Abstract
Background
Insomnia is a common sleep disorder in modern society. It causes reduced quality of life and is associated with impairments in physical and mental health. Listening to music is widely used as a sleep aid, but it remains unclear if it can actually improve insomnia in adults.
Objectives
To assess the effects of listening to music on insomnia in adults and to assess the influence of specific variables that may moderate the effect.
Search methods
We searched CENTRAL, PubMed, Embase, nine other databases and two trials registers in May 2015. In addition, we handsearched specific music therapy journals, reference lists of included studies, and contacted authors of published studies to identify additional studies eligible for inclusion, including any unpublished or ongoing trials.
Selection criteria
Randomised controlled trials and quasi‐randomised controlled trials that compared the effects of listening to music with no treatment or treatment‐as‐usual on sleep improvement in adults with insomnia.
Data collection and analysis
Two authors independently screened abstracts, selected studies, assessed risk of bias, and extracted data from all studies eligible for inclusion. Data on pre‐defined outcome measures were subjected to meta‐analyses when consistently reported by at least two studies. We undertook meta‐analyses using both fixed‐effect and random‐effects models. Heterogeneity across included studies was assessed using the I² statistic.
Main results
We included six studies comprising a total of 314 participants. The studies examined the effect of listening to pre‐recorded music daily, for 25 to 60 minutes, for a period of three days to five weeks.
Based on the Grades of Recommendations, Assessment, Development and Evaluation (GRADE) approach, we judged the evidence from five studies that measured the effect of music listening on sleep quality to be of moderate quality. We judged the evidence from one study that examined other aspects of sleep (see below) to be of low quality. We downgraded the quality of the evidence mainly because of limitations in design or being the only published study. As regards risk of bias, most studies were at high risk of bias on at least one domain: one study was at high risk of selection bias and one was judged to be at unclear risk; six studies were at high risk of performance bias; three studies were at high risk of detection bias; one study was at high risk of attrition bias and one study was judged to be at unclear risk; two studies were judged to be at unclear risk of reporting bias; and four studies were at high risk of other bias.
Five studies (N = 264) reporting on sleep quality as assessed by the Pittsburgh Sleep Quality Index (PSQI) were included in the meta‐analysis. The results of a random‐effects meta‐analysis revealed an effect in favour of music listening (mean difference (MD) ‐2.80; 95% confidence interval (CI) ‐3.42 to ‐2.17; Z = 8.77, P < 0.00001; moderate‐quality evidence). The size of the effect indicates an increase in sleep quality of the size of about one standard deviation in favour of the intervention compared to no treatment or treatment‐as‐usual.
Only one study (N = 50; low‐quality evidence) reported data on sleep onset latency, total sleep time, sleep interruption, and sleep efficiency. However, It found no evidence to suggest that the intervention benefited these outcomes. None of the included studies reported any adverse events.
Authors' conclusions
The findings of this review provide evidence that music may be effective for improving subjective sleep quality in adults with insomnia symptoms. The intervention is safe and easy to administer. More research is needed to establish the effect of listening to music on other aspects of sleep as well as the daytime consequences of insomnia.
Plain language summary
Music for insomnia in adults
Review question
This review assessed the effects of listening to music on insomnia in adults and the impact of factors that may influence the effect.
Background
Worldwide, millions of people experience insomnia. People can have difficulties getting to sleep, staying asleep or may experience poor sleep quality.
Poor sleep affects people's physical and mental health. The consequences of poor sleep are costly, for both individuals and society. Many people listen to music to improve their sleep, but the effect of listening to music is unclear.
Study characteristics
We searched electronic databases and music therapy journals to identify relevant studies. We included six studies with a total of 314 participants. The studies compared the effect of listening to music alone or with standard care to standard care alone or no treatment. The studies examined the effect of listening to pre‐recorded music daily, for 25 to 60 minutes, for a period of three days to five weeks.The evidence is current to 22 May 2015.
Key results
Five studies measured sleep quality. The findings suggest that listening to music can improve sleep quality. Only one study reported data on other aspects of sleep, including the length of time it takes to fall asleep, the amount of actual sleep someone gets, and the number of times people wake up. This study found no evidence to suggest that listening to music benefits these outcomes. None of the studies reported any negative side effects caused by listening to music.
Quality of the evidence
The quality of the evidence from the five studies that examined sleep quality was moderate. The quality of evidence for the other aspects of sleep was low. More high quality research is needed to investigate and establish the effect of listening to music on other aspects of sleep than sleep quality and on relevant daytime measures.
Summary of findings
Summary of findings for the main comparison. Listening to music compared to no treatment or treatment‐as‐usual (TAU) for adults with insomnia.
| Listening to music compared to no treatment or treatment‐as‐usual (TAU) for adults with insomnia | ||||||
| Patient or population: adults with insomnia Settings: home, sleep lab or rehabilitation centre Intervention: listening to music Comparison: no treatment or TAU | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No treatment or TAU | Listening to music | |||||
|
Sleep quality ‐ immediately post‐treatment
PSQI1. Scale from: 0 to 21 Follow‐up: 21 to 35 days |
The mean score in the intervention groups was 2.8 lower (3.42 lower to 2.17 lower) | 264 (5 studies) | ⊕⊕⊕⊝ moderate2,3 | A lower score indicates better sleep quality (i.e. fewer sleep problems). The change is about the size of one standard deviation which is considered a clinically relevant change. The studies included participants with a complaint of poor sleep (PSQI > 5)¹. |
||
|
Sleep onset latency ‐ immediately post‐treatment
PSG and morning questionnaire Follow‐up: 3 days |
See comment | See comment | 50 (1 study) | ⊕⊕⊝⊝ low4,5 | The one trial reporting this outcome found no evidence of an effect of the intervention. The data were not available for analysis. The study included participants that had reported poor sleep for at least one month (PSQI > 5)¹. |
|
| Total sleep time ‐ immediately post‐treatment PSG and morning questionnaire Follow‐up: 3 days | See comment | See comment | 50 (1 study) | ⊕⊕⊝⊝ low4,5 | The one study reporting this outcome found no evidence of an effect of the intervention. The data were not available for analysis. The study included participants that had reported poor sleep for at least one month (PSQI > 5)¹. |
|
| Sleep interruption ‐ immediately post‐treatment PSG and morning questionnaire Follow‐up: 3 days | See comment | See comment | 50 (1 study) | ⊕⊕⊝⊝ low4,5 | The one study reporting this outcome found no evidence of an effect of the intervention. The data are not available for analysis. The study included participants that had reported poor sleep for at least one month (PSQI > 5)¹. |
|
| Sleep efficiency ‐ immediately post‐treatment PSG Follow‐up: 3 days | See comment | See comment | 50 (1 study) | ⊕⊕⊝⊝ low4,5 | The one study reporting this outcome found no evidence of an effect of the intervention. The data were not available for analysis. The study included participants that had reported poor sleep for at least one month (PSQI > 5)¹. |
|
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; PSG: polysomnography; PSQI: Pittsburgh Sleep Quality Index | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Pittsburgh Sleep Quality Index. 0 indicates good sleep quality and 21 indicates severe sleep problems. Clinical cut off > 5 (Buysse 1989). 2 Limitations in the design such as inadequate allocation concealment procedures and lack of blinding. 3 The estimated effect is about one standard deviation and can be considered large. 4 Limitations in the design such as lack of blinding. 5 Only one trial measured this outcome.
Background
Description of the condition
Insomnia is one of the most common sleep disorders and affects millions of people worldwide. Insomnia can be defined as a subjective complaint of disturbed sleep in the presence of adequate opportunity and circumstance for sleep (NIH 2005). It is characterised by dissatisfaction with the quality, duration or continuity of sleep, such as problems falling asleep, maintaining sleep, early morning awakenings or complaints of non‐restorative sleep (Morin 2013). The diagnostic criteria for insomnia disorder as a clinical diagnosis vary depending on the diagnostic manual used. The fourth edition of the American Psychiatric Association's (APA) Diagnostic and Statistical Manual for Mental Disorders (DSM‐IV) defines primary insomnia as a subjective complaint of difficulty in initiating or maintaining sleep, or the presence of non‐restorative sleep, lasting for at least one month (APA 1994). According to these criteria, disturbed sleep causes clinically significant distress or impairment in social, occupational or other important areas of functioning. According to the APA criteria, primary insomnia is not the consequence of any substance use and is not linked to a major general medical condition, any mental disorder or an otherwise specified sleep disorder (APA 1994). However, the distinction between primary and secondary insomnia has been removed in the most recent update. Instead, 'insomnia disorder' is recognized as a condition requiring clinical attention independently of other medical conditions that may be present (APA 2013). Other diagnostic manuals, such as the the World Health Organization's (WHO) International Classification of Diseases, 10ͭʰ Revision (ICD‐10) and the International Classification of Sleep Disorders (ICSD‐2) distinguish between different insomnia subtypes and introduce different duration and frequency criteria (AASM 2005; WHO 1992).
Insomnia is common in people with medical or psychiatric illness and trials have found consistent relationships between insomnia and depression, anxiety disorders, and other psychological disorders, as well as substance abuse and dependence. Furthermore, insomnia is associated with a number of medical problems such as decreased immune functioning (Taylor 2003), cardiovascular disorders, hypertension, chronic pain, breathing difficulties, and gastrointestinal and urinary problems (Taylor 2007). Insomnia itself can have a number of negative daytime consequences and it is well recognised that people with insomnia experience impairments in everyday life such as fatigue and greater irritability (Riedel 2000; Shekleton 2010). People with insomnia report significantly lower quality of life than those without insomnia, and the reduction in quality of life is correlated with symptom severity (Léger 2001). Insomina affects occupational function and social relations and is associated with higher work absenteeism and increased risk of accidents, and therefore represents a condition with great costs for both the individual and society (Walsh 2004).
Estimates of the prevalence of insomnia vary according to the definitions used. A review of epidemiological trials revealed that about one third of the general population experiences symptoms of insomnia, such as difficulties initiating or maintaining sleep. When adding daytime consequences to the definition of insomnia, the prevalence rate drops to about 9% to 15% (Ohayon 2002). Sleep dissatisfaction is reported by 8% to 18% of the general population; using the DSM‐IV criteria for insomnia, a point‐prevalence rate of 6% is reported within the literature, with primary insomnia as the most frequent diagnosis (2% to 4%), followed by insomnia related to another mental disorder (1% to 3%) (Ohayon 2002).
Description of the intervention
Available treatments for insomnia include pharmacotherapy (medication), psychological and behavioural interventions, and a variety of complementary and alternative therapies. Basic education in sleep hygiene is commonly used to inform patients about lifestyle and environmental factors that may interfere with or promote sleep (Morin 2005). Although good sleep hygiene can be helpful, it is not considered sufficient to improve severe and chronic insomnia. Therefore, the most common treatment of insomnia is the use of pharmacotherapeutic interventions, including over‐the‐counter and prescribed medications (NIH 2005). Benzodiazepine receptor agonists have been approved for the treatment of insomnia by the U.S. Food and Drug Administration (FDA) and trials report beneficial short‐term effects of these agents. With the exception of eszopiclone, approved use is limited to 35 days or less (NIH 2005). However, there are some concerns about the long‐term use of these medications, due to risk of abuse, dependence, and adverse effects such as residual daytime sedation, cognitive impairments, and reduced motor co‐ordination. Furthermore, the use of hypnotics has been associated with increased mortality (Frandsen 2014; Kripke 2012).
Psychological and behavioural treatments show good efficacy in the treatment of persistent insomnia (Morin 2006b). These treatments include cognitive behavioural therapy, stimulus control therapy, sleep restriction therapy, and relaxation training, often combined in multi‐component approaches. In spite of good results, psychological and behavioural treatments appear to be under‐utilised, perhaps because they require considerable time and effort for the patient (Krystal 2004). Furthermore, there is a problem of availability, with relatively few well‐trained professionals in the field (Wilson 2010).
Given the current limitations of psychological and pharmacological treatments, different alternative and complementary interventions, one of which is music, are available to combat insomnia in adults. Trials show that listening to music is often used by adults as a self‐help intervention to improve sleep (Aritake‐Okada 2009; Morin 2006a; Urponen 1988), and a simple Google search on 'music' and 'sleep' reveals a huge market of music that is promoted for its sleep‐inducing properties. However, the efficiency of music as an intervention for insomnia remains unclear. Music is used as a therapeutic intervention in a number of areas, including pain relief (Cepeda 2006), psychiatry (Maratos 2008; Mössler 2011), neuro‐rehabilitation (Bradt 2010), and for improving psychological outcomes in medical conditions such as cancer and heart disease (Bradt 2011; Bradt 2013). Experimental and clinical studies show that music can affect autonomous nervous system functioning (Hodges 2009) as well as psychological factors such as mood and attention (Garza‐Villarreal 2014; Juslin 2001); as such, it may potentially impact sleep (see How the intervention might work). Research on the impact of music on sleep has evolved during the past 20 years, and methods for applying music listening to improve sleep quality vary across trials. Generally, the intervention involves the use of pre‐recorded music in relation to sleep initiation. Music listening can be used passively, or it can be used actively with specific instructions (e.g. relaxation instructions). The duration of the intervention period and the time spent listening to music may vary. The choice of music may be determined by the researcher or by the participants themselves. Relatively few trials on music and insomnia are randomised controlled trials (RCTs). Since the impact of the music intervention may differ depending on the design of the intervention, there is a need to evaluate the results of both RCTs and quasi‐randomised controlled trials (qRCTS) in order to retain valuable and reliable evidence.
How the intervention might work
Music has been found to influence human beings on many levels (Juslin 2001) and the impact of music listening on sleep has been attributed to different mechanisms. Several authors argue that improvement of sleep is obtained because slow soothing music enhances relaxation (Deshmukh 2009; Hernández‐Ruiz 2005; Jespersen 2012; Lai 2005). This suggestion is substantiated by trials showing reduced levels of cortisol as an effect of music listening (Koelsch 2011; Nilsson 2009), and changes in autonomous measures such as heart‐rate and blood pressure (Korhan 2011; Su 2013; Trappe 2010). These trials show that music can affect various physiological measures that reflect autonomic nervous system responses, and as such, slow soothing music may lead to a decrease in sympathetic arousal and thus improve sleep (Su 2013). From a psychological perspective, trials have shown that listening to music can reduce anxiety and stress responses (Dileo 2007; Zhang 2012), which can lead to greater relaxation and improvement of sleep. Another possible mechanism for the effect of music on sleep is the distracting power of music. Hernández‐Ruiz 2005 suggests that music can function as a focal point of attention that distracts from stressful thoughts and thereby improves sleep. A number of individual factors are also likely to influence the music experience, such as age and gender (Juslin 2011; Nieminen 2012), music preference (Vuust 2010), musical training (Brattico 2009; Vuust 2006), and culture (Hargreaves 1997). Different effects may therefore be found depending on the type of music used, the etiology of insomnia symptoms, and the length and duration of the intervention.
Why it is important to do this review
Music is commonly used to relieve sleep problems and the use of music as a non‐pharmacological intervention offers potential advantages of easy administration, low cost, and safety. Clinical trials have been performed to investigate the effect of music on sleep, but it remains unclear if the existing evidence is rigorous enough to reach conclusions about the general efficacy of the intervention. A systematic review is needed to establish the efficacy of music listening for improvement of sleep quality and thereby refute or validate the popular belief that music is helpful to promote sleep.
Objectives
To assess the effects of listening to music on sleep in adults with insomnia and to assess the influence of specific variables that may moderate the effect.
Methods
Criteria for considering studies for this review
Types of studies
The methods of this review were pre‐specified in the protocol (Jespersen 2013a).
We considered randomised controlled trials (RCTs) and quasi‐randomised controlled trials (qRCTs) that allocated participants to groups on the basis of a quasi‐random process, such as date of birth or alternate numbers for inclusion, for inclusion in the review. Since it is not possible to blind participants to the treatment (music), we included unblinded or single‐blinded trials.
Types of participants
We included adults with insomnia as documented by standardised measures (e.g. Pittsburgh Sleep Quality Index (PSQI; Buysse 1989)), objective measures (e.g. polysomnography or actigraphy), reports or diaries kept by participants, relatives or other informants; or individuals diagnosed with an insomnia disorder by standard diagnostic criteria, such as the International Classification of Diseases (ICD; WHO 1992), the Diagnostic and Statistical Manual of Mental Disorders (DSM; APA 1994) or International Classification of Sleep Disorders (ICSD; AASM 2005); or with an individual's complaint of sleep difficulties.
Types of interventions
We included any intervention that comprised listening to pre‐recorded music with or without relaxation instructions. The intervention could be self‐administered or administered by research or clinical personnel. Interventions included music listening compared with a no music control group or treatment‐as‐usual (TAU), and music therapy added to TAU compared to TAU alone.
Types of outcome measures
Primary outcomes
Our outcomes of interest were sleep‐ and insomnia‐related symptoms as measured by sleep diaries, polysomnography, actigraphy, or by standardised scales for the assessment of sleep and sleep‐related symptoms (e.g. PSQI or Insomnia Severity Index (ISI)). Furthermore, to establish the safety of the intervention, we considered the reporting of adverse events as a primary outcome. The primary outcomes were:
Sleep quality.
Sleep onset latency.
Total sleep time.
Sleep interruption (number of awakenings and waking after sleep onset).
Sleep efficiency (percent of time in bed spent asleep).
Adverse events (as reported by trialists; e.g. discomfort or hearing loss).
Secondary outcomes
Secondary outcomes of interest were waking‐related correlates and daytime consequences of insomnia. The relevant measures included:
-
Psychological outcomes.
