Abstract
Rationale
The COVID-19 pandemic has disproportionately impacted Black Americans. Inequities in systems and social determinants of health along with racial health disparities impact degree of pandemic preparedness.
Objective
In early pandemic stages, we aimed to explore: 1) state of pandemic preparedness; 2) effects of socio-ecological factors on preparedness; and 3) multi-level strategies to increase preparedness among uniquely, vulnerable Black American subgroups.
Methods
We conducted 62 in-depth interviews with Black American community members representing parents, individuals with underlying medical conditions, essential workers, and young adults. Based on the McLeroy's Model Ecological for Health Promotion, an inductive-deductive content analysis approach was used to analyze the interview data around the factors influencing preparedness on individual, interpersonal processes and primary groups, community/institutional, and public policy.
Results
Majority (56.5%) of the participants stated they were somewhat or very prepared. We identified four themes: 1) Lived Experiences during the COVID-19 Pandemic; 2) Challenges experienced during the COVID-19 Pandemic; 3) I would do this differently they say; 4) Changes Needed to Survive the Pandemic relate to Public Policy, Community/institutional factors, and Interpersonal processes and primary group(s). All participants described their adjustments to live in the new norm. Participants identified perceived challenges and solutions on multi-levels, driven by subgroup.
Conclusions
Pandemic response plans should use targeted strategies across multi-levels to enhance the preparedness of Black Americans, especially those in vulnerable groups. This could reduce the disproportionate COVID-19 disease burden exhibited by Black Americans and better prepare for future pandemics.
Keywords: COVID-19, Coronavirus disease, Preparedness, Black Americans, Public health emergency
1. Introduction
The COVID-19 pandemic has exposed the severity of biological threats and the vulnerability in preparedness plans globally (Khan et al., 2020). In the U.S., there have been over 62 million cases and 840,000 deaths as of January 12, 2022 (Centers for Disease Control and Prevention [CDC], 2022). Black Americans bear the burden of COVID-19 (Vasquez Reyes, 2020) with hospitalization and mortality rates being three and two times higher compared to White Americans (CDC, 2021b). During the Trump Administration, agenda-political factors of decision-makers and organizations, bureau-organizational factors such as policy failure (e.g., disbandment of disaster and preparedness unit), and psychological factors which can impact threat perception and decision-making in early pandemic stages exacerbated COVID-19 outcomes (Hanage et al., 2020; Parker and Stern, 2022). Pandemic preparedness is key to minimizing threats on health outcomes and existing disparities through: 1) reducing the spread of the biological threat, 2) providing personal protective equipment, 3) maintaining hospital capacity, and 4) ensuring acquisition of preventive tools (Alberti et al., 2020).
The long-standing history of inequities in our systems and social determinants of health along with disparities in chronic disease drive the unpreparedness of Black Americans (Hart et al., 2020; Satcher, 2011; Peek et al., 2021). Where these components intersect lies structural racism to create a system in which racial group inequity is perpetuated through policy, economics, community/organizational practices, cultural representations, and interpersonal dynamics (Yearby and Mohapatra, 2020, Churchwell et al., 2020). Therefore, unpreparedness is demonstrated through ones' instability in economics, poor access to COVID-19 education, and lack of access to or poor quality of care (e.g., testing, vaccines) (Ngepan, 2021; Yancy, 2020). It is further identified through an individuals’ social and community context (e.g., environmental exposures, multi-generational homes, stigma), and causes mistrust in the healthcare system, government, and researchers (Snowden and Graff, 2021; Ngepan, 2021; Yancy, 2020). This can lead to psychosocial stress which increases likelihood of COVID-19 and poor outcomes (Lee et al., 2021).
A comprehensive, multi-level response plan that centers equity is necessary to improve pandemic preparedness (Wilkins et al., 2021). Black Americans should be engaged in the development to ensure the communities are equipped with the necessary information, resources, capacities, and organizational systems (Williams and Cooper, 2020; Krouse, 2020; Alberti et al., 2020). This is especially important as certain subgroups (e.g., essential workers) are more vulnerable to unpreparedness (The Lancet, 2020; Mason et al., 2021; Lam et al., 2020). Pandemic preparedness plans have been re-enacted under Biden's administration and public health officials have offered strategies that center equity (Peek et al., 2021; Rusoja and Thomas, 2021; Alberti et al., 2020) Yet, few studies have sought to gain a comprehensive understanding of COVID-19 pandemic preparedness through the lens of uniquely vulnerable, Black American subgroups.
1.1. Socio-ecological model
Socio-ecological models have been widely applied to identify intervention targets (McLeroy et al., 1988; Lang et al., 2021; Mancera et al., 2017), including pandemic preparedness (McLeroy et al., 1988). Specifically, McLeroy's Model Ecological for Health Promotion is a public health framework that posits a behavior is determined by intrapersonal, interpersonal, institutional, community, and public policy factors. Individual factors involve the personal (e.g., knowledge, attitudes, behavior) and biological factors of an individual. Interpersonal processes and primary groups reflect close relationships, formal and informal (e.g., family, work group, friends). The institutional factors are social institution with organizational characteristics, and formal rules and regulations for operation, while community factors are the relationships among organizations and institutions. Last, public policy refers to laws and policies at the local, state, and national level (McLeroy et al., 1988). The assumption is that “health promotion interventions are based on our beliefs, understanding, and theories of the determinants of behavior, and that the five levels of analysis reflect the range of strategies available for health promotion programming” (McLeroy et al., 1988). Health promotion is a key to behavior, and in our case, is necessary to explore needs and strategies across these multi-levels to increase preparedness for the current and future pandemics.
Our qualitative study explores COVID-19 pandemic preparedness among vulnerable, Black American subgroups. We applied McLeroy's Model Ecological for Health Promotion to better understand the state of preparedness, along with challenges and strategies to inform pandemic response plans.
2. Methods
2.1. Study design and study setting
A phenomenological qualitative approach (Creswell, 2007) was chosen to explore the lived experiences and preparedness of vulnerable, Black Americans. In the U.S., there are approximately 332.5 million people and Black Americans comprise 13% of the population (U.S. Census Bureau, 2020). This study was conducted between May 2020 through September 2020 and approved by Meharry Medical College Institutional Review Board.
2.2. Sampling and recruitment
A purposive sampling method was used to recruit study participants (Creswell, 2007). Recruitment mechanisms were email, existing databases, word-of-mouth, and flyers. Participants were screened for eligibility. The inclusion criteria are: English-speaking, self-identified as Black American, over 18 years, and an essential worker (i.e., an individual whose services are necessary), parent (i.e., caregiver or legal guardian to a child), young adult (i.e., between 18 and 35 years), or an individual with an UMC. The exclusion criterion was all individuals who do not meet inclusion criteria. Individuals who identified in more than one subgroup were asked to address questions from the subgroup assigned upon study entry.
2.3. Interview protocol development
The interviewer protocol sought participants' preparedness for the COVID-19 pandemic. We asked about their lived experiences, perceived degree of preparedness, challenges, and changes needed on multi-levels to increase preparedness (See Appendix). Protocol topics were loosely mapped to constructs of McLeroy's Model Ecological for Health Promotion, allowing us to understand relevant questions for each construct while exploring emerging issues.
