Abstract
Background. Across settings, individuals from populations that are multiply stigmatized are at increased risk of HIV and experience worse HIV treatment outcomes. As evidence expands on how intersecting stigmatized identities and conditions influence HIV outcomes, researchers have used diverse quantitative approaches to measure HIV-related intersectional stigma and discrimination. To date, no clear consensus exists regarding how to best quantitatively measure and analyze intersectional stigma and discrimination.
Objectives. To review and document existing quantitative measures of HIV-related intersectional stigma and discrimination to inform research, programmatic, and policy efforts.
Search Methods. We searched 5 electronic databases for relevant studies. References of included articles were screened for possible inclusion. Additional articles were screened on the basis of consultations with experts in the field.
Selection Criteria. We included peer-reviewed studies published between January 1, 2010, and May 12, 2021, that were HIV related and presented 1 or more quantitative measures of stigma and discrimination using an intersectional lens in measure design or analysis.
Data Collection and Analysis. Systematic methods were used to screen citations and abstract data via a standardized coding form. Data were analyzed by coding categories stratified according to 2 subgroups: (1) studies incorporating a single intersectional measure and (2) studies that examined intersectional stigma through analytical approaches combining multiple measures.
Main Results. Sixteen articles met the inclusion criteria, 7 of which explicitly referenced intersectionality. Ten studies were from the United States. All of the studies included participants living with HIV. Among the 4 studies incorporating a single intersectional stigma measure, 3 explored race and gender stigma and 1 explored gender and HIV stigma. Studies involving analytic approaches (n = 12) mostly examined intersectional stigma via interaction terms in multivariate regression models. Three studies employed structural equation modeling to examine interactive effects or latent constructs of intersectional stigma.
Conclusions. Research on the measurement of HIV-related intersectional stigma and discrimination is currently concentrated in high-income settings and generally focuses on the intersection of 2 identities (e.g., race and gender). Efforts are needed to expand appropriate application of intersectionality in the development, adaptation, and use of measures of HIV-related intersectional stigma and discrimination. The use of context-, identity-, or condition-adaptable measures should be considered. Researchers should also carefully consider how to meaningfully engage communities in the process of measurement development.
Public Health Implications. The measures and analytic approaches presented could significantly enhance public health efforts in assessing the impact of HIV-related intersectional stigma and discrimination on critical health outcomes. (Am J Public Health. 2022;112(S4):S420–S432. https://doi.org/10.2105/AJPH.2021.306639)
Plain-Language Summary
We conducted a systematic review of peer-reviewed studies to document existing quantitative measures of HIV-related intersectional stigma and discrimination as a means of informing research, programmatic, and policy efforts. We included studies published between January 1, 2010, and May 12, 2021, that were HIV related, incorporated 1 or more quantitative measures of stigma and discrimination, and involved the use of an intersectional lens in measurement design or analysis. A total of 16 articles met the inclusion criteria. Among these, 7 studies explicitly referenced intersectionality, 10 were conducted in the United States, and all included participants living with HIV. Most studies examined intersectional stigma through analytic approaches (n = 12), with the majority exploring stigma via interaction terms in multivariate regression models. Only 4 studies examined intersectional stigma via a single, intersectional measure. Our results indicate that measurement of HIV-related intersectional stigma and discrimination is concentrated in high-income settings and generally focuses on the intersection of 2 identities (e.g., race and gender). Efforts are needed to expand appropriate application of intersectionality in quantitative HIV research, including intersectional stigma related to more than 2 identities, statuses, or conditions. Careful consideration should be given to how we engage communities and honor the principles of intersectionality when adapting measures for intersectional HIV research.
More than 20 years ago, African American feminist legal scholar Kimberlé Crenshaw used the term “intersectionality” to describe how multiple forms of inequalities, mainly due to race and gender, were embedded in the United States legal system and often intersected to create distinct barriers for marginalized individuals and groups.1 Through her work describing the unique experiences of discrimination and violence among African American women in the United States, she argued that individuals’ specific social realities are based on their affiliation to multiple marginalized identities and social positions.1,2 In coining the term intersectionality, Crenshaw drew on the work of previous Black feminists3,4 and argued that Black women’s experiences were more than the sum of their parts (e.g., being both Black and women), instead converging from interdependent systems of power and oppression.1,5
Over the past decade, interest in applying intersectionality as a theoretical lens and orientation to study health inequities—including in relation to HIV prevention, treatment, and care—has grown exponentially.2 The groups at highest risk for acquiring HIV in the United States and globally are those whose identities encompass multiple socially stigmatized populations, such as marginalized groups at the intersections of racial/ethnic, gender, and sexual minority status. Possible examples of groups at these unique intersections include young Latinx and Black men who have sex with men in the United States,6,7 Black and Latina transgender women living in the United States,8 and young Black women and girls in South Africa.9
Studies have also shown that people living with HIV who are members of multiply stigmatized population groups experience worse HIV treatment and care outcomes than those who are not members of such groups.10,11 For example, female sex workers living with HIV have been found to have lower rates of antiretroviral therapy adherence and viral suppression than women living with HIV who are not sex workers.12 Given this, HIV researchers have increasingly sought to understand the role of intersecting marginalized identities and conditions in shaping HIV outcomes.13–17
Understanding the complex relationships between intersectional stigmatized identities, socially marginalized positions, and HIV outcomes warrants nuanced methodological approaches.18–20 In recent years, scholars have increasingly used quantitative approaches to document and measure HIV-related intersectional stigmas and discrimination to appropriately intervene and address these challenges. However, to date, there is no clear consensus within the field regarding how to best quantitatively measure and analyze intersectional stigma and discrimination,18 including as it relates to HIV stigma. Of particular debate is whether and how intersections can be captured within a given measure or scale or be reflected through examinations of the interplay between measures of distinct types of stigma.18,20,21 Also, there is significant variation in how researchers analyze that interplay, for instance whether it is modeled via additive or multiplicative approaches.18,20,21
Given the critical need to investigate the effects of intersectional stigma on HIV-related outcomes and ongoing methodological questions, we sought to examine the state of the evidence regarding measurement of HIV-related intersectional stigma and discrimination by conducting a systematic review of peer-reviewed literature published over the past 10 years. We were motivated by a conceptualization of intersectional stigma that acknowledges the interplay of stigmas either through measurement itself or through intersectional analytic approaches. Through this review, we aim to document HIV-related intersectional stigma and discrimination measures that can serve as a key reference for researchers, practitioners, and community members to use in future research, programmatic, and policy efforts.
