Abstract
Aims
To explore the management of hypertensive patients by general cardiologists a few months after the European Society of Cardiology (ESC)–European Society of Hypertension (ESH) Guidelines publication.
Methods and results
A survey based on a 26-point questionnaire was sent to ∼69 000 worldwide ESC members, a few months after the ESC–ESH Guidelines publication. A total of 1458 responses were collected via a web-based form. Among them, 68% were men, 48% were below 45 years old, and 60% were from Europe. Current guidelines have been read, at least partially, by 92.8%. Measurement of blood pressure (BP) is mostly done using the auscultatory method (58.8%) while unattended BP is rarely performed. Different bladder cuffs are not available for different arm circumferences for 27% of responders. Routine workup in hypertensive patients includes more often 12 leads ECG (97.7%) and echocardiography (79.6%). Only 30.9% of responders systematically assess the cardiovascular risk by the SCORE system and orthostatic hypotension is systematically researched by only 39.1%. Respondents consider that BP target of 140/90 mmHg is achievable in 60–80% of patients and 130/80 mmHg in 40–60%. Guidelines are considered too tight to be achievable by 15.6%, while 77.4% consider they are exactly right. Low patient’s compliance, awareness of hypertension (HT) risk, and, at a lower degree, physician inertia, represent the main treatment challenges in reaching BP goals to most respondents, while treatment effectiveness is not in question. The present survey demonstrates specific gaps in HT management that need attention in clinical practice.
Keywords: Cardiovascular prevention, Target organ damage, Blood pressure measurement, Blood pressure targets, Gaps in hypertension
Graphical Abstract
Graphical Abstract.
Introduction
Hypertension (HT) is a major public health problem affecting more than 150 million of individuals in Central and Eastern Europe and 1.13 billion all over the word.1 High blood pressure (BP) accounts for almost 10 million of deaths and over 200 million of disability-adjusted life years during 1990–2015. Its management should be a crucial issue for physicians.2
The 2018 was a very rich year concerning HT, with the publication of the new European Society of Cardiology (ESC)–European Society of Hypertension (ESH) guidelines,3 jointly developed by the ESC and the ESH providing recommendations for doctors across Europe and beyond, on key topics, such as how to diagnose HT, how to evaluate and reduce HT-associated risk, how to decide when and how to treat HT by lifestyle advice, and when to add medications. Many aspects of the guidelines were novel with regards to drug treatment, frail and old patients, and BP targets.4 However, there is often a gap between the creation of guidelines and their implementation. The present survey aims to explore the management of hypertensive patients by general cardiologists, a few months after the ESC–ESH Guidelines publication and to identify the major potential gaps to be considered and adjusted.
Methods
This cross-sectional anonymized, worldwide survey conducted on behalf of the Council of Cardiology Practice in association with the Council on Hypertension, was based on a web questionnaire composed of two sessions. A scientific session, where respondents were asked to rate their knowledge and skills in managing patients with arterial HT and their knowledge of 2018 ESC/ESH Guidelines on Arterial Hypertension. The second session analysed the demographic characteristics of the sample. All questions are shown in Supplementary material online, Addendum table. The questionnaire was distributed electronically by the ESC to ∼69 000 cardiologists with an advert in the e-journal of Cardiology Practice and via the Newsletters of the ESC Councils of Cardiology Practice and Hypertension. The email was opened by 32% of the sample and 1458 (2.11%) agreed to answer the questionnaire. Data were collected between 15 January 2019 and 13 March 2019.
Data analysis
Descriptive analysis was undertaken with results represented as numbers and percentages.
Additional sub-analysis was carried out by gender and age (below and over 45 years, ‘younger’ and ‘older’ responders, respectively) and all pair-wise comparisons between the groups were performed using a χ2 test. Data were collected anonymously within the EU General Data Protection Regulation policy and treated by an independent committee (SOLADIS group, Lyon, France).
Results
Only 1427 of responders answered the demographic questions: 68% are men, 52% are over 45 years old, and 60% are from a European country. All of them are cardiologists, and 72.5% define themselves as ‘clinical cardiologists’. They mostly work in hospitals or clinics (65.5%).
