Abstract
Background
The CovidSurg-Cancer Consortium aimed to explore the impact of COVID-19 in surgical patients and services for solid cancers at the start of the pandemic. The CovidSurg-Gynecologic Oncology Cancer subgroup was particularly concerned about the magnitude of adverse outcomes caused by the disrupted surgical gynecologic cancer care during the COVID-19 pandemic, which are currently unclear.
Objective
This study aimed to evaluate the changes in care and short-term outcomes of surgical patients with gynecologic cancers during the COVID-19 pandemic. We hypothesized that the COVID-19 pandemic had led to a delay in surgical cancer care, especially in patients who required more extensive surgery, and such delay had an impact on cancer outcomes.
Study Design
This was a multicenter, international, prospective cohort study. Consecutive patients with gynecologic cancers who were initially planned for nonpalliative surgery, were recruited from the date of first COVID-19-related admission in each participating center for 3 months. The follow-up period was 3 months from the time of the multidisciplinary tumor board decision to operate. The primary outcome of this analysis is the incidence of pandemic-related changes in care. The secondary outcomes included 30-day perioperative mortality and morbidity and a composite outcome of unresectable disease or disease progression, emergency surgery, and death.
Results
We included 3973 patients (3784 operated and 189 nonoperated) from 227 centers in 52 countries and 7 world regions who were initially planned to have cancer surgery. In 20.7% (823/3973) of the patients, the standard of care was adjusted. A significant delay (>8 weeks) was observed in 11.2% (424/3784) of patients, particularly in those with ovarian cancer (213/1355; 15.7%; P<.0001). This delay was associated with a composite of adverse outcomes, including disease progression and death (95/424; 22.4% vs 601/3360; 17.9%; P=.024) compared with those who had operations within 8 weeks of tumor board decisions. One in 13 (189/2430; 7.9%) did not receive their planned operations, in whom 1 in 20 (5/189; 2.7%) died and 1 in 5 (34/189; 18%) experienced disease progression or death within 3 months of multidisciplinary team board decision for surgery. Only 22 of the 3778 surgical patients (0.6%) acquired perioperative SARS-CoV-2 infections; they had a longer postoperative stay (median 8.5 vs 4 days; P<.0001), higher predefined surgical morbidity (14/22; 63.6% vs 717/3762; 19.1%; P<.0001) and mortality (4/22; 18.2% vs 26/3762; 0.7%; P<.0001) rates than the uninfected cohort.
Conclusion
One in 5 surgical patients with gynecologic cancer worldwide experienced management modifications during the COVID-19 pandemic. Significant adverse outcomes were observed in those with delayed or cancelled operations, and coordinated mitigating strategies are urgently needed.
Key words: complications, COVID-19, delay, gynecologic cancer, pandemic, surgery
Introduction
The COVID-19 pandemic took the entire world off guard and led numerous healthcare systems to redesign their clinical services for the reallocation of available resources and accommodate the changes in treatment priorities.1, 2, 3, 4, 5, 6, 7, 8 This study was conducted when little was known about the true magnitude of the virus and when effective therapeutic strategies were lacking.2, 3, 4, 5, 6
AJOG at a Glance.
Why was this study conducted?
This is a large, prospective, international, gynecologic cancer cohort study summarizing the treatment alternations and their related impact on patients who were planned to have cancer surgery during the initial period of the COVID-19 pandemic (early 2020).
Key findings
In 20.7% (823/3973), care plans were changed compared with prepandemic practice, including operating in alternative hospitals, changes to perioperative systematic treatments, significant delay (>8 week; 11.2%; 424/3784), and cancellation (7.9%; 189/2430), which were associated with more frequent adverse outcomes.
What does this add to what is known?
With significant contribution in gynecologic cancer cases from low- and middle-income countries (26.9%; 1067/3973), this study provided important global data on the magnitude of care changes and the associated adverse outcomes experienced by patients with gynecologic cancer during the early stages of a global pandemic, which could be used to leverage resources for the ongoing mitigating strategies worldwide.
Women with gynecologic cancers were among the most affected populations during the pandemic, and patients appealed for more robust provision of high standard care, even in times of crisis.9 The pandemic has particularly challenged surgical care delivery for those with more advanced or relapsed disease, where surgery can be life-prolonging but not curative. Surgeries were being delayed or replaced by systemic or palliative care options that had previously been associated with poorer and less favorable outcomes.10 Moreover, other COVID-19-related events such as delayed diagnosis through the repeatedly imposed lockdowns, increased perioperative complications and mortality through the active COVID-19, and exhausted healthcare resources such as theater space and intensive care capacity were also observed.1, 2, 3, 4, 5, 6, 7 , 11
This study aimed to assess the early impact of the pandemic-related modifications to clinical management on the outcomes in surgical gynecologic cancer patients. We hypothesized that the COVID-19 pandemic had led to a delay in surgical cancer care, especially in patients who required more extensive surgery, and such delay had an impact on cancer outcomes. This study is an international prospective multicenter analysis of patients with gynecologic cancers treated during the pandemic.
Materials and Methods
Study design
This was a multicenter, international, prospective cohort study analyzing the clinical and surgical outcomes of patients with gynecologic cancer who had or were planned to have treatment as first line during the COVID-19 pandemic era. The study was part of the wider GlobalSurg-CovidSurg Consortium (https://globalsurg.org/CovidSurg/)—an umbrella study encompassing all solid cancer types and aiming to explore the impact of COVID-19 in surgical patients and services across multiple specialties.12 , 13 The study was prospectively registered (NCT04384926) and designed to inform clinical care as the pandemic evolves; the short study period encouraged wider participation at the time that resources were severely restricted owing to the competing needs to the pandemic.
Before the start of the study, each cancer group had the opportunity to add additional questions on the Case Report Form (CRF) to support the need to explore the impact of the COVID-19 pandemic particularly relevant to them. The gynecologic cancer group was particularly concerned about the impact of the pandemic on treatment adjustments and the subsequent clinical outcomes. The related outcomes are stated as secondary outcomes in this report to be consistent with the main CovidSurg-Cancer study.
Equivalent results of other cancer types and generic methods applying to all cancers (eg, inclusion criteria and patient identification) have been published previously.14 This study included hospitals that included all patients discussed for surgery regardless of whether they were operated on or not.
Any hospital that performed elective cancer surgery and was affected by the COVID-19 pandemic, was eligible to participate. The participating hospitals were identified by local principal investigators. Study approvals for participating hospitals were secured by local principal investigators before entry into the study and data collection. The study protocol was either registered as a clinical audit with institutional review or a research study obtaining ethical committee approval, depending on local and national requirements. Investigators were invited to identify a start date, representing the start of the emergence of COVID-19 in their respective hospitals.
All consecutive adult (age≥18 years) surgical patients with multidisciplinary team (MDT) decisions supporting surgery were captured by the participating centers (local principal investigators) from that point for the next 3 months (representing the first peak period of the COVID-19 pandemic). Only centers confirming the complete inclusion and follow-up of all nonoperated patients (labeled as “Group 1 hospitals” by the CovidSurg study team) were included in analyses comparing operated and nonoperated patients. The definition of lockdown stringency and the level of COVID-19 burden areas (classified as a median of at least 25 cases per 100,000 per 14 days, representing the World Health Organization [WHO] recommendations at the time of the study) were previously described.13 , 14
Patients and procedures
Inclusion criteria:
-
1.
Patients who underwent surgery for gynecologic cancer with curative or life-prolonging intent during the COVID-19 pandemic
or
-
2.
Patients with gynecologic cancer who would have been planned for curative or life-prolonging cancer surgery in the pre-COVID-era but had their surgery delayed or cancelled after multidisciplinary team discussions.
Exclusion criteria:
-
1.
Patients who were planned for palliative surgery or nonsurgical treatments
-
2.
Patients who were suspected of having or were confirmed to have SARS-CoV-2 infection at the time of the MDT decisions.
Consecutive eligible patients were identified from MDT meetings, operating lists, and outpatient or virtual clinics. The day of surgery was defined as day zero, with patients followed up for 30 days postoperatively using routine follow-up pathways. COVID-19 diagnosis was made through nasopharyngeal swab and polymerase chain reaction, computed tomography thorax, or clinical symptoms consistent with COVID-19.
Patients who had a therapeutic operation for suspected cancer that was subsequently shown to be a preinvasive or benign lesion after histologic examination and full organ resection (eg, high-grade dysplasia or carcinoma in situ) were still included in this study. Elective surgery was defined as any surgery booked in advance of a planned admission to hospital.15 The primary outcomes of the cross-specialty COVIDSurg study were the 30-day postoperative pulmonary complications (COVID-19 infection, pneumonia, acute respiratory distress syndrome, and unexpected ventilation), and they were previously reported.13
Key study outcomes of the gyneco-oncological cohort
The primary outcome of this analysis was as follows:
-
•
The incidence of pandemic-related changes in care
The secondary outcomes were as follows:
-
1.
30-day postoperative morbidity and mortality rates
-
2.
Postoperative hospital stay and critical care utilization rates
-
3.
Proportion of patients with the time between the decision for surgery to the date of surgery of >8 weeks. In the United Kingdom, the national target for providing cancer treatments from the time of the decision made by the MDT is 31 days (approximately 4 weeks). The 8-week cutoff was chosen to represent a significant delay in the time to surgery, as a recent meta-analysis suggested that a treatment delay for >4 weeks was associated with poorer cancer outcomes in a range of nongynecologic cancers.10
-
4.
Proportion of nonoperated patients with progression to incurable disease or death by 3 months after decision for surgery
-
5.
A composite outcome of unresectable disease or disease progression (eg, upstaging), emergency surgery, and death to measure the potential impact of any treatment delays or adjustment
Data collection and follow-up
Patients were recruited from the date of first COVID-19-related admission in each participating center for 3 months, as identified by the local investigators. The follow-up period was extended to 3 months from the time of study entry (when care decision was made) for each participant.
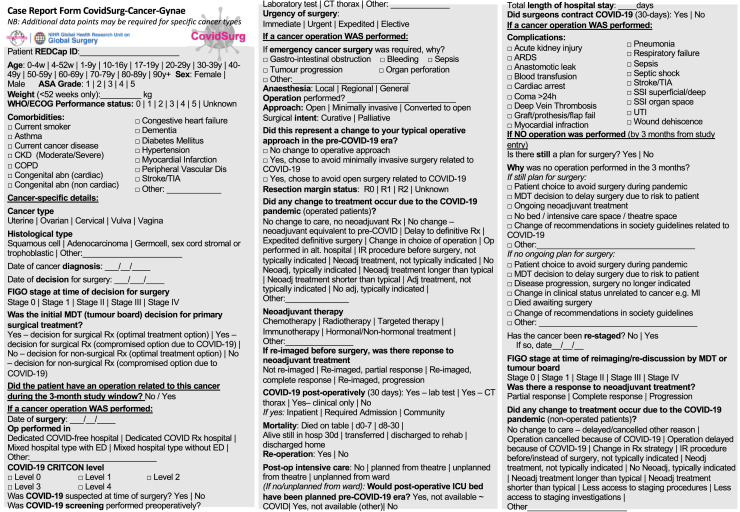
Anonymized data were collected online and stored on a secure server running the Research Electronic Data Capture (REDCap) web application16 based in the University of Birmingham, United Kingdom. The CRF of the CovidSurg-GO is presented as Supplemental Figure.
Supplemental Figure.
Case Report Form for COVIDSurg-Cancer (gyneco-oncology)
Fotopoulou. Gynecologic cancer surgery during the COVID-19 pandemic. Am J Obstet Gynecol 2022.
Statistical analysis
The study was conducted according to guidelines set by the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement for observational studies.17 Chi-square tests were used to compare differences in categorical data apart from when cell sizes were small, when the Fisher exact tests were used. Continuous nonparametric data are presented as medians and interquartile ranges, and median differences between groups were compared using the Mann–Whitney U-test. Missing data are included in summary tables when applicable. Analysis was performed used Stata SE version 16.1 (StataCorp, College Station, TX) and open-source data science tools (Pandas Data Frame [Open-Source Software] and Python [Open-Source Software] using Juptyer notebook). The collected data were checked for consistency, cleaned, and exported. Vectorized operations were used when possible to archive fast turnaround time during the debugging phase. For visualization, the Matplotlib and Seaborn packages were used.
Results
Patients and tumor-related characteristics
We recruited a total of 3973 patients from 227 centers across 52 countries with the following geographic distribution: 2402 patients (60%) from Europe and Central Asia, 484 (12%) from Latin America & Caribbean, 376 (10%) from East Asia & Pacific, 277 (7%) from South Asia, 244 (6%) from North America, 160 (4%) from the Middle East and North Africa, and 24 (1%) from Sub-Saharan Africa (Table 1 ). Only 189 patients did not undergo surgery (4.8%); these were excluded from all analyses pertaining to surgical data alone.
Table 1.
Demographics and cancer related characteristics of all included patients—surgical and nonsurgical (n=3973)a
| Uterus (n=1811) | Ovary (n=1459) | Cervix (n=462) | Vulva/vagina (n=235) | Total (n=3973) | |
|---|---|---|---|---|---|
| Age (y) | |||||
| 17–19 | 1 (0.1) | 12 (0.8) | 0 (0) | 0 (0) | 13 (0.3) |
| 20–29 | 7 (0.4) | 65 (4.5) | 24 (5.2) | 4 (1.7) | 100 (2.5) |
| 30–39 | 56 (3.1) | 113 (7.8) | 122 (26.4) | 7 (3.0) | 299 (7.5) |
| 40–49 | 175 (9.7) | 265 (18.2) | 144 (31.2) | 22 (9.4) | 608 (15.3) |
| 50–59 | 473 (26.1) | 380 (26.1) | 99 (21.4) | 52 (22.1) | 1004 (25.3) |
| 60–69 | 554 (30.6) | 380 (26.1) | 42 (9.1) | 49 (20.9) | 1027 (25.9) |
| 70–79 | 421 (23.3) | 198 (13.6) | 27 (5.8) | 58 (24.7) | 705 (17.7) |
| 80–89 | 119 (6.6) | 46 (3.2) | 4 (0.9) | 41 (17.5) | 210 (5.3) |
| >90 | 5 (0.3) | 0 (0) | 0 (0) | 2 (0.9) | 7 (0.2) |
| Region | |||||
| Europe & Central Asia | 1122 (62.0) | 820 (56.2) | 272 (58.9) | 188 (80.0) | 2408 (60.6) |
| Latin America & Caribbean | 201 (11.1) | 180 (12.3) | 85 (18.4) | 18 (7.7) | 484 (12.2) |
| East Asia & Pacific | 178 (9.8) | 141 (9.7) | 53 (11.5) | 4 (1.7) | 376 (9.5) |
| South Asia | 74 (4.1) | 177 (12.1) | 18 (3.9) | 8 (3.4) | 277 (7.0) |
| North America | 147 (8.1) | 67 (4.6) | 20 (4.3) | 10 (4.3) | 244 (6.1) |
| Middle East & North Africa | 81 (4.5) | 70 (4.8) | 4 (0.9) | 5 (2.1) | 160 (4.0) |
| Sub-Saharan Africa | 8 (0.4) | 4 (0.27) | 10 (2.2) | 2 (0.9) | 24 (0.6) |
| Income group | |||||
| High | 1400 (77.3) | 982 (67.3) | 321 (69.5) | 197 (83.8) | 2906 (73.1) |
| Upper middle | 305 (16.8) | 222 (15.2) | 115 (24.9) | 30 (12.8) | 705 (17.7) |
| Low-middle | 106 (5.9) | 255 (17.5) | 26 (5.6) | 8 (3.4) | 362 (9.1) |
| BMI (kg/m2) | |||||
| <18.5 | 25 (1.4) | 61 (4.2) | 19 (4.1) | 8 (3.4) | 113 (2.8) |
| 18.5–24.9 | 496 (27.4) | 683 (46.8) | 228 (49.4) | 86 (36.6) | 1495 (37.6) |
| 25–29.9 | 531 (29.3) | 423 (29.0) | 125 (27.1) | 73 (31.1) | 1155 (29.1) |
| 30–34.9 | 363 (20.0) | 184 (12.6) | 57 (12.3) | 37 (15.7) | 642 (16.2) |
| 35–39.9 | 195 (10.8) | 63 (4.3) | 20 (4.3) | 18 (7.7) | 296 (7.5) |
| ≥40 | 184 (10.2) | 37 (2.5) | 9 (2.0) | 9 (3.8) | 239 (6.0) |
| Not available | 17 (0.9) | 8 (0.6) | 4 (0.9) | 4 (1.7) | 33 (0.8) |
| WHO performance status | |||||
| 0 | 1065 (58.8) | 863 (59.2) | 387 (83.8) | 132 (56.2) | 2448 (61.6) |
| 1 | 520 (28.7) | 446 (30.6) | 58 (12.6) | 71 (30.2) | 1095 (27.6) |
| 2 | 124 (6.9) | 102 (7.0) | 5 (1.1) | 19 (8.1) | 250 (6.3) |
| 3 | 20 (1.1) | 13 (0.9) | 0 (0) | 4 (1.7) | 37 (0.9) |
| 4 | 1 (0.1) | 2 (0.1) | 0 (0) | 3 (1.3) | 6 (0.2) |
| Not available | 81 (4.5) | 33 (2.3) | 12 (2.6) | 6 (2.6) | 137 (3.5) |
| CCI | |||||
| 0 | 205 (11.3) | 427 (29.3) | 274 (59.3) | 27 (11.5) | 936 (23.6) |
| 1 | 387 (21.4) | 356 (24.4) | 86 (18.6) | 42 (17.9) | 871 (21.9) |
| 2 | 487 (26.9) | 341 (23.4) | 41 (8.9) | 44 (18.7) | 914 (23.0) |
| 3 | 410 (22.6) | 212 (14.5) | 37 (8.0) | 48 (20.4) | 707 (17.8) |
| 4 | 207 (11.4) | 77 (5.3) | 14 (3.0) | 39 (16.6) | 338 (8.5) |
| 5 | 76 (4.2) | 31 (2.1) | 1 (0.2) | 21 (8.9) | 130 (3.3) |
| 6 | 30 (1.7) | 11 (0.8) | 6 (1.3) | 6 (2.6) | 53 (1.3) |
| 7 | 5 (0.3) | 2 (0.1) | 1 (0.2) | 6 (2.6) | 14 (0.4) |
| 8 | 3 (0.2) | 1 (0.1) | 1 (0.2) | 2 (0.9) | 7 (0.2) |
| 9 | 1 (0.1) | 1 (0.1) | 1 (0.2) | 0 (0) | 3 (0.1) |
| ASA grade | |||||
| 1 | 381 (21.0) | 417 (28.6) | 216 (46.8) | 34 (14.5) | 1048 (26.4) |
| 2 | 1013 (55.9) | 786 (53.9) | 205 (44.4) | 137 (58.3) | 2145 (54.0) |
| 3 | 402 (22.2) | 240 (16.5) | 39 (8.4) | 61 (26.0) | 743 (18.7) |
| 4 | 9 (0.5) | 15 (1.0) | 1 (0.2) | 2 (0.9) | 27 (0.7) |
| 5 | 1 (0.1) | 0 (0) | 1 (0.2) | 0 (0) | 2 (0.1) |
| Not available | 5 (0.3) | 0 (0) | 0 (0) | 0 (0) | 8 (0.2) |
| FIGO stage | |||||
| Not cancer | 58 (3.2) | 81 (5.6) | 57 (12.3) | 24 (10.2) | 221 (5.6) |
| 1 | 1276 (70.5) | 452 (31.0) | 300 (64.9) | 142 (60.4) | 2173 (54.7) |
| 2 | 175 (9.7) | 124 (8.5) | 51 (11.0) | 22 (9.4) | 373 (9.4) |
| 3 | 202 (11.2) | 555 (38.0) | 45 (9.7) | 37 (15.7) | 839 (21.1) |
| 4 | 62 (3.4) | 227 (15.6) | 9 (2.0) | 4 (1.7) | 302 (7.6) |
| Not available | 38 (2.1) | 20 (1.4) | 0 (0) | 6 (2.6) | 65 (1.6) |
| Histology | |||||
| SCC | 22 (1.2) | 31 (2.1) | 323 (69.9) | 198 (84.3) | 578 (14.6) |
| Adenocarcinoma | 1611 (89.0) | 1116 (76.5) | 118 (25.5) | 9 (3.8) | 2854 (71.8) |
| GCST | 13 (0.7) | 110 (7.5) | 0 (0) | 3 (1.3) | 127 (3.2) |
| Other | 139 (7.7) | 34 (2.3) | 7 (1.5) | 18 (7.7) | 198 (5.0) |
| Benign/preinvasive/borderline | 21 (1.2) | 133 (9.1) | 14 (3.0) | 5 (2.1) | 173 (4.4) |
| Not available | 5 (0.3) | 35 (2.4) | 0 (0) | 2 (0.9) | 43 (1.1) |
Data are presented as total number (percentage). Details of operated vs non-operated group separately, are presented in Supplemental Table 2 and 4.
ASA grade, American Society of Anaesthesiologists Physical Status Classification system; BMI, body mass index; CCI, Charlson Comorbidity Index; FIGO, International Federation of Gynaecology and Obstetrics; GCST, germ cell, sex cord stromal or trophoblastic tumors; NACT, neoadjuvant chemotherapy; SCC, squamous cell carcinoma; WHO, World Health Organization.
Fotopoulou. Gynecologic cancer surgery during the COVID-19 pandemic. Am J Obstet Gynecol 2022.
Six patients (0.1%) did not have a recorded cancer site.
Almost half (n=1949; 49%) of the patients were ≥60 years old. Most of the patients had either uterine or ovarian cancer (n= 3270; 82%), were from high-income countries (n=2906; 73%), were either overweight or obese (n=2332; 59%), had a performance status of 0 (n=2448; 62%), had an American Society of Anaesthesiologists (ASA) grade of 1 or 2 (n=3193; 80%), and an International Federation of Gynaecology and Obstetrics (FIGO) stage 1 cancer (n=2173; 55%). The patient- and tumor-related characteristics are summarized in Table 1 and Supplemental Tables 1 and 2.
Approximately 1 in 13 (189/2430; 7.9%) operations were cancelled (Table 2 ). Those in low- and middle-income countries (LMICs; 36/156; 23%) who had stage 3 or 4 cancers (81/705; 11.5%), those in areas where there was a full lockdown (153/1339; 11%), and those in areas with low COVID-19 burden (53/321; 16%) were associated with a higher proportion of nonoperated patients. Table 2 includes only Group 1 hospitals, as they were the only ones that also included a nonoperated cohort to make a valid comparison of operated and nonoperated patients.
Table 2.
