Abstract
Objectives:
To examine the association between work-related stress (job lock and job stress appraisal) and insomnia symptoms among older Black workers, as well as the extent to which psychosocial resources (mastery, social support, and religious involvement) mediate or moderate this association.
Methods:
This study uses Ordinary Least Squares regression analysis and data from the Health and Retirement Study (HRS) on Black workers aged 51 and older (N = 924).
Results:
Job lock due to financial reasons and job stress appraisal are associated with increased insomnia symptoms among older Black workers. Religious attendance buffers the harmful effects of financial job lock on sleep quality, while religiosity exacerbates the effects of job stress on insomnia symptoms.
Discussion:
Taken together, findings underscore the utility of the Stress Process Model for understanding diverse stress and sleep experiences in later life. Furthermore, findings have the potential to inform efficacious policies for reducing work-related stress and mitigating its harmful consequences.
Keywords: stress, work, sleep, aging, Black adults
Introduction
In the coming years, Black Americans will comprise increasing shares of the older adult population (Federal Interagency Forum, 2020) as well as the labor force (Emily & Toossi, 2018). Notably, older Black Americans are retiring later than in the past due to both the raised age for eligibility for Social Security Retirement benefits and their economic precarity (Johnson, 2011; Moore et al., 2019). In order to understand older Black adults’ unique experiences with regard to work and well-being, it is important to consider how social contexts have shaped their lives. For instance, many older Black Americans came of age during the Jim Crow era and thus have endured overt and de jure racism as well as more contemporary subtle and de facto forms of racism in an array of societal domains (e.g., education, employment, housing, criminal justice, and health care systems), which has limited their opportunities for good health and economic security in later life (Bonilla-Silva, 1997; Brown & Homan, 2022; Garcia et al., 2021). Indeed, relative to their white counterparts, older Black people have lower wages (Brown, 2018), are approximately 25% less likely to have private health insurance (Brown et al., 2006), are 40% less likely to own a retirement account (Kijakazi et al., 2019; Rhee, 2013) and have approximately 5% of their net worth (Brown, 2016). Given these significant economic disadvantages, it is not surprising that 83% of Black older adults lack the retirement assets they need to last the remainder of their lifetimes (Guzman & Vulimiri, 2015).
The literature on stress and health is useful for understanding how older Black workers’ unique experiences of work-related stressors may impact their health. A large body of research has documented the deleterious health consequences of chronic strains such as work-related stressors (Mezuk et al., 2011; Mutambudzi & Javed, 2016). Two types of stressors linked to work that may be particularly relevant for the health of older Black workers are job lock and job stress. Job lock refers to workers’ perception that they do not have a choice—that is, they must continue to work despite a desire to retire (Fisher, Ryan, & Sonnega, 2016). Financial need and health insurance are two common sources of job lock that are associated with poor health, lower life satisfaction, and dissatisfaction in the workplace (Fisher et al., 2016). In addition to job lock, other sources of job stress include work overload, work-family conflict, and lack of decision-making authority (Glazer & Liu, 2017). Many Black employees also experience racialized sources of stress due to workplace discrimination—for example, policies, practices, and norms that have a disparate negative impact on Black workers (Wingfield & Chavez, 2020). Strikingly, more than half (51.8%) of older Black workers report that their jobs involve a lot of stress (Johnson, 2011). High levels of work-related stressors among older Black workers are likely to have substantial consequences for their health—including sleep.
Sleep is restorative for individual health and provides renewed energy for physical and social activities. Research shows that poor sleep is associated with higher rates of cardiovascular disease, diabetes, obesity, anxiety, depressed mood, and mortality (Buxton & Marcelli, 2010; Jackson et al., 2015; Leggett et al., 2018; Lunau et al., 2013). Not only does sleep shape health outcomes, but it is also an important aspect of health itself (Hale et al., 2020). Sleep problems have substantial economic costs, including an estimated $6.6 billion cost annually in terms of healthcare expenses and loss of work productivity (Simpson et al., 2014). Thus, it is critical to better understand the social determinants of sleep. A burgeoning body of research suggests that work-related factors that contribute to sleep loss include extended work hours, negative emotional experiences at work, and shift work (Burgard & Ailshire, 2009; Luyster et al., 2012). In fact, engaging in shift work, which is common among Black workers, is associated with increased risk of insomnia symptoms such as difficulty initiating sleep, frequent awakenings, and difficulty returning to sleep (Kecklund & Axelsson, 2016). Despite a growing literature on the social underpinnings of sleep problems, few studies have explored the social determinants of insomnia symptoms among older Black Americans (for exceptions see Bazargan et al., 2019; D. A. Johnson et al., 2016).
Drawing on the Stress Process Model (Pearlin et al., 2005) and leveraging rich data from the Health and Retirement Study, this study contributes to the literature in several ways. First, we investigate the relationship between work-related stressors (job lock and job stress appraisal) and insomnia symptoms in older Black workers. Second, we examine whether and how psychosocial resources such as mastery, social support, and religious involvement—all of which are relatively high among Black people in late life (Brown & Hargrove, 2018; Keith, 2014; Taylor, Chatters, & Levin, 2003)—have a direct association with insomnia symptoms. Third, we test the extent to which psychosocial resources mediate and/or moderate associations between work-related stressors and insomnia symptoms. While a large body of research on social stress processes suggests that these psychosocial resources have protective and buffering effects on health (Jackson & Knight 2006; Keith, 2014; Taylor, Chatters, & Brown, 2014), little is known about their effects on sleep quality among older Black workers. Lastly, whereas most prior studies on related topics have relied on community-based samples, this study utilizes nationally representative data to study Black workers’ experiences in later life.
Theoretical Framework
The stress process model (SPM) guides this study. The basic components of the SPM include stressors, psychosocial resources, and outcomes (Pearlin & Bierman, 2013). Stressors are events or experiences that can challenge the adaptive capacities of individuals. Psychosocial resources refer to the various internal and external resources that one can use to lessen the effects of stressors; and outcomes refer to the mental and physical health consequences or manifestations of stress. A strength of the SPM is that it accounts for people’s locations within social structure, which determines stress exposure, the psychosocial resources one can mobilize, and the way a person experiences stress (Aneshensel & Mitchell, 2014). The structural context of people’s lives is fundamental to the stress process and observed differences in health arise from differences in status locations within systems of inequality (Thoits, 2010). As such, work-related stressors among older Black workers are not random; rather, they are due to their subordinate status within the U.S. racial hierarchy (Brown & Hargrove, 2018; Keith, 2014).
Work-related stress and sleep.
Within the context of the SPM, work-related stressors such as job lock and job stress are chronic stressors. Chronic stress refers to ongoing problems in the social environment that impede an individual’s capacity to adequately perform social roles (Aneshensel & Mitchell, 2014). The consequences of chronic stressors are especially severe when arising within major social domains, such as work. In fact, job stress is frequently cited by workers as a cause of sleeping difficulties (Linton, 2004). Although there is a lack of evidence on the effects of work-related stress on sleep in older Black workers, numerous studies show that work-related stress can affect sleep. For example, Burgard & Ailshire (2009) found that being upset or bothered at work was associated with poorer sleep quality. High job demand, work overload, and repetitive tasks at work also increase difficulty initiating and maintaining sleep (Knudsen et al., 2007).
