, in that the diagnosis of depression is more likely to be registered than for example 15 years ago. This bias is present in other registries as well [33].
As shown in Fig. 3, the proportional use of SSRIs increased even when using the total yearly study population as a denominator, implying the increase in incidence is at least partially the result of actual morbidity.
Liu et al. also found some similarities with our study [34]. They reviewed global trends in the incidence of depression and found an estimated annual percentage change in Belgium of 0.88 (95% CI = 0.78 to 0.97) from 1990 to 2017, whereas we found an annual percentage change of 1.9 (95% CI = 0.40 to 3.30) from 2000 to 2019. In contrast with our study, they used a linear regression model. Also, their findings were based solely on surveys and self-reported data instead of diagnoses reported by FPs, which might overestimate the burden of depression as compared to actual clinical diagnoses.
We have found several Belgian studies describing the epidemiology of depression, but few focused on trends [35–37]. Wauterickx et al. found an upward trend from 1991 to 1999 based on yearly surveys [38]. On the other hand, the Belgian health interview survey showed a stable prevalence of depression between 2001 and 2018, although a peak of 14.8% was seen in 2013 [2].
In every age group a significant increase in prevalence was noted, with the highest AAPC in the 15 to 29-year-olds. This rise in prevalence in the youngest group has been described in other studies as well [4, 5, 7, 8]. It was also the only age group where no significant decline in the incidence rate was observed. Other studies have suggested that social media and problematic mobile phone use could play a role in this increase of depression [7, 39, 40]. Another explanation could be that this generation has been seeking more help in recent years. Since 2015, for example, there is a national Red Nose Day initiative in Belgium [41], focusing on increasing mental health awareness in adolescents. It is important to note in this context that younger patients tend to have worse mental health outcomes than older patients, particularly if they are not in active education or employment [42, 43].
Trends in comorbidities
Our study noted a rising trend in comorbidities from 2000 to 2019 with a disease count of 1.8 in 2019. An increase of patients with cancer was observed in the population of depressed patients. It is important for FPs and specialists to differentiate depression and non-pathological grief in these patients [44]. To the best of our knowledge, only one study examined time trends of comorbidities in relation to depression. This study, however, differed methodologically from ours in that the presence of comorbidities was linked to self-reported depression severity [45].
In addition, we also noted a rising proportion of depressed patients with alcohol abuse, as well as cardiovascular and metabolic disease. Judging from these results, we could conclude that the depressed patients in our sample became more ‘complex’, as they tended to have more diagnosed comorbidities on average later in the study. Alcohol abuse, for example, tends to be associated with higher drop-out rates from treatment [46]. Taken together, this is likely to impact the treatment of depression in a primary care context, as it will require a more multidisciplinary perspective and approach. On the other hand, part of this increase in comorbidity could be explained by increased detection rather than actual comorbidity. We have mentioned this earlier when discussing the registration effect.
Trends in medication
Consistently with previous studies [6, 10–16], we observed an increase in the prescription of antidepressive medication among patients diagnosed with depression. Earlier studies in the UK concluded that this might partly be explained by increased chronic prescription [47], something which we did not specifically study.
The decline in prescription of TCAs has also been reported in other studies. TCAs are known to have more side effects than SSRIs and SNRIs [10, 16].
The prescription of SSRIs increased from 2000 to 2004. This can be expected given that they are first choice products because of their safety profile and efficacy [48]. The peak noted in 2004 could be explained by the introduction of escitalopram on the market and the start of reimbursement in Belgium in 2003. From 2004 to 2014 we observed a decline in the prescription of SSRIs, followed by a steep increase from 2014 to 2019. The study of Noordam et al. described a decline in incident SSRI prescriptions, while noting a rise in the prevalence of all antidepressants combined. They attributed this to a shift in the guidelines recommending psychotherapy, especially for milder cases of depression, instead of medication [15].
Other studies noted that patents, marketing and reimbursement of medication could have had a large impact on prescriptions as well. For instance, after 2004 most SSRIs lost their patent and thus marketing for these products declined [12, 49]. On the other hand, reimbursement for SNRIs, bupropion and neuromodulators such as trazodone and mirtazapine, was approved between 2003 and 2008. It is fair to assume that these products were heavily promoted during the study period resulting in the rise of their prescriptions observed in this study.