2.4. Procedures
Three trained medical students and two trained researchers conducted the interviews. To screen for eligibility, participants were sent a link using REDCap (Harris et al., 2009). After providing verbal consent, participants interviews lasted between 45 and 90 minutes, pending on their lived experiences. One individual conducted each interview, and another person took notes. Participants were compensated a $30 e-gift card. All sessions were audio-recorded and transcribed using Zoom. Then, the team checked for accuracy. Transcripts were assigned unique identification numbers.
2.5. Analysis
Descriptive statistics (i.e., frequencies, percentages, and cross-tabulations) were conducted using SPSS vs 26. Data were analyzed by one PhD level researcher and one medical student. Using the questions and a preliminary review of five transcripts per group, a hierarchical coding system was developed by the last author. Then each coder used the system to independently code five transcripts, compare codes, and add or remove codes. This established reliability in the coding system. Each coder continued to use the system to code all transcripts independently. Coding saturation was met when no new codes emerged. Each coder reviewed the codes, identified differences, and resolved via consensus. Then coders performed axial coding, placing codes into categories based on their group and then by constructs of McLeroy's Model Ecological for Health Promotion. In our analyses, we combined codes related to community and institutional factors for data presentation. Inductive-deductive thematic analysis occurred through the constant comparison of codes, and identification of themes. Verification procedures were investigator triangulation, intercoder reliability, and thick, rich description (Creswell, 2007).
3. Results
Semi-interviews were conducted with 62 Black Americans including 16 parents, 16 essential workers, 15 individuals with UMCs, and 15 young adults. The majority (56.5%) stated they were somewhat or very prepared. Because we used mass recruitment, we were unable to capture response rates. See Table 1 for demographics by level of preparedness. There were no significant differences by degree of preparedness and socio-demographics (See Table 2 for examples of interview intercepts by themes and groups).
Table 1.
Socio-demographics by level of preparedness, N = 62.
| Unprepared (n = 27) |
Prepared (n = 35) |
|||||
|---|---|---|---|---|---|---|
| Mean | Standard Deviation | Mean | Standard Deviation | |||
| Age | 37.7 | 13.3 | 42.5 | 14.5 | ||
| N | % | N | % | Χ2 | p-value | |
| Gender | 0.501 | 0.479 | ||||
| Male | 7 | 25.9 | 12 | 34.3 | ||
| Female | 20 | 74.1 | 23 | 65.7 | ||
| Education | 0.050 | 0.822 | ||||
| Some College or less | 10 | 37.0 | 12 | 34.3 | ||
| Associates Degree or higher | 17 | 63.0 | 23 | 65.7 | ||
| N | % | N | % | H | p-value | |
| Category | 2.107 | 0.147 | ||||
| Essential Worker | 5 | 18.5 | 11 | 31.4 | ||
| Underlying Medical Condition | 5 | 18.5 | 10 | 28.6 | ||
| Young Adults | 9 | 33.3 | 6 | 17.1 | ||
| Parents | 8 | 33.3 | 8 | 22.9 | ||
| Income | 0.403 | 0.526 | ||||
| Less than $40,000 | 9 | 33.3 | 11 | 31.4 | ||
| $40,001-$80,000 | 5 | 18.5 | 12 | 34.3 | ||
| Over $80,000 | 8 | 29.6 | 8 | 29.6 | ||
| Do not want to answer | 5 | 18.5 | 4 | 18.5 | ||
Table 2.
Examples of interview excerpts by themes and group.
| Theme | Category | Quotation |
|---|---|---|
| Theme 1: Lived Experiences during the COVID-19 Pandemic | Essential Worker | “So I have a [great] friend, he didn't understand why you know in the job where he worked. They didn't have any form of social distancing in place, and he contracted the virus. And as I was talking to him he was telling me I don't have any taste. I can't smell it. I just feel so drained. And he had to isolate himself. I got to see a picturesque idea of what actually covid actually looked like.” |
| Parent | “It's been difficult, I actually lost two aunts. And the worst part about it was not being able to grieve as a family and collective home. And we're still not to the point where we even had an opportunity to come together and celebrate life. … It's difficult because you know that it's happened when you originally or initially hear about it. It's devastating. But then you get to go into this fantasy world or this island of denial. You know, it makes it easier to not accept …” | |
| Young Adult | “Yeah, it's really hard for everybody to be at home. It's just the routine changed the impact on my family. So there are four people in my household … I have an 11-year-old and a seven year old. So it's like they're old enough to kind of do their own thing for a while. But coming back together you know we had to find new ways to live and exist even together … you know, building tolerance levels, having more patience.” | |
| Individuals with Underlying Medical Conditions | “So for me It really freaked me out in the sense that knowing especially my father had it, that I might not see him again … I tried to get it to him and I asked, his wife to make sure that he takes it. I talked to him daily to force him to try to eat because he would not eat. I was really worried and nervous that I was going to get a call, stating that you know he was on a ventilator or that he died or something like that.” | |
| Theme 2: Challenges experienced during the COVID-19 Pandemic | Essential Worker | “It's become more challenging to say the least, because in our field, people still demand and depend on electricity. … we still have to abide by our safety policies. Now, we have to take on the Covid-19 policies so you take a lineman who's working outside you know in hundred degree weather who already have long sleeves and you tell him to wear a mask while he's working outside. You know you're putting them in a greater risk where they can dehydrate pass out, have heat exhaustion or a heat stroke. It's been tough from a professional standpoint.” |
| Parent | “It's an expensive virus when one gets it. It's an expensive virus to prepare for or to try to prepare for. Your thing's shut completely down if the food supply for any reason is cut or the window closes where you can't get groceries when you want them or need them … And then when you throw in, you know, all the black men been getting killed on TV, when you throw in those murders and what not, coupled with this invisible killer, you got the killer. We do see the police, then you've got the killer. We don't see this virus. So it's been like, is this real is this really real?” | |
| Young Adult | “So we went to a spring break, and then we're supposed to come back from spring break is when the university announced that we were going online. As well. Okay, cool. Like, I don't have to go inside, you know, have to drive across the city, but it's definitely proven to be a challenge. I think that my actual department has tried their best to be Mindful of that and like how students learn and I think that the university has tried to keep us up to date, but I think they were just lagging. There is still a lot of uncertainty.” | |
| Individuals with Underlying Medical Conditions | “I've always been a more outside person. I love to travel … And so actually I've been mostly, like 90%, in my house since March 10. And that's very unlike what I do, or normally do, I tend to like to go out, and take my kids out to different places. But because I'm a lot more at risk, I just kind of was basically shut in. And that took a toll or is constantly taking a toll on you know, my mental health.” | |
| Theme 3: I would do this differently they say …. | Essential Worker | “I will most definitely stock up on cleaning products. Most definitely. And cleaning products. I would say I would save more. And I've always been a saver.” |
| Parent | “You know, people have those emergency kits in case of bad weather and things of that nature? I would definitely keep an emergency kit with cleaning supplies I will definitely keep stashes of cleaning supplies, stashes of masks and gloves, stashes of non-perishable foods, things of that nature. I was never one of those, you know, end of the world bunker mentality people but it kind of makes sense now.” | |
| Young Adult | “Keep the steps I've already taken while adding in growing and investing in stocks, crypto, whatever it is to make you a crap ton of money and put it away for saving. So if something like this happens again, financially you will not be burdened.” | |
| Individuals with Underlying Medical Conditions | “Probably stocked up more on food supplies, you know, had one known and cleaning supplies had, you know, had one known. The necessary gear like the gloves, and the sanitizers, and the facemasks, making sure we're properly prepared for that as well.” | |