Work-related stress may induce a stress response in older Black workers that triggers physiological changes such as activating the sympathetic nervous system (i.e., fight or flight response) and the hypothalamic-pituitary-adrenal (HPA)-axis (i.e., the central stress response system), contributing to insomnia symptoms (Jackson & Knight, 2006). While there are numerous biosocial pathways by which stress can impact health (see Goosby et al., 2018 for review), allostasis and allostatic load are important to consider when dealing with chronic stressors. Allostasis is the regulatory process where homeostasis is maintained by activating various systems (e.g., HPA-axis, autonomic nervous system, metabolic system) in response to stress (Goosby et al., 2018). Prolonged activation of these systems can lead to allostatic load, which results in wear and tear on the body, compromising health. Psychological stress and reactivity to stress have been implicated in the development of insomnia symptoms (Burgard & Ailshire, 2009). Workplace stressors can trigger the body to release adrenaline and cortisol, which negatively affect sleep quality by interfering with a worker’s ability to unwind at the end of the day or causing anxiety and rumination (Burgard & Ailshire, 2009; Hicken et al., 2013).
Psychosocial resources: Mastery, social support, and religious involvement.
Psychosocial resources serve to change the situation from which stressors arise, help manage the meaning of stress, or keep symptoms of stress within manageable bounds. Common psychosocial resources examined within the stress process framework include mastery, social support and religious involvement (Pearlin & Bierman, 2013). Also referred to as mediators or moderators, psychosocial resources can serve as mechanisms through which stressors impact health (mediators), or as factors that weaken or exacerbate (i.e., moderate) the effect of stressors on health. Research shows that psychosocial resources differ by social position. For example, while Black people, experience reduced access to economic resources, their collective racial identity and religious institutions provide more protection against adversity compared to whites, particularly in later life (Taylor et al., 2014). However, repeated exposure to chronic stress can dimmish psychosocial resources, which are often used to reduce the harmful effects of stress (Aneshensel & Mitchell, 2014). Psychosocial resources examined in this study are mastery, social support, and religious involvement.
Mastery.
Mastery, which refers to a person’s belief that they can control and mange stressful situations, not only affects psychological functioning, but also the actions that people take in order to characterize or deal with stress. A high sense of mastery is associated with several positive outcomes such as greater educational attainment, higher occupational status, elevated life satisfaction, and better mental and physical health (Milaneschi et al., 2010; Pearlin & Bierman, 2013; Roepke & Grant, 2011). A high degree of mastery is often useful when faced with declining health as well as social and personal losses that occur in late life (Cairney & Krause, 2008). Mastery also buffers the effects of stress on health. For example, Pudrovska et al. (2005) found that mastery mediated and moderated the effect of economic hardship on physical and mental health in older adults. In addition, a study by Lincoln (2007) revealed that mastery mediated the association between negative interactions and mental health among older Blacks.
While these studies offer useful insights, there is limited research on the association between work-related stress, mastery, and sleep among older Black workers. The few studies examining the association between job stress and mastery found no relationship (Liu et al., 2018) and mastery did not mediate the association between job stress and depressive symptoms (Lunau et al., 2018). However, Jang et al. (2008) found that mastery mediated the relationship between perceived discrimination and well-being. No studies to our knowledge examine the effects of mastery on sleep. Despite limited research in these areas, a high sense of mastery may be important for older Black workers who often face work-related stressors such as job lock and job stress.
Social support.
Social support refers to the assistance or emotional uplift individuals can draw upon to help deal with stressful situations. Social support is important for healthy coping in late life and is associated with improved physical and mental health among older adults. Research shows that older adults who receive support have lower blood pressure, reduced mortality rates, and higher cognitive functioning (Gow et al., 2013; Holt-Lunstad et al., 2010). Social support may also reduce the stress response by assisting individuals with coping and by enhancing self-esteem and perceived control over the environment (Pearlin et al., 1981).
There is ample evidence that social support is beneficial with regards to sleep. For example, higher levels of perceived social support are associated with better sleep quality, less fatigue, fewer sleeping difficulties, and longer sleep duration (Troxel et al., 2007; 2010). With respect to moderating effects of social support on the stress-sleep relationship, evidence is mixed, with results from some studies providing support for the buffering effects of sleep (e.g., Pow et al., 2017; Troxel et al., 2007) and other studies not yielding evidence of such buffering effects (e.g., Crain et al., 2014; Nordin et al., 2012). It remains an open question as to whether social support mediates or buffers the effects of work-related stressors on sleep among older Black workers.
Religious involvement.
Religion has proven to be an important and effective coping strategy for Black people, despite their marginalized position in society. The institution of the church holds a special place within the Black community. Not only a beacon of spiritual support and guidance, the Black church has also been a strong force in the fight for Civil Rights and equality. There is an extensive literature that provides evidence of the powerful role of religion in the lives of Black Americans (for review of literature see Nguyen, 2020; Taylor et al., 2014). Older Blacks report higher levels of religious involvement compared to their younger and white counterparts (Taylor et al., 2007). Religious involvement is an effective coping resource that helps older Blacks deal with stress because it provides systems of meaning and faith-based social support (Taylor et al., 2003).
Religious involvement can be characterized as organizational (e.g., religious attendance), non-organizational (e.g., prayer, reading religious texts), and subjective religiousness (hereafter religiosity), which refers to the strength of one’s religious identity, religious importance, and the role of religious beliefs in daily life (Taylor et al., 2014). Religious attendance is an important coping strategy because it connects people with supportive networks and provides spiritual and emotional uplift, which can directly benefit health and help deal with job stress (Chatters et al., 2008). Activities associated with non-organizational religious involvement, such as prayer, are beneficial in reducing stress because they provide a sense of control and give meaning to events, of-tentimes centering God as in control (Henderson, 2016). Prayer is also a common psychological resource for coping with stress (Brown & Hargrove, 2018). Brown & Hargrove (2018) found that greater frequency of prayer buffered the harmful effects of traumatic events on self-rated health among older Black men. Moreover, 90 percent of Blacks indicate that prayer is an important coping strategy when dealing with stress (Chatters et al., 2008). Religiosity is also a source of emotional and instrumental support for Blacks. For example, studies show that having faith in God improves well-being among older Blacks living with dementia and religiosity (e.g., closeness to God, sanctification of the body, internalized beliefs) increases healthy behaviors such as stress management, exercise, and healthy eating among older adults (Epps & Williams, 2020; Homan & Boyatzis, 2010).
Religious involvement may be an effective coping strategy because it limits the physiological response to stress (e.g., allostatic load, increase in cortisol) due to improved physiological functioning of the HPA-axis (Seybold, 2007). Studies show that religious involvement has direct, protective effects with regards to improved health and well-being, particularly in relation to psychiatric and mood disorders (Chatters et al., 2015; Ellison et al., 2017). There is also evidence that religious involvement decreases mortality risks in Blacks as well as buffers the effects of work-family conflict on life satisfaction among Black adults (Ellison et al., 2000; Henderson, 2016).
