Summary
Background
Knowledge of the adverse problems related to SARS-CoV-2 infection in marginalised and deprived groups may help to prioritise more preventive efforts in these groups. We examined adverse outcomes associated with SARS-CoV-2 infection among vulnerable segments of society.
Methods
Using health and administrative registers, a population-based cohort study of 4.4 million Danes aged at least 15 years from 27 February 2020 to 15 October 2021 was performed. People with 1) low educational level, 2) homelessness, 3) imprisonment, 4) substance abuse, 5) supported psychiatric housing, 6) psychiatric admission, and 7) severe mental illness were main exposure groups. Chronic medical conditions were included for comparison. COVID-19-related outcomes were: 1) hospitalisation, 2) intensive care, 3) 60-day mortality, and 4) overall mortality. PCR-confirmed SARS-CoV-2 infection and PCR-testing were also studied. Poisson regression analysis was used to compute adjusted incidence and mortality rate ratios (IRRs, MRRs).
Findings
Using health and administrative registers, we performed a population-based cohort study of 4,412,382 individuals (mean age 48 years; 51% females). In all, 257,450 (5·8%) individuals had a PCR-confirmed SARS-CoV-2 infection. After adjustment for age, calendar time, and sex, we found that especially people experiencing homelessness had high risk of hospitalisation (IRR 4·36, 95% CI, 3·09-6·14), intensive care (IRR 3·12, 95% CI 1·29-7·52), and death (MRR 8·17, 95% CI, 3·66-18·25) compared with people without such experiences, but increased risk was found for all studied groups. Furthermore, after full adjustment, including for status of vaccination against SARS-CoV-2 infection, individuals with experiences of homelessness and a PCR-confirmed SARS-CoV-2 infection had 41-times (95% CI, 24·84-68·44) higher risk of all-cause death during the study period compared with individuals without. Supported psychiatric housing was linked to almost 3-times higher risk of hospitalisation and 60-day mortality following SARS-CoV-2 infection compared with the general population with other living circumstances.
Interpretation
Socially marginalised and psychiatrically vulnerable individuals had substantially elevated risks of adverse health outcomes following SARS-CoV-2 infection. The results highlight that pandemic preparedness should address inequalities in health, including infection prevention and vaccination of vulnerable groups.
Funding
Novo Nordisk Foundation.
Keywords: SARS-Cov-2, SARS Virus, COVID-19, Homeless Persons, Psychiatry, Public health, Prisoners, Substance-Related Disorders, Disease, Pandemics, Epidemiology, Registries, Health policy, Death, Hospitalizaiton, Intenstive Care Units, Health Disparity, Minority and Vulnerable Populations, Vulnerable populations, Social Vulnerability
Research in context.
Evidence before this study
We searched PubMed for studies of social, psychiatric, and medical factors and Covid-19-related outcomes. We used the terms: “homeless*”, “shelter*”, “prison*”, “jail*”, “detention*”, “psych*”, “mental*”, “substance*”, “misuse*”, “alcohol use disorder*”, “drug use disorder*”, (combined with “OR”) “AND” “coronavirus”, “Covid-19”, “2019-nCoV”, “SARS-CoV-2” (combined with “OR”) in November, 2020 without language restrictions. Since, we have received weekly alerts. We scanned reference lists to identify important papers.
Predictors of adverse Covid-19-related outcomes include e.g. high age, male sex, non-White ethnicity, and medical disorders. Meta-analyses have confirmed a link between mental disorders and increased risk of severe health outcomes in people with SARS-CoV-2 infection. Studies have linked overcrowding to increased risk of SARS-CoV-2 infection and outbreaks of SARS-CoV-2 infection have been reported in homeless shelters and prisons, primarily in the USA.
Little is known of the associations between specific factors measuring social deprivation and the risk of morbidity and mortality following SARS-CoV-2 infection. Population-based studies including homelessness, imprisonment, and specific psychiatric groups, e.g. individuals in supported psychiatric housing, have been lacking.
Most studies of vulnerable subgroups have been limited to selected geographical areas, included small study samples, cross-sectional study design, or short follow-up.
No previous population-based study has been able to analyse risks of adverse health problems according to social, psychiatric, and medical predictors in detail with long follow-up ending after all individuals have been offered two doses of vaccine against SARS-CoV-2 infection.