| Theme 4: Changes Needed to Survive the Pandemic relate to Public Policy, Community/institutional factors, and Interpersonal processes and primary group(s) | Essential Worker | “Yeah, I think government they just need to be honest. I just feel like everybody's campaigning for something and it has nothing to do just solely with the coronavirus but its just to get the next person in office. So we'll say whenever we can. We've lost so many people to the coronavirus, and it's just so sad. Like, where's the compassion. Like think about that and then just be totally honest, transparent, what's really happening so that we can deal with this as a whole society. And as far as schools like teachers and Gosh so many people just don't necessarily want to be at work, but have to be a work and they put their lives on line and health care workers too.” |
| Parent | “They might be handling it better than some other places but nowhere near as well as you would hope the National Institutes of Health would handle it. But the good thing they did was they installed hand sanitizer dispensers. I mean, they're all over the building like everywhere all so that's probably the best thing that they did. And I say, handing out masks. When you come in. Those are the two measures that they really took but they could have done much better.” | |
| Young Adult | “State officials and stuff, sit (expletive) down and stop putting everything into the media right away until you truly know every single last piece of information to the state officials again stop instilling fear into people. There's a way to deliver something to get people to understand without putting fear in them.” | |
| Individuals with Underlying Medical Conditions | “. I kind of feel like You know, there needs to be a bigger stance on requiring people to do what is necessary to come back the virus, New York. They did a great job in And making sure that the virus was contained and you know getting everything under control. But then, Georgia. Instead of following suit what New York was doing, they decided to do their own thing and allowed you know for the virus to get worse here in Georgia. So I just kind of wished it they would make more of a mandate nationwide to combat the whole thing.” |
3.1. Theme 1: Lived experiences during the COVID-19 pandemic
Participants who were prepared were aware of the virus' potential to spread, and had trusted information sources (i.e., jobs, child's school, friends in STEM/medical careers). They had a stockpile of essentials, limited or full access to healthcare, savings and/or multiple incomes, or had a childcare plan (i.e., remote job or family/friends assistance). Many who had access to essentials ensured relatives and friends had the items needed to survive and protect themselves. Those who were unprepared described dissimilar experiences. Participants highlighted living the unknown, a public health pandemic on top of a racial pandemic, changing of lifestyle behaviors, and experiences of COVID-19 diagnoses. We briefly describe the experiences of those unprepared.
Living the Unknown. Participants perceived the pandemic was “surreal” and initially believed it would be “short-lived” (e.g., one week). Participants described how major life events (e.g., having a baby, graduation, prom, funerals) were missed or few attendees, physically distanced, or spent alone. Living in the pandemic with no end in sight invoked fear, and many were “mentally unprepared” of the “impact on our country and all over the world”. Many were unsure if they were engaging in proper behaviors daily to protect their family from COVID-19.” Participants, especially essential workers and individuals with UMCs, even discussed the idea of preparing a will as they perceived they would not survive a COVID diagnosis. A few participants across each group indicated a vaccine was needed; however, many lacked trust in the government, pharmaceutical companies, and researchers due to Operation “warp speed” and historical abuses in research. Last, the inability to retrieve essentials, lack or limited money, and the inability to see family or friends created “anxiety” for many participants and caused them to question pandemic survival.
“Public health pandemic on top of a racial pandemic”. Many participants described the uneasiness and inequities in living in a public health pandemic during a racial pandemic. Many perceived the racial pandemic prepared them and their children for the COVID-19 pandemic. They felt they “grew up in the third world, so you've always been prepared. … Yeah, every, every day, every day is like a pandemic.” Minority-owned business owners described their inability to receive loans to survive the pandemic. Young males expressed fear in mask wearing since they are a perceived threat in society. Parents with sons were not prepared to discuss racism (e.g., incidences like George Floyd), and how to properly wear face masks and stay safe. Last, parents describe the inequities in the school systems with many Black American children getting “left behind”. Parents emphasized the lack of funding investment by the government to equip schools and students with digital technology, trained teachers, and proper safety measures (e.g., cleaning, provide face masks). This led some parents to homeschool their children.
Face-to-Face with COVID-19. Many participants described a COVID-19 experience, personally or with loved ones or co-workers. Experiences range from being asymptomatic to death, sparking fear in participants. If someone died from COVID-19, participants further described their grieving process as being “a fantasy world” or “island of denial” due to the physical distancing. These experiences provided a “picturesque idea of what COVID actually looked like.” Essential workers and parents further described how COVID-19 diagnoses among workers at jobs and childcare facilities caused businesses to suffer financially or shut down, creating duress.
Changing lifestyle behaviors. A major lifestyle change was how participants “interact and engage socially” with family, friends, and co-workers daily. Most participants attempted to avoid individuals who were not physically distancing and large crowds (e.g., grocery stores, churches, and clubs). Some cleaned excessively especially essential workers due to perceived high-risk and wanting to protect their “loved ones”. Essential workers described their jobs either being prepared by providing proper protective equipment (PPE) or having little-to-no PPE. Young adults, particularly college students, shared experiences of being in constant interaction with peers or co-workers with few preventive measures against COVID-19. Individuals with UMC perceived they became “prisoners” in their homes to ensure their safety. Parents were now learning technology, and how to do their jobs and homeschool their children due to fear or closure of schools or daycare. Children were adjusting to the new norm of limited-to-no socialization with peers, interacting with a “computer screen” if school-aged, and missing life events (i.e., birthdays, proms). Last, participants discussed improved or worsened eating habits and/or physical activity.
3.2. Theme 2: Challenges experienced during the COVID-19 pandemic
Multi-level challenges during the COVID-19 pandemic are described below.
Public Policy. Participants expressed the inactivation of the pandemic response plan led to several issues. They highlighted poor communication from national leaders, creating confusion and fueling mis- and dis-information on COVID-19 and the vaccines. This left many feeling the pandemic was too politicized. Poor promotion of community mitigation of viral spread (e.g., mask use and physical distancing) and the silencing of public health officials was a major concern. Participants further perceived policies were not implemented at the national, state, or local levels to address the health emergencies especially in minority communities which reflected the American people not engaging in proper preventive actions. Many, especially individuals with UMCs and parents, further perceived the healthcare system was not ready to respond. This reflected the government not providing personal protective equipment (PPE) and supplies (e.g., ventilators). Similarly, essential workers felt the government did not enforce workplace safety and provide PPE. Parents were concerned of the inequitable response in education to ensure children maintained their educational opportunities and achievements. Almost all participants indicated the economic response “stimulus” disbursements were not enough and were inequitably distributed. Among young adults, many perceived they were overlooked in the policy decisions especially since they were dependents under their parents with no access to federal funding (i.e., stimulus) and/or healthcare. Overall, participants felt overwhelmed with lack of support from the national, state, and local governments.
