Supplemental Digital Content is Available in the Text.
Abstract
BACKGROUND
Chin augmentation with hyaluronic acid (HA) injections can effectively improve mental appearance.
OBJECTIVE
To introduce a HA injection technique for chin augmentation and evaluate its clinical effects.
METHODS
A total of 326 patients who received HA injection for chin augmentation from January 2018 to May 2021 were retrospectively reviewed. All patients were injected with the technique according to the anatomical morphology of the chin using a needle and cannula. Patient data were collected, the effects were analyzed, and adverse reactions were observed and recorded.
RESULTS
There were 326 patients involved in this study with a mean age of 26.4 years. The median volume of HA injected was 1.85 mL. The shape and contour of the chin was significantly improved in all patients immediately after injection. Most improvements were retained up to 6 months and partial improvements remained visible for 12 months. Swelling and pain occurred in 284 patients (87.1%), local ecchymosis occurred in 31 patients (9.5%), and asymmetry was found in 8 patients (2.5%). There were no other complications such as infection, embolism, necrosis, nodule, or witch's chin. All patients reported satisfaction with results of the HA injections.
CONCLUSION
Injection of HA according to the anatomical morphology of the chin is a safe and effective technique for chin augmentation and results in high patient satisfaction.
The chin is a critical component of the face and plays an important role in the perception of facial aesthetics.1 The structure of the chin includes the skin, muscle, fat, and bone, and mental skeletal configuration is the most important element of the chin shape and contour. Anatomical morphology landmarks pertinent to the mental skeleton include the pogonion, the menton, and the paragonion. The pogonion is the most projecting central portion and determines the anterior projection of the chin. The menton is the inferior most portion and determines the vertical height of the chin. The paragonion is a protruding region lateral to the pogonion on both sides and determines the transverse width of the chin2 (Figure 1).
Figure 1.
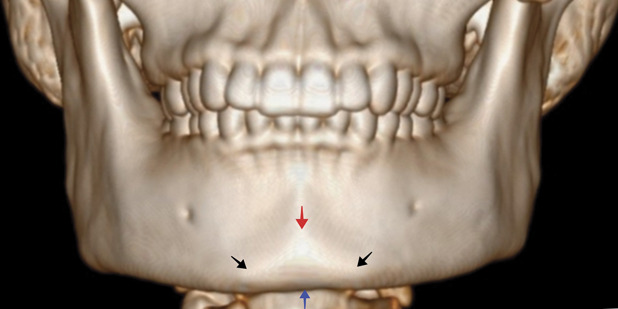
The anatomical morphology landmarks of the mental skeleton: The pogonion (red arrow) determines the anterior projection, the menton (blue arrow) determines the vertical height, and the paragonion (black arrow) determines the transverse width of the chin.
Options for chin augmentation include surgical genioplasty, alloplastic implants, autologous fat transfer, and injection of dermal fillers.2–4 Surgery requires extensive dissection and may cause complications such as rejection reactions, infection, bone absorption, implant movement, and nerve injury. The viability of autologous fat grafting remains unpredictable.
Hyaluronic acid (HA) injection has been a proven treatment for chin augmentation and facial rejuvenation for more than 10 years with an established record of safety and effectiveness. It offers a nonsurgical, temporary method of correcting mild to moderate chin deformity.5–7 Several techniques using cannulas or needles are used to inject HA when performing chin augmentation.8–11 In this article, the authors describe their injection technique according to the anatomical morphology of the chin with HA for chin augmentation and explore the clinical and aesthetic effects of this novel approach.
Materials
This is a retrospective study. Between January 2018 and May 2021, 742 patients underwent HA injection for chin augmentation in the Plastic Surgery Department of the China-Japan Friendship Hospital and MAGIC BeauCare Clinic. Injection locations were identified based on the unique anatomical morphology of each patients' chin. As a control measure, 416 patients who underwent any type of filler injection and/or surgical treatments for the chin previously were excluded from this study. Consequently, 326 patients were involved in this study.
The procedures performed in this study were in accordance with the ethical standards of the Declaration of Helsinki and clinical practice guidelines from the ethic committees of the hospital and clinic. All participants were fully informed about the treatment protocol and potential risks, and signed informed consent and photograph release forms were obtained before injection.
Methods
Before injection, makeup was removed and, participants' face was washed thoroughly. Topical anesthetic cream was applied for 30 to 40 minutes to relieve pain. Patients were semirecumbent at the time of injection. The entire injection areas were carefully cleansed with an antiseptic solution. Chin and adjacent areas were sterilized 3 times with ethanol.