There are a few studies that examine the association between religious involvement and sleep; however, the findings are mixed about whether the effects are beneficial or harmful. On the one hand, research shows that forgiveness, viewing the body as sacred, frequency of prayer, and religious attendance improve sleep quality (Ellison et al., 2011; Hill et al., 2006; Krause & Ironson, 2017; Lawler-Row, 2010). On the other hand, there is evidence that religious doubts are associated with poor sleep quality and difficulty falling asleep (Ellison et al., 2011). Despite this burgeoning literature, we know very little about the direct or buffering effects of religious involvement on sleep, especially among older Black workers.
The Current Study
Three research questions guide this study. First, does work-related stress (i.e., job lock and job stress appraisal) affect insomnia symptoms among older Black workers? Second, do psychosocial resources such as mastery, social support, and religious involvement have a direct effect on insomnia symptoms? Third, do these psychosocial resources mediate or moderate the association between work-related stress and insomnia symptoms? Answering these questions will provide valuable insights about mechanisms underlying the work-related stress-sleep relationship among Black workers in later life.
Data and Methods
Data.
Data are from the Health and Retirement Study (HRS), which is a biennial longitudinal survey of households in the United States with at least one adult over the age of 50. The HRS is funded by the National Institute on Aging and is housed at the Institute for Social Research at the University of Michigan. The HRS, which began in 1992, is a nationally representative sample of the U.S. population over age 50. Sampling for the study used a multistage area probability design. Black and Hispanic households were oversampled. HRS core public release data, Rand HRS data, and the Psychosocial Leave Behind are used in this analysis. The Psychosocial Leave Behind is a special module for which a randomized half of the core sample in 2014 was invited to complete; the other halve was invited to complete the survey in 2016. This study uses pooled data from waves 2014 and 2016. Given the focus of the study, the sample is restricted to older Black workers aged 51 and over (N = 924).
Insomnia Symptoms.
The dependent variable for this study is insomnia symptoms. Respondents were asked how often they (1) had trouble falling asleep, (2) had trouble waking too early and not falling back asleep, (3) had trouble waking during the night, and (4) felt rested when they woke up in the morning. Frequency of each item was assessed on a scale of 1 (rarely or never), 2 (sometimes), and 3 (most of the time). The fourth item was reverse coded to align with higher levels of insomnia symptoms. The four items were then summed to create an index of insomnia symptoms ranging from 4 to 12. The Chronbach’s alpha reliability is .63.
Work-related stress.
Work-related stress is the focus of this study and is assessed by three measures. The first two measures were two questions related to job lock. Working respondents who participated in the psychosocial leave behind were asked: “Right now, would you like to leave work altogether, but plan to keep working because 1) you need the money (1 = yes) and 2) you need health insurance (1 = yes)?”. The third measure is a measure of job stress appraisal (hereafter job stress) where respondents who were working in 2014 and 2016 were asked whether their job involved a lot of stress. The scale ranged from (1) strongly agree to (4) strongly disagree. This measure was reverse coded so that higher values indicate more job-related stress.
Psychosocial resources.
Psychosocial resources for this study include mastery, positive social support, religious attendance, frequency of prayer, and religiosity. Mastery was assessed with the 7-item Pearlin Mastery scale (Pearlin, 1999), which captures the degree to which respondents feel they are in control of their lives. Respondents were asked to rank the following items on a scale ranging from 1 (strongly disagree) to 6 (strongly agree): (1) “I can do just about anything I really set my mind to,” (2) “What happens to me in the future mostly depends on me,” (3) “I often feel helpless in dealing with the problems of life,” (4) “Other people determine most of what I can and cannot do,” (5) “What happens in my life is often beyond my control” (6) “I have little control over the things that happen to me,” and (7) “There is really no way I can solve the problems that I have.” The last five items were reverse coded to indicate a higher degree of mastery. Items were summed to create a scale ranging from 12 to 42 (Chronbach’s alpha = .76).
A measure of positive social support was created based on respondents’ perceived support from their spouse, children, family, and friends. For each group, respondents were asked three items: (1) “How much do they really understand your feelings”; (2) “Can you rely on them for a serious problem”; and (3) “How much can you open up about your worries?”. Responses ranged from 1 (a lot) to 4 (not at all). This measure was reverse coded to indicate higher levels of social support. Response from each group were compiled into one measure of positive social support that range from 7 to 48 (Chronbach’s alpha =.58).
Organizational religious involvement was assessed with religious attendance. Respondents were asked “About how often have you attended religious services during the past year?” Answers ranged from (1) more than once a week, (2) once a week, (3) two or three times a month, (4) one or more times a year, and (5) not at all. The measure was reverse coded to indicate higher religious attendance. Non-organizational religious involvement was captured with two measures, frequency of prayer and religiosity. For frequency of prayer, participants were asked how often they prayed privately in places other than a church or synagogue; item responses ranged from 1 (never) to 7 (daily). Religiosity was measured with a 4-item index on a scale of 1 (strongly disagree) to 6 (strongly agree) where respondents were asked whether (1) “I believe in a God who watches over me,” (2) “The events in my life unfold according to a Divine or greater plan,” (3) “I try hard to carry my religious beliefs over into all my other dealings in life,” and (4) “I find strength and comfort in my religion.” (Bierman et al., 2018). The range is 4–24 and the Chronbach’s alpha reliability coefficient is .94.
Control variables.
To estimate the unique impact of jobs stress, job lock, and psychosocial resources on insomnia symptoms, analyses control for a range of factors that theoretical and empirical research have suggested may be related to the key independent and dependent variables, including gender, marital status, age, income, education, labor force status, and chronic conditions. Gender was coded as female (1 = yes) and male (reference). Marital status was coded as married (1 = yes) and not married (reference). Age and education were measured in years. Total household income was used and logged to correct for skewness. Labor force status was measured as full-time (1 = yes) and part-time (reference). Finally, any chronic conditions is a measure that captured the presence of chronic conditions (1 = yes) verses no chronic conditions (reference). Specifically, respondents were asked whether they were ever diagnosed with any of the following conditions: arthritis, high blood pressure, diabetes, cancer, lung disease, stroke, and heart disease.
Analytic Strategy
We begin analyses by estimating descriptive statistics for all study variables (Table 1). Next, we utilize Ordinary Least Squares (OLS) regression models to estimate the relationships among work-related stressors, psychosocial resources, and insomnia symptoms. Model one estimates the effects of job lock and job stress on insomnia symptoms. To examine the extent to which psychosocial resources have a direct effect as well as mediate the relationship between work-related stress and insomnia symptoms, each of the psychosocial resources are added in a stepwise fashion to Models 2–4 (mediation analysis uses the Baron & Kenny (1986) approach). Model five is the full model that includes all study variables. Sobel (1982) tests were used to estimate mediation based on the full model (Model 5). Finally, potential moderating effects were assessed with statistical interactions between job lock, job stress, and each psychosocial measure. Models six and seven show the results for statistically significant moderation effects. All regression analyses control for demographic and economic measures, utilize sample weights, and are estimated with SAS 9.4.
