Abstract
Aims
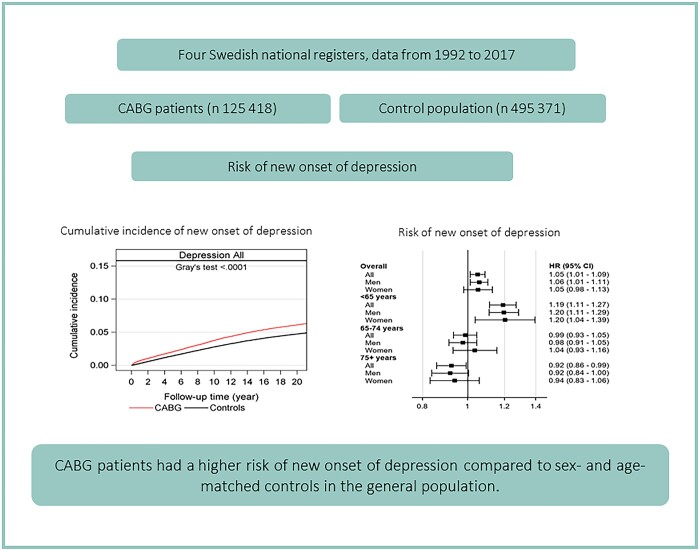
A diagnosis of depression in patients with coronary heart disease is associated with worse outcomes. This study examined the long-term risk for new onset of depression after coronary artery bypass grafting (CABG) compared to an age- and sex-matched control group from the general population.
Methods and results
In total, 125 418 primary isolated CABG patients and 495 371 matched controls were included from 1992 to 2017. The SWEDEHEART registry and three other national registers were used to acquire information about baseline characteristics and depression. The adjusted risk of depression was estimated by using Cox regression models adjusted for patient characteristics, and socioeconomic variables, described by hazard ratios (HR) and 95% confidence intervals (CI). In total, 6202 (4.9%) CABG patients and 17 854 (3.6%) controls developed depression. The cumulative incidence of depression was higher in CABG patients than in the control population [6.1%, 95% CI 6.0–6.3 vs. 4.7% (4.7–4.8), P < 0.0001]. Overall, the CABG group had a marginally increased adjusted risk of depression compared to controls [adjusted HR (aHR): 1.05 (1.01–1.09), P = 0.0091]. In age-specific analyses, the increased risk compared to controls was only present in patients <65 years [aHR: 1.19 (1.11–1.27), P <0.0001] and was only evident during the first 5 years after surgery.
Conclusion
Patients who underwent CABG had a higher risk of new onset of depression compared to sex- and age-matched controls in the general population. The risk of depression was especially pronounced in younger patients during the first 5 years after surgery.
Keywords: Coronary artery bypass grafting, Depression, Survival
Graphical Abstract
Graphical Abstract.
Introduction
Depression affects 30–40% of all patients undergoing CABG1 and is an established risk factor for cardiovascular morbidity and mortality.2 The prevalence of depression in the general population ranges between 5% and 9% with a higher prevalence in women than in men.1 A preoperative diagnosis of depression is associated with increased risks of re-hospitalization, heart failure, stroke, myocardial infarction, and death after CABG.2–4 Depression after cardiac surgery increases the risk of poor physical and emotional recovery5 and has been found to increase cardiac readmissions for up to 6 months postoperatively and rates of cardiac events for up to 8 years.6,7 Depression is also the strongest predictor for the poor quality of life in patients with coronary artery disease.8 In a large study including >1 million patients, new onset of depression was present in 5.6% of patients readmitted within 14–90 days after CABG.5 However, it is not known whether CABG patients have an increased risk of new onset of depression after CABG compared to individuals in the general population.
The aim of this nationwide population-based cohort study was to investigate the long-term risk of new onset of depression after CABG by comparing patients with an age- and sex-matched control group from the general population.
Methods
Design
We conducted a nationwide population-based cohort study. The present study was composed according to recommendations in the Strengthening the Reporting of Observational Studies in Epidemiology statement.9
Study population and data sources
All patients over 18 years of age (n = 128 139) who underwent a primary isolated CABG in Sweden during 1992–2017 were identified from the SWEDEHEART (Swedish Web-system for Enhancement and Development of Evidence-based care in Heart disease Evaluated According to Recommended Therapies) registry.10–12
The Swedish Total Population Register13 held by Statistics Sweden was used to assign four controls without cardiac surgery for each CABG patient, matched by sex, age, and home county (n = 509 966). Date of inclusion of the controls was the day of surgery for the matching CABG patient. Patients and controls with a previous history of depression were excluded (n = 2721 CABG patients and n = 14 595 controls). Flowchart describing the inclusion and exclusion process is presented in Supplementary material online, Figure S1.
