Abstract
HIV pre-exposure prophylaxis (PrEP) is highly effective at preventing HIV; however, PrEP use among transgender individuals remains low. We conducted a systematic review to identify barriers and facilitators to PrEP uptake, adherence, and persistence among transgender individuals in the United States. We conducted a literature search in PubMed and CINAHL databases in March 2021 and followed PRISMA guidelines. Studies were eligible if they were published in a peer-reviewed journal and reported interest, uptake, adherence, and/or persistence of PrEP use among transgender individuals. Articles that did not disaggregate results for transgender participants were excluded. Data from included articles were coded using content analysis and narratively synthesized using a framework matrix. We screened 254 unique articles published after US Food and Drug Administration approval of PrEP, and 33 articles were included in the review. Five themes were identified in the literature, including (1) PrEP concentrations were lower among individuals taking feminizing hormones, but the difference did not appear clinically significant; (2) concerns regarding interactions between gender-affirming hormone therapy and PrEP remain a large barrier; (3) PrEP initiation may facilitate increased self-advocacy and self-acceptance; (4) lack of trust in medical institutions impacts PrEP uptake; and (5) social networks have a significant influence on PrEP knowledge, interest, and adherence. Additional research is needed involving transgender men and nonbinary persons, and efforts to improve PrEP persistence among the transgender community are needed. Training health care providers to provide inclusive and affirming care is perhaps one of the strongest areas for intervention to increase PrEP uptake and persistence.
Keywords: HIV, pre-exposure prophylaxis, transgender, systematic review
Introduction
Transgender populations shoulder a disproportionate HIV burden around the world. In the United States, an estimated 0.4–0.6% of adults identify as transgender,1,2 but transgender persons accounted for 2% of HIV incidence in 2018. Between 2006 and 2017, an estimated 18.8% of transgender women and 2.0% of transgender men in the United States were living with HIV.3 These studies specifically highlighted transgender individuals and did not discuss nonbinary populations.
HIV pre-exposure prophylaxis (PrEP) was introduced in 2012 as a daily medication to prevent HIV and use has been recommended by the Centers for Disease Control and Prevention (CDC) since 2014.4,5 The first PrEP medication approved by the US Food and Drug Administration (FDA), Truvada, was a combination of two antiretroviral drugs, oral tenofovir disproxil fumarate and emtricitabine (TDF/FTC).6 In 2019, a second drug combination (i.e., Descovy, tenofovir alafenamide and emtricitabine) was approved by the FDA as PrEP for transgender women and cisgender men who have sex with men (cMSM).7 PrEP use has led to a 30.7% reduction in HIV incidence among cMSM,8 and PrEP is highly effective when taken as prescribed.9
The CDC's 2017 guideline criteria for PrEP eligibility are not specifically inclusive of transgender individuals and uses cMSM as the standard,10 current at the time of data extraction for this systematic review. CDC eligibility criteria for cMSM include the following: (1) HIV-negative adults who had anal sex without condoms with a male partner in the past 6 months; (2) a history of any past STIs in the past 6 months; and (3) sexual partner who is HIV positive; and/or (4) not in a primary or monogamous relationship with a cisgender male without HIV infection.
Nonetheless, current PrEP use in the transgender community remains low, with one study reporting that among their study cohort, 92% of transgender women without HIV stated they knew of PrEP, but only 32% reported use.11 A second study showed that transgender women were significantly less likely (p < 0.05) to be aware of PrEP than cMSM.12 In addition, there are significant racial and ethnic disparities in HIV among transgender populations. Black and Hispanic/Latinx transgender individuals accounted for 48% and 32% of new diagnoses in 2018, respectively.13 In the United States, PrEP prescriptions between 2014 and 2016 were predominantly utilized by White individuals (68.7%), compared to 11.2%, 13.1%, and 4.5% for Black, Hispanic, and Asian individuals, respectively.14
There has been a significant amount of research dedicated to PrEP efficacy and uptake among cMSM, with less focus on uptake, adherence, and persistence of PrEP among transgender populations in the United States, despite findings that nearly two-thirds of transgender men who have sex with men in the United States met clinical guidelines for PrEP.15 For these reasons, we undertook this systematic review to assess the current state of PrEP uptake, adherence, and persistence among transgender individuals to identify scientific gaps and future research directions.
Methods
We conducted a systematic review of currently available literature regarding barriers and facilitators to PrEP uptake among transgender populations with narrative synthesis. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (i.e., PRISMA) guidelines were used for this systematic review.
Study selection
We conducted a literature search using PubMed and CINAHL databases on March 2, 2021. This search utilized the Boolean string [(“pre-exposure prophylaxis” OR “PrEP” OR “antiretroviral prophylaxis”) AND (HIV OR AIDS) AND (transgender)]. Articles were sorted and extracted using EndNote X9 to identify duplicates before application of inclusion and exclusion criteria during title and abstract review.
Eligibility criteria
Studies were eligible for full-text review if they were published in a peer-reviewed journal and met the following inclusion criteria: (1) included HIV-negative transgender and/or nonbinary participants, and/or (2) discussed biological, psychological, or social facilitators and/or barriers to PrEP interest, uptake, adherence, effectiveness, and/or persistence among transgender individuals. Articles were excluded if they featured a study group with more than half of included individuals living with HIV. Once primary inclusion and exclusion criteria were applied, each article underwent full-text review, to which additional exclusion criteria were applied. An article was excluded if it was a systematic review, the study was still ongoing, or analyses were not stratified for transgender individuals.
Data collection process
During full-text review, findings were reviewed and coded using inductive and deductive content analysis16 led by the first author. More specifically, a list of a priori codes was identified by the first and senior author. After full-text review of the extracted literature, overlapping themes in the literature were collaboratively identified, code definitions were created, and the final codebook was applied to the literature. Data were then organized using a framework matrix in Microsoft Excel, allowing within- and between-article analyses across themes.17
Results
A total of 289 records were identified from the databases (PubMed k = 246 and CINAHL k = 43), representing 254 unique articles. One hundred five articles were removed during title and abstract review. After full-text review of the remaining 149 studies, 33 articles fulfilled the eligibility criteria and were included in our final analysis (see Fig. 1 for flow diagram). Thirty articles included transgender women in the study population, seven of which also included cMSM as a stratified population. Eleven studies were inclusive of transgender men in the study population. All 33 articles are synthesized in Table 1.