Comparison of operated and non-operated cohorts at hospitals that have included all patients discussed at tumor boards (group 1 hospitals; n=2430)
| Non-operated (n=189) | Operated (n=2241) | Proportion not operated | P value | |
|---|---|---|---|---|
| Age (y) | ||||
| 17–19 | 0 (0) | 6 (0.3) | 0/6 (0) | .793 |
| 20–29 | 6 (3.2) | 53 (2.4) | 6/59 (10.2) | |
| 30–39 | 11 (5.8) | 163 (7.3) | 11/174 (6.3) | |
| 40–49 | 24 (12.7) | 297 (13.3) | 24/321 (7.5) | |
| 50–59 | 38 (20.1) | 555 (24.8) | 38/593 (6.4) | |
| 60–69 | 49 (25.9) | 584 (26.1) | 49/633 (7.7) | |
| 70–79 | 34 (18.0) | 449 (20.0) | 34/483 (7.0) | |
| 80–89 | 26 (13.8) | 130 (5.8) | 26/156 (16.7) | |
| >90 | 1 (0.5) | 4 (0.2) | 1/5 (20) | |
| Income group | ||||
| High | 132 (69.8) | 1885 (84.1) | 132/2017 (6.5) | .003 |
| Upper middle | 21 (11.1) | 236 (10.5) | 21/257 (8.2) | |
| Low-middle | 36 (19.1) | 120 (5.4) | 36/156 (23.1) | |
| BMI (kg/m2) | ||||
| <18.5 | 4 (2.1) | 53 (2.4) | 4/57 (7.0) | .933 |
| 18.5–24.9 | 72 (38.1) | 796 (35.5) | 72/868 (8.3) | |
| 25–29.9 | 43 (22.8) | 636 (28.4) | 43/679 (6.3) | |
| 30–34.9 | 34 (18.0) | 371 (16.6) | 34/405 (8.4) | |
| 35–39.9 | 12 (6.4) | 198 (8.8) | 12/210 (5.7) | |
| ≥40 | 19 (10.1) | 160 (7.1) | 19/179 (10.6) | |
| Not available | 5 (2.7) | 27 (1.2) | 5/32 (15.6) | |
| WHO performance status | ||||
| 0 | 77 (40.7) | 1408 (62.8) | 77/1485 (5.2) | .054 |
| 1 | 79 (41.8) | 601 (26.8) | 79/680 (11.6) | |
| 2 | 25 (13.2) | 153 (6.8) | 25/178 (14.0) | |
| 3 | 4 (2.1) | 24 (1.1) | 4/28 (14.3) | |
| 4 | 2 (1.1) | 2 (0.1) | 2/4 (50) | |
| Not available | 2 (1.1) | 53 (2.4) | 2/4 (50) | |
| CCI | ||||
| 0 | 40 (21.2) | 477 (21.3) | 40/517 (7.7) | .568 |
| 1 | 28 (14.8) | 475 (21.2) | 28/503 (5.6) | |
| 2 | 43 (22.8) | 532 (23.7) | 43/575 (7.5) | |
| 3 | 28 (14.8) | 424 (18.9) | 28/452 (6.2) | |
| 4 | 27 (14.3) | 198 (8.8) | 27/225 (12.0) | |
| 5 | 10 (5.3) | 86 (3.8) | 10/96 (10.4) | |
| 6 | 12 (6.3) | 32 (1.4) | 12/44 (27.3) | |
| 7 | 1 (0.5) | 9 (0.4) | 1/10 (10) | |
| 8 | 0 (0) | 5 (0.2) | 0/5 (0) | |
| 9 | 0 (0) | 3 (0.1) | 0/3 (0) | |
| ASA grade | ||||
| 1 | 36 (19.1) | 536 (23.9) | 36/572 (6.3) | .259 |
| 2 | 91 (48.2) | 1235 (55.1) | 91/1326 (6.9) | |
| 3 | 55 (29.1) | 450 (20.1) | 55/505 (10.9) | |
| 4 | 3 (1.6) | 16 (0.7) | 3/19 (15.8) | |
| 5 | 0 (0) | 1 (<0.1) | 0/1 (0) | |
| Not available | 4 (2.1) | 3 (0.1) | 4/7 (57) | |
| Cancer site | ||||
| Uterus | 60 (31.8) | 1036 (46.2) | 60/1096 (5.5) | .101 |
| Ovary | 104 (55.0) | 798 (35.6) | 104/902 (11.5) | |
| Cervix | 13 (6.9) | 254 (11.3) | 13/267 (4.9) | |
| Vagina/vulva | 12 (6.4) | 152 (6.8) | 12/164 (7.3) | |
| Not available | 0 (0) | 1 (<0.1) | 0/1 (0) | |
| FIGO stagea | ||||
| Not cancer | 9 (4.8) | 121 (5.4) | 9/130 (6.9) | .044 |
| 1 or 2 | 93 (49.2) | 1440 (64.3) | 93/1533 (6.1) | |
| 3 or 4 | 81 (42.9) | 624 (27.8) | 81/705 (11.5) | |
| Not available | 6 (3.2) | 56 (2.5) | 6/62 (9.7) | |
| Lockdown stringency | ||||
| Full | 153 (81.0) | 1186 (52.9) | 153/1339 (11.4) | .001 |
| Moderate | 29 (15.3) | 457 (20.4) | 29/486 (6.0) | |
| Light | 7 (3.7) | 598 (26.7) | 7/605 (1.2) | |
| COVID-19 burden | ||||
| High burden | 136 (72.0) | 1973 (88.0) | 136/2109 (6.5) | .008 |
| Low burden | 53 (28.0) | 321 (13.2) | 53/321 (16.5) |
Data presented as total number (percentage) or proportion (percentage).
ASA grade, American Society of Anaesthesiologists Physical Status Classification system; BMI, body mass index; CCI, Charlson Comorbidity Index; FIGO, International Federation of Gynaecology and Obstetrics; WHO, World Health Organization.
Fotopoulou. Gynecologic cancer surgery during the COVID-19 pandemic. Am J Obstet Gynecol 2022.
Comparison of those with cancer and FIGO-stage only.
The treatment intent, surgical details, and postoperative outcomes are summarized in Table 3 . The median time from MDT decision to surgery was 3 weeks (interquartile range, 1–5 weeks); 11.2% (424/3784) patients underwent surgery more than 8 weeks after the initial MDT decision.
Table 3.
Treatment intent, surgical details and postoperative outcomes of patients who underwent gynecologic cancer surgery (n=3784)
| Uterus (n=1751) | Ovary (n=1355) | Cervix (n=449) | Vulva/vagina (n=223) | Total (n=3784) | P value | |
|---|---|---|---|---|---|---|
| Treatment intenta | ||||||
| Curative | 1669 (95.3) | 1095 (80.8) | 426 (94.8) | 204 (91.5) | 3400 (89.9) | .977 |
| Life-prolonging | 79 (4.5) | 258 (19.0) | 23 (5.1) | 19 (8.5) | 379 (10.0) | |
| Palliative | 2 (0.1) | 2 (0.2) | 0 (0) | 0 (0) | 4 (0.1) | |
| Not available | 1 (0.1) | 0 (0) | 0 (0) | 0 (0) | 1 (<0.1) | |
| Neoadjuvant therapy | ||||||
| Chemotherapy | 29 (1.7) | 279 (20.6) | 15 (3.3) | 5 (2.2) | 328 (8.7) | <.0001 |
| Radiotherapy | 19 (1.1) | 1 (0.1) | 2 (0.5) | 3 (1.4) | 25 (0.7) | .008 |
| Hormonal therapy | 14 (0.8) | 2 (0.1) | 0 (0) | 0 (0) | 16 (0.4) | .024 |
| Targeted therapy | 0 (0) | 4 (0.3) | 0 (0) | 0 (0) | 4 (0.1) | .127 |
| Other | 0 (0) | 1 (0.1) | 0 (0) | 0 (0) | 1 (<0.1) | .774 |
| Time to operation | 3 (1–5) | 3 (1–5) | 3 (1–5) | 3 (2–5) | 3 (1–5) | <.0001 |
| ≤8 wk | 1605 (91.7) | 1142 (84.3) | 405 (90.2) | 202 (90.6) | 3360 (88.8) | |
| >8 wk | 146 (8.3) | 213 (15.7) | 44 (9.8) | 21 (9.4) | 424 (11.2) | |
| Areas of surgical resectionb | ||||||
| Pelvis/Perineal | 1443 (82.4) | 616 (45.5) | 374 (83.3) | 189 (84.8) | 2624 (69.3) | <.0001 |
| Midabdominal | 122 (7.0) | 430 (31.7) | 6 (1.3) | 4 (1.8) | 562 (14.9) | |
| Upper-abdominal | 120 (6.9) | 171 (12.6) | 27 (6.0) | 1 (0.5) | 319 (8.4) | |
| Others | 66 (3.8) | 138 (10.2) | 42 (9.4) | 29 (13.0) | 279 (7.4) | |
| Bowel surgery | ||||||
| No | 1734 (99.0) | 1252 (92.4) | 439 (97.8) | 220 (98.7) | 3651 (96.5) | <.0001 |
| Yes | 17 (1.0) | 103 (7.6) | 10 (2.2) | 3 (1.4) | 133 (3.5) | |
| Approach | ||||||
| Open | 751 (42.9) | 1101 (81.3) | 292 (65.0) | 204 (91.5) | 2353 (62.2) | <.0001 |
| Minimally-invasive | 963 (55.0) | 211 (15.6) | 150 (33.4) | 17 (7.6) | 1342 (35.5) | |
| Converted | 37 (2.1) | 42 (3.1) | 5 (1.1) | 0 (0) | 84 (2.2) | |
| Not available | 0 (0) | 1 (0.1) | 2 (0.5) | 2 (0.9) | 5 (0.1) | |
| Postoperative stay (d) | 3 (1–5) | 5 (3–8) | 3 (1–5) | 3 (2–6) | 4 (2–6) | .0001 |
| 30-d surgical morbidity | ||||||
| Any complications | 274 (15.7) | 303 (22.4) | 88 (19.6) | 65 (29.2) | 731 (19.3) | <.0001 |
| Respiratory complications | 18 (1.0) | 32 (2.4) | 4 (0.9) | 4 (1.8) | 58 (1.5) | .030 |
| COVID-19 infection | 7 (0.4) | 14 (1.0) | 1 (0.2) | 0 (0) | 22 (0.6) | .087 |
| Wound infection | 67 (3.8) | 54 (4.0) | 20 (4.4) | 28 (12.6) | 169 (4.5) | |
| Hemorrhage | 44 (2.5) | 78 (5.8) | 7 (1.6) | 2 (0.9) | 131 (3.5) | <.0001 |
| Ileus | 25 (1.4) | 52 (3.8) | 12 (2.7) | 0 (0) | 89 (2.4) | <.0001 |
| Urinary tract infection | 25 (1.4) | 29 (2.1) | 18 (4.0) | 5 (2.2) | 77 (2.0) | <.0001 |
| Wound dehiscence | 30 (1.7) | 11 (0.8) | 5 (1.1) | 25 (11.2) | 71 (1.9) | .016 |
| Sepsis | 14 (0.8) | 16 (1.2) | 4 (0.9) | 3 (1.3) | 37 (1.0) | <.0001 |
| Thromboembolism | 12 (0.7) | 17 (1.3) | 0 (0) | 1 (0.4) | 30 (0.8) | .817 |
| Kidney Injury | 7 (0.4) | 17 (1.3) | 3 (0.7) | 1 (0.4) | 28 (0.7) | .095 |
| Other organ injury | 8 (0.5) | 10 (0.7) | 6 (1.3) | 1 (0.4) | 25 (0.7) | .092 |
| Anastomosis leak | 2 (0.1) | 4 (0.3) | 1 (0.2) | 1 (0.4) | 8 (0.2) | .337 |
| Cardiac arrest | 0 (0) | 8 (0.6) | 0 (0) | 0 (0) | 8 (0.2) | .764 |
| Myocardial infarction | 2 (0.1) | 1 (0.1) | 1 (0.2) | 0 (0) | 4 (0.1) | .006 |
| Stroke | 1 (0.1) | 2 (0.1) | 0 (0) | 0 (0) | 3 (0.1) | .915 |
| Other complications | 84 (4.8) | 97 (7.2) | 35 (7.8) | 20 (9.0) | 237 (6.3) | .836.007 |
| 30-d surgical mortality | 8 (0.5) | 20 (1.5) | 0 (0) | 2 (0.9) | 30 (0.8) | .003 |
Six patients (0.1%) did not have a recorded cancer site. Data presented as total number (percentage) or median (interquartile range).
Fotopoulou. Gynecologic cancer surgery during the COVID-19 pandemic. Am J Obstet Gynecol 2022.
Curative+life-prolonging vs palliative operation
Midabdominal=any operation involving mid-abdominal procedures, but not upper-abdominal surgery; Upper-abdominal=any operations involving upper-abdominal procedures.
Overall, 20.2% (279/1355) of ovarian cancer patients received neoadjuvant chemotherapy. Of those, 712/1355 (52.3%) had FIGO Stage III/IV disease. In this group, 253/712 (35.5%) had neoadjuvant chemotherapy, and 165/712 (23.2%) experienced a significant delay (>8 weeks) for their operations. In those who had FIGO Stage III/IV disease and experienced significant delays, 138/165 (83.6%) had neoadjuvant chemotherapy, compared with 115/547 (21.0%) for those who did not experience a delay (P<.0001). In those who had FIGO stage I/II disease and experienced significant delays (7.3%; 40/548), 10/40 (25.0%) had neoadjuvant chemotherapy compared with 15/508 (3.0%) for those who did not experience a delay (P<.0001).
Most areas of surgical resection were confined to the pelvis and/or perineum (2624/3784; 69%); 15% (562/3784) involved the midabdomen and 8.4% (319/3784) involved the upper abdomen. The overall bowel resection rate was 3.5% (133/3784). A minimally-invasive approach was applied in 35.5% of all patients (1342/3784) and in 55% (963/1751) and 33% (150/449) of uterine and cervical cancers, respectively.
The surgical 30-day morbidity and mortality profile of the surgical cohort is presented in Table 3. The overall complication rate was 19.3% (731/3784). The postoperatively confirmed COVID-19 infection rate was 0.6% (22/3784) in the entire surgical cohort. Patients with ovarian and uterine cancer represented 95% (21/22) of the entire COVID-19 infected group. Thirty (0.8%) patients died within 30 days of their operations.
Examining separately the surgical morbidity profile of the patients who acquired postoperative COVID-19 infections (Supplemental Table 4), significant differences were noted compared with the uninfected cohort, with a notable increase in respiratory complications (27.3% vs 1.4%; P<.0001), wound infection (18.2% vs 4.4%; P=.002), postoperative ileus (13.6% vs 2.3%; P<.0001), urinary tract infection (13.6% vs 2.0%; P<.0001), and anastomotic leak (for those who had bowel surgery, 1/4; 25% vs 7/129; 5.4%; P<.0001). The length of stay was significantly longer in the COVID-19-infected group (median of 8.5 days vs 4 days; P=.0001). The 30-day mortality rate was 18.2% (2/22) vs 0.7% (26/3762) in the COVID-19-infected and uninfected groups, respectively (P<.0001). Only 1 preoperative factor and 1 intraoperative factor were significantly associated with COVID-19 infection; they were WHO performance status (P=.003) and the rate of bowel resection (18.2% vs 3.4%; P<.0001). Multivariate modeling was not performed owing to the very low number of postoperative COVID-19 infections (n=22).
We also compared the patient characteristics and outcomes for those who had a prolonged hospital stay of ≥14 days. The cutoff is used for the continual National Health Service England audit that required mandatory data submission for every hospital in the United Kingdom. Those patients with poorer performance status and higher ASA score, higher disease stage, higher comorbidities index, having had an open surgery, respiratory complications, bowel surgery, and low COVID-19 burden had a higher risk of staying in the hospital longer than 14 days postoperatively (Supplemental Table 5).
When evaluating the impact of the COVID-19 pandemic on the type of treatment the patients received, we demonstrated that 20.7% (823/3973) of all patients (both operated and nonoperated) had their standard of care adjusted (Table 4 and Supplementary Table 3).
Table 4.
Summary of pandemic-related changes in care in operated patients by cancer type (n=3778)a
| Uterus (n=1751) | Ovary (n=1355) | Cervix (n=449) | Vulva/vagina (n=223) | Total (n=3778) | P value | |
|---|---|---|---|---|---|---|
| Any change in care | 332 (19.0) | 201 (14.8) | 58 (12.9) | 43 (19.3) | 634 (17.0) | .001 |
| Alternative hospitals | 215 (12.3) | 117 (8.6) | 42 (9.4) | 28 (12.6) | 402 (10.6) | .006 |
| Delay to definitive surgery | 198 (11.3) | 115 (8.5) | 34 (7.6) | 34 (15.3) | 381 (10.1) | .001 |
| Change of choice of operations | 77 (4.4) | 15 (1.1) | 7 (1.6) | 6 (2.7) | 105 (2.8) | <.0001 |
| Expedited surgery | 39 (2.2) | 31 (2.3) | 6 (1.3) | 4 (1.8) | 80 (2.1) | .631 |
| Non-routine use of neoadjuvant treatments | 18 (1.0) | 24 (1.8) | 0 (0) | 0 (0) | 42 (1.1) | .005 |
| Neoadjuvant treatments not given | 5 (0.3) | 4 (0.3) | 2 (0.5) | 0 (0) | 11 (0.3) | .796 |
| Longer neoadjuvant treatments | 1 (0.1) | 36 (2.7) | 0 (0) | 0 (0) | 37 (1.0) | <.0001 |
| Shorter neoadjuvant treatments | 2 (0.1) | 15 (1.1) | 0 (0) | 0 (0) | 17 (0.5) | <.0001 |
| Non-routine use of adjuvant treatments | 4 (0.2) | 3 (0.2) | 1 (0.2) | 0 (0) | 8 (0.2) | .918 |
| Adjuvant treatments not given | 14 (0.8) | 4 (0.3) | 4 (0.9) | 0 (0) | 22 (0.6) | .145 |
| Not recruited to a clinical trial | 3 (0.2) | 1 (0.1) | 1 (0.2) | 0 (0) | 5 (0.1) | .771 |
| Recruited to a clinical trial (not routine) | 2 (0.1) | 0 (0) | 0 (0) | 0 (0) | 2 (0.1) | .509 |
Data presented as total number (percentage). Multiple changes were reported for each patient when appropriate.
Fotopoulou. Gynecologic cancer surgery during the COVID-19 pandemic. Am J Obstet Gynecol 2022.
Six patients (0.1%) did not have a recorded cancer site and were excluded from this table.
Patients in LMICs (76/326; 23.3%; P<.0001) and areas under full lockdown (P<.0001) had poorer performance status (P<.0001), more comorbidities (P=.024), higher ASA grade (P=.010), ovarian cancer (213/1355, 15.7%; P<.0001) and FIGO stage 3 or 4 diseases (198/1060, 18.7%; P<.0001) were more likely to have their operations more than 8 weeks after the initial decision (Table 5 ).
Table 5.
Comparisons of patients and outcomes who have received any operations by time to surgery (≤8 weeks vs >8 weeks; n=3784)
| ≤8 wk (n=3360) | >8 wk (n=424) | Proportion >8 wk | P value | |
|---|---|---|---|---|
| Age (y) | ||||
| 17–19 | 12 (0.4) | 1 (0.2) | 1/13 (7.7) | .165 |
| 20–29 | 84 (2.5) | 10 (2.4) | 10/94 (10.6) | |
| 30–39 | 259 (7.7) | 29 (6.8) | 29/288 (10.1) | |
| 40–49 | 507 (15.1) | 77 (18.2) | 77/584 (13.2) | |
| 50–59 | 853 (25.4) | 113 (26.7) | 113/966 (11.7) | |
| 60–69 | 882 (26.3) | 96 (22.6) | 96/978 (9.8) | |
| 70–79 | 603 (18.0) | 68 (16.0) | 68/671 (10.1) | |
| 80–89 | 156 (4.6) | 28 (6.6) | 28/184 (15.2) | |
| >90 | 4 (0.1) | 2 (0.5) | 2/6 (33.3) | |
| Income group | ||||
| High | 2501 (74.4) | 273 (64.4) | 273/2774 (9.8) | <.0001 |
| Upper middle | 609 (18.1) | 75 (17.7) | 75/684 (11.0) | |
| Low-middle | 250 (7.4) | 76 (17.9) | 76/326 (23.3) | |
| BMI (kg/m2) | ||||
| <18.5 | 91 (2.7) | 18 (4.3) | 18/109 (16.5) | .364 |
| 18.5–24.9 | 1260 (37.5) | 163 (38.4) | 163/1423 (11.5) | |
| 25–29.9 | 995 (29.6) | 117 (27.6) | 117/1112 (10.5) | |
| 30–34.9 | 549 (16.3) | 59 (13.9) | 59/608 (9.7) | |
| 35–39.9 | 250 (7.4) | 34 (8.0) | 34/284 (12.0) | |
| ≥40 | 190 (5.7) | 30 (7.1) | 30/220 (13.6) | |
| Not available | 25 (0.7) | 3 (0.7) | 3/28 (10.7) | |
| WHO performance status | ||||
| 0 | 2152 (64.0) | 219 (51.7) | 219/2371 (9.2) | <.0001 |
| 1 | 858 (25.5) | 158 (37.3) | 158/1016 (15.6) | |
| 2 | 189 (5.6) | 36 (8.5) | 36/225 (16.0) | |
| 3 | 29 (0.9) | 4 (0.9) | 4/33 (12.1) | |
| 4 | 4 (0.1) | 0 (0) | 0/4 (0) | |
| Not available | 128 (3.8) | 7 (1.7) | 7/135 (5.2) | |
| CCI | ||||
| 0 | 791 (23.5) | 105 (24.8) | 105/896 (11.7) | .024 |
| 1 | 740 (22.0) | 103 (24.3) | 103/843 (12.2) | |
| 2 | 789 (23.5) | 82 (19.3) | 82/871 (9.4) | |
| 3 | 617 (18.4) | 62 (14.6) | 62/679 (9.1) | |
| 4 | 266 (7.9) | 45 (10.6) | 45/311 (14.5) | |
| 5 | 100 (3.0) | 20 (4.7) | 20/120 (16.7) | |
| 6 | 37 (1.1) | 4 (0.9) | 4/41 (9.8) | |
| 7 | 13 (0.4) | 0 (0) | 0/13 (0) | |
| 8 | 5 (0.2) | 2 (0.5) | 2/7 (28.6) | |
| 9 | 2 (0.1) | 1 (0.2) | 1/3 (33.3) | |
| ASA grade | ||||
| 1 | 917 (27.3) | 95 (22.4) | 95/1012 (9.4) | .010 |
| 2 | 1834 (54.6) | 220 (51.9) | 220/2054 (10.7) | |
| 3 | 582 (17.3) | 106 (25.0) | 106/688 (15.4) | |
| 4 | 21 (0.6) | 3 (0.7) | 3/23 (12.5) | |
| 5 | 4 (0.1) | 0 (0) | 0/4 (0) | |
| Not available | 2 (0.1) | 0 (0) | 0/2 (0) | |
| Cancer site | ||||
| Uterus | 1605 (47.8) | 146 (34.4) | 146/1751 (8.3) | <.0001 |
| Ovary | 1142 (34.0) | 213 (50.2) | 213/1355 (15.7) | |
| Cervix | 405 (12.1) | 44 (10.4) | 44/449 (9.8) | |
| Vagina/vulva | 202 (6.0) | 21 (5.0) | 21/223 (9.4) | |
| Not available | 6 (0.2) | 0 (0) | 0/6 (0) | |
| FIGO stage | ||||
| Not cancer | 179 (5.3) | 33 (7.8) | 33/212 (15.6) | <.0001 |
| 1 or 2 | 2262 (67.3) | 191 (45.1) | 191/2453 (7.8) | |
| 3 or 4 | 862 (25.7) | 198 (46.7) | 198/1060 (18.7) | |
| Not available | 57 (1.7) | 2 (0.5) | 2/59 (3.4) | |
| Lockdown stringency | ||||
| Full | 1577 (46.9) | 340 (80.2) | 340/1917 (17.7) | <.0001 |
| Moderate | 853 (25.4) | 51 (12.0) | 51/904 (5.6) | |
| Light | 839 (25.0) | 22 (5.2) | 22/861 (2.6) | |
| COVID-19 burden | ||||
| High burden | 2376 (70.7) | 283 (66.8) | 283/2659 (10.6) | .240 |
| Low burden | 917 (27.3) | 131 (30.9) | 131/1048 (12.5) | |
| Not available | 67 (2.0) | 10 (2.4) | 10/77 (13.0) | |
| Surgery performed | ||||
| Pelvis/perineal | 2366 (70.4) | 258 (60.9) | 258/2624 (9.8) | <.0001 |
| Midabdominal | 451 (13.4) | 111 (26.2) | 111/562 (19.8) | |
| Upper-abdominal | 291 (8.7) | 28 (6.6) | 28/319 (8.8) | |
| Others | 252 (7.5) | 27 (6.4) | 27/279 (9.7) | |
| Bowel surgery | ||||
| No | 3251 (96.8) | 400 (94.3) | 400/3651 (11.0) | .011 |
| Yes | 109 (3.2) | 24 (5.7) | 24/133 (18.1) | |
| Approach | ||||
| Open | 2042 (60.8) | 311 (73.4) | 311/2353 (13.2) | <.0001 |
| Minimally-invasive | 1235 (36.8) | 107 (25.2) | 107/1342 (8.0) | |
| Converted | 78 (2.3) | 6 (1.4) | 6/84 (7.1) | |
| Not available | 5 (0.2) | 0 (0) | 0/5 (0) | |
| Postoperative complication | ||||
| Any complications | 640 (19.1) | 91 (21.5) | 91/731 (12.5) | .235 |
| Respiratory complications | 51 (1.5) | 7 (1.7) | 7/58 (12.1) | .834 |
| Mortality | 26 (0.8) | 4 (0.9) | 4/30 (13.3) | .711 |
| Compositea | 601 (17.9) | 95 (22.4) | 95/696 (13.7) | .024 |
Data presented as total number (percentage) or proportion (percentage). For postoperative outcomes, data were collected at 30 days after the surgeries.