This is something family physicians should be vigilant about, given that a recent systematic review of scientific evidence did not find the newer medications safer or more efficacious than SSRIs or TCAs [50]. According to the NICE guidelines, SSRIs and TCAs in certain indications are still the first-line treatment, combined with psychotherapy, for moderate to severe depression [51]. For less severe depression, medication should not be used, but psychotherapy should be offered. This approach is also supported by a recent meta-analysis [52].
Strengths and limitations
The major strengths of this study are the inclusion of a large sample of family practice patients, representative of the general Flemish population [23]. We had two decades of medical information available and because of the very nature of the data collection, information on comorbidities and prescriptions as well. To our knowledge, this is the first comprehensive registry-based study to describe trends in the prevalence and incidence of depression and the first to describe trends in comorbidities and antidepressive medication from 2000 to 2019.
Our study has a few limitations as well. In Belgium, patients do not need to be registered with a particular FP. This means that they have free choice in which FP to consult for new episodes or follow-up. Therefore, our patient population can vary even when the registering FPs stayed the same. In 2016, the Usual Provider Continuity Index was higher than 75% for over 65% of the Belgian population [53]. This means that at least 65% of patients have three out of four family practice visits with their usual FP, instead of with another FP. However, only 40% of patients have an exclusive FP relationship [53], meaning that they only go to their own FP.
The current study used the denominator YCG. Former research has shown that the YCG accounts for 80% of the total practice population [24]. The YCG is not the perfect denominator as it can contain different biases. However, the YCG is the most realistic approach in countries without capitation [24]. Furthermore, by using data from the INTEGO registry we can only extract data registered by FPs in the EMR, with respect to both coded diagnoses and medication prescriptions.
We also do not know which diagnostic tools the FPs used to arrive at the diagnosis and whether they over- or underdiagnosed depression. It was not possible to study an important pillar of depression treatment, namely psychotherapy, since it was not registered in the EMR.
Conclusion
In this registry-based study of the Flemish population, we noted an increasing trend in the age-adjusted prevalence of depression and a decreasing trend in incidence from 2000 to 2015, followed by a steep increase from 2015 to 2019. A significant rise in the average number of comorbidities at diagnosis was seen. This increased complexity of patients makes the approach to depression in a primary care context more challenging, implying the need for a multidisciplinary approach.
Additionally, there was a rise in the prescription of antidepressants with a steeper increase in recent years, which suggests that first-line treatment of depression in Flanders is still very much dependent on medication.
Supplementary Information
Acknowledgements
Not applicable.
Abbreviations
- AAPC
Average annual percentage change
- APC
Annual percentage change
- ATC
Anatomical Therapeutic Chemical classification
- EMR
Electronic medical record
- FP
Family physician
- ICPC-2
International Classification of Primary Care 2
- MAOI
Monoamine oxidase inhibitor
- NDRI
Norepinephrine–dopamine reuptake inhibitor
- SNRI
Selective serotonin and noradrenalin reuptake inhibitor
- SSRI
Selective serotonin reuptake inhibitor
- TCA
Tricyclic antidepressant
- WHO
World Health Organization
- YCG
Yearly contact group
Authors’ contributions
RW and SGB wrote the manuscript. PM and SGB performed statistical analyses. BV conceived the study design. PM, KC, MVN, GVP, LC and BV provided valuable input and co-wrote the manuscript. All authors reviewed and approved the final version of the manuscript.
Funding
This study was funded by a research project of the Research Foundation Flanders (FWO).
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available due to inclusion of protected health information but can be made available subsequent to further de-identification upon reasonable request to the corresponding author (SGB).
Declarations
Ethics approval and consent to participate
The INTEGO procedures used in this study are approved by the ethical review board of the KU Leuven Faculty of Medicine (no. ML 1723) and by the Belgian Privacy Commission (no. SCSZG/13/079) [23, 24]. INTEGO was waived the need for individual informed consent, but operates under an opt-out procedure for patients who do not wish their data to be included. This was approved by the aforementioned ethical review board.
All the procedures in this study are in accordance with current national guidelines and regulations.
Patient data were pseudonymized before use.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Roosje Walrave and Simon Gabriël Beerten are both joint first authors.
References
- 1.Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gisle L, Drieskens S, Demarest S, Heyden J. Geestelijke gezondheid: gezondheidsenquête 2018. Published online 2018.