FIG. 1.
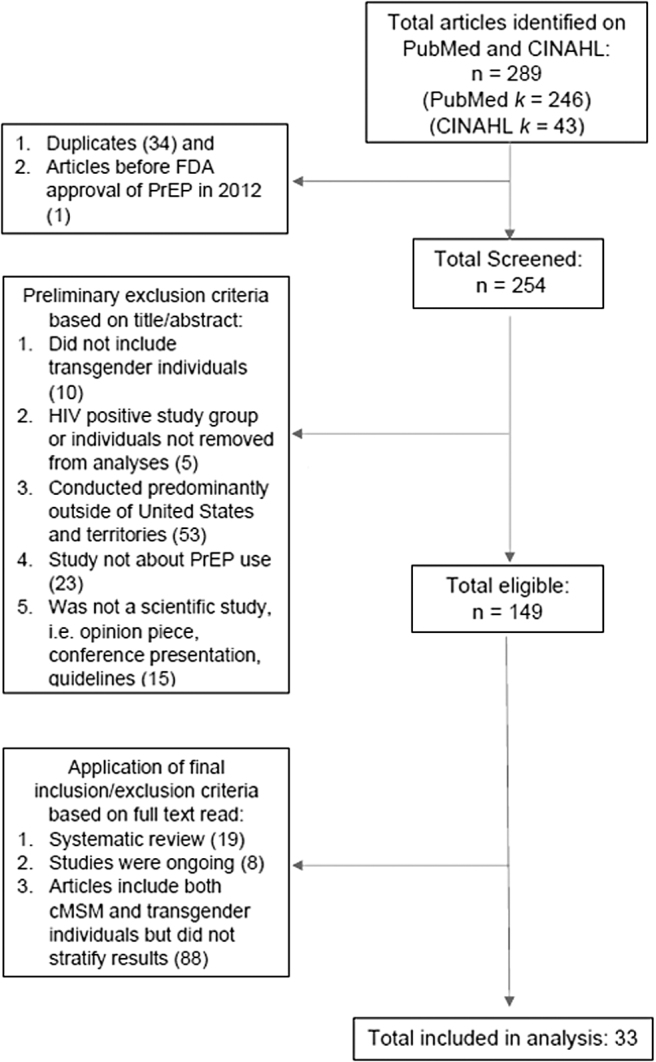
Flow diagram for systematic review of the literature related to barriers and facilitators to HIV PrEP among transgender populations in the United States. PrEP, pre-exposure prophylaxis.
Table 1.
Systematic Review Findings of Barriers and Facilitators to HIV Pre-Exposure Prophylaxis Among Transgender Populations in the United States
| Authors | Year | Study type | N | Includes transgender men? | Includes cMSM? | Findings |
|---|---|---|---|---|---|---|
| Andrzejewski et al. | 2021 | Cross-sectional | 1029 (n TGW = 468) | Yes (n = 297) | No | Medical gender affirmation was positively associated with PrEP awareness in transgender males and nonbinary individuals. |
| Barreraset al. | 2019 | Focus groups | 91 (n = 39 TGW) | No | Yes (n = 52) | TGW felt they had less access to health care, insurance, or other support services than cMSM, which affected their access to PrEP. Also reported concerns about drug interactions between PrEP and hormone therapy. |
| Brooks et al. | 2019 | Focus groups | 19 | No | No | BLTW reported concerns about being perceived as HIV positive if they took PrEP, that they were more likely to participate in higher-risk sexual behaviors, associated with negative labels (i.e., slut or whore) from ex-partners or friends. They did identify themselves as resources for disseminating information regarding PrEP |
| Cahill et al. | 2020 | Focus groups | 19 | No | No | Themes that emerged ranged from concerns about hormone interactions with PrEP, to the need for gender-affirming health care and medical and government mistrust, to misinformation or lack of information about PrEP preventing individuals from becoming interested or obtaining it. |
| Chandler et al. | 2021 | Cross-sectional | 490 | No | No | 55.5% of the study sample was aware of PrEP, but only 21.8% of the sample reported PrEP use. Awareness was higher among individuals living with HIV or those with unknown status than those who reported HIV-negative status. High levels of reported transphobia, but less report of health care discrimination. Higher risk behaviors were positively associated with PrEP use. |
| Cirrincione et al. | 2020 | Prospective cohort | 15 | No | No | Plasma levels of TDF/FTC among transgender women were lower compared to the cisgender control group. The decreased levels were less substantial among nonobese participants than it was for obese participants. On average, study plasma levels of TDF/FTC were higher than those in previous studies, and were within the guideline concentrations for prevention, demonstrating that concurrent use with FHT is reasonable. |
| D'Avanzo et al. | 2019 | Mixed methods—Focus groups + cluster analysis | 78 | Yes (n = 4) | No | Medical mistrust was found to be linked to decreased knowledge of where to obtain PrEP in an affirming location. This was more apparent among White transgender women with higher levels of education. Transgender women in the study sample were more likely to have heard about PrEP in trans-competent health care settings. |
| D'Avanzo et al. | 2021 | Cluster analysis | 125 | No | No | Individuals who reported strong belonging to the transgender community were more likely to have knowledge and positive attitudes about PrEP and report using it and/or know other transgender women who utilize PrEP. |
| Hood et al. | 2018 | Cross-sectional | 126 | No | No | Individuals on PrEP were likely to have obtained it at the same facility they were receiving gender-affirming care. Approximately two-third of the study sample who was not interested in PrEP had indications for it. |
| Horvath et al. | 2019 | Mixed methods | 202 | Yes (n = 77) | No | Barriers included low access due to cost, concerns about medication interactions and long-term effects, medical mistrust/previous poor experiences, and concerns about insurance disclosure to parents. |
| Klein and Golub | 2019 | Focus groups | 30 | No | No | To increase interest in PrEP uptake, gender-affirming and diverse messaging and care need to be available, which includes stopping the combination of transgender individuals with cisgender MSM in health care settings and for PrEP advertising purposes. In addition, providers should be more involved in the conversation and obtainment of PrEP in this population. |
| Kuhns et al. | 2016 | Cross-sectional | 180 | No | No | In the study sample, there were low levels of awareness and uptake, but once PrEP was further discussed with participants, there was high interest (68.9%) and indication (61.7%). Factors that were associated with indication were higher # CAS partners and self-perceived group membership among the transgender community. |
| Nieto et al. | 2021 | Focus groups | 18 | No | No | BLTW reported feeling unrepresented in advertising and HIV prevention efforts, as they felt it was more targeted at cisgender gay men, and this affected their interest in initiating PrEP. Also, medical mistrust affected engagement in care for BLTW. |
| Ogunbajo et al. | 2021 | Individual semistructured interviews; cross-sectional data collection | 30 | No | No | PrEP uptake and adherence were negatively impacted by structural-level factors among the study sample (i.e., employment opportunities, transportation, housing concerns/instability, perception of high PrEP expenses). Psychological factors included depressive symptoms and substance use, as well as concern regarding hormone interactions. |
| Poteat et al. | 2019 | Mixed methods | 98 | No | No | Individuals in the study reported high awareness and willingness (75% of the cohort), but low initiation. Individuals who were less willing to initiate PrEP reported concerns about drug interactions with hormone therapy, but those on PrEP did not report any interaction. Increased willingness was significantly associated with history of sex work. |
| Rael et al. | 2018 | Focus groups | 18 | No | No | The barriers identified by this study were participant worries about medication side effects, especially when initiating the medication, difficulty with adherence due to the large pill size and daily administration, social stigma regarding potential misinterpretation of PrEP adherence as HIV medication adherence, and messaging targeting cisgender individuals that was not inclusive. |