Added value of this study
We studied 4.4 million individuals from age 15 years and above followed for around 20 months with complete information on PCR-test and SARS-CoV-2 infection. A total of 257,450 (5·8%) individuals had a confirmed SARS-CoV-2 infection.
Socially marginalised and psychiatrically vulnerable individuals had substantially elevated risks of adverse health outcomes following SARS-CoV-2 infection. Representative data on people with low educational level, or experiences of homelessness, imprisonment, substance abuse, supported psychiatric housing, psychiatric admission, severe mental illness, and chronic medical conditions were presented. Even following adjustment for vaccination status, most of these groups had markedly higher morbidity and mortality than people from the general population not being in the specific groups.
Especially high vulnerability was found for individuals experiencing homelessness. Among people with SARS-CoV-2 infection, people using homeless shelters in Denmark had around 4-times higher risk of hospital admission and 8-times higher risk of death compared with people without homeless shelter experiences.
Implications of all the available evidence
The compiled evidence confirms that psychiatrically vulnerable groups, including those in supported psychiatric housing, constituted a high-risk group as regards adverse health outcomes in high-income countries during the COVID-19 pandemic. Individuals with psychiatric morbidity should be prioritised to an even higher degree for infection prevention and vaccination. In addition to this, we now have documentation of severe health problems during the pandemic associated with homelessness, imprisonment, and a low educational level in Denmark with a well-established safety net.
While our results suggested lower PCR-confirmed infection rates and reduced testing in the socially and psychiatrically vulnerable groups, these findings are not consistent or easily compared with other studies. The compiled evidence strengthens the argument of focusing on infection prevention and vaccination of vulnerable groups, with a stronger focus on psychiatric and social vulnerability to reduce problems with inequality in health during and after a pandemic. From a research perspective, there is a need for studying vulnerable groups in future e.g. focusing on the effect of vaccination, the interaction between social factors and psychiatric morbidity, test patterns, and long-term morbidity.
Alt-text: Unlabelled box
The coronavirus disease 2019 (COVID-19) pandemic remains a worldwide health problem.1 Vaccine against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection has high efficacy.2 Two doses of the mRNA COVID-19 vaccines (and during a later stage where the delta (B.1.617.2) variant became the predominant driver of the pandemic a third dose) have been found to have high effectiveness in preventing SARS-CoV-2 infection and protecting against morbidity and mortality across age-groups based on real-world data.3,4 However, factors such as limited access to vaccines, fear of being vaccinated, and possible waning immunity over time, make global immunisation a difficult target to reach.5 Socially marginalised individuals (especially those experiencing homelessness or imprisonment)6,7 but also individuals with mental disorders and substance abuse have been found have lower vaccine uptake than in the general population in a few high-income countries.
Crowding has been associated with an increased risk of infection.8 Marginalised population groups such as people experiencing homelessness, psychiatric disorders, and imprisonment are often living in crowded settings9 and have high prevalence of underlying disorders.10 Chronic medical conditions and mental disorders have consistently been associated with increased risk of hospitalisation and mortality in people infected with SARS-CoV-2.11, 12, 13 In a systematic review of people experiencing homelessness, increased risk of SARS-CoV-2 infection, morbidity and mortality has been suggested, but the literature is scarce.14 However, the importance of preventing infections in marginalised sub-groups has been claimed,15, 16, 17 and vaccination against COVID-19 has in some countries, e.g. in Denmark and the UK, been prioritised also for people with severe mental disorders,15,18 and people experiencing homelessness.7 COVID-19 outbreaks have been reported in shelters for homeless people,14,19 but representative data on individuals experiencing homelessness, imprisonment, supported psychiatric housing, and substance abuse is lacking.20,21 Social disadvantage, psychiatric disorders, and chronic medical conditions often co-occur,16 and studies compiling information on these factors are relevant.
Our primary hypotheses were that population groups with experiences of social marginalisation and with severe psychiatric morbidity, including substance abuse, would have high risk of SARS-CoV-2 infection-related severe health outcomes similar to or even higher than people with chronic medical conditions. Our secondary hypothesis was that especially people experiencing social marginalisation, but also people with severe psychiatric morbidity and substance abuse would have high risk of PCR-confirmed SARS-CoV-2 infection compared with individuals from the general population.