Depression.
Anxiety.
Quality of life.
-
Physical outcomes.
Fatigue.
Daytime sleepiness.
Pain.
-
Physiological outcomes.
Heart rate.
Heart rate variability.
Blood pressure.
We included trials that measured psychological outcomes by standardized questionnaires with established reliability and validity (e.g. Beck Depression Inventory (BDI; Beck 1996), State‐Trait Anxiety Inventory (STAI; Spielberger 1983), Short‐Form 36 (SF‐36) health survey (Ware 1992)). We included trials that measured physical outcomes with standardised procedures such as the Multiple Sleep Latency Test (MSLT) or validated rating scales. We included trials that measured physiological outcomes with standardized procedures such as an electrocardiogram (ECG).
We considered the trial period and follow‐up as described in the included trials. When assessing outcomes in relation to time points, we grouped the data as: immediate post‐intervention, short‐term (post‐intervention to one month), medium‐term (between one and three months follow‐up), and long‐term (more than three months follow‐up) effects.
We reported all primary outcomes in Table 1.
Search methods for identification of studies
We did not apply any restrictions on date, language, or publication status when searching for trials or when deciding on trial inclusion.
Electronic searches
To identify the relevant trials, we searched the following electronic databases on 22 May 2015.
Cochrane Central Register of Controlled Trials (CENTRAL), 2015, Issue 4, part of theCochrane Library, and includes the Cochrane Developmental Psychosocial and Learning Problems Group Specialised Register.
PubMed (ncbi.nlm.nih.gov/pubmed), 1950 to 22 May 2015.
Embase (Elsevier), 1980 to 22 May 2015.
CINAHL (EBSCOhost), 1982 to 22 May 2015.
PsycINFO (ProQuest), 1967 to 22 May 2015.
Web of Science (Science Citation Index Expanded, Social Sciences Citation Index, Arts and Humanities Citation Index, Conference Proceedings Citation Index ‐ Science, and Conference Proceedings Citation Index ‐ Social Science and Humanities), 1980 to 22 May 2015.
SCOPUS (Elsevier), 1960 to 22 May 2015.
ClinicalTrials.gov (ClinicalTrials.gov), all available years searched 22 May 2015.
Current Controlled Trials (controlled‐trials.com/), all available years searched 22 May 2015.
Répertoire International de Littérature Musicale (RILM; EBSCOhost), 1969 to 22 May 2015.
The search strategies for the databases can be found in Appendix 1.
Searching other resources
We handsearched 15 journals, which are listed in Appendix 2, and searched the bibliographies of retrieved articles and relevant reviews to identify potential trials missed by the electronic searches. We also performed a citation search in ISI Web of Science to identify reports that had cited any relevant trials retrieved by the search to discover more recent trials that could have been missed. In addition, we contacted experts in the field to identify any unpublished trials.
Data collection and analysis
Selection of studies
Two authors (KVJ and JK) independently screened all titles and abstracts. All papers for which the title or abstract referred to a trial on music and sleep were retrieved in full. In cases where there was insufficient information in the title or abstract to determine the relevance of a paper, we retrieved the full text. Both authors independently reviewed the full‐text papers against a previously prepared inclusion criteria form to assess the trial's eligibility for inclusion. Disagreements were discussed and a third author (PJ) was involved in making the final decision. We kept a record of excluded articles and the reason for their exclusion (Characteristics of excluded studies).
Data extraction and management
Using a standardized coding form, the first two authors (KVJ and JK), who were blinded to each other’s assessment, extracted the data. Disagreements were resolved by consensus. If outcome data were not available, we contacted the authors of the trial.
From each trial, we extracted the following information.
1. General information
Author
Year of publication
Title
Journal (title, volume, pages) or if unpublished source
Country
Language of publication
2. Trial design
Design (e.g. parallel or cross‐over design)
Method of randomisation (and concealment)
Nature of the control group (e.g. no treatment or TAU)
Losses to follow‐up
Blinding of trial evaluators
Washout period in cross‐over design
Inclusion criteria
Exclusion criteria
3. Participants
Total sample size
Number in experimental group
Number in control group
Age
Gender
Ethnicity
Diagnosis
Comorbidities
Sleep quality (and reason for poor sleep)
Duration of disorder
Previous or additional treatments
4. Intervention
Type of music employed (characteristics)
Music selection (selected by participant or researcher)
Who provided the music (participant or research personal)
Length and frequency of intervention sessions
Intervention period (duration of intervention)
How participants were exposed to music (e.g. headphones or loudspeakers)
Listening instructions
5. Outcomes
Methods of sleep assessment
Secondary outcome measures
Pre‐test means and post‐test means or change scores and standard deviations, for all groups for all outcomes specified above
Baseline differences
Follow‐up period
Assessment of risk of bias in included studies
Two authors (KVJ and JK) independently assessed the risk of bias by using the tool described (and the criteria outlined) in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). They solved disagreements by discussion with the fourth author (PV). When information for evaluating methodological criteria was absent, we contacted the authors to obtain further information.
We graded each trial for risk of bias in each of the following domains.
1. Random sequence generation (checking for possible selection bias)
We assessed the method used to generate the allocation sequence for each included trial in sufficient detail to allow an assessment of whether it produced comparable groups.
We rated the risk of bias as follows.
Low risk of bias (adequate method of random sequence generation: e.g. any truly random process such as random number table; computer random number generator).
High risk of bias (inadequate method of random sequence generation: e.g. any non‐random process such as odd or even date of birth; hospital or clinic record number).
Unclear risk of bias (insufficient information about the method of random sequence generation to permit a judgement of low risk or high risk of bias).
2. Allocation concealment (checking for possible selection bias)
We assessed the method used to conceal the allocation sequence for each included trial and determined whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We rated the risk of bias as follows.
Low risk of bias (adequate method of allocation concealment: e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes).
High risk of bias (inadequate method of allocation concealment: e.g. open random allocation; unsealed or non‐opaque envelopes; alternation; date of birth).
Unclear risk of bias (insufficient information to permit a judgement of low risk or high risk of bias).
3. Blinding of participants and personnel (checking for possible performance bias)
We assessed the different methods used to blind personnel from knowledge of which intervention a participant received for each included trial. Since it is not possible to blind a participant to the treatment (music), we assessed trials at low risk of bias if we judged that the lack of blinding was not affecting the results. We assessed blinding of participants and personnel separately for different outcomes or classes of outcomes, since we expected certain outcomes (e.g. laboratory measurements and physiological data such as heart rate or blood pressure) to be unaffected by blinding of participants and personnel.
We rated the risk of bias as follows.
Low risk of bias (adequate method of blinding; outcome not likely to be influenced by lack of blinding).
High risk of bias (inadequate method of blinding; outcome likely to be influenced by lack of blinding).
Unclear risk of bias (insufficient information to permit a judgement of low risk or high risk of bias).
4. Blinding of outcome assessment (checking for possible detection bias)
We assessed the methods used to blind outcome assessment for each included trial. We assessed blinding separately for different outcomes or classes of outcomes, as stated above.
We rated the risk of bias as follows.
Low risk of bias (adequate method of blinding; outcome not likely to be influenced by lack of blinding).
High risk of bias (inadequate method of blinding; outcome likely to be influenced by lack of blinding).
Unclear risk of bias (insufficient information to permit a judgement of low risk or high risk of bias).
5. Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations)
We assessed data on attrition, exclusions, and reasons to determine if they introduced bias. We described the completeness of data for each included trial and for each outcome or class of outcomes. We assessed whether attrition and exclusions were reported, the numbers of participants included at each stage of the analysis (compared with the total participants randomised), whether reasons for attrition or exclusion were reported, and whether missing data were balanced across groups or were likely to be related to outcomes.
We judged whether incomplete data was dealt with adequately and rated the risk of bias as follows.
Low risk of bias (no missing outcome data; balanced missing outcome data; appropriate methods of imputing missing data).
High risk of bias (missing outcome data; unbalanced missing outcome data; inappropriate methods of imputing missing data).
Unclear risk of bias (insufficient information to permit a judgement of low risk or high risk of bias).
6. Selective reporting bias
We investigated the possibility of selective outcome reporting bias for each included trial. We conducted electronic searches to identify protocols of respective trials as a source to judge selective reporting.
We rated the risk of bias as follows.
Low risk of bias (all pre‐specified and expected outcomes were reported).
High risk of bias (not all pre‐specified and expected outcomes were reported; outcome that was not pre‐specified was reported; outcome was reported incompletely).
Unclear risk of bias (insufficient information to permit a judgement of low risk or high risk of bias).
7. Other bias
We assessed other risks of bias, specifically a risk of bias from baseline differences and a risk of bias from carry‐over or period effects for cross‐over trials.
We rated the risk of bias as follows.
Low risk of bias (the trial appeared to be free of other sources of bias).
High risk of bias (there was at least one important risk of bias).
Unclear risk of bias (insufficient information to permit a judgement of low risk or high risk of bias).
With reference to each of the above domains, we assessed the likely magnitude and direction of the bias and whether we considered it likely to impact the findings. We explored the impact of the level of bias by undertaking sensitivity analyses – see subsection on Sensitivity analysis.
Measures of treatment effect
Two authors (KVJ and JK) independently extracted data from trials identified for inclusion to ensure accuracy. We used Review Manager 5 (RevMan; RevMan 2014) for data entry and analyses.
Continuous data
We analysed continuous outcomes measured on the same scale between trials (e.g. PSQI) using the mean difference (MD).
Ordinal data
We analysed ordinal data measured on scales (i.e. sleep quality on visual analogue scales) as continuous data and the intervention effect was expressed as a difference in means.
Please see Jespersen 2013 and Appendix 3 for additional methods archived for future updates of this review.
Unit of analysis issues
Cluster‐randomised trials
We did not identify any cluster‐randomised trials. For further information on how these kinds of studies will be dealt with in future updates of this review, see Jespersen 2013a and Appendix 3.
Cross‐over trials
We did not identify any cross‐over trials. For further information on how these kinds of studies will be dealt with in future updates of this review, see Jespersen 2013a and Appendix 3.
Trials with more than two treatment arms
If a trial reported multiple treatment arms, we only used comparisons between the music intervention and the control or TAU group. For further information on how we will deal with other trials with more than two treatment arms, see Jespersen 2013a and Appendix 3 .
Dealing with missing data
For included trials, we noted levels of attrition in the incomplete outcome data section of the 'Risk of bias' tables beneath the Characteristics of included studies tables. Where information about the presented data set was missing in the trial reports, or if there was a lack of detail or a discrepancy between different reports, or clarification was needed, we tried to retrieve relevant information by contacting the authors of the trial. Where data were missing due to loss to follow‐up or dropout, we attempted to obtain complete outcome data from trial authors to include all participants randomised to each group in the analyses. If any outcome data remained missing, or if trial authors did not respond within a reasonable time, we analysed data on an available case basis, based on the numbers of participants for whom outcome data (continuous and dichotomous) were known. We did not impute missing data. For more information on how we will deal with missing data in future updates of this review, see Jespersen 2013a and Appendix 3.
Assessment of heterogeneity
We assessed clinical and methodological heterogeneity by examining the characteristics of the trials. The similarities between interventions (e.g. dose, frequency), participants (e.g. age), trial design (e.g. allocation concealment, blinding, losses to follow‐up), and the outcomes are reported in the Included studies subsection. Heterogeneity of treatment response was assessed visually from the forest plot of the mean difference (MD) and the Chi² test. In addition, heterogeneity was assessed statistically according to the standard method using the I² statistic, calculated for each comparison on each outcome. Substantial heterogeneity was assumed if I² was greater than 50%, indicating that 50% of the variability in the outcome cannot be explained by sampling variation. For further information on how we will deal with heterogeneity in future updates of this review, see Jespersen 2013a and Appendix 3.
Assessment of reporting biases
We attempted to minimize the potential for publication bias by our comprehensive search strategy that included evaluating published and unpublished literature.
Where we suspected reporting bias, we contacted trial authors asking them to provide missing outcome data.
For further information on how we will deal with reporting bias in future updates of this review, see Jespersen 2013a and Appendix 3.
Data synthesis
We entered all trials included in the systematic review into Review Manager 5 (RevMan 2014) and checked for data entry errors. We conducted a meta‐analysis when there were data from at least two included trials and substantial heterogeneity was absent. We undertook meta‐analyses using both fixed‐effect and random‐effects models. Where there was agreement between the results of both analyses, we reported the results from random‐effects models as it conveys the variability better. If fixed‐effect and random‐effect models revealed different results, we investigated possible sources of heterogeneity or inconsistency among trials in the magnitude or direction of effects.
Assessing the quality of the evidence
Using the approach developed by the Grading of Recommendation, Assessment, Development and Evaluation (GRADE) working group, we rated the quality of the evidence as 'high', 'moderate', 'low' or 'very low' (GRADE 2013). Evidence from RCTs were given an initial 'high quality' rating, but the assessment was downgraded if the trial methodology had a risk of bias, if there was substantial inconsistency among the results, if the evidence was indirect or imprecise, and if there was evidence of publication bias. The assessment was upgraded if a large effect was found. The results of the GRADE assessment for the primary outcomes is found in Table 1. The table was constructed using the GRADEpro software (GRADEpro 2014).
Subgroup analysis and investigation of heterogeneity
We carried out the following subgroup analyses (ranked in order of importance).
Researcher‐selected music versus participant‐selected music.
Music listening alone versus music listening with relaxation instructions.
The subgroup analyses were exploratory and conducted as recommended in section 9.6 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
For further information on other intended subgroup analyses, see Jespersen 2013a and Appendix 3.
Sensitivity analysis
We conducted the following sensitivity analyses to determine the impact of trial quality and risks of bias on the results of the meta‐analyses.
Excluded trials with inadequate methods of random sequence generation.
Excluded trials using inadequate methods of allocation concealment.
Excluded trials using inadequate methods of blinding outcome assessment.
For additional information on other intended sensitivity analyses, see Jespersen 2013a and Appendix 3.
Results
Description of studies
Results of the search
After removing duplicates, we identified 465 records during the search conducted in May 2015 (see Figure 1). After screening titles and abstracts, we identified 71 references that were considered potentially relevant and retrieved them for further examination. One potentially relevant trial was published by two of the authors of this review. To avoid the influence of dual authorship, two authors with no involvement in the trial (JK and PJ) assessed the eligibility and risks of bias of this trial. We excluded 55 trials (from 61 reports) (see Excluded studies). We included six trials (eight reports) that matched the inclusion criteria. We categorised one trial (two reports) as 'awaiting classification', since there was insufficient information to assess inclusion and exclusion. We identified two relevant ongoing trials.
1.
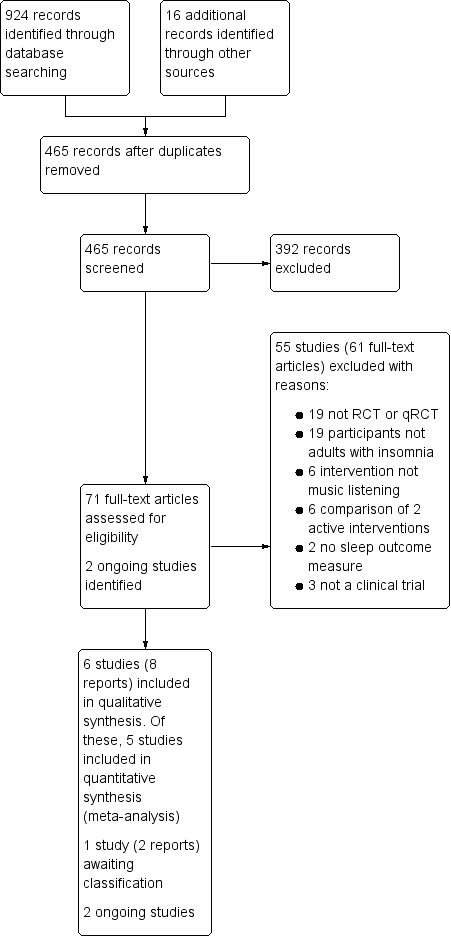
Study flow diagram
Included studies
Six trials met the inclusion criteria for this review (see Characteristics of included studies). Five were RCTs (Chang 2012; Harmat 2008; Kullich 2003; Lai 2005; Shum 2014) and one was a qRCT (Jespersen 2012). All trials used a parallel group design. One trial examined the effects of music listening on sleep quality in adults with insomnia related to pain (Kullich 2003), and one on its effects on insomnia related to psychological trauma (Jespersen 2012). Two trials included older adults with sleep problems (Lai 2005; Shum 2014), and two trials provided no information on the reason for poor sleep quality (Chang 2012; Harmat 2008).
The trials were conducted in five different countries. Two were conducted in Taiwan (Chang 2012; Lai 2005), one in Singapore (Shum 2014), one in Hungary (Harmat 2008), one in Denmark (Jespersen 2012), and one in Austria (Kullich 2003).
Trial size
The six included trials comprised a total of 314 participants. Trial sample sizes ranged from 15 to 65 participants with an average sample size of 52 (median 60). One trial had a small sample size of 15 participants (Jespersen 2012), and the remaining five trials had sample sizes between 50 and 65 participants (Chang 2012; Harmat 2008; Kullich 2003; Lai 2005; Shum 2014).
Setting
Four of the included trials measured the effect of the music listening intervention in the participants' own home (Harmat 2008; Jespersen 2012; Lai 2005; Shum 2014). In three of these trials, data were collected during a weekly visit to the participants' homes (Jespersen 2012; Lai 2005; Shum 2014), and in two of these trials, participants were also telephoned once or twice a week to ensure compliance with the protocol (Lai 2005; Shum 2014). In the fourth trial, the intervention group, but not the control group, was telephoned once a week to assess compliance (Harmat 2008).