ASA grade, American Society of Anaesthesiologists Physical Status Classification system; BMI, body mass index; CCI, Charlson Comorbidity Index; FIGO, International Federation of Gynaecology and Obstetrics; WHO, World Health Organization.
Fotopoulou. Gynecologic cancer surgery during the COVID-19 pandemic. Am J Obstet Gynecol 2022.
A composite outcome of unresectable disease or disease progression, emergency surgery and death.
In those who had an operation more than 8 weeks after the initial decision, the operations were more likely to be open surgery (P<.0001), involve midabdominal surgery (P<.0001), and require bowel resections (P=.011).
There was no significant difference in 30-day mortality (26/3360; 0.8% vs 4/424; 0.9%, P=0.771) in those who had delayed operations. However, a significance difference was observed for the composite of adverse outcomes owing to delay in operations, which included unresectable disease or disease progression, emergency surgery, and death (95/424; 22.4% vs 601/3360; 17.9%, P=.024), compared with those who had operations within 8 weeks of their MDT decisions.
In nonoperated patients (Supplementary Table 3) (189/2430; 7.9%), 1 in 20 (5/189; 2.7%) died within 3 months of MDT decision for surgery, and 1 in 5 (34/189; 18%) experienced disease progression and death.
Comment
Principal findings
This was a large prospective international study (with 1 in 4 participants from LMICs) to evaluate the impact of the COVID-19 crisis on the treatment delivery and outcomes of gynecologic cancer patients initially had plans for nonpalliative cancer surgery during the initial months of the pandemic. We demonstrated that 1 in 5 surgical gynecologic cancer patients had their standard of care adjusted as a result of the COVID-19 pandemic.
Although treatment alterations were not associated with a significant difference in 30-day postoperative mortality, significant delay (>8 weeks) in the time to surgery was associated with a composite of adverse outcomes (Table 5), including disease progression and death compared with those who did not experience a delay. In those in whom operation was cancelled, 1 in 5 had disease progression, and 1 in 20 died within 3 months of their MDT decisions.
Results in the context of what is known
Our results suggest that the surgical morbidity profile appeared to be equivalent to the historic surgical morbidity data outside of the COVID-19 pandemic18, 19, 20 in contrast to previous single-center data, suggesting higher morbidity rates.11 It is plausible that the modifications of surgical approaches have influenced the overall morbidity profile during the pandemic. For example, in patients undergoing colorectal cancer surgery,14 there was a significant increase in the overall rate of stoma formation (34.2% vs 27.2% in the prepandemic era), especially end stoma formation (70% vs 43.6% prepandemic).
Despite this study being conducted during the first wave of the COVID-19 pandemic, a low perioperative COVID-19 infection rate (0.6%) was observed. Our data appeared more favorable than the previously reported experience,13 , 14 , 21 with a lower incidence of postoperative COVID-19 infection (0.6% vs 3.8%) and lower 30-day mortality in the non-COVID19-infected patients’ cohort (0.7% vs 1.8%). Consistent with previous reports,13 , 14 , 21 patients infected with COVID-19 had a significantly longer postoperative stay and higher surgical morbidity and mortality (63.6% and 18.2%, respectively) than uninfected patients. The cause of the more favorable outcomes in patients with gynecologic cancer than previously reported experiences is likely to be multifactorial and could be related to the overall less radical surgical procedures. Only 3.5% of our operated patients underwent bowel resections, which is a surrogate marker of surgical radicality. Nevertheless, similar to previous reports,14 our data also confirmed that bowel resection was associated with higher risks of perioperative COVID-19 infection, other surgical morbidity, and longer hospitalization. These data consistently demonstrated the significant difference in surgical mortality between COVID-19-infected and uninfected patients, regardless of the type and site of surgery.
In addition to the well-established risk factor of prolonged hospital stay, we showed that low COVID-19 burden areas were associated with significantly higher rates of increased hospitalization (>14 days). It is possible that the healthcare systems that were least affected by the pandemic continued to operate for complex patients with a high disease burden, who in turn required a longer hospital stay.
Although published recommendations highlighted expected delays in gynecologic cancer delivery, the published evidence demonstrated some variations of the impact of COVID-19. For example, Bruce et al22 suggested that the number of referrals to gynecologic oncology decreased during the early stages of the pandemic, but the time to evaluation and treatment initiation were unaffected. In contrast, a number of surveys and retrospective cohort studies have described delays in consultations and treatments.23, 24, 25, 26 This study specifically evaluated the impact of the significant delay in the time to surgery on oncologic outcomes in patients with gynecologic cancers. One in 10 patients experienced significant delay (>8 weeks) to surgery (Table 5), particularly patients with ovarian cancer (213/1355; 15.7%), multiple comorbidities, stage III/IV disease (198/1060; 18.7%), and those in LMICs (76/326; 23.3%). A significant delay in time to surgery was associated with neoadjuvant chemotherapy use in patients with ovarian cancer (83.6% vs 21% for FIGO Stage III/IV disease; 25% vs 3.0% for FIGO stage I/II disease). The results highlighted this delay disproportionately affect those who required more complex surgery, at higher anesthetic risks and in areas where resources were scarce (LMICs and areas in full lockdown with subsequently low COVID-19 burden). Consistent with a previous systematic review,10 treatment delay was associated with poorer outcomes.
Strengths and limitations
This work evaluated the outcomes of the largest cohort of surgical gynecologic cancer patients during the COVID-19 pandemic. Our data covered all regions of the world to minimize geographic bias and generate conclusions that could be applied to different healthcare systems. It delivered a global view on cancer surgery delivery and outcomes—an area where comprehensive prospective data are scarce. Similar to other large-scale international datasets, this study includes heterogeneity between the cohorts; bias toward high-income countries; and significant variations in the surgical practice, pathways, and infrastructures; which made direct translation to practice for individual patients challenging.
There are very limited existing multicentered international studies with similar coverage of LMICs reporting detailed outcomes and complication rates of gynecologic cancer surgery.18, 19, 20 However, they had different classifications and recording methods compared with this current study. Therefore, direct comparison was inappropriate, which limited our ability to identify any change in the morbidity and mortality rates because of the COVID-19 pandemic.
The study and follow-up periods for CovidSurg-Cancer were deliberately short to encourage wider participations and a rapid turnover of data to inform practice. Although the comparison of a retrospective cohort could aid direct comparison of management adjustments and outcomes and it would have been performed in a single-center setting,11 the resources required to do so globally at the first peak of the pandemic could not be justified. We also acknowledge that post-MDT patient selections have contributed to the associations between surgical delay or cancellation and poorer outcomes, but the results highlight the need to target resources for those with complex care needs to ensure that they receive their planned urgent life-prolonging operations.
Clinical implications
Gynecologic cancer surgery during the early stages of the COVID-19 pandemic and before the availability of vaccination and effective treatments appeared to be safe, with a low risk of COVID-19 infection.14 With significant contribution from LMICs (26.9%; 1067/3973), these data also provide a global snapshot of the morbidity and mortality rates experienced by patients undergoing gynecologic cancer surgery. This study identified that a significant proportion of patients had their surgical plans delayed or cancelled, which was associated with poorer outcomes. The results represent an early and clear signal that robust mechanisms and pathways are urgently needed to ensure adequate cancer care even in times of crisis without detrimental oncologic compromise. With this large data set estimating the number of treatment plan alternations globally, the results could be used to coordinate plans and allocate resources as required to rescue and salvage the detrimental effects. Yet, few health systems have established consensus agreements to date.1 , 8 These results will also add to the evidence for future pandemics and the planning of relevant studies during a worldwide crisis in the future.
Research implications
The data were collected during the initial phase of the pandemic when the impingement of the virus was completely new, when none of the patients were vaccinated, and when protective measures were immature. Continued evaluation of the impact of the COVID-19 pandemic on cancer care delivery in the medium- and long-term is required. Population-based studies will be required to evaluate which patient subgroups (eg, cancer types or stage) were the most adversely affected. Comparative studies are also required to identify effective ways to mitigate the detrimental impact of the pandemic on cancer care.
Conclusions
The new rising incidence of COVID-19 worldwide owing to emerging variants combined with incomplete vaccination coverage has continued to disrupt healthcare delivery, and our results remain highly relevant. Despite the very low risk of perioperative COVID-19 infection, those infected had substantially poorer outcomes. The high rates of pandemic-related treatment plan modifications were associated with early negative impact on oncological outcomes. Robust strategies for the safe provision of surgical cancer care when the pandemic is transitioning into an endemic state are urgently needed.
Acknowledgments
We thank all contributing centers for their work on this study and for delivery care during the pandemic.
Footnotes
Additional members of the COVIDSurg Gynecological Cancer Collaborators have been listed in the Appendix.
E.L. and S.S. share senior authorship.
The authors report no conflict of interest.
The British Gynaecological Cancer Society supported this study with a small grant. N.A.R. is funded through the National Institutes of Health/National Cancer Institute Cancer Centre Support Grant P30 CA008748. The funders played no role in the design or interpretation of this study.
Cite this article as: Fotopoulou C, Khan T, Bracinik J, et al. Outcomes of gynecologic cancer surgery during the COVID-19 pandemic: an international, multicenter, prospective CovidSurg-Gynecologic Oncology Cancer study. Am J Obstet Gynecol 2022;227:735.e1-25.
Contributor Information
CovidSurg Gynecological Cancer Collaborators:
Dmitri Nepogodiev, Kwabena Siaw-Acheampong, Ruth A. Benson, Edward Bywater, Daoud Chaudhry, Brett E. Dawson, Jonathan P. Evans, James C. Glasbey, Rohan R. Gujjuri, Emily Heritage, Conor S. Jones, Sivesh K. Kamarajah, Chetan Khatri, Rachel A. Khaw, James M. Keatley, Andrew Knight, Samuel Lawday, Elizabeth Li, Harvinder S. Mann, Ella J. Marson, Kenneth A. McLean, Siobhan C. Mckay, Emily C. Mills, Gianluca Pellino, Maria Picciochi, Elliott H. Taylor, Abhinav Tiwari, Joana FF. Simoes, Isobel M. Trout, Mary L. Venn, Richard JW. Wilkin, Aneel Bhangu, Joana FF. Simoes, Tom EF. Abbott, Sadi Abukhalaf, Michel Adamina, Adesoji O. Ademuyiwa, Arnav Agarwal, Murat Akkulak, Ehab Alameer, Derek Alderson, Felix Alakaloko, Markus Albertsmeier, Osaid Alser, Muhammad Alshaar, Sattar Alshryda, Alexis P. Arnaud, Knut Magne Augestad, Faris Ayasra, José Azevedo, Brittany K. Bankhead-Kendall, Emma Barlow, David Beard, Ruth A. Benson, Ruth Blanco-Colino, Amanpreet Brar, Ana Minaya-Bravo, Kerry A. Breen, Chris Bretherton, Igor Lima Buarque, Joshua Burke, Edward J. Caruana, Mohammad Chaar, Sohini Chakrabortee, Peter Christensen, Daniel Cox, Moises Cukier, Miguel F. Cunha, Giana H. Davidson, Anant Desai, Salomone Di Saverio, Thomas M. Drake, John G. Edwards, Muhammed Elhadi, Sameh Emile, Shebani Farik, Marco Fiore, J Edward Fitzgerald, Samuel Ford, Tatiana Garmanova, Gaetano Gallo, Dhruva Ghosh, Gustavo Mendonça Ataíde Gomes, Gustavo Grecinos, Ewen A. Griffiths, Magdalena Gruendl, Constantine Halkias, Ewen M. Harrison, Intisar Hisham, Peter J. Hutchinson, Shelley Hwang, Arda Isik, Michael D. Jenkinson, Pascal Jonker, Haytham MA Kaafarani, Debby Keller, Angelos Kolias, Schelto Kruijff, Ismail Lawani, Hans Lederhuber, Sezai Leventoglu, Andrey Litvin, Andrew Loehrer, Markus W. Löffler, Maria Aguilera Lorena, Maria Marta Modolo, Piotr Major, Janet Martin, Hassan N. Mashbari, Dennis Mazingi, Symeon Metallidis, Ana Minaya-Bravo, Helen M. Mohan, Rachel Moore, David Moszkowicz, Susan Moug, Joshua S. Ng-Kamstra, Mayaba Maimbo, Ionut Negoi, Milagros Niquen, Faustin Ntirenganya, Maricarmen Olivos, Kacimi Oussama, Oumaima Outani, Marie Dione Parreno-Sacdalanm, Francesco Pata, Carlos Jose Perez Rivera, Thomas D. Pinkney, Willemijn van der Plas, Peter Pockney, Ahmad Qureshi, Dejan Radenkovic, Antonio Ramos-De la Medina, Toby Richards, Keith Roberts, April C. Roslani, Martin Rutegård, Juan José Segura-Sampedro, Irène Santos, Sohei Satoi, Raza Sayyed, Andrew Schache, Andreas A. Schnitzbauer, Justina O. Seyi-Olajide, Neil Sharma, Catherine A. Shaw, Richard Shaw, Sebastian Shu, Kjetil Soreide, Antonino Spinelli, Grant D. Stewart, Malin Sund, Sudha Sundar, Stephen Tabiri, Philip Townend, Georgios Tsoulfas, Gabrielle H. van Ramshorst, Raghavan Vidya, Dale Vimalachandran, Oliver J. Warren, Duane Wedderburn, Naomi Wright, Lesley Booth, Neil Barker, Shirley Cooke, Suzanne Doré, Nigel Horwood, Emmy Runigamugabo, Carrie Tierney Weir, Albania: Dajti I, Allemand C, Boccalatte LA, Figari M, Lamm M, Larrañaga J, Marchitelli C, Noll F, Odetto D, Perrotta M, Saadi J, Zamora L, A.M. Ballester, Tapper KE, Zeff N, Valenzuela JI, Alurralde C, Anastasio J, Apas Perez de Nucci A, Caram EL, Eskinazi D, Mendoza JP, Usandivaras M, Badra R, Esteban A, García JS, García PM, Gerchunoff JI, S.M. Lucchini, M.A. NIgra, Vargas L, Hovhannisyan T, Stepanyan A, Vasey CE, Watson EGR, Ip C, Kealey J, Lim CSH, Sengupta S, Ward S, Wong E, Gould T, Gourlay R, Griffiths B, Gananadha S, McLaren M, Cecire J, Joshi N, Salindera S, Sutherland A, Ahn JH, Charlton G, Chen S, Gauri N, Hayhurst R, Jang S, Jia F, Mulligan C, Yang W, Ye G, Zhang H, Ballal M, Gibson D, Hayne D, McMillan H, Moss J, Pugliese MJ, Richards T, Seow YTN, Thian A, Viswambaram P, Vo UG, Bennetts J, Bright T, M. Brooke-Smith, Fong R, Gricks B, Huang L, Lam YH, Nathan A, B.S. Ong, Ooi E, Szpytma M, Watson D, Bagraith K, Caird S, Chan E, Dawson C, Ho D, Hui N, Izwan S, Jeyarajan E, Jordan S, Liang R, Lim A, Nolan GJ, Oar A, Parker D, Puhalla H, Quennell A, Rutherford L, Sommerville C, Townend P, Von Papen M, Wullschleger M, Dawson AC, Drane A, Blatt A, Cope D, Egoroff N, Fenton M, Gani J, Lott N, Pockney P, Shugg N, Elliott M, Phung D, Phan D, Townend D, Bong C, Gundara J, Frankel A, Bowman S, Guerra GR, Gerns N, McGeorge S, Riddell A, Roberts M, Rukin N, Bolt J, Buddingh K, N.N. Dudi-Venkata, Jog S, Kroon HM, Sammour T, Smith R, Stranz C, Batstone M, Lah K, McGahan W, Mitchell D, Morton A, Pearce A, Roberts M, Sheahan G, Swinson B, Waldron A, Walker P, Alam N, Banting S, Chong L, Choong P, Clatworthy S, Foley D, Fox A, Hii MW, Knowles B, Mack J, Read M, Rowcroft A, Ward S, Wright G, Dawson AC, Drane A, Lun EWY, Lanner M, Burtscher J, F. Trivik-Barrientos, Königsrainer I, Bauer M, Freyschlag C, Kafka M, Messner F, Öfner D, Tsibulak I, Holawe S, Zimmermann M, Emmanuel K, Grechenig M, Gruber R, Harald M, Öhlberger L, Presl J, Wimmer A, Namazov İ, Samadov E, Barker D, Boyce R, Corbin S, Doyle A, Eastmond A, Gill