Abstract
Background
There is an increasing demand for kidney retransplantation. Most studies report inferior outcomes compared to primary transplantation, consequently feeding an ethical dilemma in the context of chronic organ shortage.
Objective
To assess variables influencing long-term graft survival after kidney retransplantation. Material and Methods. All patients transplanted at our center between 2000 and 2016 were analyzed retrospectively. Survival was estimated with the Kaplan–Meier method, and risk factors were identified using multiple Cox regression.
Results
We performed 1,376 primary kidney transplantations and 222 retransplantations. The rate of retransplantation was 67.8% after the first graft loss, with a comparable 10-year graft survival compared to primary transplantation (67% vs. 64%, p=0.104) but an inferior graft survival thereafter (log-rank p=0.026). Independent risk factors for graft survival in retransplantation were age ≥ 50 years, time on dialysis ≥1 year, previous graft survival <2 years, ≥1 mild comorbidity in the Charlson–Deyo index, active smoking, and life-threatening complications (Clavien–Dindo grade IV) at first transplantation.
Conclusion
Graft survival is comparable for first and second kidney transplantation within the first 10 years. Risk factors for poor outcomes after retransplantation are previous graft survival, dialysis time after graft failure, recipient age, comorbidities, and smoking. Patients with transplant failure should have access to retransplantation as early as possible.
1. Introduction
The expansion of indications for kidney transplantation and the increasing use of extended criteria grafts inevitably lead to a higher number of patients with graft failure. Given the current high overall rate of kidney transplants, which will assumably continue to rise, the growing number of patients requiring kidney retransplantation is a challenge [1]. Furthermore, recent changes in organ allocation policy, with higher allocation scores for human leukocyte antigen (HLA) antibodies, indirectly enhance the likelihood of retransplantation in patients after graft failure [2, 3]. Patients undergoing kidney retransplantation benefit from improved survival [4–6] and better quality of life [7] compared to patients who remain on dialysis in this situation. In fact, return to dialysis after graft failure has poor outcomes with high mortality rates [8–11]. The outcome is then even inferior to dialysis prior to first transplantation [12]. Graft survival data after retransplantation are, however, controversial. Some studies report inferior outcomes compared to primary transplantation [13–15], while others present comparable results for retransplantations in the long-term follow-up [1, 16]. Data on risk factors for poor outcomes after retransplantation though are scarce. In the present work, as a first step, we characterize the cohort of patients who have received a second kidney transplant. The following and actual aim of the work is to identify candidate profiles who will benefit from retransplantation.
2. Methods
We retrospectively reviewed medical records of all patients who underwent kidney transplantation at our institution between January 1, 2000, and December 31, 2016. Patients were followed up until December 31, 2017. Due to the low number of third and fourth transplantations, we assessed first and second kidney transplantations only. The local ethics committee reviewed and approved the study protocol (project number 2018–00153).
We assessed recipient characteristics, including pre-, intra-, and postoperative parameters. The age-independent Charlson–Deyo index was used to estimate the impact of multiple recipient comorbidities [17]. Graft survival was defined as the time from transplantation until the patient returned to dialysis or died with a functioning graft. Patient survival was defined as the time from transplantation to death of the patient with or without a functional graft. Death-censored graft survival was defined by the time from transplantation to return to dialysis while censoring death with a functional graft. Extended criteria donor (ECD) was defined as age ≥60 years or 50 to 59 years with at least 2 of the following: arterial hypertension, serum creatinine level 132 μmol/l, and cerebrovascular cause of death [18].
Human leukocyte antigen (HLA) mismatch was defined as the number of mismatches within HLA A, B, and DR, totaling a maximum of 6 possible mismatches. HLA-donor-specific antibodies (DSA) detection was using a sensitive single antigen bead assay (Luminex®), and intensity was measured by mean fluorescence intensity (MFI). MFI levels above 1,000 were considered relevant. No patients were excluded from analysis, irrespective of MFI levels or previous episodes of acute rejection. However, it was our policy to avoid transplantations with DSA, especially with MFI levels > 1,000, whenever possible. All patients that underwent retransplantation received monoclonal antibodies for induction therapy (Thymoglobulin® or Basiliximab®).
We accounted our models for era effects, which occurred in May 2008 due to the start of allocation according to donor-specific antibodies. Complications were assessed according to the validated and severity-oriented Clavien–Dindo classification [19, 20].