Of the remaining two trials, one was conducted in a sleep laboratory (Chang 2012), and one implemented the intervention at an inpatient rehabilitation facility for persons with low‐back pain (Kullich 2003).
Participants
The participants in the included trials were between 19 and 83 years of age. One trial did not report gender (Lai 2005), but in the remaining five trials, the majority of participants were women (70%).
Five studies stated that they recruited participants with complaints of insomnia, and all trials used scores greater than five on the Pittsburgh Sleep Quality Index (PSQI) as evidence of insomnia symptoms. One trial did not include sleep difficulties as inclusion criteria, but all participants had PSQI scores greater than five, indicating insomnia problems (Kullich 2003). The severity of the sleep difficulties varied, with mean PSQI scores at baseline ranging from 6.8 to 16.0. Four of the trials reported mean baseline scores around 10 (Chang 2012; Kullich 2003; Lai 2005; Shum 2014).
The target populations in the six trials were diverse. One trial recruited traumatized refugees (Jespersen 2012), and another recruited patients undergoing rehabilitation for low‐back pain (Kullich 2003). Four trials recruited persons with insomnia that were otherwise healthy (Chang 2012; Harmat 2008; Lai 2005; Shum 2014), and two of these trials focused on older adults (Lai 2005; Shum 2014).
Interventions
All included trials used listening to pre‐recorded music as the main intervention. Four trials examined the effects of listening to music only (Chang 2012; Harmat 2008; Jespersen 2012; Shum 2014), and two trials examined music listening with relaxation instructions (Kullich 2003; Lai 2005). In all trials, music was used once a day. Four trials instructed participants to listen to the music at bedtime (Chang 2012; Harmat 2008; Jespersen 2012; Lai 2005). The remaining two trials did not specify what time of the day to listen to the music (Kullich 2003; Shum 2014). The length of the music listening sessions ranged from 25 to 60 minutes with an average of 43 minutes (median 45). The duration of the intervention period ranged from 3 to 35 days, with four trials having an intervention period of 21 days (Harmat 2008; Jespersen 2012; Kullich 2003; Lai 2005), one trial having an intervention period of three days (Chang 2012), and one trial assessing five weeks of intervention (Shum 2014).
The music used in the intervention was selected by the researchers in five trials (Harmat 2008; Jespersen 2012; Kullich 2003; Lai 2005; Shum 2014). Two of these trials gave participants a choice among four or six types of music in different genres (Lai 2005; Shum 2014 respectively). The remaining three trials used the same music for all participants. The sixth trial encouraged participants to bring their own preferred music for bedtime listening (Chang 2012). Those who did not bring their own music (more than half) listened to music prepared by the researchers. In total, 10 participants listened to their own preferred music and 149 participants listened to music chosen by the researcher.
All trials provided information on the music used in the study. The genres reported were Western and Chinese classical music, new age, eclectic, popular oldies, and jazz. Four trials gave information on the specific recordings used (composition title and composer) (Harmat 2008; Jespersen 2012; Kullich 2003; Lai 2005). Two trials stated the specific pieces of music used, but did not give performance‐specific information (Chang 2012; Shum 2014). Four trials described characteristics of the music (Chang 2012; Jespersen 2012; Lai 2005; Shum 2014). These shared common features such as low tempo (52 to 85 beats per minute), stable dynamic structure, and no strong rhythmic accentuation.
Four trials compared the music listening intervention to a no‐treatment control group (Chang 2012; Harmat 2008; Lai 2005; Shum 2014), and two trials compared music listening adjunctive to treatment‐as‐usual (TAU) versus TAU alone (Jespersen 2012; Kullich 2003). One trial had two active intervention groups (Harmat 2008), but only data from the music listening group compared to the no‐treatment control group were included in this review.
Outcomes
Five trials reported on sleep quality using the PSQI (Harmat 2008; Jespersen 2012; Kullich 2003; Lai 2005; Shum 2014). One trial used the polysomnography to objectively measure sleep onset latency, total sleep time, sleep interruption, and sleep efficiency (Chang 2012). The same trial also used a morning questionnaire to report subjective measures of sleep onset latency, total sleep time, and sleep interruption. No trials reported adverse events or deterioration of outcomes during the intervention period. None of the trials reported any secondary outcomes of interest to this review (see the Methods section). Harmat 2008 did measure levels of depression, but only in the intervention group and not in the control group.
Funding sources
Four trials were funded or partly funded by a grant from a national research council, university, government or foundation (Chang 2012; Harmat 2008; Jespersen 2012; Kullich 2003). Two trials reported no information on funding sources (Lai 2005; Shum 2014).
Excluded studies
We excluded 55 trials (from 61 reports) from this review. We excluded 19 trials because they did not have an RCT or qRCT design (e.g. no control group or no randomisation procedure); 19 trials because the participants were not adults with insomnia as defined in the Types of participants subsection (some trials used participants with no sleep problems, some included both good and poor sleepers, and some had no clear documentation of the insomnia problems). We excluded six trials because the intervention was not music listening (e.g. choir singing); six trials because they compared two active interventions (e.g. music versus muscle relaxation techniques); two trials because they had no sleep outcome measure, and three trials because they were not clinical trials (e.g. reflections on practice). We listed the reasons for exclusion for each individual trial in the Characteristics of excluded studies table.
Ongoing studies
Two relevant studies were still ongoing when this review was written (NCT02321826; NCT02376686); see Characteristics of ongoing studies.
Trials awaiting classification
One potentially relevant but unpublished trial was identified (Miller 2002). The trial is referred to in published material (Bernatzky 2011), but there is insufficient information to assess the trial for inclusion or exclusion. The author has been contacted, but has yet to respond (see Characteristics of studies awaiting classification).
Risk of bias in included studies
We assessed the six included trials for risk of bias across the following domains: 1) random sequence generation (selection bias); 2) allocation concealment (selection bias); 3) blinding of participants and personnel (performance bias); 4) blinding of outcome assessment (detection bias); 5) incomplete outcome data (attrition bias); 6) selective reporting (reporting bias); and 7) other bias. The results are depicted in Figure 2. Figure 3 provides a summary of the risk of bias results for each of the included trials. Reasons for the judgement are described in the risk of bias tables beneath the Characteristics of included studies tables.
2.
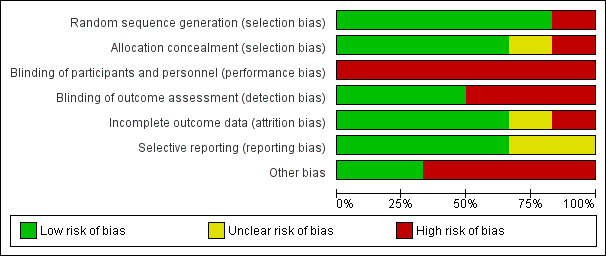
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included trials
3.
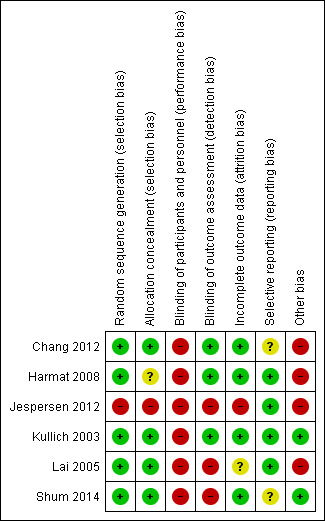
Risk of bias summary: review authors' judgements about each risk of bias item for each included trial
Allocation
All trials described the randomisation procedures applied. Five trials used a true randomisation procedure (e.g. using a computerized randomisation table), and were judged to be at low risk of bias (Chang 2012; Harmat 2008; Kullich 2003; Lai 2005; Shum 2014). One trial used a quasi‐randomised alternation procedure and was judged to be at high risk of bias (Jespersen 2012).
Four trials described measures taken to conceal allocation and were rated as being at low risk of bias (Chang 2012; Kullich 2003; Lai 2005; Shum 2014). One trial had limited information on allocation concealment and was judged to be unclear for a risk of bias (Harmat 2008), and one trial had no concealment procedure and was judged at high risk of bias (Jespersen 2012).
Blinding
Due to the nature of the intervention, it is not possible to blind participants and it can be difficult to blind personnel or researchers. Bias was considered likely to have occurred in those trials using subjective reports of sleep quality when participants were not blinded (Harmat 2008; Jespersen 2012; Kullich 2003; Lai 2005; Shum 2014). Bias was considered less likely to have occurred in the one trial involving objective measures of sleep, although this trial also included subjective measures of sleep (Chang 2012). Therefore, all trials were judged to be at high risk of performance bias.
In one trial, the technician scoring the polysomnography and the researchers doing the statistical analyses were blinded to group allocation (Chang 2012). One trial reported that group allocation was coded to blind the outcome assessors (Harmat 2008, and another trial reported that the data assessment was done by administrative personnel who were unaware of group allocation (Kullich 2003). These three trials were judged to be at low risk of detection bias. However, the three remaining trials were unblinded and rated as being at high risk of detection bias (Jespersen 2012; Lai 2005; Shum 2014).
Incomplete outcome data
Four trials reported no attrition and no missing data and were rated as being at low risk of attrition bias (Chang 2012; Harmat 2008; Kullich 2003; Shum 2014). In two of these studies (Harmat 2008; Kullich 2003) the information on attrition was not included in the published report but was provided by the authors at our request. One trial had unclear information on attrition and was rated as being unclear for this risk of bias (Lai 2005). Another trial reported the dropout of four participants resulting in an uneven distribution between groups, and was consequently rated as being at high risk of attrition bias (Jespersen 2012). We conducted a sensitivity analysis and found that including or excluding this study did not change the results. Therefore, we included it in successive analyses.
Selective reporting
One trial did not include outcome measures for the no‐treatment control group in the published report, but this information was provided by the authors at our request and did not change the results or conclusions of the published paper (Harmat 2008). Hence, we did not suspect reporting bias and judged the trial to be at low risk of reporting bias. In two trials, there was some uncertainty about the full reporting of outcomes, so these trials were rated as being unclear for the risk of reporting bias (Chang 2012; Shum 2014). There was no evidence of selective reporting in the remaining three trials, which were judged to be at low risk of reporting bias (Jespersen 2012; Kullich 2003; Lai 2005).
Other potential sources of bias
Other potential sources of bias were detected in four trials (Chang 2012; Harmat 2008; Jespersen 2012; Lai 2005). Three trials reported baseline differences between the intervention and control group (Chang 2012; Jespersen 2012; Lai 2005), and in one trial, methods of data collection differed between the intervention and control group (Harmat 2008). Thus, these trials were judged to be at high risk for other biases. No other risks of bias was detected in the final two trials and so these trials were rated as being at low risk for other bias (Kullich 2003; Shum 2014).
Effects of interventions
See: Table 1
For an overview, see Table 1. All outcomes are reported as immediate post‐treatment effects.
Primary outcomes
Sleep quality
Five trials, comprising 264 participants, reported on sleep quality and were pooled in meta‐analyses (Harmat 2008; Jespersen 2012; Kullich 2003; Lai 2005; Shum 2014; Analysis 1.1). All trials measured sleep quality with the PSQI and had an intervention period of 21 to 35 days. Meta‐analyses using both fixed‐effect and random‐effects models revealed good agreement and thus we have reported the results from the random‐effects models. The results of the analysis revealed a significant effect in favour of the intervention (mean difference (MD) ‐2.80, 95% confidence interval (CI) ‐3.42 to ‐2.17; Z = 8.77, P < 0.00001; Figure 4). The size of the effect indicates an increase of sleep quality and a decrease of symptoms of insomnia of approximately one standard deviation (SD) in favour of the intervention compared to no treatment or TAU respectively. No statistical heterogeneity was indicated (Tau² = 0.00; I² = 0%).
1.1. Analysis.
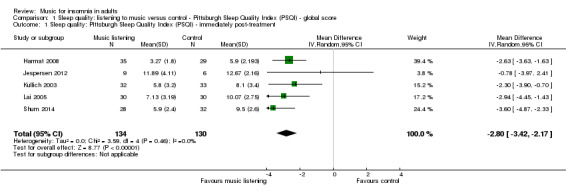
Comparison 1 Sleep quality: listening to music versus control ‐ Pittsburgh Sleep Quality Index (PSQI) ‐ global score, Outcome 1 Sleep quality: Pittsburgh Sleep Quality Index (PSQI) ‐ immediately post‐treatment.
4.
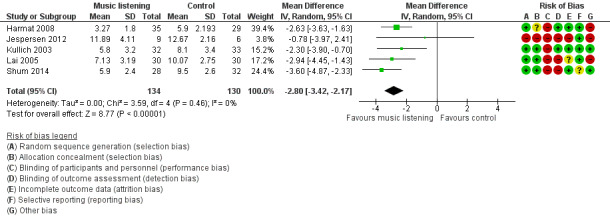
Forest plot of comparison: 1 Sleep quality: listening to music versus control ‐ Pittsburgh Sleep Quality Index (PSQI) ‐ global score, outcome: 1.1 Sleep quality: Pittsburgh Sleep Quality Index (PSQI) ‐ immediately post‐treatment.
Sleep onset latency
One trial, including 50 participants and a three‐day intervention period, measured sleep onset latency with polysomnography (PSG) and a morning questionnaire (Chang 2012). The trial found no evidence of an effect of the intervention on sleep onset latency.
Total sleep time
One trial registered total sleep time with PSG and a morning questionnaire and found no evidence of an effect of the intervention (Chang 2012).
Sleep interruption
One trial measured sleep interruption with PSG and a morning questionnaire (number of awakenings and wake time after sleep onset) (Chang 2012). The trial found no evidence of an effect of the intervention.
Sleep efficiency
Chang 2012 also measured sleep efficiency outcomes with PSG, and found no evidence of an effect of the intervention.
Adverse events
No trial reported a deterioration on a primary outcome or reported any other adverse events.
Secondary outcomes
The secondary outcomes included sleep‐related psychological outcomes (depression, anxiety, and quality of life), physical outcomes (fatigue, daytime sleepiness, and pain), and physiological outcomes (heart rate, heart rate variability, and blood pressure). Only one of these outcomes (i.e. quality of life) was reported in the included trials.
Quality of life
One trial reported an outcome that could be seen as a measure of quality of life. Jespersen 2012 measured the general well‐being of participants with a standardised questionnaire; the outcome was measured before and after the intervention period. They found a significant improvement in the music listening group (P < 0.025), but not in the control group. There were no statistically significant differences detected between the post‐intervention scores of the two groups. The result must be interpreted with caution since the data come from only one trial with a small sample size and high risk of bias.
Subgroup analyses
The included trials enabled us to conduct two of the pre‐defined subgroup analyses. The outcome for both subgroup analyses was sleep quality.
Researcher‐selected music versus participant‐selected music
We explored the influence of music selection, comparing researcher‐selected music (Harmat 2008; Jespersen 2012; Kullich 2003) and participant‐selected music (choice among researcher pre‐selected collection; Lai 2005; Shum 2014). The results of the analysis revealed significant effects on sleep quality regardless of whether music was selected by the researchers (MD ‐2.42; 95% CI ‐3.24 to ‐1.60; Z = 5.80; P < 0.0001; N = 144; Analysis 1.2), or by the participants based on a pre‐selected choice (MD ‐3.35, 95% CI ‐4.28 to ‐2.42; Z = 7.06, P < 0.0001; N = 130). Again, both effects reflected a difference of about one SD between groups, with slightly greater effects in trials that gave participants a choice among pre‐selected music. No significant subgroup differences were found (Figure 5). However, the statistical power available from these five studies was limited, and this may account for our inability to identify potential differences.
1.2. Analysis.
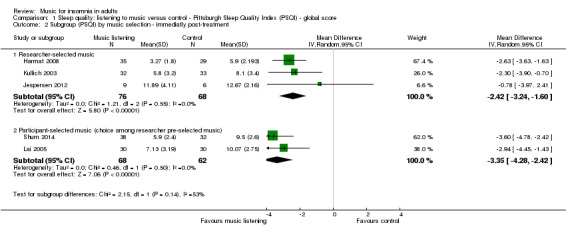
Comparison 1 Sleep quality: listening to music versus control ‐ Pittsburgh Sleep Quality Index (PSQI) ‐ global score, Outcome 2 Subgroup (PSQI) by music selection ‐ immediatly post‐treatment.
5.
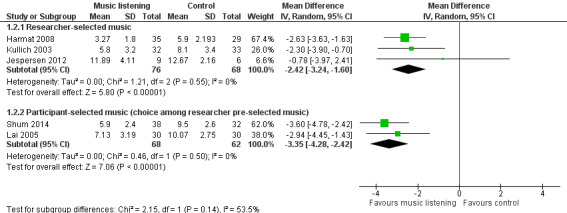
Forest plot of comparison: 1 Sleep quality: listening to music versus control ‐ Pittsburgh Sleep Quality Index (PSQI) ‐ global score, outcome: 1.2 Subgroup (PSQI) by music selection ‐ immediately post‐treatment.
Music listening alone versus music listening and relaxation instructions
Finally, we were able to compare trials that applied music listening alone (Harmat 2008; Jespersen 2012; Shum 2014) to trials that used music listening and relaxation instructions (Kullich 2003; Lai 2005). Again, the results of the analysis revealed significant effects on sleep quality regardless of whether the intervention was applied without relaxation instructions (MD ‐2.85; 95% CI ‐3.92 to ‐1.78; Z = 5.23; P < 0.00001; N = 149; Analysis 1.3) or with relaxation instructions (MD ‐2.64; 95% CI ‐3.74 to ‐1.54; Z = 4.71; P < 0.00001; N = 125), with similar effect sizes. No significant subgroup differences were found (Figure 6), but similar to the above mentioned subgroup analysis, it may be due to lack of statistical power.