R, Haynes A, Millar S, O’Shea M, Padmore G, Paquette N, Phillips E, St. John S, Walkes K, Abeloos J, De Backer T, De Ceulaer J, Dick C, A. Diez-Fraile, Lamoral P, Spaas C, Ceelen W, Pattyn P, Van de putte D, Van Nieuwenhove Y, Van Ramshorst G, W. Willaert, L. Bazzett-Matabele, Chiyapo SP, D. Ramogola-Masire, Ramontshonyana G, Seiphetlheng A, Vuylsteke P, Abdallah EA, Aguiar Júnior S, Baiocchi G, Carvalho GB, Coimbra FJF, Kowalski LP, Makdissi F, Marques N, Marques T, Soares Dos Santos S, Tirapelli Gonçalves B, Vartanian JG, Dos Reis R, Camara P, De Lima RK, Della Giustina E, Hoffmann PV, Gatti A, Nardi C, Oliva R, Nacif L, Carvalho Ferro C, Gomes Mendonça Ataíde G, Lima Buarque I, Lira dos Santos Leite A, L. Pol-Fachin, Santos Bezerra T, Maylson Ramos da Silva A, Windson de Araújo Silvestre D, Vieira Barros A, Campbell L, De Cicco R, Cecconello I, Gregorio P, Pontual Lima L, Ribeiro Junior U, Takeda FR, Terra RM, Faccini Teixeira M, Kowalski LP, M.A.V. Kulcsar, Matos LL, Nunes KS, Laporte G, Salem M, Barakat Awada J, Ijichi TR, Kim NJ, Marreiro A, Muller B, Nunes R, Bodanese B, Eidt ER, Isoton JC, Lemos Vieira da Cunha M, Regina de Sampaio L, Vendrame C, Zeni M, Zortéa JA, Zortéa MR, Sokolov M, Kidane B, Srinathan S, Munro A, Helyer L, McKeen D, Boutros M, Caminsky NG, Ghitulescu G, Jamjoum G, Moon J, Pelletier J, Vanounou T, Wong S, Cheng D, MacNeil SD, Martin J, Boutros M, Dumitra S, Kouyoumdjian A, Schmid S, Spicer J, Agarwal A, Brar A, Dada J, Dare A, Hameed U, Osman F, Johnston B, Russell C, Groot G, Persad A, Pham H, Wood M, Brar A, Ko M, Rajendran L, Boutros M, Demyttenaere S, Garfinkle R, Brown C, Karimuddin A, Lee N, Liu J, Madani Kia T, P.T. Phang, Raval M, Tom K, J. Abou-Khalil, Martel A, Nessim C, Stevenson J, Al Riyami S, Bali K, Bigam D, Dajani K, Dell A, Modolo MM, Ramirez Nieto P, Sepulveda R, Molero A, Bolbaran A, Ruiz I, Heredia F, Bellolio F, Besser N, Grasset E, Guaman JO, Inzunza M, Irarrázaval MJ, Jarry C, Quintana Martinic M, Riquoir Altamirano C, Romero Manqui CA, Ruiz Esquide M, Vargas Añazco C, Almeciga A, Fletcher A, Merchan A, Merchan A, Quijano T, Sanabria D, F. Arias-Amézquita, Cétares C, Cortes Murgueitio N, J.L. Gomez-Mayorga, G. Herrera-Almario, Rodriguez J, Sanabria D, Iglesias P, Puentes LO, Calvache JA, C.M. Orozco-Chamorro, Rojas DA, A. Sánchez-Gómez, Abadia M, Acosta J, Almeciga A, Angel Aristizabal J, Bonilla A, Caicedo L, Calderon Quiroz PH, Cervera Bonilla S, Diaz S, Facundo H, Garcia Mora M, Guevara O, Guzman L, Herrera Mora DR, Jimenez Ramirez LJ, Lehmann C, Manrique E, Mariño I, Medina M, Pinilla Morales RE, Puerto A, Puerto Horta J, Quintero M, Rey Ferro M, Rodriguez J, Saénz A, Santana D, Serrano W, Suescun O, Trujillo Sanchez LM, Velasquez Cuasquen BG, Mendoza Quevedo J , Bogota, Bačić G, Karlović D, Kršul D, Zelić M, Luksic I, Mamic M, Bacic I, Bakmaz B, Ćoza I, Dijan E, Katusic Z, Mihanovic J, Morović D, Rakvin I, Almezghwi H, Arslan K, Besim H, Özant A, Özçay N, Frantzeskou K, Gouvas N, Kokkinos G, Papatheodorou P, Pozotou I, Stavrinidou O, Yiallourou A, Martinek L, Skrovina M, Straka M, Szubota I, Peteja M, Žatecký J, Javurkova V, Klat J, Antony S, Avlund T, Berg KD, Borre M, Christensen P, Elkjær MC, Ernst A, Fensman SK, Haldrup M, Harbjerg JL, Iversen LH, P.T. Jensen, Jeppesen TD, Kjaer DW, Kristensen HØ, Lund N, Maigaard Axelsen S, Mekhael M, Mikic N, Ostenfeld EB, Ebbehøj AL, Krarup P, Schlesinger N, Smith H, Batista S, Crespo A, Díaz PJ, Rivas R, J. Rodriguez-Abreu, Tactuk N, El Kassas M, Omar W, Tawheed A, Talaat M, Abdelsamed A, Azzam AY, Salem H, Seleim A, Abdelmajeed A, Abdou M, Abosamak NE, A.L. Sayed M, Ashoush F, Atta R, Elazzazy E, Elnemr M, Elsayed Hewalla ME, Elsherbini I, Essam E, Ewedah M, Ghallab I, Hassan E, Ibrahim M, Metwalli M, Mourad M, M.S. Qatora, Ragab M, Sabry A, Saifeldin H, Samih A, Samir Abdelaal A, Shehata S, Shenit K, Attia D, Kamal N, Osman N, A.M. Abbas, Abd Elazeem HAS, A.Y. Abd-Elkariem, Abdelkarem MM, Alaa S, Ashraf M, Ayman A, Azizeldine MG, Elkhayat H, Emad Mashhour A, Gaber M, Hamza HM, Hawal I, Hetta HF, K. Ali A, M.elghazaly S, Mohammed MM, Monib FA, M.A. Nageh, Saad A, Saad MM, Shahine M, Yousof EA, Youssef A, M. El-Deeb, Fawzy M, Ghaly G, Ibraheem M, Eldaly A, Esmail E, ElFiky M, Nabil A, Alrahawy M, Sakr A, Soliman H, Soltan H, Amira G, Sallam I, Sherief M, Sherif A, Abdelrahman A, Aboulkassem H, Ghaly G, Hamdy R, Morsi A, Salem H, Sherif G, Abdeldayem H, Abdelkader Salama I, Balabel M, Fayed Y, Sherif AE, Elmorsi R, Emile S, Refky B, Abd-elsalam S, Badr H, Elbahnasawy M, Elzoghby M, Essa M, Gamal Badr S, Ghoneim A, Hamad O, Hamada M, Hammad M, Hawila A, M.S. Morsy, Salman S, Sarsik S, Bekele K, Kauppila JH, Sarjanoja E, Helminen O, Huhta H, Kauppila JH, Beyrne C, Jouffret L, Lugans L, L. Marie-Macron, Chouillard E, De Simone B, Fredon F, Roux A, Bettoni J, Dakpé S, Devauchelle B, Lavagen N, Testelin S, Boucher S, Breheret R, Gueutier A, Kahn A, J. Kün-Darbois, Barrabe A, Lakkis Z, Louvrier A, Manfredelli S, Mathieu P, Chebaro A, Drubay V, El amrani M, Eveno C, Lecolle K, Legault G, Martin L, Piessen G, Pruvot FR, Truant S, Zerbib P, Ballouhey Q, Barrat B, Fourcade L, Laloze J, Salle H, Taibi A, Tricard J, Usseglio J, Bergeat D, Merdrignac A, Le Roy B, Perotto LO, Scalabre A, Gornes H, Vaysse C, Vergriete K, Aimé A, Ezanno A, Malgras B, Arnaud AP, Fustec E, Lavoue V, Tesson C, Bouche P, Tzedakis S, Cotte E, Glehen O, Lifante J, Bendjemar L, Braham H, Charre L, El Arbi N, Morel-chevillet L, Police A, Villefranque V, Volpin E, D’Urso A, Felli E, Mutter D, Pessaux P, Seeliger B, Barbé Y, Bardet J, Barret E, Berry R, Boddaert G, Bonnet S, Brian E, Cathala N, Cathelineau X, Denet C, Fuks D, Gossot D, Grigoroiu M, Laforest A, Y. Levy-Zauberman, C. Louis-Sylvestre, Macek P, Mombet A, Moumen A, Pourcher G, Rozet F, Sanchez Salas R, Seguin-givelet A, Tribillon E, Crenn V, De Vergie S, Duchalais E, Espitalier F, Ferron C, Fragnaud H, Malard O, Regenet N, Rigaud J, Varenne Y, Waast D, Bork U, Distler M, Fritzmann J, Kirchberg J, Praetorius C, Riediger C, Weitz J, Welsch T, Wimberger P, Beyer K, Kamphues C, Lauscher J, Loch FN, Schineis C, Albertsmeier M, Angele M, Kappenberger A, Niess H, Schiergens T, Werner J, Becker R, Jonescheit J, Doerner J, Seiberth R, Pergolini I, Reim D, Herzberg J, Honarpisheh H, Strate T, Boeker C, Hakami I, Mall J, Liokatis P, Smolka W, Vassos N, Mannheim, Nowak K, Reinhard T, Hölzle F, Modabber A, Winnand P, Anthuber M, Shiban E, Sommer B, Sommer F, Wolf S, Howaldt H, Knitschke M, Kauffmann P, Wolfer S, Kleeff J, Lorenz K, Michalski C, Ronellenfitsch U, Schneider R. Saale, Bertolani E, Königsrainer A, Löffler MW, Quante M, Steidle C, Überrück L, Yurttas C, Betz CS, Bewarder J, Böttcher A, Burg S, Busch C, Dreimann M, Frosch KH, Gosau M, Heuer A, Izbicki J, Klatte TO, Koenig D, Moeckelmann N, Nitschke C, Perez D, Priemel M, Reiter A, Smeets R, Speth U, Stangenberg M, Thole S, Uzunoglu FG, Viezens L, Vollkommer T, Zeller N, Battista MJ, Gillen K, Hasenburg A, Krajnak S, Linz VC, Schwab R, K. Amo-Antwi, Appiah-kubi A, Konney T, Tawiah A, Boatey S, Issaka A, M.A. Korsah, Sheriff M, Angelou K, Haidopoulos D, Rodolakis A, Antonakis P, Bramis K, Chardalias L, Contis I, Dafnios N, Dellaportas D, Fragulidis G, Gklavas A, Konstadoulakis M, Memos N, Papaconstantinou I, Polydorou A, Theodosopoulos T, Vezakis A, Antonopoulou MI, Manatakis DK, Tasis N, Arkadopoulos N, Danias N, Economopoulou P, Frountzas M, Kokoropoulos P, Larentzakis A, Michalopoulos N, Nastos C, Parasyris S, Pikoulis E, Selmani J, Sidiropoulos T, Vassiliu P, Bouchagier K, Klimopoulos S, Paspaliari D, Stylianidis G, Akrivou D, Baxevanidou K, Bouliaris K, Chatzikomnitsa P, Delinasios G, Doudakmanis C, Efthimiou M, Giaglaras A, Kalfountzos C, Kolla C, Koukoulis G, Zervas K, Zourntou S, Baloyiannis I, Diamantis A, Gkrinia E, Hajiioannou J, Korais C, Koukoura O, Perivoliotis K, Saratziotis A, Skoulakis C, Symeonidis D, Tepetes K, Tzovaras G, Zacharoulis D, Alexoudi V, Antoniades K, Astreidis I, Christidis P, Deligiannidis D, Grivas T, Ioannidis O, Kalaitsidou I, Loutzidou L, Mantevas A, Michailidou D, Nikolaidou E, Papadopoulou S, Paraskevopoulos K, Politis S, Stavroglou A, Tatsis D, Tilaveridis I, Vahtsevanos K, Venetis G, Karaitianos I, Tsirlis T, Dinas K, C. Margioula-Siarkou, Petousis S, Baili E, Charalabopoulos A, Liakakos T, Schizas D, Spartalis E, Syllaios A, Zografos C, Anthoulakis C, C.D. Christou, Papadopoulos V, Tooulias A, Tsolakidis D, Tsoulfas G, Zouzoulas D, Athanasakis E, Chrysos E, Tsiaoussis I, Xenaki S, Xynos E, Barrios Duarte A, Lopez Muralles I, Lowey MJ, Portilla AL, Recinos G, Chan JYK, S.M. Chan, Chong CCN, Futaba K, M.F. Ho, Hon SF, Lau RWH, Mak TWC, Ng CF, Ng CSH, Ng KKC, Ng SSM, Teoh AYB, Teoh JY, Foo CC, Banky B, Suszták N, Misra S, Pareek P, Vishnoi JR, Ambre S, Balasubiramaniyan V, Chappity P, Chaudhary I, Colney L, Das MK, Imaduddin M, Jain A, Jena SK, Kar M, Mandal S, Mishra A, Mishra SS, Mishra TS, Mitra JK, Mittal Y, Muduly DK, Nayak P, Parida PK, Pradhan P, Rajan DK, Rebba E, Samal DK, Singh A, Sultania M, Agarwal SP, Agrawal A, Arora RK, Chaturvedi J, Garg PK, Gaurav A, Gupta A, Kottayasamy Seenivasagam R, D.D. Maharaj, Majumdar KS, Mishra N, Mittal A, Narain TA, Nirjhar R, Poonia DR, Sadhasivam S, Singh MP, Tiwari AR, Akula AK, Bandegudda SK, Bindlish RP, Chaitanya A, Chandrasekhara Rao LM, Dalakoti P, Dasu S, Giridhar A, Gorijavolu NB, Iyer RR, Jayakarthik Y, Jonathan GT, M.B. Kalla, Kheni Y, Kumar CS, Murtuza SA, Naidu CCK, Nalukurthi RK, Nemade HO, Nusrath S, Patnaik SC, Raju KVVN, Ramalingam PR, Rao KV, Rayani BK, Reddy Kallam, Reddy SRR, Saksena AR, Sebastian JA, Sharma RM, Thammineedi SR, Krishnamurthy A, Madhupriya S, Raja A, Ramakrishnan AS. Chennai, Dutt UK, D.N. Ghosh, Grewal S, Hans P, P.D. Haque, Jain R, P.A. Kingsley, Mahajan A, Mandrelle K, Michael V, Mukherjee P, Varghese A, Varghese SS, Veetil SK, Gaikwad P, George AJ, S.M. James, Jesudason MR, Mittal R, Moorthy M, Riju J, Sebastian A, Sen S, Singh S, Sreekar D, Thomas V, Titus DK, Yezzaji HS, Aggarwal M, Dhamija P, Kumar A, Chisthi MM, Gejoe G, Gopakumar D, Kollengode VV, Kuttanchettiyar KG, Yadev I, Balasubramanian A, Chaturvedula L, Dharanipragada K, Kalayarasan R, Manikandan R, Penumadu P, Lakshminarayana B, Mathew S, Reddihalli PV, Shivdas S, Akhtar N, Chaturvedi A, Gupta S, Kumar V, Rajan S, Agrawal N, Ahluwalia P, Arora A, K. Batra-Modi, Biswas M, Chaturvedi A, Chaturvedi H, Gautam G, Jain M, Jain S, Kumar S, Nayyar R, Singh S, Tiwari A, Bhushan Rangappa V, Kadapathri A, Kolur T, Pethkar R, Pillai V, Popli G, Sharma J, Shetty V, Subramaniam N, Williams J, Agarwal P, Agarwal V, Baghel A, Sharma DB, Silodia A, Singh KN, Yadav SK, Aziz G, Chowdri N, Mehraj A, Parray FQ, Shah ZA, Wani RA, Ahmed Z, Bali RS, M.A. Bhat, Laharwal AR, Mahmood M, Mir IS, Muzamil J, Najar FA, Rashid A, Rather MH, Zaieem M, Aggarwal G, Agrawal V, Ahmed A, Ahmed R, Bhaumik J, Ghosh A, Gupta S, Jain D, Jain PV, Kewlani V, Pipara A, Shakya S, Sharma A, Thambudorai R, Badwe RA, Bakshi G, Chandankhede U, Chaudhari V, Chaukar D, Chitkara G, Dash B, Deshmukh A, deSoouza A, Gulia A, Maheshwari A, Moiyadi A, Nair D, Nair NS, Niyogi D, Pal M, Pandey D, Patkar S, Poddar P, Pramesh CS, Puri A, Saklani A, Shetty P, Shrikhande SV, Shylasree TS, Singh V, Thiagarajan S, Islam AA, Kembuan G, Pajan H, Rahim F, Brouki Milan P, Mozafari M, Rezaei Tavirani M, Tizmaghz A, Safari H, Aremu M, A. Canas-Martinez, Cullivan O, Murphy C, Owens P, Pickett L, Akmenkalne L, Byrne J, Corrigan M, Cullinane C, Daly A, Fleming C, Jordan P, Kayyal MY, Killeen S, Lynch N, McCarthy A, Mustafa H, O’Brien S, O’Leary P, Syed WAS, Vernon L, O'Duffy F, McHugh A, Moran T, Callanan D, Dias A, Huang L, Ionescu A, Sheahan P, Balasubramanian I, Boland M, Carrington E, Conlon K, Cullinane C, Evoy D, Fagan J, Fearon N, Gallagher T, Geary E, Geraghty J, Hanly A, Heneghan H, Kennedy N, Kennelly R, Maguire D, Martin ST, McCartan D, McDermott EW, McPartland D, Ng KC, Prichard RS, Stafford T, Winter D, Alazawi D, Barry C, Boyle T, Butt W, Connolly E, Donlon N, Donohue C, B.A. Fahey, Farrell R, Fitzgerald C, Kinsella J, Larkin J, Lennon P, Maguire PJ, Mccormick P, Mehigan BJ, Mohan H, Nugent TS, O’Sullivan H, Ravi N, Reynolds JV, Rogers A, Shokuhi P, Smith J, Smith LA, Timon C, Bashir Y, Bass G, Conlon K, Connelly T, Creavin B, Earley H, Elliott JA, Gillis A, Kavanagh D, Madden A, Manecksha RP, Neary P, O’Connell C, O’riordan J, Reynolds IS, Rice D, Ridgway P, Thomas A, Umair M, Whelan M, Carroll P, Collins C, Corless K, Finnegan L, Fowler AL, Hogan A, Kerin M, Lowery A, McAnena P, McKevitt K, Nugent E, Ryan É, Coffey JC, Cunningham RM, Devine M, D.M. Nally, Peirce C, Tormey S, Hardy N, Neary P, O’Malley S, Ryan M, Gaziants V, Gold- Deutch R, Lavy R, L. Kalmovich-Muallem, Zmora O, Macina S, Mariani NM, Opocher E, Pisani Ceretti A, Ferrari F, Odicino F, Sartori E, Cotsoglou C, Granieri S, Bianco F, Camillo’ A, Colledan M, Tornese S, M.F. Zambelli, Bissolotti G, Fusetti S, Lemma F, Marino M, Marino MV, Mirabella A, Vaccarella G, Sena G, Agostini C, Alemanno G, Bartolini I, Bergamini C, Bruscino A, Checcucci C, De Vincenti R, Di Bella A, Fambrini M, Fortuna L, Maltinti G, Muiesan P, Petraglia F, Prosperi P, M.N. Ringressi, Risaliti M, Sorbi F, Taddei A, Tucci R, Bassi C, Bortolasi L, Campagnaro T, Casetti L, Conci S, De Pastena M, Esposito A, Fontana M, Guglielmi A, Landoni L, Malleo G, Marchegiani G, Nobile S, Paiella S, Pedrazzani C, Rattizzato S, Ruzzenente A, Salvia R, Turri G, Tuveri M, Altomare DF, Papagni V, Picciariello A, Bellora P, D’Aloisio G, Ferrari M, Francone E, Gentilli S, Nikaj H, Andreani L, Bianchini M, Capanna R, Caretto M, Chiarugi M, Coccolini F, Cremonini C, Di Franco G, Domenici L, Furbetta N, Gadducci A, Garibaldi S, Gianardi D, Giannini A, Guadagni S, Morelli L, Musetti S, Palmeri M, Perutelli A, Simoncini T, Tartaglia D, Anania G, Carcoforo P, Chiozza M, De Troia A, Koleva Radica M, Portinari M, Sibilla MG, Urbani A, Fabbri N, Feo CV, Gennari S, Parini S, Righini E, Ampollini L, M.F. Arcuri, Bellanti L, Bergonzani M, Bertoli G, Bocchialini G, Cattelani L, D’Angelo G, Gussago F, Lanfranco D, Manigrasso E, Musini L, Poli T, Polotto S, Santoro GP, Varazzani A, Aguzzoli L, Annessi V, Borgonovo G, Castro Ruiz C, Coiro S, Falco G, Mandato VD, Mastrofilippo V, M.T. Montella, Zizzo M, Grossi U, Novello S, Romano M, Rossi S, Zanus G, Esposito G, Frongia F, Pisanu A, Podda M, Belluco C, Lauretta A, Montori G, Moras L, Olivieri M. Irccs, Aviano, Bussu F, Carta AG, Cossu ML, Cottu P, Fancellu A, Feo CF, Ginesu GC, Giuliani G, Madonia M, Perra T, Piras A, Porcu A, Rizzo D, A.M. Scanu, Tedde A, Tedde M, Aversano A, Carbone F, Delrio P, Di Lauro K, Fares Bucci A, Rega D, Spiezio G, Pirozzolo G, Recordare A, Vignotto C, Badalamenti G, Campisi G, Cordova A, Franza M, Maniaci G, Rinaldi G, Toia F, Calabrò M, Farnesi F, Lunghi EG, Muratore A, Pipitone Federico NS, D’Andrea G, Familiari P, Picotti V, De Palma G, Luglio G, Pagano G, Tropeano FP, Antonelli B, Baldari L, Beltramini GA, Boni L, Cassinotti E, Gianni’ A, Pignataro L, Rossi G, Torretta S, Abatini C, Baia M, Biasoni D, Bogani G, Cadenelli P, Capizzi V, Cioffi SPB, Citterio D, Comini LV, Cosimelli M, Fiore M, Folli S, Gennaro M, Giannini L, Gronchi A, Guaglio M, Macchi A, Martinelli F, Mazzaferro V, Mosca A, Pasquali S, Piazza C, Raspagliesi F, Rolli L, Salvioni R, Sarpietro G, Sarre C, Sorrentino L, Agnes A, Alfieri S, Belia F, Biondi A, Cauteruccio M, Cozza V, D’Ugo D, De Simone V, Fagotti A, Gasparini G, Gordini L, Litta F, Lombardi CP, Lorenzon L, Maccauro G, Marra AA, Marzi F, Moro A, Parello A, Perrone E, Persiani R, Ratto C, Rosa F, Saponaro G, Scambia G, Scrima O, Sganga G, Tudisco R, Vitiello R, Ziranu A, Belli A, Granata V, Izzo F, Palaia R, Patrone R, Carrano FM, Carvello MM, De Virgilio A, Di Candido F, Ferreli F, Gaino F, Mercante G, Rossi V, Spinelli A, Spriano G, Santos PMDD, De Nardi C, D.M. Donati, Frisoni T, Palmerini E, Aprile A, Barra F, Batistotti P, Ferrero S, Fregatti P, Massobrio A, Pertile D, Scabini S, Soriero D, Sparavigna M, Adamoli L, Ansarin M, Cenciarelli S, Chu F, De Berardinis R, Fumagalli Romario U, Mastrilli F, Pietrobon G, Tagliabue M, Badellino E, Biglia N, Chiado’ Piat F, Ferrero A, Massobrio R, De Manzoni Garberini A, Mazzotti F, Pasini F, Ugolini G, Barone R, Birolo SL, Caccetta M, Deirino A, Garino M, Grasso