First, HA with high elasticity was injected into the supraperiosteal plane at the paragonion close to the inferior border of the mandibula and roughly perpendicular to the nasal alar or medial canthus with a 27-gauge sharp hypodermic needle. A bolus technique was performed, and the injected volume on each side was typically 0.2 to 0.4 mL and no more than 0.5 mL. The purpose of this injection was to increase the bone volume of the paragonion region and determine mental transverse width.
Second, HA with high elasticity was injected as a supraperiosteal depot with the bolus technique at the pogonion about 15 to 20 mm superior to the inferior mandibular border on the midline through a 27-gauge sharp hypodermic needle. The injected volume was typically 0.3 to 0.4 mL and no more than 0.5 mL. The purpose of this injection was to increase the bone volume of the pogonion region and add anterior projection to the chin.
Hyaluronic acid with high elasticity was then injected into the subcutaneous plane in the rhombic area which is formed by the pogonion, the menton, and the paragonion of both sides through a blunt-tipped 25-gauge, 3-cm cannula. The entry point of the cannula was the same as first injection step at the right side's paragonion. A fanning technique was performed. The injected volume was typically 0.2 to 0.3 mL and no more than 0.5 mL. The purpose of this injection was to increase soft-tissue volume, taper the projection, and create a smooth transition of the chin.
For individuals with prejowl sulcus or labiomandibular grooves, HA with high elasticity was injected into the subcutaneous plane through a blunt-tipped 25-gauge, 5-cm cannula from the same entry point as the first injection step at the paragonion. A retrograde linear threading technique was performed along the mandibula to soften the prejowl sulcus, and a fanning technique was performed to soften the labiomandibular grooves on both sides. The injected volume in this area was typically 0.2 to 0.4 mL and no more than 0.5 mL each side (Figure 2).
Figure 2.
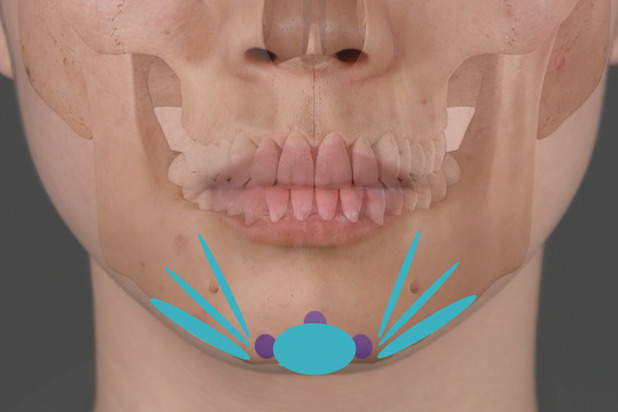
HA was injected onto the supraperiosteal plane with a sharp needle to increase the bone volume and enhance the projection and width of the chin. Subcutaneous plane fanning, threading injections were performed with a cannula to smoothen the overlying skin, soften the prejowl sucus, and reduce the labiomandibular groove on both sides. HA, hyaluronic acid.
During the injection process, an aspiration test was performed for at least 10 seconds before injection. The index finger of the opposite hand was placed at the lower mandibular edge so as to confirm the location and prevent product leakage into the inferior border of the mandibula. Local pressure was palpated with the finger, and the color of the skin was observed. If there was an abnormal reaction such as sudden pain or local whitening, the injection was immediately stopped. After the injection, immediate pressure was applied to the injection area for 5 minutes, and cold compress was applied for 30 minutes to minimize bruising. The effect was evaluated immediately after and 6 months and 1 year after the injection, during which time adverse reactions were observed and recorded. All patients were welcomed to return for follow-up if they experienced any problems or complications at any time.
Results
There were 326 patients (298 female and 28 male) involved in the study; the mean age was 26.4 years (range from 18 to 52); the median injected volume was 1.85 mL (range from 1 to 3) . The shape and contour of the chin was significantly improved in all patients immediately after injection. At the 6-month follow-up, most of the improvements were retained, and partial improvements remained visible 12 months after the injections. Swelling and pain occurred in 284 patients (87.1%) and resolved spontaneously within 2 days. Local ecchymosis occurred in 31 patients (9.5%) with most of them in the central part of the chin. Twenty-nine disappeared within 1 week and 2 disappeared within 2 weeks. Asymmetry was found in 8 patients (2.5%) and corrected by touch-up injection with 0.1 to 0.3 mL of HA.