1.3. Analysis.
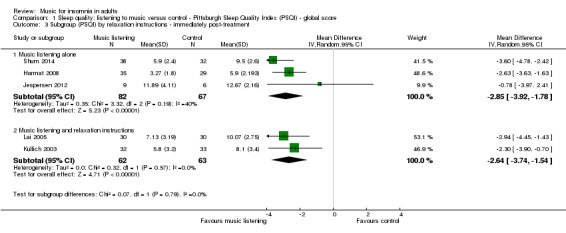
Comparison 1 Sleep quality: listening to music versus control ‐ Pittsburgh Sleep Quality Index (PSQI) ‐ global score, Outcome 3 Subgroup (PSQI) by relaxation instructions ‐ immediately post‐treatment.
6.
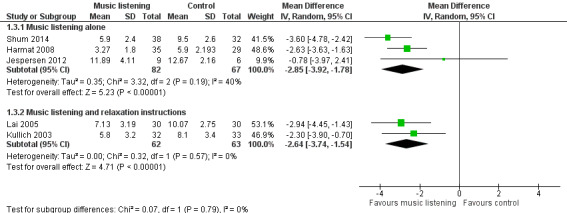
Forest plot of comparison: 1 Sleep quality: listening to music versus control ‐ Pittsburgh Sleep Quality Index (PSQI) ‐ global score, outcome: 1.3 Subgroup (PSQI) by relaxation instructions ‐ immediately post‐treatment.
Sensitivity analyses
We conducted a series of sensitivity analyses to determine the impact of trial quality and risk of bias on the results of the meta‐analysis for the outcome of sleep quality. First, we excluded trials with inadequate methods of random sequence generation (Jespersen 2012). The effect of music listening on sleep quality was slightly enhanced (MD ‐2.88; 95% CI ‐3.52 to ‐2.24; K (number of trials) = 4) compared to the pooled analysis (Analysis 1.1). Second, we excluded trials using inadequate methods of allocation concealment (Harmat 2008; Jespersen 2012). Again, the effect of music listening on sleep quality was slightly enhanced (MD ‐3.05; 95% CI ‐3.88 to ‐2.22, K = 3). Lastly, we excluded trials using inadequate methods of blinding outcome assessment (Jespersen 2012; Lai 2005; Shum 2014). Compared to the pooled analysis; a similar effect was revealed (MD ‐2.54; 95% CI ‐3.38 to ‐1.69; K = 2). In sum, the sensitivity analyses revealed that excluding trials with inadequate randomisation, allocation concealment or blinding of outcome assessment did not change the results of the meta‐analyses.
Discussion
Summary of main results
We found six trials that met the inclusion criteria for this review. These trials evaluated the effect of listening to music for insomnia in adults. Music listening was compared to no treatment or standard care. We conducted a meta‐analysis using a random‐effects model for the primary outcome of sleep quality that was reported by five of the included trials. The meta‐analysis (Analysis 1.1) showed a large effect of about one standard deviation (SD) in favour of the intervention (Figure 4). The results were consistent across the included trials and sensitivity analyses showed that the beneficial effect of the intervention remained unchanged when excluding trials using inadequate methods of (1) random sequence generation (Jespersen 2012), (2) allocation concealment (Harmat 2008; Jespersen 2012), or (3) blinding outcome assessment (Jespersen 2012; Lai 2005; Shum 2014). Subgroup analyses revealed no difference whether (1) the music was selected by research personnel or the participant (Analysis 1.2), or (2) whether music listening was accompanied by relaxation instructions or not (Analysis 1.3). Only one trial reported on the additional primary outcomes and found no evidence of an effect of the intervention on sleep onset latency, total sleep time, sleep interruption or sleep efficiency (Chang 2012). Adverse events were not reported in any of the trials, and only one trial reported any of the secondary outcomes identified as relevant for this review; it found no clear effect on quality of life in the participants listening to music (Jespersen 2012). For an overview of the results see (Table 1).
Overall completeness and applicability of evidence
Outcomes
Only one of the pre‐defined primary outcomes in this review (sleep quality) was reported by more than one trial. This outcome of sleep quality was reported in five of the six trials and measured with the same questionnaire (Pittsburg Sleep Quality Index (PSQI)), giving substantial weight for a meta‐analysis. The fact that people experienced improvement in sleep quality is important, and the improvement is large enough to be considered clinically relevant. As most trials focused narrowly on subjective sleep quality, there is little information on other aspects of sleep that might be affected by the intervention. However, one trial that did report other sleep outcomes, found no effect on 'sleep onset latency', 'total sleep time', 'sleep interruption', or 'sleep efficacy' (Chang 2012). Yet, it is worth noticing that the intervention period of this trial was only three days compared to 21 to 35 days in the other included trials (see duration, dosage, and setting below). It is unclear if these results are related to the short intervention period or the method for measuring sleep. Five of the six included trials used subjective measures of sleep. Only Chang 2012 used objective methods to measure sleep and found shortened stage two sleep and prolonged rapid eye movement (REM) sleep. The percentage of sleep in each sleep stage is a relatively common reported sleep outcome even though it is not included in the reporting standards for polysomnography in insomnia studies (Buysse 2006). Changes in the amount of sleep in each sleep stage are not always easily interpreted, and it was not included in the primary outcomes of this review in order to keep the list of primary outcomes simple and clear. Therefore, these results are not reported in the results section. Since there can be a discrepancy between subjective and objective measures of sleep, it is recommended to document treatment efficacy with multiple outcomes and multiple assessment modalities (Morin 2003). Currently, there is very limited knowledge as to whether listening to music can improve objective measures of sleep.
Only one of the pre‐defined secondary outcomes was reported in any of the trials. This reflects a lack of data on how the music intervention may affect the waking correlates and consequences of insomnia, such as mood, quality of life, daytime fatigue, pain, heart rate or blood pressure. These measures are important for determining effects beyond the reduction of insomnia symptoms. Insomnia is associated with considerable daytime dysfunction and an effective treatment should improve not only sleep, but also daytime functioning.
No trial reported a deterioration on a primary outcome or other adverse events. Even though adverse events were not among the primary outcomes of the individual trials, it is considered unethical not to report any such events. The absence of these reports may therefore support the safety of the intervention.
Population
The trials were heterogenous with regard to participant characteristics. The majority of the included trials did not describe the participants' characteristics in sufficient detail. All participants experienced insomnia as defined in this review as dissatisfaction with the quality, duration or continuity of sleep. However, the studies used different words to describe the condition (insomnia, poor sleep, sleep problems), and all trials relied on the PSQI for the identification of sleep problems. The PSQI is a well‐validated tool to measure sleep problems, with a clear cut‐off score distinguishing good and poor sleepers (Buysse 1989). However, it is not a specific screening tool for insomnia and the exact nature of the sleep problems are not revealed by the global PSQI score. It is therefore unclear if the participants suffered from difficulties initiating sleep, maintaining sleep, non‐restorative sleep or any combination of these. The amount of daytime dysfunction resulting from the insomnia was not described, and only one trial reported information on the duration of the insomnia (Chang 2012). It could be argued that other tools, such as the Insomnia Severity Index (Bastien 2001), would make a better screening tool for insomnia. It is important to note that none of the participants had a clinical diagnosis of an insomnia disorder (primary or secondary insomnia, psychophysiological insomnia, etc.). This means that the results of this review do not give us any information on the effect of the intervention on persons diagnosed with an insomnia disorder. Furthermore, none of the studies report screening for other sleep disorders, and it cannot be excluded that some of the sleep complaints of the participants was due to other sleep disorders such as sleep apnea or restless legs syndrome. Some trials did not give any information on the underlying cause of insomnia; others related insomnia to a wide range of different conditions, such as pain, psychological trauma or old age. Therefore, we cannot draw any conclusions regarding the effect of listening to music on different population groups. In spite of this high population diversity, the effect of the music intervention was consistent, and it may be that the efficacy of the music listening intervention is not dependent on a particular etiology or insomnia subtype. As mentioned in the Description of the condition, insomnia symptoms are associated with a number of disorders and may be seen as a precursor to depression (Baglioni 2011), as a factor affecting the long‐term outcomes in neurological diseases (Mayer 2011), or a factor contributing to risk of falling in the elderly population (Latimer Hill 2007). Early and safe interventions may therefore be of great importance to both healthy and diseased populations.
Intervention
All trials used pre‐recorded music for the intervention, which reflects the common use of music listening in many clinical and at‐home settings. We were interested in the effect of music interventions that can be used by the general population or in clinical settings, and therefore we did not include studies using live music interventions. Most of the included trials used researcher‐selected music without any clear rationale for the choice of the music. Some trials provided information on the specific characteristics of the music, and these features (e.g. slow tempo and low rhythmic accentuation) fit well with the literature describing the characteristics of potentially sedative music (Wigram 2002). Such detailed description of the music should be obligatory when reporting these kinds of trials since they can help clinicians make well‐informed music selections. Still, it is a limitation that almost all trials used only music chosen by the researchers. Musical taste varies widely among individuals and preferences as well as familiarity with the music may influence the efficacy of the intervention. Some trials gave participants a choice, but only among a limited number of pre‐selected music styles. To some degree this does take individual preferences into account and may enhance the participants' sense of control, which can be an important factor, especially in institutional or hospital settings where people can feel disempowered. When exploring the impact of giving participants a choice among pre‐selected music versus the use of researcher‐selected music, we found no difference in the effect on sleep quality (see Analysis 1.2). However, trials comparing the effects of researcher‐selected music to participant‐selected music are lacking. Some trials added relaxation instructions to the music listening intervention, but subgroup analyses showed no statistically significant differences in effect between trials with and without relaxation instructions (see Analysis 1.3). The music interventions used in these kinds of trials are called a number of names, including music listening, music therapy or simply, music. A common distinction is made between music medicine and music therapy, with music therapy involving an active therapeutic process between the patient and therapist, including the use of music (Bruscia 1998). This is not the case in any of the included trials, and the interventions in this review fall within the music medicine domain.
Duration and setting
Based on this review, listening to music daily for three weeks is sufficient to find an improvement of subjective sleep quality only. As described above, the trial using only three days of intervention did not find evidence of an effect of music on measures of 'sleep onset latency', 'total sleep time', 'sleep interruption', or 'sleep efficiency' (Chang 2012). There were too few trials to determine if these results were due to the short intervention period. The relationship between the duration of the intervention and the effect of the intervention remains unclear, and more research is needed to establish optimal duration of music interventions for adults with insomnia. There is also a lack of information on the long term effects of the intervention, since the longest intervention period implemented was 35 days.
In the included trials, music was used daily for about 45 minutes. This frequency and dosage of the intervention seems beneficial, given the reported effects on sleep quality. However, we cannot conclude if changes in these parameters would affect the effect of the intervention. Similarly, there is limited information on the significance of the timing of the intervention, even though most trials reported the use of music at bedtime. In most trials, the intervention was administered by participants in their own homes. This indicates that music listening can be effective as a self‐administered intervention. However, it is important to note that these trials included weekly contact from researchers to ensure compliance. This may be particularly important with elderly populations or populations with comorbid disorders.
Quality of the evidence
All included trials were at high risk of bias on at least one of the rated items, consequently the results of this review need to be interpreted with caution. Due to the nature of the intervention, blinding of the participants was not possible, and only half of the trials reported blinding of outcome assessors. This may result in overestimation of the treatment effects, especially since a self‐report questionnaire was used to assess the main outcome of sleep quality in most trials. A placebo effect cannot be excluded. It will be important to have more studies with objective outcome measures of sleep since these are less sensitive to the placebo effect than subjective measures. Sensitivity analyses revealed no impact of inadequate randomisation, allocation concealment or blinding of outcome assessors on the results. The positive effect on sleep quality was consistent across all trials, with small confidence intervals in most trials. Three trials reported baseline differences in some aspects of the sleep measures, and this may be due to the relatively small sample sizes (mean 52; median 60). For some trials, we received additional methodological and statistical information from the principal investigators, which improved the quality of the review. When summarizing the assessment of risk of bias of individual studies, the results of the sensitivity analyses, and taking into account GRADE judgements of the overall quality of the evidence (see Table 1), the results indicate effectiveness of music listening for improving sleep quality in adults with insomnia symptoms.
Potential biases in the review process
We conducted extensive electronic searches and handsearches, and we contacted first authors and relevant experts for information on unpublished trials. Therefore, it seems unlikely that we missed important trials within this field. However, one can never be completely sure that all trials have been identified.
Agreements and disagreements with other studies or reviews
We found two other systematic reviews on the efficacy of music listening for improvement of sleep quality in the literature (De Niet 2009; Wang 2014). These reviews had different inclusion and exclusion criteria and therefore included a different set of trials. The major difference was the population under review. Both reviews included adults only, but in the trials included by Wang 2014, the participants did not necessarily suffer from insomnia, resulting in a broader range of included trials. The review by De Niet 2009 only included trials in which the participants were adults with sleep complaints. However, it seems that they did not strictly apply this inclusion criteria, since they included one trial in which not all participants had poor sleep (Hérnandez‐Ruíz 2005) and one trial with no clear documentation of the participants' sleep problems (Zimmerman 1996). These variations result in differences in the trials included in the reviews. De Niet 2009 included five trials (N = 308); three of these are also included in the present review (Harmat 2008; Kullich 2003; Lai 2005). The remaining trials included in this review were not published in 2009. Wang 2014 included 10 trials (N = 557); four of these are also included in this review (Chang 2012; Harmat 2008; Kullich 2003; Lai 2005). Both reviews included meta‐analyses with sleep quality as the primary outcome, and they found statistically significant moderate effect sizes consistent with the results of this review. The present review adds to the robustness of the findings by following rigorous methodology, including an extensive search strategy, clear inclusion criteria, and careful assessment and reporting of risk of bias.
Authors' conclusions
Implications for practice.
The findings of the meta‐analysis suggest that listening to music may improve sleep quality in different populations experiencing insomnia symptoms. Furthermore, the results indicate that the intervention is safe and easy to administer. No conclusions can be drawn on the effect of music listening on other aspects of sleep or on related physiological and psychological aspects of daytime function, since no trials or only single trials reported these outcomes. More research is needed to clarify the effect of the intervention on outcomes beyond self‐reports of sleep quality. Since the studies report limited information on the nature of participants' sleep problems, it is not possible to draw any conclusions with regard to the effect on insomnia subtypes such as difficulties with sleep initiation, sleep maintenance or non‐restorative sleep. None of the participants were diagnosed with insomnia, and we do not know if listening to music can improve sleep in adults diagnosed with insomnia disorder.
All included trials used music that was characterized as sedative or relaxing. However, these included a number of different musical styles (e.g. classical, new age, jazz, etc.) and at this point, it is not clear if some types of music may be more effective than others. In the literature, it is often recommended that participants are allowed to choose their own preferred music. In this review, there was no difference in the effect on sleep quality between trials using researcher‐selected music and trials giving the participants a choice among a number pre‐selected types of music. Very few participants were offered the possibility to bring their own preferred music, and the effect of purely participant‐selected music could not be investigated.
Implications for research.
More high‐quality randomised controlled trials are needed to assess the effectiveness of music listening for treating insomnia. Future trials need to pay close attention to reducing risk of bias. Randomisation needs to be properly concealed, and although blinding of participants is not possible with a music intervention, blinding of researchers and outcome assessors should be prioritised to minimise performance and detection biases.
Future research should consider a wider range of outcomes. In particular, more research should include objective measures of sleep, such as polysomnography and actigraphy, that are less sensitive to detection bias. The use of objective measures of sleep would reduce the impact of any placebo effect. Furthermore, there is a lack of knowledge of the effect of listening to music on daytime consequences and waking correlates of insomnia. It is important to know if the reported changes in sleep patterns or sleep quality are sufficient to affect daytime function. Furthermore, longer follow‐up periods are important to genuinely establish the effectiveness of music and its long‐term effect.
More research is needed to establish the effect of the intervention on different insomnia groups. Insomnia is a highly heterogenous disease with different aetiology and severity. Future trials should take care to define and appropriately measure sleep disturbances and provide detailed information on the cause, duration and severity of symptoms, as well as any comorbid conditions. Participants should be screened for other sleep disorders to clarify the nature of the sleep complaint. It is also recommended that researchers employ well‐defined criteria for insomnia such as the diagnostic criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM) or International Classification of Sleep Disorders (ICSD). This would improve the precision of the clinical diagnosis and hence improve comparability across trials.
The music therapy literature recommends that music used for sedative purposes should be characterised by a slow tempo and an absence of abrupt changes and rhythmic complexity (Wigram 2002). These recommendations are supported by experimental research in the field of music psychology, but more controlled clinical trials are needed to examine which aspects of music are important to achieve an improvement in sleep. In addition, the relationship between the objective characteristics of the music and the subjective preferences of the individual remain unclear, and more trials are needed to investigate potential differences in effect between music selected by the researcher and that selected by the participant. Another aspect of the intervention that remains unclear is the optimal frequency, timing, and duration of the intervention. Further research into these domains is important for assessing the effectiveness of the intervention and for providing the best treatment options for people with insomnia.
What's new
| Date | Event | Description |
|---|---|---|
| 27 November 2015 | Amended | Typographical error corrected |
Acknowledgements
We would like to thank the editorial team of the Cochrane Developmental, Psychosocial and Learning Problems Group (CDPLPG) for their excellent advice and support. We are also grateful to research librarian Edith Clausen for her assistance with the search process and to PhD student Mia Dong for translations. We thank Dr. Kullich, Dr. Bernatzky, and Dr. Harmat for kindly providing additional information about their trials.