Table 1.
Weighted Means, Proportions, and Standard Deviations (S.D.) for Study Variables, Health and Retirement Study, 2014–2016 (N = 924).
| Variables | Mean/Proportion | S.D. |
|---|---|---|
| Dependent Variable | ||
| Insomnia symptoms | 5.33 | 4.10 |
| Independent Variable | ||
| Job lock: Financial | .34 | — |
| Job lock: Insurance | .47 | — |
| Job stress | 2.57 | 1.19 |
| Mediators/Moderators | ||
| Mastery | 35.78 | 8.74 |
| Positive social support | 31.17 | 11.13 |
| Religious attendance | 3.32 | 1.96 |
| Religiosity | 21.06 | 7.80 |
| Frequency of prayer | 5.41 | 3.31 |
| Control Variables | ||
| Female | .62 | — |
| Age (years) | 60.37 | 8.69 |
| Married | .55 | — |
| Education (years) | 13.71 | 3.03 |
| Income (logged) | 10.66 | 1.92 |
| Work full-time | .65 | — |
| Any chronic condition | .80 | — |
Results
Table 1 displays descriptive information for the study population. The mean for insomnia symptoms among study participants is 5.33. Thirty four percent of respondents reported job lock due to financial reasons, while 47% continued to work due to a need for health insurance. The mean for job stress is 2.57. Respondents reported a high degree of mastery (35.78), positive social support (31.17), and religiosity (21.06). The mean for religious attendance is 3.32 and frequency of prayer is 5.41. Sixty-two percent of the sample is female and 55% is married. The mean for education is 13.71 and logged household income (measured in thousands of dollars) is 10.66. The average age for study participants is 60 years, 65% of respondents work full-time, and 80% of respondents report being diagnosed with any chronic condition.
Table 2 presents regression estimates of the impact of work-related stress and psychosocial factors on insomnia symptoms (net of demographic and economic control variables). Results from Model 1 show that both financial job lock (β = .279, p < .001) and job stress (β = .097, p < .05) are associated with increased symptoms of insomnia. Models two through four add measures of mastery, social support, and religious involvement, respectively. Across all three models, financial job lock (β = .278 p < .001; β = .279 p < .001; β = .276 p < .001), and job stress (β = .096 p < .05; β = .099 p < .05; β = .093 p < .05), respectively, are positively associated with insomnia symptoms. However, estimates from Models 2, 3, and 4, also indicate that none of the psychosocial measures have a direct effect nor mediate the effect of job lock (financial) and job stress on insomnia symptoms. Sobel tests confirm that there is no evidence of mediation. Psychosocial resources are weakly correlated (correlations ranged from .04 to .29) and there was no evidence of collinearity. It is important to note that while all three measures of religious involvement are added simultaneously in model 4, supplemental analysis added each measure separately and none were significant. Finally, model five is the full model that contains all study variables; financial job lock (β = .276, p<.001) as well as job stress (β = .093, p < .05) are associated with increased insomnia symptoms.
Table 2.
Insomnia Symptoms Regressed on Job Lock, Job Stress, and Psychosocial Resources (N = 924).
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | |
|---|---|---|---|---|---|---|---|
| β | β | β | β | β | β | β | |
| Job lock | |||||||
| Financial | .279g | .278g | .279g | .276g | .276g | .480g | .277g |
| Health insurance | −.081 | −.081 | −.082 | −.080 | −.082 | −.086 | −.079 |
| Job stress | |||||||
| Job stress | .097e | .096e | .099e | .093e | .093e | .089e | −.139 |
| Psychosocial resources | |||||||
| Mastery | −.014 | −.026 | −.023 | −.026 | |||
| Positive social support | .033 | .036 | .026 | .040 | |||
| Religious attendance | −.051 | −.054 | .001 | −.051 | |||
| Religiosity | .066 | .066 | .060 | −.120 | |||
| Frequency of prayer | .014 | .016 | .017 | .019 | |||
| Controls | |||||||
| Femalea | .070 | .070 | .067 | .068 | .065 | .063 | .062 |
| Age | .314g | .316g | .311g | .315g | .313g | .321g | .309g |
| Marriedb | .075 | .075 | .058 | .079 | .062 | .071 | .051 |
| Education | −.072 | −.071 | −.070 | −.070 | −.066 | −.069 | −.067 |
| Income | −.064 | −.063 | −.063 | −.064 | −.059 | −.061 | −.057 |
| Work full-timec | −.011 | −.010 | −.013 | −.016 | −.017 | −.009 | −.017 |
| Any chronic conditionsd | .074 | .075 | .074 | .072 | .074 | .068 | .074 |
| Interactions | |||||||
| Financial × religious attendance | −.228e | ||||||
| Job stress × religiosity | .304e | ||||||
| R2 | .22 | .22 | .22 | .23 | .23 | .24 | .24 |
male (reference).
not married (reference).
part-time (reference).
no chronic conditions (reference).
p < .05.
p < .01.
p < .001.
In order to examine whether psychosocial resources “buffer” (or moderate) the effects of work-related stress on insomnia symptoms, supplemental analyses estimated interactions between both measures of job lock, job stress, and each of the psychosocial resources. However, only two interactions were statistically significant. First, Model 6 shows that there is a significant interaction between financial job lock and religious attendance (β = −.228, p < .05). Figure 1 shows that when compared to respondents not experiencing financial job lock, the harmful effect of financial job lock on insomnia symptoms is reduced with increased religious attendance. Results from Model seven show that there is a statistically significant interaction between job stress and religiosity (β = .304, p < .05), indicating that religiosity moderates the effects of job stress on insomnia symptoms. Figure 2 provides a graphical depiction of the interaction, showing that the harmful effects of job stress on insomnia symptoms increases with high levels of religiosity (compared to those with low levels of religiosity). It is important to note that age is consistently associated with increased insomnia symptoms, which aligns with prior research.
Figure 1.