As of December 29, 2021, 191 patients (58.6%) returned to the hospital and clinic for a repeat injection between 8 and 15 months after initial injection. The follow-up injection technique was the same as initial injection treatment with volume roughly half that of the initial injection. There were no other complications such as infection, embolism, necrosis, nodule, or witch's chin. All patients reported satisfaction with the results of the HA injection treatment. Preinjection and postinjection photographs are shown in Figures 3 and 4 and Supplemental Digital Content 1, Figure S1, http://links.lww.com/DSS/B63.
Figure 3.

Case 1, a 23-year-old woman who received the injection of 2.0 mL of hyaluronic acid for chin augmentation. (A) Before injection, (B) immediately after injection, and (C) 9 months after injection.
Figure 4.
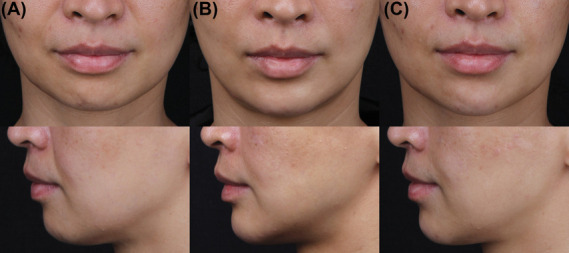
Case 2, a 38-year-old woman who received the injection of 1.4 mL of hyaluronic acid for chin augmentation and a total of 8 U of botox into the hyperdynamic mentalis muscle. (A) Before injection, (B) immediately after injection, and (C) 6 months after injection.
Discussion
The chin is defined by the labiomental crease superiorly, the labiomandibular groove laterally, and the submental cervical crease inferiorly.12 A stereoscopic chin and a smooth jawline are considered standards of beauty and can influence an individual's psychosocial well-being.13 Although aging is one of the causes of chin deformity, the most predominant factor for chin deformity is mental skeleton dysplasia.
All procedures used in chin augmentation technique were performed to alter or simulate the ideal aesthetic shape and contour of the mental skeleton. Alloplastic implants are best for those patients who have adequate vertical chin height but need more projection because implants can only produce significant changes in anterior projection.14 Surgical genioplasty is a larger procedure that can correct all deficiencies. Both these surgical approaches involve extensive dissection and thus confer higher risk of significant complications such as implant rejection or migration, scarring, infection, bone resorption, mental nerve injury, and also result in permanent alteration of the chin which may not look natural.3,4
By contrast, HA injection offers a nonsurgical, temporary alternative that requires no incisions or anesthesia and allows patients to return to work as quickly as the same day. HA allows for correction of vertical, sagittal, and transverse deficiencies of the chin as well as treatment of adjacent structures such as lips and nose.
HJ Moon and colleagues9 described an expert consensus on HA injections for Chinese patients in which they demand injection at 4 sites with 0.25 mL administered at each site through a sharp needle from the point 5 mm superior to the mandibular border on the midline to augment the central part of the chin. We think this technique is useful for patients with mild chin retrusion, but it is not suitable for patients with moderate retrogenia, microgenia, prejowl sulcus, or labiomandibular groove who need more comprehensive treatments.
Sahan and colleagues10 share their experience of chin augmentation and rejuvenation with HA by using a cannula from a single, midline entry point on the menton. A retrograde, lateral-to-medial tunneling technique in a multilayered fashion both supraperiosteally and subcutaneously was performed through the single-entry point. The median injected filler volume for augmentation of the mental area was 2.25 mL. Six percent of patients required a touch-up injection to correct asymmetry, 96% of patients experienced slight to moderate erythema and edema, and 8% of patients exhibited ecchymosis. Eighteen percent of patients were improved, 56% of patients were much improved, and 26% of patients were very much improved according to GAIS. We believe it is not easy to inject accurately into the desired position and plane by the long blunt cannula through the middle entry point because the chin is a three-dimensional structure. In clinical practice, we perform supraperiosteal injection at the paragonion and pogonion to simulate the ideal aesthetic mental skeletal morphology by using a sharp needle which is more precise and simpler than a blunt cannula. In the procedure by Sahan and colleagues, after the injections at the supraperiosteal plane, the projection, length, and width of the chin were enhanced. Additional subdermal fanning, threading type injections were performed to firm and smoothen the overlying skin, soften the prejowl sucus, and reduce the labiomandibular groove on both sides.