Community and Institutional Factors. All participants expressed unpreparedness of community institutions and organizations. There were lack of pandemic response plans and many resisted updating workplace safety standards to protect employees. For example, some participants highlighted few required face masks and physical distancing, leading to high COVID-19 rates. Many community institutions closed due to the economic “hit”, which led some participants being furloughed or job loss. There were food and PPE shortages, with many perceiving “grocery stores should have been more prepared.”
Parents described how schools scrambled to format their curriculum for Zoom lectures to institute stay-at-home policies to keep students safe. While some schools were able to provide parental assistance, other districts were unable to adapt to remote learning, lacked skilled and “ready” teachers for remote learning, and were unable to provide computers and hotspots. They further described absence of their child's teacher on the virtual platform at times. This made inequities in education more apparent. Among college students, there was an issue of colleges not being prepared to conduct remote learning and proper sanitation stations.
Participants described the unpreparedness of their jobs although some were perceived more adaptable. Particularly, essential workers discussed how they had to continue working without or little provision of the proper PPE, despite COVID-19 exposures, poor physical distancing protocols, and lack of sanitation stations. Some further described their requirement to work with COVID-19 symptoms until providing a positive test. This was because jobs did not: 1) offer sick leave; 2) prioritize workplace safety; and/or 3) emphasize health over labor shortage. Last, participants described how medical homes were not equipped for telehealth visits and were cancelling upcoming visits, particularly essential workers, individuals with UMC, and parents. Some participants with UMCs further perceived their doctors were either trying to make money by forcing them to keep doctors’ appointments and placed them at risk by not offering telehealth visits.
Last, the lack of education by scientists and healthcare providers on the current science around SARS-CoV-2, COVID-19, and future developments (e.g., vaccines, drugs) was commonly cited. While key scientists such as Dr. Fauci was considered reputable for some, participants were disappointed that scientists were not more engaged with communities. Collectively, these challenges caused mental health issues among some participants, and in some cases, tension in the community institutions.
Interpersonal Processes and Primary Groups. Almost all participants, especially those with UMCs, perceived the pandemic isolated them from family and friends, negatively affecting their mental health. Families were unsure of how to manage home life, especially being overworked, adjusting to working from home, and ensuring their children had a proper education. They also mentioned the strain of being together continuously during lockdown. Many parents discussed their inability to teach the children the material offered by the schools, or the issues with doing their job and assisting their children with their work. Some parents even highlighted the issues in maintaining food security, describing the financial burden to ensure their children were fed daily, a resource provided by schools. Furthermore, participants especially individuals with UMCs and parents expressed the need for improved communication between healthcare professionals and their patients to learn about COVID-19 and improve or ensure maintenance of health. Last, many felt their family and peers did not respect the prevention guidelines, spread misinformation, and lacked empathy, placing them and their families at risk.
Individual factors. Unemployment, financial disarray, limited access to necessities (e.g., food) and healthcare, and the mental toll of isolation during the lockdown were major issues. Other issues included lack of exercise or health food options to prepare the body for a possible COVID-19 diagnosis. A few participants further highlighted how people in marginalized communities like themselves live “check-to-check” or do not make enough to care for themselves and/or their families with the pandemic exacerbating these issues. They were less likely to get and/or understand pandemic-related information or able to adapt to the necessary changes (i.e., buying PPE, physical distance in multi-generational homes). Furthermore, they have limited access to care, especially if experienced job loss. Essential workers felt they were faced with a dilemma, choosing work and placing their families at-risk or staying home to experience unemployment. In addition, they expressed frustration with repeat COVID-19 tests which caused discomfort and their insurance being charged or the fact they were not required to test often due to workplace requirements. Young adults did not perceive they had many challenges except for the financial adjustment (i.e., job loss, little-to-no savings, or healthcare) or the inability to see family due to not physical distancing. Last, parents described the mental distress on their children, having to adjust to isolation or minimal interaction with peers and the new way of learning remotely.
3.3. Theme 3: I would do this differently, they say … (Individual)
The most commonly cited change was stocking up on essential products (e.g., food, cleaning supplies, masks, hand sanitizer). Additional changes, especially among young adults and essential workers, were taking the pandemic more seriously and engaging in preventive behaviors (I.e., face mask wearing, physical distancing, getting a primary care doctor or keeping appointments, eating healthier). In addition, participants stated they would be more proactive in watching the news or internet for updates from scientific experts about the disease and prevention (e.g., vaccines and behaviors). Being information sources to family and friends was important to many participants. Some even discussed how they would not take life for granted and spend more time with loved ones, especially among parents. A notable change parents mentioned was teaching their children to be “more clean and cautious”, including wearing masks, hand sanitizing, and “covering cough's”. A few parents also highlighted the need for technology training to virtually homeschool their children and work remote.
The idea of multiple income sources was common among parents and young adults. A few young adults stated they will begin investing in stocks to financially prepare for future pandemics. Parents stated they would start their own businesses. However, many young adults and individuals with UMCs stated they would not change anything. For example, those with UMC were already engaging in preventive behaviors daily and a few stated they would continue to rely on God to protect them. Most young adults did not believe they could prepare for a pandemic. Participants that were representative of marginalized communities emphasized they cannot prepare for pandemics especially the associated financial burden (e.g., job loss, increased supply cost such as food and masks, health care expenses). Last, many perceived community members like themselves should help in decision-making or advocating to ensure these groups receive resources to survive the pandemic.
3.4. Theme 4: Changes needed to survive the pandemic relate to public policy, community/institutional factors, and interpersonal processes and primary group(s)
Participants described several changes they perceived needed to occur across the multi-levels to survive pandemics. We briefly describe these changes.
Public Policy. All participants highlighted the need for the government to take the pandemic “seriously”, investing in and providing consistent, accurate, and ongoing communication on COVID-19 and access to the necessary preventive PPE (e.g., masks, tests). They also perceived the need for a coordinated response across all levels of government and key stakeholders (e.g., healthcare workers, employers, educators). Young adults wanted the government to stop putting the US population in fear through their messaging and providing misinformation. Participants further suggested the reactivation of the pandemic response plan and listening to top science experts and community to inform those plans. The need for mandates to wear face masks was commonly cited across participants. In addition, participants perceived government officials should lead by example in following recommendations (e.g., wearing masking, physical distancing). Additional suggestions by young adults were providing and enforcing guidelines for travel.
For economics, majority of participants wanted the national government to better distribute and regulate funds distributed to hospitals and small businesses. They, especially young adults, perceived a better plan was needed for those unemployed and the stimulus checks should be better regulated since many were still working and “collecting checks”. Participants suggested unlinking insurance with jobs since many were without insurance once unemployed and provision of education around insurance options. Parents stated the national government should invest more funds into education while ensuring its’ equitable distribution to ensure safety and proper education for students across different economic backgrounds. Young adults, especially those in college, requested economic policies that addressed their needs, especially if furloughed or did not receive a stimulus package since they were dependents of their parents. Some even suggested “rent and mortgage freezes” and increased minimum wage.