| Rael et al. | 2019 | Focus groups | 18 | No | No | Focus groups identified gender-affirming, inclusive, and informative messaging as an important facilitator to uptake and adherence. |
| Reback et al. | 2019 | Prospective cohort | 187 (n = 58 transgender women) | No | Yes (n = 129) | The use of counseling and daily text reminders was significantly associated with PrEP adherence among participants. |
| Reisner et al. | 2017 | Mixed methods | 181 | Yes | No | HIV-uninfected participants reported low rates of PrEP uptake, even though they engaged in behaviors that put them at higher risk for infection. Participants were more likely to engage in prevention services if they were older and provided gender affirmation. |
| Reisner et al. | 2019 | Cross-sectional | 857 transgender men | Yes | No | Reports of high partner stigma, compared to no partner stigma, were associated with increased odds of PrEP indication. Those trans MSM who reported sex with cis-male(s) and one or more partner(s) of other gender(s) had higher odds of PrEP indication than trans MSM who exclusively reported sex with cis-males. |
| Reisner et al. | 2021 | Cross-sectional | 843 Transgender Men | Yes | No | Surgical gender affirmation, no health care discrimination, and social media as a primary health information source were associated with increased odds of PrEP uptake and persistence (all p < 0.05). |
| Restar et al. | 2018 | Randomized control trial | 230 | No | No | Medical mistrust and concerns about side effects were identified as two of the main reasons for not being interested in PrEP among the study sample. |
| Rowniak et al. | 2017 | Focus groups | 22 Transgender Men | Yes | No | One major barrier reported among the study population was that medical providers did not provide necessary information to learn about and obtain PrEP. |
| Sevelius et al. | 2016 | Focus groups | 30 | No | No | Barriers to PrEP use among the study population included marketing that focused predominantly on cMSM and was not trans-inclusive, lack of trans-specific services (including providing PrEP within a program that acknowledges resource constraints), clinics treating transwomen as “just another guy,” transphobia leads to medical mistrust, and concerns about interactions with hormones. |
| Sevelius et al. | 2020 | Cross-sectional | 190 (n TGW = 91) | Yes (n = 99) | No | PrEP use among participants (n = 5) was associated with meeting CDC indications for HIV testing. Transfeminine individuals were less likely to know about PrEP than transmasculine individuals. Individuals who did not receive affirmation of their gender identity were less likely to know about PrEP. |
| Shieh et al. | 2019 | Prospective cohort | 16 | No | Yes | TGW had higher creatinine clearance than cisgender men. Possible upregulation of angiotensin-2 receptor expression may lead to increased clearances; testosterone downregulates angiotensin-2 receptor expression, subsequently leading to a possible reduction among transgender women |
| Westmoreland et al. | 2020 | Prospective cohort | 10504 (n TGW = 65) | Yes (n = 63) | Yes | TGW were significantly more likely to report being PrEP naive (p = 0.02), whereas transgender men were more likely to report current PrEP use, although the association was not significant. |
| Wilson et al. | 2015 | Cross-sectional | 233 | No | No | Data led investigators to believe that more education about PrEP in the transgender community was warranted, as significantly less transwomen in San Francisco knew about PrEP than cMSM. Investigators highlighted that barriers to knowledge and access were that there was less research involving transgender women, less medical venues specifically for transwomen (compared to those for cMSM), and less marketing/educational materials for PrEP for transgender individuals. |
| Wilson et al. | 2016 | Retrospective cohort | 298 | No | No | More YTW who had a history of sex work were candidates than those without similar history. 57.9% of sex workers were eligible for PrEP based on the criteria. After learning more about PrEP, 73.9% were interested in taking. Having health insurance was a facilitator. Barriers included daily administration, interactions with hormone therapy, and concern about medication side effects. |
| Wilson et al. | 2020 | Cross-sectional | 369 | No | Yes | Transgender women were significantly less likely to be aware of PrEP than cMSM, to have discussed PrEP with a provider, or to be adherent (all p < 0.05). |
| Wood et al. | 2017 | Mixed methods | 25 | No | Yes | Facilitators included the desire to remain HIV-negative adherence motivator, protection of trans-community, and the use of PrEP as an opportunity to strengthen emotional relationships and physical closeness in serodiscordant relationships. Barriers included cost, the prioritization of hormones over HIV prevention, adherence challenges, side effects, and concerns about stigma. |
| Wood et al. | 2019 | Focus groups | 31 | No | No | Stigma, most commonly identified, becomes barrier to disclosing PrEP use to their support networks and limits ability to receive adherence support; HIV-related stigma (misperception of being HIV positive) and homophobia from family, health care professionals, peers, and partners |
| Zarwell et al. | 2021 | Cross-sectional | 294 | Yes (n = 157) | No | 91.5% of sample reported knowing about PrEP, but only 17.4% stated they had previously received a prescription, more frequently among transgender men than women (p < 0.0001). Reasons for discontinuation: side effects (predominantly GI), access to providers, changes in sexual activity/relationship status, and cost/insurance coverage |
BLTW, Black and Latinx transgender women; CDC, Centers for Disease Control and Prevention; cMSM, cisgender men who have sex with men; FHT, feminizing hormone therapy; GI, gastrointestinal; MSM, men who have sex with men; PrEP, pre-exposure prophylaxis; TDF/FTC, tenofovir disproxil fumarate and emtricitabine; TGW, transgender women; YTW, young transgender women.