To assemble the study database, the Swedish personal identity number14 was used by the National Board of Health and Welfare. Baseline characteristics were obtained from the SWEDEHEART register and the Swedish National Patient Register (NPR).15 The NPR has a complete national coverage from 1987 for all diagnoses and all patients hospitalized in Sweden. We used the NPR to identify patients with a diagnosis of depression using the International Classification of Diseases (ICD), version 9 from 1987 to 1996 and version 10 from 1997 onwards. Principal and contributing diagnoses of depression were collected from the NPR using ICD-9 codes 296, 311, 300.4, and 309.0 and the ICD-10 code F3. Information about diagnoses for comorbidities in individuals undergoing CABG and individuals in the control group was collected from the NPR before the date of admission for CABG surgery (Supplementary material online, Table S1). Information about socioeconomic status was obtained from the Longitudinal Integration Database for Health Insurance and Labor Market Studies (LISA).16 Level of education was stratified into <10, 10–12, and >12 years. Annual disposable household income at the year of surgery was stratified into quintiles from Q1 (lowest) to Q5 (highest), with the consumer price index used to adjust income over time. Civil status was categorized as married/cohabiting, unmarried/not cohabiting, divorced, and widowed. The Cause of Death Registry was used to identify cases of death.17
Primary outcome and follow-up
The primary outcome in this study was the new onset of depression after CABG. The day of CABG surgery was defined as the index date. All individuals undergoing CABG in Sweden between 1 January 1992 and 31 December 2017 were included and the follow-up ended on 31 December 2017. Patients and controls who emigrated (n = 21, <0.1% and n = 68, <0.1%, respectively) were censored at the time of emigration. The follow-up for the primary outcome was complete.
Statistical analysis
Categorical variables are presented as n (%), while continuous variables are presented as mean (standard deviation)/median (min; max)/n or as median and interquartile range (IQR) as applicable. For comparison between two groups, Fisher’s exact test (lowest one-sided P-value multiplied by 2) was used for dichotomous variables, the Mantel–Haenszel chi-square trend test was used for ordered categorical variables, the chi-square test was used for non-ordered categorical variables, and the Mann–Whitney U-test was used for continuous variables. Incidence rates for new onset of depression were estimated as the number of individuals diagnosed with the event of depression divided by the total follow-up time in the study and reported as the number of cases per 1000 person-years. Exact Poisson limits were used to estimate 95% confidence intervals (CI) for the event rates. Cumulative incidence functions handling death as competing risk were graphically presented, and unadjusted comparisons were made between the groups using Gray’s test.
Cox proportional hazards regression was used to estimate the risk of depression, with a first model adjusted for age and sex and a second model adjusted for age, sex, marital status, education, income, year of surgery, myocardial infarction, hypertension, diabetes, heart failure, atrial fibrillation, stroke, peripheral vascular disease, renal failure, chronic respiratory disease, cancer, congenital heart disease, and hyperlipidaemia. Hazard ratios (HR) with 95% CI were calculated as relative differences between the groups. Interactions between the group variable, the age category (<65, 65–74, ≥75 years), and sex were investigated and found to be significant, and so as well as presenting overall estimates, all analyses were additionally stratified on age category and sex. The proportional hazards assumption was evaluated by reviewing log [−log(survival)] vs. log(time) curves. To have this assumption fulfilled, the curves should be parallel. The curves revealed that the relative difference between the patient and control group diminished over time. Hence, time-specific analyses in 5-year intervals from the surgery were also performed. Missing data for the variables measuring education (2.4%) and income (<0.1%) were handled as their own category in the analysis adjustments. All tests were two-tailed. All calculations were performed using version 9.4 of SAS (SAS Institute Inc., Cary, NC, USA).
Ethical standards
The study was performed in accordance with the Declaration of Helsinki and was approved by the Regional Research Ethics Committee in Gothenburg (registration number: 139-16). To ensure anonymity, all personal identifiers were replaced by codes in the dataset before analysis. The need for individual patient consent was waived by the committee.
Results
Baseline characteristics
The distribution of demographic and clinical characteristics of the study population at the start of follow-up is presented in Table 1. We identified 125 418 individuals who underwent primary isolated CABG between January 1992 and December 2017, and 495 371 age-, sex-, and county-matched controls were included from the general population. The median follow-up time was 10.5 (IQR: 5.7–15.4) years in the CABG group and 9.1 (IQR 3.9–14.8) years among controls. In both the patient group and the control group, the mean age was 67.3 years and 22% of the participants were women. The CABG group and the control population were not balanced regarding most baseline characteristics (Table 1). Patients undergoing CABG had a higher proportion of comorbidities than the control population. Baseline characteristics by sex and age groups are shown in Supplementary material online, Table S2.
Table 1.