2.1. Statistical Analysis
Statistical analysis was performed with IBM SPSS Statistics 25.0 (IBM Corp, 2015, Armonk, NY) and Stata 13.1 (StataCorp LP, College Station, Tex). Categorical variables were compared by chi-square test or Fisher exact test for expected frequencies <5. Continuous variables were analyzed by the Mann–Whitney test. Survival was estimated by the Kaplan–Meier method and compared with the log-rank test. Cox regression was used to assess risk factors for graft failure (using the time to failure or death as a dependent variable) as well as the chance of retransplantation (using the time to retransplantation as a dependent variable). First, every variable was checked with a univariate (enter) model. Variables with a p value <0.2 [21] were tested in a multivariable stepwise backward Cox regression model. The number of factors introduced into the final multivariable models was calculated by considering sample size and the number of occurring events (graft failure and retransplantation, respectively) [22]. To confirm that variables show a stable significance, they had to be frequent in number. Linear regression was used to test collinearity between variables. A variance inflation factor >5 and a tolerance <0.2 was defined as indicating a collinearity problem.
3. Results
3.1. Donor and Recipient Characteristics
Out of 1,598 kidney transplantations, 1,376 (86.1%) were first transplantations, 192 (12.0%) second, 28 (1.8%) third, and 2 (0.1%) were fourth transplantations. Loss of follow-up after first and second transplantations was 3.1% (n = 43) and 1.6% (n = 3), respectively. Second transplant patients had less diabetes or cystic disease as the underlying cause of primary kidney failure compared to first transplantation, 15.9% versus 6.8% and 16.7% versus 10.4%, respectively. The median duration of dialysis between first and second transplantation was longer than before the first transplant, 2.5 versus 1.7 years, respectively. Second transplant recipients were less likely to get an ECD or donor after circulatory death (DCD) graft, 25.9% versus 6.3% and 6.8% versus 0%, respectively. The living donation was also less frequent in the setting of second transplantation (32.3% vs. 22.4%). Detailed recipient characteristics are listed in Table 1.
Table 1.
Patient characteristics and surgical details.
| Patient's characteristics | 1st transplantation | 2nd transplantation | p value |
|---|---|---|---|
| n | 1,376 | 192 | |
| Age, median (years, range) | 48.4 (2–81) | 46.2 (13–73) | 0.3 |
| Gender (male/female (%)) | 63.2/36.8 | 62.5/37.5 | 0.8 |
|
| |||
| Time on dialysis, median (years, range) 1–3 years ≥3 years CAPD |
1.7 (0–15.5) 436 (32.7%) 408 (30.6%) 218 (15.8%) |
2.5 (0–17.7) 55 (29.4%) 85 (45.5%) 43 (22.4%) |
<0.001 0.002 <0.001 0.02 |
|
| |||
| Time on the waiting list, median (days, range) | 329 (0–13,951) | 623 (0–4,443) | 0.1 |
|
| |||
| BMI (kg/cm2) | |||
| >30 | 138 (10.0%) | 11 (5.7%) | 0.06 |
| <17 | 8 (0.6%) | 2 (1.0%) | 0.4 |
|
| |||
| Underlying disease | |||
| Diabetes | 219 (15.9%) | 13 (6.8%) | <0.001 |
| Hypertension | 204 (14.8%) | 21 (10.9%) | 0.2 |
| Glomerulopathy | 238 (17.3%) | 57 (29.7%) | <0.001 |
| Cystic disease | 230 (16.7%) | 20 (10.4%) | 0.02 |
|
| |||
| Types of transplantation | |||
| Preemptive | 232 (16.9%) | 14 (7.3%) | 0.001 |
| Living donors | 443 (32.3%) | 149 (22.4%) | 0.006 |
| (i) Unrelated | 239 (54%) | 92 (62%) | |
| (ii) Related | 204 (46%) | 57 (38%) | |
| (1) 1st degree | 94% | 82% | |
| (2) 2nd degree | 6% | 18% | |
| DCD | 94 (6.8%) | 2 (1.0%) | 0.002 |
| Extended donors | 357 (25.9%) | 12 (6.3%) | <0.001 |
|
| |||
| Charlson–Deyo index, median | 2 (2–8) | 2 (2–6) | 0.6 |
| Cold ischemia time, median (hours) | 8 (1–37) | 9 (1–29) | 0.6 |
|
| |||
| HLA mismatches | |||
| Median (range) | 3 (0–6) | 4 (0–6) | <0.001 |
| 0 | 92 (6.7%) | 2 (1.0%) | 0.002 |
| 1–2 | 347 (25.3%) | 35 (18.2%) | 0.03 |
| 3–5 | 831 (60.5%) | 136 (70.8%) | 0.005 |
| ≥6 | 104 (7.6%) | 19 (9.9%) | 0.05 |
|
| |||
| DSA | |||
| Any patient with DSA | 638 | 101 | |
| Median number (range) of DSA | 0 (0–5) | 0 (0–6) | <0.001 |
| Patients with: | |||
| No DSA | 541 (84.8%) | 54 (53.5%) | <0.001 |
| 1 DSA | 68 (10.7%) | 29 (28.7%) | <0.001 |
| 2 DSA | 20 (3.1%) | 12 (11.9%) | <0.001 |
| ≥3 DSA | 9 (1.4%) | 6 (5.9%) | 0.01 |
|
| |||
| DSA cumulative MFI | |||
| Median (range) | 0 (0–12,949) | 0 (0–25,741) | <0.001 |
| Mean ± SD | 361+/−50.6 | 2,087+/−432 | |
| 0 | 541 (84.8%) | 54 (53.5%) | <0.001 |
| 1–1,000 | 38 (6.0%) | 12 (11.9%) | 0.03 |
| 1,001–2,000 | 25 (3.9%) | 11 (10.9%) | 0.002 |
| >2,000 | 34 (5.3%) | 24 (23.8%) | <0.001 |
|
| |||
| Clavien–Dindo index, major | |||
| IIIb | 8.8% | 8.9% | 0.9 |
| IVa | 3.1% | 2.6% | 0.2 |
| IVb | 0.9% | 0% | 0.4 |
| V | 0.7% | 1.0% | 0.6 |
Note. BMI, body mass index (kg/m2); CAPD, continuous ambulatory peritoneal dialysis; DCD, donor after circulatory death; HLA, human leukocyte antigen; DSA, donor-specific antibody; MFI, mean fluorescence densitometry; SD, standard deviation.