Community and Institution. Participants wanted all community institutions including providers, community organizations, and schools to collaborate and conduct communication campaigns on COVID-19, preventive measures, and resources (e.g., healthcare services, food banks) including “online tools with ads and videos”. They perceived all institutions should be equipped with sanitation stations, and enforce preventive behaviors (i.e., face masks and physical distancing). If community institutions are providers for consumers (e.g., grocery stores, pharmacies), plans should ensure essentials and a resource directory are available.
Schools. Parents highlighted schools needed equitable pandemic plans (e.g., distribution of computers with hotspots) to prepare for future outbreaks. Plans should ensure all schools can revert to remote learning with educators and parents being trained to use technology and effective strategies to engage children of all ages. They should also ensure the safety of teachers and students-sanitation throughout the day, physical distancing when possible, and the provision of masks and hand sanitizers. School administrators should then effectively communicate these plans to the teachers, parents, and students. Parents who had children in summer camps/daycares expressed similar measures should be taken. Last, young adults stated colleges need pandemic response plans including conversion of in-person classes to online, physical distancing, and sanitation stations.
Healthcare Providers. Most participants cited a pandemic plan is needed by healthcare providers to be able to act promptly. Continual updates should be given to patients to help navigate the healthcare system and the pandemic in general. Transparency in updates are necessary even if it is “I do not know”. Participants with UMCs perceived telehealth visits should be immediately available or plans that promote “safety” during visits. Few parents perceived cancelled or shortened appointments with their child's provider was unacceptable, and alternative strategies for engagement should be available. Most suggested “stepping up” on cleanliness to prevent COVID-19 transmission. Young adults stated providers could offer more immune-building strategies to prepare for a possible COVID-19 diagnosis.
Employers. The need for new or improved workplace safety standards was cited by most participants. Continual cleaning of workplaces, sanitation station availability, and the enforcement of face masks were recommended especially by those with UMCs, essential workers, and parents. Due to the nature of their jobs, essential workers perceived employers should require COVID-testing daily, physical distancing when possible, and face mask use. Participants, especially young adults and essential workers, perceived employers should have better sick pay, or not take away paid time off for those with COVID-19. Parents and those with UMCs emphasized the need to implement work from home policies which ensures safety for employers and children. This would address those with UMCs fearing COVID-19 exposure and parents dealing with daycare and school closures. Essential workers with children perceived employers should be more understanding, demonstrate gratitude, and shut down if needed. However, essential workers did recognize that institutions are different, policies will vary, and their jobs were needed.
Scientists and Pharmaceutical Companies. Participants, especially essential workers and those with UMCs, stressed the need for scientists to be more active in pandemic response. Specifically, they need to communicate continually on the public health issue (i.e., SARS-CoV-2), the transmission, and solutions (e.g., vaccines, face mask use). They “don't need to make people feel intimidated or be cocky”. Particularly, participants felt honesty and transparency were important and state their limitations in knowledge when unsure of community questions. Some even felt they should have been in the community prior to the pandemic to educate on science and to build trust so that they would have been more prepared to respond to the pandemic and the community would be more apt to accept recommendations. However, participants with UMCs perceived scientists should have been more prepared or aware of this issue to ensure an effective response. Pharmaceutical companies should make medications more affordable, especially to those who are unable to work.
Interpersonal processes and primary groups. Most participants perceived their peers should take the pandemic more seriously and be considerate of others. Particularly, they emphasized the need for peers to be prepared to follow guidelines such as physical distancing or being around the same people consistently and wear masks. Parents further emphasized the need for their peers to be more trusting and listen to the experts. Last, the idea of being empathetic towards others and their situations (e.g., those with UMCs) were commonly mentioned.
4. Discussion
Pandemic preparedness is complex, yet a necessary process to have an effective response, especially for vulnerable groups (CDC, 2021a) We believe we are the first to understand the experiences and preparedness of uniquely, vulnerable Black American subgroups during the early phase of the COVID-19 pandemic. While over half of participants indicated they were somewhat or very prepared, it was unsurprising for essential workers and individuals with UMCs to report greater levels of preparedness due to the emphasis placed on protecting these populations in early pandemic stages (The Lancet, 2020; Kompaniyets et al., 2021; Hanage et al., 2020; Elbeddini and Tayefehchamani, 2021).
4.1. Lived experiences
Participants described their COVID-19 lived experiences while living in the U.S. with existing inequities in systems and social determinants that are deeply rooted in structural racism (Bailey et al., 2021). Similar to studies on past and current pandemics (Steelfisher et al., 2010; Hanage et al., 2020), our data highlighted the poor, inequitable COVID-19 response of the government. As a result, many experienced the loss of a family member, friend, or co-worker. Some, particularly parents of young boys and young adult males further lived in fear and was not prepared to discuss and face race-based social identity threats by community and police. Kahn and Money confirmed these findings with social identify threat leading to lower face mask usage among Black Americans (Kahn and EEL, 2021). In addition, the lack of or limited information around the virus and preventive behaviors fueled mis- and dis-information. Participants further perceived this trickled down to poor communication by communities and organizations. This is a common concern across emergency preparedness efforts (Fineberg, 2014). Because effective communication is vital during a pandemic (Cowper, 2020) and those with limited access to care are less likely to receive information (Vaughn and Tinker, 2009), plans should be informed using various stakeholders including community members.
4.2. Challenges during pandemic
Using the McLeroy's Model Ecological for Health Promotion, we found that factors on multi-levels interplay and influence perceived preparedness differently among Black American subgroups, which is critical in informing pandemic response plans. Our study demonstrated over half of individuals across groups were prepared (e.g., access to supplies, healthcare, jobs, and/or family/peers for childcare). However, almost all individuals across groups described the inequitable distribution of resources at the societal level, which yielded different insights on their ability to prepare. Essential workers are key to the critical functions of the U.S., and are primarily Black American and Latino with many left unprotected and unprepared during the pandemic especially in early stages (CDC, 2020). Our data confirmed these findings with many essential workers describing little to no PPE along with poor workplace safety, PTO benefits, and healthcare coverage. Many young adults, a vulnerable group (Son et al., 2020), are less prepared today for adulthood than previous generations (Twenge and Park, 2019). Many take risks due to experiencing their freedom from moral supervision of parents (Scneider and Morris, 1991), and they lack or have limited education, financial and social support, and healthcare access (Arora et al., 2015) This situation is evident in our study with young adults engaging in high-risk COVID behaviors (e.g., poor physical distancing and face mask use) and their cited need for financial support from the government.