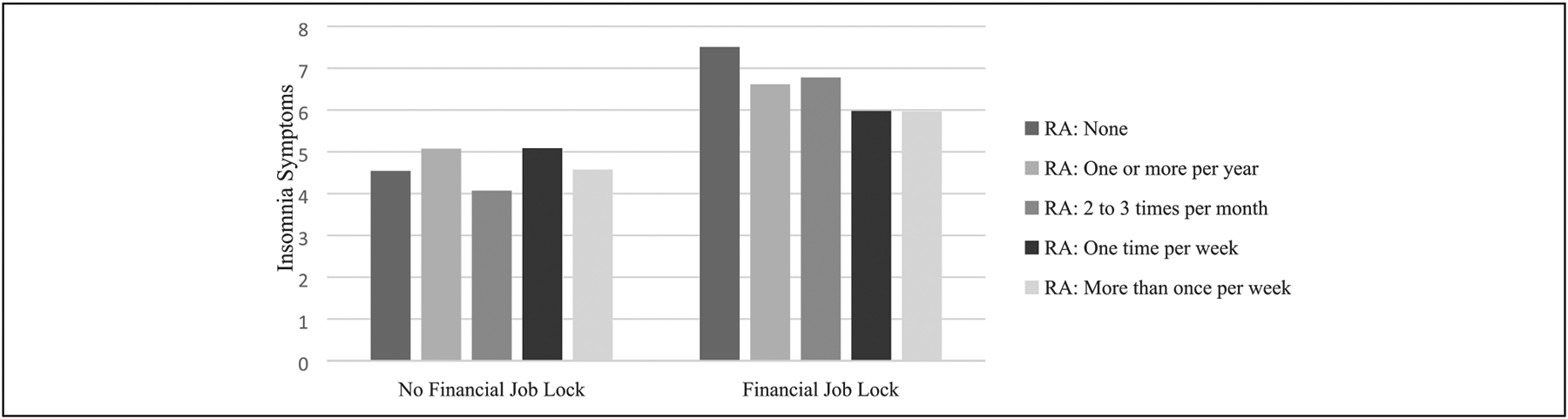
Interaction of financial job lock and religious attendance on insomnia symptoms.
Figure 2.
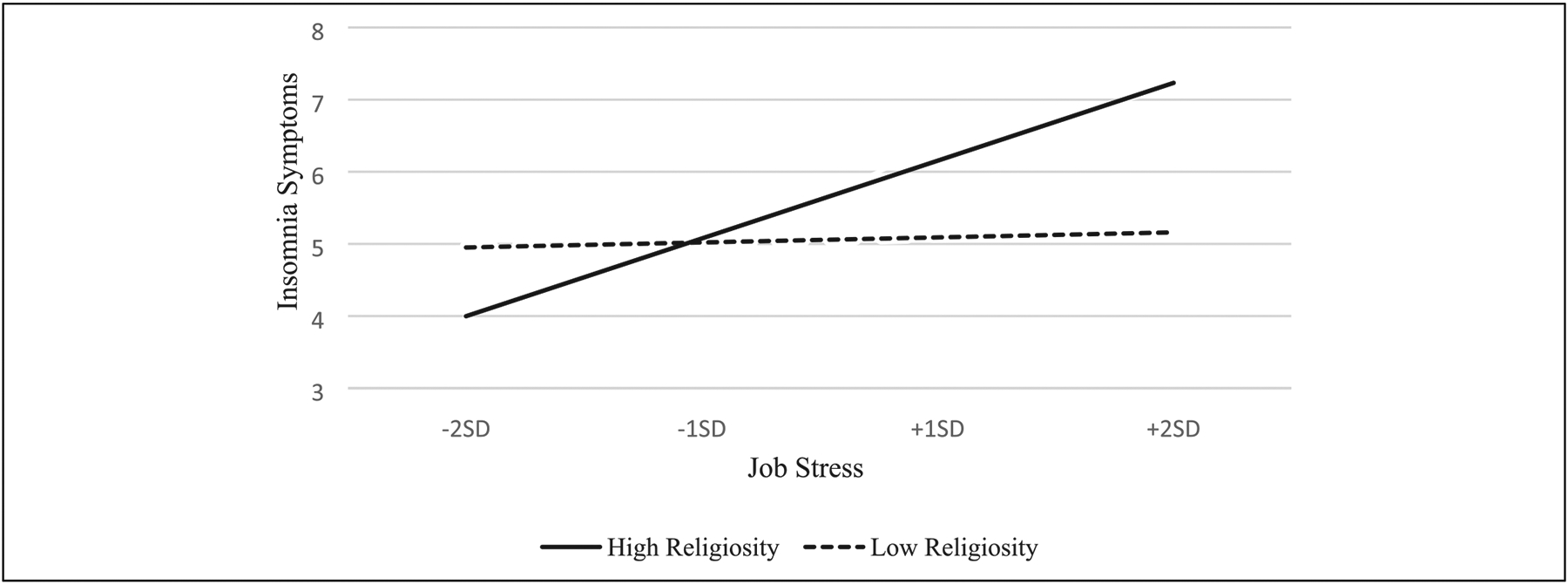
Interaction of job stress and religiosity on insomnia symptoms.
Discussion
The primary focus of this study was to examine the effects of work-related stress on insomnia symptoms among older Black workers. We also sought to investigate whether psychosocial resources, such as mastery, social support, and religious involvement, have direct, mediating, and moderating effects. Findings show that work-related stress undermines sleep quality. Specifically, older Black workers who continue to work due to economic necessity are at an increased risk for insomnia symptoms. Likewise, job stress is also associated with increased symptoms of insomnia. These findings are broadly consistent with previous research on links between work-related stress and poor sleep.
Notably, we found no evidence that psychosocial resources mediate the effect of job lock and job stress on insomnia symptoms. This suggests that the psychosocial resources examined in this study do not lie on the causal pathway between work-related stress and insomnia symptoms, and that workplace stressors likely impact sleep via other mechanisms. Results, however, did reveal evidence of moderation processes whereby religious attendance and religiosity buffered and exacerbated, respectively, the effects of work-related stress on insomnia symptoms. First, religious attendance buffered the effects of job lock on insomnia symptoms. Specifically, higher levels of religious attendance diminished the harmful effects of financial job lock on insomnia symptoms. Religious attendance is an important coping strategy because it can provide a sense of meaning, community, and access to faith-based social support (Chatters et al., 2008, 2015). For older Black workers, engaging with people who share the same beliefs can be a source of comfort and relief from a stressful work environment. Church members can provide emotional and informational support regarding ways to deal with stress, encouragement to rely on divine control of stressful situations, and provide information about better economic opportunities (Chatters et al. 2015). The buffering effect of religious attendance found in this study is not only consistent with previous research, (Bierman et al., 2018) but it also aligns with other models of the religion-health connection such as the stressor response model, which suggests that individuals increase the frequency of religious behaviors (e.g., religious attendance) when faced with stressors (Ellison & Levin, 1998). It is worth noting that while research suggests that gender is related to both job stress and insomnia symptoms, this study did not find evidence of gender differences in the relationship between work-related stress and insomnia symptoms.
Second, the deleterious effects of jobs stress on symptoms of insomnia are exacerbated in the presence of high religiosity. These findings align with research that reveal that religiousness may be harmful for individual well-being (Ellison & Lee, 2010). For example, Lechner et al. (2014) found that religiosity exacerbated the association between family-related uncertainties and psychological distress. In the context of this study, perhaps when faced with persistent job stress, older Black workers, with a high degree of religiosity, may begin to have religious doubts about why they are continuing to work under stressful conditions and lacking finances if “God is in control.” Furthermore, job stress may provoke feelings of disappointment that one’s circumstances have not changed or induce spiritual struggles, such as religious doubting—which can undermine well-being (Ellison & Lee, 2010).