PrEP concentrations were lower among individuals taking feminizing hormones, but the difference did not appear clinically significant
Two studies sought to identify potential interactions between feminizing hormone therapy (FHT) and PrEP, specifically TDF/FTC. Each study found hormone concentrations, specifically estradiol, were unaffected among study participants taking PrEP; however, PrEP concentrations were significantly lower among transgender women compared to cMSM enrolled in each respective study cohort. Nonetheless, these values remained in the protective concentration ranges.18,19 One study posited that this difference in plasma PrEP concentration was not due to decreased bioavailability of the drug, but instead due to increased creatinine clearance among transgender women taking FHT that includes androgen blockers, which reduce testosterone, thereby potentially increasing angiotensin-2 receptors. This led to increased excretion of PrEP in the urine of study participants.18 The second study also found PrEP concentrations were lower among transgender women taking FHT, but these concentrations were at a protective level.19
Concerns regarding interactions between gender-affirming hormone therapy and PrEP remain a large barrier
For many transgender individuals, gender affirmation using hormone therapy is extremely important.20 Ten studies included in this systematic review (31.3%) provided information regarding transgender individuals' attitudes and beliefs about interactions between PrEP and gender-affirming hormone therapy.20–29 Multiple studies reported mid-to-high levels of PrEP awareness and knowledge among transgender women, but low initiation due to concerns and beliefs about interactions with hormone therapy.23,25,27,28 One study identified medical gender affirmation as positively associated with PrEP awareness among transgender men and nonbinary individuals.30 In another study, participants who began hormone therapy procured through informal channels reported concerns about working with medical providers or taking PrEP alongside hormone therapy.20,22
PrEP initiation may facilitate increased self-advocacy and self-acceptance among transgender persons
Although many barriers to initiating and adhering to PrEP are described throughout the literature, multiple studies demonstrate that PrEP is an important resource for transgender individuals. Transgender women with a history of sex work were shown to be more willing to initiate PrEP compared to transgender women in their study sample without a history of sex work.25 PrEP use was associated with increased ability to advocate for oneself among current sex workers, as they were able to maintain control of their HIV status without need for condom negotiation, the use of which could have potentially led to decreased payment.31 PrEP was also found to provide transgender women with a strategy for controlling their HIV risk when they are not in control of their exposure.
Transgender individuals are at a disproportionate risk for intimate partner violence, and many of them may encounter violence if they propose the use of a condom.20,31 One study also found that young transgender women were motivated to adhere to PrEP to reduce their risk for HIV acquisition and protect the transgender community, and that PrEP provided protection for individuals who previously felt that acquiring HIV was inevitable.29
PrEP not only confers protection against HIV but also has the potential to facilitate improved social interactions and mental health.20 In one study, PrEP use was associated with increased comfort in sexuality—specifically decreased internalized homophobia—and increased self-efficacy among young transgender women, which led to improved trust and intimacy between study participants and their support systems.29 Increased disclosure of PrEP use also impacted how individuals in their study communicated with members of their community by allowing them to inform and answer questions about PrEP.20,29
Systemic and social marginalization of transgender individuals lead to decreased PrEP uptake
Our review identified several social and economic marginalizing barriers that prevent transgender persons from accessing PrEP. Poverty,24,32,33 criminalization of sex work, and other structural barriers, including difficulty maintaining housing,24,31,34,35 previous incarceration leading to challenges obtaining employment,12 and lack of health insurance,21,23,24,28,33 were barriers to PrEP initiation.21,24 In addition, lack of gender-affirming health care,10 advertisement of PrEP as a medication for cMSM,20,22,26,31,36 and social stigma29,31,34,37,38 were also found to be barriers to PrEP among the transgender population. Of noteworthy concern, 29.4% of transgender individuals were identified as living in poverty in the United States in 2019.39 Also, transgender individuals are often subject to discrimination, leading many to engage in sex work for financial support.22,32
More than half (57.9%) of individuals with a history of sex work in a study cohort were eligible for PrEP, which was significantly more than the study population without a history.28 The cost of PrEP was identified as a barrier to initiation23,40 and adherence33 among transgender individuals. Moreover, lack of gender-congruent identification was shown to delay transgender women's access to PrEP and hormone therapy.41
The lack of transgender-specific messaging further contributes to structural barriers to PrEP. In one study, only 30% of the transgender study population met 2017 CDC PrEP criteria, which focus predominantly on cMSM.34 Multiple studies reported the lack of transgender-specific messaging and priority focus only on cMSM as barriers to knowledge and interest in PrEP.20,22,31,36 Gender affirmation was found to be a facilitator to PrEP awareness and use.30,42 While structural barriers significantly impact transgender persons access to PrEP, social stigma was found to affect knowledge, initiation, adherence, and persistence.