- 3.Compton WM, Conway KP, Stinson FS, Grant BF. Changes in the prevalence of major depression and comorbid substance use disorders in the United States between 1991-1992 and 2001-2002. Am J Psychiatry. 2006;163(12):2141–2147. doi: 10.1176/ajp.2006.163.12.2141. [DOI] [PubMed] [Google Scholar]
- 4.Weinberger AH, Gbedemah M, Martinez AM, Nash D, Galea S, Goodwin RD. Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychol Med. 2018;48(8):1308–1315. doi: 10.1017/S0033291717002781. [DOI] [PubMed] [Google Scholar]
- 5.Mojtabai R, Olfson M, Han B. National Trends in the Prevalence and Treatment of Depression in Adolescents and Young Adults. Pediatrics. 2016;138(6). [DOI] [PMC free article] [PubMed]
- 6.Jeuring HW, Comijs HC, Deeg DJH, Stek ML, Huisman M, Beekman ATF. Secular trends in the prevalence of major and subthreshold depression among 55-64-year olds over 20 years. Psychol Med. 2018;48(11):1824–1834. doi: 10.1017/S0033291717003324. [DOI] [PubMed] [Google Scholar]
- 7.Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005-2017. J Abnorm Psychol. 2019;128(3):185–199. doi: 10.1037/abn0000410. [DOI] [PubMed] [Google Scholar]
- 8.Duffy ME, Twenge JM, Joiner TE. Trends in Mood and Anxiety Symptoms and Suicide-Related Outcomes Among U.S. Undergraduates, 2007-2018: Evidence From Two National Surveys. J Adolesc Health Off Publ Soc Adolesc Med. 2019;65(5):590–598. doi: 10.1016/j.jadohealth.2019.04.033. [DOI] [PubMed] [Google Scholar]
- 9.Yu B, Zhang X, Wang C, Sun M, Jin L, Liu X. Trends in depression among Adults in the United States, NHANES 2005-2016. J Affect Disord. 2020;263:609–620. doi: 10.1016/j.jad.2019.11.036. [DOI] [PubMed] [Google Scholar]
- 10.Henriksson S, Isacsson G. Increased antidepressant use and fewer suicides in Jämtland county, Sweden, after a primary care educational programme on the treatment of depression. Acta Psychiatr Scand. 2006;114(3):159–167. doi: 10.1111/j.1600-0447.2006.00822.x. [DOI] [PubMed] [Google Scholar]
- 11.Mojtabai R. Increase in antidepressant medication in the US adult population between 1990 and 2003. Psychother Psychosom. 2008;77(2):83–92. doi: 10.1159/000112885. [DOI] [PubMed] [Google Scholar]
- 12.Marcus SC, Olfson M. National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry. 2010;67(12):1265–1273. doi: 10.1001/archgenpsychiatry.2010.151. [DOI] [PubMed] [Google Scholar]
- 13.Sultana J, Italiano D, Spina E, Cricelli C, Lapi F, Pecchioli S. Changes in the prescribing pattern of antidepressant drugs in elderly patients: an Italian, nationwide, population-based study. Eur J Clin Pharmacol. 2014;70(4):469–478. doi: 10.1007/s00228-013-1636-z. [DOI] [PubMed] [Google Scholar]
- 14.Mojtabai R, Olfson M. National trends in long-term use of antidepressant medications: results from the U.S. Natl Health Nutr Exam Surv. J Clin Psychiatry. 2014;75(2):169–177. doi: 10.4088/JCP.13m08443. [DOI] [PubMed] [Google Scholar]
- 15.Noordam R, Aarts N, Verhamme KM, Sturkenboom MCM, Stricker BH, Visser LE. Prescription and indication trends of antidepressant drugs in the Netherlands between 1996 and 2012: a dynamic population-based study. Eur J Clin Pharmacol. 2015;71(3):369–375. doi: 10.1007/s00228-014-1803-x. [DOI] [PubMed] [Google Scholar]
- 16.Luo Y, Kataoka Y, Ostinelli EG, Cipriani A, Furukawa TA. National Prescription Patterns of Antidepressants in the Treatment of Adults With Major Depression in the US Between 1996 and 2015: A Population Representative Survey Based Analysis. Front Psychiatry. 2020;11(35). [DOI] [PMC free article] [PubMed]
- 17.Smith DJ, Court H, McLean G, Martin D, Langan Martin J, Guthrie B. Depression and multimorbidity: a cross-sectional study of 1,751,841 patients in primary care. J Clin Psychiatry. 2014;75(11):8. doi: 10.4088/JCP.14m09147. [DOI] [PubMed] [Google Scholar]