Although there was no evidence of mediation and limited support for moderation processes involving the other psychosocial resources examined, there are additional results from this study that warrant further discussion. For example, unlike previous research (Crain et al., 2014; Nordin et al., 2012; Pow et al., 2017), we did not find evidence for an effect of social support on sleep (direct, mediating, or moderating). Although social support from family and friends are beneficial to older Blacks, perhaps when faced with work-related stressors, social support from the work environment (e.g., supervisors, co-workers) may be more beneficial. While having social support from the work environment does not negate work-related stressors, older Black workers, who may feel isolated on the job due to race- or age-based discrimination, may take comfort in knowing that they are not alone in experiencing work-related stressors, such as financial job lock. Although there are measures of supervisor and co-worker support in the HRS Psychosocial Leave Behind, these questions were not asked in the waves of data used in this study.
This study is not without limitations. First, the analysis is cross-sectional. As such, we are unable to determine causality of the relationship between work-related stress and insomnia symptoms. While it is likely that work-related stress gives rise to symptoms of insomnia, an inability to get quality sleep can also affect work performance in ways that may give rise to stress. Future research should use longitudinal data to examine the effects of work-related stress on sleep among older Black workers. Second, our measure of job stress does not provide details about specific work-related stressors older Black Americans may be experiencing. Specifically, there are numerous job stressors such as physical demanding jobs, workplace discrimination, and ageism that are more specific; perhaps some job stressors are more harmful to sleep compared to others. Finally, the psychosocial measures used in this study may be more effective in dealing with purely mental health outcomes. While sleep clearly has a psychological component, it also strongly influenced by physiological processes. As such, resources that reduce stress hormones may be more effective in dealing with work-related stress. Examining physical activity as stress reliever in older Black workers is a promising area for future study.
Despite these limitations, this study has several strengths. One important contribution is the examination of the experience of older Black workers who are often invisible in the literature. Considering increased labor force participation by older Blacks, understanding their workplace experiences is important to ensure supportive working environments. We also examine an understudied health outcome—insomnia symptoms. Sleep is an important aspect of maintaining good mental and physical health, which is particularly vital for older adults who are already at increased risk for poor sleep due to aging processes. Understanding how social determinants affect sleep can provide more insight about the causal path linking stress and mental and physical health. Moreover, we contribute to the literature on the role of psychosocial resources as mediators or moderators of stress within both a marginalized population (i.e., older Black workers) and an under-examined health outcome (i.e., sleep). Taken together, findings underscore the utility of the Stress Process Model for understanding diverse stress and health experiences in later life. Furthermore, results from this study have the potential to inform policies and practices to restructure the workplace in ways that are less stressful for older Black workers.
Acknowledgments
The authors would like to thank Dr. Christy Erving for feedback on this project. The authors also acknowledge feedback from anonymous reviewers, which helped improve the final version of the paper.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Duke Aging Center Postdoctoral Research Training Grant (NIA T32 AG000029).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Aneshensel CS, & Mitchell UA (2014). The stress process: Its origins, evolution, and future. In Aneshensel CS, & Phelan JC (Eds.), Sociology of mental health (pp. 53–74). Springer. 10.1007/978-3-319-07797-0_3. [DOI] [Google Scholar]
- Baron RM,, & Kenny DA (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bazargan M, Mian N, Cobb S, Vargas R, & Assari S (2019). Insomnia Symptoms among African American Older Adults in Economically Disadvantaged Areas of South Los Angeles. Brain Sciences, 9(11), 306. 10.3390/brainsci9110306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bierman A, Lee Y, & Schieman S (2018). Chronic discrimination and sleep problems in late life: Religious involvement as buffer. Risk Analysis: an Official Publication of the Society for Risk Analysis, 40(10), 933–955. 10.1177/0164027518766422. [DOI] [PubMed] [Google Scholar]
- Bonilla-Silva E (1997). Rethinking racism: Toward a structural interpretation. Archives of Suicide Research: Official Journal of the International Academy for Suicide Research, 62(3), 465–480. 10.2307/2657316. [DOI] [Google Scholar]
- Brown E, Jackson JS, & Faison NA (2006). The work and retirement experiences of aging Black Americans. Annual Review of Gerontology and Geriatrics, 26(1), 39–60. 10.1891/0198-8794.26.1.39. [DOI] [Google Scholar]
- Brown TH (2016). Diverging fortunes: Racial/ethnic inequality in wealth trajectories in middle and late life. Race and Social Problems, 8(1), 29–41. 10.1007/s12552-016-9160-2. [DOI] [Google Scholar]
- Brown TH (2018). Racial stratification, immigration, and health inequality: A life course-intersectional approach. Social Forces, 96(4), 1507–1540. 10.1093/sf/soy013. [DOI] [Google Scholar]
- Brown TH, & Hargrove TW (2018). Psychosocial mechanisms underlying older Black men’s health. The Journals of Gerontology: Series B, 73(2), 188–197. 10.1093/geronb/gbx091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown T, & Homan P (2022, March 21). Structural Racism and Health Stratification in the U.S.: Connecting Theory to Measurement. 10.31235/osf.io/3eacp [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgard SA, & Ailshire JA (2009). Putting work to bed: stressful experiences on the job and sleep quality. Journal of Health and Social Behavior, 50(4), 476–492. 10.1177/002214650905000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buxton OM, & Marcelli E (2010). Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Social Science & Medicine, 71(5), 1027–1036. 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- Cairney J, & Krause N (2008). Negative life events and age-related decline in mastery: Are older adults more vulnerable to the control-eroding effect of stress? The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 63(3), S162–S170. 10.1093/geronb/63.3.s162. [DOI] [PubMed] [Google Scholar]