Multiple studies found lack of awareness about PrEP at the start of the study was due to HIV-related stigma.23,26 In a study of African American and Latina transgender women, individuals in the study stated people they knew had perceptions that these individuals are living with HIV, or that it was only a matter of time before they seroconverted.37 HIV stigma was also indicated as a barrier to PrEP because individuals taking antiretrovirals may be assumed to be living with HIV.26,31,43 Many transgender individuals stated that they experienced shame due to transphobia, and the fear of additional social stigma surrounding PrEP was a deterrent.29,31,34,37,38 Concern about increased intimate partner violence was also a barrier to PrEP initiation among transgender individuals,31 and one study stated that intimate partner violence was often experienced by transgender women when discussing HIV prevention methods with partners, limiting prevention empowerment and HIV status disclosure.31
Lack of trust in medical institutions impacts PrEP uptake
Lack of trust in medical teams was identified as a major barrier to PrEP initiation and adherence among transgender persons. Multiple studies identified medical mistrust as a factor for decreased PrEP knowledge among transgender individuals.34,44 Medical mistrust—or medical distrust when previously mistreated in health care—has arisen for many reasons, including the history of unethical government, medical, and pharmacological studies on racial minorities.20,22 Moreover, transphobia,10 including being misgendered in a clinic,31 may lead to decreased interest and uptake of PrEP among transgender individuals. Negative interactions often arose due to lack of trans-competent or trans-friendly clinics22,31,34 that combine transgender women or nonbinary individuals with cMSM.10 In addition, incomplete information about PrEP, its efficacy, and its potential side effects was often not relayed by physicians to their transgender patients.22,27,34,36,43
Study participants identified concerns about the excessive focus on HIV for transgender patients among health care providers and institutions, when holistically supportive care was desired, including the prioritization of hormone therapy.25 Some individuals were concerned about speaking about sexual behaviors with their medical provider due to fears of judgment or that their provider may stop prescribing gender-affirming hormones.20 One study, however, found that most participants in their cohort heard of PrEP from their medical provider.44
Social networks have a significant influence on PrEP knowledge, interest, and adherence
Interpersonal relationships were found to have a significant influence, either positively or negatively, on transgender individuals' interest in and adherence to PrEP. Friends and social networks are often a source of information about PrEP,29,40,43 as well as possible support. Young transgender women who reported a strong sense of belonging within the transgender community were more likely found to have positive attitudes about PrEP and subsequent initiation or adherence.45,46
Discussion
We conducted a systematic review of the literature to identify barriers and facilitators for PrEP initiation, adherence, and persistence among transgender individuals. Institutional marginalization, HIV and PrEP stigma, transphobia, and social networks were identified as significant barriers to PrEP uptake and persistence. Although transgender individuals are also a priority population in the CDC's guidelines, early clinical recommendations often focused on cMSM and individuals in serodiscordant relationships, thereby systematically excluding transgender individuals as a critical demographic in HIV prevention.5 Moreover, the rollout of PrEP largely prioritized cMSM in advertising and messaging, resulting in many studies reporting transgender individuals having lower awareness and interest of PrEP due to the lack of trans-specific information.22,26,31,36
We found HIV and PrEP stigmas to be salient within the reviewed literature, where individuals worried about being perceived as living with HIV if they were taking antiretroviral medication31,40 and were concerned about being perceived as promiscuous for considering PrEP. Social networks also heavily influenced individuals' interest and adherence to PrEP. Social networks can provide support and guidance to transgender individuals navigating decisions about PrEP, but we found social networks to also be a source of stress for individuals not open or out about their gender identity or interest in PrEP, and this was identified as a barrier to transgender individuals' knowledge, interest, and adherence to PrEP.
Concern regarding potential intimate partner violence resulting from conversations about HIV prevention was also a barrier to PrEP initiation or adherence.31,34 One area that needs additional research is identification of the experiences with PrEP among transgender people of color, as most of the studies included in this systematic review had predominantly White samples. Of the studies that focused on transgender women of color, medical distrust and lack of representation in PrEP advertising were mentioned more frequently.
Concerns about medication interactions between hormone therapy and PrEP remains an important barrier to expanding PrEP among transgender people. Researchers found statistically, but not necessarily clinically, significant lower PrEP concentrations among those on FHT, but no change in FHT concentrations among those on PrEP.18 In addition, more recent research published after our original data pull found that hormone therapy among transgender men and women did not affect PrEP concentrations from 4 weeks of daily administration.47
Further physiologic and pharmacokinetic research are important for guiding recommendations about dosing and delivery methods, including event-driven and long-acting injectable (LAI) PrEP.48,49 One phase 3 clinical trial was halted early due to a significant improvement in protection from LAI PrEP compared to daily oral administration among transgender women and cMSM.50 Collectively, additional research is needed to identify the long-term health implications of PrEP among transgender individuals on hormone therapy—both feminizing and masculinizing—to support shared PrEP decision-making between caregivers and transgender patients. Also, future research with LAI PrEP should be inclusive of transgender men, as most recent studies have excluded them as part of the study population.
Interest in PrEP was often linked to prior knowledge or awareness of the medication. Transgender individuals with less PrEP knowledge were less likely to be interested in initiation,22,51 and those with low awareness were very interested once the medication and regimen were explained to them.20,25–27 Although this systematic review focuses on transgender individuals' experience with PrEP in the United States, studies have been done around the world about this topic. Among these studies, multiple groups have focused on identifying the acceptability of PrEP among transgender women in lower-income countries.
Overall, these studies found low awareness about PrEP among transgender women in these settings, but high interest once they were informed about it as a prevention method.52–55 While outside the scope of this article, a comprehensive review of PrEP research among transgender communities in low- and middle-income countries would be an important avenue for future research, given the expanding literature.
Expanding provider knowledge of PrEP for use among transgender people is important for increasing PrEP uptake, as providers have a critical role in facilitating PrEP to transgender individuals who could benefit from PrEP. Structurally, systems of care are generally designed for cisgender patients, such as the documentation of biological sex as gender in the electronic medical record and the need for additional documentation to include “preferred” name and pronouns. This creates challenges in all aspects of care, including PrEP. Unfortunately, providers face unique barriers to prescribing PrEP,56 including challenges related to navigating patient insurance and copay assistance programs.56–58 Removing these structural barriers and disseminating accurate information about how PrEP will not interfere with HRT are potentially impactful ways to increase PrEP uptake and persistence among transgender individuals.
Another prominent barrier to PrEP uptake and persistence identified in the literature was lack of trust in medical institutions, which was identified in 19 studies included in this review. Researchers identified significant barriers in the medical system preventing transgender individuals from learning about or accessing PrEP through traditional routes,24,25,27 despite the importance and appropriateness in receiving PrEP information at medical appointments. This information is also relevant to holistic care for transgender individuals who are transitioning and/or receiving hormone therapy. These barriers ranged from lack of trans-competent care teams or clinical environments to the inherent focus on HIV prevention in clinics instead of providing holistic care that meets all the patients' health needs.34
Combining HIV treatment and prevention with gender-affirming care would decrease the burden of multiple appointments and financial costs on this population.59 In addition, transgender women may have difficulty obtaining PrEP and other HIV-related services such as testing and counseling from locations that were originally designed for cis-gender individuals, and may experience more potential discrimination and transphobia from providers and other patients.60
Improving medical education for nurses, medical assistants, and physicians to be more inclusive of transgender individuals and tailoring care to their experiences may improve medical trust among this population. Training programs to increase the quality of taking a sexual health history among medical residents61 and increase PrEP prescribing practices among family planning providers62 offer evidence-based models to build upon by incorporating trans-affirming care modules and topics related to hormone therapy into the educational requirements of health care providers.63,64 A major facilitator for PrEP initiation and adherence was the increased self-efficacy, intimacy with partners, and self-acceptance among transgender individuals.