The Center for Music in the Brain is funded by the Danish National Research Foundation (DNRF117).
Appendices
Appendix 1. Search strategies
Cochrane Central Register of Controlled Trials (CENTRAL)
CENTRAL, 2014 (5), searched 22 May 2015 [67 records]
#1 MeSH descriptor: [Music] explode all trees #2 MeSH descriptor: [Music Therapy] explode all trees #3 music* #4 (#1 or #2 or #3) #5 MeSH descriptor: [Sleep] explode all trees #6 MeSH descriptor: [Sleep Disorders] explode all trees #7 sleep* #8 insomnia* #9 wakeful* #10 sleepless* #11 dyssomn* #12 (#5 or #6 or #7 or #8 or #9 or #10 or #11) #13 (#4 and #12)
PubMed (ncbi.nlm.nih.gov/pubmed)
PubMed, 1950 to current, searched 22 May 2015 [91 records]
#1 Music [Mesh] #2 Music therapy [Mesh] #3 music* #4 (#1 OR #2 OR #3) #5 Sleep [Mesh] #6 Sleep disorders [Mesh] #7 sleep* #8 insomnia* #9 wakeful* #10 sleepless* #11 dyssomn* #12 (#5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11) #13 randomized controlled trial [Publication Type] #14 controlled clinical trial [Publication Type] #15 clinical trial [Publication Type] #16 Clinical Trials as Topic [Mesh] #17 randomized [Title/Abstract] #18 placebo [Title/Abstract] #19 randomly [Title/Abstract] #20 trial [Title/Abstract] #21 (#13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20) #22 (#4 AND #12 AND #21)
Embase
Embase (Elsevier), 1980 to current, searched 22 May 2015 [194 records]
#1. 'music'/exp #2. 'music therapy'/exp #3. music* #4. 'music'/exp OR 'music therapy'/exp OR music* #5. 'sleep'/exp #6. 'sleep disorder'/exp #7. sleep* #8. insomnia* #9. wakeful* #10. sleepless* #11. dyssomn* #12. 'sleep'/exp OR 'sleep disorder'/exp OR sleep* OR insomnia* OR wakeful* OR sleepless* OR dyssomn* #13. 'randomized controlled trial'/de #14. 'controlled clinical trial'/de #15. 'clinical trial'/de #16. 'clinical trial (topic)'/exp #17. randomized:ab #18. placebo:ab #19. randomly:ab #20. trial:ab #21. 'randomized controlled trial'/de OR 'controlled clinical trial'/de OR 'clinical trial'/de OR 'clinical trial (topic)'/exp OR randomized:ab OR placebo:ab OR randomly:ab OR trial:ab #22. 'music'/exp OR 'music therapy'/exp OR music* AND ('sleep'/exp OR 'sleep disorder'/exp OR sleep* OR insomnia* OR wakeful* OR sleepless* OR dyssomn*) AND ('randomized controlled trial'/de OR 'controlled clinical trial'/de OR 'clinical trial'/de OR 'clinical trial (topic)'/exp OR randomized:ab OR placebo:ab OR randomly:ab OR trial:ab)
Cumulative Index to Nursing and Allied Health Literature (CINAHL)
CINAHL (EBSCOhost), 1982 to current, searched 22 May 2015 [177 records]
S1 MH music S2 MH music therapy S3 music* S4 (S1 OR S2 OR S3) S5 MH sleep S6 MH sleep disorders S7 sleep* S8 insomnia* S9 wakeful* S10 sleepless* S11 dyssomn* S12 (S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11) S13 (S4 AND S12)
PsycINFO
PsycINFO (Proquest), 1967 to current, searched 22 May 2015 [55 records]
S1 SU.EXACT.EXPLODE("Music") S2 SU.EXACT.EXPLODE("Music Therapy") S3 music* S4 SU.EXACT.EXPLODE("Music") OR SU.EXACT.EXPLODE("Music Therapy") OR music* S5 SU.EXACT.EXPLODE("Sleep") S6 SU.EXACT.EXPLODE("Sleep Disorders") S7 sleep* S8 insomnia* S9 wakeful* S10 sleepless* S11 dyssomn* S12 SU.EXACT.EXPLODE("Sleep") OR SU.EXACT.EXPLODE("Sleep Disorders") OR sleep* OR insomnia* OR wakeful* OR sleepless* OR dyssomn* S13 SU.EXACT.EXPLODE("Clinical Trials") S14 ab(randomized) OR ti(randomized) S15 ab(placebo) OR ti(placebo) S16 ab(randomly) OR ti(randomly) S17 ab(trial) OR ti(trial) S18 SU.EXACT.EXPLODE("Clinical Trials") OR (ab(randomized) OR ti(randomized)) OR (ab(placebo) OR ti(placebo)) OR (ab(randomly) OR ti(randomly)) OR (ab(trial) OR ti(trial)) S19 (SU.EXACT.EXPLODE("Music") OR SU.EXACT.EXPLODE("Music Therapy") OR music*) AND (SU.EXACT.EXPLODE("Sleep") OR SU.EXACT.EXPLODE("Sleep Disorders") OR sleep* OR insomnia* OR wakeful* OR sleepless* OR dyssomn*) AND (SU.EXACT.EXPLODE("Clinical Trials") OR (ab(randomized) OR ti(randomized)) OR (ab(placebo) OR ti(placebo)) OR (ab(randomly) OR ti(randomly)) OR (ab(trial) OR ti(trial)))
Web of Science databases
Science Citation Index Expanded, Social Sciences Citation Index and Arts and Humanities Citation Index , 1970 to current Conference Proceedings Citation Index ‐ Science and Conference Proceedings Citation Index ‐ Social Science and Humanities, 1990 to current
Searched 22 May 2015 [69 records]
#1 TOPIC: (music*) #2 TOPIC: (sleep*) #3 TOPIC: (insomnia*) #4 TOPIC: (wakeful*) #5 TOPIC: (sleepless*) #6 TOPIC: (dyssomn*) #7 (#2 OR #3 OR #4 OR #5 OR #6) #8 TOPIC: (randomized controlled trial) #9 TOPIC: (controlled clinical trial) #10 TOPIC: (clinical trial) #11 TOPIC: (trial) #12 TITLE: (randomized) #13 TITLE: (placebo) #14 TITLE: (randomly) #15 TITLE: (trial) #16 (#8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15) #17 (#1 AND #7 AND #16)
SCOPUS
SCOPUS (Elsevier), 1960 to current, searched 22 May 2015 [178 records]
1 TITLE‐ABS‐KEY(music*) 2 TITLE‐ABS‐KEY(sleep*) 3 TITLE‐ABS‐KEY(insomnia*) 4 TITLE‐ABS‐KEY(wakeful*) 5 TITLE‐ABS‐KEY(sleepless*) 6 TITLE‐ABS‐KEY(dyssomn*) 7 (TITLE‐ABS‐KEY(sleep*)) OR (TITLE‐ABS‐KEY(insomnia*)) OR (TITLE‐ABS‐KEY(wakeful*)) OR (TITLEABS‐KEY(sleepless*)) OR (TITLE‐ABS‐KEY(dyssomn*)) 8 TITLE‐ABS‐KEY(trial*) 9 TITLE‐ABS‐KEY(randomized) 10 TITLE‐ABS‐KEY(randomly) 11 TITLE‐ABS‐KEY(placebo) 12 (TITLE‐ABS‐KEY(trial*)) OR (TITLE‐ABS‐KEY(randomized)) OR (TITLE‐ABS‐KEY(randomly)) OR (TITLEABS‐KEY(placebo)) 13 (TITLE‐ABS‐KEY(music*)) AND ((TITLE‐ABS‐KEY(sleep*)) OR (TITLE‐ABS‐KEY(insomnia*)) OR (TITLEABS‐KEY(wakeful*)) OR (TITLE‐ABS‐KEY(sleepless*)) OR (TITLE‐ABS‐KEY(dyssomn*))) AND ((TITLEABS‐KEY(trial*)) OR (TITLE‐ABS‐KEY(randomized)) OR (TITLE‐ABS‐KEY(randomly)) OR (TITLEABS‐KEY(placebo)))
Répertoire International de Littérature Musicale (RILM)
RILM (EBSCOhost), 1969 to current, searched 22 May 2015 [n = 56 records]
S1 music* S2 sleep* S3 insomnia* S4 (S2 OR S3) S5 SU therapy S6 trial* S7 TI randomized OR AB randomized S8 (S5 OR S6 OR S7) S9 (S1 AND S4 AND S8)
ClinicalTrials.gov (clinicaltrials.gov/)
ClinicalTrials.gov, searched 22 May 2015 [n = 34 records]
music* AND (sleep* OR insomnia*)
Current Controlled Trials (controlled‐trials.com)
Current Controlled Trials, searched 22 May 2015 [n = 3 records]
music* AND (sleep* OR insomnia*)
Appendix 2. Handsearched journals
Australian Journal of Music Therapy (1990 to 2014, vol 25).
British Journal of Music Therapy (1987 to December 2014, vol 28 (2)).
Canadian Journal of Music Therapy (1993 to 2014, vol 20 (1)).
New Zealand Journal of Music Therapy (2010 to 2013, vol 11).
Nordic Journal of Music Therapy (1992 to May 2015, vol 24 (3)).
Music and Medicine (2009 to April 2015, vol 7(2)).
Music Therapy Perspectives (2004 to 2014, vol 32 (2)).
Music Therapy Today (online) (2001 to 2014, vol 10(1)).
Voices (online) (2001 to 2015, vol 15(2)).
The International Journal of Arts Medicine (1991 to 1999).
Journal of Music Therapy (1980 to Fall 2014, vol 51(3)).
The Arts in Psychotherapy (1980 to April 2015, vol 43).
Musik‐,Tanz‐ und Kunsttherapie (German) (1995 to January 2014, vol 25(1)).
Musiktherapeutische Umschau (German) (1980 to 2014, vol 35(4)).
Musik und Gesundsein (German) (2011 to 2015, vol. 27).
Appendix 3. Additional methods archived for future updates of this review
| Analysis | Methods |
| Measures of treatment effect |
Dichotomous data For dichotomous data, we will present the results as summary odd ratios (OR) with 95% confidence intervals (CI). Continuous data The standardized mean difference (SMD) will be used to combine trials that measure the same outcome, but use different scales. All outcomes will be presented with 95% CIs. If a trial provided multiple interchangeable measures of the same construct at the same time point, we will calculate the average SMD across these outcomes and the average of their estimated variances. Where trials report the same outcomes using continuous and dichotomous measures, we will re‐express ORs as SMDs allowing dichotomous and continuous data to be pooled together as described in section nine of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Ordinal data Ordinal data measured on shorter scales will be analysed as dichotomous data by combining categories, and the intervention effect will be expressed using OR. |
| Unit of analysis issues |
Cluster‐randomised trials We anticipate that trials using clustered randomisation will have controlled for clustering effects. In case of doubt, we will contact the first authors to ask for individual participant data to calculate an estimate of the intracluster correlation coefficient (ICC). If this is not possible, we will obtain external estimates of the ICC from a similar trial or from a study of a similar population as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). When the ICC is established, we will use it to reanalyse the trial data. If ICCs from other sources are used, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC Cross‐over trials Cross‐over trials will be analysed using combined data from all study periods, or using first period data if combined data is not available Trials with more than two treatment arms If more than one of the interventions is a music intervention, and there is sufficient information in the trial to assess the similarity of the interventions, we will combine similar music interventions to allow for a single pair‐wise comparison |
| Dealing with missing data | We will explore the impact of including studies with high levels of missing data by performing sensitivity analyses based on consideration of best and worst case scenarios. The potential impact of missing data on the findings of the review will be addressed in the 'Discussion' section of the review |
| Assessment of heterogeneity | Where significant heterogeneity is present, we intend to investigate it by conducting a subgroup analysis based on the participant clinical characteristics and interventions of the included studies (see subsection on 'Subgroup analyses' below) |
| Assessment of reporting bias | If sufficient study data are available for individual outcomes, we will draw and inspect funnel plots for evidence of reporting or publication bias. We will assess funnel plot asymmetry visually and statistically by means of the Bee and Mazumdar (Begg 1994) and the Egger et al tests (Egger 1997), if sufficient studies are available; ten or more studies are recommended. If asymmetry is suggested by visual assessment or detected in any of these tests, we will perform exploratory analyses to investigate if it reflects a publication bias or a true relationship between trial size and effect size |
| Subgroup analyses | We will conduct the following subgroup analyses.
|
| Sensitivity analysis | We will conduct a sensitivity analysis excluding trials using inadequate methods of blinding personnel |
Data and analyses
Comparison 1. Sleep quality: listening to music versus control ‐ Pittsburgh Sleep Quality Index (PSQI) ‐ global score.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Sleep quality: Pittsburgh Sleep Quality Index (PSQI) ‐ immediately post‐treatment | 5 | 264 | Mean Difference (IV, Random, 95% CI) | ‐2.80 [‐3.42, ‐2.17] |
| 2 Subgroup (PSQI) by music selection ‐ immediatly post‐treatment | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Researcher‐selected music | 3 | 144 | Mean Difference (IV, Random, 95% CI) | ‐2.42 [‐3.24, ‐1.60] |
| 2.2 Participant‐selected music (choice among researcher pre‐selected music) | 2 | 130 | Mean Difference (IV, Random, 95% CI) | ‐3.35 [‐4.28, ‐2.42] |
| 3 Subgroup (PSQI) by relaxation instructions ‐ immediately post‐treatment | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Music listening alone | 3 | 149 | Mean Difference (IV, Random, 95% CI) | ‐2.85 [‐3.92, ‐1.78] |
| 3.2 Music listening and relaxation instructions | 2 | 125 | Mean Difference (IV, Random, 95% CI) | ‐2.64 [‐3.74, ‐1.54] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Chang 2012.
| Methods | Randomised controlled trial Design: 2‐arm parallel group design Blindness: single‐blinded, technician scoring PSG and researchers responsible for statistical analysis not aware of group allocation |
|
| Participants | Adults who experienced insomnia for at least 1 month, documented by a PSQI score > 5 N: 50 Age: mean 32 (SD 11) years; range 22 to 58 years Sex: 3 males; 47 females Setting: sleep laboratory Country: Taiwan |
|
| Interventions |
Music characteristics: Rural Spring Field, Woman under the Moon (Chinese music), Going Home (Czech music), Destiny, Heart Lotus (Taiwanese music), and Memory (composed by the authors). Tempos ranged from 60 to 85 bpm, minor tonalities, smooth melodies, and no dramatic changes in volume or rhythm. The music was expected to be familiar to participants Length of sessions: 45 minutes Frequency of sessions: daily at bedtime Duration of intervention period: 3 consecutive days |
|
| Outcomes |
We contacted the author 16 December 2014 to obtain data on the raw post‐scores, but we have not yet received a reply |
|
| Notes | Trial start and end dates: the trial was conducted from May 2010 to June 2011 Funding sources: the trial was funded by the National Science Counsil, Taiwan |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomly assigned (...), using the drawing of lots" (Chang 2012; p 924) |
| Allocation concealment (selection bias) | Low risk | "All lots (labels) are packed in a jar that was prepared by another person. Researchers therefore did not know beforehand which group each participant would be assigned to" (Chang 2012; p 924) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Due to the nature of the intervention, blinding of participants was not possible. It is unclear if this affected the objective sleep measures, but likely that it affected the subjective measures of sleep. Blinding of personnel at the sleep laboratory was not reported. Since the intervention was music, it is likely that they were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The technician scoring the polysomnography and the researchers doing the statistical analyses were not aware to which group the data belonged |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts and no missing data |
| Selective reporting (reporting bias) | Unclear risk | We found no published protocol on this study. Sleep efficiency, based on a self‐report questionnaire, was not reported. All other measures of interest were included in the analysis |
| Other bias | High risk | Baseline differences in measures of depression and self‐reported number of awakenings, with the music group experiencing significantly more depression and arousals than the control group |
Harmat 2008.
| Methods | Randomised controlled trial Design: 3‐arm parallel group design Blindness: single blinded, group allocation was coded for the person doing the statistics (Harmat 2014 [pers comm]) |
|
| Participants | Students with poor sleep documented by PSQI scores > 5 N: 94 (64 included in this review) Age: mean 22.6 (SD 2.9) years; range 19 to 28 years Sex: 21 males; 73 females Setting: homes of the participants Country: Hungary |
|
| Interventions |
Music characteristics: The Most Relaxing Classical (2 CD, Edited by Virgin 1999). Popular pieces from Baroque to Romantic Length of sessions: 45 minutes Frequency of sessions: daily at bedtime Duration of intervention period: 3 weeks |
|
| Outcomes |
|
|
| Notes | Trial start and end dates: the trial was conducted in 2006 Funding sources: the work was supported by the Hungarian Ministry of Education, the National Research Fund (Hungary), the Ferenc Faludi Academy, and the János Bolyai Research Fellowship of the Hungarian Academy of Sciences |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised using a computerised randomisation table and variable block randomisation |
| Allocation concealment (selection bias) | Unclear risk | No information on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Due to the nature of the intervention, blinding of participants was not possible. It is likely that this affected the subjective outcome measures. The intervention was used at home with no personnel involved |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The group allocation was coded (Harmat 2014 [pers comm]) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition in the included groups (Harmat 2014 [pers comm]) |
| Selective reporting (reporting bias) | Low risk | We found no published protocol on this study. Outcomes from the no‐intervention control group were not reported in the publication, but were provided by the first author at request (Harmat 2014 [pers comm]). These data did not alter the results or conclusions of the trial |
| Other bias | High risk | The trial design involved a difference between the intervention and control group. The intervention group registered sleep quality once a week, whereas the control group only registered sleep quality before and after the intervention period. In addition, the intervention group, but not the control group, was contacted weekly by telephone to assess compliance with the protocol |
Jespersen 2012.