Patient characteristics at baseline in the coronary artery bypass grafting group and the matched control population
| CABG group, n (%) | Matched control population, n (%) | P-value | |
|---|---|---|---|
| No. patients | 125 418 | 495 371 | |
| Age, mean (SD) | 67.3 (9.3) | 67.3 (9.3) | 0.82 |
| Sex | 0.50 | ||
| Men | 97 790 (78.0) | 385 804 (77.9) | |
| Women | 27 628 (22.0) | 109 567 (22.21) | |
| Comorbidities | |||
| Myocardial infarction | 60 143 (48.0) | 23 064 (4.7) | <0.0001 |
| Diabetes | 27 022 (21.5) | 30 242 (6.1) | <0.0001 |
| Hypertension | 50 477 (40.2) | 53 652 (10.8) | <0.0001 |
| Heart failure | 20 114 (16.0) | 18 957 (3.8) | <0.0001 |
| Atrial fibrillation | 22 030 (17.6) | 26 252 (5.3) | <0.0001 |
| Prior stroke | 8485 (6.8) | 24 122 (4.9) | <0.0001 |
| Chronic respiratory disease | 7754 (6.2) | 19 233 (3.9) | <0.0001 |
| Renal failure | 3152 (2.5) | 4497 (0.9) | <0.0001 |
| Congenital heart disease | 536 (0.4) | 484 (0.1) | <0.0001 |
| Peripheral vascular disease | 8877 (7.1) | 12 076 (2.4) | <0.0001 |
| Cancer | 9619 (7.7) | 47 573 (9.6) | <0.0001 |
| Hyperlipidaemia | 31 611 (25.2) | 12 160 (2.5) | <0.0001 |
| Marital status | <0.0001 | ||
| Married/cohabiting | 82 362 (65.7) | 307 807 (62.1) | |
| Not married | 12 309 (9.8) | 64 704 (13.1) | |
| Divorced | 17 721 (14.1) | 72 146 (14.6) | |
| Widowed | 13 026 (10.4) | 50 714 (10.2) | |
| Education | <0.0001 | ||
| <10 years | 59 667 (48.3) | 225 419 (46.7) | |
| 10–12 years | 45 214 (36.6) | 170 304 (35.3) | |
| >12 years | 18 722 (15.1) | 86 823 (18.0) | |
| Missing | 1815 | 12 825 | |
| Income | <0.0001 | ||
| Q1 (lowest) | 21 287 (17.0) | 102 862 (20.8) | |
| Q2 | 26 289 (21.0) | 97 795 (19.7) | |
| Q3 | 27 422(21.9) | 96 796 (19.5) | |
| Q4 | 26 846 (21.4) | 97 301 (19.6) | |
| Q5 | 23 573 (18.8) | 100 581 (20.3) | |
| Missing | 1 | 36 |
CABG, coronary artery bypass grafting; SD, standard deviation.
Incidence of depression
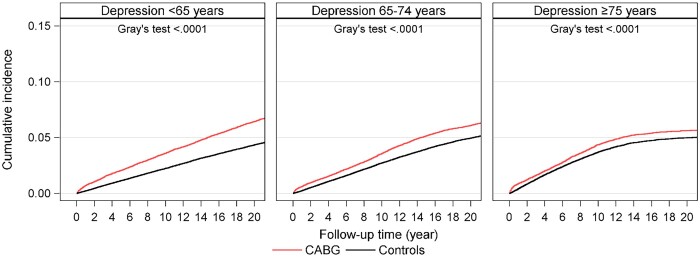
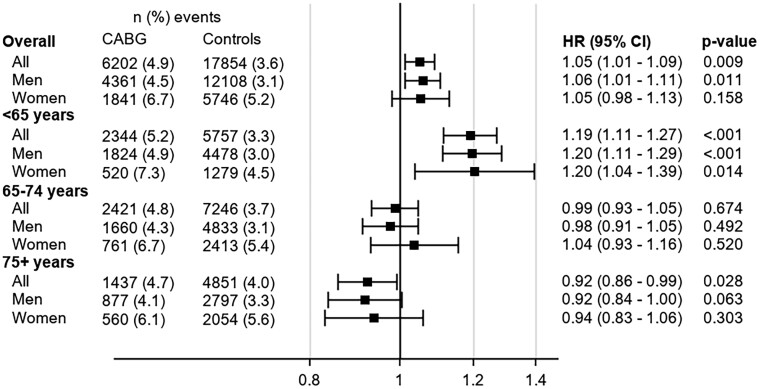
During follow-up, a total of 6202 (4.9%) patients in the CABG group and 17 854 (3.6%) in the control population developed new onset of depression (Table 2). Crude event rates for total follow-up are shown in Table 2, and crude event rates within the first 5 years in Supplementary material online, Table S3. The overall cumulative incidence of new onset of depression, accounting for the competing risk of death, was higher in the CABG group than in the control population (6.1%, 95% CI: 6.0–6.3 vs. 4.7%, 95% CI: 4.7–4.8, P < 0.0001) after 20 years of follow-up (Figure 1 and Supplementary material online, Table S4). The corresponding incidences of depression were higher in CABG patients regardless of age category (Figure 2 and Supplementary material online, Table S4). Both women and men undergoing CABG had higher cumulative incidences than women and men in the control population (women 7.9%, 95% CI: 7.6–8.3 vs. 6.6%, 95% CI, 6.4–6.8; and men 5.6%, 95% CI: 5.4–5.7 vs. 4.2%, 95% CI: 4.1–4.3) (Supplementary material online, Figure S2 and Supplementary material online, Table S4). The cumulative incidence rate for new onset of depression by age group and sex is presented in Supplementary material online, Figure S3 and Supplementary material online, Table S4.