Many members of the transgender community are subjected to oppressive transphobia and social stigma due to their gender identity, so it was an important finding that the use of PrEP provided the opportunity for self-acceptance, decreased internalized transphobia, and improved interpersonal relationships among transgender individuals who took PrEP.20,29 The use of PrEP allowed individuals who had less autonomy related to their HIV exposure, such as sex workers, to take control of their protection. Transgender individuals also reported increased intimacy after discussing PrEP use with their partners.29 Internalized transphobia and homophobia have negative implications on quality of life, and self-affirmation is important to combating the negative effects associated with these thoughts and benefiting from the social network and support of the transgender community.45,46 This social support can then be leveraged to support PrEP uptake and persistence.
Our systematic review is not without limitation. First, we focused our review on thematically describing the current state of literature, but we did not assess the rigor of studies reviewed. Second, it is possible some research may have been inadvertently missed in our review. Only 11 studies included transgender men, and many studies combined transgender men and women for analyses due to small sample sizes. Moreover, combining transgender individuals can result in diluting important information from each demographic.
Additional research is needed among transgender men and nonbinary individuals, given the relatively limited data published to date. In addition, although risk perception is something that has been frequently discussed in global literature,61,62,65 very few studies included in this review highlighted this theme. This is an area that needs additional research among transgender individuals in the United States and their interest, uptake, and adherence to PrEP.
Our systematic review and data extraction identified 33 primary research articles reporting factors contributing to the underutilization of PrEP among transgender populations. A predominant barrier identified was concern about the effect of PrEP on decreasing hormone therapy concentrations and subsequently leading to decreased interest and uptake of PrEP. These findings have important implications on PrEP decision-making within the context of hormone therapy, as it was found in multiple studies that hormone therapy levels were unchanged among individuals on PrEP.
Moreover, we identified the significant negative impacts of multiple experiences of marginalization on PrEP uptake and persistence, whereby institutional exclusion, HIV and PrEP stigma, transphobia, and the negative effects of social networks impede PrEP use. HIV prevention was also found to be secondary to other priorities in the reviewed literature, particularly the prioritization of hormone therapy. Access to gender-affirming health care is an urgent priority to improve access and trustworthiness of PrEP, which may enhance self-efficacy and empowerment for trans individuals to reduce the HIV burden among transgender persons in the United States.
Author Disclosure Statement
A.E.P. receives research funding from Gilead Sciences, Inc. All other authors declare that they have no conflict of interests.
Funding Information
Funding support was provided by the National Institute of Mental Health (K01-MH118939, PI: S.A.J.; K01-MH112412, PI: K.G.Q.). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1. Meerwijk EL, Sevelius JM. Transgender population size in the United States: A meta-regression of population-based probability samples. Am J Public Health 2017;107:e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Flores AR, Herman JL, Gates GJ, et al. How Many Adults Identify as Transgender in the United States? Los Angeles, CA: T.W. Institute; 2016. [Google Scholar]
- 3. Becasen JS, Denard CL, Mullins MM, et al. Estimating the prevalence of HIV and sexual behaviors among the US Transgender Population: A systematic review and meta-analysis, 2006–2017. Am J Public Health 2019;109:e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention. Preexposure prophylaxis for the prevention of HIV infection in the United States 2014. A Clinical Practice Guideline. 2014. Available at: https://www.sfdph.org/dph/files/newsMediadocs/2014PR/PrEPguidelines2014.pdf (Last accessed April 6, 2022).
- 5. Centers for Disease Control and Prevention. Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 Update: A Clinical Practice Guideline. 2018. Available at: https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf (Last accessed April 6, 2022).
- 6. US Food and Drug Administration. FDA approves first medication to reduce HIV risk. 2012. Available at: https://wayback.archiveit.org/7993/20170406045106/https://www.fda.gov/ForConsumer/ConsumerUpdates/ucm311821.htm (Last accessed April 6, 2022).
- 7. US Food and Drug Administration. FDA approves second drug to prevent HIV infection as part of ongoing efforts to end the HIV epidemic. 2019. Available at: https://www.fda.gov/news-events/press-announcements/fda-approves-second-drug-prevent-hiv-infection-part-ongoing-efforts-end-hiv-epidemic (Last accessed April 6, 2022).
- 8. LeVasseur MT, Goldstein ND, Tabb LP, et al. The effect of PrEP on HIV incidence among men who have sex with men in the context of condom use, treatment as prevention, and seroadaptive practices. J Acquir Immune Defic Syndr 2018;77:31–40. [DOI] [PubMed] [Google Scholar]
- 9. Spinner CD, Boesecke C, Zink A, et al. HIV pre-exposure prophylaxis (PrEP): A review of current knowledge of oral systemic HIV PrEP in humans. Infection 2016;44:151–158. [DOI] [PubMed] [Google Scholar]
- 10. Klein A, Golub SA. Increasing access to pre-exposure prophylaxis among transgender women and transfeminine nonbinary individuals. AIDS Patient Care STDS 2019;33:262–269. [DOI] [PubMed] [Google Scholar]
- 11. Centers for Disease Control and Prevention. HIV infection, risk, prevention, and testing behaviors among transgender women—National HIV Behavioral Surveillance 7 U.S. Cities 2019–2020. HIV Surveillance Special Report 27. 2021. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-special-report-number-27.pdf (Last accessed April 6, 2022).