- 18.Read JR, Sharpe L, Modini M, Dear BF. Multimorbidity and depression: A systematic review and meta-analysis. J Affect Disord. 2017;221:36–46. doi: 10.1016/j.jad.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 19.Birk JL, Kronish IM, Moise N, Falzon L, Yoon S, Davidson KW. Depression and multimorbidity: Considering temporal characteristics of the associations between depression and multiple chronic diseases. Health Psychol. 2019;38(9):802–811. doi: 10.1037/hea0000737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet Lond Engl. 2007;370(9590):851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 21.Rait G, Walters K, Griffin M, Buszewicz M, Petersen I, Nazareth I. Recent trends in the incidence of recorded depression in primary care. Br J Psychiatry. 2009;195(6):520–524. doi: 10.1192/bjp.bp.108.058636. [DOI] [PubMed] [Google Scholar]
- 22.Davies MR, Buckman JEJ, Adey BN, et al. Comparison of symptom-based versus self-reported diagnostic measures of anxiety and depression disorders in the GLAD and COPING cohorts. J Anxiety Disord. 2022;85:102491. doi: 10.1016/j.janxdis.2021.102491. [DOI] [PubMed] [Google Scholar]
- 23.Truyers C, Goderis G, Dewitte H, Akker M, vanden, Buntinx F. The Intego database: background, methods and basic results of a Flemish general practice-based continuous morbidity registration project. BMC Med Inform Decis Mak. 2014;14(1):48. doi: 10.1186/1472-6947-14-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bartholomeeusen S, Kim CY, Mertens R, Faes C, Buntinx F. The denominator in general practice, a new approach from the Intego database. Fam Pract. 2005;22(4):442–447. doi: 10.1093/fampra/cmi054. [DOI] [PubMed] [Google Scholar]
- 25.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. doi: 10.1002/(SICI)1097-0258(20000215)19:3<335::AID-SIM336>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 26.Gask L. Is depression a chronic illness? For the motion. Chronic Illn. 2005;1(2):101–106. doi: 10.1177/17423953050010020501. [DOI] [PubMed] [Google Scholar]
- 27.Andrews G. Should depression be managed as a chronic disease? BMJ. 2001;322(7283):419–421. doi: 10.1136/bmj.322.7283.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Judd LL. The Clinical Course of Unipolar Major Depressive Disorders. Arch Gen Psychiatry. 1997;54(11):989–991. doi: 10.1001/archpsyc.1997.01830230015002. [DOI] [PubMed] [Google Scholar]
- 29.Buckman JEJ, Underwood A, Clarke K, et al. Risk factors for relapse and recurrence of depression in adults and how they operate: A four-phase systematic review and meta-synthesis. Clin Psychol Rev. 2018;64:13–38. doi: 10.1016/j.cpr.2018.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Burcusa SL, Iacono WG. Risk for recurrence in depression. Clin Psychol Rev. 2007;27(8):959–985. doi: 10.1016/j.cpr.2007.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moreno-Agostino D, Wu YT, Daskalopoulou C, Hasan MT, Huisman M, Prina M. Global trends in the prevalence and incidence of depression:a systematic review and meta-analysis. J Affect Disord. 2020;281:235–243. doi: 10.1016/j.jad.2020.12.035. [DOI] [PubMed] [Google Scholar]
- 32.Horwitz AV, Wakefield JC. The Loss of Sadness: How Psychiatry Transformed Normal Sorrow into Depressive Disorder. Oxford University Press; 2007:xv, 287. [DOI] [PubMed]
- 33.Hoff G, de Lange T, Bretthauer M, et al. Registration bias in a clinical quality register. Endosc Int Open. 2019;7(1):E90–E98. doi: 10.1055/a-0806-7006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu Q, He H, Yang J, Feng X, Zhao F, Lyu J. Changes in the global burden of depression from 1990 to 2017: Findings from the Global Burden of Disease study. J Psychiatr Res. 2020;126:134–140. doi: 10.1016/j.jpsychires.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 35.Ansseau M, Fischler B, Dierick M, Mignon A, Leyman S. Prevalence and impact of generalized anxiety disorder and major depression in primary care in Belgium and Luxemburg: the GADIS study. Eur Psychiatry. 2005;20(3):229–235. doi: 10.1016/j.eurpsy.2004.09.035. [DOI] [PubMed] [Google Scholar]
- 36.Brault MC, Meuleman B, Bracke P. Depressive symptoms in the Belgian population: disentangling age and cohort effects. Soc Psychiatry Psychiatr Epidemiol. 2012;47(6):903–915. doi: 10.1007/s00127-011-0398-0. [DOI] [PubMed] [Google Scholar]
- 37.Bruffaerts R, Bonnewyn A, Demyttenaere K. The epidemiology of depression in Belgium. A review and some reflections for the future. Tijdschr Psychiatr. 2008;50(10):655–665. [PubMed] [Google Scholar]