Table 2.
Diagnosis of new onset depression, incidence rates with 95% confidence intervals and age-, sex-, and multivariable-adjusted hazard ratios with 95% confidence intervals by age group
| Diagnosis of depression, n (%) |
Incidence rate per 1000 person-years (95% CI) |
Hazard ratio (95% CI) |
||||
|---|---|---|---|---|---|---|
| CABG | Control | CABG | Control | Crude a | Multivariable adjustedb | |
| Total population | ||||||
| All individuals | 6202 (4.9) | 17 854 (3.6) | 4.58 (4.47–4.70) | 3.69 (3.64–3.75) | 1.25 (1.21–1.28) | 1.05 (1.01–1.09) |
| <65 years | 2344 (5.2) | 5757 (3.3) | 4.02 (3.86–4.19) | 2.75 (2.68–2.82) | 1.47 (1.40–1.54) | 1.19 (1.11–1.27) |
| 65–74 years | 2421 (4.8) | 7246 (3.7) | 4.61 (4.43–4.80) | 3.89 (3.80–3.98) | 1.19 (1.14–1.25) | 0.99 (0.93–1.05) |
| ≥75 years | 1437 (4.9) | 4851(4.0) | 5.84 (5.54–6.15) | 5.56 (5.40–5.72) | 1.05 (0.99–1.12) | 0.92 (0.86–0.99) |
| Men | ||||||
| All individuals | 4361 (4.5) | 12 108 (3.1) | 4.13 (4.01–4.25) | 4.13 (4–01 - 4.25) | 1.25 (1.21–1.29) | 1.06 (1.01–1.11) |
| <65 years | 1824 (4.9) | 4478 (3.0) | 3.73 (3.56–3.91) | 3.73 (3.56–3.91) | 1.44 (1.37–1.52) | 1.20 (1.11–1.29) |
| 65–74 years | 1660 (4.3) | 4833 (3.1) | 4.14 (3.94–4.35) | 4.14 (3.94–4.35) | 1.18 (1.12–1.25) | 0.98 (0.92–1.05) |
| ≥75 years | 877 (4.1) | 2797 (3.3) | 5.26 (4.91–5.62) | 5.26 (4.91–5.62) | 1.06 (0.98–1.14) | 0.92 (0.84–1.00) |
| Women | ||||||
| All individuals | 1841 (6.7) | 5746 (5.2) | 6.20 (5.92–6.49) | 5.03 (4.90–5.16) | 1.24 (1.17–1.30) | 1.05 (0.98–1.13) |
| <65 years | 520 (7.3) | 1279 (4.5) | 5.56 (5.09–6.06) | 3.53 (3.34–3.73) | 1.58 (1.43–1.75) | 1.20 (1.04–1.39) |
| 65–74 years | 761 (6.7) | 2413 (5.4) | 6.12 (5.69–6.57) | 5.07 (4.87––5.28) | 1.22 (1.13–1.32) | 1.04 (0.93–1.16) |
| ≥75 years | 560 (6.1) | 2054 (5.6) | 7.07 (6.50–7.68) | 6.75 (6.47–7.05) | 1.04 (0.95–1.15) | 0.94 (0.83–1.06) |
CI, confidence intervals; HR, hazard ratios.
The study population was age- and sex-matched to the control population.
Multivariable-adjusted model is adjusted for age, sex, marital status, education, income, year of surgery, and comorbidities at baseline: myocardial infarction, hypertension, diabetes, heart failure, atrial fibrillation, stroke, peripheral vascular disease, renal failure, chronic respiratory disease, cancer, congenital heart disease, and hyperlipidaemia.
Figure 1.
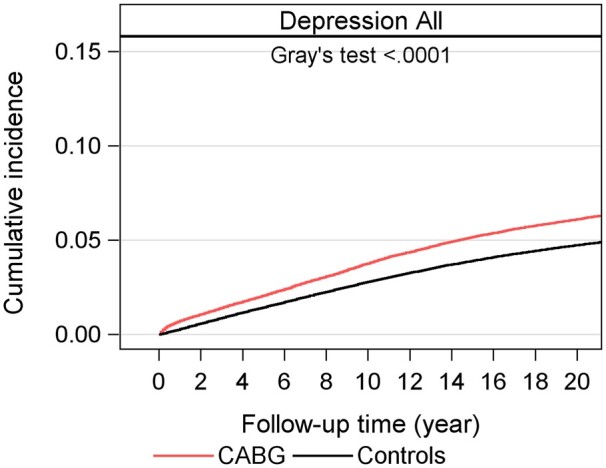
Cumulative incidence of new on-set of depression in 125 418 patients who underwent coronary artery bypass grafting in Sweden 1992–2017 compared to an age- and sex-matched control population.