M, Marafante C, Masciandaro A, Moggia E, Mungo S, Murgese A, Raggio E, Federico P, Maida P, Marra E, Marte G, Petrillo A, Tammaro T, Tufo A, Berselli M, Borroni G, Cocozza E, Conti L, Desio M, Livraghi L, Marchionni V, Quintodei V, Rizzi A, Baldi C, Corbellini C, Sampietro GM, Bordoni P, Clarizia G, Fleres F, Franzini M, Grechi A, Longhini A, Spolini A, Cellerino P, Galfrascoli E, Iacob G, Baldini E, Capelli P, Conti L, S.M. Isolani, Ribolla M, Bondurri A, Colombo F, Ferrario L, Guerci C, Maffioli A, Armao T, Ballabio M, Bisagni P, Gagliano A, Longhi M, Madonini M, Pizzini P, A.M. Baietti, Biasini M, Maremonti P, Neri F, Prucher GM, Ricci S, Ruggiero F, Zarabini AG, Impellizzeri H, Inama M, Moretto G, Barmasse R, Mochet S, Morelli L, Usai A, Bianco F, Incollingo P, Giacometti M, Zonta S, Marino Cosentino L, Sagnotta A, Dell’Oro C, Fruscio R, Grassi T, Negri S, Nespoli LC, Tamini N, Zambetti B, Anastasi A, Bartalucci B, Bellacci A, Canonico G, Capezzuoli L, Di Martino C, Ipponi P, Linari C, Montelatici M, Nelli T, Spagni G, Tirloni L, Vitali A, Abate E, Casati M, Casiraghi T, Laface L, Schiavo M, Arminio A, Cotoia A, Lizzi V, Vovola F, Vergari R, D’Ugo S, Depalma N, M.G. Spampinato, Annicchiarico A, Catena F, Giuffrida M, Perrone G, Baronio G, Carissimi F, Montuori M, Pinotti E, Bartolucci P, Binda B, Brachini G, Bruzzaniti P, Chiappini A, Chiarella V, Ciccarone F, Cicerchia PM, Cirillo B, Crocetti D, De Toma G, Di bartolomeo A, Duranti G, Fiori E, Fonsi GB, Franco G, Frati A, Giugliano M, Iannone I, La Torre F, Lapolla P, Leonardo C, Marruzzo G, Meneghini S, Mingoli A, Ribuffo D, Salvati M, Santoro A, Sapienza P, Scafa AK, Simonelli L, Zanacana G, Zambon M, Zuppi E, Capolupo GT, Carannante F, Caricato M, Mascianà G, Mazzotta E, Gattolin A, Migliore M, Rimonda R, Sasia D, Travaglio E, Chessa A, Fiorini A, Norcini C, Colletti G, Confalonieri M, Costanzi A, Frattaruolo C, Mari G, Monteleone M, Bandiera A, Bocciolone L, Bonavina G, Candiani M, Candotti G, De Nardi P, Gagliardi F, Medone M, Mortini P, Negri G, Parise P, Piloni M, Sileri P, Vignali A, Belvedere A, Bernante P, Bertoglio P, Boussedra S, Brunocilla E, Cervellera M, Cescon M, Cipriani R, Cisternino G, De Crescenzo E, De Iaco P, Del Gaudio M, Dondi G, Droghetti M, Germinario G, Gori A, Frio F, Jovine E, Mineo Bianchi F, Morezzi D, Neri J, Parlanti D, A.M. Perrone, Pezzuto AP, Pignatti M, Pinto V, Poggioli G, Ravaioli M, Rottoli M, Russo IS, Sartarelli L, Schiavina R, Serenari M, Serra M, Solli P, Tonini V, Taffurelli M, Tanzanu M, Tesei M, Violante T, Zanotti S, Borghi F, Cianflocca D, Di Maria Grimaldi S, Donati D, Gelarda E, Geretto P, Giraudo G, Giuffrida MC, Maione F, Marano A, Palagi S, Pellegrino L, Peluso C, Giaccardi S, Testa V, Agresta F, Prando D, Zese M, Aquila F, Gambacciani C, Lippa L, Pieri F, Santonocito OS, Armatura G, Bertelli G, Frena A, Marinello P, Notte F, Patauner S, Scotton G, Fulginiti S, Gallo G, Sammarco G, Vescio G, Balercia P, Catarzi L, Consorti G, Asti ELG, Bernardi D, Bonavina L, Lovece A, Di Marzo F, Fujiwara H, Hashimoto D, Yamaki S, Yamamoto T, Daiko H, Ishikawa M, Ishiyama K, Iwata S, Kanematsu K, Kanemitsu Y, Kato T, Kawai A, Kobayashi E, Kobayashi Kato M, Moritani K, Nakagawa M, Nakatani F, Oguma J, Tanase Y, Uno M, Hada T, Iwahashi H, Miyamoto M, Suminokura J, Takano M, Fujiwara K, Fujiwara N, Kurosaki A, Ababneh H, Al Abdallah M, Ayasra F, Ayasra Y, Hammad F, Qasem A, Abu Za’nouneh FJ, A.A. Al-Shraideh, Fahmawee T, Hmedat A, Ibrahim A, Obeidat K, Abdel Al S, Abdel Jalil R, Abou Chaar MK, M. Al-Masri, H. Al-Najjar, Alawneh F, Alsaraireh O, Elayyan M, Ghanem R, Lataifeh I, Fakhradiyev I, Saliev T, Tanabayeva S, Almahmeed H, Almazeedi S, Alsabah S, Jamal M, Aldokali N, Senossi O, M.T. Subhi, Algallai M, Alwarfly S, AlZAEDE. S, Gahwagi M, Moftah M, Abusannoga M, Alawami A, Alawami M, Albashri M, Malek A, Burgan D, Kamoka E, Kilani AI, Salamah A, Salem M, Shuwayyah A, Abdelkabir M, Altomi I, Altoumi M, Bouhuwaish A, Elmabri A, Omar M, Taher AS, Abdulwahed E, Alshareea E, Aribi N, Aribi S, Biala M, Ghamgh R, Morgom M, Alansari SAA, Aldayri Z, Alsoufi A, Elhadi A, Elhajdawe F, Ellojli I, ERgebi AAD, Kredan A, Msherghi A, Nagib T, Abudher A, Alshareef K, Elamin F, Bradulskis S, Dainius E, Kubiliute E, Kutkevičius J, Parseliunas A, Subocius A, Venskutonis D, Rasoaherinomenjanahary F, Razafindrahita JB, Samison LH, Ong EC, Abdul Maei N, Ngo CW, Ramasamy S, Hamdan KH, Ibrahim MR, Tan JA, Thanapal MR, Choong E, Lim RZM, Amin Sahid N, Hayati F, Jayasilan J, Sriram RK, Subramaniam S, Ibrahim AF, Che jusoh A, Hussain AH, Mohamed Sidek AS, Mohd Yunus, Soh JY, Wong MP, Zakaria AD, Zakaria Z, Kampan N, Mohd Azman ZA, Nur Azurah AG, Zainuddin AA, Fadzli AN, Fathi NQ, Koh PS, Liew YT, Roslani AC, Tang CY, Teoh LY, Wong WJ, Xavier R, Yahaya AS, Alvarez MR, Arrangoiz R, Cordera F, M.A. De la Rosa Abaroa, A. Gómez-Pedraza, Hernandez R, A. Maffuz-Aziz, Posada JA, A.I. Lupián-Angulo, Soulé Martínez CE, Aboharp Hasan Z, ALvarado Silva C, Bazan Soto A, Hernández Rubio A, Jiménez Villanueva X, Otoniel LR, Sosa Duran EE, Becerra García FC, J. Melchor-Ruan, Romero Bañuelos E, D. Vilar-Compte, A. Alfaro-Goldaracena, Buerba GA, R.A. Castillejos-Molina, Chan C, I. Dominguez-Rosado, H. Medina-Franco, Mercado MÁ, M. Oropeza-Aguilar, Peña Gómez Portugal E, O.E. Posadas-Trujillo, F. Rodriguez-Covarrubias, N. Salgado-Nesme, Sarre C, Vilatoba M, Arkha Y, Bechri H, El Ouahabi A, Oudrhiri MY, El Azhari A, S.M. Louraoui, Rghioui M, Bougrine M, Derkaoui hassani F, El abbadi N, Amrani L, Belkhadir ZH, Benkabbou A, Chakib O, El Ahmadi B, El Bouazizi Y, Essangri H, Ghannam A, A.M. Majbar, Mohsine R, Souadka A, Borgstein ABJ, Gisbertz SS, Van Berge Henegouwen MI (Amsterdam UMC, Cancer Center Amsterdam, University of Amsterdam, Hompes R, Meima-van Praag EM, Pronk A, Sharabiany S, Grotenhuis B, Hartveld L, Reijers S, W. Van Houdt, Baaij J, Bolster-van Eenennaam M, De Graaff M, Sloothaak D, Van Duijvendijk P, Ebben LDA, Kuiper SZ, Melenhorst J, Poeze M, Sluijpers NRF, Vaassen LAA, L. Posma-Bouman, Derksen T, Franken J, Oosterling S, De Bree R, Konsten J, Van Heinsbergen M, Adeyeye A, Akinmade A, Enoch E, Fayose S, Abur P, Fidelis L, Nwabuoku SE, Oyelowo N, Sholadoye TT, M.A. Tolani, Olaogun J, Abiyere H, Adebara I, Adeniyi A, Adeyemo O, Babalola O, Bakare A, Banjo O, Okunlola A, Adeniran A, Atobatele K, Eke G, Faboya O, Ogunyemi A, Omisanjo O, Oshodi O, Oshodi Y, Williams O, Ademuyiwa A, Afolabi B, Akinajo O, Alakaloko F, Atoyebi O, Balogun O, Belie O, Bode C, Chibuike George I, Elebute O, O. Ladipo-Ajayi, Ohazurike E, Okunowo A, Olajide TO, J. Seyi-Olajide, Daniel A, Egbuchulem IK, Lawal TA, Nwaorgu O, Ogundoyin O, Olulana D, Onakoya P, Oyelakin O, Abdullahi H, Agida E, O. Aisuodionoe-Shadrach, Ajibola H, Akaba G, Sani AS, Chinda J, Dawang Y, Garba S, Mshelbwala P, Obande J, Olori S, Olute A, Osagie O, Pius Ogolekwu I, Umar A, L. Abdur-Rahman, Adeleke N, Adeyeye A, Aremu I, Bello J, Olasehinde O, Popoola A, Raji HO, Massoud JG, Massoud R, Sorour TM, Abassy J, Ahmed K, Alvi A, Arshad M, Khan S, Pirzada A, Saleem A, Siddiqui T, Turk K, Hanif F, Haroon M, Khan MI, Jamal A, Kerawala AA, Memon AS, Nafees Ahmed R, Rai L, Javed S, Mahmood U, Shabbir RK, Yaqoob E, Afzal A, Ahmed Riaz S, Akbar A, Ali AA, Ali G, Janjua A, Mohsin M, Naqi SA, Saleem I, Shaukat A, Sohail M, M.F. Afzal, Khokhar MI, Latif F, Ayub B, Hassan N, Martins RS, Ramesh P, Sayyed R, Ayyaz M, Butt U, Kashif M, Khan WH, Qureshi AU, Umar M, Waris Farooka M, Wasim T, Bhatti ABH, Ayubi A, Rashid I, Waqar SH, I. Al-Slaibi, I.A. Alzeerelhouseini H, Jobran F, Abukhalaf SA, Arrue E, Cukier M, H. Rodriguez-Zentner, G. Borda-Luque, León Palacios JL, Lizzetti G, Vasquez Ojeda XP, Falcon Pacheco GM, Robles R, Jocson R, Teh C, Uy Magadia E, Major P, Bąk M, Dubieńska K, Ławnicka A, Murawa D, Bobiński M, Kotarski J, K. Rasoul-Pelińska, Brociek A, Chloupek A, Janik M, Kowalewski P, Kwiatkowski A, Panasiewicz P, Roszkowski R, Rot P, Sroczyński P, Walędziak M, Azevedo C, Machado D, Mendes F, De Sousa X, Fernandes U, Ferreira C, Guidi G, Leal C, Marçal A, Marques R, Martins D, Melo A, Tenreiro N, Vaz Pereira R, Vieira B, Almeida JI, R. Almeida-Reis, Correia de Sá T, Costa MJMA, Fernandes V, Ferraz I, Lima da Cruz L, Lima da Silva C, Lopes L, Machado N, Marialva J, Nunes Coelho M, Pedro J, Pereira C, Ribeiro A, Ribeiro CG, Santos R, Saraiva P, Silva RL, Tavares F, Teixeira M, Valente P, Almeida AC, Amaral MJ, Andrade R, Athayde Nemésio R, Breda D, Camacho C, Canhoto C, Colino M, Correia S, Costa M, De Barros J, De Oliveira López AL, Duque M, Garrido S, Guerreiro P, Guimarães A, Lázaro A, Lopes C, Martins R, Nogueira O, Oliveira A, Oliveira JM, Rodrigues M, Ruivo A, Santos E, Silva M, Simões J, Valente da Costa A, Almeida A, Castanheira Rodrigues S, Cavaleiro Leitão de Carvalho AS, Devezas V, Faria CS, Jácome F, Magalhães Maia M, Nogueiro J, Pereira A, A. Pereira-Neves, T. Pina-Vaz, H. Santos-Sousa, Silveira H, Vaz S, Vieira P, Gomes da Costa A, Lobo Antunes I, Pinto J, Tojal A, Cardoso N, Cardoso P, Domingues JC, Henriques P, Manso MI, Martins dos Santos G, Martins R, Morais H, Pereira R, Revez T, Ribeiro R, Ribeiro, VI, Soares A, Sousa S, Teixeira J, Amorim E, Baptista VH, M.F. Cunha, Dias B, Fazenda A, Melo Neves JP, Policarpo F, Sampaio da Nóvoa Gomes Miguel, II, Veiga D, Bandovas JP, Borges N, Branquinho A, Chumbinho B, Correia J, Fidalgo H, Figueiredo de Barros I, Frade S, Gomes J, Kam da Silva Andrade A, Maciel J, Pereira Rodrigues A, Pina S, Silva N, Silveira Nunes I, Sousa R, Ascensão J, Azevedo P, Costeira B, Cunha C, Garrido R, Gomes H, Lourenço I, Mendinhos G, Miranda P, Nobre Pinto A, Peralta Ferreira M, Ribeiro J, Rio Rodrigues L, Sousa Fernandes M, Azevedo J, Galvão D, Soares AC, Vieira A, Vieira B, Patrício B, Vieira Paiva Lopes AC, Cunha R, Faustino A, Freitas A, Jacob Oliveira B, A.B. Martins, Mendes JR, Parreira R, Rosa J, Teves M, Abreu da Silva A, Claro M, Costa Santos D, Deus AC, Grilo JV, Castro Borges F, Corte Real J, Henriques S, Lima MJ, Matos Costa P, Alagoa Joao A, Azevedo P, Camarneiro R, Capunge I, Fragoso M, Frazão J, Martins A, Pedro V, Pera R, Ramalho de Almeida F, Sampaio Soares A, Vale R, Vasconcelos M, Brito da Silva F, Caiado A, Fonseca F, Ângelo M, Baiao JM, Martins Jordão D, Vieira Caroço T, Messias J, Millan A, Salgado I, Santos P, Baía C, Canotilho R, A.M. Correia, Ferreira Pinto AP, Peyroteo M, Videira JF, Escobar P, Maldonado Santiago M, Kassir R, Sauvat F, Bonci E, Gata V, Titu S, Bezede C, Chitul A, Ciofic E, Cristian D, Grama F, Pirtea L, Secosan C, Ciubotaru C, Negoi I, Negoita VM, Stoica B, Ginghina O, Iordache N, Iosifescu RV, Mardare M, Mirica RM, Spanu A, A.B. Văcărașu, Zamfir-Chiru-Anton M, Garmanova T, Kazachenko E, Markaryan D, Rodimov S, Tsarkov P, Tulina I, Abelevich A, Bazaev A, Kokobelyan AK, A. Yanishev, Litvin A, Litvina Y, Provozina A, Agapov M, Galliamov E, Kakotkin V, Kubyshkin V, Semina E, Камалов А, Novikova A, Zakharenko A, Alshahrani M, Alsharif F, Eskander M, Al Raddadi R, Majrashi S, Mashat A, Akeel N, Alharthi M, Aljiffry M, Basendowah M, Farsi A, Ghunaim M, Khoja A, Maghrabi A, Malibary N, Nassif M, Nawawi A, Saleem A, Samkari A, Trabulsi N, A. Azab M, Aldosri M, Alghanem A, Alguraigari A, ALjohani K, Alqahtani D, Alzaidi TM, Basyouni A, Elhussain E, Jaloun H, Mudawi I, Shafei M, Al Awwad S, Alghamdi M, Alnumani T, Nasser M, Said bayazeed A, Abdelrhman S, Awad S, Ghedan S, I. Sharara M, Mashaly A, Aburahmah M, Al Otaibi F, Al-alem I, I.A. Al-Badawi, AlDahash H, Alhazzaa N, Alhefdhi A, Alhelal B, AlKattan K, Almalik O, Alomair A, Alomar O, Alotaibi NH, Alresaini F, Alrifai O, Alsakka M, Alsalamah R, Alsemari M, Alsobhi S, AlSumai T, Farrash F, Khan P, Mahasin Z, Othman E, Pant R, Robaidi H, Saleh W, Salem H, Shaheen M, Spangenberg P, Velagapudi S, Al Habes H, Alamri A, Alkarak S, Alqannas M, Alyami M, Alzamanan M, D. Cortés-Guiral, Elawad A, Adi H, Al ahmad F, Al Ayed A, Al zahrani A, Alalawi Y, Alishi Y, Alqahtani B, AlAamer O, Alriyees L, Alselaim N, Alfaifi J, Alkreedees N, Almutrafi SN, Alramadhan M, Alshitwi A, D’Souza J, Abdulkareem A, Ajlan A, Akkour K, A. Al-Habib, K. Al-Khayal, Alatar A, Alburakan A, Alhalal H, Alhassan B, Alhassan N, Aljassir F, Alobeed O, Alsaif A, Alsaif F, Alshammari S, Alshaygy I, Barry M, Bin Nasser A, Bin Traiki T, Bokhari A, Elwatidy S, Helmi H, Madkhali A, Nouh T, P.D. Rabah, Zubaidi A, Al Amri A, Abdulfattah F, Al Hasan I, E. Al-Kharashi, Alanazi F, Albaqami F, Alghamdi A, Alghuliga A, Aljaber F, Alsowaina K, Alsuhaibani A, Arab N, Badahdah F, Alobaysi S, Alshahrani A, Alzahrani A, Paunovic I, Slijepcevic N, Aleksić L, Antic A, Barisic G, Ceranic M, Ebrahimi K, Galun D, Grubač Ž, Ivanović N, Jelenkovic J, Kecmanović D, Kmezić S, Knezevic D, Krivokapic Z, Latinčić S, Markovic V, Matić S, Miladinov M, Pavlov M, Pejovic I, Radenkovic D, Sabljak P, Skrobić O, Šljukić V, Tadic B, Vasljević J, Velickovic D, Zivanovic M, Doklestic K, Gregoric P, Ivancevic N, Loncar Z, Micic D, Perovic M, Srbinovic L, Andrijasevic S, Bozanovic T, Cerovic Popovic R, Dokic M, Janjic T, Jeremic K, Kadija S, Ladjevic Likic I, Mirkovic L, Pantovic S, Pilic I, Radojevic M, Stefanovic A, Vidakovic S, Vilendecic Z, Antic S, Dunđerović D, Jelovac D, Jezdic Z, Konstantinovic V, Kotlar B, Kuzmanovic C, Lazić M, Pajić S, Petrovic M, Popovic F, Pucar A, Romic M, Sumrak S, Vujanac V, Bascarevic V, Bogdanovic I, Grujičić D, Ilic R, Jokovic M, Milićević M, Milisavljević F, Miljković A, Paunovic A, Šćepanović V, Stanimirovic A, Todorovic M, Folic M, Jotic A, Krejovic Trivic S, Milovanovic J, Trivic A, Bumbasirevic U, Dzamic Z, Kajmaković B, Prijović N, Zivkovic M, Buta M, Cvetkovic A, Djurisic I, Gacic S, Goran M, Inic Z, Jeftic N, Jevric M, Jokic V, Markovic I, Milanović M, Nikolic S, Pejnovic L, Savković N, Spurnic I, Stevic D, Stojiljkovic D, Vucic N, Zegarac M, Karamarkovic A, Kenic M, Kovacevic B, Krdzic I, Milutinović V, Savic G, Chan CW, Lieske B, Gális B, Šimko K, Cokan A, Crnobrnja B, Dovnik A, Knez J, Pakiž M, Almgla N, Bernon M, Boutall A, Cairncross L, Chinnery G, Herman A, Hilton T, Jonas E, Kloppers C, Malherbe F, Mugla W, Nel D, Rayamajhi S, Scriba M, Van Wyngaard T, Vogel J, A.M. Castaño-Leon, Delgado Fernandez J, Eiriz Fernandez C, Espino Segura-Illa M, Esteban Sinovas O, Garcia Perez D, Gomez P, L. Jimenez-Roldan, Lagares A, L. Moreno-Gomez, Paredes I, Pérez Núñez A, Sánchez Aniceto G, Santas Alegret M, Fernández Rodríguez P, Paniagua García Señorans M, R. Sanchez-Santos, Vigorita V, Acrich E, Baena Sanfeliu E, Barrios O, Golda T, Santanach C, M. Serrano-Navidad, Sorribas Grifell M, Vives RV, Arce Gil J, Escolà D, Jiménez A, Alcázar JA, M. Angoso-Clavijo, F. Blanco-Antona, A. Carabias-Orgaz, Díaz Maag R, Eguía Larrea M, Esteban Velasco C, Garcia J, A.G.P. García-Plaza, J.I. Gonzalez-Muñoz, L. Muñoz-Bellvis, F.C. Parreño-Manchado, Sánchez Tocino JM, A.B. Sanchez-Casado, Trebol J, Hernandez Gutierrez J, Tébar Zamora A, Sánchez Mozo A, Cayetano Paniagua L, Gomez Fernandez L, Artigues E, J.C. Bernal-Sprekelsen, Catalá Bauset JC, J. Gilabert-Estellés, Collera P, Diaz Del Gobbo R, Farre Font R, Flores Clotet R, Gómez Díaz CJ, Guàrdia N, Guariglia CA, Osorio A, Sanchez Jimenez R, Sanchon L, Soto Montesinos C, Albi Martin B, García Villayzán JE, L. Alonso-Lamberti, Assaf M, Baeza Pintado N, Carabias A, J. García-Quijada, Huertas Fernandez, Jimenez Miramón J, Jimenez V, Jover JM, Landeo Agüero SA, Leon R, M.B. Martín Salamanca, Pérez Simón V, Ponce S, Rodriguez JL, Salazar A, Valle Rubio A, Aguado H, Aldecoa Ansorregui I, Bravo Infante R, De Lacy FB, Di Somma A, B. Díaz-Feijoo, Enseñat Nora J, Fabregas N, Ferrés A, Gil Ibañez B, Gonzalez Sanchez JJ, Gracia I, Hoyos Castro JA, A.M. Lacy, Langdon C, Momblán D, Morales X, Oleaga L, Otero A, Pedrosa L, Poblete Carrizo J, Reyes Figueroa LA, P. Roldan Ramos, J. Rumia-Arboix, A.I. Tercero-Uribe, Topczewski TE, Torales J, Torne A, Torné R, V. Turrado-Rodriguez, Valero R, Valverde S, Anula R, Avellana R, Camarero Rodríguez E, Catalán Garza V, Dziakova J, García Alonso M, Lasses Martínez B, López Antoñanzas L, Muguerza JM, Ochagavía S, Peña Soria MJ, D. Rivera-Alonso, Saez Carlin P, Sánchez del Pueblo C, Sanz Ortega G, R. Sanz-Lopez, Torres A, M. Garcés-Albir, Lopez F, J. Martín-Arévalo, D. Moro-Valdezate, V. Pla-Marti, Beltrán de Heredia J, De Andrés-Asenjo B, Gómez Sanz T, Jezieniecki C, Nuñez