- 38.Wauterickx N, Bracke P. Unipolar depression in the Belgian population: trends and sex differences in an eight-wave sample. Soc Psychiatry Psychiatr Epidemiol. 2005;40(9):691–699. doi: 10.1007/s00127-005-0928-8. [DOI] [PubMed] [Google Scholar]
- 39.Augner C, Hacker GW. Associations between problematic mobile phone use and psychological parameters in young adults. Int J Public Health. 2012;57(2):437–441. doi: 10.1007/s00038-011-0234-z. [DOI] [PubMed] [Google Scholar]
- 40.Lin LY, Sidani JE, Shensa A, et al. Association between Social Media Use and Depression among U.S. Young Adults. Depress Anxiety. 2016;33(4):323–331. doi: 10.1002/da.22466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rode Neuzen Dag. Accessed October 6, 2021. www.rodeneuzendag.be
- 42.Saunders R, Buckman JEJ, Stott J, et al. Older adults respond better to psychological therapy than working-age adults: evidence from a large sample of mental health service attendees. J Affect Disord. 2021;294:85–93. doi: 10.1016/j.jad.2021.06.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Buckman JEJ, Stott J, Main N, et al. Understanding the psychological therapy treatment outcomes for young adults who are not in education, employment, or training (NEET), moderators of outcomes, and what might be done to improve them. Psychol Med. 2021;25:1–12. doi: 10.1017/S0033291721004773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Widera EW, Block SD. Managing grief and depression at the end of life. Am Fam Physician. 2012;86(3):259–264. [PubMed] [Google Scholar]
- 45.Leung J, Fan VS, Mahadevan R. How do different chronic condition comorbidities affect changes in depressive symptoms of middle aged and older adults? J Affect Disord. 2020;272:46–49. doi: 10.1016/j.jad.2020.03.125. [DOI] [PubMed] [Google Scholar]
- 46.Buckman JEJ, Naismith I, Saunders R, et al. The Impact of Alcohol Use on Drop-out and Psychological Treatment Outcomes in Improving Access to Psychological Therapies Services: an Audit. Behav Cogn Psychother. 2018;46(5):513–527. doi: 10.1017/S1352465817000819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moore M, Yuen HM, Dunn N, Mullee MA, Maskell J, Kendrick T. Explaining the rise in antidepressant prescribing: a descriptive study using the general practice research database. BMJ. 2009;339:b3999. doi: 10.1136/bmj.b3999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Declercq T, Vanden Ameele H, Callens J, Cloetens H. Richtlijn voor goede medische praktijkvoering: Depressie bij volwassenen. Antwerpen. Domus Medica. Published online 2017.
- 49.Serna C, Cruz I, Galván L, Real J, Gascó E, Soler-González J. Evolution of the prevalence and incidence of consumption of antidepressants in a Spanish region (2002-2007) Ment Health Fam Med. 2010;7(1):9–15. [PMC free article] [PubMed] [Google Scholar]
- 50.Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y. Comparative Efficacy and Acceptability of 21 Antidepressant Drugs for the Acute Treatment of Adults With Major Depressive Disorder: A Systematic Review and Network Meta-Analysis. Focus Am Psychiatr Publ. 2018;16(4):420–429. doi: 10.1176/appi.focus.16407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.National Collaborating Centre for Mental Health (UK). In: Depression: The Treatment and Management of Depression in Adults (Updated Edition): British Psychological Society; 2010. http://www.ncbi.nlm.nih.gov/books/NBK63748/. [PubMed]
- 52.Furukawa TA, Shinohara K, Sahker E, et al. Initial treatment choices to achieve sustained response in major depression: a systematic review and network meta-analysis. World Psychiatry. 2021;20(3):387–396. doi: 10.1002/wps.20906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Devos C, Cordon A, Lefèvre M, et al. Performance of the Belgian Health System – Report 2019. Belgian Health Care Knowledge Centre (KCE). 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and analysed during the current study are not publicly available due to inclusion of protected health information but can be made available subsequent to further de-identification upon reasonable request to the corresponding author (SGB).