Figure 2.
Cumulative incidence of new on-set of depression, accounted for competing risk, for the coronary artery bypass grafting group and control group overall, by age category.
Risk of depression
In the crude model, the overall risk of new onset of depression was higher in the CABG group than in the control population (HR: 1.25, 95% CI: 1.21–1.28) (Figure 3 and Table 2). This risk was attenuated after adjustment for comorbidities [adjusted HR (aHR)): 1.05, 95% CI: 1.10–1.09]. Due to the significant interaction between group and age category, the association between CABG and new onset of depression was also investigated by age categories. Among the youngest individuals in the CABG group (<65 years), the risk of depression was higher than in the control population (aHR: 1.19, 95% CI: 1.11–1.27), but no such association was observed in the 65–75-year-old CABG group (aHR: 0.99, 95% CI: 0.93–1.05) or in the ≥75 years CABG group (aHR: 0.92, 95% CI: 0.86–0.99). Sex-specific analyses in patients aged <65 years showed an increased risk of depression in the CABG group for both men (aHR: 1.20, 95% CI: 1.11–1.29) and women (aHR: 1.20, 95% CI: 1.04–1.39) (Figure 3 and Table 2).
Figure 3.
Adjusted hazard ratios with 95% confidence intervals for time to new onset of depression by age category and sex.
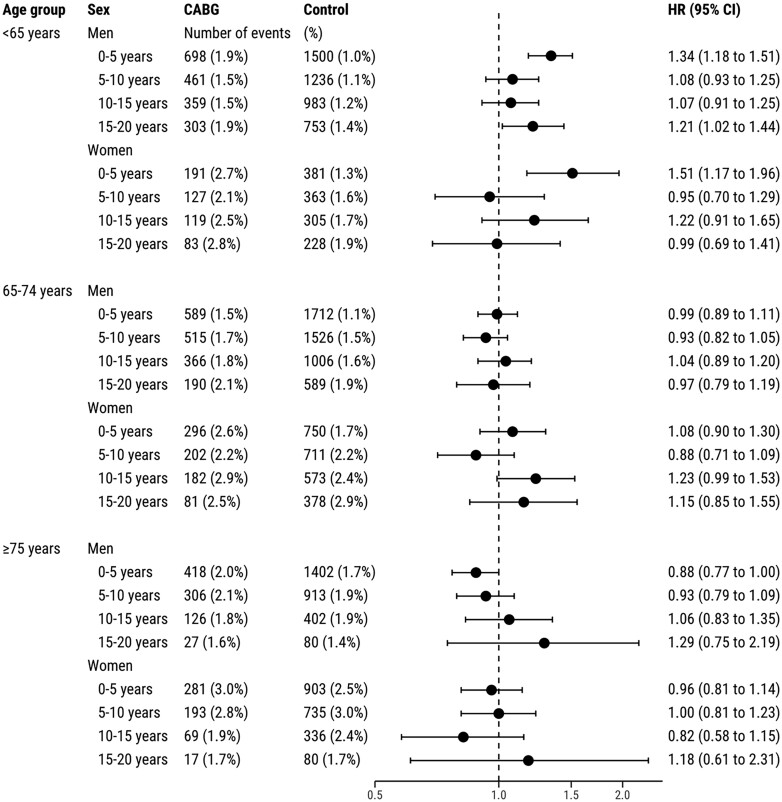
Risk of depression by age group, sex, and time period
The risk of depression in the CABG group compared to the control population was also studied in time periods: 0–5, 5–10, 10–15, and 15–20 years after surgery (Figure 4). In the CABG group, both men and women in the youngest age group (<65 years) had a significantly increased risk of depression during the first 5 years after surgery (aHR: 1.34, 95% CI: 1.18–1.51 in men; and aHR: 1.51, 95% CI: 1.17–1.96 in women). During the later time periods, the risk of new-onset depression in patients <65 years was not significantly higher in the CABG group. In contrast, patients aged 65–74 and ≥75 years undergoing CABG had no increased risk of depression compared to controls from the general population during the first 5 years (aHR: 1.02, 95% CI: 0.92–1.12; and aHR: 0.90, 95% CI: 0.81–1.00, respectively) or during the following time periods (Figure 4).
Figure 4.
Adjusted risk for new onset of depression in patients who underwent coronary artery bypass grafting compared to the control population by age category, sex, and follow-up time period.
Discussion
The main finding in this large nationwide population-based cohort study was that younger CABG patients had an increased risk of new-onset depression, compared to matched controls from the general population, during the first 5 years after surgery.