Within our study period, 283 patients were evaluated for a first retransplantation. Of these 192 (67.8%) underwent a retransplantation. The main reason for the decline in patients for retransplantation was reduced physical condition, followed by malignancies and infection (Table 2).
Table 2.
Listing for retransplantation.
| 2nd transplantation | |
|---|---|
| n | 283 |
| Relisted and retransplanted | 192 (67.8%) |
|
| |
| On waiting list Death on waiting list Removed from list Patient moved to another country |
22 (7.8%) 2 (0.7%) 1 (0.4%) 1 (0.4%) |
|
| |
| Death while evaluation for wait-listing | 6 (2.1%) |
|
| |
| Excluded from retransplantation due to reduced general condition | 24 (8.5%) |
| Malignancy | 5 (1.8%) |
| Infection | 3 (1.1%) |
| Increased risk for rejection | 2 (0.7% |
| Compliance problems | 3 (1.1%) |
| Unknown | 6 (2.3%) |
|
| |
| Patient refused relisting | 15 (5.3%) |
3.2. Graft and Patient Survival
Graft survival is shown in Figure 1. Median graft survival for first and second kidney transplantation was 15.3 (95% CI 13.9–16.8) and 13.5 (95% CI 11.0–16.0) years, respectively. Overall graft loss was 35.1% and 36.0% after first and second kidney transplantation, respectively.
Figure 1.
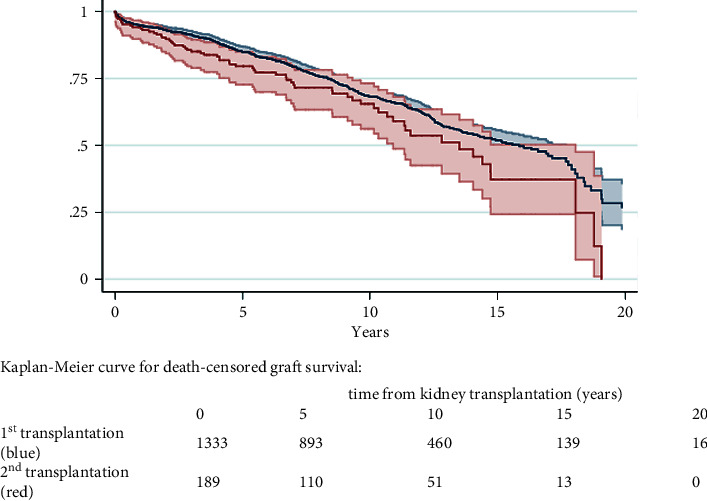
Graft survival.
While no significant difference in graft survival was seen within the first 10 years after transplantation (p=0.104), this changed over time and was then lower for retransplantation (p=0.026). Multiple Cox regression model, adjusted for recipient, donor, and era variables, identified the second transplantation as a risk factor for lower graft survival (p=0.003; Table 3).
Table 3.