Tables 1–3 resume the main results, based on the analysis of the 1458 global responders: 88% of them self-report a good level of HT knowledge. Based on their professional experience, they estimate that HT patient is mainly managed by clinical cardiologists (87.6% of the answers), followed by internal medicine specialists (62.6%) and nephrologists (34.4%). Analysis by age (not detailed in the tables) shows that younger doctors feel to be less expert in the field of HT compared to older doctors (19.4% vs. 35.4%, P < 0.001), with a higher prevalence of non-readers of currents guidelines (8.6% vs. 5.6%, P < 0.05) among them, while more often older doctors have read guidelines in details (25.4% vs. 16.2%, P < 0.001). Unattended BP is performed more frequently by older doctors (9.4% vs. 5.5%, P < 0.006) as well as the use of different bladder cuffs (83.2% vs. 62.2%), routine assessment of orthostatic hypotension (OH) (25.4% vs. 15.8%), the performance of home blood pressure measurement (88.9% vs. 81.6%) and ambulatory blood pressure measurement (84.5% vs. 77.1%) (all P < 0.001).
Table 1.
Population data
| What is your knowledge about hypertension? | |||
| Good, or expert | Poor, or fair enough for simple situations | ||
| 1289 (88.4%) | 169 (11.6%) | ||
| Have you read the latest ESC–ESH Guidelines? | |||
| Yes | No | ||
| 1353 (92.8%) | 105 (7.2%) | ||
| Rate your interest in ESC–ESH Guidelines | |||
| Guidelines important for routine clinical practice | Did not read or considered as an ‘information in case of’ | ||
| 1112 (76.3%) | 346 (23.7%) | ||
| Who is taking care of hypertensive patient in your professional experience?a | |||
| Clinical cardiologist | Internal medicine | Nephrologist | |
| 1277 (87.6%) | 912 (62.6%) | 501 (34.4%) | |
ESC, European Society of Cardiology; ESH, European Society of Hypertension.
Multiple answers allowed.
Table 2.
Blood pressure measurements and risk stratification
| How do you measure BP? | |||||
| Auscultatory | Automatic sphygmomanometer near to the patient | Unattended automatic sphygmomanometer | |||
| 857 (58.8%) | 492 (33.7%) | 109 (7.5%) | |||
| Have you several cuffs adapted to arm circumferences? | |||||
| Yes | No | ||||
| 1065 (73%) | 393 (27%) | ||||
| Do you look for orthostatic hypotension? | |||||
| Always in older or diabetics | Systematically, at least at first visit | Never | |||
| 645 (44.2%) | 569 (39.1%) | 244 (16.7%) | |||
| Do you perform HBPM? | |||||
| Yes | No | ||||
| 1247 (85.5%) | 211 (14.5%) | ||||
| Do you perform ABPM? | |||||
| Yes | No | ||||
| 1179 (80.9%) | 279 (19.1%) | ||||
| In which case do you perform out of office measurements?a | |||||
| To eliminate white coat or masked hypertension | To define resistant hypertension | Always to confirm hypertension | |||
| 1172 (80.4%) | 741 (50.8%) | 693 (47.5%) | |||
| Do you assess the cardiovascular risk by the SCORE system? | |||||
| In some cases | Always | Never | |||
| 772 (52.9%) | 450 (30.9%) | 236 (16.2%) | |||
| Which routine workup in hypertensive patients?a | |||||
| 12 leads ECG | Echocardiography | Carotid U Sound | Ankle Brachial Index | ||
| 1424 (97.7%) | 1160 (79.6%) | 426 (29.2%) | 307 (21.1%) | ||
ABPM, ambulatory blood pressure measurement; BP, blood pressure; HBPM, home blood pressure measurement; ECG, electrocardiogram.
Multiple answers allowed.
Table 3.