METHODS
Guided by previous work,5,22 we defined intersectional stigma as internalized, perceived, anticipated, or enacted stigma (the latter also referred to here as discrimination23,24) related to the unique intersection of multiple marginalized identities, statuses, or conditions. Using this definition, we explored measures and analytic models related to intersectional stigma, focusing on any 2 or more intersections of social stigmas (e.g., substance use, sex work) or interlocking systems of oppression (e.g., race, gender, class) relevant for understanding HIV-related risks and outcomes.
Inclusion Criteria
We included studies in the review if they met the following criteria:
-
1.
They presented work relevant to HIV risk and outcomes. Examples of these studies are those that (a) included people living with HIV, (b) compared populations of people living with HIV with those not living with HIV, or (c) assessed an HIV-related outcome (e.g., HIV stigma, HIV prevention, or HIV care and treatment outcomes).
-
2.
They presented information on stigma measures using an intersectional lens. This included (a) single measures (i.e., scales, indices, or indicators) that considered stigma experiences at unique intersections (e.g., one scale measuring the specific stigma experiences of Black women living with HIV) and (b) multiple measures that considered the intersectional nature of multiple forms of stigma (e.g., one measure of HIV stigma and a separate measure of racism). If multiple measures were used, we required authors to explore their intersectional effects through analytic approaches (e.g., interaction terms, latent variable models combining multiple stigma measures).
-
3.
They presented quantitative data.
-
4.
They were published in a peer-reviewed journal between January 1, 2010, and May 12, 2021.
Exclusion Criteria
We excluded studies if they met any of the following criteria:
-
1.
They did not examine intersectional stigma or discrimination. This includes studies that measured one form of stigma (e.g., HIV stigma, sex work stigma) among vulnerable populations but did not consider the other unique identities, statuses, or conditions of those populations.
-
2.
They used exclusively additive analytic approaches to explore intersectional stigma or discrimination. This includes studies combining multiple indexes or measures to yield a single sum score capturing intersectional stigma or discrimination. Such approaches assume that each stigmatized identity, social status, or condition is independent from the others,20,25 which does not align with our conceptualization of intersectional stigma.
-
3.
They included multiple stigma measures but did not bring them together analytically (e.g., studies that entered multiple stigma scales independently in a regression model but did not use interaction terms to explore their intersecting effects).
-
4.
They presented research on perpetration of stigma rather than experiences of stigma.
-
5.
They were conference abstracts, commentaries or editorials, protocol papers, or exclusively qualitative studies.
We did not restrict studies according to design, geographic location, subgroups, or language.
Search Strategy and Terms
We searched 5 electronic databases (PubMed, PsycINFO, the Cumulative Index to Nursing and Allied Health Literature, EMBASE, and the Cochrane Library) for relevant studies. Our search terms included (1) HIV or AIDS; (2) stigma, discrimination, and other relevant terms; and (3) intersectional, interlocking, layered, and other relevant terms (full search terms are available from the authors upon request). We also reviewed secondary references of included articles for possible inclusion of other relevant work. Finally, we consulted with 2 key experts in the field to identify any additional studies.
Screening
After deduplicating our search results, we screened articles for inclusion. Screening occurred in 3 phases. First, 1 trained study member screened the titles, abstracts, and citation information of all records and removed irrelevant articles. Second, resulting titles and abstracts were screened in duplicate by 2 trained study members working independently. Third, studies were pulled for full-text reviews on the basis of consensus between the 2 reviewers, with referral to senior study members as needed. Any article for which no consensus regarding inclusion was reached was included in a full-text review. Finally, we obtained full-text articles of all selected abstracts, and 2 members of the team independently assessed these articles to determine final study selection. During each phase, we retained excluded articles that were relevant and could serve as background material for our review.
Data Abstraction
Two trained study members completed the data abstraction of all included articles. Data abstraction was conducted in duplicate for the first 10 articles, with differences resolved through consensus and referral to a senior study team member when necessary. Two reviewers independently conducted the remaining abstraction. A standardized coding form was used to gather the following information from each included study: study identification (authors and year of publication), study description (study design and setting, period of study, sample size, and relevant study population characteristics), authors’ conceptualization of intersectionality, types of intersectional stigma assessed, form and level of stigma, information on measures (e.g., description, rigor), relevant intersectional stigma results, study limitations, source of funding, and references for secondary screening.
We classified forms of stigma as internalized (feelings of inferiority or of deserved negative outcomes owing to one’s affiliation to a marginalized identity, status, or condition), perceived (perceptions of stigmatizing attitudes by the public toward one’s affiliated group), anticipated (expectations of poor treatment or outcomes owing to one’s affiliation to a marginalized identity, status, or condition), and enacted (unjust treatment due to one’s affiliation to a marginalized identity, status, or condition).26,27 Furthermore, we classified levels of stigma as individual (stigma held within individuals), interpersonal (stigma occurring between individuals), societal (stigma exhibited by members of communities), and structural (stigma within institutions and structures of power).
Data Analysis
All data were analyzed through coding of categories. We stratified analyses by 2 subgroups: (1) studies that incorporated a single intersectional measure (e.g., stigma toward women living with HIV) and (2) studies that examined intersectional stigma through the use of analytical approaches bringing together multiple stigma measures (e.g., interactive effects of HIV and gender stigmas). Given the heterogeneity in populations, study designs, measures, types of stigma, and outcomes, we did not conduct a meta-analysis of the data and instead present the synthesized data narratively.
RESULTS
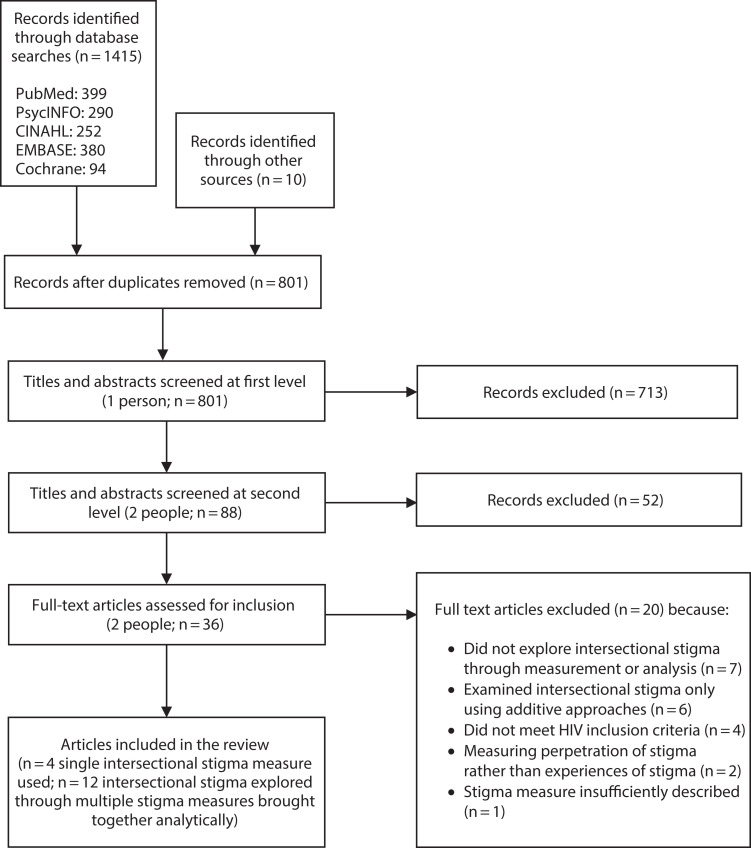
A total of 1415 published citations were identified through our initial search, and 10 additional citations were identified from consultation with 2 key experts (Figure 1). After removal of duplicates, 801 citations were part of the first-level title and abstract screening, with 713 records excluded during this phase. In addition, 88 citations were part of the second-level title and abstract screening, resulting in the further exclusion of 52 citations.