Del Barrio H, Ortiz de Solórzano Aurusa FJ, Romero de Diego A, Ruiz Soriano M, Trujillo Díaz J, Vazquez Fernandez A, P. Lora-Cumplido, Sosa MV, Balague C, Ballester E, Moral A, Sánchez López A, Targarona EM, A. Galvan-Perez, E. Gonzalez-Gonzalez, A.M. Minaya Bravo, San Miguel-Mendez C, Alonso de la Fuente N, Cazador Labat M, Cecchini L, Espinosa CA, Jimenez Toscano M, López Campillo A, Mancebo G, Martorell P, Munarriz M, E.J. Grau-Talens, B. Martin-Perez, Benavides Buleje JA, Carrasco Prats M, Fernández PV, A. Fernández-López, García Escudero D, García Porcel VJ, Garcia Soria V, Giménez Francés C, González Valverde FM, E. Gurrea-Almela, P. López-Morales, Marco Garrido A, Martínez Alonso JA, Medina E, Muñoz Camarena JM, P.A. Parra Baños, Peña Ros E, Ramirez Faraco M, M. Ruiz-Marín, Sanchez Rodriguez C, Valero Soriano M, Allué Cabañuz M, Colsa Gutiérrez P, García Domínguez M, Gimenez Maurel T, Martín Anoro LF, Ponchietti L, Rodriguez Artigas JM, Roldón Golet M, Utrilla Fornals A, Estaire Gómez M, Fernández Camuñas Á, Garcia Santos EP, Jimenez Higuera E, López de la Manzanara Cano CA, C. Martínez-Pinedo, Moreno Pérez A, V. Muñoz-Atienza, D. Padilla-Valverde, Picón Rodríguez R, Redondo Calvo FJ, S. Sánchez-García, D. Sanchez-Pelaez, Curtis Martínez C, A. Fernández-Candela, L. Sánchez-Guillén, Colombari RC, Del valle E, Fernández M, Lozano Lominchar P, Martín L, Rey Valcarcel C, M.A. Steiner, Tudela M, Zorrilla Ortúzar J, Alcaide Matas F, García Pérez JM, Troncoso Pereira P, Blas Laina JL, Cros B, Escartin J, Garcia Egea J, Nogués A, Talal El-Abur I, Yánez C, I. Mora-Guzmán, Cárdenas Puiggrós L, Abellán M, Achalandabaso Boira M, Jorba R, Memba Ikuga R, Olona C, Sales Mallafré R, Aguilo O, Cavallé Busquets P, Gavalda Pellice MGP, Jorda Sole M, Mateu I, Miralles Curto M, Salinas Peña J, Fernández Martínez D, García Flórez LJ, L. Solar-Garcia, Aragon Achig EJ, Barbier L, Caja Vivancos P, Gainza A, García Gutierrez JJ, G. García-Operé, J. Gómez-Suárez, M. Jiménez-Jiménez, Mallabiabarrena Ormaechea G, Marín H, Martin Playa P, Melchor Corcóstegui I, J.A. Municio-Martín, Oñate M, L.A. Pascua-Gómez, M.A. Pesántez Peralta, Prieto Calvo M, Rodriguez Fraga A, Villalabeitia Ateca I, De Andres Olabarria U, Durán Ballesteros M, Fernández Pablos FJ, F.J. Ibáñez-Aguirre, Sanz Larrainzar A, B. Ugarte-Sierra, M.A. Acosta Mérida, Ortiz López D, Yepes Cano AF, Correa Bonito A, De la Hoz Rodríguez Á, Delgado Búrdalo L, Di Martino M, García Sánz I, García Septiem J, Maqueda González R, E. Martin-Perez, Muñoz de Nova JL, Calvo Espino P, Guillamot Ruano P, Colao García L, Díaz Pérez D, Esteban Agustí E, Galindo Jara P, Gutierrez Samaniego M, M.A. Hernandez Bartolome, Serrano González J, Alonso Poza A, Diéguez B, M. García-Conde, M. Hernández-García, Losada M, C.M. Chiesa-Estomba, González García JÁ, Larruscain E, J.A. Sistiaga-Suárez, Alvarez E, Chavarrias N, Frías L, García Pineda V, Gegúndez Simón A, Gómez Rivas J, Gortázar de las Casas S, Gracia M, Guevara J, Hernández Gutierrez A, Loayza A, María Dolores DT, Martí C, Melendez M, E. Moreno-Palacios, Perez Y, Prieto Nieto MI, P. Ramos-Martín, I. Rubio-Perez, Saavedra J, Sánchez Méndez JI, Siegrist Ridruejo J, Toribio Vazquez C, Urbieta A, Yebes A, Zapardiel I, D. Aparicio-López, Cantalejo diaz M, M.D.C. De Miguel Ardevines, Dobón Rascón MÁ, V. Duque-Mallén, Gascon Ferrer I, M.T. González-Nicolás Trébol, C. Gracia-Roche, Herrero Lopez M, Jariod Ferrer UM, Kälviäinen H, Lanzon A, Martinez German A, Matute M, Redondo C, Sánchez Fuentes N, M.S. Santero-Ramirez, Saudí S, Simón Sanz MV, Uson T, Blazquez Martin A, Diez Alonso M, García Rico E, Garcia-Loarte Gomez E, Garcia-Moreno Nisa F, Gutierrez Calvo A, Hernandez P, Lasa I, F. Mendoza-Moreno, Morales Palacios N, Ovejero Merino E, Vera Mansilla C, Acero J, Haddad A, Barranquero AG, Caballero Silva U, Cabañero Sánchez A, Cavestany Garcia-Matres C, Cerro Zaballos C, Fra Fernández S, Moreno Mata N, Muñoz Molina GM, Núñez J, Ocaña J, Ramos D, Acebes García F, Bailón M, Bueno Cañones AD, Choolani Bhojwani E, P. Marcos-Santos, Miguel T, Pacheco Sánchez D, B. Pérez-Saborido, Sanchez Gonzalez J, F.J. Tejero-Pintor, Alconchel F, Conesa A, Gil Martínez J, Gutiérrez Fernández AI, Lopez Abad A, T. Nicolás-López, Ramirez Romero P, Roca Calvo MJ, Rodrigues K, Ruiz Manzanera JJ, Soriano AI, Cano A, L. Capitan-Morales, Cintas Catena J, J. Gomez-Rosado, Oliva Mompean F, Pérez Sánchez, Río Lafuente FD, Torres Arcos C, J. Valdes-Hernandez, Bruna Esteban M, Cholewa H, Domingo S, Frasson M, Lago V, Marina Martin T, Martínez Chicote C, J. Sancho-Muriel, B. Estraviz-Mateos, Fernández Gómez Cruzado L, González de Miguel M, Landaluce-olavarria A, Lecumberri D, Abad Gurumeta A, A. Abad-Motos, E. Martínez-Hurtado, J. Ripollés-Melchor, Ruiz Escobar A, A. Cuadrado-García, Garcia-Sancho Tellez L, Heras Aznar J, Maté Mate P, Ortega Vázquez I, Picardo AL, Rojo López JA, Sanchez Cabezudo Noguera F, Serralta de Colsa D, Anchuelo Latorre J, Cagigas Fernandez C, Caiña Ruiz R, Fernandez Diaz MJ, Gomez Ruiz M, Hernanz F, Jimeno Fraile J, P. Martínez-Pérez, Poch C, Santarrufina Martinez S, Valbuena Jabares V, C. Moliner-Sachez, L. Pingarron-Martin, J. Rey-Biel, Ruiz Martin I, Cagigal Ortega EP, Cervera I, Díaz Peña P, Garcia de Castro Rubio E, Enjuto D, Fernández Bernabé P, Garcés García R, Gonzalez J, Hernández I, N. Herrera-Merino, Marqueta De Salas M, Martinez Pascual P, Perez Gonzalez M, Ramos Bonilla A, Rodríguez Gómez L, Alfonso Garcia M, A. Craus-Miguel, Fernández Vega L, E. Ferrer-Inaebnit, Gil Catalán A, González Argente FX, Jeri S, Oseira A, Pujol Cano N, J.J. Segura-Sampedro, Soldevila Verdeguer C, Villalonga B, Bescós C, R. Blanco-Colino, Brana I, Caimari B, De Pablo García-Cuenca A, F. Duran-Valles, E. Espin-Basany, Giralt López de Sagredo J, Pamias J, Pellino G, Prat N, Pujol Pina R, Saez barba M, Arulanantham A, Bandara GBKD, Jayarajah U, Ravindrakumar S, Rodrigo VSD, Ali Adil AA, Elhafiz MHY, Ali EE, Awadelkarim M, Bakheit I, Elbahri H, Hamid HKS, M.E.A. Essa, Ahmed AA, Abubakr Hassan, Momin Majed Yousuf Hilles, Saleh M, Arkani S, Freedman J, Elbe P, Lindqvist EK, Angenete E, Park J, Taflin H, Greiff L, Hagander L, Älgå A, Heinius G, Nordberg M, Pieniowski E, Gkekas I, Löfgren N, Rutegård M, Sund M, Arigoni M, Bernasconi M, Christoforidis D, Di Giuseppe M, La Regina D, Mongelli F, Chevallay M, Dwidar O, Gialamas E, Sauvain M, Giger R, Hool S, Klenke F, Kollàr A, Kurze C, Mueller SA, Kiessling S, Stoeckli S, Adamina M, Bächler T, Crugnale AS, Giardini M, Guglielmetti L, Peros G, Solimene F, Gass M, Metzger J, Scheiwiller A, Gutschow C, Turina M, Al Asadi T, Alkhateb S, Altom R, Bakkar B, Maa Albared S, Melhem S, Hamdan A, Hammed A, Hammed S, Hossain M, Mahfoud M, Moussa A, Alsayyad R, Alsrouji S, Ashour G, Hareth Al-Nahr M, Slitin A, Tanos C, Kacem MJ, Maghrebi H, Sebai A, Aghayeva A, Hamzaoglu I, Sahin I, Akaydin E, Aliyeva Z, Aytac E, Baca B, Dülgeroğlu O, Ozben V, Ozmen BB, Uras C, Arikan AE, Bilgin IA, Bozkırlı B, Ceyhan GO, Kara H, Karahasanoğlu T, Uras C, Celik H, Meydanli MM, Akbas A, Altinel Y, Calikoglu F, Ercan G, Ercetin C, Hacım NA, Meriç S, Tokocin M, Vartanoglu T, Yigitbas H, Akilli H, Ayhan A, Kuscu E, Doğangün M, Iflazoğlu N, Yalkın Ö, Turna A, M.A. Onan, Akgor U, Cennet O, Dincer HA, Erol T, Gultekin M, Orhan N, Ozgul N, Salman MC, Soyak B, Aydemir L, Başaran B, Kara H, Sen C, Ulusan M, Açıkgöz AS, Alhamed A, Aykanat Y, Bese T, Cebi S, Demirkıran F, Ergün S, Kayan B, M.F. OZcelık, Sanli AN, Uludağ SS, Velidedeoglu M, Zengin AK, M.A. Bozkurt, Kara Y, Kocatas A, Candas Altinbas B, A.B. Çekiç, Eyuboglu K, Guner A, Türkyılmaz S, M.A. Usta, Cimenoglu B, Demirhan R, Saracoglu K, Azamat İF, Balik E, Buğra D, Giray B, C.B. Kulle, Taskiran C, Vatansever D, Güler SA, Güreşin A, Tatar OC, Utkan NZ, Yildirim A, Yüksel E, Abbasov A, Yanar H, Ugurlu MU, Akin E, Altintoprak F, Bayhan Z, Cakmak G, Çapoğlu R, Çelebi F, Demir H, Dikicier E, Firat N, Gönüllü E, M.B. Kamburoğlu, Kocer B, Küçük IF, Mantoglu B, Çolak E, Kucuk GO, M.S. Uyanik, Goksoy B, Bozkurt E, Citgez B, Mihmanli M, Tanal M, Yetkin G, Akalin M, Arican C, Avci EK, Aydin C, Demirli Atıcı S, Emiroglu M, Kaya T, Kebabçı E, Kilinc G, Kirmizi Y, Öğücü H, Salimoğlu S, Sert İ, Tugmen C, Tuncer K, Uslu G, Yeşilyurt D, Karaman E, Kolusarı A, Yildiz A, Gultekin FA, Lule H, Oguttu B, Abdelgalil K, Agilinko J, Ahmeidat A, Barabasz M, Bekheit M, Cheung LK, Colloc T, Cymes W, Elhusseini M, Gradinariu G, Hannah A, B.S. Kamera, Mignot G, Shaikh S, Sharma P, I. Abu-Nayla, Agrawal A, A. Al-Mohammad, Ali S, Ashcroft J, Azizi A, Baker O, Balakrishnan A, Byrne M, Colquhoun A, Cotter A, Coughlin P, Davies RJ, Durrani A, Elshaer M, Fordington S, Forouhi P, Georgiades F, Grimes H, Habeeb A, Hudson V, Hutchinson P, Irune E, Jah A, Khan DZ, Kolias A, Kyriacou H, Lamb B, Liau S, Luke L, Mahmoud R, Mannion R, Masterson L, Mitrofan C, Mohan M, Morris A, Murphy S, O’Neill JR, Price S, Pushpa-rajah J, W. Raby-Smith, Ramzi J, S.M. Rooney, Santarius T, Singh AA, Stewart GD, Tan XS, Townson A, Tweedle E, Walker C, Waseem S, Yordanov S, Jones T, Kattakayam A, Loh C, Lunevicius R, Nunes Q, Pringle S, Schache A, Shaw R, Sheel A, Sud A, Sundhu M, Rossborough C, Angelou D, Choynowski M, McAree B, McCanny A, Neely D, Kamel F, Kumar L, Madani R, Nisar P, Tutoveanu G, Ali S, M.N. Bittar, Creanga M, Elniel M, Law J, Youssef M, Ahad S, De La Cruz Monroy MFI, Hashem M, Langlands F, Mosley F, Oktseloglou V, Omar I, Patel F, Alanbuki A, Patel M, Shabana A, Rathinaezhil R, Perera E, Raveendran D, K. Ravi-Shankar, Thiruchelvam J, Che Bakri NA, Jawad Z, Jiao L, Nazarian S, Vashisht R, Arrowsmith L, Campbell W, Grove T, Kontovounisios C, Warren O, Rolland P, Aggarwal A, Brown S, Jelley C, Neal N, Kaur R, Leung E, Sundar S, Doulias T, Li M, Martin E, Rodwell H, Clifford R, Eardley N, Krishnan E, Manu N, Martin E, Roy Mahapatra S, Serevina OL, Smith C, Vimalachandran D, Bordenave M, Houston R, Putnam G, Robson A, Tustin H, Emslie K, Labib PL, Marchbank A, Miller D, Minto G, Natale J, Nwinee H, Panahi P, Rogers L, Abubakar A, Akhter Rahman MM, Chan E, O’Brien H, Sasapu K, Inglis R, Ng HJ, De Gea Rico A, Ghazali N, Lambert J, Markose G, Math S, Sarantitis I, Shreshtha D, Simpson R, Sonanis S, Sultana A, Taggarsi M, Timbrell S, Vaz OP, Vitone L, Day A, Dent H, Fahim M, Waheed S, Hunt A, Laskar N. Hastings, Gupta A, Steinke J, Thrumurthy S, Massie E, McGivern K, Rutherford D, Wilson M, Hardie J, Kazzaz S, T. Bacarese-Hamilton, Ip M, James A, Salerno G, Stockdale T, Handa S, Kaushal M, Kler A, Patel P, Redfern J, Tezas S, Aawsaj Y, Amonkar S, Barry C, Blackwell L, Blake D, Carter J, Emerson H, Fisher A, Katory M, Korompelis P, McCormick W, Mustafa A, Pearce L, Ratnavelu N, Reehal R, Damola A, Kretzmer L, Lalou L, Lim P, Manku B, Parwaiz I, Sandher M, Stafford J, Abdelkarim M, Asqalan A, Gala T, Ibrahim S, Maw A, Mithany R, Morgan R, Sundaram Venkatesan G, Holroyd D, Jamieson N, Jones C, Shin JS, Ang K, Caruana EJ, Chandarana K, M.F. Chowdhry, Mohammad A, Nakas A, Rathinam S, Banfield D, Boal M, Brown O, Dean H, Dwerryhouse S, Higgs S, Vallance A, Boyd E, Irvine V, Kirk A, Bakolas G, Boulton A, Chandock A, Khan T, Kumar M, Agoston P, Billè A, Challacombe B, Fraser S, K. Harrison-Phipps, King J, McCrindle S, Mehra G, Mills L, Najdy M, Nath R, Okiror L, Pilling J, Rizzo V, Routledge T, Sayasneh A, Stroman L, Wali A, Fehervari M, Fotopoulou C, Habib N, S. Hamrang-Yousefi, Jawad Z, Jiao L, Pai M, Ploski J, Rajagopal P, Saso S, Sodergren M, Spalding D, Laws S, Hardie C, McNaught C, Alam R, Budacan A, Cahill J, Kalkat M, Karandikar S, Kenyon L, Naumann D, Patel A, Chen F, Cheung J, Ayorinde J, Chase T, Cuming T, Ghanbari A, Humphreys L, Tayeh S, Aboelkassem Ibrahim A, Bichoo R, Cao H, Chai AKW, Choudhury J, Evans C, Fitzjohn H, Ikram H, Khalifa E, Langstroth M, Loubani M, McMillan A, Nazir S, Qadri SSA, Robinson A, Ross E, Sehgal T, Wilkins A, Dixon J, Dunning J, Freystaetter K, Jha M, Kusuma VRM, Lester S, Madhavan A, Thulasiraman SV, Viswanath Y, T. Curl-Roper, Delimpalta C, Liao CCL, Velchuru V, Westwood E, Belcher E, G. Bond-Smith, Chidambaram S, Di Chiara F, Fasanmade K, Fraser L, Fu H, Ganau M, Gore S, Goricar M, Graystone J, Jeyaretna D, Khatkar H, Lami M, Maher M, Mastoridis S, McVeigh J, Mihai R, Myatt R, Piper R, Prabhu S, Risk OBF, Selbong U, Shah K, Silva P, Smillie R, Soleymani majd H, Sravanam S, Stavroulias D, Tebala GD, Vatish M, Verberne C, Wallwork K, M.A. Williams, Winter SC, Ahmed I, Djouani A, Eddy B, Folkard S, Hassan F, Kommu S, Papadopoulos G, Simoes A, Streeter E, J. Tait-Bailey, Thomas M, Wang W, Yao M, Anscomb N, R. Baldwin-Smith, Davies M, Grainger C, Haji A, Haq A, J.W. Nunoo-Mensah, Rizk M, Bhatti MI, H. Boyd-Carson, Elsey E, Gemmill E, Herrod P, Jibreel M, Lenzi E, Saafan T, Sapre D, Sian T, Watson N, Athanasiou A, Borg E, Bourke G, Bradshaw L, Brunelli A, Burke J, Coe P, Costigan F, Elkadi H, Ho M, Johnstone J, Kanatas A, Kantola V, Kaufmann A, Laios A, Lam S, MacInnes E, Munot S, Nahm C, Otify M, Pompili C, Raslan M, Salminen H, Smith I, Theophilou G, Toogood G, Wade R, Ward D, West C, A. Al-Harbawee, Alharawee A, Annamalai S, Ashmore C, Boddy A, Hossain T, Irvine E, Kassam K, Kourdouli A, Chean CS, Dharamavaram S, Gvaramadze A, Jibril A, Kulkarni N, Pereira I, Prusty L, Shanthakunalan K, Srikumar B, Thekkinkattil D, Adegbola S, Menakaya C, Noel J, Harky A, Shackcloth M, Askari A, Chan C, Cirocchi N, Kudchadkar S, Patel K, Sagar J, Shaw S, Talwar R, Abdalla M, Edmondson R, Ismail O, Jones D, Newton K, Stylianides N, Aderombi A, Andaleeb U, Bajomo O, Beatson K, Garrett W, Mehmood M, Ng V, R. Al-Habsi, Brimioulle M, Divya GS, Keeler B, Soulsby RE, Taylor A, B. Al-Sarireh, Clancy R, Cripps P, Dobbs T, Egan R, Fabre I, Harries R, Henry A, Kittur M, Li Z, Parkins K, Soliman F, Spencer N, Thompson D, Burgess C, Gemmell C, Grieco C, Hollyman M, Hunt L, Morrison J, Ojha S, Abbadessa F, Barnard S, Chan C, Dawe N, Hammond J, Koshy RM, Mahmoud Ali F, McPherson I, Mellor C, Moir J, Pandanaboyana S, Powell J, Rai B, Rogers A, Roy C, Sachdeva A, Saleh C, Tingle S, Williams T, Manickavasagam J, McDonald C, McGrath N, McSorley N, Ragupathy K, Ramsay L, Solth A, Aristotelous C, Kakisi O, Seebah K, Shaikh I, Sreedharan L, Touil L, Youssef M, Shah J, Ameerally P, Baguley M, Gnanachandran C, Heer B, Rogers M, Woods R, Aujayeb A, Mills S, Abu J, E. Addae-Boateng, Bratt D, Brock L, Burnside N, S. Cadwell-Sneath, Gajjar K, Gan C, Grundy C, Hallam K, Hassell K, Hawari M, Joshi A, Khout H, Konstantinidi K, R.X.N. Lee, Nunns D, Schiemer R, Walton T, Weaver H, Whisker L, Williamson K, McVeigh J, Myatt R, M.A. Williams, Ahmed ME, Bukhari SI, Illingworth B, Kanthasamy S, Knights E, Ong SL, Pujari R, Tan KHM, Vanker R, Michel M, Patil S, Ravindran S, Sarveswaran J, Scott L, Biliatis I, Edmond M, King E, Babawale O, Hodgson D, Ismail M, Khan J, Lokman U, Phan YC, Almond M, Bhangu A, Breik O, Cato LD, Chowdhury YA, Desai A, Ford S, Griffiths E, Idle M, Kamal M, Karia K, Kisiel A, Kulkarni R, Mak JKC, Martin T, Nankivell P, Parente A, Parmar S, A.M. Pathanki, Phelan L, Praveen P, Saeed S, Sharma N, Singh J, Solomou G, Soon WC, Stevens A, Tirotta F, Topham C, Ughratdar I, Vijayan D, Ballantyne K, Barker L, Chapman K, Charalambous M, Chianakwalam C, English C, Evans J, Fell A, Frimpong D, Halkias C, Iyer R, Merh R, Neagu G, Nikolaou S, Poddar A, Pronisceva V, Reddy V, Williams N, Alakandy L, Bhattathiri P, Brown J, Canty M, Day E, Geddes A, Grivas A, Hassan S, Lammy S, Littlechild P, Maseland C, Mathieson C, McCaul J, McMahon J, O’Kane R, St. George E, Suttner N, Taylor W, Tilling E, English W, Kaul S, Khan AH, Khan F, Mansuri A, Mukherjee S, Patel M, Sarigul M, Singh S, Smith C, Tan KL, Vulliamy P, Woodham A, Yang YH, Adiamah A, Brewer H, Chowdhury A, Evans J, Humes D, Jackman J, Koh A, C. Lewis-Lloyd, Navarro A, Oyende O, Reilly J, Vohra R, Worku D, Cool P, Cribb G, Shepherd K, Bisset C, Moug S, Chadha R, Elson N, Galleano R, Faulkner G, Langone A, Panayi Z, Saleh P, Tuminello F, Underwood C, Brixton G, Findlay L, Klatte T, Majkowska A, Manson J, Potter R, W. Al-Khyatt, Awad S, Bhalla A, Chia Z, Daliya P, Goyal A, Grimley E, Hamad A, Kumar A, Malcolm FL, Ng JCK, Phillips A, Theophilidou E, Williams S, Bowden J, Campain N, Daniels I, Evans C, Fowler G, John J, Massey L, McDermott F, McGrath J, McLennan A, Ng M, Pascoe J, Rajaretnam N, Angamuthu N, Bulathsinhala