- 12. Wilson EC, Turner CM, Arayasirikul S, et al. Disparities in the PrEP Continuum for trans women compared to MSM in San Francisco, California: Results from population-based cross-sectional behavioural surveillance studies. J Int AIDS Soc 2020;23 Suppl 3(Suppl 3):e25539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Centers for Disease Control and Prevention. HIV Surveillance Report, 2018 (Updated). Vol. 31. 2020. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2018-updated-vol-31.pdf (Last accessed April 6, 2022).
- 14. Huang YA, Zhu W, Smith DK, et al. HIV preexposure prophylaxis, by race and ethnicity—United States, 2014–2016. MMWR Morb Mortal Wkly Rep 2018;67:1147–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Reisner SL, Moore CS, Asquith A, et al. High risk and low uptake of pre-exposure prophylaxis to prevent HIV acquisition in a national online sample of transgender men who have sex with men in the United States. J Int AIDS Soc 2019;22:e25391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Braun V, ClarkV. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. [Google Scholar]
- 17. Spencer L, Ritchie J, Ormston R, O'Conner W, Barnard M.. Analysis: Principles and processes. In: Ritchie J, Lewis J, Nicholls CM, Ormston R (eds.) Qualitative Research Practice, 2nd ed. Thousand Oaks, CA: Sage Publications, Inc.; 2014. [Google Scholar]
- 18. Shieh E, Marzinke MA, Fuchs EJ, et al. Transgender women on oral HIV pre-exposure prophylaxis have significantly lower tenofovir and emtricitabine concentrations when also taking oestrogen when compared to cisgender men. J Int AIDS Soc 2019;22:e25405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cirrincione LR, Podany AT, Havens JP, et al. Plasma and intracellular pharmacokinetics of tenofovir disoproxil fumarate and emtricitabine in transgender women receiving feminizing hormone therapy. J Antimicrob Chemother 2020;75:1242–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Nieto O, Fehrenbacher AE, Cabral A, et al. Barriers and motivators to pre-exposure prophylaxis uptake among Black and Latina transgender women in Los Angeles: Perspectives of current PrEP users. AIDS Care 2021;33:244–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Barreras JL, Linnemayr SL, MacCarthy S. “We have a Stronger Survival Mode”: Exploring knowledge gaps and culturally sensitive messaging of PrEP among Latino men who have sex with men and Latina transgender women in Los Angeles, CA. AIDS Care 2019;31:1221–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cahill SR, Keatley J, Wade Taylor S, et al. “Some of Us, We Don't Know Where We're Going To Be Tomorrow.” Contextual factors affecting PrEP use and adherence among a diverse sample of transgender women in San Francisco. AIDS Care 2020;32:585–593. [DOI] [PubMed] [Google Scholar]
- 23. Horvath KJ, Todd K, Arayasirikul S, et al. Underutilization of pre-exposure prophylaxis services among transgender and nonbinary youth: Findings from Project Moxie and TechStep. Transgend Health 2019;4:217–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ogunbajo A, Storholm ED, Ober AJ, et al. Multilevel barriers to HIV PrEP uptake and adherence among Black and Hispanic/Latinx transgender women in Southern California. AIDS Behav 2021;25:2301–2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Poteat T, Wirtz A, Malik M, et al. A gap between willingness and uptake: Findings from mixed methods research on HIV prevention among Black and Latina transgender women. J Acquir Immune Defic Syndr 2019;82:131–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rael CT, Martinez M, Giguere R, et al. Barriers and facilitators to oral PrEP use among transgender women in New York City. AIDS Behav 2018;22:3627–3636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Restar AJ, Kuhns L, Reisner SL, et al. Acceptability of antiretroviral pre-exposure prophylaxis from a cohort of sexually experienced young transgender women in two U.S. cities. AIDS Behav 2018;22:3649–3657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wilson E, Chen Y-H, Pomart WA, et al. Awareness, interest, and HIV pre-exposure prophylaxis candidacy among young transwomen. AIDS Patient Care STDS 2016;30:147–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wood S, Lee S, Barg FK, et al. Young transgender women's attitudes toward HIV pre-exposure prophylaxis. J Adolesc Health 2017;60:549–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Andrzejewski J, Dunville R, Johns MM, et al. Medical gender affirmation and HIV and sexually transmitted disease prevention in transgender youth: Results from the Survey of Today's Adolescent Relationships and Transitions, 2018. LGBT Health 2021;8:181–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sevelius JM, Keatley J, Calma N, et al. ‘I am Not a Man’: Trans-specific barriers and facilitators to PrEP acceptability among transgender women. Glob Public Health 2016;11:1060–1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kuhns LM, Reisner SL, Mimiaga MJ, et al. Correlates of PrEP indication in a multi-site cohort of young HIV-uninfected transgender women. AIDS Behav 2016;20:1470–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zarwell M, John SA, Westmoreland D, et al. PrEP uptake and discontinuation among a U.S. National Sample of Transgender Men and Women. AIDS Behav 2021;25:1063–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wilson EC, Jin H, Liu A, et al. Knowledge, indications and willingness to take pre-exposure prophylaxis among transwomen in San Francisco, 2013. PLoS One 2015;10:e0128971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Westmoreland DA, Pantalone DW, Patel VV, et al. Demographic, behavioral, and geographic differences between men, transmen, and transwomen currently on PrEP, former PrEP users, and those having never used PrEP. AIDS Behav 2020;24:1304–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rael CT, Martinez M, Giguere R, et al. Knowledge about oral PrEP among transgender women in New York City. AIDS Behav 2019;23:2779–2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Brooks RA, Cabral A, Nieto O, et al. Experiences of pre-exposure prophylaxis stigma, social support, and information dissemination among Black and Latina transgender women who are using pre-exposure prophylaxis. Transgend Health 2019;4:188–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chandler CJ, Creasy SL, Adams BJ, et al. Characterizing biomedical HIV prevention awareness and use among Black transgender women in the United States. AIDS Behav 2021;25:2929–2940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Badgett MV, Choi SK, Wilson BDM. LGBT poverty in the United States: A study of differences between sexual orientation and gender identity groups. UCLA; 2019. Available at: https://escholarship.org/uc/item/37b617z8 (Last accessed March 31, 2022).