FIGURE 1—
Citation Search and Screening Process: HIV-Related Intersectional Stigma and Discrimination Measurement, January 1, 2010–May 12, 2021
The remaining 36 citations were included in the full-text review.21,28–62 Of these 36 citations, 20 were excluded because they did not explore intersectional stigma through either a single measure or a combined analytic approach,21,28–33 they examined intersectional stigma through an additive approach,34–39 they were insufficiently HIV related,40–43 they measured stigma perpetration rather than experiences of stigma,44,45 or their description of stigma measures or analyses was insufficient, precluding our ability to understand the authors’ assessment of intersectional stigma.46 This resulted in 16 articles meeting the inclusion criteria for our review.
Study Descriptions
Table 1 presents a description of the 16 included studies.47–62 Of these studies, 10 were conducted in the United States, 2 in Russia, 1 in Botswana, 1 in Canada, 1 in China, and 1 in the Dominican Republic. Some studies collected data in multiple languages (data not shown), including 3 studies in the United States53,56,60 conducted among English- and Spanish-speaking participants, 1 study in Canada59 conducted among English- and French-speaking participants, and 1 study in Botswana50 conducted among Setswana- and English-speaking participants.
TABLE 1—
Description of Included Studies Using an Intersectional Stigma Measure or Analytic Approach: HIV-Related Intersectional Stigma and Discrimination Measurement, January 1, 2010–May 12, 2021
| Authors | Setting | Population | Analytic Sample, No. | Study Design | Outcomes Studied |
| Baguso et al.47 | United States | Transgender women living with HIV | 123 | Cross sectional | Engagement with HIV care, ART use, detectable or unknown viral load |
| Bogart et al.51 | United States | Black, African American MSM living with HIV | 152 | Prospective cohort | ART adherence |
| Bogart et al.52 | United States | Black, African American MSM living with HIV | 181 | Cross sectional (baseline survey as part of prospective study) | Depression, PTSD |
| Bogart et al.53 | United States | Black and Latino MSM living with HIV | 181 Black participants, 167 Latino participants | Prospective (Black participants), cross sectional (Latino participants) | Side effect severity, AIDS symptoms, CD4 cell count, undetectable viral load, emergency department use |
| Calabrese et al.54 | Russia | People living with HIV who inject drugs | 383 | Cross sectional | Health status, health service use |
| Carrasco et al.55 | Dominican Republic | Cis-gender female sex workers living with HIV | 228 | Cross sectional (follow-up data from a prospective cohort study) | Consistent condom use, social cohesion |
| Dale and Safren48 | United States | Cis-gender Black women living with HIV | 100 | Cross sectional (baseline data from an intervention study) | PTSD symptoms, posttraumatic cognitions |
| Dale et al.49 | United States | Cis-gender Black women living with HIV | 100 | Cross sectional (baseline data from an intervention study) | Barriers to HIV-related care |
| Earnshaw et al.56 | United States | Clients living with HIV at a community clinic who reported use of illicit substances, misuse of prescription drugs, or use of alcohol in the past 3 months | 85 | Cross sectional | Depressive symptoms |
| Earnshaw et al.57 | United States | Black gay and bisexual men who were newly diagnosed with HIV, gonorrhea, chlamydia, or syphilis; 31.8% of participants were diagnosed with HIV | 151 | Prospective cohort | HIV/STI internalized stigma |
| English et al.58 | United States | Sexual minority men (biologically and self-identified as male and as gay, bisexual, or another nonheterosexual identity); the sample was composed of Black (42.7%), Latino (30.0%), and multiracial (25.3%) participants, 57.1% of whom were living with HIV | 170 | Prospective cohort | Substance use (drug use and heavy drinking), emotion regulation difficulties |
| Logie et al.59 | Canada | Women living with HIV who were members of marginalized communities (including indigenous, Black, and transgender communities) represented in Canada’s HIV epidemic | 1367 | Cross sectional | ART adherence, CD4 count, viral load |
| Reisen et al.60 | United States | Latino gay men living with HIV | 301 | Cross sectional | Depression, gay collective identity |
| Vetrova et al.61 | Russia | People living with HIV who injected drugs and had a documented ART naive status (i.e., they had never started treatment) | 188 | Observational prospective cohort | Access to health care, use of health care |
| Yang et al.62 | China | MSM living with HIV | 193 | Cross sectional (baseline survey as part of prospective study) | Depression, anxiety, psychological resilience, quality of life |
| Yang et al.50 | Botswana | Clients living with HIV from a dedicated infectious disease center and members of the general community without a reported HIV status | 38 focus groups, 46 in-depth Interviews | Mixed methods | Scale development: construct validity examined with validated HIV stigma scale, depressive symptoms, self-esteem, and social support |
Note. ART = antiretroviral therapy; MSM = men who have sex with men; PTSD = posttraumatic stress disorder; STI = sexually transmitted infection. A total of 16 studies were included in the review.