S, Chowdhury S, Davidson B, Fusai G, Gilliland J, Hart C, Hidalgo Salinas C, Knowles J, Machairas N, Mirnezami R, Pissanou T, Pollok JM, Raptis DA, Soggiu F, Tzerbinis H, Varcada M, Xyda S, Beamish A, Davies E, Foulkes R, Magowan D, Nassa H, Ooi R, Price C, Smith L, Solari F, Tang A, Williams G, Abd Kahar NN, Y. Al-Tamimi, Bacon A, Beasley N, Catto J, Chan LH, Chew D, Crank M, Ilenkovan N, Macdonald M, Narice B, Rominiyi O, Saad S, Sinha S, Thompson A, Varley I, Brennan P, Drake T, Harrison EM, Linder G, Mayes J, McGregor R, Pasricha R, Skipworth RJE, Zamvar V, Davies E, Hawkin P, Raymond T, Ryska O, Baron R, Dunne D, Gahunia S, Halloran C, Howes N, McKinney R, McNicol F, Rajput K, Russ J, Sutton R, Szatmary P, Tan JR, Thomas A, Whelan P, Anzak A, Banerjee A, Fuwa O, Hughes F, J.D. Jayasinghe, Knowles C, Kocher HM, Leal Silva I, Ledesma FS, Minicozzi A, Navaratne L, Patki P, Rahman R, Ramamoorthy R, Sohrabi C, Tanabalan C, Thaha M, Thakur B, Venn M, Yip V, Baumber R, Parry J, Evans S, Jeys L, Morris G, Parry M, Stevenson J, Ahmadi N, Aresu G, Z.M. Barrett-Brown, Coonar A, Durio Yates H, Gearon D, Hogan J, King M, Peryt A, Pradeep IS, Smith C, Adishesh M, Atherton R, Baxter K, Brocklehurst M, Chaudhury M, Krishnamohan N, McAleer J, Owens G, Parkin E, Patkar P, Phang I, Aladeojebi A, Ali M, Ali S, Barmayehvar B, Gaunt A, Gowda M, Halliday E, Kitchen M, Mansour F, Nanjaiah P, Thomas M, Zakai D, N. Abbassi-Ghadi, Assalaarachchi H, Currie A, Flavin M, Frampton A, Hague M, Hammer C, Hopper J, Horsnell J, Humphries S, Kamocka A, Madhuri TK, Preston S, Singh P, Stebbing J, Tailor A, Walker D, Coomber E, Jaunoo S, Kennedy L, Williams O, Airey A, Bunni J, Crowley R, Fairhurst K, Frost J, George R, Lee S, Mitchell S, Phull J, Richards S, Aljanadi F, Campbell A, Glass A, Hraishawi I, Jones M, McIlmunn C, McIntosh S, Mhandu P, O’Donnell C, Turkington R, Z. Al-Ishaq, Bhasin S, Bodla AS, Burahee A, Crichton A, A. El-Ghobashy, Fossett R, Pigadas N, Rahman E, Snee D, Vidya R, Yassin N, Colombo F, Fountain D, M.T. Hasan, Karabatsou K, Laurente R, Pathmanaban O, Barlow C, Ding D, Foster J, Longstaff L, C. Brett-Miller, Buruiana FE, Kaur R, Leung E, Sundar S, Al-mukhtar A, Brown S, Edwards J, Giblin A, Kelty C, Lee M, Lye G, Newman T, Sharkey A, Steele C, Sureshkumar Shah N, Whitehall E, Blair J, Lakhiani A, W. Parry-Smith, Sahu B, Athwal R, Baker A, Jones L, Konstantinou C, Ramcharan S, Singh S, Vatish J, Wilkin R, Alzetani A, Amer K, Badran A, Colvin HV, Ethunandan M, Sekhon GK, Shakoor Z, Shields H, Singh R, Talbot T, Wensley F, Lawday S, Lyons A, Newman S, Chung E, Hagger R, Hainsworth A, Hunt I, Karim A, Owen H, Ramwell A, Santhirakumaran G, Smelt J, Tan C, Vaughan P, Williams K, Baker C, Davies A, Gossage J, Kelly M, Knight W, Bromage S, Hall J, Kaushik V, Rudic M, Vallabh N, Zhang Y, Harris G, James G, Kang C, Lin DJ, Rajgor AD, Royle T, Scurrah R, Steel B, Watson LJ, Kocher HM, Choi D, Hutchison R, Jain A, Luoma V, Marcus HJ, May R, Menon A, Pramodana B, Webber L, Hayes A, Jones R, Sivarajah G, Smith M, Smrke A, Strauss D, Abouelela FAM, Aneke IA, Asaad P, Brown B, Collis J, Duff S, Khan A, Moura F, Taylor M, Wadham B, Warburton H, Elmoslemany T, M.D. Jenkinson, Millward CP, Zakaria R, Mccluney S, Parmar C, Shah S, Allison J, M.S. Babar, Bowen J, Collard B, Goodrum S, Lau K, Patel A, Sargent M, Scott R, Thomas E, Whitmore H, Balasubramaniam D, Jayasankar B, Kapoor S, Ramachandran A, Semple C, Elhamshary A, Imam SMB, Kapriniotis K, Kasivisvanathan V, Lindsay J, S. Rakhshani-Moghadam, Beech N, Chand M, Green L, Kalavrezos N, Kiconco H, McEwen R, Schilling C, Sinha D, Pereca J, Singh J, Chopra S, Egbeare D, Thomas R, Arumugam S, Ibrahim B, Khan K, Combellack T, Hill G, Jones S, Kornaszewska M, Mohammed M, Tahhan G, Valtzoglou V, Williams J, Blencowe N, Eskander P, Gash K, Gourbault L, Hanna M, Maccabe TA, Main B, Olivier J, Newton C, Roswadowski S, Ryan N, Teh E, West D, Al-omishy H, Baig M, Bates H, Di Taranto G, Dickson K, Dunne N, Gill C, Howe D, Jeevan D, Khajuria A, A. Martin-Ucar, McEvoy K, Naredla P, Ng V, Robertson S, Sait M, Sarma DR, Shanbhag S, Shortland T, Simmonds S, Skillman J, Tewari N, Walton G, M.A. Akhtar, Brunt A, McIntyre J, Milne K, Rashid MM, Sgrò A, Stewart KE, Turnbull A, A.K. Abou-Foul, Gossedge G, O’Donnell S, Oldfield F, Thomson S, Aguilar Gonzalez M, Talukder S, Boyle C, Fernando D, Gallagher K, Laird A, Tham D, Bath M, Patki P, Sohrabi C, Tanabalan C, Basnyat P, Davis H, Montauban P, Shrestha A, Agarwal K, Arif T, Magee C, Nambirajan T, Powell S, Vinayagam R, Flindall I, Hanson A, Mahendran V, Green S, Lim M, MacDonald L, Miu V, Onos L, Sheridan K, Young R, Alam F, Griffiths O, Houlden C, Jones R, Kolli VS, Lala AK, Leeson S, Peevor R, Seymour Z, Consorti E, Gonzalez R, Grolman R, R. Kwan-Feinberg, Liu T, Merzlikin O, San Francisco, Brown A, Cooper Z, Hirji S, Jolissaint J, Mahvi D, Okafor B, Raut CP, Roxo V, Salim A, Bessen S, Chen L, Dagrosa L, Fay K, Fleischer C, Hasson R, Henderson E, Leech M, Loehrer A, Markey C, Paydarfar J, Rosenkranz K, Telma K, Tocci N, I. Wilkinson-Ryan, Wilson M, Bokenkamp M, Brown K, Fleming D, Haynes A, Heron C, Hill C, Kay H, Leede E, McElhinney K, Olson KA, Osterberg EC, Riley C, Srikanth P, Barbour J, Blazer D, DiLalla GA, Fayanju O, Hwang ES, Kahmke R, Kazaure H, Lazarides A, Lee W, Lidsky M, Menendez C, Moris D, Plichta J, Pradhan MC, Puscas L, Rice HE, Rocke D, Rosenberger L, Scheri R, B.D. Smith, M.T. Stang, Tolnitch L, Turnage K, Visgauss J, Walton FS, Watts T, Zani S, Farma J, Cardona K, Russell MC, Clark J, Kwon D, Goel N, Kronenfeld J, Bigelow B, Etchill E, A. Gabre-Kidan, Jenny H, Kent A, Ladd MR, Long C, Malapati H, Margalit A, Rapaport S, Rose J, Stevens K, Tsai L, Vervoort D, Yesantharao P, Dehal A, Klaristenfeld D, Huynh K, Kaafarani H, Naar L, Qadan M, Brown L, Ganly I, Mullinax JE, Alpert N, Gillezeau C, F.A.C.S.B.A. Miles DDS MD, Taioli E, Cha DE, Gleeson E, Horn C, Sarpel U, Gusani N, Hazelton J, Maines J, Oh JS, Ssentongo A, Ssentongo P, Bhama A, Colling K, Najarian M, Azam M, Choudhry A, Marx W, Abedin Y, Arzumanov G, Chokshi R, Gabrilovich S, Glass N, Kalyoussef E, F.P. Parvin-Nejad, Roden D, Stein J, A. Suarez-Ligon, Tsui G, Zhao K, Fleming J, Fuson A, Gigliotti J, Ovaitt A, Ying Y, Abel MK, Andaya V, Bigay K, M.A. Boeck, Chen L, Chern H, Corvera C, I. El-Sayed, Glencer A, Ha P, B.C.S. Hamilton, Heaton C, Hirose K, D.M. Jablons, Kirkwood KS, Kornblith LZ, Kratz JR, Lee RH, Miller PN, Nakakura EK, B. Nunez-Garcia, O’Donnell RJ, Ozgediz D, Park P, Robinson B, Sarin A, Sheu B, Varma MG, Wai KC, Wustrack R, Xu MJ, Zimel M, San Francisco, CA) Beswick D, Goddard J, Manor J, Song J, Denver/Colorado Springs/Loveland, Cioci A, Pavlis W, Rakoczy K, Ruiz G, Saberi R, Fullmer T, Gaskill C, Gross N, Kiong K, Roland CL, Zafar SN, Abdallah M, Abouassi A, Aigbivbalu E, Almasri M, Eid J, George B, Kulkarni G, Marwan H, Mehdi M, San Andrés M, Sundaresan J, Aoun SG, Ban VS, Batjer HH, Bosler K, Caruso J, Sumer B, Abbott D, Acher A, Aiken T, Barrett J, Foley E, Schwartz PB, Zafar SN, Hawkins AT, Maiga A, Ruzgar NM, Sion M, Ullrich S, Laufer J, Scasso S, H. Al-Naggar, M. Al-Shehari, Almassaudi A, Alsayadi M, Alsayadi R, Nahshal M, Shream S, AL-Ameri S, and Aldawbali M
Appendix
Supplemental Table 1.
Demographics of patients who underwent any operations (n=3778)a
| Uterus (n=1751) | Ovary (n=1355) | Cervix (n=449) | Vulva/vagina (n=223) | Total (n=3778) | |
|---|---|---|---|---|---|
| Age (y) | |||||
| 17–19 | 1 (0.1) | 12 (0.9) | 0 (0) | 0 (0) | 13 (0.3) |
| 20–29 | 7 (0.4) | 60 (4.4) | 23 (5.1) | 4 (1.8) | 94 (2.5) |
| 30–39 | 53 (3.0) | 106 (7.8) | 121 (27.0) | 7 (3.1) | 287 (7.6) |
| 40–49 | 172 (9.8) | 246 (18.2) | 142 (31.6) | 22 (9.9) | 582 (15.4) |
| 50–59 | 460 (26.3) | 362 (26.7) | 96 (21.4) | 48 (21.5) | 966 (25.6) |
| 60–69 | 539 (30.8) | 353 (26.1) | 37 (8.2) | 47 (21.1) | 976 (25.8) |
| 70–79 | 409 (30.8) | 179 (13.2) | 26 (5.8) | 56 (25.1) | 670 (17.7) |
| 80–89 | 106 (6.1) | 37 (2.7) | 4 (0.9) | 37 (16.6) | 184 (4.9) |
| >90 | 4 (0.2) | 0 (0) | 0 (0) | 2 (0.9) | 6 (0.2) |
| Region | |||||
| Europe & Central Asia | 1078 (61.6) | 756 (55.8) | 268 (59.7) | 177 (79.37) | 2279 (60.3) |
| Latin America & Caribbean | 196 (11.1) | 174 (12.8) | 81 (18.0) | 17 (7.6) | 467 (12.4) |
| East Asia & Pacific | 178 (10.2) | 141 (10.4) | 50 (11.1) | 4 (1.8) | 373 (9.9) |
| South Asia | 73 (4.2) | 150 (11.1) | 18 (4.0) | 8 (3.6) | 249 (6.6) |
| North America | 142 (8.1) | 65 (4.8) | 20 (4.5) | 10 (4.5) | 237 (6.3) |
| Middle East & North Africa | 79 (4.5) | 65 (4.8) | 4 (0.9) | 5 (2.2) | 153 (4.1) |
| Sub-Saharan Africa | 6 (0.3) | 4 (0.3) | 8 (1.8) | 2 (0.9) | 20 (0.5) |
| Income group | |||||
| High | 1351 (77.2) | 914 (67.5) | 317 (70.6) | 186 (83.4) | 2768 (73.3) |
| Upper middle | 298 (17.0) | 249 (18.4) | 108 (24.1) | 29 (13.0) | 684 (18.1) |
| Low-middle | 102 (5.8) | 192 (14.2) | 24 (5.4) | 8 (3.6) | 326 (8.6) |
| BMI (kg/m2) | |||||
| <18.5 | 24 (1.4) | 58 (4.3) | 19 (4.2) | 8 (3.6) | 109 (2.9) |
| 18.5–24.9 | 482 (27.5) | 637 (47.0) | 222 (49.4) | 80 (35.9) | 1421 (37.6) |
| 25–29.9 | 520 (29.7) | 393 (29.0) | 125 (27.8) | 71 (31.8) | 1109 (29.4) |
| 30–34.9 | 350 (20.0) | 170 (12.6) | 52 (11.6) | 35 (15.7) | 607 (16.1) |
| 35–39.9 | 188 (10.7) | 59 (4.4) | 20 (4.5) | 17 (7.6) | 284 (7.5) |
| ≥40 | 174 (9.9) | 31 (2.3) | 7 (1.6) | 9 (4.0) | 220 (5.8) |
| Not available | 14 (0.8) | 7 (0.5) | 4 (0.9) | 3 (1.4) | 28 (0.7) |
| WHO performance status | |||||
| 0 | 1045 (59.7) | 815 (60.2) | 380 (84.6) | 130 (58.3) | 2370 (62.7) |
| 1 | 491 (28.0) | 409 (30.2) | 53 (11.8) | 63 (28.3) | 1016 (26.9) |
| 2 | 115 (6.6) | 87 (6.4) | 4 (0.9) | 19 (8.5) | 225 (6.0) |
| 3 | 18 (1.0) | 11 (0.8) | 0 (0) | 4 (1.8) | 33 (0.9) |
| 4 | 1 (0.1) | 1 (0.1) | 0 (0) | 2 (0.9) | 4 (0.1) |
| Not available | 81 (4.6) | 32 (2.4) | 12 (2.7) | 5 (2.2) | 130 (3.4) |
| CCI | |||||
| 0 | 200 (11.4) | 396 (29.2) | 270 (60.1) | 27 (12.1) | 893 (23.6) |
| 1 | 378 (21.6) | 340 (25.1) | 85 (18.9) | 40 (17.9) | 843 (22.3) |
| 2 | 477 (27.2) | 317 (23.4) | 35 (7.8) | 41 (18.4) | 870 (23.0) |
| 3 | 398 (22.7) | 199 (14.7) | 36 (8.0) | 46 (20.6) | 679 (18.0) |
| 4 | 196 (11.2) | 64 (4.7) | 13 (2.9) | 37 (16.6) | 310 (8.2) |
| 5 | 71 (4.1) | 28 (2.1) | 1 (0.2) | 19 (8.5) | 119 (3.2) |
| 6 | 23 (1.3) | 7 (0.5) | 6 (1.3) | 5 (2.2) | 41 (1.1) |
| 7 | 4 (0.2) | 2 (0.2) | 1 (0.2) | 6 (2.7) | 13 (0.3) |
| 8 | 3 (0.2) | 1 (0.1) | 1 (0.2) | 2 (0.9) | 7 (0.2) |
| 9 | 1 (0.1) | 1 (0.1) | 1 (0.2) | 0 (0) | 3 (0.1) |
| ASA grade | |||||
| 1 | 375 (21.4) | 392 (28.9) | 212 (47.2) | 33 (14.8) | 1012 (26.8) |
| 2 | 991 (56.6) | 729 (53.8) | 199 (44.3) | 131 (58.7) | 2050 (54.3) |
| 3 | 374 (21.4) | 221 (16.3) | 36 (8.0) | 56 (25.1) | 687 (18.2) |
| 4 | 8 (0.5) | 13 (1.0) | 1 (0.2) | 2 (0.9) | 24 (0.6) |
| 5 | 1 (0.1) | 0 (0) | 1 (0.2) | 0 (0) | 2 (0.1) |
| Not available | 2 (0.1) | 0 (0) | 0 (0) | 1 (0.5) | 3 (0.1) |
| FIGO Stage | |||||
| Not cancer | 57 (3.3) | 76 (5.6) | 57 (12.7) | 21 (9.4) | 211 (5.6) |
| 1/2 | 1406 (80.3) | 548 (40.4) | 339 (75.5) | 156 (70.0) | 2449 (64.8) |
| 3/4 | 255 (14.6) | 712 (52.6) | 53 (11.8) | 40 (17.9) | 1060 (28.1) |
| Not available | 33 (1.9) | 19 (1.4) | 0 (0) | 6 (2.7) | 58 (1.5) |
| Histology | |||||
| SCC | 22 (1.3) | 31 (2.3) | 310 (69.0) | 188 (84.3) | 551 (14.6) |
| Adenocarcinoma | 1554 (88.8) | 1030 (76.0) | 118 (26.3) | 9 (4.0) | 2711 (71.8) |
| GCST | 13 (0.7) | 106 (7.8) | 0 (0) | 3 (1.4) | 122 (3.2) |
| Other | 137 (7.8) | 34 (2.5) | 7 (1.6) | 17 (7.6) | 195 (5.2) |
| Benign/preinvasive/borderline | 21 (1.2) | 129 (9.6) | 14 (3.1) | 4 (1.8) | 168 (4.5) |
| Not available | 4 (0.2) | 25 (1.9) | 0 (0) | 2 (0.9) | 31 (0.8) |
Data are presented as total number (percentage). Details of operated vs non-operated group separately, are presented in Supplemental Tables 2 and 4.
ASA grade, American Society of Anaesthesiologists Physical Status Classification system; BMI, body mass index; CCI, Charlson Comorbidity Index; FIGO, International Federation of Gynaecology and Obstetrics; GCST, germ cell, sex cord stromal or trophoblastic tumors; NACT, neoadjuvant chemotherapy; SCC, squamous cell carcinoma; WHO, World Health Organization.
Fotopoulou. Gynecologic cancer surgery during the COVID-19 pandemic. Am J Obstet Gynecol 2022.
Six patients (0.1%) did not have a recorded cancer site and were excluded from this table.
Supplemental Table 2.
Demographics of patients did not undergo any operations (n=189)
| Uterus (n=60) | Ovary (n=104) | Cervix (n=13) | Vulva/vagina (n=12) | Total (n=189) | |
|---|---|---|---|---|---|
| Age (y) | |||||
| 17–19 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| 20–29 | 0 (0) | 5 (4.8) | 1 (7.7) | 0 (0) | 6 (3.2) |
| 30–39 | 3 (5.0) | 7 (6.7) | 1 (7.7) | 0 (0) | 11 (5.8) |
| 40–49 | 3 (5.0) | 19 (18.3) | 2 (15.4) | 0 (0) | 24 (12.7) |
| 50–59 | 13 (21.7) | 18 (17.3) | 3 (23.1) | 4 (33.3) | 38 (20.1) |
| 60–69 | 15 (25.0) | 27 (26.0) | 5 (38.5) | 2 (16.7) | 49 (25.9) |
| 70–79 | 12 (20.0) | 19 (18.3) | 1 (7.7) | 2 (16.7) | 34 (18.0) |
| 80–89 | 13 (21.7) | 9 (8.7) | 0 (0) | 4 (33.3) | 26 (13.8) |
| >90 | 1 (1.7) | 0 (0) | 0 (0) | 0 (0) | 1 (0.5) |
| Region | |||||
| Europe & Central Asia | 44 (73.3) | 64 (61.5) | 4 (30.8) | 11 (91.7) | 123 (65.1) |
| Latin America & Caribbean | 6 (10.0) | 6 (5.8) | 4 (30.8) | 1 (8.3) | 17 (9.0) |
| East Asia & Pacific | 0 (0) | 0 (0) | 3 (23.1) | 0 (0) | 3 (1.6) |
| South Asia | 1 (1.7) | 27 (26.0) | 0 (0) | 0 (0) | 28 (14.8) |
| North America | 5 (8.3) | 2 (1.9) | 0 (0) | 0 (0) | 7 (3.7) |
| Middle East & North Africa | 2 (3.3) | 5 (4.8) | 0 (0) | 0 (0) | 7 (3.7) |
| Sub-Saharan Africa | 2 (3.3) | 0 (0) | 2 (15.4) | 0 (0) | 4 (2.1) |
| Income group | |||||
| High | 49 (81.7) | 68 (65.4) | 4 (30.8) | 11 (91.7) | 132 (69.4) |
| Upper middle | 7 (11.7) | 6 (5.8) | 7 (53.9) | 1 (8.3) | 21 (11.1) |
| Low-middle | 4 (6.7) | 30 (28.9) | 2 (15.4) | 0 (0) | 36 (19.1) |
| BMI (kg/m2) | |||||
| <18.5 | 1 (1.7) | 3 (2.9) | 0 (0) | 0 (0) | 4 (2.1) |
| 18.5–24.9 | 14 (23.3) | 46 (44.2) | 6 (46.2) | 6 (50) | 72 (38.1) |
| 25–29.9 | 11 (18.3) | 30 (28.9) | 0 (0) | 2 (16.7) | 43 (22.8) |
| 30–34.9 | 13 (21.7) | 14 (13.5) | 5 (38.5) | 2 (16.7) | 34 (18.0) |
| 35–39.9 | 7 (11.7) | 4 (3.9) | 0 (0) | 1 (8.3) | 12 (6.4) |
| ≥40 | 11 (18.3) | 6 (5.8) | 2 (15.4) | 0 (0) | 19 (10.1) |
| Not available | 3 (5.0) | 1 (1.0) | 0 (0) | 1 (8.3) | 5 (2.7) |
| WHO Performance Status | |||||
| 0 | 20 (33.3) | 48 (46.2) | 7 (53.9) | 2 (16.7) | 77 (40.7) |
| 1 | 29 (48.3) | 37 (35.6) | 5 (38.5) | 8 (66.7) | 79 (41.8) |
| 2 | 9 (15.0) | 15 (14.4) | 1 (7.7) | 0 (0) | 25 (13.2) |
| 3 | 2 (3.3) | 2 (1.9) | 0 (0) | 0 (0) | 4 (2.1) |
| 4 | 0 (0) | 1 (1.0) | 0 (0) | 1 (8.3) | 2 (1.1) |
| Not available | 0 (0) | 1 (1.0) | 0 (0) | 1 (8.3) | 2 (1.1) |
| CCI | |||||
| 0 | 5 (8.3) | 31 (29.8) | 4 (30.8) | 0 (0) | 40 (21.2) |
| 1 | 9 (15.0) | 16 (15.4) | 1 (7.7) | 2 (16.7) | 28 (14.8) |
| 2 | 10 (16.7) | 24 (23.1) | 6 (46.2) | 3 (25.0) | 43 (22.8) |
| 3 | 12 (20.0) | 13 (12.5) | 1 (7.7) | 2 (16.7) | 28 (14.8) |
| 4 | 11 (18.3) | 13 (12.5) | 1 (7.7) | 2 (16.7) | 27 (14.3) |
| 5 | 5 (8.3) | 3 (2.9) | 0 (0) | 2 (16.7) | 10 (5.3) |
| 6 | 7 (11.7) | 4 (3.9) | 0 (0) | 1 (8.3) | 12 (6.4) |
| 7 | 1 (1.7) | 0 (0) | 0 (0) | 0 (0) | 1 (0.5) |
| ASA grade | |||||
| 1 | 6 (10.0) | 25 (24.0) | 4 (30.8) | 1 (8.3) | 36 (19.1) |
| 2 | 22 (36.7) | 57 (54.8) | 6 (46.2) | 6 (50.0) | 91 (48.2) |
| 3 | 28 (46.7) | 19 (18.3) | 3 (23.1) | 5 (41.7) | 55 (29.1) |
| 4 | 1 (1.7) | 2 (1.9) | 0 (0) | 0 (0) | 3 (1.6) |
| 5 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Not available | 3 (5.0) | 1 (1.0) | 0 (0) | 0 (0) | 4 (2.1) |
| FIGO stage | |||||
| Not cancer | 1 (1.7) | 5 (4.8) | 0 (0) | 3 (25.0) | 9 (4.8) |
| 1/2 | 45 (75.0) | 28 (26.9) | 12 (92.3) | 8 (66.7) | 93 (49.2) |
| 3/4 | 9 (15.0) | 70 (67.3) | 1 (7.7) | 1 (8.3) | 81 (42.9) |
| Not available | 5 (8.3) | 1 (1.0) | 0 (0) | 0 (0) | 6 (3.2) |
| Histology | |||||
| SCC | 0 (0) | 0 (0) | 13 (100.0) | 10 (83.3) | 23 (12.2) |
| Adenocarcinoma | 57 (95.0) | 86 (82.7) | 0 (0) | 0 (0) | 143 (75.7) |
| GCST | 0 (0) | 4 (3.9) | 0 (0) | 0 (0) | 4 (2.1) |
| Other | 2 (3.3) | 0 (0) | 0 (0) | 1 (8.3) | 3 (1.6) |
| Benign/preinvasive/borderline | 0 (0) | 4 (3.9) | 0 (0) | 1 (8.3) | 5 (2.7) |
| Not available | 1 (1.7) | 10 (9.6) | 0 (0) | 0 (0) | 11 (5.8) |
Data presented as total number (percentage) unless stated otherwise.