Using Danish nationwide registers, we aimed to study whether social marginalisation and psychiatric vulnerability were associated with SARS-CoV-2 infection-related adverse outcomes: hospitalisation, intensive care, and mortality in a population-based sample.
Methods
Study design and participants
We conducted a nationwide, register-based cohort study including all people born prior to October 15, 2006, from 15 years of age and above living in Denmark on Feb 27, 2020 (i.e. date of the first confirmed case of SARS-CoV-2 infection in Denmark)22 with follow-up until Oct 15, 2021. Individuals having their 15th year birthday during the follow-up period were included from that specific date. The cohort was constructed using the Danish Civil Registration System, containing information on e.g. vital status and postal address. Danish residents are assigned a personal identification number (the CPR number) which is used for accurate linkage between registers.23,24
Data
Exposures
Population groups selected for this study were individuals with 1) a low educational level, /or experiences of 2) homelessness, 3) imprisonment, 4) substance abuse, 5) supported psychiatric housing, 6) psychiatric admission, 7) severe mental illness, and 8) chronic medical condition. The last group was primarily included for comparison as medical disorders have been documented to be associated with high risk of severe outcomes in several large studies.13 Disorders were pre-existing, referring to the time prior to Feb 27, 2020. Supplementary groups studied were individuals with crisis shelter stays, alcohol and drug use disorder, and any mental disorder (Appendix, Supplementary table 1, p. 1-2).
To establish the most recent residence in supported psychiatric and social (i.e. homeless and crisis shelters) housing facilities, postal addresses of these facilities in Denmark from the official Danish national website “Tilbudsportalen” were obtained and linked with individual-level postal address information from the Civil Registration Register. Information on homelessness was primarily retrieved from the Danish Homeless Register, 1999-2020. Individuals experiencing homelessness was in the current study defined as individuals having at least one homeless shelter contact or residing in a homeless shelter at some point during a three-year period from 2018 and until 2021. Thus, the definition was comparable to previous Danish register-studies of homelessness.25,26 This definition covers primarily the homeless shelter population using temporary accommodation under the Consolidation Act on Social Services, Section 110. In Denmark, this type of accommodation should be offered by the municipalities to people without a home or who cannot live in their own home who also have special problems and need some extra support. A CPR-number is furthermore required for this type of accommodation.27 Thus, if compared to FEANTSA's homelessness definition, our definition covers primarily the “Houselessness” under the operational category: “People in accommodation for homelessness”.28 Since our definition is broad, it also includes people shifting between a living situation as “Houseless” and some of the other living situations: “Rooflessness”, “Insecure Housing”, and “Inadequate Housing”.28 Data on imprisonments was obtained from the Danish Central Criminal Register, 1991-2020, and information on imprisonment was included for the period 2018-2020 (Appendix, Supplementary table 1, p. 1-2).
Data on psychiatric disorders including substance abuse was obtained from the Danish National Patient Register,29 containing information on public and private psychiatric admissions, outpatient contacts, and diagnoses since 1995. Information on psychiatric diagnoses 1967-1995 was retrieved from the Danish Psychiatric Central Research Register.30 The psychiatric diagnoses were defined according to the international Classification of Disease 10th revision (ICD-10) and corresponding ICD-8 codes. Relevant prescriptions from the Danish National Prescription Registry31 and self-reported data on treatment from the Registry of Drug Abusers Undergoing Treatment (SIB)32 and the National Registry of Alcohol Treatment (NAB)33 were included in the definition of substance abuse. For alcohol use disorders, a few medical diagnostic codes were included (Appendix, Supplementary table 2, p. 3).
Information on medical conditions was collected from the Danish National Patient Register29 providing dates and diagnoses from all somatic inpatient contacts since 1977 and outpatient contacts since 1995. An algorithm from a previous study including 31 specific medical conditions was used in the definitions.34 Information on dispensed prescriptions including dates and Anatomical Therapeutic Chemical (ATC) codes was collected from the Danish National Prescription Registry (Appendix, Supplementary table 3, p. 4-5). The 31 medical conditions could furthermore be placed within the following nine general medical condition categories: the circulatory system, the endocrine system, the pulmonary system and allergy, the gastrointestinal system, the urogenital system, the musculoskeletal system, the haematological system, cancers, and the neurological system.34 We defined chronic medical conditions as having at least one of these previously defined conditions whereas the non-exposed group included individuals without any of these conditions.