All of the included studies involved people living with HIV, with most exploring outcomes among male-identifying members of sexual minority groups51–53,57,58,60,62 and cisgender women.48–50,59 Three studies explored individuals who injected drugs54,61 or who reported use of illicit drugs, misuse of prescription drugs, or use of alcohol.56 One study explored cisgender female sex workers,55 and another explored transgender women.47 The majority of studies employed a cross-sectional design (n = 11). Among the investigated outcomes, most related to mental health and well-being48,50,52,56,60,62 or HIV treatment and care.47,49,51,53,54,59
Intersectionality and Forms and Levels of Stigma
Among the included studies, 7 explicitly referenced intersectionality theory or frameworks in their work,54,56–61 reflecting on the interdependence of socially marginalized identities, conditions, or statuses in influencing health outcomes (Table 2). Although the remainder of the studies did not explicitly reference intersectionality theory or frameworks, they indicated the “intersectional,”48,49 “overlapping,”47 “layered,”55 “synergistic,”62 “simultaneous,”51 “concurrent,”53 or “combined”52 effects of multiple identities, conditions, or statuses on the health of socially marginalized groups. Among the 16 included studies, 4 explored intersectional stigma through a single measure,47–50 whereas 12 employed analytic approaches to bring together multiple stigma measures.51–62 Most studies explored the intersection of 2 types of stigma (n = 11), with the remaining studies exploring the intersection of 3 types (n = 5). Studies explored different forms of stigma, including enacted (n = 11), internalized (n = 8), perceived (n = 3), and anticipated (n = 2) stigma. In addition, studies examined intersectional stigma at the individual (n = 8), interpersonal (n = 10), structural (n = 6), and societal (n = 1) levels.
TABLE 2—
Use of Intersectionality Theory or Frameworks and Characterization of Forms and Levels of Stigma, by Study: HIV-Related Intersectional Stigma and Discrimination Measurement, January 1, 2010– May 12, 2021
| Authors | Explicit Reference to Intersectionality Theory or Framework | Intersectional Stigma Explored Through a Single Measure | Type of Stigma | Form of Stigma | Level of Stigma |
| Baguso et al.47 | X | Gender identity or presentation, race | Enacted | Structural | |
| Bogart et al.51 | Race, HIV, sexual orientation | Enacted | Interpersonal, structural | ||
| Bogart et al.52 | Race, HIV, sexual orientation | Enacted | Interpersonal, structural | ||
| Bogart et al.53 | Race/ethnicity, HIV, sexual orientation | Enacted | Interpersonal, structural | ||
| Calabrese et al.54 | X | HIV status, drug use | Internalized | Individual | |
| Carrasco et al.55 | HIV, sex work | Internalized | Individual | ||
| Dale and Safren48 | X | Gender, race | Enacted | Interpersonal | |
| Dale et al.49 | X | Gender, race | Enacted | Interpersonal | |
| Earnshaw et al.56 | X | Substance use, HIV | Internalized | Individual | |
| Earnshaw et al.57 | X | Race, sexual orientation, HIV/STI | Internalized | Individual | |
| English et al.58 | X | Race, sexual orientation | Internalized, enacted | Individual, interpersonal | |
| Logie et al.59 | X | HIV, race, gender | Internalized, perceived, anticipated, enacted | Individual, interpersonal | |
| Reisen et al.60 | X | Sexual orientation, ethnicity | Enacted | Interpersonal, structural | |
| Vetrova et al.61 | X | Substance use, HIV | Internalized, perceived, anticipated, enacted | Individual, interpersonal | |
| Yang et al.62 | HIV, sexual orientation | Internalized, enacted | Individual, interpersonal, structural | ||
| Yang et al.50 | X | Gender, HIV | Perceived | Societal |
Note. STI = sexually transmitted infection. A total of 16 studies were included in the review.
Intersectional Stigma Via Single Measures
Appendix A (available as a supplement to the online version of this article at http://www.ajph.org) presents the measurement descriptions of studies exploring intersectional stigma through a single measure.47–50 In all 4 studies, a single scale was used to measure intersectional stigma.
Two of the 4 included studies, both conducted by Dale et al.,48,49 were based on the same sample and employed the same intersectional stigma measure to estimate the effects of gendered racial microaggressions among Black women living with HIV in a large urban city in the southeastern United States. These studies, although involving the same measure, analyzed the measure differently by using sum48 or average49 scores from a validated scale63 to explore the frequency and appraisal of gendered racial microaggressions. Both studies, which employed regression models to explore the effects of intersectional gender and race stigma on posttraumatic stress disorder symptoms or conditions48 and barriers to HIV-related care,49 reported good internal consistency (Cronbach α > 0.90 for each subscale).
In a separate study, Baguso et al.47 adapted an existing scale64 to explore enacted stigma due to gender identity or presentation and race among transgender women living with HIV in San Francisco, California. In this study, the authors measured intersectional stigma by asking respondents about experiences of discrimination, followed by a question attributing such experiences to their race, gender identity or presentation, or both.47 The authors reported an internal consistency (Cronbach α) of 0.76 for their measure. The measure was dichotomized, and respondents who attributed experiences of discrimination to both gender identity or presentation and race were classified as experiencing intersectional gender and race stigma. The authors used logistic regression to explore the relationship between intersectional gender and race stigma and HIV treatment and care outcomes.47
Finally, only 1 measure was developed to focus on the intersectional stigma experiences of people living with HIV. In their study, Yang et al.50 examined intersectional (HIV and gender) stigma experiences among women living with HIV in Botswana. The authors developed the Cultural Factors Shape Stigma subscale, which the authors determined to have strong content validity, good internal consistency (Cronbach α = 0.90), and high test–retest reliability (P = .92).50 Construct validity assessments revealed a positive, marginally significant correlation with the validated Berger HIV Internalized Stigma Scale26 (ρ = 0.24; P = .095) and a strong correlation with the validated Center for Epidemiologic Studies Depression Scale65 (ρ = 0.39; P = .005).50
Intersectional Stigma Via Multiple Measures
Appendix A also presents the analytic approaches of 12 studies assessing intersectional stigma through multiple stigma measures.51–62 In most studies, authors generated a sum or average score for each stigma measure and subsequently explored 2- or 3-way interactions via multivariable logistic or linear regression models.51–54,56,57,60–62
In addition to exploring interactive effects through regression analyses, 2 studies (Vetrova and colleagues’ exploration of substance use and HIV stigma61 and Yang and colleagues’ examination of HIV and sexual orientation stigma62) developed 4-level group categorizations of intersectional stigma. These stigma groups (classified as “high–high,” “high–low,” “low–high,” and “low–low”) were used in comparisons of the outcomes of interest.61,62
Three studies employed structural equation modeling to explore the effects of intersectional stigma through multiple stigma measures.55,58,59 The first study explored the influences of latent sex work and HIV internalized stigma constructs on social cohesion and consistent condom use among cisgender female sex workers living with HIV in the Dominican Republic.55 In this study, Carrasco et al.55 assessed 4 mediation models, including a model testing the interactive effects of latent constructs of HIV and sex work internalized stigmas.55
In a second study, English et al.58 examined the interactive effects of the latent constructs of racial discrimination and internalized sexual orientation stigma among sexual minority men living in New York City. In this study, the authors used longitudinal structural equation modeling to explore the interactive effects of baseline stigma related to race (enacted) and sexual orientation (internalized) on substance use at a 12-month follow-up, mediated by emotional regulation at baseline and internalizing symptoms at a 6-month follow-up.58
The third study, conducted by Logie et al.,59 was based on a sample of women living with HIV from marginalized communities in Ontario, Quebec, and British Columbia, Canada. In this study, the authors used structural equation modeling to examine the impact of a latent intersectional stigma construct (indicated by latent constructs of internalized HIV stigma, racial discrimination, and gender discrimination) on HIV outcomes (antiretroviral therapy adherence, CD4 count, viral load) via social support, depression, resilience, and drug use.59
DISCUSSION
We identified 16 studies from 6 countries assessing the effects of intersectional stigma on health-related outcomes, including HIV-related, mental health, and substance use outcomes. Of these 16 studies, only 4 employed a single intersectional stigma scale; the remaining 12 used multiple stigma scales or indices, which were then combined analytically. All 16 studies were conducted among people living with HIV, with several (n = 7) conducted among male-identifying members of sexual minority groups.