Risk factors for graft loss in first and second transplantation.
| HR | 95% CI | p value | |
|---|---|---|---|
| Number of transplantations | |||
| 1 | Ref | ||
| 2 | 1.5 | 1.1–2.0 | 0.003 |
| ≥3 | 3.3 | 1.7–6.1 | <0.001 |
|
| |||
| Recipient age (years) | |||
| <50 | Ref | ||
| 50–59 | 1.2 | 0.9–1.6 | 0.1 |
| 60–69 | 1.9 | 1.4–2.5 | <0.001 |
| ≥70 | 2.9 | 1.8–4.8 | <0.001 |
|
| |||
| Time on dialysis (years) | |||
| <1 | Ref | ||
| 1-2 | 1.2 | 0.9–1.5 | 0.2 |
| 2–4 | 1.4 | 1.1–1.8 | 0.003 |
| >4 | 1.7 | 1.3–2.2 | <0.001 |
|
| |||
| Charlson–Deyo index∗ | |||
| 2 (kidney disease only) | Ref | ||
| 3 (≤1 mild comorbidity) | 1.2 | 0.9–1.6 | 0.1 |
| 4 (≥2 mild or 1 moderate comorbidity) | 1.8 | 1.4–2.4 | <0.001 |
| ≥5 (multiple comorbidities) | 2.3 | 1.7–3.0 | <0.001 |
|
| |||
| Smoking | 1.3 | 1.1–1.5 | 0.01 |
|
| |||
| Comorbidities∗ | |||
| Myocardial infarction | 1.3 | 1.0–1.7 | 0.04 |
| Congestive heart failure | 3.1 | 2.1–4.5 | <0.001 |
| PAD | 1.4 | 1.0–1.8 | 0.03 |
| Diabetes with end organ failure | 1.2 | 1.0–1.3 | 0.02 |
| Moderate – severe liver disease | 1.3 | 1.0–1.6 | 0.04 |
Note. HR, hazard ratio; CI, confidence interval; PAD, peripheral artery disease. ∗Charlson–Deyo index was analyzed for scoring points and in a second model using the same confounders for underlying comorbidities to avoid interactions.
The mortality rate was 16.8% and 16.9% after the first and second transplantation, respectively (p=0.9). Causes of death between the two groups did not differ significantly, with infections, heart failure, and malignancies being the main reasons for death in both groups.
3.3. Likelihood and Risk Factors for Retransplantation
Using time from graft loss to retransplantation as a dependent variable in a multiple Cox regression model, chances of retransplantation were higher among candidates younger than 65 years at the time of first graft loss, with less comorbidities (Charlson–Deyo index ≤ 3), and less than 3 years on dialysis. Previous graft survival of more than 5 years was also a positive prognostic factor for being retransplanted (Table 4). Multiple Cox regression model (Table 5) revealed the following as risk factors for graft survival in retransplantation: age ≥ 50 years, Charlson–Deyo index ≥ 3 (equal to ≥ 1 mild comorbidity), time on dialysis ≥ 1 year, previous graft survival < 2 years, active smoking, and life-threatening complications (Clavien–Dindo grade IV) at first transplantation. Previous graft loss due to acute rejection, a number of HLA mismatches, and DSA did not have a significant impact on the loss of the subsequent graft. When the detected risk factors for retransplantation (Table 5) were compared to the risk factors in the overall population (Table 3), retransplantation was revealed to be more vulnerable in regard to increasing age, comorbidities, and length of the previous dialysis, but not for increasing HLA mismatch.
Table 4.
Likelihood of retransplantation.
| LR | 95% CI | p value | |
|---|---|---|---|
| Age < 65 years at graft loss | 2.7 | 1.3–5.5 | 0.008 |
| ≤1 light comorbidity (Charlson–Deyo index ≤ 3) | 1.5 | 1.0–2.4 | 0.04 |
| BMI < 30 kg/m2 | 2.1 | 1.0–4.8 | 0.04 |
| Previous graft survival > 5 years | 1.5 | 1.1–2.0 | 0.01 |
| Prior dialysis < 3 years | 1.5 | 1.2–2.4 | 0.001 |
| Initial peritoneal dialysis | 1.5 | 1.1–2.2 | 0.02 |
| Number of previous transplantations | 1.4 | 1.0–2.0 | 0.04 |
Note. LR, likeliness ratio; CI, confidence interval; BMI, body mass index (kg/m2).
Table 5.
Risk factors for graft survival in retransplantation.
| HR | 95% CI | p value | |
|---|---|---|---|
| Age ≥ 50 years at retransplantation | 1.8 | 1.1–2.9 | 0.03 |
| ≥1 light comorbidity (Charlson–Deyo index ≥ 3) | 1.8 | 1.1–3.0 | 0.03 |
| Clavien–Dindo index ≥ IV after first transplantation | 2.9 | 1.1–7.5 | 0.03 |
| Previous graft survival < 2 years | 1.6 | 1.0–2.6 | 0.04 |
| Prior dialysis ≥ 1 year | 1.7 | 1.0–3.2 | 0.04 |
| Current smoker | 2.6 | 1.6–4.5 | <0.001 |
Note. HR, hazard ratio; CI, confidence interval.
4. Discussion
Kidney retransplantation accounts for approximately 15% of transplant activity [14, 23, 24], a number constantly increasing over the past two decades. Within this cohort, nearly two-thirds of patients losing their first graft were retransplanted. In times of chronic organ shortage, growing rates of retransplantations fuel the delicate discussion on utility and fairness.