Another significant issue that emerged in our data is the inequitable school funding systems, in which less state and local funding is received by 45 percent of high-poverty schools (US Department of U.S. Department of Education, 2021). This fueled parental discussion around the inequities in remote learning from lack of provision of technology to untrained teachers along with food insecurity and inability to teach school lessons. This important finding encourages a deeper review of school funding policies and re-distribution of funds to ensure “no child get's left behind”. Many individuals with UMCs cite they were prepared. Yet, similar to past studies (Elbeddini and Tayefehchamani, 2021), our findings did demonstrate the pandemic, in some cases, limited or removed healthcare access and some of the activities they used to cope with their situations (e.g., socialization, exercise). Collectively, these barriers, especially healthcare access, are considered the greatest threats to the individual (e.g., mental stress, financial loss, multi-generational homes, no childcare) along with family, community, and national security (Satcher, 2011). These findings suggest that preparedness response plans should be targeted across groups and their context.
4.3. Multi-level strategies to increase preparedness
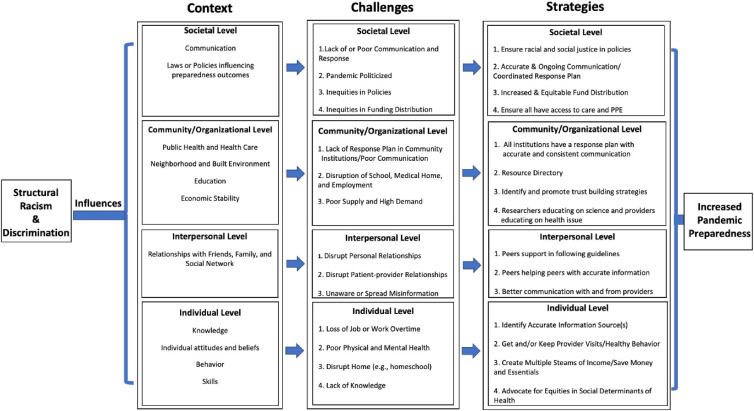
Identifying interventions on multi-levels targeting hard-to-reach populations is essential Black Americans is important (Vlahov et al., 2007). However, it is the change in the societal level factors that create the best opportunity for changes at the organizational and community levels which will positively impact the individual and their interpersonal influencers (Alberti et al., 2020). Our participants highlighted the need for the government at the national, state, and local levels along with community institutions and organizations to provide a quicker, yet equitable response in the areas such as education, housing, healthcare, and economics (See Fig. 1 and Table 3 for details). As identified in previous work (Alberti et al., 2020), participants also perceived these plans should be guided by community input and recommendations of public health officials with continual updates with accurate information. This is to help reduce the impact the current systems have on individual and family outcomes during the COVID-19 pandemic (e.g., economic instability) along with the mitigation of confusion and fear as occurred during the H1N1 and Ebola pandemics (Gray et al., 2018; Fineberg, 2014).
Fig. 1.
Preparedness by context: Challenges and strategies.
Table 3.
Recommendations to increase preparedness of black americans for future pandemics.
|
|
|
|
|
|
Strategies offered by participants at the community/organizational level included the provision of COVID-19 education including etiology, drugs, and vaccines by researchers and medical providers, the most trusted information source (Hamel et al., 2020). During past pandemics, providers were needed for an effective response which creates a higher work volume, social pressure, and personal risk (Yakuba et al., 2016; Johnson and Butcher, 2021). So, this request is not unusual, but it adds pressure to healthcare workers. The emergence of researchers as an information source was surprising and revitalizing considering the years of research (Corbie-Smith et al., 2002; Durant et al., 2011), demonstrating the distrust Black Americans have in researchers and the process. Unsurprisingly, the need for empathy from peers, especially among the essential workers and individuals with UMCs, was common. Studies indicate empathy is low among Americans, which is a direct relationship to engagement in preventive behaviors such as self-isolation and face mask wearing (Pfattheicher et al., 2020; Petrocchi et al., 2021). Hence, further study of this concept is necessary to begin to address the COVID-19 pandemic.
In recognizing change should start at the societal level, participants did identify areas where they could increase their preparedness. Changes included saving and investing money, keeping a stockpile of essential items, and engaging in preventive behaviors daily (e.g., working out, eating healthier). More importantly, all agreed to spend time with family and friends post-pandemic. However, past studies and even a few participants indicate that many individuals especially those in marginalized communities are unable to engage in many of these behaviors pre-pandemic (Quinn and Kumar, 2014) which points to the need to address the existing structural inequities. Some young adults and individuals with UMC did not foresee many changes which could be made. This is unsurprising as studies are showing many young adults today are less prepared for adulthood than previous generations (Twenge and Park, 2019) and many take risks due to experiencing their freedom from moral supervision of parents (Scneider and Morris, 1991). Further exploration is needed on how individuals with UMCs prepared for pandemics to inform future pandemic preparation efforts. Findings demonstrate a myriad of changes are needed on multi-levels to ensure an equitable response in the COVID-19 and future pandemics.
4.4. Strengths and limitations
To our knowledge this is the first study to capture perspectives on pandemic preparedness among Black American subgroups: essential workers, young adults, parents, and individuals with UMCs. Gaining insight on their lived experiences along with challenges and perceived changes needed to improve preparedness provides tailored, intervention targets to increase preparedness. There are limitations. This study's findings may not be generalizable to all members of the Black American population. Perspectives of all subgroups within the Black American population (e.g., children) are not included. Intersectionality could play a role in participants' answers. Lastly, it is possible that researchers' personal biases influenced with data collection and interpretations.
5. Conclusions
This study explored preparedness using McLeroy's Model Ecological for Health Promotion among Black American subgroups for the COVID-19 pandemic along with perceived challenges related to underlying system inequities and health disparities and solutions to increase preparedness. While many participants indicated they were prepared in our study, all experienced challenges and provided suggestions to improve their preparedness for current and future pandemics. As an initial step to address these concerns, we served as a health education resource post-interviews to educate on COVID-19 and public health recommendations and linked participants to resources when necessary. To further inform preparedness plans as they are reenacted, Table 3 provides recommendations informed by study participants to increase pandemic preparedness among vulnerable Black American subgroups. Further studies are needed to determine if these findings resonate with other groups (e.g., children) and groups in other geographical areas especially those considered hard-to-reach. Studies should also explore in depth systems stakeholders' degree of preparedness and their needs to engage with uniquely, vulnerable Black American subgroups. For example, future studies should explore the role researchers can play in addressing educational needs (e.g., vaccines) of Black Americans during a pandemic. Study findings could be leveraged to inform targeted multi-level strategies for response plans that could increase preparedness across sub-groups within the Black American population.
Credit author statement
Jennifer Cunningham-Erves: Conceptualization, Methodology, Validation, Formal analysis, Resources, Data curation, Writing – original draft, Writing – review & editing, Visualization, Supervision, Planning Administration, Funding acquisition; Imari Parham: Validation, Formal analysis, Data curation, Writing – original draft, Writing – review & editing; Jamal Moss: Investigation, Data curation, Visualization, Writing – review & editing; Iman Barre: Investigation, Data curation, Visualization, Writing – review & editing; Leah Alexander: Conceptualization, Writing – review & editing, Supervision, Planning Administration, Visualization, Funding acquisition; Jamaine Davis: Conceptualization, Writing – review & editing, Visualization, Supervision, Planning Administration, Funding acquisition; Taneisha Gillyard: Data curation, Visualization, Writing – review & editing;
Data statement
Research data are not shared due to ethical restrictions.
Declaration of competing interest
None.