In the general population, the prevalence of depression worldwide ranges between 5% and 9% and is higher in women than in men.1 Moreover, the incidence of depression is about 2–3 times higher in patients with coronary heart disease than in the general population.18,19 In a review by Tully and Baker,1 30–40% of individuals undergoing CABG were affected by any depression (i.e. major, minor, or dysthymia) immediately leading up to and after surgery, but the studies differed markedly in study design and exposure.1 In the present study, we aimed to assess the association between CABG and new onset of severe depression compared to the general population. Depressive status was established from ICD codes in the NPR with almost 100% coverage since 1973.15 There are reasons to believe that a large proportion of patients undergoing cardiac surgery are under-diagnosed and under-treated for depression. Many patients might be depressed without knowing or do not want to seek help. Ideally, the ICD-based diagnoses in the present study should have been completed with patient-reported symptoms of depression. However, by using ICD codes, we were able to capture the most severely ill patients as all patients with an ICD code in the NPR have been treated for their depression in a hospital or by a psychiatrist in a specialized outpatient clinic. We found that individuals undergoing CABG had a higher proportion and risk of new onset of depression compared to matched controls from the general population. Previous studies investigating this risk have lacked a control population.1,5 To our knowledge, no previous study has investigated the risk of depression in patients undergoing CABG compared with an age- and sex-matched control population.
Chronic illness and cardiovascular diseases are known risk factors for developing depression.20 In the present study, individuals who underwent CABG had a higher proportion of cardiovascular comorbidities than the control population, which could have contributed to their higher risk of developing depression. However, the increase in risk remained after adjustments for comorbidities and social factors such as marital status, education, and household income. Moreover, this increased risk was more pronounced among the youngest CABG patients than in the older age groups. New onset of depression after CABG might therefore be attributed to factors than those we adjusted for in the statistical analysis. Lifestyle behaviours, poor social functioning, and emotional distress, for example, have been described as contributing to impaired health status following cardiac surgery.21,22
Our results imply that younger age (<65 years) was associated with a higher risk of new onset of depression in individuals who underwent CABG, a finding that has been described previously.5 The risk of depression in patients with coronary artery disease is correlated to known cardiovascular risk factors such as previous stroke, heart failure, and diabetes. In general, younger individuals with depression are more likely than their non-depressed counterparts to smoke, to be physically inactive, to have higher body mass index, and to be less adherent to medication.23 These personal and behavioural factors are also associated with coronary artery disease.24 In the present study, the youngest patients had a markedly higher burden of comorbidities than individuals of the same age in the general population.
CABG is a procedure associated with increased levels of preoperative anxiety.25 It is possible that preoperative anxiety has a higher impact on postoperative new onset of depression in younger patients than in older patients, due to expectance and acceptance. An older person might be better prepared for illness than a younger person and therefore might accept the situation more easily. For a young person, a severe heart condition has a huge impact on daily life activities and work capacity. Moreover, socioeconomic disadvantages such as low disposable family income are associated with increased risk of depression and mortality after CABG26–28 and are more pronounced among younger CABG patients.20 The youngest patients are often in paid employment, and a CABG procedure involves sick leave and loss of income. It is therefore possible that loss of income has a greater impact on new onset of depression among younger patients than among elderly patients. It is also possible that younger individuals undergoing CABG have greater difficulties coping with the consequences of a life-threatening disease that requires surgery and lifelong medical treatment since, unlike older individuals, they might not be prepared for the possibility of having heart disease.
Screening for depression in all patients with cardiovascular disease (CVD) has been recommended by the American Heart Association (AHA) since 2008.19 A recent statement from the AHA29 further stressed the importance of screening for depression in these patients and also emphasized that psychological health should be taken into account when evaluating patients with or at risk of CVD. CVD should not be addressed as an isolated condition, but rather as one part of an integrated system consisting of mind, heart, and body. A previous study showed that ∼10% of patients who screened negative at the time of surgery had a positive depression screen 1 year after CABG.30
The results from the present study suggest that individuals undergoing CABG should be screened for depression on a regular basis during the first 5 years after surgery for the early identification of depression. If depression is detected by these screenings, it is more likely to be treated, and work disability with further loss of income, poor quality of life, and cardiac readmissions might be avoided.
Strengths and limitations
The main strengths of this study are related to the nationwide coverage, including a large population with four matched controls from the general population for each patient in the CABG population, an extensive follow-up (20 years), and no loss to follow-up. Due to the large number of individuals included, statistically significant results may arise, although effect sizes were limited. Therefore, significant associations should be interpreted with caution because they may not necessarily be clinically relevant. Limitations include the observational study design, which carries the risk of residual confounding and selection bias, and the lack of information about behavioural or lifestyle factors. In the present study, the diagnoses for depression in the NPR were limited to hospitalized patients and to out-patients treated in hospitals; diagnoses for patients treated at primary care facilities and by general practitioners were not included. Hence, our registry-based study design has identified patients with severe depression. In this study, age- and sex-matched individuals from the general population were used as a control group. It can be argued that a more appropriate control group would be patients with a comparable disease or patients who have undergone surgery similar to CABG. However, previous studies investigating the risk of new-onset depression in CABG patients have lacked any control population and we believe that it is thus reasonable to first compare the patients to the general population.