- Chatters LM, Taylor RJ, Jackson JS, & Lincoln KD (2008). Religious coping among African Americans, Caribbean Blacks and non-Hispanic whites. Journal of Community Psychology, 36(3), 371–386. 10.1002/jcop.20202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatters LM, Taylor RJ, Woodward AT, & Nicklett EJ (2015). Social support from church and family members and depressive symptoms among older African Americans. The American Journal of Geriatric Psychiatry, 23(6), 559–567. 10.1016/j.jagp.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crain TL, Hammer LB, Bodner T, Kossek EE, Moen P, Lilienthal R, & Buxton OM (2014). Work-family conflict, family-supportive supervisor behaviors (FSSB), and sleep outcomes. Journal of Occupational Health Psychology, 19(2), 155–167. 10.1037/a0036010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellison C, DeAngelis R, & Güven M (2017). Does religious involvement mitigate the effects of major discrimination on the mental health of African Americans? Findings from the Nashville Stress and Health Study. Religions, 8(9), 195. 10.3390/rel8090195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellison CG, Bradshaw M, Storch J, Marcum JP, & Hill TD (2011). Religious doubts and sleep quality: Findings from a nationwide study of Presbyterians. Review of Religious Research, 53(2), 119–136. 10.1007/s13644-011-0019-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellison CG, Hummer RA, Cormier S, & Rogers RG (2000). Religious involvement and mortality risk among African American adults. Risk Analysis: an Official Publication of the Society for Risk Analysis, 22(6), 630–667. 10.1177/0164027500226003. [DOI] [Google Scholar]
- Ellison CG, & Lee J (2010). Spiritual struggles and psychological distress: Is there a dark side of religion? Social Indicators Research, 98(3), 501–517. 10.1007/s11205-009-9553-3. [DOI] [Google Scholar]
- Ellison CG, & Levin JS (1998). The religion-health connection: Evidence, theory, and future directions. Health Education & Behavior, 25(6), 700–720. 10.1177/109019819802500603. [DOI] [PubMed] [Google Scholar]
- Emily R, & Toossi M (2018). Blacks in the labor force. Career Outlook. U.S. Bureau of Labor Statistics. Retrieved from https://www.bls.gov/careeroutlook/2018/article/Blacks-in-the-labor-force.htm (February 2018). [Google Scholar]
- Epps F, & Williams IC (2020). The importance of religiosity to the well-being of African American older adults living with dementia. Journal of Applied Gerontology, 39(5), 509–518. 10.1177/0733464818820773. [DOI] [PubMed] [Google Scholar]
- Federal Interagency Forum on Aging-Related Statistics. (2020). Older Americans 2020: Key indicators of well-being. U.S. Government Printing Office. [Google Scholar]
- Fisher GG, Ryan LH, Sonnega A, & Naudé MN (2016). Job lock, work, and psychological well-being in the United States. Work, Aging and Retirement, 2(3), 345–358. 10.1093/workar/waw004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia MA, Homan PA, García C, & Brown TH (2021). The color of COVID-19: Structural racism and the disproportionate impact of the pandemic on older Black and Latinx adults. The Journals of Gerontology: Series B, 76(3), e75–e80. 10.1093/geronb/gbaa114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glazer S, & Liu C (2017). Work, stress, coping, and stress management. In Oxford Research Encyclopedia of Psychology. Published Online. 10.1093/acrefore/9780190236557.013.30. [DOI] [Google Scholar]
- Goosby BJ, Cheadle JE, & Mitchell C (2018). Stress-related biosocial mechanisms of discrimination and African American health inequities. Annual Review of Sociology, 44(1), 319–340. 10.1146/annurev-soc-060116-053403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gow AJ, Corley J, Starr JM, & Deary IJ (2013). Which social network or support factors are associated with cognitive abilities in old age? Gerontology, 59(5), 454–463. 10.1159/000351265. [DOI] [PubMed] [Google Scholar]
- Guzman E, & Vulimiri M (2015). African American retirement insecurity. Center for Global Policy Solutions. [Google Scholar]
- Hale L, Troxel W, & Buysse DJ (2020). BuysseSleep Health: An Opportunity for Public Health to Address Health Equity. Annual Review of Public Health, 41(1), 81–99. 10.1146/annurev-publhealth-040119-094412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson AK (2016). Jesus didn’t teach us to juggle: Religious involvement, work-family conflict, and life satisfaction among African Americans. Journal of Family Issues, 37(11), 1558–1584. . [DOI] [Google Scholar]
- Hicken MT, Lee H, Ailshire J, Burgard SA, & Williams DR (2013). Every shut eye, ain’t sleep”: The role of racism-related vigilance in racial/ethnic disparities in sleep difficulty. Race and Social Problems, 5(2), 100–112. 10.1007/s12552-013-9095-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill TD, Burdette AM, Ellison CG, & Musick MA (2006). Religious attendance and the health behaviors of Texas adults. Preventive Medicine, 42(4), 309–312. 10.1016/j.ypmed.2005.12.005. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, & Layton JB (2010). Social relationships and mortality risk: A meta-analytic review. Plos Medicine, 7(7), e1000316. 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homan KJ, & Boyatzis CJ (2010). Religiosity, sense of meaning, and health behavior in older adults. The International Journal for the Psychology of Religion, 20(3), 173–186. 10.1080/10508619.2010.481225. [DOI] [Google Scholar]
- Jackson CL, Redline S, & Emmons KM (2015). Sleep as a potential fundamental contributor to disparities in cardiovascular health. Annual Review of Public Health, 36, 417–440. 10.1146/annurev-publhealth-031914-122838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, & Knight KM (2006). Race and self-regulatory health behaviors: The role of the stress response and the HPA axis in physical and mental health disparities. In Schaie KW & Carstensen LL (Eds.), Social structures, aging, and self-regulation in the elderly (pp. 189–239). Springer Publishing Company. [Google Scholar]
- Jang Y, Chiriboga DA, & Small BJ (2008). Perceived discrimination and psychological well-being: The mediating and moderating role of sense of control. The International Journal of Aging and Human Development, 66(3), 213–227. 10.2190/AG.66.3.c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson DA, Lisabeth L, Lewis TT, Sims M, Hickson DA, Samdarshi T, Taylor H, & Diez Roux AV (2016). The contribution of psychosocial stressors to sleep among African Americans in the Jackson Heart Study. Sleep, 39(7), 1411–1419. 10.5665/sleep.5974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson RW (2011). 50+ african American workers: A status report, implications, and recommendations. https://assets.aarp.org/rgcenter/econ/aa-workers-11.pdf.