Legal permission was obtained from the Danish Data Protection Agency (P-2020-439), Statistics Denmark, and the Danish Health Data Authority. Ethical permission is not required for register-based studies according to Danish regulations.
Outcomes
The primary outcomes were a) hospitalisation (duration more than 12 hours) and b) intensive care within 14 days from a PCR-confirmed SARS-CoV-2 infection, c) mortality within 60 days from a positive PCR-test, and d) all-cause mortality during follow-up. Dates of all positive PCR-tests based on throat swabs and conducted in any of the free-of-charge Danish test stations were retrieved from the national Danish Microbiology Database (MiBa),22,35 with the last update on October 15, 2021. PCR-test data were provided through the Danish Health Data Authority. Information on follow-up mortality was provided from the Civil Registration System.
We also studied the secondary outcomes a) PCR-confirmed SARS-CoV-2 infection and b) having a PCR-test during the study period.
Statistical analyses
Each of the four outcomes (a-d) were analysed separately. Thus, we fitted a separate Poisson regression model for each of the outcomes. In the analyses of outcome a-c, cohort participants were followed from the date of a PCR-confirmed SARS-CoV-2 infection (at the earliest on the cohort member's 15th birthday) and until they experienced one of the outcomes (hospitalisation, intensive care, or mortality), were lost to follow-up e.g. due to emigration, or end of the study period on Oct 15, 2021. In the two analyses of morbidity (a-b), individuals who died during follow-up were censored. In the analysis of outcome d (i.e. all-cause mortality during follow-up) and of the secondary outcome a (i.e. PCR-confirmed SARS-CoV-2 infection), cohort members were followed from Feb 27, 2020 or their 15th birthday (flow-chart in Appendix p. 6). Poisson regression analysis approximates a Cox regression and was used to calculate incidence rate ratios (IRRs), mortality rate ratios (MRRs), and Wald 95% confidence intervals (CIs). We performed the regression analyses for each of the eight population groups (i.e., eight main analyses per outcome) in which all individuals qualifying for the analysis were included, without adjusting for the other population groups. All the regression analyses were adjusted for age (5-year groups), sex (male, female), and calendar time (in months). In a second model, country of birth (Denmark, other Western countries, or non-Western countries), living area (defined as the area of postal address at the time of study separated in the following 11 large Danish areas: Capital City Region Copenhagen (including any missing values), Metropolitan Copenhagen, North Zealand, West- and South Zealand, East Zealand, Region of Southern Denmark, North Jutland Region, Mid Jutland Region, West Jutland Region, South Jutland Region, and Bornholm), and vaccination against SARS-CoV-2 infection (2 doses of vaccine, 1 dose, or no vaccine) were included.7 We furthermore included a fully adjusted model that in addition to model 2 were mutually adjusted for all other population groups studied (outcome a-c). Residential covariates were handled as time-dependent variables. An age- and sex-adjusted logistic regression analysis was conducted to study the association between the population groups and the odds of having a PCR-test for SARS-CoV-2 infection (secondary outcome b). Furthermore, we studied whether sex modified the association between each population group and hospitalisation and death (outcome a and c), respectively, on the multiplicative (tested with Likelihood ratio test) and additive scale (calculation of RERI) in the individuals with SARS-CoV-2-infection.36
To study the absolute numbers of the adverse outcomes (a-c) as well as PCR-confirmed SARS-CoV-2 infection by population group compared with “non-exposed” (i.e. those not qualifying for the specific population group studied in each analysis) individuals in the general Danish population aged 15 years and above (for these analyses, individuals had to be 15 years of age from the beginning of follow-up), the Aalen-Johansson estimator was used to calculate cumulative incidence functions considering competing risks from loss to follow-up due to emigration.37 Additionally, in the analysis of hospitalisation and intensive care (a-b) and of SARS-CoV-2 infection, death was also considered as a competing risk. Gray's test was used to study whether there was evidence of difference between the groups at a type I error rate (alpha) of 5%.38 All curves were smoothed to ensure anonymity of cohort members. The statistical analyses were performed using SAS software (version 9.4.).