Reports on graft survival after kidney retransplantation are conflicting and the prognosis of retransplantation compared to first transplantation remains unclear. Within our cohort, graft and patient survival rates within 10 years were comparable for first and second transplantations and seem to decline thereafter, favoring first transplantation. This time lag difference in outcome has been demonstrated before. Trèbern-Launay et al. showed an increased risk for graft failure in retransplantations, with a delayed effect becoming evident beyond 4 years of follow-up [13]. Magee et al. 2007 reported worse outcomes in retransplantation already from the first year post-transplantation [14]. On the other hand, there is data reporting comparable graft survival rates for retransplantation and first transplantation [16, 25]. Arnol et al. reported almost identical long-term graft survival up to 10 and 15 years [16]. Of note, in this particular study, the time between first and second transplantations was exceptionally short, with a median dialysis time of only 16 months. Another series reported equal incidence rates of acute rejection and 8-year survival rates [1].
There are currently no recommendations for the management of patients with a failed kidney transplant, nor are there clear decision criteria for relisting. To date, no scoring system to predict outcome after repeat kidney transplantation, such as the lung allocation score for lung transplantation [26], is available. Published data on this subject essentially has in common that the results of retransplantation are influenced by the outcome of the first transplantation [16, 27–29]. This is consistent with our analysis in which prolonged primary graft survival was protective for retransplant outcome. Nevertheless, recommendations for the management of patients after graft failure cannot yet be derived from this.
Our analyses show that there are indeed some risk factors for second graft loss and should have an impact on the management of patients after graft loss at initial transplantation. In our cohort, dialysis duration before retransplantation is a considerably stronger risk factor for graft loss than before initial transplantation. While dialysis for 2 or more years was a risk factor for first graft failure, the risk of subsequent organ loss after retransplantation is already present after 1 year of dialysis. These data are consistent with reports on the negative effect of waiting time and dialysis on kidney transplant outcomes [30–32], but the impact appears to be compounded after a second transplant. Dialysis time of less than 3 years significantly increased the likelihood of retransplantation in our cohort. Hence, the duration of dialysis is one of the strongest influencing factors for retransplantation. The patients in our cohort were on dialysis for an average of over 600 days before being retransplanted. This time on dialysis before repeat transplantation was long compared to other reports [16], probably reflecting low access to living donation for retransplantation. Results after living donor retransplantation are still superior compared to primary deceased donor transplantation [14], and preemptive living donations have a well-known beneficial effect on long-term graft survival, minimizing the morbidity associated with dialysis restart and improving clinical outcomes [30]. In our cohort, however, we did not detect a direct benefit for preemptive retransplantations, but we detected that duration of dialysis before retransplantation was a stronger risk factor for graft loss than the duration of dialysis before initial transplantation. This is particularly evident when dialysis time is exceeding one year. This indirectly suggests a beneficial effect for preemptive retransplantations.
Of note, smoking was the strongest risk factor for graft loss after retransplantation in our cohort. The adverse effects of smoking have been reported for primary transplants, being associated with an increased risk of graft loss and death [33, 34]. However, this has not yet been described for retransplantation. Consistent with prior studies, recipient age was a risk factor for graft loss [35, 36]. While the risk of graft loss for first transplants increased from the age of 60, this is true for retransplants already from 50. Interestingly, severe obesity was not a risk factor for retransplantation in our cohort. This is in contrast to previous studies [13, 28] and the general knowledge of elevated surgical risks in obese recipients [37–39]. However, this missing effect was probably related to the overall low rate of obese recipients in our cohort.
Retransplantations carry an increased immunological risk regarding rejection and complications of immunosuppression [16, 40]. However, in our cohort, a number of HLA mismatches were not a risk factor for graft survival, even though the number was higher for retransplantations. This is in line with previous studies [28, 41] but conversely to others [42]. The same is true for DSA. While the total number of DSA and rates of MFI were higher in retransplantations, we did not detect any influence on graft survival. In addition, we did not detect acute rejection as a predictor of second graft survival. This is conflicting with previous results that identified preformed DSA as a risk factor for acute rejection and graft loss in first transplantation and retransplantations [43, 44]. This missing association between immunologic risk factors and long-term retransplant outcome in our cohort has likely been positively influenced by our strict attempts to avoid DSA and MFI levels >1,000 in the last decade.
This study has some limitations. It is a retrospective analysis and readers need to consider the limitations and error rate of data. Loss of follow-up was very low for the transplanted population. However, we did not compare the results to a matched dialysis cohort after graft loss. Limited statement regarding survival benefits of retransplantation compared to staying on dialysis is possible.