Just under half of the included studies (n = 7) made explicit reference to intersectionality as a motivating theory, framework, or perspective. Most of the remaining studies either did not acknowledge intersectionality or referred briefly to “intersectional stigma” but did not situate their work within the intersectionality literature or define intersectionality. Furthermore, several of the included studies applied intersectionality during post hoc analyses but did not consider intersectionality during study design or implementation. A recent review by Bauer et al.66 revealed a parallel trend in the broader literature.
As such, given the recent proliferation of quantitative intersectional HIV research, we encourage scholars to think critically about their conceptualization of intersectionality from the outset. This will help shape how intersectional stigma is measured and whether the selected measurement approach aligns with conceptual underpinnings. Logie et al. exemplified this notion by using intersectionality theory to guide their analytic approach when assessing intersectional HIV, race, and gender stigma.59
Others have pointed out the importance of studying intersectional stigma from a multilevel perspective.23 The studies included in our review were most likely to measure intersectional stigma at the individual and interpersonal levels. We did not identify any studies of community or organizational intersectional stigma, suggesting a need for additional research in these areas. However, the fact that 6 studies measured structural stigma is promising, given the structural nature and embeddedness of intersectional stigma, discrimination, and oppression.
Most studies included in our review did not measure intersectional stigma through a single scale or index but, instead, combined new and existing measures of stigma to quantitatively estimate the effects of intersectional stigma. This is consistent with Mena and colleagues’ finding that most intersectionality-based analyses in other health fields rely on combining multiple stigma scales analytically.67 We caution researchers using these approaches to carefully consider their assumptions and motivations, particularly when applying measures not intended to be used intersectionally.66
We did not include in our review studies measuring intersectional stigma by combining multiple stigma scales through additive approaches (e.g., by yielding a sum score) because they did not align with our conceptualization of intersectionality20,25 and how the interdependence of multiple identities, social conditions, or statuses affects health outcomes. Rather, represented in this review were analyses that examined intersectionality beyond these additive approaches. This aligns with recent calls to employ moderation approaches, multilevel modeling, and latent variable models to model intersectional experiences when using multiple existing scales.18
Among those studies that incorporated dedicated intersectional stigma measures (n = 4), only 1 was specifically developed for the study population of interest (Batswana women living with HIV).50 Others were adaptations or reapplications of existing scales, none of which reported substantial community involvement. Our findings suggest that it is feasible to adapt or tailor existing measures for intersectional HIV-related research. Given the time and resources required to develop scales tailored toward unique intersectional experiences among marginalized communities, scholars should consider using context-, identity-, or condition-adaptable measures when possible. When adapting measures for intersectional HIV research, scholars should carefully consider how to meaningfully engage communities and honor the principles of intersectionality throughout their approach.
Although not an intersectional stigma measure, Kerrigan et al.68 provided an example of how to develop a scale in conjunction with the community for whom the scale is intended. In their work, the authors used in-depth and cognitive interviews to define measure domains and items and then assessed the content validity of a sex work stigma scale among cisgender female sex workers living in the Dominican Republic and Tanzania while also assessing the construct validity of the scale against other existing measures. Similar methods could be employed when approaching the development of intersectional stigma measures.
Furthermore, although our inclusion criteria covered studies that examined HIV stigma or other HIV-related outcomes among both people living with HIV and other populations, we identified studies of intersectional stigma conducted only among people living with HIV. This suggests an opportunity for additional quantitative intersectional stigma research in the field of HIV prevention, which is of particular importance given that the qualitative literature suggests that intersectional stigma and discrimination play an important role in access to and uptake of HIV testing and prevention interventions (e.g., preexposure prophylaxis).69–72 Also, the majority of studies we included considered intersectional stigmas related to HIV and only 1 or 2 additional identities or conditions. Additional efforts are needed to understand the more complex effects of large numbers of intersectional identities.66
Finally, although there is a growing body of qualitative literature around intersectional stigma and HIV in low-income settings,73–75 we found no corresponding quantitative studies. Indeed, most of our studies (n = 11) were conducted in high-income settings; the remainder (n = 5) were conducted in upper-middle-income settings. Given the growing concentration of HIV epidemics among multiply marginalized communities worldwide, additional intersectional stigma research in low-income settings is warranted. Such studies would provide a more nuanced description of how intersecting identities are experienced in more marginalized communities, allowing for transnational and multilevel analyses to be conducted. Also, as reflected in some of the studies wherein data were collected in multiple languages (n = 5), using culturally and linguistically congruent measures to examine intersectional stigma and discrimination is advantageous because these measures allow for more in-depth exploration of intersecting realities across diverse groups.
Limitations
Our review involved some limitations. For example, we included studies that did not explicitly reference intersectionality as a motivating theory or framework. This may have resulted in the inclusion of studies that did not set out to do intersectional research. We also excluded non-peer-reviewed articles and conference abstracts. This exclusion, although made in an effort to allow for included articles to have undergone more thorough quality checks through the peer-review process and to present more complete information, could have led to disregard of relevant work related to intersectional stigma measurement. Despite these limitations, the results of our review of HIV-related intersectional stigma and discrimination measures and analytic approaches can serve as a key reference for researchers, practitioners, and community members in future research, programmatic, and policy efforts.
Conclusions
There is a growing body of quantitative research examining HIV-related intersectional stigma and discrimination, although current research is concentrated in high-income settings and involves people living with HIV and members of sexual minority groups. In this review, we have identified gaps in the development and adaptation of tailored, multidimensional measures of intersectional stigma and discrimination. Further efforts are required to ensure that intersectionality is appropriately defined and applied in quantitative research from the outset and to explore the potential of more complex analytic and measurement approaches for studying intersectional stigma as it relates to HIV. High-quality, innovative approaches to quantitatively measuring and analyzing HIV-related intersectional stigma have great potential to improve the HIV response and increase equity in HIV testing, treatment, and prevention outcomes by allowing for a more nuanced understanding of the effects of individuals’ intersecting realities on their health trajectories.