- Kecklund G, & Axelsson J (2016). Health consequences of shift work and insufficient sleep. Bmj: British Medical Journal, 355, i5210. 10.1136/bmj.i5210. [DOI] [PubMed] [Google Scholar]
- Keith VM (2014). Stress, discrimination, and coping in late life. In Whitfield KE, & Baker T (Eds.), Handbook of Minority Aging (pp. 65–84). Springer. [Google Scholar]
- Kijakazi K, Smith KE, & Runes C (2019). African American economic security and the role of Social Security. Library Catalog. [Google Scholar]
- Knudsen HK, Ducharme LJ, & Roman PM (2007). Job stress and poor sleep quality: data from an American sample of full-time workers. Social Science & Medicine, 64(10), 1997–2007. 10.1016/j.socscimed.2007.02.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause N, & Ironson G (2017). Is involvement in religion associated with better sleep quality? Pastoral Psychology, 66(5), 595–608. 10.1007/s11089-017-0766-0. [DOI] [Google Scholar]
- Lawler-Row KA (2010). Forgiveness as a mediator of the religiosity—Health relationship. Plastic and Reconstructive Surgery, 2(1), 1–16. 10.1037/a0017584. [DOI] [Google Scholar]
- Lechner CM, Tomasik MJ, Silbereisen RK, & Wasilewski J (2014). Religiosity reduces family-related uncertainties but exacerbates their association with distress. The International Journal for the Psychology of Religion, 24(3), 185–200. 10.1080/10508619.2013.847700. [DOI] [Google Scholar]
- Leggett AN, Sonnega AJ, & Lohman MC (2018). The association of insomnia and depressive symptoms with all-cause mortality among middle-aged and old adults. International Journal of Geriatric Psychiatry, 33(9), 1265–1270. 10.1002/gps.4923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincoln KD (2007). Financial strain, negative interactions, and mastery: Pathways to mental health among older African Americans. Journal of Black Psychology, 33(4), 439–462. 10.1177/0095798407307045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linton SJ (2004). Does work stress predict insomnia? A prospective study. British Journal of Health Psychology, 9(2), 127–136. [DOI] [PubMed] [Google Scholar]
- Liu Y, Croft JB, Wheaton AG, Perry GS, Chapman DP, Strine TW, McKnight-Eily LR, & Presley-Cantrell L (2013). Association between perceived insufficient sleep, frequent mental distress, obesity and chronic diseases among US adults, 2009 behavioral risk factor surveillance system. BMC Public Health, 13(1), 84–88. 10.1186/1471-2458-13-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lunau T, Wahrendorf M, Dragano N, & Siegrist J (2013). Work stress and depressive symptoms in older employees: impact of national labour and social policies. BMC Public Health, 13(1), 1086. 10.1186/1471-2458-13-1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lunau T, Wahrendorf M, Müller A, Wright B, & Dragano N (2018). Do resources buffer the prospective association of psychosocial work stress with depression? Longitudinal evidence from ageing workers. Scandinavian Journal of Work, Environment & Health, 44, 183–191. 10.5271/sjweh.3694. [DOI] [PubMed] [Google Scholar]
- Luyster FS, Strollo PJ, Zee PC, & Walsh JK (2012). Sleep: a health imperative. Sleep, 35(6), 727–734. 10.5665/sleep.1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezuk B, Kershaw KN, Hudson D, Lim KA, & Ratliff S (2011). Job strain, workplace discrimination, and hypertension among older workers: The health and retirement study. Race and Social Problems, 3(1), 38–50. 10.1007/s12552-011-9041-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milaneschi Y, Bandinelli S, Corsi AM, Vazzana R, Patel KV, Ferrucci L, & Guralnik JM (2010). Personal mastery and lower body mobility in community-dwelling older persons: The Invecchiare in Chianti study. Journal of the American Geriatrics Society, 58, 98–103. 10.1111/j.1532-5415.2009.02611.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore K, Ghilarducci T, & Webb A (2019). The inequitable effects of raising the retirement age on blacks and low-wage workers. The Review of Black Political Economy, 46(1), 22–37. 10.1177/0034644619843529. [DOI] [Google Scholar]
- Mutambudzi M, & Javed Z (2016). Job strain as a risk factor for incident diabetes mellitus in middle and older age US workers. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 71(6), 1089–1096. 10.1093/geronb/gbw091. [DOI] [PubMed] [Google Scholar]
- Nguyen AW (2020). Religion and mental health in racial and ethnic minority populations: A review of the literature. Innovation in Aging, 4(5), 1–13. 10.1093/geroni/igaa035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordin M, Westerholm P, Alfredsson L, & Åkerstedt T (2012). Social support and sleep: Longitudinal relationships from the WOLF study. Psychology, 3(12A), 1223–1230. 10.4236/psych.2012.312a181. [DOI] [Google Scholar]
- Pearlin LI (1999). The stress process revisited: Reflections on concepts and their interrelationships. In Aneshensel CS, & Phelan JC (Eds.), Handbook of the sociology of mental health (pp. 395–415). Kluwer Academic/Plenum. 10.1007/0-387-36223-1_19. [DOI] [Google Scholar]
- Pearlin LI, & Bierman A (2013). Current Issues and Future Directions in Research into the Stress Process. In Aneshensel CS, Phelan JC, & Bierman A (Eds.), −40 in Handbook of the Sociology of Mental Health (2nd ed., pp. 325–340). Springer. 10.1007/978-94-007-4276-5_16. [DOI] [Google Scholar]
- Pearlin LI, Lieberman MA, Menaghan EG, & Mullan JT (1981). The stress process. Journal of Health and Social Behavior, 22(4), 337–356. 10.2307/2136676. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Schieman S, Fazio EM, & Meersman SC (2005). Stress, health, and the life course: Some conceptual perspectives. Journal of Health and Social Behavior, 46(2), 205–219. 10.1177/002214650504600206. [DOI] [PubMed] [Google Scholar]
- Pow J, King DB, Stephenson E, & DeLongis A (2017). Does social support buffer the effects of occupational stress on sleep quality among paramedics? A daily diary study. Journal of Occupational Health Psychology, 22(1), 71–85. 10.1037/a0040107. [DOI] [PubMed] [Google Scholar]
- Pudrovska T, Schieman S, Pearlin LI, & Nguyen K (2005). The sense of mastery as a mediator and moderator in the association between economic hardship and health in late life. Journal of Aging and Health, 17(5), 634–660. 10.1177/0898264305279874. [DOI] [PubMed] [Google Scholar]
- Rhee N (2013). Race and retirement insecurity in the United States. National Institute on Retirement Security. [Google Scholar]
- Roepke SK, & Grant I (2011). Toward a more complete understanding of the effects of personal mastery on cardiometabolic health. Health Psychology, 30(5), 615–632. 10.1037/a0023480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seybold KS (2007). Physiological mechanisms involved in religiosity/spirituality and health. Journal of Behavioral Medicine, 30(4), 303–309. 10.1007/s10865-007-9115-6. [DOI] [PubMed] [Google Scholar]
- Simpson C, Allegra JC, Ezeamama AE, Elkins J, & Miles T (2014). The impact of mid- and late-life loss on insomnia: Findings from the health and retirement study, 2010 cohort. Family & Community Health, 37(4), 317–326. 10.1097/FCH.0000000000000039. [DOI] [PubMed] [Google Scholar]
- Sobel ME (1982). Asymptotic confidence intervals for indirect effects in structural equation models. Sociological Methodology, 13, 290–312. 10.2307/270723. [DOI] [Google Scholar]
- Taylor RJ, Chatters LM, & Brown RK (2014). African American religious participation. Review of Religious Research, 56(4), 513–538. 10.1007/s13644-013-0144-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, & Jackson JS (2007). Religious and spiritual involvement among older African Americans, Caribbean Blacks, and non-Hispanic whites: Findings from the national survey of American life. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 62(4), S238–S250. 10.1093/geronb/62.4.s238. [DOI] [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, & Levin J (2003). Religion in the lives of African Americans: Social, psychological, and health perspectives. Sage Publications. [Google Scholar]
- Thoits PA (2010). Stress and health: Major findings and policy implications. Journal of Health and Social Behavior, 51 Suppl(1_-suppl), S41–S53. 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- Troxel WM, Buysse DJ, Monk TH, Begley A, & Hall M (2010). Does social support differentially affect sleep in older adults with versus without insomnia?. Journal of Psychosomatic Research, 69(5), 459–466. 10.1016/j.jpsychores.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Robles TF, Hall M, & Buysse DJ (2007). Marital quality and the marital bed: Examining the covariation between relationship quality and sleep. Sleep Medicine Reviews, 11(5), 389–404. 10.1016/j.smrv.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingfield AH, & Chavez K (2020). Getting in, getting hired, getting sideways looks: Organizational hierarchy and perceptions of racial discrimination. Archives of Suicide Research: Official Journal of the International Academy for Suicide Research, 85(1), 31–57. 10.1177/0003122419894335. [DOI] [Google Scholar]