Our results highlight the importance of including prior transplant outcomes to improve decision-making for repeat wait-listing and predicting retransplant outcomes. As long as consensus on relisting is lacking, a clear definition of risk factors is crucial to optimize patient selection for repeated transplantation. With this long-monitored cohort of retransplanted patients, we were able to identify risk factors that increase the risk of graft loss and should therefore be taken into account in the preparation for retransplantation. Most importantly, the data show that early relisting, which is associated with younger age of the patient and shorter dialysis time, increases the chances of longer graft survival. Relisting should therefore be initiated promptly, potentially before graft failure. However, this might be limited in patients with primary disease recurrence-related graft failure or those who lost their graft for antibody-mediated rejection. In this regard, the data also clearly show that patient adherence is essential medically but also with a focus on lifestyle, as a BMI <30 is more likely to lead to relisting and nicotine abstinence to longer graft survival.
5. Conclusion
Kidney retransplantation has comparable long-term outcomes to primary transplantation. Outcome after retransplantation depends on previous graft survival, dialysis time after first graft failure, recipient age, comorbidities, and smoking. Due to the excellent long-term outcome, patients with transplant failure should be offered retransplantation at the earliest.
Abbreviations
- BMI:
Body mass index
- CAPD:
Continuous ambulatory peritoneal dialysis
- DBD:
Donor after brain death
- DCD:
Donor after circulatory death
- DSA:
Donor specific antibody
- ECD:
Extended criteria donor
- HLA:
Human leukocyte antigen
- MFI:
Mean fluorescence intensity
- PAD:
Peripheral artery disease.
Data Availability
The data used to support the findings of this study are restricted by the ethics committee in Zürich in order to protect patients' privacy.
Conflicts of Interest
All authors declare that there are no conflicts of interest.
Authors' Contributions
Jonas Ehrsam and Fabian Rössler contributed equally.
References
- 1.Gruber S. A., Brown K. L., El-Amm J. M., et al. Equivalent outcomes with primary and retransplantation in African-American deceased-donor renal allograft recipients. Surgery . 2009;146(4):646–653. doi: 10.1016/j.surg.2009.05.020. [DOI] [PubMed] [Google Scholar]
- 2.Stewart D. E., Kucheryavaya A. Y., Klassen D. K., Turgeon N. A., Formica R. N., Aeder M. I. Changes in deceased donor kidney transplantation one year after KAS implementation. American Journal of Transplantation . 2016;16(6):1834–1847. doi: 10.1111/ajt.13770. [DOI] [PubMed] [Google Scholar]
- 3.Israni A. K., Salkowski N., Gustafson S., et al. New national allocation policy for deceased donor kidneys in the United States and possible effect on patient outcomes. Journal of the American Society of Nephrology . 2014;25:1842–1848. doi: 10.1681/asn.2013070784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ojo A. O., Wolfe R. A., Agodoa L. Y., et al. Prognosis after primary renal transplant failure and the beneficial effects of repeat transplantation: multivariate analyses from the United States renal data system. Transplantation . 1998;66(12):1651–1659. doi: 10.1097/00007890-199812270-00014. [DOI] [PubMed] [Google Scholar]
- 5.Rao P. S., Schaubel D. E., Wei G., Fenton S. S. A. Evaluating the survival benefit of kidney retransplantation. Transplantation . 2006;82(5):669–674. doi: 10.1097/01.tp.0000235434.13327.11. [DOI] [PubMed] [Google Scholar]
- 6.Clark S., Kadatz M., Gill J., Gill J. S. Access to kidney transplantation after a failed first kidney transplant and associations with patient and allograft survival: an analysis of national data to inform allocation policy. Clinical Journal of the American Society of Nephrology . 2019;14(8):1228–1237. doi: 10.2215/cjn.01530219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee A. J., Morgan C. L., Conway P., Currie C. J. Characterisation and comparison of health-related quality of life for patients with renal failure. Current Medical Research and Opinion . 2005;21(11):1777–1783. doi: 10.1185/030079905x65277. [DOI] [PubMed] [Google Scholar]
- 8.Kaplan B., Meier-Kriesche H. U. Death after graft loss: an important late study endpoint in kidney transplantation. American Journal of Transplantation . 2002;2(10):970–974. doi: 10.1034/j.1600-6143.2002.21015.x. [DOI] [PubMed] [Google Scholar]