Acknowledgements
The authors thank the members of the African American community for their valuable insights on their lived experiences during the COVID-19 pandemic. This work was supported by the National Center for Advancing Translational Sciences (NCATS) Clinical Translational Science Award (CTSA) Award Number: 5UL1TR0002243-03). The content hereof is the sole responsibility of the authors. The funders had no role in the design, implementation, analysis, and write-up of the study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2022.115185.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Alberti P.M., Lantz P.M., Wilkins C.H. Equitable pandemic preparedness and rapid response: lessons from COVID-19 for pandemic health equity. J. Health Polit. Policy Law. 2020;45:921–935. doi: 10.1215/03616878-8641469. https://doi:10.1215/03616878-8641469 [DOI] [PubMed] [Google Scholar]
- Arora S.K., Shah D., Chaturvedi S., Gupta P. Defining and measuring vulnerability in young people. Indian J. Community Med. 2015;40:193–197. doi: 10.4103/0970-0218.158868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey Z.D., Feldman J.M., Bassett M.T. How structural racism works - racist policies as a root cause of U.S. Racial health inequities. N. Engl. J. Med. 2021;384:768–773. doi: 10.1056/NEJMms2025396. https://doi:10.1056/NEJMms2025396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . Department of Health and Human Services; Atlanta, GA: 2021. Planning and Preparedness Resources.https://www.cdc.gov/flu/pandemic-resources/planning-preparedness/index.html [Online] Available: [Google Scholar]
- Centers for Disease Control and Prevention . Hospitalization, and Death by Race/Ethnicity; 2021. Risk for COVID-19 Infection.https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html [Online]. Available: [Google Scholar]
- Centers for Disease Control and Prevention . U.S. Department of Health and Human Services; Atlanta, GA: 2022. COVID Data Tracker.https://covid.cdc.gov/covid-data-tracker/#datatracker-home [Online] Available: [Google Scholar]
- Churchwell K., Elkind M., Benjamin R.M., Carson A.P., Chang E.K., Lawrence W., Mills A., Odom T.M., Rodriguez C.J., Rodriguez F., Sanchez E., Sharrief A.Z., Sims M., Williams O., American Heart Association Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American heart association. Circulation. 2020;142:e454–e468. doi: 10.1161/CIR.0000000000000936. [DOI] [PubMed] [Google Scholar]
- Corbie-Smith G., Thomas S.B., St George D.M. Distrust, race, and research. Arch. Intern. Med. 2002;162:2458–2463. doi: 10.1001/archinte.162.21.2458. https://doi:10.1001/archinte.162.21.2458 [DOI] [PubMed] [Google Scholar]
- Cowper A. Covid-19: are we getting the communications right? BMJ. 2020;368:m919. doi: 10.1136/bmj.m919. https://doi:10.1136/bmj.m919 [DOI] [PubMed] [Google Scholar]
- Creswell J.W. second ed. Sage Publications; Newbury Park, California: 2007. Qualitative Inquiry and Research Design: Choosing Among Five Approaches. [Google Scholar]
- Durant R.W., Legedza A.T., Marcantonio E.R., Freeman M.B., Landon B.E. Different types of distrust in clinical research among whites and African Americans. J. Natl. Med. Assoc. 2011;103:123–130. doi: 10.1016/s0027-9684(15)30261-3. https://doi:10.1016/s0027-9684(15)30261-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbeddini A., Tayefehchamani Y. Amid COVID-19 pandemic: challenges with access to care for COPD patients. Res. Soc. Adm. Pharm. 2021;17:1934–1937. doi: 10.1016/j.sapharm.2020.06.002. https://doi:10.1016/j.sapharm.2020.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fineberg H.V. Pandemic preparedness and response--lessons from the H1N1 influenza of 2009. N. Engl. J. Med. 2014;370:1335–1342. doi: 10.1056/NEJMra1208802. https://doi:10.1056/NEJMra1208802 [DOI] [PubMed] [Google Scholar]
- Gray N., Stringer B., Bark G., Heller Perache A., Jephcott P., Broeder R. ‘When Ebola enters a home, a family, a community’. A Qualitative study of population perspectives on Ebola control measures in rural and urban areas of Sierra Leone. PLoS Neglected Trop. Dis. 2018;12 doi: 10.1371/journal.pntd.0006461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamel L., Kirzinger A., Munana C., Brodie M. 2020. KFF COVID-19 Vaccine Monitor.https://www.kff.org/coronavirus-covid-19/report/kff-covid-19-vaccine-monitor-december-2020/ : [Online]. Available: [Google Scholar]
- Hanage W.P., Testa C., Chen J.T., Davis L., Pechter E., Seminario P., Santillana M., Krieger N. COVID-19: US federal accountability for entry, spread, and inequities-lessons for the future. Eur. J. Epidemiol. 2020;35:995–1006. doi: 10.1007/s10654-020-00689-2. https://doi:10.1007/s10654-020-00689-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inf. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. https://doi:10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart P.S., Chinn S., Soroko S. Politicization and polarization in COVID-19 news coverage. Sci. Commun. 2020;42:679–697. doi: 10.1177/1075547020950735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson S.B., Butcher F. Doctors during the COVID-19 pandemic: what are their duties and what is owed to them? J. Med. Ethics. 2021;47:12–15. doi: 10.1136/medethics-2020-106266. https://doi:10.1136/medethics-2020-106266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn K.B., Eel M. Group Processes and Intergroup Relations; 2021. (Un)masking Threat: Racial Minorities Experience Race-Based Social Identity Threat Wearing Face Masks during COVID-19.https://doi:10.1177/1368430221998781 [Google Scholar]
- Khan G., Sheek-Hussein M., Al Suwaidi A.R., Idris K., Abu-Zidan F.M. Novel coronavirus pandemic: a global health threat. Turk. J. Emerg. Med. 2020;20:55–62. doi: 10.4103/2452-2473.285016. https://doi:10.4b2473.285016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kompaniyets L., Agathis N.T., Nelson J.M., Preston L.E., Ko J.Y., Belay B., Pennington A.F., Danielson M.L., DeSisto C.L., Chevinsky J.R., Schieber L.Z., Yusuf H., Baggs J., Mac Kenzie W.R., Wong K.K., Boehmer T.K., Gundlapalli A.V., Goodman A.B. Underlying medical conditions associated with severe COVID-19 illness among children. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.11182. https://doi:10.1001/jamanetworkopen.2021.11182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krouse H.J. COVID-19 and the widening gap in health inequity. Otolaryngol. Head Neck Surg. 2020;163:65–66. doi: 10.1177/0194599820926463. https://doi:10.1177/0194599820926463 [DOI] [PubMed] [Google Scholar]
- Lam K., Lu A.D., Shi Y., Covinsky K.E. Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Intern. Med. 2020;180:1389–1391. doi: 10.1001/jamainternmed.2020.2671. https://doi:10.1001/jamainternmed.2020.2671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang S., Gibson S., Ng K.W., Truby H. Understanding children and young people's experiences pursuing weight loss maintenance using the Socio-ecological Model: a qualitative systematic literature review. Obes. Rev. 2021;22 doi: 10.1111/obr.13172. https://doi:10.1111/obr.13172 [DOI] [PubMed] [Google Scholar]