In conclusion, patients who underwent primary isolated CABG had an increased risk of new onset of depression compared to matched controls from the general population. The risk was especially pronounced in younger patients during the first 5 years after surgery.
Lead author biography

Susanne J. Nielsen is an operating theatre nurse and associate professor in cardiovascular epidemiology at the Department of Cardiothoracic Surgery, Sahlgrenska University Hospital, Gothenburg, Sweden, and Institute of Medicine, Sahlgrenska Academy, University of Gothenburg. Her research interest includes cardiovascular epidemiology, cardiovascular surgery, and secondary prevention.
Data availability
The data underlying this article were provided by the Swedish Board of Health and Welfare, Swedish Association of Local Authorities and Regions, Swedish Statistics, and the SWEDEHEART registry. Data will be shared on request to the corresponding author with enclosed permission from these parties.
Supplementary material
Supplementary material is available at European Heart Journal Open online.
Supplementary Material
Acknowledgements
The authors thank the SWEDEHEART registry for providing data for the study.
Funding
The study was supported by the Swedish Heart-Lung Foundation (grant no. 20180560 to AJ, grant no. 20160420 to SJN, and grant no. 20190533 to US); the Swedish state (grant no. ALFGBG-725131 to AJ and ALFGBG-942665 to SN) under the agreement between the Swedish government and the county councils concerning economic support of research and education of doctors (ALF agreement); Västra Götaland Region (grant nos. VGFOUREG-847811 and VGFOUREG-665591 to AJ); and the Stiftelsen Familjen Nils Winbergs Fond.
Conflict of interest: A.J. has received fees for consultancy or lectures from Werfen, Boehringer-Ingelheim, Portola, Baxter, and LFB, all unrelated to the present work.
References
- 1. Tully PJ, Baker RA.. Depression, anxiety, and cardiac morbidity outcomes after coronary artery bypass surgery: a contemporary and practical review. J Geriatr Cardiol 2012;9:197–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Stenman M, Holzmann MJ, Sartipy U.. Antidepressant use before coronary artery bypass surgery is associated with long-term mortality. Int J Cardiol 2013;167:2958–2962. [DOI] [PubMed] [Google Scholar]
- 3. Stenman M, Holzmann MJ, Sartipy U.. Relation of major depression to survival after coronary artery bypass grafting. Am J Cardiol 2014;114:698–703. [DOI] [PubMed] [Google Scholar]
- 4. Connerney I, Shapiro PA, McLaughlin JS, Bagiella E, Sloan RP.. Relation between depression after coronary artery bypass surgery and 12-month outcome: a prospective study. Lancet 2001;358:1766–1771. [DOI] [PubMed] [Google Scholar]
- 5. Aguayo E, Lyons R, Juo YY, Bailey KL, Seo YJ, Dobaria V, Sanaiha Y, Benharash P.. Impact of new-onset postoperative depression on readmission outcomes after surgical coronary revascularization. J Surg Res 2019;233:50–56. [DOI] [PubMed] [Google Scholar]
- 6. Tully PJ, Baker RA, Turnbull D, Winefield H.. The role of depression and anxiety symptoms in hospital readmissions after cardiac surgery. J Behav Med 2008;31:281–290. [DOI] [PubMed] [Google Scholar]
- 7. Burg MM, Benedetto MC, Soufer R.. Depressive symptoms and mortality two years after coronary artery bypass graft surgery (CABG) in men. Psychosom Med 2003;65:508–510. [DOI] [PubMed] [Google Scholar]
- 8. Lane D, Carroll D, Ring C, Beevers DG, Lip GY.. Effects of depression and anxiety on mortality and quality-of-life 4 months after myocardial infarction. J Psychosom Res 2000;49:229–238. [DOI] [PubMed] [Google Scholar]
- 9. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP.. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–349. [DOI] [PubMed] [Google Scholar]
- 10. Jernberg T, Attebring MF, Hambraeus K, Ivert T, James S, Jeppsson A, Lagerqvist B, Lindahl B, Stenestrand U, Wallentin L.. The Swedish Web-system for enhancement and development of evidence-based care in heart disease evaluated according to recommended therapies (SWEDEHEART). Heart 2010;96:1617–1621. [DOI] [PubMed] [Google Scholar]
- 11. Emilsson L, Lindahl B, Köster M, Lambe M, Ludvigsson JF.. Review of 103 Swedish Healthcare Quality Registries. J Intern Med 2015;277:94–136. [DOI] [PubMed] [Google Scholar]
- 12. Vikholm P, Ivert T, Nilsson J, Holmgren A, Freter W, Ternström L, Ghaidan H, Sartipy U, Olsson C, Granfeldt H, Ragnarsson S, Friberg Ö.. Validity of the Swedish Cardiac Surgery Registry. Interact Cardiovasc Thorac Surg 2018;27:67–74. [DOI] [PubMed] [Google Scholar]
- 13. Ludvigsson JF, Almqvist C, Bonamy AK, Ljung R, Michaëlsson K, Neovius M, Stephansson O, Ye W.. Registers of the Swedish total population and their use in medical research. Eur J Epidemiol 2016;31:125–136. [DOI] [PubMed] [Google Scholar]