Treatment strategies
| In high normal range patients (130–139/85–89 mmHg), do you propose a drug treatment | |||||||||
| Only in some clinical cases | Never | ||||||||
| 1261 (86.5%) | 197 (13.5%) | ||||||||
| At which BP level (mmHg) do you start drug treatment in very old (>80 years) patients?a | |||||||||
| SBP ≥ 180 | SBP ≥ 160 | SBP ≥ 150 | SBP ≥ 140 | Clinical context | |||||
| 109 (7.5%) | 434 (29.8%) | 601 (41.2%) | 398 (27.3%) | 575 (39.4%) | |||||
| In which proportion of patients do you start drug treatment with a dual combination in one pill? | |||||||||
| More than 60% | Less than 60% | ||||||||
| 668 (46%) | 790 (54%) | ||||||||
| In your daily practice, which BP target to reach when you treat HT patient? | |||||||||
| 140/90 mmHg | 130/80 mmHg | 140/90 mmHg or −25% reduction | SBP 120–130 and DBP 70–80 mmHg | ||||||
| 313 (21.5%) | 568 (39%) | 165 (11.2%) | 412 (28.3%) | ||||||
| In your experience, how many treated patients achieve the 140/90 BP target? | |||||||||
| 0–40% | 40–60% | >60% | |||||||
| 170 (11.7%) | 572 (39.2%) | 716 (49.1%) | |||||||
| In your experience, how many treated patients achieve the 130/80 BP target? | |||||||||
| 0–40% | 40–60% | >60% | |||||||
| 701 (48.1%) | 583 (40%) | 174 (11.9%) | |||||||
| The 2018 ESC/ESH Guidelines on Arterial Hypertension are | |||||||||
| Not tight enough | Too tight, not achievable | Just right | |||||||
| 102 (7.0%) | 228 (15.6%) | 1128 (77.4%) | |||||||
BP, blood pressure; DBP, diastolic blood pressure; ESC, European Society of Cardiology; ESH, European Society of Hypertension; HT, hypertension; SBP, systolic blood pressure.
Multiple answers allowed.
Discussion
This survey obtained a low but predictable response rate of 2.11%, according to response rates of similar previous surveys of the Council for Cardiology Practice of the ESC (from 1.3% to 4.7%) and for similar voluntary email-based surveys (from 0.2% to 6.3%).5–7 Even if HT is most managed by primary care, this survey goes from a cardiologist’s point of view. Of course, considering the low response rate, these results cannot account for the representative of the whole cardiology set. Nevertheless, this survey shows some interesting results about the perceptions of a large sample of physicians and highlights some important aspects in the management of HT, with specific regards to BP measurement, cardiovascular (CV) risk assessment, BP thresholds and targets, and drug treatment approaches.
‘Conventional’ measurement of BP using auscultatory or automatic sphygmomanometers is generally performed as recommended by current guidelines; only 7.5% of the cardiologists use unattended measurements, and this reduces the potential discrepancies imputable to this technique.8 Almost 1/3 of responders declare unavailability of different bladder cuffs which might result in a high burden of inaccurate BP measurement.9,10
Systematic assessment of OH, encouraged by the guidelines, seems particularly underused: 16.7% never look for it and only 44.2% research it in older than 65 years or diabetic patients. Yet OH is associated with increased morbidity and mortality particularly in the elderly, treated with multiple drugs, or diabetics.11,12 The recent SPRINT trial did not find a direct correlation with CV events but confirmed the association of OH with serious adverse events leading to hospitalization.13 Blood pressure assessment by ‘out of office techniques’ to detect white coat HT, masked (uncontrolled) HT and nocturnal HT is largely promoted by the Guidelines. Different epidemiological studies have demonstrated their superior prognostic power in hypertensive patients, which further promote their use in daily clinical practice14–16 and, indeed, these techniques are largely used by more than 80% of the responders. Conversely, systematic assessment of CV risk by the SCORE system, strongly suggested by current guidelines3 seems far to be routinely used (30%). This is intriguing, taking into account that responders did read the guidelines planning the risk assessment modalities and that they consider it as a main factor in the treatment strategy (see BP in the high normal range drug therapy). The complexity and/or the time-consuming nature of such an assessment may be an explanation. On the other hand, the detection of markers of organ damage, to better define individual prognosis17 seems well managed: in particular, echocardiography is systematically used by 79.6%, confirming that it has become an easy-to-use tool in the cardiologist’s daily practice. The majority (54%) consider dual combination single pill as initial treatment, and this is a particularly interesting result, as coming only a few months after the Guidelines release.