- 9.Knoll G., Muirhead N., Trpeski L., Zhu N., Badovinac K. Patient survival following renal transplant failure in Canada. American Journal of Transplantation . 2005;5(7):1719–1724. doi: 10.1111/j.1600-6143.2005.00921.x. [DOI] [PubMed] [Google Scholar]
- 10.Rao P. S., Schaubel D. E., Jia X., Li S., Port F. K., Saran R. Survival on dialysis post-kidney transplant failure: results from the scientific registry of transplant recipients. American Journal of Kidney Diseases . 2007;49(2):294–300. doi: 10.1053/j.ajkd.2006.11.022. [DOI] [PubMed] [Google Scholar]
- 11.Bonani M., Achermann R., Seeger H., et al. Dialysis after graft loss: a swiss experience. Nephrology Dialysis Transplantation . 2020;35(12):2182–2190. doi: 10.1093/ndt/gfaa037. [DOI] [PubMed] [Google Scholar]
- 12.Johnston O., Rose C. L., Gill J. S. Risks and benefits of preemptive second kidney transplantation. Transplantation . 2013;95(5):705–710. doi: 10.1097/tp.0b013e31827a938f. [DOI] [PubMed] [Google Scholar]
- 13.Trébern-Launay K., Foucher Y., Giral M., et al. Poor long-term outcome in second kidney transplantation: a delayed event. PLoS One . 2012;7(10) doi: 10.1371/journal.pone.0047915.e47915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Magee J. C., Barr M. L., Basadonna G. P., et al. Repeat organ transplantation in the United States, 1996–2005. American Journal of Transplantation . 2007;7(s1):1424–1433. doi: 10.1111/j.1600-6143.2007.01786.x. [DOI] [PubMed] [Google Scholar]
- 15.Klintmalm G. B., Kaplan B. The kidney allocation system claims equity: it is time to review utility and fairness. American Journal of Transplantation . 2017;17(12):2999–3000. doi: 10.1111/ajt.14457. [DOI] [PubMed] [Google Scholar]
- 16.Arnol M., Prather J. C., Mittalhenkle A., Barry J. M., Norman D. J. Long-term kidney regraft survival from deceased donors: risk factors and outcomes in a single center. Transplantation . 2008;86(8):1084–1089. doi: 10.1097/tp.0b013e318187ba5c. [DOI] [PubMed] [Google Scholar]
- 17.Charlson M. E., Pompei P., Ales K. L., MacKenzie C. R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases . 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 18.Merion R. M., Ashby V. B., Wolfe R. A., et al. Deceased-donor characteristics and the survival benefit of kidney transplantation. JAMA . 2005;294(21):p. 2726. doi: 10.1001/jama.294.21.2726. [DOI] [PubMed] [Google Scholar]
- 19.Dindo D., Demartines N., Clavien P. A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of Surgery . 2004;240(2):205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clavien P. A., Barkun J., de Oliveira M. L., et al. The Clavien-Dindo classification of surgical complications: five-year experience. Annals of Surgery . 2009;250(2):187–196. doi: 10.1097/sla.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 21.Sauerbrei W. The use of resampling methods to simplify regression models in medical statistics. Journal of the Royal Statistical Society: Series A C . 1999;48(3):313–329. doi: 10.1111/1467-9876.00155. [DOI] [Google Scholar]
- 22.Hosmer D. L. S. Applied Logistic Regression . 2nd. Hoboken, NJ, USA: John Wiley & Sons; 2000. [Google Scholar]
- 23.Saran R., Li Y., Robinson B., et al. US renal data system 2015 annual data report: epidemiology of kidney disease in the United States. American Journal of Kidney Diseases . 2016;67:S1–S305. doi: 10.1053/j.ajkd.2015.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mourad G., Minguet J., Pernin V., et al. Similar patient survival following kidney allograft failure compared with non-transplanted patients. Kidney International . 2014;86(1):191–198. doi: 10.1038/ki.2014.6. [DOI] [PubMed] [Google Scholar]
- 25.Santos A. H., Jr., Casey M. J., Womer K. L. Analysis of risk factors for kidney retransplant outcomes associated with common induction regimens: a study of over twelve-thousand cases in the United States. Journal of Transplantation . 2017;2017:1–10. doi: 10.1155/2017/8132672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weiss E. S., Allen J. G., Merlo C. A., Conte J. V., Shah A. S. Lung allocation score predicts survival in lung transplantation patients with pulmonary fibrosis. The Annals of Thoracic Surgery . 2009;88(6):1757–1764. doi: 10.1016/j.athoracsur.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 27.Abouljoud M. S., Deierhoi M. H., Hudson S. L., Diethelm A. G. Risk factors affecting second renal transplant outcome, with special reference to primary allograft nephrectomy. Transplantation . 1995;60(2):138–143. doi: 10.1097/00007890-199507270-00005. [DOI] [PubMed] [Google Scholar]
- 28.Gjertson D. W. A multi-factor analysis of kidney regraft outcomes. Clinical Transplants . 2002;2:335–349. [PubMed] [Google Scholar]