ACKNOWLEDGMENTS
Funding for this review includes support from the National Institute of Mental Health through grants R01 MH110158 (principal investigator: Deanna Kerrigan), R01 MH125798 (principal investigator: Michael D. Sweat), and F31 MH124583 (Kaitlyn Atkins) and from the DC Center for AIDS Research through grant P30 AI117970.
We acknowledge Gregory Greenwood and the other organizers of the National Institute of Mental Health HIV-Related Intersectional Stigma Research Advances and Opportunities Workshop, which inspired this review. We also thank the authors of and participants in all of the works included in the review, as well as the 2 key experts from the field of intersectional stigma who provided additional input on relevant research. Finally, we thank Kevin O’Reilly for his input on and review of the article.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
HUMAN PARTICIPANT PROTECTION
No protocol approval was needed for this research because secondary data were used.
REFERENCES
- 1.Crenshaw K. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford Law Rev. 1991;43(6):1241–1299. doi: 10.2307/1229039. [DOI] [Google Scholar]
- 2.Carbado DW, Crenshaw KW, Mays VM, Tomlinson B. Intersectionality: mapping the movements of a theory. Du Bois Rev. 2013;10(2):303–312. doi: 10.1017/S1742058X13000349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Combahee River Collective. 2022. https://www.blackpast.org/african-american-history/combahee-river-collective-statement-1977
- 4.Truth S.2022. https://www.nps.gov/articles/sojourner-truth.htm
- 5.Bowleg L. The problem with the phrase women and minorities: intersectionality—an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–1273. doi: 10.2105/AJPH.2012.300750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muessig KE, Golinkoff JM, Hightow-Weidman LB, et al. Increasing HIV testing and viral suppression via stigma reduction in a social networking mobile health intervention among Black and Latinx young men and transgender women who have sex with men (HealthMpowerment): protocol for a randomized controlled trial. JMIR Res Protoc. 2020;9(12):e24043. doi: 10.2196/24043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arrington-Sanders R, Hailey-Fair K, Wirtz AL, et al. Role of structural marginalization, HIV stigma, and mistrust on HIV prevention and treatment among young Black Latinx men who have sex with men and transgender women: perspectives from youth service providers. AIDS Patient Care STDS. 2020;34(1):7–15. doi: 10.1089/apc.2019.0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Becasen JS, Denard CL, Mullins MM, Higa DH, Sipe TA. Estimating the prevalence of HIV and sexual behaviors among the US transgender population: a systematic review and meta-analysis, 2006–2017. Am J Public Health. 2019;109(1):e1–e8. doi: 10.2105/AJPH.2018.304727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muula AS. HIV infection and AIDS among young women in South Africa. Croat Med J. 2008;49(3):423–435. doi: 10.3325/cmj.2008.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hargreaves JR, Busza J, Mushati P, Fearon E, Cowan FM. Overlapping HIV and sex-work stigma among female sex workers recruited to 14 respondent-driven sampling surveys across Zimbabwe, 2013. AIDS Care. 2017;29(6):675–685. doi: 10.1080/09540121.2016.1268673. [DOI] [PubMed] [Google Scholar]
- 11.Kennedy CE, Baral SD, Fielding-Miller R, et al. “They are human beings, they are Swazi”: intersecting stigmas and the positive health, dignity and prevention needs of HIV-positive men who have sex with men in Swaziland. J Int AIDS Soc. 2013;16(suppl 3):18749. doi: 10.7448/IAS.16.4.18749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Diabaté S, Zannou DM, Geraldo N, et al. Antiretroviral therapy among HIV-1 infected female sex workers in Benin: a comparative study with patients from the general population. World J AIDS. 2011;1(3):94–99. doi: 10.4236/wja.2011.13014. [DOI] [Google Scholar]
- 13.Lyons CE, Olawore O, Turpin G, et al. Intersectional stigmas and HIV-related outcomes among a cohort of key populations enrolled in stigma mitigation interventions in Senegal. AIDS. 2020;34(suppl 1):S63–S71. doi: 10.1097/QAD.0000000000002641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baral SD, Friedman MR, Geibel S, et al. Male sex workers: practices, contexts, and vulnerabilities for HIV acquisition and transmission. Lancet. 2015;385(9964):260–273. doi: 10.1016/S0140-6736(14)60801-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nixon S, Cameron C, Cameron D, et al. The intersectionality of HIV and disability in Zambia: results from the Sepo Study. Can J Infect Dis Med Microbiol. 2011;22 [Google Scholar]
- 16.Kerrigan D, Vazzano A, Bertoni N, Malta M, Bastos FI. Stigma, discrimination and HIV outcomes among people living with HIV in Rio de Janeiro, Brazil: the intersection of multiple social inequalities. Glob Public Health. 2017;12(2):185–199. doi: 10.1080/17441692.2015.1064459. [DOI] [PubMed] [Google Scholar]
- 17.Baral S, Beyrer C, Muessig K, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(7):538–549. doi: 10.1016/S1473-3099(12)70066-X. [DOI] [PubMed] [Google Scholar]
- 18.Turan JM, Elafros MA, Logie CH, et al. Challenges and opportunities in examining and addressing intersectional stigma and health. BMC Med. 2019;17(1):7. doi: 10.1186/s12916-018-1246-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med. 2014;110:10–17. doi: 10.1016/j.socscimed.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 20.Bowleg L. When Black + lesbian + woman ≠ Black lesbian woman: the methodological challenges of qualitative and quantitative intersectionality research. Sex Roles. 2008;59(5):312–325. doi: 10.1007/s11199-008-9400-z. [DOI] [Google Scholar]
- 21.Algarin AB, Zhou Z, Cook CL, Cook RL, Ibañez GE. Age, sex, race, ethnicity, sexual orientation: intersectionality of marginalized-group identities and enacted HIV-related stigma among people living with HIV in Florida. AIDS Behav. 2019;23(11):2992–3001. doi: 10.1007/s10461-019-02629-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, Turan JM. Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. Am J Public Health. 2017;107(6):863–869. doi: 10.2105/AJPH.2017.303744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stangl AL, Earnshaw VA,, Logie CH, et al. The Health Stigma and Discrimination Framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019;17(1):31. doi: 10.1186/s12916-019-1271-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc. 2013;16(suppl 2):18734. doi: 10.7448/IAS.16.3.18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dubrow J.2022. https://kb.osu.edu/bitstream/handle/1811/69557/ASK_2008_85_100.pdf?sequence=1&isAllowed=y