The relation between physician age and performance remains largely unknown, particularly with respect to patient outcomes. Previous studies have demonstrated a higher mortality rate in patients treated by older physicians mainly related to varying years of experience.18 Our survey instead reports that older than 44 years physicians read more deeply guidelines and more often perform important diagnostic tools in patients with HT.
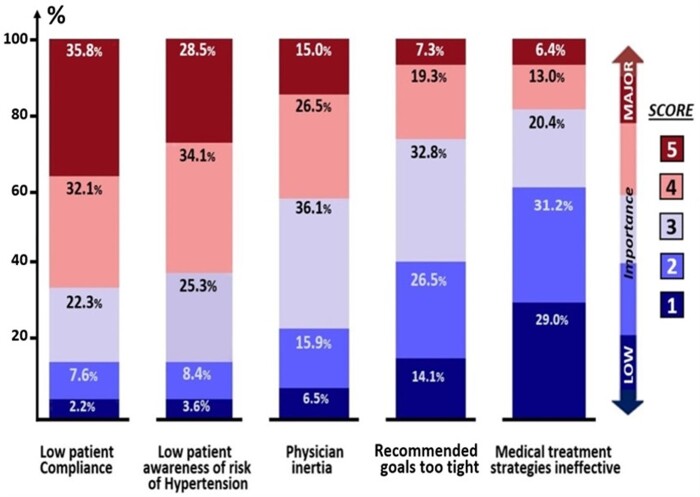
Likewise, considering recent evidence from randomized control trials,3 more tight targets BP have been suggested. Indeed (Table 3), the majority (67%) of respondents declare aiming at a systolic BP (SBP) target <130 mmHg. when treating, which is in line with the recommended goals, although the majority (88%) consider that such a target will be reached in <60%. Less unanimous are the expressed treatment modalities in older patients (>80 years), in terms of the starting SBP level and the targets of the treatment, which may reflect a case-by-case tailored decision. Patients’ compliance and awareness of HT risk are the main fields of improvement underlined by most (68% and 62%) of the responders (Figure 1) On the other hand, and in contrast with the literature data,19 physician inertia is not considered as a major challenge by 68% of respondents. This may only reflect the difficulty of an objective auto-evaluation of each own practice. The whole strongly emphasizes the importance of awareness campaigns on HT intended for patients and physicians. Finally, and encouraging to be noted, the majority does not challenge the recommended goal levels, nor the medical treatment effectiveness (Figure 1), and three over four estimates that the Guidelines on HT are ‘just right’ (Table 3).
Figure 1.
(Question no. 21) Relative importance of different main challenges in reaching European Society of Cardiology–European Society of Hypertension blood pressure goals, scoring from low (1) to major (5) importance.
Limitations
The rate of response to this kind of surveys is generally low, due to problems, such as time constraints and perceiving the participation invite as spam; the present study is no exception. One must be aware that the answers may not fully represent the opinions of the wider physician community from all over the world. Besides, as a phenomenon of an email-based survey, the given responses could reflect the ‘ideal’ practice as viewed by the responders’ knowledge that could not represent the real-life practice. Furthermore, respondents are predominantly male, probably reflecting the distribution of sex among specialties involved in the care of hypertensive patients, an aspect that requires a more in-depth search. An analysis of demographic and geographical data of our survey will be further performed in a specific article. Another limitation is that the study was conducted only a few months after publication of the new ESC–ESH guidance and it is likely that the awareness and uptake of new guidance take longer to permeate into routine practice. Rather than an evaluation of the impact of the new guidelines, the present study must be considered as a valuable dataset from a global community of cardiologists depicting their ‘real-world’ practice at a precise moment.