- 29.Miles C. D., Schaubel D. E., Jia X., Ojo A. O., Port F. K., Rao P. S. Mortality experience in recipients undergoing repeat transplantation with expanded criteria donor and non-ECD deceased-donor kidneys. American Journal of Transplantation . 2007;7(5):1140–1147. doi: 10.1111/j.1600-6143.2007.01742.x. [DOI] [PubMed] [Google Scholar]
- 30.Mange K. C., Joffe M. M., Feldman H. I. Effect of the use or nonuse of long-term dialysis on the subsequent survival of renal transplants from living donors. New England Journal of Medicine . 2001;344(10):726–731. doi: 10.1056/nejm200103083441004. [DOI] [PubMed] [Google Scholar]
- 31.Meier-Kriesche H. U., Kaplan B. Waiting time on dialysis as the strongest modifiable risk factor for renal transplant outcomes: a paired donor kidney analysis. Transplantation . 2002;74(10):1377–1381. doi: 10.1097/00007890-200211270-00005. [DOI] [PubMed] [Google Scholar]
- 32.Wong G., Chua S., Chadban S. J., et al. Waiting time between failure of first graft and second kidney transplant and graft and patient survival. Transplantation . 2016;100(8):1767–1775. doi: 10.1097/tp.0000000000000953. [DOI] [PubMed] [Google Scholar]
- 33.Ghadian A., Nemati E., Rostami Z., Einollahi B. Impact of cigarette smoking on kidney transplant recipients: a systematic review. Iranian Journal of Kidney Diseases . 2011;5(3):p. 141. [PubMed] [Google Scholar]
- 34.Sung R. S., Althoen M., Howell T. A., Ojo A. O., Merion R. M. Excess risk of renal allograft loss associated with cigarette smoking. Transplantation . 2001;71(12):1752–1757. doi: 10.1097/00007890-200106270-00009. [DOI] [PubMed] [Google Scholar]
- 35.Sood P., Gao X., Mehta R., et al. Kidney transplant outcomes after primary, repeat and kidney after nonrenal solid organ transplantation: a single-center experience. Transplantation Direct . 2016;2(6):p. e75. doi: 10.1097/txd.0000000000000586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ingsathit A., Kantachuvesiri S., Rattanasiri S., et al. Long-term outcome of kidney retransplantation in comparison with first kidney transplantation: a report from the Thai transplantation registry. Transplantation Proceedings . 2013;45(4):1427–1430. doi: 10.1016/j.transproceed.2012.08.029. [DOI] [PubMed] [Google Scholar]
- 37.Curran S. P., Famure O., Li Y., Kim S. J. Increased recipient body mass index is associated with acute rejection and other adverse outcomes after kidney transplantation. Transplantation . 2014;97(1):64–70. doi: 10.1097/tp.0b013e3182a688a4. [DOI] [PubMed] [Google Scholar]
- 38.Cannon R. M., Jones C. M., Hughes M. G., Eng M., Marvin M. R. The impact of recipient obesity on outcomes after renal transplantation. Annals of Surgery . 2013;257(5):978–984. doi: 10.1097/sla.0b013e318275a6cb. [DOI] [PubMed] [Google Scholar]
- 39.Lynch R. J., Ranney D. N., Shijie C., Lee D. S., Samala N., Englesbe M. J. Obesity, surgical site infection, and outcome following renal transplantation. Annals of Surgery . 2009;250(6):1014–1020. doi: 10.1097/sla.0b013e3181b4ee9a. [DOI] [PubMed] [Google Scholar]
- 40.Pham P. T., Everly M., Faravardeh A., Pham P. C. Management of patients with a failed kidney transplant: dialysis reinitiation, immunosuppression weaning, and transplantectomy. World Journal of Nephrology . 2015;4(2):p. 148. doi: 10.5527/wjn.v4.i2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dinis P., Nunes P., Marconi L., et al. Kidney retransplantation: removal or persistence of the previous failed allograft? Transplantation Proceedings . 2014;46(6):1730–1734. doi: 10.1016/j.transproceed.2014.05.029. [DOI] [PubMed] [Google Scholar]
- 42.Tinckam K. J., Rose C., Hariharan S., Gill J. Re-examining risk of repeated HLA mismatch in kidney transplantation. Journal of the American Society of Nephrology . 2016;27(9):2833–2841. doi: 10.1681/asn.2015060626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lucisano G., Thiruvengadam S., Hassan S., et al. Donor-specific antibodies detected by single antigen beads alone can help risk stratify patients undergoing retransplantation across a repeat HLA mismatch. American Journal of Transplantation . 2020;20(2):441–450. doi: 10.1111/ajt.15595. [DOI] [PubMed] [Google Scholar]
- 44.Betjes M. G. H., Sablik K. S., Otten H. G., Roelen D. L., Claas F. H., de Weerd A. Pretransplant donor-specific anti-HLA antibodies and the risk for rejection-related graft failure of kidney allografts. Journal of Transplantation . 2020;2020:10. doi: 10.1155/2020/5694670.5694670 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are restricted by the ethics committee in Zürich in order to protect patients' privacy.