- 14. Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, Ekbom A.. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol 2009;24:659–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, Heurgren M, Olausson PO.. External review and validation of the Swedish national inpatient register. BMC Public Health 2011;11:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ludvigsson JF, Svedberg P, Olén O, Bruze G, Neovius M.. The longitudinal integrated database for health insurance and labour market studies (LISA) and its use in medical research. Eur J Epidemiol 2019;34:423–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Brooke HL, Talbäck M, Hörnblad J, Johansson LA, Ludvigsson JF, Druid H, Feychting M, Ljung R.. The Swedish cause of death register. Eur J Epidemiol 2017;32:765–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Vaccarino V, Badimon L, Bremner JD, Cenko E, Cubedo J, Dorobantu M, Duncker DJ, Koller A, Manfrini O, Milicic D, Padro T, Pries AR, Quyyumi AA, Tousoulis D, Trifunovic D, Vasiljevic Z, De Wit C, Bugiardini R.. Depression and coronary heart disease: 2018 position paper of the ESC working group on coronary pathophysiology and microcirculation. Eur Heart J 2020;41:1687–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lichtman JH, Bigger JT Jr, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lespérance F, Mark DB, Sheps DS, Taylor CB, Froelicher ES.. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation 2008;118:1768–1775. [DOI] [PubMed] [Google Scholar]
- 20. Li H, Ge S, Greene B, Dunbar-Jacob J.. Depression in the context of chronic diseases in the United States and China. Int J Nurs Sci 2019;6:117–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bauer LK, Caro MA, Beach SR, Mastromauro CA, Lenihan E, Januzzi JL, Huffman JC.. Effects of depression and anxiety improvement on adherence to medication and health behaviors in recently hospitalized cardiac patients. Am J Cardiol 2012;109:1266–1271. [DOI] [PubMed] [Google Scholar]
- 22. Huffman JC, Celano CM, Beach SR, Motiwala SR, Januzzi JL.. Depression and cardiac disease: epidemiology, mechanisms, and diagnosis. Cardiovasc Psychiatry Neurol 2013;2013:695925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Whooley MA, de Jonge P, Vittinghoff E, Otte C, Moos R, Carney RM, Ali S, Dowray S, Na B, Feldman MD, Schiller NB, Browner WS.. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA 2008;300:2379–2388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Malakar AK, Choudhury D, Halder B, Paul P, Uddin A, Chakraborty S.. A review on coronary artery disease, its risk factors, and therapeutics. J Cell Physiol 2019;234:16812–16823. [DOI] [PubMed] [Google Scholar]
- 25. Korbmacher B, Ulbrich S, Dalyanoglu H, Lichtenberg A, Schipke JD, Franz M, Schäfer R.. Perioperative and long-term development of anxiety and depression in CABG patients. Thorac Cardiovasc Surg 2013;61:676–681. [DOI] [PubMed] [Google Scholar]
- 26. Nielsen S, Giang KW, Wallinder A, Rosengren A, Pivodic A, Jeppsson A, Karlsson M.. Social factors, sex, and mortality risk after coronary artery bypass grafting: population-based cohort study. J Am Heart Assoc 2019;8:e011490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Poole L, Leigh E, Kidd T, Ronaldson A, Jahangiri M, Steptoe A.. The combined association of depression and socioeconomic status with length of post-operative hospital stay following coronary artery bypass graft surgery: data from a prospective cohort study. J Psychosom Res 2014;76:34–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Dalén M, Ivert T, Holzmann MJ, Sartipy U.. Household disposable income and long-term survival after cardiac surgery: a Swedish nationwide cohort study in 100,534 patients. J Am Coll Cardiol 2015;66:1888–1897. [DOI] [PubMed] [Google Scholar]
- 29. Levine GN, Cohen BE, Commodore-Mensah Y, Fleury J, Huffman JC, Khalid U, Labarthe DR, Lavretsky H, Michos ED, Spatz ES, Kubzansky LD.. Psychological health, well-being, and the mind-heart-body connection: a scientific statement from the American Heart Association. Circulation 2021;143:e763–e83. [DOI] [PubMed] [Google Scholar]
- 30. Stenman M, Sartipy U.. Longitudinal changes in depression screening results in cardiac surgery patients. J Thorac Dis 2019;11:920–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article were provided by the Swedish Board of Health and Welfare, Swedish Association of Local Authorities and Regions, Swedish Statistics, and the SWEDEHEART registry. Data will be shared on request to the corresponding author with enclosed permission from these parties.