Conclusion
Our survey, driven only a few months after the ESC–ESH Guidelines publication, enlighten the modalities of hypertensive patient management in a daily cardiology practice. It outlines some inconsistencies, as the management of HT in older patients, the low resort to risk stratification tables, and the search for OH. It focuses on the importance of patient compliance and of his awareness of HT risk. In this way, it opens some key outlooks for future implementation strategies.
Lead author biography

Marc Ferrini, MD, is a former associate head of service at Saint Joseph et Saint Luc Hospital, Lyon, France, and a general cardiologist, with special attention in hypertension, peripheral vascular disease, heart failure, and non-invasive imaging. He is the current chairman of the ESC Council of Cardiology Practice. He contributed to several publications, particularly and most recently on gender-related differences in the management of hypertension (Archives of Cardiovascular Diseases 2012), ambulatory hypertensive patients treated in France (Archives of Cardiovascular Diseases 2013), diabetes and cardiovascular complications (European Journal of Preventive Cardiology 2019), e-Health in general cardiology (European Heart Journal—Digital Health 2021), and late phase of COVID 19 pandemic in general cardiology (Heart Failure 2021). He gave several presentations at the ESC Congresses (2016–2020).
Supplementary material
Supplementary material is available at European Heart Journal Open online.
Conflict of interest: none declared.
Data availability: The data underlying this article are available in the article and in its online supplementary material.
Supplementary Material
Contributor Information
Costantino Mancusi, Hypertension Research Center, Federico II University Hospital, Naples, Italy.
Giovanni de Simone, Hypertension Research Center, Federico II University Hospital, Naples, Italy.
Riccardo Asteggiano, School of Medicine, University of Insubria, ASST-Settelaghi, Varese, Italy; LARC (Laboratorio Analisi e Ricerca Clinica), Turin, Italy.
Dimitri Richter, Euro Clinic Hospital, Athens, Greece.
Bryan Williams, Institute of Cardiovascular Sciences, University College London, London, UK; National Institute for Health Research, University College London Hospitals Biomedical Research Centre, London, UK.
Marc Ferrini, CH Saint Joseph et Saint Luc, 55 rue Vendome, Lyon 69006, France.
References
- 1. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet 2017;389:37–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, Alexander L, Estep K, Hassen Abate K, Akinyemiju TF, Ali R, Alvis-Guzman N, Azzopardi P, Banerjee A, Bärnighausen T, Basu A, Bekele T, Bennett DA, Biadgilign S, Catalá-López F, Feigin VL, Fernandes JC, Fischer F, Gebru AA, Gona P, Gupta R, Hankey GJ, Jonas JB, Judd SE, Khang Y-H, Khosravi A, Kim YJ, Kimokoti RW, Kokubo Y, Kolte D, Lopez A, Lotufo PA, Malekzadeh R, Melaku YA, Mensah GA, Misganaw A, Mokdad AH, Moran AE, Nawaz H, Neal B, Ngalesoni FN, Ohkubo T, Pourmalek F, Rafay A, Rai RK, Rojas-Rueda D, Sampson UK, Santos IS, Sawhney M, Schutte AE, Sepanlou SG, Shifa GT, Shiue I, Tedla BA, Thrift AG, Tonelli M, Truelsen T, Tsilimparis N, Ukwaja KN, Uthman OA, Vasankari T, Venketasubramanian N, Vlassov VV, Vos T, Westerman R, Yan LL, Yano Y, Yonemoto N, Zaki MES, Murray CJL. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. JAMA 2017;317:165–182. [DOI] [PubMed] [Google Scholar]
- 3. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I. 2018 ESC/ESH Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. Eur Heart J 2018;39:3021–3104. [CVOCROSSCVO] [DOI] [PubMed] [Google Scholar]
- 4. Williams B, Mancia G. Ten commandments of the 2018 ESC/ESH HTN guidelines on hypertension in adults. Eur Heart J 2018;39:3007–3008. [DOI] [PubMed] [Google Scholar]