It was believed that the use of cannulas may significantly reduce the risk of adverse events while maintaining similar efficacy to needle injection because of their ability to assist injectors in avoiding sharp trauma of the soft tissue and blood vessels.15–17
The occurrence of ecchymosis in our study was 9.5% which is a little higher than that in the study by Sahan, most of which occurred in the central part of the chin where a sharp needle was used. This indicates that a sharp needle does increase trauma and bruising, but we still recommend using a sharp needle for more precise injection as those symptoms dissipated within 1 week in our study in all but 2 cases which required another week for healing.
Chin augmentation with HA injection is subject to many of the same potential complications that can arise with use of HA anywhere on the face. Symptoms such as swelling, bruising, redness, pain, nodules, granuloma, and infection should be treated promptly even if they are in other locations beyond HA injections.7,11,18 As the skin on the chin is quite thick, contour irregularity with supraperiosteal injection is often not of particular concern. However, superficial injection of fillers may produce irregularity, especially with mentalis contraction and animation. In our clinical practice, patients with hyperactive mentalis muscle were injected in 2 points at the paragonion with 4 U of onabotulinumtoxinA, each into the mentalis muscle. Concomitant injection of neuromodulators into a hyperdynamic mentalis muscle can improve the aesthetic appearance of the chin and may also prolong the filler's longevity.19
Vascular complications from chin injection are quite rare but do occur. Yuan and colleagues20 described vascular compromise after injecting 0.1 mL of PLLA in the right lateral chin characterized by an immediate sensation of warmth extending to the lower lip and central chin numbness. Fang and colleagues presented a case with ischemic involvement of chin and neck skin after submental artery involvement after hyaluronic acid filler injection in the chin region. Excessive pain and blanching of skin on the chin occurred immediately after the injection, and livedo reticularis was beginning to show around the blanched skin 10 minutes after injection.21
Improving injection technology and capacity to identify the signs and symptoms of possible intravascular injection are important. We believe the key to safe injection technology is to inject slowly, with low pressure, in the correct plane, and the use of aspiration before injection. Although there has been some controversy regarding the value of aspiration before injection, negative aspiration does not guarantee the avoidance of intravascular injection.22 Positive aspiration confirms that the tip of the needle or cannula entered the blood vessel. Aspiration was performed before injection in all patients in our study, and there were 2 positive cases. Thus, we concluded that it is paramount to perform the aspiration some seconds before the HA injection, and the injection must be interrupted if blood is seen in the syringe.
Pain, pallor, livedo, slow capillary refill, and tenderness are the usual early symptoms and signs of positive aspiration.23 Some of these symptoms and signs may be absent or occur later so close and consistent observation of patient after HA injection is necessary. In our clinical practice, patients were required to be observed for at least half an hour after injection and must be confirmed safe by the doctor before they leave the clinic. Patients were also required to take a clear photograph of the injection area and send it to us within the first day after HA treatment. In cases where the aforementioned signs and symptoms were observed, patients were required to return and undergo further examination.
Suspected ischemic complications of chin HA injection should be addressed with high-dose hyaluronidase, warm compresses, massage, and possibly topical nitroglycerin as early as possible.24,25
Conclusions
Although HA injection is not a permanent method of chin augmentation, it provides the largest flexibility in correcting chin deformities. With our injection technique, the shape and contour of chin can be improved comprehensively without severe complications. We hope our technique can be considered as a viable option for chin augmentation with HA injection.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.dermatologicsurgery.org).
The authors have indicated no significant interest with commercial supporters.
The authors have indicated no significant interest with commercial supporters.
Contributor Information
Li Ma, Email: 534321301@qq.com.
Jingyi Wang, Email: crazybbwang@163.com.