| Methods | Quasi‐randomised controlled trial Design: 2‐arm parallel group design Blindness: not blinded |
|
| Participants | Traumatised refugees with sleep problems documented by PSQI score > 5 N: 15 (19 included; 4 dropped out) Age: mean 37 years; range 26 to 57 Sex: 6 males; 9 females Setting: homes of the participants Country: Denmark |
|
| Interventions |
Music characteristics: MusiCure compilation 'Inducing Sleep' (Tracks 1, 2, and 5; Eje 2004). Tempo 52 bpm, stable dynamic contour and repetitive structure Instruments: piano, harp, guitar, oboe, cello, and nature sounds (waves and birdsong) Length of sessions: 60 minutes Frequency of sessions: daily at bedtime Duration of intervention period: 3 weeks |
|
| Outcomes |
|
|
| Notes | Trial start and end dates: the trial was conducted in 2010 Funding sources: the work was supported by Trygfonden and the Danish Ministry for Refugee, Immigration and Integration Affairs |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Used an alternation procedure based on gender |
| Allocation concealment (selection bias) | High risk | Allocation could be foreseen due to the alternation procedure |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Due to the nature of the intervention, blinding of participants was not possible. It is likely that this affected the subjective outcome measures. The intervention was used at home with no personnel involved |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 4 participants dropped out. Data from dropouts were excluded in the final analyses. No missing data |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported and included in the analysis |
| Other bias | High risk | Baseline difference in sleep quality with the music group experiencing more sleep problems than the control group |
Kullich 2003.
| Methods | Randomised using a computer‐based randomisation list (Kullich 2014b [pers comm]) Design: 2‐arm parallel group design Blindness: single blinded. Data assessment performed by non‐trial personnel (Kullich 2014b [pers comm]) |
|
| Participants | Adults with low back pain and sleep difficulties (PSQI scores > 5) N: 65 Age: mean age reported by group. Music group mean age 47.0 (SD 9.7); control group mean age 49.7 (SD 7.9); range 21 to 68 Sex: 41 males; 24 females Setting: rehabilitation facility Country: Austria |
|
| Interventions |
Music characteristics: CD 'Entspannung bei Schmerzen' (Mentalis Verlag, ISBN: 3‐932239‐95‐4). No further information provided Length of sessions: 25 minutes Frequency of sessions: once a day, no time specified Duration of intervention period: 3 weeks +/‐ 2 days |
|
| Outcomes |
|
|
| Notes | Trial start and end dates: there is no information on when the trial was conducted Funding sources: the trial was supported by the Ludwig Boltzmann Institut (Saalfelden), the Herbert von Karajan Centrum (Wien), Salzburg University, and the Mozart University (Salzburg) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐based randomisation list (Kullich 2014b [pers comm]) |
| Allocation concealment (selection bias) | Low risk | Allocation done by another person (not the doctor) who referred the participant to the trial (Kullich 2014b [pers comm]) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Due to the nature of the intervention, blinding of participants was not possible. It is likely that this affected the subjective measures of sleep. There was no information on the blinding of the personnel at the rehabilitation facility |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Data were assessed by non‐trial personnel (secretary). Data analysis was performed by a researcher who was aware of group allocation, but did not know the patients (Kullich 2014b [pers comm]) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition or missing data (Kullich 2014b [pers comm]) |
| Selective reporting (reporting bias) | Low risk | We found no published protocol on this study, but there was no indication of selective reporting. Measures on sleep quality were reported without SDs in the publication, but these were provided by the first author on request (Kullich 2014a [pers comm]). These data did not alter the conclusions of the trial |
| Other bias | Low risk | No other risk of bias detected |
Lai 2005.
| Methods | Randomised controlled trial Design: 2‐arm parallel group design Blindness: not blinded |
|
| Participants | Older adults with sleep problems documented by PSQI scores > 5 N: 60 Age: mean 67 (SD 5) years; range 60 to 83 Sex: not reported Setting: homes of the participants Country: Taiwan |
|
| Interventions |
Music characteristics: the choices of music included 5 types of Western music (new age, eclectic, popular oldies, classical, and slow jazz), and 1 type of Chinese music (folk music). Tempos ranged from 60 to 80 bpm without accented beats, percussive characteristics or syncopation. The music was expected to be familiar to the participants Length of sessions: 45 minutes Frequency of sessions: daily at bedtime Duration of intervention period: 3 weeks |
|
| Outcomes |
|
|
| Notes | Trial start and end date: the trial was conducted in 2000 Funding sources: no information provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Permuted block randomisation with sealed envelopes stratified on gender |
| Allocation concealment (selection bias) | Low risk | "The envelopes were prepared by a different person so that the investigator (first author) was blind to block size and order of assignment" (Lai 2005; p 235) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Due to the nature of the intervention, blinding of participants was not possible. It is likely that this affected the subjective outcome measures. The intervention was used at home with no personnel involved |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear information on attrition. One man was withdrawn due to hospitalisation. No information on completeness of data |
| Selective reporting (reporting bias) | Low risk | We found no published protocol on this study, but there was no indication of selective reporting |
| Other bias | High risk | Baseline differences in 2 sleep component scores with the music group experiencing shorter sleep duration and more daytime dysfunction |
Shum 2014.
| Methods | Randomised controlled trial Design: 2‐arm parallel group design Blindness: not blinded |
|
| Participants | Older adults with poor sleep quality, documented by PSQI scores > 5 N: 60 Age: mean 64 years; range 57 to 68 years Sex: 20 males; 40 females Setting: homes of the participants Country: Singapore |
|
| Interventions |
Music characteristics: the 4 types of researcher selected music included 1) Western classical (Bach: Allemande, Sarabande; Mozart: Romance from Eine kleine Nachtmusik; Chopin: Nocturne); 2), Chinese classical (Spring River in the Moonlight; Variation on Yang Pass); 3) New Age (Shizuki, Lord of the Wind); and 4) Jazz (Everlasting; Winter Wonderland; In Love in Vain). All compositions were soft, with no lyrics, and tempos ranging from 60 to 80 bpm Length of sessions: 40 minutes Frequency of sessions: once a day, no time specified Duration of intervention period: 5 weeks |
|
| Outcomes |
|
|
| Notes | Trial start and end dates: the trial was conducted from January 2012 to January 2013 Funding sources: no information provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Two cards were put inside a bag in each draw, with one labelled as "intervention" and the other as "control". Each participant was asked to draw one card from the bag to allocate him or her into either the intervention or control group" (Shum 2014; p 51) |
| Allocation concealment (selection bias) | Low risk | The above mentioned procedure makes it unlikely that the allocation was foreseen |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Due to the nature of the intervention, blinding of participants was not possible. It is likely that this affected the subjective outcome measures. The intervention was used at home with no personnel involved |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts and no missing data |
| Selective reporting (reporting bias) | Unclear risk | We found no published protocol on this study. The primary outcome of sleep quality (PSQI ‐ global scale) was fully reported, but the results of the component scores were not reported, which is common in other trials using the PSQI |
| Other bias | Low risk | No other risk of bias detected |
BDI: Beck Depression Inventory. BPM: beats per minute. CD: compact disc. GEE: generalised estimating equation. PSG: polysomnograpgh. PSQI: Pittsburgh Sleep Quality Index. REM: rapid eye movement. SD: standard deviation. TAU: treatment‐as‐usual. TST: total sleep time.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abdollahnejad 2006 | Not RCT or qRCT (no control group) |
| Beattie 2013 | Intervention not music listening (active music making (choir)) |
| Blanaru 2012 | Comparison of 2 interventions (music listening versus muscle relaxation techniques) |
| Bloch 2010 | Not RCT or qRCT (within‐subject design) |
| Bonebreak 1996 | Not a clinical trial (reflections on practice) |
| Bonnet 2000 | Not a clinical trial (experimental trial investigating the impact of music on wakefulness) |
| Bozcuk 2006 | Not RCT or qRCT (no control group) |
| Breitenfeld 1992 | Not RCT or qRCT (no control group) |
| Chan 2010 | Participants not adults with insomnia (not all participants had insomnia. No inclusion criteria of insomnia and PSQI < 5) |
| Chen 2014 | Participants not adults with insomnia (young adults with different sleep latencies. Poor sleepers (PSQI < 5) excluded) |
| De Niet 2010 | Not RCT or qRCT (no randomisation) |
| Demi̇rbağ 2014 | Intervention not music listening (intervention a combination of music, massage, and aromatherapy) |
| Deshmukh 2009 | Comparison of 2 interventions (music listening versus hypnotic medications) |
| Dorn 2014 | Participants not adults with insomnia (infants) |
| DuRousseau 2011 | Not RCT or qRCT (no randomisation) |
| Field 1999 | Participants not adults with insomnia (children) |
| Gao 2014 | Intervention not music listening (comprehensive sleep management including music) |
| Garunkstiene 2014 | Participants not adults with insomnia (infants) |
| Gitanjali 1998 | Not RCT or qRCT (no randomisation). Participants not adults with insomnia (healthy volunteers) |
| Hu 2015 | Participants not adults with insomnia (ICU patients with no documentation of insomnia) |
| Hérnandez‐Ruíz 2005 | Participants not adults with insomnia (some participants were 'good sleepers') |
| Iwaki 2003 | Not RCT or qRCT (no randomisation). Participants not adults with insomnia (healthy university students who normally listened to music at bedtime) |
| Johnson 2003 | Not RCT or qRCT (no control group) |
| Kayumov 2003 | Comparison of 2 interventions (individualized versus non‐individualized 'brain music') |
| Koenig 2013 | Participants not adults with insomnia (healthy university students with no sleep problems) |
| Lai 2012 | Comparison of 2 interventions (live music with nursing presence versus pre‐recorded music) |
| Lai 2015 | Intervention not music listening (music videos) |
| Lazic 2007 | Participants not adults with insomnia (healthy university students) |
| Levin 1998 | Not RCT or qRCT (no randomisation). Comparison of 2 interventions (individualized versus non‐individualized 'brain music') |
| Lindenmuth 1992 | Not RCT or qRCT (within‐subject design comparing healthy adults of old age to older adults with senile dementia of the Alzheimer type) |
| Liu 2006 | Intervention not music listening (vibroacustic intervention) |
| Loewy 2005 | Participants not adults with insomnia (children) |
| Loewy 2013 | Participants not adults with insomnia (infants) |
| Lü 2008 | Not RCT or qRCT (no control group) |
| Ma 2004 | Participants not adults with insomnia (pre‐operative patients with no documentation of insomnia) |
| Mandel 2007 | No sleep outcome measure |
| Mornhinweg 1995 | Not RCT or qRCT (no control group) |
| Naghdi 2015 | Not RCT or qRCT (no control group) |
| Oxtoby 2013 | Participants not adults with insomnia (university students. Around half the participants experienced no sleep problems) |
| Picard 2014 | Not RCT or qRCT (no control group) |
| Reinhardt 1999 | No sleep outcome measure (sleep only registered in intervention group, not control group) |
| Renzi 2000 | Participants not adults with insomnia (post‐operative patients with no documentation of insomnia) |
| Robinson 2005 | Not RCT or qRCT (no control group). Intervention not music listening (combination of interventions, including back rubs, warm drinks, aroma therapy, and relaxation music) |
| Ryu 2012 | Participants not adults with insomnia (patients at cardiac care unit with no documentation of insomnia) |
| Sithinamsuwan 2012 | Participants not adults with insomnia (some participants were 'good sleepers' with PSQI scores < 5) |
| Skogar 2013 | Comparison of 2 interventions (music listening versus tactile touch) |
| Smith 2004 | Not a clinical trial (experimental trial testing the Attentional Behavioral Cognitive (ABC) relaxation theory) |
| Street 2014 | Not RCT or qRCT (no control group) |
| Su 2013 | Participants not adults with insomnia (patients at intensive care unit with unclear documentation of insomnia) |
| Sørensen 2005 | Not RCT or qRCT (no control group) |
| Tan 2004 | Participants not adults with insomnia (children) |
| Tegeler 2012 | Intervention not music listening (feedback of neural EEG‐activity using single tones derived through mathematical algorithms) |
| Wormit 2012 | Not RCT or qRCT (no control group). Intervention not music listening (active music therapy) |
| Zimmerman 1996 | Participants not adults with insomnia (pre‐operative patients with no documentation of insomnia) |
| Ziv 2008 | Comparison of 2 interventions (music listening versus progressive muscular relaxation) |
EEG: electroencephalography. PSQI: Pittsburgh Sleep Quality Index. qRCT: quasi‐randomised controlled trial. RCT: randomised controlled trial.
Characteristics of studies awaiting assessment [ordered by study ID]
Miller 2002.
| Methods | Randomised controlled trial |
| Participants | Post‐operative patients |
| Interventions |
|
| Outcomes | Sleep quality (PSQI) Well‐being Consumption of analgesics, hypnotics, and sedatives |
| Notes | This is an unpublished trial. On 9 September 2014, we requested further information from the author, but have yet to receive a response |
PSQI: Pittsburgh Sleep Quality Index.
Characteristics of ongoing studies [ordered by study ID]
NCT02321826.
| Trial name or title | Music for insomnia |
| Methods | Randomised controlled trial |
| Participants | Adults with insomnia |
| Interventions |
|
| Outcomes | Subjective sleep quality (PSQI) and objective sleep measures (PSG + actigraphy) |
| Starting date | February 2015 |
| Contact information | kira@cfin.au.dk |
| Notes |
NCT02376686.
| Trial name or title | Music intervention in the treatment of sleep disorders for depressed patients |
| Methods | Randomised controlled trial |
| Participants | Inpatients with depression and insomnia |
| Interventions |
|
| Outcomes | Subjective sleep quality and objective sleep quality (actigraphy) |
| Starting date | April 2014 |
| Contact information | k.cattapan@sanatorium‐kilchberg.ch |
| Notes |
Differences between protocol and review
We made the following three adjustments to the protocol Jespersen 2013.
We edited the title and the background section on 'Description of the condition' based on the comments of the reviewers.
We added a section to the methods describing the assessment of the quality of the evidence using the Grades of Recommendation, Assessment, Development and Evaluation (GRADE) approach.
We specified and ensured that trials involving any of the review authors were assessed by two authors with no involvement in the trial.
Contributions of authors
Co‐ordinated the review: Kira Vibe Jespersen. Drafted the protocol: Kira Vibe Jespersen, Julian Koenig, Poul Jennum, and Peter Vuust. Developed the search strategy: Kira Vibe Jespersen and Peter Vuust. Selected which trials to include: Kira Vibe Jespersen and Julian Koenig (Poul Jennum). Arbitrated in the event of dispute: Peter Vuust. Extracted data from trials: Kira Vibe Jespersen and Julian Koenig (Poul Jennum). Entered data into RevMan software: Kira Vibe Jespersen and Julian Koenig. Carried out the analysis: Kira Vibe Jespersen and Julian Koenig. Interpreted the analysis: Kira Vibe Jespersen, Julian Koenig, Poul Jennum, and Peter Vuust. Drafted the final review: Kira Vibe Jespersen and Julian Koenig. Kept the review up to date: Kira Vibe Jespersen and Julian Koenig.
Sources of support
Internal sources
-
Kira Vibe Jespersen: Department of Clinical Medicine, Aarhus University, Denmark.
Salary support
-
Julian Koenig: Department of Psychology, The Ohio State University, USA.
Salary support
-
Poul Jennum: Danish Centre for Sleep Medicine, Glostrup University Hospital, Denmark.
Salary support
-
Peter Vuust: Department of Clinical Medicine, Aarhus University and the Royal Academy of Music, Aarhus, Denmark.
Salary support
External sources
No sources of support supplied
Declarations of interest
Kira V Jespersen ‐ is the author of a trial that is included in the review*. Julian Koenig ‐ none known. Poul Jennum ‐ none known. Peter Vuust ‐ is a co‐author of a trial that is included in the review*.
*As Kira Jespersen and Peter Vuust are authors on the Jespersen 2012 trial. This trial was assessed by two authors (JK; PJ) with no involvement in the study.