- 5. Murphy CC, Craddock Lee SJ, Geiger AM, Cox JV, Ahn C, Nair R, Gerber DE, Halm EA, McCallister K, Skinner CS. A randomized trial of mail and email recruitment strategies for a physician survey on clinical trial accrual. BMC Med Res Methodol 2020;20:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. So R, Shinohara K, Aoki T, Tsujimoto Y, Suganuma AM, Furukawa TA. Effect of recruitment methods on response rate in a web-based study for primary care physicians: factorial randomized controlled trial. J Med Internet Res 2018;20:e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Koo M, Skinner H. Challenges of internet recruitment: a case study with disappointing results. J Med Internet Res 2005;7:e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Filipovský J, Seidlerová J, Kratochvíl Z, Karnosová P, Hronová M, Mayer O Jr. Automated compared to manual office blood pressure and to home blood pressure in hypertensive patients. Blood Press 2016;25:228–234. [DOI] [PubMed] [Google Scholar]
- 9. Palatini P, Parati G. Blood pressure measurement in very obese patients: a challenging problem. J Hypertens 2011;29:425–429. [DOI] [PubMed] [Google Scholar]
- 10. Palatini P, Asmar R. Cuff challenges in blood pressure measurement. J Clin Hypertens (Greenwich) 2018;20:1100–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fleg JL, Evans GW, Margolis KL, Barzilay J, Basile JN, Bigger JT, Cutler JA, Grimm R, Pedley C, Peterson K, Pop-Busui R, Sperl-Hillen J, Cushman WC. Orthostatic hypotension in the ACCORD (action to control cardiovascular risk in diabetes) blood pressure trial: prevalence, incidence, and prognostic significance. Hypertension 2016;68:888–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Juraschek SP, Daya N, Rawlings AM, Appel LJ, Miller ER III, Windham BG, Griswold ME, Heiss G, Selvin E. Association of history of dizziness and long-term adverse outcomes with early vs later orthostatic hypotension assessment times in middle-aged adults. JAMA Intern Med 2017;177:1316–1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Juraschek SP, Taylor AA, Wright JT Jr, Evans GW, Miller ER III, Plante TB, Cushman WC, Gure TR, Haley WE, Moinuddin I, Nord J, Oparil S, Pedley C, Roumie CL, Whittle J, Wiggers A, Finucane C, Anne Kenny R, Appel LJ, Townsend RR; for the SPRINT Research Group. Orthostatic hypotension, cardiovascular outcomes, and adverse events: results from SPRINT. Hypertension 2020;75:660–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mancia G, Verdecchia P. Clinical value of ambulatory blood pressure: evidence and limits. Circ Res 2015;116:1034–1045. [DOI] [PubMed] [Google Scholar]
- 15. Kario K, Kanegae H, Tomitani N, Okawara Y, Fujiwara T, Yano Y, Hoshide S. Nighttime blood pressure measured by home blood pressure monitoring as an independent predictor of cardiovascular events in general practice. Hypertension 2019;73:1240–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Niiranen TJ, Rissanen H, Johansson JK, Jula AM. Overall cardiovascular prognosis of isolated systolic hypertension, isolated diastolic hypertension and pulse pressure defined with home measurements: the Finn-home study. J Hypertens 2014;32:518–524. [DOI] [PubMed] [Google Scholar]
- 17. Tocci G, Figliuzzi I, Presta V, Attalla El Halabieh N, Citoni B, Coluccia R, Battistoni A, Ferrucci A, Volpe M. Adding markers of organ damage to risk score models improves cardiovascular risk assessment: prospective analysis of a large cohort of adult outpatients. Int J Cardiol 2017;248:342–348. [DOI] [PubMed] [Google Scholar]
- 18. Tsugawa Y, Newhouse JP, Zaslavsky AM, Blumenthal DM, Jha AK. Physician age and outcomes in elderly patients in hospital in the US: observational study. BMJ 2017;357:j1797. [CVOCROSSCVO] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hyman DJ, Pavlik VN, Vallbona C. Physician role in lack of awareness and control of hypertension. J Clin Hypertens 2000;2:324–330. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.