ASA grade, American Society of Anaesthesiologists Physical Status Classification system; BMI, body mass index; CCI, Charlson Comorbidity Index; FIGO, International Federation of Gynaecology and Obstetrics; GCST, germ cell, sex cord stromal or trophoblastic tumors; NACT, neoadjuvant chemotherapy; SCC, squamous cell carcinoma; WHO, World Health Organization.
Fotopoulou. Gynecologic cancer surgery during the COVID-19 pandemic. Am J Obstet Gynecol 2022.
Supplementary Table 3.
Summary of pandemic-related changes in care and outcomes at the last follow-up in non-operated patients by cancer type (n=189)
| Uterus (n=60) | Ovary (n=104) | Cervix (n=13) | Vulva/vagina (n=12) | Total (n=189) | P value | |
|---|---|---|---|---|---|---|
| Did not have surgery owing to the pandemic | 50 (83.3) | 87 (83.7) | 10 (76.9) | 11 (91.7) | 158 (83.6) | .802 |
| Operation cancelled owing to the pandemic | 9 (15.0) | 11 (10.6) | 2 (15.4) | 1 (8.3) | 23 (12.2) | .804 |
| Postponed owing to the pandemic | 28 (46.7) | 62 (59.6) | 8 (61.5) | 6 (50.0) | 104 (55.0) | .403 |
| Changed to nonsurgical treatment | 9 (15.0) | 9 (8.7) | 3 (23.1) | 2 (16.7) | 23 (12.2) | .344 |
| Managed by interventional radiologists | 1 (1.7) | 1 (1.0) | 0 (0) | 0 (0) | 2 (1.1) | .921 |
| Received neoadjuvant treatment | 5 (8.3) | 18 (17.3) | 2 (15.4) | 1 (8.3) | 26 (13.8) | .404 |
| Neoadjuvant treatments not given | 3 (5.0) | 3 (2.9) | 0 (0) | 0 (0) | 6 (3.2) | .683 |
| Longer neoadjuvant treatments | 1 (1.7) | 15 (14.4) | 0 (0) | 0 (0) | 16 (8.5) | .014 |
| Shorter neoadjuvant treatments | 1 (1.7) | 2 (1.9) | 0 (0) | 0 (0) | 3 (1.6) | .923 |
| Limited access to staging procedure | 0 (0) | 5 (4.8) | 0 (0) | 0 (0) | 5 (2.7) | .241 |
| Limited access to staging investigations | 0 (0) | 2 (1.9) | 0 (0) | 0 (0) | 2 (1.1) | .648 |
| Mortality | 2 (3.3) | 3 (2.9) | 0 (0) | 0 (0) | 5 (2.7) | .846 |
| Compositea | 6 (10.0) | 21 (20.2) | 5 (38.5) | 2 (16.7) | 34 (18.0) | .084 |
Data presented as total number (percentage). Multiple changes were reported for each patient when appropriate.
Fotopoulou. Gynecological cancer surgery during the COVID-19 pandemic. Am J Obstet Gynecol 2022.
A composite outcome of unresectable disease or disease progression, emergency surgery and death.
Supplemental Table 4.
Complication rates by COVID-19 status of patients who have received any operations (n=3784)
| Uninfected (n=3762) | COVID-19 (n=22) | P value | |
|---|---|---|---|
| Cancer site | |||
| Uterus | 1774 (46.4) | 7 (31.8) | .087 |
| Ovary | 1341 (35.7) | 14 (63.6) | |
| Cervix | 448 (11.9) | 1 (4.6) | |
| Vulva/vagina | 223 (5.9) | 0 (0) | |
| Age (y) | |||
| 17–19 | 13 (0.4) | 0 (0) | .266 |
| 20–29 | 92 (2.5) | 2 (9.1) | |
| 30–39 | 288 (7.7) | 0 (0) | |
| 40–49 | 581 (15.4) | 3 (13.6) | |
| 50–59 | 962 (25.6) | 4 (18.2) | |
| 60–69 | 974 (25.9) | 4 (18.2) | |
| 70–79 | 664 (17.7) | 7 (31.8) | |
| 80–89 | 182 (4.8) | 2 (9.1) | |
| >90 | 6 (0.2) | 0 (0) | |
| BMI (kg/m2) | |||
| <18.5 | 107 (2.8) | 2 (9.1) | .257 |
| 18.5–24.9 | 1413 (37.6) | 10 (45.5) | |
| 25–29.9 | 1105 (29.4) | 7 (31.8) | |
| 30–34.9 | 608 (16.2) | 0 (0) | |
| 35–39.9 | 283 (7.5) | 1 (4.6) | |
| ≥40 | 218 (5.8) | 2 (9.1) | |
| Not available | 28 (0.7) | 0 (0) | |
| WHO Performance Status | |||
| 0 | 2364 (62.8) | 7 (31.8) | .003 |
| 1 | 1006 (26.7) | 10 (45.5) | |
| 2 | 220 (5.9) | 5 (22.7) | |
| 3 | 33 (0.9) | 0 (0) | |
| 4 | 4 (0.1) | 0 (0) | |
| Not available | 135 (3.6) | 0 (0) | |
| CCI | |||
| 0 | 891 (23.7) | 5 (22.7) | .097 |
| 1 | 841 (22.4) | 2 (9.1) | |
| 2 | 869 (23.1) | 2 (9.1) | |
| 3 | 672 (17.9) | 7 (31.8) | |
| 4 | 308 (8.2) | 3 (13.6) | |
| 5 | 117 (3.1) | 3 (13.6) | |
| 6 | 41 (1.1) | 0 (0) | |
| 7 | 13 (0.4) | 0 (0) | |
| 8 | 7 (0.2) | 0 (0) | |
| 9 | 3 (0.1) | 0 (0) | |
| ASA grade | |||
| 1 | 1006 (26.7) | 6 (27.3) | .177 |
| 2 | 2046 (54.4) | 8 (36.4) | |
| 3 | 681 (18.1) | 7 (31.8) | |
| 4 | 23 (0.6) | 1 (4.6) | |
| 5 | 2 (0.1) | 0 (0) | |
| Not available | 4 (0.2) | 0 (0) | |
| FIGO stage | |||
| Not cancer | 2442 (64.9) | 11 (50.0) | .315 |
| 1/2 | 1050 (27.9) | 10 (45.5) | |
| 3/4 | 59 (1.6) | 0 (0) | |
| Not available | 211 (5.6) | 1 (4.6) | |
| Surgery performed | |||
| Pelvis/perineal | 2609 (69.4) | 15 (68.2) | .884 |
| Midabdominal | 558 (14.8) | 4 (18.2) | |
| Upper-abdominal | 318 (8.5) | 1 (4.6) | |
| Others | 277 (7.4) | 2 (9.1) | |
| Bowel surgery | |||
| No | 3633 (96.6) | 18 (81.8) | <.0001 |
| Yes | 129 (3.4) | 4 (18.2) | |
| Approach | |||
| Open | 2335 (62.1) | 18 (81.8) | .178 |
| Minimally-invasive | 1339 (35.6) | 3 (13.6) | |
| Converted | 83 (2.2) | 1 (4.6) | |
| Not available | 5 (0.1) | 0 (0) | |
| Postoperative stay (d) | 4 (2–6) | 8.5 (5–17) | .0001 |
| Postoperative complication | |||
| Any complications | 717 (19.1) | 14 (63.6) | <.0001 |
| Respiratory complications | 52 (1.4) | 6 (27.3) | <.0001 |
| Wound infection | 164 (4.4) | 4 (18.2) | .002 |
| Hemorrhagea | 129 (3.4) | 2 (9.1) | .147 |
| Ileus | 86 (2.3) | 3 (13.6) | <.0001 |
| Urinary tract infection | 74 (2.0) | 3 (13.6) | <.0001 |
| Wound dehiscence | 69 (1.8) | 2 (9.1) | .012 |
| Sepsis | 34 (0.9) | 3 (13.6) | <.0001 |
| Thromboembolism | 30 (0.8) | 0 (0) | .674 |
| Kidney injury | 27 (0.72) | 1 (4.6) | .037 |
| Other organ injury | 24 (0.6) | 1 (4.6) | .024 |
| Anastomosis leak | 7 (0.2) | 1 (4.6) | <.0001 |
| Cardiac arrest | 8 (0.2) | 0 (0) | .829 |
| Myocardial infarction | 4 (0.1) | 0 (0) | .878 |
| Stroke | 3 (0.1) | 0 (0) | .895 |
| Other complications | 233 (6.2) | 4 (18.2) | .021 |
| Mortality | 26 (0.7) | 4 (18.2) | <.0001 |
Data are presented as total number (percentage) or mean (interquartile range). For postoperative outcomes, data were collected at 30 days after the surgeries.
ASA grade, American Society of Anaesthesiologists Physical Status Classification system; BMI, body mass index; CCI, Charlson Comorbidity Index; FIGO, International Federation of Gynaecology and Obstetrics; WHO, World Health Organization.
Fotopoulou. Gynecologic cancer surgery during the COVID-19 pandemic. Am J Obstet Gynecol 2022.
Haemorrhage requiring blood transfusion.
Supplemental Table 5.
Comparisons of patients and outcomes who have received any operations by length of stay (<14 days vs ≥14 days; n=3772)a
| <14 d (n=3595) | ≥14 d (n=177) | Proportion ≥14 d | P value | |
|---|---|---|---|---|
| Age (y) | ||||
| 17–19 | 13 (0.4) | 0 (0) | 0/13 (0) | .034 |
| 20–29 | 92 (2.6) | 2 (1.1) | 2/94 (2.1) | |
| 30–39 | 281 (7.8) | 7 (4.0) | 7/288 (2.4) | |
| 40–49 | 563 (15.7) | 21 (11.9) | 21/584 (3.6) | |
| 50–59 | 929 (25.8) | 37 (20.9) | 37/966 (3.8) | |
| 60–69 | 919 (25.7) | 56 (31.6) | 56/975 (5.7) | |
| 70–79 | 622 (17.3) | 43 (24.3) | 43/665 (6.5) | |
| 80–89 | 170 (4.7) | 11 (6.2) | 11/181 (6.1) | |
| >90 | 6 (0.2) | 0 (0) | 0/6 (0) | |
| Income group | ||||
| High | 2634 (73.3) | 129 (72.9) | 129/2763 (4.7) | .888 |
| Upper middle | 652 (18.1) | 31 (17.5) | 31/683 (4.5) | |
| Low-middle | 309 (8.6) | 17 (9.6) | 17/326 (5.2) | |
| BMI (kg/m2) | ||||
| <18.5 | 100 (2.8) | 9 (5.1) | 9/109 (8.3) | .164 |
| 18.5–24.9 | 1349 (37.5) | 73 (41.2) | 73/1422 (5.1) | |
| 25–29.9 | 1058 (29.4) | 52 (29.4) | 52/1110 (4.7) | |
| 30–34.9 | 579 (16.1) | 27 (15.3) | 27/606 (4.5) | |
| 35–39.9 | 276 (7.7) | 6 (3.4) | 6/282 (2.1) | |
| ≥40 | 211 (5.9) | 8 (4.5) | 8/219 (3.7) | |
| Not available | 22 (0.6) | 2 (1.1) | 2/24 (8.3) | |
| WHO performance status | ||||
| 0 | 2293 (63.8) | 75 (42.4) | 75/2368 (3.2) | <.0001 |
| 1 | 947 (26.3) | 61 (34.5) | 61/1008 (6.1) | |
| 2 | 193 (5.4) | 31 (17.5) | 31/224 (13.8) | |
| 3 | 28 (0.8) | 5 (2.8) | 5/33 (15.2) | |
| 4 | 3 (0.1) | 1 (0.6) | 1/4 (25) | |
| Not available | 131 (3.6) | 4 (2.3) | 4/135 (3.0) | |
| CCI | ||||
| 0 | 869 (24.2) | 27 (15.3) | 27/896 (3.0) | .001 |
| 1 | 815 (22.7) | 28 (15.8) | 28/843 (3.3) | |
| 2 | 819 (22.8) | 49 (27.7) | 49/868 (5.7) | |
| 3 | 638 (17.8) | 37 (20.9) | 37/675 (5.5) | |
| 4 | 288 (8.0) | 21 (11.9) | 21/309 (6.8) | |
| 5 | 109 (3.0) | 9 (5.1) | 9/118 (7.6) | |
| 6 | 36 (1.0) | 4 (2.3) | 4/40 (10) | |
| 7 | 13 (0.4) | 0 (0) | 0/13 (0) | |
| 8 | 6 (0.2) | 1 (0.6) | 1/6 (14.3) | |
| 9 | 2 (0.1) | 1 (0.6) | 1/2 (33.3) | |
| ASA grade | ||||
| 1 | 980 (27.3) | 31 (17.5) | 31/1011 (3.1) | <.0001 |
| 2 | 1957 (54.4) | 89 (50.3) | 89/2046 (4.4) | |
| 3 | 632 (17.6) | 53 (29.9) | 53/685 (7.7) | |
| 4 | 21 (0.6) | 3 (1.7) | 3/24 (12.5) | |
| 5 | 2 (0.1) | 0 (0) | 0/2 (0) | |
| Not available | 3 (0.1) | 1 (0.6) | 1/4 (25) | |
| Cancer site | ||||
| Uterus | 1709 (47.5) | 34 (19.2) | 34/1743 (2.0) | <.0001 |
| Ovary | 1249 (34.7) | 104 (58.8) | 104/1353 (7.7) | |
| Cervix | 428 (11.9) | 21 (11.9) | 21/449 (4.7) | |
| Vagina/vulva | 203 (5.7) | 18 (10.2) | 18/221 (8.1) | |
| Not available | 6 (0.2) | 0 (0) | 0/6 (0) | |
| FIGO stage | ||||
| Not cancer | 205 (5.7) | 6 (3.4) | 6/211 (2.8) | <.0001 |
| 1 or 2 | 2384 (66.3) | 59 (33.3) | 59/2443 (2.4) | |
| 3 or 4 | 947 (26.3) | 112 (63.3) | 112/1059 (10.6) | |
| Not available | 59 (1.6) | 0 (0) | 0/59 (0) | |
| Lockdown stringency | ||||
| Full | 1819 (50.6) | 91 (51.4) | 91/1910 (4.8) | .006 |
| Moderate | 846 (23.5) | 57 (32.2) | 57/903 (6.3) | |
| Light | 829 (23.1) | 28 (15.8) | 28/857 (3.3) | |
| COVID-19 burden | ||||
| High burden | 2557 (71.1) | 90 (50.9) | 90/2647 (3.4) | <.0001 |
| Low burden | 961 (26.7) | 87 (49.2) | 87/1048 (8.3) | |
| Not available | 77 (2.1) | 0 (0) | 0/77 (0) | |
| Surgery performed | ||||
| Pelvis/perineal | 2521 (70.1) | 93 (52.5) | 93/2614 (3.6) | <.0001 |
| Midabdominal | 523 (14.6) | 39 (22.0) | 39/562 (6.9) | |
| Upper-abdominal | 304 (8.5) | 15 (8.5) | 15/319 (4.7) | |
| Others | 247 (6.9) | 30 (17.0) | 30/277 (10.8) | |
| Bowel surgery | ||||
| No | 3494 (97.2) | 145 (81.9) | 145/3639 (4.0) | <.0001 |
| Yes | 101 (2.8) | 32 (18.1) | 32/133 (24.1) | |
| Approach | ||||
| Open | 2190 (60.9) | 159 (89.8) | 159/2349 (6.8) | <.0001 |
| Minimally-invasive | 1324 (36.8) | 11 (6.2) | 11/1335 (0.8) | |
| Converted | 76 (2.1) | 7 (4.0) | 7/83 (8.4) | |
| Not available | 5 (0.1) | 0 (0) | 0/5 (0) | |
| Postoperative complication | ||||
| Any complications | 608 (16.9) | 120 (67.8) | 120/728 (16.5) | <.0001 |
| Respiratory complications | 35 (1.0) | 23 (13.0) | 23/58 (39.7) | <.0001 |
| Mortality | 20 (0.6) | 10 (5.7) | 10/30 (33.3) | <.0001 |
Data presented as total number (percentage) or proportion (percentage).
ASA grade, American Society of Anaesthesiologists Physical Status Classification system; BMI, body mass index; CCI, Charlson Comorbidity Index; FIGO, International Federation of Gynaecology and Obstetrics; WHO, World Health Organization.
Fotopoulou. Gynecologic cancer surgery during the COVID-19 pandemic. Am J Obstet Gynecol 2022.
Twelve patients (0.32%) did not have recorded length of stay. For postoperative outcomes, data were collected at 30 days after the operations.
Supplementary Data
References
- 1.Taylor A., Sundar S.S., Bowen R., et al. British Gynaecological Cancer Society recommendations for women with gynecological cancer who received non-standard care during the COVID-19 pandemic. Int J Gynecol Cancer. 2022;32:9–14. doi: 10.1136/ijgc-2021-002942. [DOI] [PubMed] [Google Scholar]
- 2.Wang Y., Zhang S., Wei L., et al. Recommendations on management of gynecological malignancies during the COVID-19 pandemic: perspectives from Chinese gynecological oncologists. J Gynecol Oncol. 2020;31:e68. doi: 10.3802/jgo.2020.31.e68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vecchione L., Stintzing S., Pentheroudakis G., Douillard J.Y., Lordick F. ESMO management and treatment adapted recommendations in the COVID-19 era: colorectal cancer. ESMO Open. 2020;5 doi: 10.1136/esmoopen-2020-000826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Royal College of Obstetricians and Gynaecologists; British Gynaecological Cancer Society Joint RCOG/BGCS guidance for care of patients with gynaecological cancer during the COVID-19 pandemic. 2021. https://www.bgcs.org.uk/covid-19/ Available at:
- 5.The National Institute for Health and Care Excellence Specialty guides for patient management during the coronavirus pandemic The United Kingdom. 2020. https://www.nice.org.uk/covid-19/specialty-guides Available at:
- 6.Ramirez P.T., Chiva L., Eriksson A.G.Z., et al. COVID-19 global pandemic: options for management of gynecologic cancers. Int J Gynecol Cancer. 2020;30:561–563. doi: 10.1136/ijgc-2020-001419. [DOI] [PubMed] [Google Scholar]
- 7.American Society of Clinical Oncology COVID-19 patient care information. 2022. https://www.asco.org/covid-resources/patient-care-info Available at:
- 8.Fader A.N., Huh W.K., Kesterson J., et al. When to operate, hesitate and reintegrate: Society of Gynecologic Oncology surgical considerations during the COVID-19 pandemic. Gynecol Oncol. 2020;158:236–243. doi: 10.1016/j.ygyno.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gultekin M., Ak S., Ayhan A., et al. Perspectives, fears and expectations of patients with gynaecological cancers during the COVID-19 pandemic: a Pan-European study of the European Network of Gynaecological Cancer Advocacy Groups (ENGAGe) Cancer Med. 2021;10:208–219. doi: 10.1002/cam4.3605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hanna T.P., King W.D., Thibodeau S., et al. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ. 2020;371:m4087. doi: 10.1136/bmj.m4087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leung E., Pervaiz Z., Lowe-Zinola J., et al. Maintaining surgical care delivery during the COVID-19 pandemic: a comparative cohort study at a tertiary gynecological cancer centre. Gynecol Oncol. 2021;160:649–654. doi: 10.1016/j.ygyno.2020.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.COVIDSurg Collaborative Effect of COVID-19 pandemic lockdowns on planned cancer surgery for 15 tumour types in 61 countries: an international, prospective, cohort study. Lancet Oncol. 2021;22:1507–1517. doi: 10.1016/S1470-2045(21)00493-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glasbey J.C., Nepogodiev D., Simoes J.F.F., et al. Elective cancer surgery in COVID-19-free surgical pathways during the SARS-CoV-2 pandemic: an international, multicenter, comparative cohort study. J Clin Oncol. 2021;39:66–78. doi: 10.1200/JCO.20.01933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glasbey J.C., Nepogodiev D., Simoes J.F.F., et al. Outcomes from elective colorectal cancer surgery during the SARS-CoV-2 pandemic. Colorectal Dis. 2021;23:732–749. doi: 10.1111/codi.15431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Confidential Enquiry into Patient Outcome and Death The NCEPOD Classification of Intervention. 2004. https://www.ncepod.org.uk/classification.html Available at:
- 16.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research Electronic Data Capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sammour T., Lewis M., Thomas M.L., Lawrence M.J., Hunter A., Moore J.W. A simple web-based risk calculator (www.anastomoticleak.com) is superior to the surgeon's estimate of anastomotic leak after colon cancer resection. Tech Coloproctol. 2017;21:35–41. doi: 10.1007/s10151-016-1567-7. [DOI] [PubMed] [Google Scholar]
- 18.Burnell M., Iyer R., Gentry-Maharaj A., et al. Benchmarking of surgical complications in gynaecological oncology: prospective multicentre study. BJOG. 2016;123:2171–2180. doi: 10.1111/1471-0528.13994. [DOI] [PubMed] [Google Scholar]
- 19.Kehoe S., Hook J., Nankivell M., et al. Primary chemotherapy versus primary surgery for newly diagnosed advanced ovarian cancer (CHORUS): an open-label, randomised, controlled, non-inferiority trial. Lancet. 2015;386:249–257. doi: 10.1016/S0140-6736(14)62223-6. [DOI] [PubMed] [Google Scholar]
- 20.Vergote I., Tropé C.G., Amant F., et al. Neoadjuvant chemotherapy or primary surgery in Stage IIIC or IV ovarian cancer. N Engl J Med. 2010;363:943–953. doi: 10.1056/NEJMoa0908806. [DOI] [PubMed] [Google Scholar]
- 21.Levitt E.B., Patch D.A., Mabry S., et al. Association between COVID-19 and mortality in hip fracture surgery in the national COVID cohort collaborative (N3C): a retrospective cohort study. J Am Acad Orthop Surg Glob Res Rev. 2022;6:e21. doi: 10.5435/JAAOSGlobal-D-21-00282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bruce S.F., Huysman B., Bharucha J., et al. Impact of the COVID-19 pandemic on referral to and delivery of gynecologic oncology care. Gynecol Oncol Rep. 2022;39 doi: 10.1016/j.gore.2022.100928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Altın D., Yalçın İ., Khatib G., et al. Management of gynecological cancers in the COVID-19 era: a survey from Turkey. J Turk Ger Gynecol Assoc. 2020;21:265–271. doi: 10.4274/jtgga.galenos.2020.2020.0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frey M.K., Ellis A.E., Zeligs K., et al. Impact of the coronavirus disease 2019 pandemic on the quality of life for women with ovarian cancer. Am J Obstet Gynecol. 2020;223:725.e1–725.e9. doi: 10.1016/j.ajog.2020.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen Z., Zhang C., Yin J., et al. Challenges and opportunities for ovarian cancer management in the epidemic of Covid-19: lessons learned from Wuhan, China. J Ovarian Res. 2021;14:35. doi: 10.1186/s13048-021-00784-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jacome L.S., Deshmukh S.K., Thulasiraman P., Holliday N.P., Singh S. Impact of COVID-19 pandemic on ovarian cancer management: adjusting to the new normal. Cancer Manag Res. 2021;13:359–366. doi: 10.2147/CMAR.S287152. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.