Edited (no change to conclusions)
References
References to studies included in this review
Chang 2012 {published data only}
- Chang ET, Lai HL, Chen PW, Hsieh YM, Lee LH. The effects of music on the sleep quality of adults with chronic insomnia using evidence from polysomnographic and self‐reported analysis: a randomized control trial. International Journal of Nursing Studies 2012;49(8):921‐30. [DOI] [PubMed] [Google Scholar]
Harmat 2008 {published and unpublished data}
Jespersen 2012 {published data only}
- Jespersen KV. The Impact of Music on Sleep: A Review and Empirical Study of Music Listening as Intervention for Sleep Improvement [Master thesis]. Aarhus, Denmark: Department of Psychology and Behavioural Sciences, Aarhus University, 2010. [Google Scholar]
- Jespersen KV, Vuust P. The effect of relaxation music listening on sleep quality in traumatized refugees: a pilot study. Journal of Music Therapy 2012;49(2):205‐29. [DOI] [PubMed] [Google Scholar]
Kullich 2003 {published and unpublished data}
- Kullich W, Bernatzky G, Hesse HP, Wendtner F, Likar R, Klein G. Music therapy ‐ impact on pain, sleep, and quality of life in low back pain [Musiktherapie ‐ Wirkung auf schmerz, schlaf und lebensqualität bei low back pain]. Wiener Medizinische Wochenschrift 2003; Vol. 153, issue 9‐10:217‐21. [DOI] [PubMed]
Lai 2005 {published data only}
- Lai H. The Effects of Music Therapy on Sleep Quality in Elderly People [PhD thesis]. Ann Arbor: UMI Dissertation Services, 2004. [Google Scholar]
- Lai HL, Good M. Music improves sleep quality in older adults. Journal of Advanced Nursing 2005; Vol. 49, issue 3:234‐44. [DOI] [PubMed]
Shum 2014 {published data only}
- Shum A, Taylor BJ, Thayala J, Chan MF. The effects of sedative music on sleep quality of older community‐dwelling adults in Singapore. Complementary Therapies in Medicine 2014;22(1):49‐56. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Abdollahnejad 2006 {published data only}
- Abdollahnejad MR. Music therapy in the Tehran therapeutic community. Therapeutic Communities 2006;27(1):147‐58. [Google Scholar]
Beattie 2013 {published data only}
- Beattie E, McCrow J, Quinn L, Doyle C, Pachana N. Effect of a choir intervention on behaviour, sleep and social engagement of community‐dwelling people with dementia. International Psychogeriatrics. Proceedings of the 16th International Congress; 2013 October 1‐4; Seoul; Korea. Cambridge, UK: Cambridge University Press, 2013; Vol. 25 Suppl S1:S30.
Blanaru 2012 {published data only}
- Blanaru M, Bloch B, Vadas L, Arnon Z, Ziv N, Kremer I, et al. The effects of music relaxation and muscle relaxation techniques on sleep quality and emotional measures among individuals with posttraumatic stress disorder. Mental Illness 2012;4(2):59‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haimov I, Blanaro M, Arnon Z, Ziv N, Bloch B, Reshef A, et al. The effects of music and muscle relaxation therapies on sleep quality in individuals with post‐traumatic stress disorder. Journal of Sleep Research. Abstracts of the 20th Congress of the European Sleep Research Society; 2010 September 14‐18; Lisbon; Portugal. 2010; Vol. 19:364.
Bloch 2010 {published data only}
- Bloch B, Reshef A, Vadas L, Haliba Y, Ziv N, Kremer I, et al. The effects of music relaxation on sleep quality and emotional measures in people living with schizophrenia. Journal of Music Therapy 2010;47(1):27‐52. [DOI] [PubMed] [Google Scholar]
Bonebreak 1996 {published data only}
- Bonebreak KJ. A sound way to induce relaxation and natural sleep: a safe alternative to sedation. American Journal of Electroneurodiagnostic Technology 1996;36(4):264‐8. [Google Scholar]
Bonnet 2000 {published data only}
- Bonnet MH, Arand DL. The impact of music upon sleep tendency as measured by the multiple sleep latency test and maintenance of wakefulness test. Physiology & Behavior 2000;71(5):485‐92. [DOI] [PubMed] [Google Scholar]
Bozcuk 2006 {published data only}
- Bozcuk H, Artac M, Kara A, Ozdogan M, Sualp Y, Topcu Z, et al. Does music exposure during chemotherapy improve quality of life in early breast cancer patients? A pilot study. Medical Science Monitor 2006;12(5):CR200‐5. [PubMed] [Google Scholar]
Breitenfeld 1992 {published data only}
- Breitenfeld D, Breitenfeld T, Bergovec M. Music instead of sleeping pills [Glazba za uspavljivanje mjesto tableta za spavanje]. Tonovi: Časopis Glazbenih Pedagoga 1992;7:36. [Google Scholar]
Chan 2010 {published data only}
- Chan MF. A randomised controlled study of the effects of music on sleep quality in older people. Journal of Clinical Nursing 2011;20(7‐8):979‐87. [DOI] [PubMed] [Google Scholar]
- Chan MF, Chan EA, Mok E. Effects of music on depression and sleep quality in elderly people: a randomised controlled trial. Complementary Therapies in Medicine 2010;18(3‐4):150‐9. [DOI] [PubMed] [Google Scholar]
Chen 2014 {published data only}
- Chen CK, Pei YC, Chen NH, Huang LT, Chou SW, Wu KP, et al. Sedative music facilitates deep sleep in young adults. Journal of Alternative and Complementary Medicine 2014;20(4):312‐7. [DOI] [PubMed] [Google Scholar]
Demi̇rbağ 2014 {published data only}
- Demi̇rbağ BC, Erci̇ B. The effects of sleep and touch therapy accompanied by music and aromatherapy on the impact level of fibromyalgia, fatigue and sleep quality in fibromyalgia patients. TAF Preventive Medicine Bulletin 2014;13(1):57‐64. [Google Scholar]
De Niet 2010 {published data only}
- Niet G, Tiemens B, Hutschemaekers G. Can mental healthcare nurses improve sleep quality for inpatients?. British Journal of Nursing 2010;19(17):1100‐5. [DOI] [PubMed] [Google Scholar]
- Niet G, Tiemens B, Achterberg T, Hutschemaekers G. Applicability of two brief evidence‐based interventions to improve sleep quality in inpatient mental health care. International Journal of Mental Health Nursing 2011;20(5):319‐27. [DOI] [PubMed] [Google Scholar]
Deshmukh 2009 {published data only}
- Deshmukh AD, Sarvaiya AA, Seethalakshmi R, Nayak AS. Effect of Indian classical music on quality of sleep in depressed patients: a randomized controlled trial. Nordic Journal of Music Therapy 2009;18(1):70‐8. [Google Scholar]
Dorn 2014 {published data only}
- Dorn F, Wirth L, Gorbey S, Wege M, Zemlin M, Maier RF, et al. Influence of acoustic stimulation on the circadian and ultradian rhythm of premature infants. Chronobiology International 2014;31(9):1062‐74. [PUBMED: 25133792] [DOI] [PubMed] [Google Scholar]
DuRousseau 2011 {published data only}
- DuRousseau DR, Mindlin G, Insler J, Levin II. Operational study to evaluate music‐based neurotraining at improving sleep quality, mood, and daytime function in a first responder population. Journal of Neurotherapy 2011;15:389‐98. [Google Scholar]
Field 1999 {published data only}
- Field T. Music enhances sleep in preschool children. Early Child Development and Care 1999;150(1):65‐8. [Google Scholar]
Gao 2014 {published data only}
- Gao R, Lv Y, Li X, Zhou K, Jin X, Dang S, et al. Effects of comprehensive sleep management on sleep quality in university students in mainland China. Sleep and Biological Rhythms 2014;12(3):194‐202. [DOI: 10.1111/sbr.12063] [DOI] [Google Scholar]
Garunkstiene 2014 {published data only}
- Garunkstiene R, Buinauskiene J, Uloziene I, Markuniene E. Controlled trial of live versus recorded lullabies in preterm infants. Nordic Journal of Music Therapy 2014;23(1):71‐88. [Google Scholar]
Gitanjali 1998 {published data only}
- Gitanjali B. Effect of the Karnatic music raga "Neelambari" on sleep architecture. Indian Journal of Physiology and Pharmacology 1998;42(1):119‐22. [PubMed] [Google Scholar]
Hérnandez‐Ruíz 2005 {published data only}
- Hérnandez‐Ruíz E. Effect of music therapy on the anxiety levels and sleep patterns of abused women in shelters. Journal of Music Therapy 2005;42(2):140‐58. [DOI] [PubMed] [Google Scholar]
Hu 2015 {published data only}
- Hu RF, Jiang XY, Hegadoren KM, Zhang YH. Effects of earplugs and eye masks combined with relaxing music on sleep, melatonin and cortisol levels in ICU patients: a randomized controlled trial. Critical Care 2015;19:1‐9. [PUBMED: 25881268] [DOI] [PMC free article] [PubMed] [Google Scholar]
Iwaki 2003 {published data only}
- Iwaki T, Tanaka H, Hori T. The effects of preferred familiar music on falling asleep. Journal of Music Therapy 2003;40(1):15‐26. [DOI] [PubMed] [Google Scholar]
Johnson 2003 {published data only}
- Johnson JE. The use of music to promote sleep in older women. Journal of Community Health Nursing 2003;20(1):27‐35. [DOI] [PubMed] [Google Scholar]
Kayumov 2003 {published data only}
- Kayumov L, Moller HJ. Brain music: a novel somatic treatment for insomnia and anxiety. 156th Annual Meeting of the American Psychiatric Association, 2003 May 17‐22, San Francisco (CA). 2003:Nr405.
Koenig 2013 {published data only}
- Koenig J, Jarczok MN, Warth M, Harmat L, Hesse N, Jespersen KV, et al. Music listening has no positive or negative effects on sleep quality of normal sleepers: results of a randomized controlled trial. Nordic Journal of Music Therapy 2013;22(3):233‐42. [Google Scholar]
Lai 2012 {published data only}
- Lai HL, Li YM, Lee LH. Effects of music intervention with nursing presence and recorded music on psycho‐physiological indices of cancer patient caregivers. Journal of Clinical Nursing 2012;21(5‐6):745‐56. [DOI] [PubMed] [Google Scholar]
Lai 2015 {published data only}
- Lai H‐L, Chang E‐T, Li Y‐M, Huang C‐Y, Lee L‐H, Wang H‐M. Effects of music videos on sleep quality in middle‐aged and older adults with chronic insomnia: a randomized controlled trial. Biological Research for Nursing 2015;17(3):340‐7. [PUBMED: 25237150] [DOI] [PubMed] [Google Scholar]
Lazic 2007 {published data only}
- Lazic SE, Ogilvie RD. Lack of efficacy of music to improve sleep: a polysomnographic and quantitative EEG analysis. International Journal of Psychophysiology 2007;63(3):232‐9. [DOI] [PubMed] [Google Scholar]
Levin 1998 {published data only}
- Levin II. "Music of the Brain" in the treatment of insomnia patients. Zhurnal Nevrologii i Psikhiatrii Imeni S.S. Korsakova 1997;97(4):39‐43. [PubMed] [Google Scholar]
- Levin Y. "Brain music" in the treatment of patients with insomnia. Neuroscience and Behavioral Physiology 1998;28(3):330‐5. [DOI] [PubMed] [Google Scholar]
Lindenmuth 1992 {published data only}
- Lindenmuth GF, Patel M, Chang PK. Effects of music on sleep in healthy elderly and subjects with senile dementia of the Alzheimer type. American Journal of Alzheimer's Disease and Other Dementias 1992;7(2):13‐20. [Google Scholar]
Liu 2006 {published data only}
- Liu W, Kong J, Han B, Jin Y, Liu G, Gao F, et al. Effect of the somatosensory vibro‐music relaxation therapy on treatment of physical and psychological symptoms on sub‐health patients: a randomized controlled clinical trial. Chinese Journal of Rehabilitation Medicine 2006;21(11):1008‐11. [Google Scholar]
Loewy 2005 {published data only}
- Loewy J, Hallan C, Friedman E, Martinez C. Sleep/sedation in children undergoing EEG testing: a comparison of chloral hydrate and music therapy. American Journal of Electroneurodiagnostic Technology 2006;46(4):343‐55. [PubMed] [Google Scholar]
- Loewy J, Hallan C, Friedman E, Martinez C. Sleep/sedation in children undergoing EEG testing: a comparison of chloral hydrate and music therapy. Journal of PeriAnesthesia Nursing 2005;20(5):323‐31. [DOI] [PubMed] [Google Scholar]
Loewy 2013 {published data only}
- Loewy J, Stewart K, Dassler A‐M, Telsey A, Homel P. The effects of music therapy on vital signs, feeding, and sleep in premature infants. Pediatrics 2013;131(5):902‐18. [DOI] [PubMed] [Google Scholar]
Lü 2008 {published data only}
- Lü X, Lu Y, Liao X. Study on influence of music therapy on quality of life of cancer patients. Chinese Nursing Research 2008;22(1B):106‐8. [Google Scholar]
Ma 2004 {published data only}
- Ma Y, He DL, Jing LS, Wang J, Zha XX, Tan HM. Study of music intervention therapy on the sleep quality of preoperative patients. Chinese Journal of Clinical Rehabilitation 2004;8(6):1024‐5. [Google Scholar]
Mandel 2007 {published data only}
- Mandel SE, Hanser SB, Secic M, Davis BA. Effects of music therapy on health‐related outcomes in cardiac rehabilitation: a randomized controlled trial. Journal of Music Therapy 2007;44(3):176‐97. [DOI] [PubMed] [Google Scholar]
Mornhinweg 1995 {published data only}
- Mornhinweg GC, Voignier RR. Music for sleep disturbance in the elderly. Journal of Holistic Nursing 1995;13(3):248‐54. [DOI] [PubMed] [Google Scholar]
Naghdi 2015 {published data only}
- Naghdi L, Ahonen H, Macario P, Bartel L. The effect of low‐frequency sound stimulation on patients with fibromyalgia: a clinical study. Pain Research & Management 2015;20(1):e21‐7. [PUBMED: 25545161] [DOI] [PMC free article] [PubMed] [Google Scholar]
Oxtoby 2013 {published data only}
- Oxtoby J, Sacre S, Lurie‐Beck J, Pedersen IN. The impact of relaxing music on insomnia‐related thoughts and behaviours. Australian Journal of Music Therapy 2013;24:67‐86. [Google Scholar]
Picard 2014 {published data only}
- Picard LM, Bartel LR, Gordon AS, Cepo D, Wu Q, Pink LR. Music as a sleep aid in fibromyalgia. Pain Research & Management 2014;19(2):97‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reinhardt 1999 {published data only}
- Reinhardt U. Investigations into synchronisation of heart rate and musical rhythm in a relaxation therapy in patients with cancer pain. Forschende Komplementarmedizin 1999;6(3):135‐41. [DOI] [PubMed] [Google Scholar]
Renzi 2000 {published data only}
- Renzi C, Peticca L, Pescatori M. The use of relaxation techniques in the perioperative management of proctological patients: preliminary results. International Journal of Colorectal Disease 2000;15(5‐6):313‐6. [DOI] [PubMed] [Google Scholar]
Robinson 2005 {published data only}
- Robinson SB, Weitzel T, Henderson L. The Sh‐h‐h‐h Project: nonpharmacological interventions. Holistic Nursing Practice 2005;19(6):263‐6. [DOI] [PubMed] [Google Scholar]
Ryu 2012 {published data only}
- Ryu MJ, Park JS, Park H. Effect of sleep‐inducing music on sleep in persons with percutaneous transluminal coronary angiography in the cardiac care unit. Journal of Clinical Nursing 2012;21(5‐6):728‐35. [DOI] [PubMed] [Google Scholar]
Sithinamsuwan 2012 {published and unpublished data}
- Sithinamsuwan P, Saengwanitch S, Pinidbunjerdkool A, Ukritchon S, Mungthin M. The effect of Thai traditional music on cognitive function, psychological health and quality of sleep among older Thai individuals with dementia. Journal of the American Geriatrics Society 2012;60(Suppl s4):S61. [Google Scholar]
Skogar 2013 {published data only}
- Skogar O, Borg A, Larsson B, Robertsson L, Andersson L, Andersson P, et al. "Effects of Tactile Touch on pain, sleep and health related quality of life in Parkinson's disease with chronic pain": a randomized, controlled and prospective study. European Journal of Integrative Medicine 2013;5(2):141‐52. [Google Scholar]
Smith 2004 {published data only}
- Smith JC, Joyce CA. Mozart versus new age music: relaxation states, stress, and ABC relaxation theory. Journal of Music Therapy 2004;41(3):215‐24. [DOI] [PubMed] [Google Scholar]
Street 2014 {published data only}
- Street W, Weed D, Spurlock A. Use of music in the treatment of insomnia: a pilot study. Holistic Nursing Practice 2014;28(1):38‐42. [DOI] [PubMed] [Google Scholar]
Su 2013 {published data only}
- Su CP, Lai HL, Chang ET, Yiin LM, Perng SJ, Chen PW. A randomized controlled trial of the effects of listening to non‐commercial music on quality of nocturnal sleep and relaxation indices in patients in medical intensive care unit. Journal of Advanced Nursing 2013;69(6):1377‐89. [DOI] [PubMed] [Google Scholar]
Sørensen 2005 {published data only}
- Sørensen TE. Treating psychiatric anxiety patients with MusiCure: a pilot project [Behandling af angste psykiatriske patienter med MusiCure: et pilotprojekt]. Collected Work: Musikterapi i Psykiatrien 2005;4:77. [Google Scholar]
Tan 2004 {published data only}
- Tan LP. The effects of background music on quality of sleep in elementary school children. Journal of Music Therapy 2004;41(2):128‐50. [DOI] [PubMed] [Google Scholar]
Tegeler 2012 {published data only}
- Gerdes L, Gerdes P, Lee SW, Tegeler CH. HIRREM™: a noninvasive, allostatic methodology for relaxation and auto‐calibration of neural oscillations. Brain and Behavior 2013;3(2):193‐205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tegeler CH, Kumar SR, Conklin D, Lee SW, Gerdes L, Turner DP, et al. Open label, randomized, crossover pilot trial of high‐resolution, relational, resonance‐based, electroencephalic mirroring to relieve insomnia. Brain and Behavior 2012;2(6):814‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wormit 2012 {published data only}
- Wormit AF, Warth M, Koenig J, Hillecke TK, Bardenheuer HJ. Evaluating a treatment manual for music therapy in adult outpatient oncology care. Music and Medicine 2012;4(2):65‐73. [Google Scholar]
Zimmerman 1996 {published data only}
- Zimmerman L, Nieveen J, Barnason S, Schmaderer M. The effects of music interventions on postoperative pain and sleep in coronary artery bypass graft (CABG) patients. Scholarly Inquiry for Nursing Practice 1996;10(2):153‐74. [PubMed] [Google Scholar]
Ziv 2008 {published data only}
- Ziv N, Rotem T, Arnon Z, Haimov I. The effect of music relaxation versus progressive muscular relaxation on insomnia in older people and their relationship to personality traits. Journal of Music Therapy 2008;45(3):360‐80. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Miller 2002 {published and unpublished data}
- Bernatzky G, Presch M, Anderson M, Panksepp J. Emotional foundations of music as a non‐pharmacological pain management tool in modern medicine. Neuroscience & Biobehavioral Reviews 2011;35(9):1989‐99. [DOI] [PubMed] [Google Scholar]
- Miller K, Bernatzky G, Wendtner F. The purpose of music and relaxation for health promotion after surgical procedures ‐ results of a prospective, randomized study. Proceedings of the 10th World Congress on Pain IASP; 2002 August 17‐22; San Diego. Seattle: International Association for the Study of Pain (IASP) Press, 2003.