- 26.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV Stigma Scale. Res Nurs Health. 2001;24(6):518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 27.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17(5):1785–1795. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.English D, Carter JA, Bowleg L, Malebranche DJ, Talan AJ, Rendina HJ. Intersectional social control: the roles of incarceration and police discrimination in psychological and HIV-related outcomes for Black sexual minority men. Soc Sci Med. 2020;258:113121. doi: 10.1016/j.socscimed.2020.113121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Konkor I, Lawson ES, Antabe R, et al. An intersectional approach to HIV vulnerabilities and testing among heterosexual African Caribbean and Black men in London, Ontario: results from the weSpeak Study. J Racial Ethn Health Disparities. 2020;7(6):1140–1149. doi: 10.1007/s40615-020-00737-3. [DOI] [PubMed] [Google Scholar]
- 30.Orza L, Bewley S, Logie CH, et al. How does living with HIV impact on women’s mental health? Voices from a global survey. J Int AIDS Soc. 2015;18(suppl 5):20289. doi: 10.7448/IAS.18.6.20289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sileo KM, Wanyenze RK,, Mukasa B, Musoke W, Kiene SM. The intersection of inequitable gender norm endorsement and HIV stigma: implications for HIV care engagement for men in Ugandan fishing communities. AIDS Behav. 2021;25(9):2863–2874. doi: 10.1007/s10461-021-03176-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wesson P, Vittinghoff E, Turner C, Arayasirikul S, McFarland W, Wilson E. Intercategorical and intracategorical experiences of discrimination and HIV prevalence among transgender women in San Francisco, CA: a quantitative intersectionality analysis. Am J Public Health. 2021;111(3):446–456. doi: 10.2105/AJPH.2020.306055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Williamson TJ, Mahmood Z, Kuhn TP, Thames AD. Differential relationships between social adversity and depressive symptoms by HIV status and racial/ethnic identity. Health Psychol. 2017;36(2):133–142. doi: 10.1037/hea0000458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elafros MA, Gardiner JC, Sikazwe I, et al. Evaluating layered stigma from comorbid HIV and epilepsy among Zambian adults. eNeurologicalSci. 2018;13:56–62. doi: 10.1016/j.ensci.2017.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goodin BR, Owens MA, White DM, et al. Intersectional health-related stigma in persons living with HIV and chronic pain: implications for depressive symptoms. AIDS Care. 2018;30(suppl 2):66–73. doi: 10.1080/09540121.2018.1468012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Meanley SP, Plankey MW, Matthews DD, et al. Lifetime prevalence and sociodemographic correlates of multifactorial discrimination among middle-aged and older adult men who have sex with men. J Homosex. 2021;68(10):1591–1608. doi: 10.1080/00918369.2019.1702353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meanley SP, Stall RD, Hawk ME, et al. Multifactorial discrimination, discrimination salience, and prevalent experiences of internalized homophobia in middle-aged and older MSM. Aging Ment Health. 2020;24(7):1167–1174. doi: 10.1080/13607863.2019.1594161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Muñoz-Laboy M, Guidry JA, Kreisberg A. Internalised stigma as durable social determinant of HIV care for transnational patients of Puerto Rican ancestry. Glob Public Health. 2021;4:1–20. doi: 10.1080/17441692.2021.1919173. [DOI] [PubMed] [Google Scholar]
- 39.Sereda Y, Kiriazova T, Makarenko O, et al. Stigma and quality of co-located care for HIV-positive people in addiction treatment in Ukraine: a cross-sectional study. J Int AIDS Soc. 2020;23(5):e25492. doi: 10.1002/jia2.25492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.English D, Carter JA, Forbes N, et al. Intersectional discrimination, positive feelings, and health indicators among Black sexual minority men. Health Psychol. 2020;39(3):220–229. doi: 10.1037/hea0000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Haile R, Rowell, Cunsolo TL, Parker EA, Padilla MB, Hansen NB. An empirical test of racial/ethnic differences in perceived racism and affiliation with the gay community: implications for HIV risk. J Soc Issues. 2014;70(2):342–359. doi: 10.1111/josi.12063. [DOI] [Google Scholar]
- 42.Jefferson K, Neilands TB, Sevelius J. Transgender women of color: discrimination and depression symptoms. Ethn Inequal Health Soc Care. 2013;6(4):121–136. doi: 10.1108/EIHSC-08-2013-0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wilson EC, Chen Y-H, Arayasirikul S, Raymond HF, McFarland W. The impact of discrimination on the mental health of transfemale youth and the protective effect of parental support. AIDS Behav. 2016;20(10):2203–2211. doi: 10.1007/s10461-016-1409-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Varas-Díaz N, Rivera-Segarra E, Neilands TB, et al. HIV/AIDS and intersectional stigmas: Examining stigma related behaviours among medical students during service delivery. Glob Public Health. 2019;14(11):1598–1611. doi: 10.1080/17441692.2019.1633378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Windsor LC, Benoit E, Ream GL, Forenza B. The Provider Perception Inventory: psychometrics of a scale designed to measure provider stigma about HIV, substance abuse, and MSM behavior. AIDS Care. 2013;25(5):586–591. doi: 10.1080/09540121.2012.726338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kerr J, Northington T, Sockdjou T, Maticka-Tyndale E. Perceived neighborhood quality and HIV-related stigma among African diasporic youth; results from the African, Caribbean, and Black Youth (ACBY) Study. J Health Care Poor Underserved. 2018;29(2):651–663. doi: 10.1353/hpu.2018.0049. [DOI] [PubMed] [Google Scholar]
- 47.Baguso GN, Turner CM, Santos GM, et al. Successes and final challenges along the HIV care continuum with transwomen in San Francisco. J Int AIDS Soc. 2019;22(4):e25270. doi: 10.1002/jia2.25270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dale SK, Safren SA. Gendered racial microaggressions predict posttraumatic stress disorder symptoms and cognitions among Black women living with HIV. Psychol Trauma. 2019;11(7):685–694. doi: 10.1037/tra0000467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dale SK, Dean T, Sharma R, Reid R, Saunders S, Safren SA. Microaggressions and discrimination relate to barriers to care among Black women living with HIV. AIDS Patient Care STDS. 2019;33(4):175–183. doi: 10.1089/apc.2018.0258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yang LH, Ho-Foster AR, Becker TD, et al. Psychometric validation of a scale to assess culturally-salient aspects of HIV stigma among women living with HIV in Botswana: engaging “what matters most” to resist stigma. AIDS Behav. 