- Lee D., Paul C., Pilkington W.P., Mulrooney T., Diggs S.N., Kumar D. Examining the effects of social determinants of health on COVID-19 related stress, family's stress and discord, and personal diagnosis of COVID-19. J. Affect. Disord. Rep. 2021;5 doi: 10.1016/j.jadr.2021.100183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancera B.M., Dorgo S., Provencio-Vasquez E. Risk factors for hispanic male intimate partner violence perpetration. Am. J. Men's Health. 2017;11:969–983. doi: 10.1177/1557988315579196. https://doi:10.1177/1557988315579196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason T.B., Barrington-Trimis J., Leventhal A.M. Eating to cope with the COVID-19 pandemic and body weight change in young adults. J. Adolesc. Health. 2021;68:277–283. doi: 10.1016/j.jadohealth.2020.11.011. https://doi:10.1016/j.jadohealth.2020.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeroy K.R., Bibeau D., Steckler A., Glanz K. An ecological perspective on health promotion programs. Health Educ. Q. 1988;15(4):351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- Ngepan N. Socio-economic determinants of global COVID-19 mortalities: policy lessons for current and future pandemics. Health Pol. Plann. 2021;36:418–434. doi: 10.1093/heapol/czaa161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker C.F., Stern E.K. The Trump Administration and the COVID-19 crisis: exploring the warning-response problems and missed opportunities of a public health emergency. Publ. Adm. 2022 doi: 10.1111/padm.12843. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peek M.E., Simons R.A., Parker W.F., Ansell D.A., Rogers S.O., Edmonds B.T. COVID-19 among african Americans: an action plan for mitigating disparities. Am. J. Publ. Health. 2021;111:286–292. doi: 10.2105/AJPH.2020.305990. https://doi:10.2105/ajph.2020.305990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrocchi S., Bernardi S., Malacrida R., Traber R., Gabutti L., Grignoli N. Affective empathy predicts self-isolation behaviour acceptance during coronavirus risk exposure. Sci. Rep. 2021;11 doi: 10.1038/s41598-021-89504-w. https://doi:10.1038/s41598-021-89504-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfattheicher S., Nockur L., Bohm R., Sassenrath C., Petersen M.B. The emotional path to action: empathy promotes physical distancing and wearing of face masks during the COVID-19 pandemic. Psychol. Sci. 2020;31:1363–1373. doi: 10.1177/0956797620964422. https://doi:10.1177/0956797620964422 [DOI] [PubMed] [Google Scholar]
- Quinn S.C., Kumar S. Health inequalities and infectious disease epidemics: a challenge for global health security. Biosecur. Bioterror. 2014;12:263–273. doi: 10.1089/bsp.2014.0032. https://doi:10.1089/bsp.2014.0032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusoja E.A., Thomas B.A. The COVID-19 pandemic, Black mistrust, and a path forward. eClinicalMedicine. 2021;35 doi: 10.1016/j.eclinm.2021.100868. https://doi:10.1016/j.eclinm.2021.100868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satcher D. The impact of disparities in health on pandemic preparedness. J. Health Care Poor Underserved. 2011;22:36–37. doi: 10.1353/hpu.2011.0099. https://doi:10.1353/hpu.2011.0099 [DOI] [PubMed] [Google Scholar]
- Scneider D., Morris J. Risk taking behaviors of college students. Environ. Behav. 1991;23:575–591. [Google Scholar]
- Snowden L.R., Graff G. COVID-19, social determinants past, present, and future, and african Americans' health. J. Racial. Ethn. Health Disparities. 2021;8:12–20. doi: 10.1007/s40615-020-00923-3. https://doi:10.1007/s40615-020-00923-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son C., Hegde S., Smith A., Wang X., S asangohar F. Effects of COVID-19 on college students' mental health in the United States: interview survey study. J. Med. Internet Res. 2020;22 doi: 10.2196/21279. https://doi:10.2196/21279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steelfisher G.K., Blendon R.J., Bekheit M.M., Lubell K. The public's response to the 2009 H1N1 influenza pandemic. N. Engl. J. Med. 2010;362:e65. doi: 10.1056/NEJMp1005102. https://doi:10.1056/NEJMp1005102 [DOI] [PubMed] [Google Scholar]
- The Lancet The plight of essential workers during the COVID-19 pandemic. Lancet. 2020;395:1587. doi: 10.1016/S0140-6736(20)31200-9. https://doi:10.1016/s0140-6736(20)31200-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge J.M., Park H. The decline in adult activities among U.S. Adolescents, 1976-2016. Child Dev. 2019;90:638–654. doi: 10.1111/cdev.12930. https://doi:10.1111/cdev.12930 [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau . U.S. Departmant of Commerce; Washington, D.C.: 2020. U.S. And World Population Clock.https://www.census.gov/popclock [Online] Available: [Google Scholar]
- U.S. Department of Education . 2021. Equity of Opportunity.https://www.ed.gov/equity [Online] Washington, DC. Available: [Google Scholar]
- Vasquez Reyes M. The disproportional impact of COVID-19 on african Americans. Health Hum. Rights. 2020;22:299–307. [PMC free article] [PubMed] [Google Scholar]
- Vaughn E., Tinker T. Effective health risk communication about pandemic influenza for vulnerable populations. Am. J. Publ. Health. 2009;99:S324–S332. doi: 10.2105/AJPH.2009.162537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlahov D., Coady M.H., Galea S., Ompad D.C., Barondess J.A. Pandemic preparedness and hard to reach populations. Am. J. Disaster Med. 2007;2:281–283. [PubMed] [Google Scholar]
- Wilkins C., Friedman E., Churchwell A., Slayton J., Jones P., Pulley J.M., Kripalani S. A systems approach to addressing COVID-19 health inequities. NEJM Catalyst Innovat. Care Deliv. 2021;2:1. doi: 10.1056/CAT.20.0374. [DOI] [Google Scholar]
- Williams D.R., Cooper L.A. COVID-19 and health equity-A new kind of "herd immunity. JAMA. 2020;323:2478–2480. doi: 10.1001/jama.2020.8051. https://doi:10.1001/jama.2020.8051 [DOI] [PubMed] [Google Scholar]
- Yakuba A., Folayan M.O., Sani-Gwarzo N., Nguku P., Peterson K., Brown B. The Ebola outbreak in Western Africa: ethical obligations for care. J. Med. Ethics. 2016;42:209–210. doi: 10.1136/medethics-2014-102434. https://doi:10.1136/medethics-2014-102434 [DOI] [PubMed] [Google Scholar]
- Yancy C.W. COVID-19 and african Americans. JAMA. 2020;323:1891–1892. doi: 10.1001/jama.2020.6548. https://doi:10.1001/jama.2020.6548 [DOI] [PubMed] [Google Scholar]
- Yearby R., Mohapatra S. Law, structural racism, and the COVID-19 pandemic. J. Law Biosci. 2020;7 doi: 10.1093/jlb/lsaa036. https://doi:10.1093/jlb/lsaa036 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.