References
- 1.Lee EI. Aesthetic alteration of the chin. Semin Plast Surg 2013;27:155–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chin OY, Sykes JM. Optimizing the chin and jawline appearance: does Surgery or injection make sense? Facial Plast Surg 2019;35:164–71. [DOI] [PubMed] [Google Scholar]
- 3.Sati S, Havlik RJ. An evidence-based approach to genioplasty. Plast Reconstr Surg 2011;127:898–904. [DOI] [PubMed] [Google Scholar]
- 4.Wang Q, Chen X, Wang X, Du Y. A reliable method for chin augmentation by mechanical micronization of lipoaspirates. Aesthet Plast Surg 2021;45:1507–17. [DOI] [PubMed] [Google Scholar]
- 5.Beer K, Stonehouse A, Dunn M. Hyaluronic acid soft tissue filler for the treatment of the hypoplastic chin: an observational study. Dermatol Surg 2020;46:1092–101. [DOI] [PubMed] [Google Scholar]
- 6.Ogilvie P, Sattler G, Gaymans F, Belhaouari L, et al. Safe, effective chin and jaw restoration with VYC-25L hyaluronic acid injectable gel. Dermatol Surg 2019;45:1294–303. [DOI] [PubMed] [Google Scholar]
- 7.Moradi A, Shirazi A, David R. Nonsurgical chin and jawline augmentation using calcium hydroxylapatite and hyaluronic acid fillers. Facial Plast Surg 2019;35:140–8. [DOI] [PubMed] [Google Scholar]
- 8.Maio M. MD CodesTM: a methodological approach to facial aesthetic treatment with injectable hyaluronic acid fillers. Aesthet Plast Surg 2021;45:690–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moon HJ, Gao ZW, Hu ZQ, Wang H, et al. Expert consensus on hyaluronic acid filler facial injection for Chinese patients. Plast Reconstr Surg Glob Open 2020;8:e3219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sahan A, Karaosmanoglu N, Ozdemir Cetinkaya P. Chin augmentation with the use of cannula from a single, midline entry point: evaluation of 50 patients. J Cosmet Dermatol 2020;19:1301–6. [DOI] [PubMed] [Google Scholar]
- 11.Vazirnia A, Braz A, Fabi SG. Nonsurgical jawline rejuvenation using injectable fillers. J Cosmet Dermatol 2020;19:1940–7. [DOI] [PubMed] [Google Scholar]
- 12.Pilsl U, Anderhuber F. The chin and adjacent fat compartments. Dermatol Surg 2010;36:214–8. [DOI] [PubMed] [Google Scholar]
- 13.de Maio M, Wu WTL, Goodman GJ, Monheit G, et al. Facial assessment and injection guide for botulinum toxin and injectable hyaluronic acid fillers: focus on the lower face. Plast Reconstr Surg 2017;140:393e–404e. [DOI] [PubMed] [Google Scholar]
- 14.Sykes JM, Fitzgerald R. Choosing the best procedure to augment the chin: is anything better than an implant? Facial Plast Surg 2016;32:507–12. [DOI] [PubMed] [Google Scholar]
- 15.Alam M, Tung R. Injection technique in neurotoxins and fillers: indications, products, and outcomes. J Am Acad Dermatol 2018;79:423–35. [DOI] [PubMed] [Google Scholar]
- 16.Alam M, Kakar R, Dover JS, Harikumar V, et al. Rates of vascular occlusion associated with using needles vs cannulas for filler injection. JAMA Dermatol 2021;157:174–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hexsel D, Soirefmann M, Porto MD, Siega C, et al. Double-blind, randomized, controlled clinical trial to compare safety and efficacy of a metallic cannula with that of a standard needle for soft tissue augmentation of the nasolabial folds. Dermatol Surg 2012;38:207–14. [DOI] [PubMed] [Google Scholar]
- 18.Heydenrych I, Kapoor KM, De Boulle K, Goodman G, et al. A 10-point plan for avoiding hyaluronic acid dermal filler-related complications during facial aesthetic procedures and algorithms for management. Clin Cosmet Investig Dermatol 2018;11:603–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hsu AK, Frankel AS. Modification of chin projection and aesthetics with onabotulinumtoxinA injection. JAMA Facial Plast Surg 2017;19:522–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yuan JT, Chang TW, Yu SS, Arron ST, et al. Mental artery occlusion from poly-L-lactic acid injection at the lateral chin. Dermatol Surg 2017;43:1402–5. [DOI] [PubMed] [Google Scholar]
- 21.Fang M, Rahman E, Kapoor KM. Managing complications of submental artery involvement after hyaluronic acid filler injection in chin region. Plast Reconstr Surg Glob Open 2018;6:e1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goodman GJ, Magnusson MR, Callan P, Roberts S, et al. Aspiration before tissue filler-an exercise in futility and unsafe practice. Aesthet Surg J 2022;42:89–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rzany B, DeLorenzi C. Understanding, avoiding, and managing severe filler complications. Plast Reconstr Surg 2015;136:196S–203S. [DOI] [PubMed] [Google Scholar]
- 24.Wibowo A, Kapoor KM, Philipp-Dormston WG. Reversal of post-filler vision loss and skin ischaemia with high-dose pulsed hyaluronidase injections. Aesthet Plast Surg 2019;43:1337–44. [DOI] [PubMed] [Google Scholar]
- 25.Cohen JL, Biesman BS, Dayan SH, DeLorenzi C, et al. Treatment of hyaluronic acid filler-induced impending necrosis with hyaluronidase: consensus recommendations. Aesthet Surg J 2015; 35: 844–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