- 40. Wood S, Gross R, Shea JA, et al. Barriers and facilitators of PrEP adherence for young men and transgender women of color. AIDS Behav 2019;23:2719–2729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Reback CJ, Clark KA, Rünger D, et al. A promising PrEP navigation intervention for transgender women and men who have sex with men experiencing multiple syndemic health disparities. J Community Health 2019;44:1193–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Reisner S, Jadwin-Cakmak L, White Hughto J, et al. Characterizing the HIV Prevention and Care Continua in a sample of transgender youth in the U.S. AIDS Behav 2017;21:3312–3327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rowniak S, Ong-Flaherty C, Selix N, et al. Attitudes, beliefs, and barriers to PrEP among trans men. AIDS Educ Prev 2017;29:302–314. [DOI] [PubMed] [Google Scholar]
- 44. D'Avanzo PA, Bass SB, Brajuha J, et al. Medical mistrust and PrEP perceptions among transgender women: A cluster analysis. Behav Med 2019;45:143–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. D'Avanzo PA, Bass SB, Kelly PJ, et al. Community belonging and attitudes towards HIV pre-exposure prophylaxis (PrEP) among transgender women. AIDS Behav 2021;25:2728–2742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kuhns L, Reisner S, Mimiaga M, Gayles T, Shelendich M, Garofalo R. Correlates of PrEP indication in a multi-site cohort of young HIV-uninfected transgender women. AIDS Behav 2016;20:1470–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Grant RM, Pellegrini M, Defechereux PA, et al. Sex hormone therapy and tenofovir diphosphate concentration in dried blood spots: Primary results of the interactions between Antiretrovirals and Transgender Hormones Study. Clin Infect Dis 2021;73:e2117–e2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Rael CT, Lopez-Rios J, McKenna SA, et al. Transgender women's barriers, facilitators, and preferences on tailored injection delivery strategies to Administer Long-Acting Injectable Cabotegravir (CAB-LA) for HIV Pre-exposure Prophylaxis (PrEP). AIDS Behav 2021;25:4180–4192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Rael CT, Martinez M, Giguere R, et al. Transgender women's concerns and preferences on potential future long-acting biomedical HIV prevention strategies: The case of Injections and Implanted Medication Delivery Devices (IMDDs). AIDS Behav 2020;24:1452–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Landovitz RJ, Donnell D, Clement ME, et al. Cabotegravir for HIV prevention in cisgender men and transgender women. N Engl J Med 2021;385:595–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sevelius J, Murray LR, Martinez Fernandes N, et al. Optimising HIV programming for transgender women in Brazil. Cult Health Sex 2019;21:543–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Chakrapani V, Shunmugam M, Rawat S, et al. Acceptability of HIV pre-exposure prophylaxis among transgender women in India: A qualitative investigation. AIDS Patient Care STDS 2020;34:92–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Galka JM, Wang M, Azwa I, et al. Willingness to use pre-exposure prophylaxis (PrEP) for HIV prevention and PrEP implementation preferences among transgender women in Malaysia. Transgend Health 2020;5:258–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Jalil EM, Grinsztejn B, Velasque L, et al. Awareness, willingness, and PrEP eligibility among transgender women in Rio de Janeiro, Brazil. J Acquir Immune Defic Syndr 2018;79:445–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Wilson EC, Jalil EM, Castro C, et al. Barriers and facilitators to PrEP for transwomen in Brazil. Glob Public Health 2019;14:300–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Pleuhs B, Quinn KG, Walsh JL, et al. Health care provider barriers to HIV pre-exposure prophylaxis in the United States: A systematic review. AIDS Patient Care STDS 2020;34:111–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. McMahan VM, McCanta L, Tran D, et al. Administrative and related barriers to covering the costs of preexposure prophylaxis at a Safety-net Clinic in Seattle, Washington. Clin Infect Dis 2020;71:2509–2512. [DOI] [PubMed] [Google Scholar]
- 58. Calabrese SK, Magnus M, Mayer KH, et al. Putting PrEP into practice: Lessons learned from early-adopting U.S. providers' firsthand experiences providing HIV pre-exposure prophylaxis and associated care. PLoS One 2016;11:e0157324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Reisner SL, Radix A, Deutsch MB. Integrated and gender-affirming transgender clinical care and research. J Acquir Immune Defic Syndr 2016;72 Suppl 3(Suppl 3):S235–S242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Auerbach JD, Moran L, Watson C, et al. We are all women: Barriers and facilitators to inclusion of transgender women in HIV Treatment and Support Services Designed for Cisgender Women. AIDS Patient Care STDS 2020;34:392–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Wang Z, Lau J, Yang X, et al. Acceptability of daily use of free oral pre-exposure prophylaxis (PrEP) among transgender women sex workers in Shenyang, China. AIDS Behav 2017;21:3287–3298. [DOI] [PubMed] [Google Scholar]
- 62. Plotzker R, Seekaew P, Jantarapakde J, et al. Importance of risk perception: Predictors of PrEP acceptance among Thai MSM and TG women at a Community-Based Health Service. J Acquir Immune Defic Syndr 2017;76:473–481. [DOI] [PubMed] [Google Scholar]
- 63. Frasca K, Castillo-Mancilla J, McNulty MC, et al. A mixed methods evaluation of an inclusive sexual history taking and HIV Prevention Curriculum for Trainees. J Gen Intern Med 2019;34:1279–1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Bunting SR, Saqueton R, Batteson TJ. A guide for designing student-led, interprofessional community education initiatives about HIV risk and pre-exposure prophylaxis. MedEdPORTAL 2019;15:10818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Hoagland B, Moreira RI, De Boni RB, et al. High pre-exposure prophylaxis uptake and early adherence among men who have sex with men and transgender women at risk for HIV infection: The PrEP Brasil Demonstration Project. J Int AIDS Soc 2017;20:21472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Hood JE, Eljallad T, Abad J, et al. Getting pre-exposure prophylaxis to high-risk transgender women: lessons from Detroit, USA. Sex Health 2018;15:562–569. [DOI] [PubMed] [Google Scholar]
- 67. Reisner SL, Moore CS, Asquith A, et al. The pre-exposure prophylaxis cascade in at-risk transgender men who have sex with men in the United States. LGBT Health 2021;8:116–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Sevelius JM, Poteat T, Luhur WE, et al. HIV Testing and PrEP Use in a National Probability Sample of Sexually Active Transgender People in the United States. J Acquir Immune Defic Syndr 2020;84:437–442. [DOI] [PMC free article] [PubMed] [Google Scholar]