References to ongoing studies
NCT02321826 {published data only}
- NCT02321826. Music for insomnia. www.clinicaltrials.gov (accessed 12 June 2015).
NCT02376686 {published data only}
- NCT02376686. Music intervention in the treatment of sleep disorders for depressed patients. www.clinicaltrials.gov (accessed 12 June 2015).
Additional references
AASM 2005
- American Academy of Sleep Medicine. International Classification of Sleep Disorders: Diagnostic and Coding Manual. 2nd Edition. Westchester, IL: American Academy of Sleep Medicine, 2005. [Google Scholar]
APA 1994
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM‐IV). 4th Edition. Arlington, VA: American Psychiatric Publishing, 1994. [Google Scholar]
APA 2013
- American Psychiatric Association, American Psychiatric Association DSM‐5 Task Force. Diagnostic and Statistical Manual of Mental Disorders (DSM‐5). 5th Edition. Washington, DC: American Psychiatric Publishing, 2013. [Google Scholar]
Aritake‐Okada 2009
- Aritake‐Okada S, Kaneita Y, Uchiyama M, Mishima K, Ohida T. Non‐pharmacological self‐management of sleep among the Japanese general population. Journal of Clinical Sleep Medicine 2009;5(5):464‐9. [PUBMED: 19961033] [PMC free article] [PubMed] [Google Scholar]
Baglioni 2011
Bastien 2001
- Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine 2001;2(4):297‐307. [PUBMED: 11438246] [DOI] [PubMed] [Google Scholar]
Beck 1996
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory ‐ Second Edition (BDI‐II). San Antonio, TX: Psychological Corporation, 1996. [Google Scholar]
Begg 1994
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50(4):1088‐101. [PubMed] [Google Scholar]
Bernatzky 2011
- Bernatzky G, Presch M, Anderson M, Panksepp J. Emotional foundations of music as a non‐pharmacological pain management tool in modern medicine. Neuroscience & Biobehavioral Reviews 2011;35(9):1989‐99. [DOI] [PubMed] [Google Scholar]
Bradt 2010
- Bradt J, Magee WL, Dileo C, Wheeler BL, McGilloway E. Music therapy for acquired brain injury. Cochrane Database of Systematic Reviews 2010, Issue 7. [DOI: 10.1002/14651858.CD006787.pub2] [DOI] [PubMed] [Google Scholar]
Bradt 2011
- Bradt J, Dileo C, Grocke D, Magill L. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database of Systematic Reviews 2011, Issue 8. [DOI: 10.1002/14651858.CD006911.pub2] [DOI] [PubMed] [Google Scholar]
Bradt 2013
- Bradt J, Dileo C, Potvin N. Music for stress and anxiety reduction in coronary heart disease patients. Cochrane Database of Systematic Reviews 2013, Issue 12. [DOI: 10.1002/14651858.CD006577.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brattico 2009
- Brattico E, Pallesen KJ, Varyagina O, Bailey C, Anourova I, Järvenpää M, et al. Neural discrimination of nonprototypical chords in music experts and laymen: an MEG study. Journal of Cognitive Neuroscience 2009;21(11):2230‐44. [DOI] [PubMed] [Google Scholar]
Bruscia 1998
- Bruscia KE. Defining Music Therapy. Gilsum, NH: Barcelona Publishers, 1998. [Google Scholar]
Buysse 1989
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Research 1989;28(2):193‐213. [PUBMED: 2748771] [DOI] [PubMed] [Google Scholar]
Buysse 2006
- Buysse DJ, Ancoli‐Israel S, Edinger JD, Lichstein KL, Morin CM. Recommendations for a standard research assessment of insomnia. Sleep 2006;29(9):1155‐73. [DOI] [PubMed] [Google Scholar]
Cepeda 2006
- Cepeda MS, Carr DB, Lau J, Alvarez H. Music for pain relief. Cochrane Database of Systematic Reviews 2006, Issue 2. [DOI: 10.1002/14651858.CD004843.pub2] [DOI] [PubMed] [Google Scholar]
De Niet 2009
- Niet GJ, Tiemens BG, Kloos MW, Hutschemaekers GJ. Review of systematic reviews about the efficacy of non‐pharmacological interventions to improve sleep quality in insomnia. International Journal of Evidence‐Based Healthcare 2009;7(4):233‐42. [DOI] [PubMed] [Google Scholar]
Dileo 2007
- Dileo C, Bradt J. Music therapy: applications to stress management. In: Lehrer PM, Woolfolk RL, Sime WE editor(s). Principles and Practice of Stress Management. 3rd Edition. New York: Guilford Press, 2007. [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. British Medical Journal 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eje 2004
- MusiCure, 4. Northern Light [music CD]. Gefion Records 2004.
Frandsen 2014
Garza‐Villarreal 2014
- Garza‐Villarreal EA, Wilson AD, Vase L, Brattico E, Barrios FA, Jensen TS, et al. Music reduces pain and increases functional mobility in fibromyalgia. Frontiers in Psychology 2014; Vol. 5:90. [PUBMED: 24575066] [DOI] [PMC free article] [PubMed]
GRADE 2013
- Schünemann H, Brozek J, Guyatt G, Oxman A (editors). GRADE handbook: introduction to GRADE handbook: handbook for grading the quality of evidence and strength of recommendations using the GRADE approach. Updated October 2013. www.guidelinedevelopment.org/handbook (accessed 12 June 2015).
GRADEpro 2014 [Computer program]
- McMaster University. GRADEpro. Version 3.6. McMaster University, 2014.
Hargreaves 1997
- Hargreaves DJ, North AC (editors). The Social Psychology of Music. Oxford: Oxford University Press, 1997. [Google Scholar]
Harmat 2014 [pers comm]
- Harmat L. RE: Page proofs and question [personal communication]. Email to: J Koenig 26 September 2014.
Hernández‐Ruiz 2005
- Hernández‐Ruiz E. Effect of music therapy on the anxiety levels and sleep patterns of abused women in shelters. Journal of Music Therapy 2005;42(2):140‐58. [PUBMED: 15913391] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hodges 2009
- Hodges DA. Bodily responses to music. In: Hallam S, Cross I, Thaut M editor(s). The Oxford Handbook of Music Psychology. Oxford: Oxford University Press, 2009:121‐30. [Google Scholar]
Jespersen 2013a
- Jespersen KV, Koenig J, Jennum P, Vuust P. Listening to music for improving sleep in adults with insomnia. Cochrane Database of Systematic Reviews 2013, Issue 3. [DOI: 10.1002/14651858.CD010459] [DOI] [Google Scholar]
Juslin 2001
- Juslin PN, Sloboda JA. Music and Emotion: Theory and Research. Oxford: Oxford University Press, 2001. [Google Scholar]
Juslin 2011
- Juslin PN, Liljeström S, Laukka P, Västfjäll D, Lundqvist L‐O. Emotional reactions to music in a nationally representative sample of Swedish adults: prevalence and causal influences. Musicae Scientiae 2011;15(2):174‐207. [DOI: 10.1177/1029864911401169] [DOI] [Google Scholar]
Koelsch 2011
- Koelsch S, Fuermetz J, Sack U, Bauer K, Hohenadel M, Wiegel M, et al. Effects of music listening on cortisol levels and propofol consumption during spinal anesthesia. Frontiers in Psychology 2011;2:58. [PUBMED: 21716581] [DOI] [PMC free article] [PubMed] [Google Scholar]
Korhan 2011
- Korhan EA, Khorshid L, Uyar M. The effect of music therapy on physiological signs of anxiety in patients receiving mechanical ventilatory support. Journal of Clinical Nursing 2011;20(7‐8):1026‐34. [PUBMED: 21323778] [DOI] [PubMed] [Google Scholar]
Kripke 2012
- Kripke DF, Langer RD, Kline LE. Hypnotics' association with mortality or cancer: a matched cohort study. BMJ Open 2012;2(1):e000850. [DOI] [PMC free article] [PubMed] [Google Scholar]
Krystal 2004
- Krystal AD. The changing perspective on chronic insomnia management. Journal of Clinical Psychiatry 2004;65 Suppl 8:20‐5. [PUBMED: 15153064] [PubMed] [Google Scholar]
Kullich 2014a [pers comm]
- Kullich W. Fw: Data Request / Cochrane Review [personal communication]. Email to: J Koenig 15 September 2014.
Kullich 2014b [pers comm]
- Kullich W. Re: Data Request / Cochrane Review [personal communication]. Email to: J Koenig 25 September 2014.
Latimer Hill 2007
- Latimer Hill E, Cumming RG, Lewis R, Carrington S, Couteur DG. Sleep disturbances and falls in older people. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 2007;62(1):62‐6. [PUBMED: 17301039] [DOI] [PubMed] [Google Scholar]
Léger 2001
- Léger D, Scheuermaier K, Philip P, Paillard M, Guilleminault C. SF‐36: evaluation of quality of life in severe and mild insomniacs compared with good sleepers. Psychosomatic Medicine 2001;63(1):49‐55. [PUBMED: 11211064] [DOI] [PubMed] [Google Scholar]
Maratos 2008
- Maratos A, Gold C, Wang X, Crawford M. Music therapy for depression. Cochrane Database of Systematic Reviews 2008, Issue 1. [DOI: 10.1002/14651858.CD004517.pub2] [DOI] [PubMed] [Google Scholar]
Mayer 2011
- Mayer G, Jennum P, Riemann D, Dauvilliers Y. Insomnia in central neurologic diseases – occurrence and management. Sleep Medicine Reviews 2011;15(6):369‐78. [PUBMED: 21481621] [DOI] [PubMed] [Google Scholar]
Morin 2003
- Morin CM. Measuring outcomes in randomized clinical trials of insomnia treatments. Sleep Medicine Reviews 2003;7(3):263‐79. [DOI] [PubMed] [Google Scholar]
Morin 2005
- Morin CM. Psychological and behavioral treatments for primary insomnia. In: Kryger MH, Roth T, Dement WC editor(s). Principles and Practice of Sleep Medicine. 4th Edition. Philadelphia: Elsevier Saunders, 2005:726‐37. [Google Scholar]
Morin 2006a
- Morin CM, LeBlanc M, Daley M, Gregoire JP, Mérette C. Epidemiology of insomnia: prevalence, self‐help treatments, consultations, and determinants of help‐seeking behaviors. Sleep Medicine 2006;7(2):123‐30. [PUBMED: 16459140] [DOI] [PubMed] [Google Scholar]
Morin 2006b
- Morin CM, Bootzin RR, Buysse DJ, Edinger JD, Espie CA, Lichstein KL. Psychological and behavioral treatment of insomnia: update of the recent evidence (1998‐2004). Sleep 2006;29(11):1398‐414. [PUBMED: 17162986] [DOI] [PubMed] [Google Scholar]
Morin 2013
- Morin CM, Jarrin DC. Epidemiology of insomnia: prevalence, course, risk factors, and public health burden. Sleep Medicine Clinics 2013;8(3):281‐97. [DOI] [PubMed] [Google Scholar]
Mössler 2011
- Mössler K, Chen X, Heldal TO, Gold C. Music therapy for people with schizophrenia and schizophrenia‐like disorders. Cochrane Database of Systematic Reviews 2011, Issue 12. [DOI: 10.1002/14651858.CD004025.pub3] [DOI] [PubMed] [Google Scholar]
Nieminen 2012
- Nieminen S, Istók E, Brattico E, Tervaniemi M. The development of the aesthetic experience of music: preference, emotions, and beauty. Musicae Scientiae 2012;16(3):372‐91. [Google Scholar]
NIH 2005
- National Institute of Health. National Institutes of Health State of the science conference statement on manifestations and management of chronic insomnia in adults, June 13‐15, 2005. Sleep 2005;28(9):1049‐57. [PUBMED: 16268373] [DOI] [PubMed] [Google Scholar]
Nilsson 2009
- Nilsson U. The effect of music intervention in stress response to cardiac surgery in a randomized clinical trial. Heart & Lung: The Journal of Critical Care 2009;38(3):201‐7. [PUBMED: 19486788] [DOI] [PubMed] [Google Scholar]
Ohayon 2002
- Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Medicine Reviews 2002;6(2):97‐111. [PUBMED: 12531146] [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Riedel 2000
- Riedel BW, Lichstein KL. Insomnia and daytime functioning. Sleep Medicine Reviews 2000;4(3):277‐98. [PUBMED: 12531170] [DOI] [PubMed] [Google Scholar]
Shekleton 2010
- Shekleton JA, Rogers NL, Rajaratnam SM. Searching for the daytime impairments of primary insomnia. Sleep Medicine Reviews 2010;14(1):47‐60. [PUBMED: 19963414] [DOI] [PubMed] [Google Scholar]
Spielberger 1983
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State‐Trait Anxiety Inventory. Palo Alto (CA): Consulting Psychologists Press, 1983. [Google Scholar]
Taylor 2003
- Taylor DJ, Lichstein KL, Durrence HH. Insomnia as a health risk factor. Behavioral Sleep Medicine 2003;1(4):227‐47. [PUBMED: 15600216] [DOI] [PubMed] [Google Scholar]
Taylor 2007
- Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ. Comorbidity of chronic insomnia with medical problems. Sleep 2007;30(2):213‐8. [PUBMED: 17326547] [DOI] [PubMed] [Google Scholar]
Trappe 2010
- Trappe HJ. The effects of music on the cardiovascular system and cardiovascular health. Heart 2010;96(23):1868‐71. [PUBMED: 21062776] [DOI] [PubMed] [Google Scholar]
Urponen 1988
- Urponen H, Vuori I, Hasan J, Partinen M. Self‐evaluations of factors promoting and disturbing sleep: an epidemiological survey in Finland. Social Science & Medicine 1988;26(4):443‐50. [PUBMED: 3363395] [DOI] [PubMed] [Google Scholar]
Vuust 2006
- Vuust P, Roepstorff A, Wallentin M, Mouridsen K, Østergaard L. It don't mean a thing...keeping the rhythm during polyrhythmic tension, activates language areas (BA47). NeuroImage 2006;31(2):832‐41. [DOI] [PubMed] [Google Scholar]
Vuust 2010
- Vuust P, Gebauer L, Hansen NC, Jørgensen SR, Møller A, Linnet J. Personality influences career choice: sensation seeking in professional musicians. Music Education Research 2010;12(2):219‐30. [Google Scholar]
Walsh 2004
- Walsh JK. Clinical and socioeconomic correlates of insomnia. Journal of Clinical Psychiatry 2004;65 Suppl 8:13‐9. [PUBMED: 15153063] [PubMed] [Google Scholar]
Wang 2014
- Wang C‐F, Sun Y‐L, Zang H‐X. Music therapy improves sleep quality in acute and chronic sleep disorders: a meta‐analysis of 10 randomized studies. International Journal of Nursing Studies 2014;51(1):51‐62. [DOI] [PubMed] [Google Scholar]
Ware 1992
- Ware JE Jr, Sherbourne CD. The MOS 36‐item short‐form health survey (SF‐36): I. Conceptual framework and item selection. Medical Care 1992;30(6):473‐83. [PubMed] [Google Scholar]
WHO 1992
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems (ICD‐10). 10th Edition. Geneva: World Health Organization, 1992. [Google Scholar]
Wigram 2002
- Wigram T, Pedersen IN, Bonde LO. A Comprehensive Guide to Music Therapy: Theory, Clinical Practice, Research and Training. London: Jessica Kingsley Publishers, 2002. [Google Scholar]
Wilson 2010
- Wilson SJ, Nutt DJ, Alford C, Argyropoulos SV, Baldwin DS, Bateson AN, et al. British Association for Psychopharmacology consensus statement on evidence‐based treatment of insomnia, parasomnias and circadian rhythm disorders. Journal of Psychopharmacology 2010;24(11):1577‐601. [PUBMED: 20813762] [DOI] [PubMed] [Google Scholar]
Zhang 2012
- Zhang JM, Wang P, Yao JX, Zhao L, Davis MP, Walsh D, et al. Music interventions for psychological and physical outcomes in cancer: a systematic review and meta‐analysis. Supportive Care in Cancer 2012;20(12):3043‐53. [PUBMED: 23052912] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Jespersen 2013
- Jespersen KV, Koenig J, Jennum P, Vuust P. Listening to music for improving sleep in adults with insomnia. Cochrane Database of Systematic Reviews 2013, Issue 3. [DOI: 10.1002/14651858.CD010459] [DOI] [Google Scholar]