2021;25(2):459–474. doi: 10.1007/s10461-020-03012-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bogart LM, Wagner GJ, Galvan FH, Klein DJ. Longitudinal relationships between antiretroviral treatment adherence and discrimination due to HIV-serostatus, race, and sexual orientation among African-American men with HIV. Ann Behav Med. 2010;40(2):184–190. doi: 10.1007/s12160-010-9200-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bogart LM, Wagner GJ, Galvan FH, Landrine H, Klein DJ, Sticklor LA. Perceived discrimination and mental health symptoms among Black men with HIV. Cultur Divers Ethnic Minor Psychol. 2011;17(3):295–302. doi: 10.1037/a0024056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bogart LM, Landrine H, Galvan FH, Wagner GJ, Klein DJ. Perceived discrimination and physical health among HIV-positive Black and Latino men who have sex with men. AIDS Behav. 2013;17(4):1431–1441. doi: 10.1007/s10461-012-0397-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Calabrese SK, Burke SE, Dovidio JF, et al. Internalized HIV and drug stigmas: interacting forces threatening health status and health service utilization among people with HIV who inject drugs in St. Petersburg, Russia. AIDS Behav. 2016;20(1):85–97. doi: 10.1007/s10461-015-1100-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Carrasco MA, Nguyen TQ, Barrington C, Perez M, Donastorg Y, Kerrigan D. HIV stigma mediates the association between social cohesion and consistent condom use among female sex workers living with HIV in the Dominican Republic. Arch Sex Behav. 2018;47(5):1529–1539. doi: 10.1007/s10508-018-1186-7. [DOI] [PubMed] [Google Scholar]
- 56.Earnshaw VA, Smith LR, Cunningham CO, Copenhaver MM. Intersectionality of internalized HIV stigma and internalized substance use stigma: implications for depressive symptoms. J Health Psychol. 2015;20(8):1083–1089. doi: 10.1177/1359105313507964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Earnshaw VA, Reed NM, Watson RJ, Maksut JL,, Allen AM, Eaton LA. Intersectional internalized stigma among Black gay and bisexual men: a longitudinal analysis spanning HIV/sexually transmitted infection diagnosis. J Health Psychol. 2021;26(3):465–476. doi: 10.1177/1359105318820101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.English D, Rendina HJ, Parsons JT. The effects of intersecting stigma: a longitudinal examination of minority stress, mental health, and substance use among Black, Latino, and multiracial gay and bisexual men. Psychol Violence. 2018;8(6):669–679. doi: 10.1037/vio0000218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Logie CH, Williams CC, Wang Y, et al. Adapting stigma mechanism frameworks to explore complex pathways between intersectional stigma and HIV-related health outcomes among women living with HIV in Canada. Soc Sci Med. 2019;232:129–138. doi: 10.1016/j.socscimed.2019.04.044. [DOI] [PubMed] [Google Scholar]
- 60.Reisen CA, Brooks KD, Zea MC, Poppen PJ, Bianchi FT. Can additive measures add to an intersectional understanding? Experiences of gay and ethnic discrimination among HIV-positive Latino gay men. Cultur Divers Ethnic Minor Psychol. 2013;19(2):208–217. doi: 10.1037/a0031906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vetrova MV, Cheng DM, Bendiks S, et al. HIV and substance use stigma, intersectional stigma and healthcare among HIV-positive PWID in Russia. AIDS Behav. 2021;25(9):2815–2826. doi: 10.1007/s10461-021-03172-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yang X, Li X, Qiao S, et al. Intersectional stigma and psychosocial well-being among MSM living with HIV in Guangxi, China. AIDS Care. 2020;32(suppl 2):5–13. doi: 10.1080/09540121.2020.1739205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lewis JA, Neville HA. Construction and initial validation of the Gendered Racial Microaggressions Scale for Black women. J Couns Psychol. 2015;62(2):289–302. doi: 10.1037/cou0000062. [DOI] [PubMed] [Google Scholar]
- 64.Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61(7):1576–1596. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 65.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 66.Bauer GR, Churchill SM, Mahendran M, Walwyn C, Lizotte D, Villa-Rueda AA. Intersectionality in quantitative research: a systematic review of its emergence and applications of theory and methods. SSM Popul Health. 2021;14:100798. doi: 10.1016/j.ssmph.2021.100798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mena E, Bolte G. Intersectionality-based quantitative health research and sex/gender sensitivity: a scoping review. Int J Equity Health. 2019;18(1):199. doi: 10.1186/s12939-019-1098-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kerrigan D, Karver TS, Barrington C, et al. Development of the Experiences of Sex Work Stigma Scale using item response theory: implications for research on the social determinants of HIV. AIDS Behav. 2021;25(suppl 2):175–188. doi: 10.1007/s10461-021-03211-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tsang EY, Qiao S, Wilkinson JS, Fung AL, Lipeleke F, Li X. Multilayered stigma and vulnerabilities for HIV infection and transmission: a qualitative study on male sex workers in Zimbabwe. Am J Mens Health. 2019;13(1):1557988318823883. doi: 10.1177/1557988318823883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Quinn K, Bowleg L, Dickson-Gomez J. “The fear of being Black plus the fear of being gay”: the effects of intersectional stigma on PrEP use among young Black gay, bisexual, and other men who have sex with men. Soc Sci Med. 2019;232:86–93. doi: 10.1016/j.socscimed.2019.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.LeMasters K, Atkins K, Oloonabadi SA, Munn T, Eng E, Lightfoot AF. How can we PrEP? Exploring Black MSM’s experiences with pre-exposure prophylaxis through Photovoice. AIDS Educ Prev. 2021;33(1):16–32. doi: 10.1521/aeap.2021.33.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Were D, Atkins K, Musau A, Plotkin M, Curran K. Manifestations of stigma in the context of a national oral pre-exposure prophylaxis (PrEP) scale-up program in Kenya. Paper presented at: 10th IAS Conference on HIV Science. Mexico City: Mexico; July 2019. [Google Scholar]
- 73.MacPherson EE, Phiri M, Sadalaki J, et al. Sex, power, marginalisation and HIV amongst young fishermen in Malawi: exploring intersecting inequalities. Soc Sci Med. 2020;266:113429. doi: 10.1016/j.socscimed.2020.113429. [DOI] [PubMed] [Google Scholar]
- 74.Rai SS, Peters RMH, Syurina EV, Irwanto I, Naniche D, Zweekhorst MBM. Intersectionality and health-related stigma: insights from experiences of people living with stigmatized health conditions in Indonesia. Int J Equity Health. 2020;19(1):206. doi: 10.1186/s12939-020-01318-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sekoni AO, Jolly K, Gale NK. Hidden healthcare populations: using intersectionality to theorise the experiences of LGBT+ people in Nigeria, Africa. Glob Public Health. 2022;17(1):134–149. doi: 10.1080/17441692.2020.1849351. [DOI] [PubMed] [Google Scholar]