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the manuscript. SFN, MO, and CH had full access to all the data in the study, and all authors approved the final manuscript as submitted.
Results
From February 27, 2020, to October 15, 2021, 4,412,382 individuals (2,232,650 females and 2,179,732 males) were included in the cohort accounting for 7,007,288 person-years at risk. The mean age of participants was 48 (SD=20) years. The sub-cohort with PCR-confirmed SARS-CoV-2 infection consisted of 257,450 (5·8%) individuals with a mortality rate (MR) of 71 (95% CI, 68-73) per 1000 person-years. All the studied population groups had higher unadjusted rates of adverse outcomes (Table 1). Results for the supplementary population groups are presented in Appendix.
Table 1.
Study characteristics in the general population and in individuals with PCR-confirmed SARS-CoV-2 infection.
| General population |
PCR-confirmed SARS-CoV-2 infected individuals |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Deaths |
Deaths within 60 days |
Hospitalisation within 14 days |
Intensive care within 14 days |
|||||||||||||
| n | Pyrs* | MR† | (95% CI) | n | Pyrs* | MR† | (95% CI) | n | Pyrs* | IR† | (95% CI) | n | Pyrs* | IR† | (95% CI) | |
| Total | 82,171 | 7,007,288 | 12 | (12-12) | 2863 | 40,446 | 71 | (68-73) | 11,232 | 10,057 | 1117 | (1096-1138) | 1395 | 10,387 | 134 | (127-142) |
| Age, years mean (SD) | 48 (20) | 40 (18) | ||||||||||||||
| Sex | ||||||||||||||||
| Male | 41,910 | 3,457,218 | 12 | (12-12) | 1568 | 19,892 | 79 | (75-83) | 6062 | 4923 | 1231 | (1201-1263) | 921 | 5101 | 181 | (169-193) |
| Female | 40,261 | 3,550,070 | 11 | (11-11) | 1295 | 20,554 | 63 | (60-67) | 5170 | 5134 | 1007 | (980-1035) | 474 | 5286 | 90 | (82-98) |
| Country of origin | ||||||||||||||||
| Denmark | 77,937 | 6,100,164 | 13 | (13-13) | 2574 | 29,593 | 87 | (84-90) | 8096 | 7332 | 1104 | (1080-1129) | 1027 | 7584 | 135 | (127-144) |
| Other Western countries | 2212 | 331,886 | 7 | (6-7) | 69 | 1932 | 36 | (28-45) | 393 | 494 | 796 | (721-879) | 43 | 505 | 85 | (63-115) |
| Non-Western countries | 2022 | 575,238 | 4 | (3-4) | 220 | 8922 | 25 | (22-28) | 2743 | 2232 | 1229 | (1184-1276) | 325 | 2298 | 141 | (127-158) |
| Vaccination | ||||||||||||||||
| Two doses | 22,872 | 1,221,948 | 19 | (18-19) | 154 | 2678 | 58 | (49-67) | 490 | 628 | 781 | (714-853) | 43 | 644 | 67 | (50-90) |
| One dose | 3892 | 357,667 | 11 | (11-11) | 298 | 2937 | 101 | (91-114) | 529 | 665 | 796 | (731-867) | 44 | 681 | 65 | (48-87) |
| No vaccine | 55,407 | 5,427,673 | 10 | (10-10) | 2411 | 34,832 | 69 | (67-72) | 10,213 | 8765 | 1165 | (1143-1188) | 1308 | 9062 | 144 | (137-152) |
| Low educational level | ||||||||||||||||
| Yes | 36,355 | 1,962,318 | 19 | (18-19) | 1242 | 12,563 | 99 | (94-105) | 3853 | 3109 | 1239 | (1201-1279) | 489 | 3227 | 152 | (139-166) |
| No | 45,816 | 5,044,970 | 9 | (9-9) | 1621 | 27,883 | 58 | (55-61) | 7379 | 6948 | 1062 | (1038-1087) | 906 | 7160 | 127 | (119-135) |
| Homelessness | ||||||||||||||||
| Yes | 313 | 10,697 | 29 | (26-33) | 6 | 47 | 128 | (58-286) | 33 | 11 | 3084 | (2192-4338) | 5 | 12 | 413 | (172-991) |
| No | 81,858 | 6,996,591 | 12 | (12-12) | 2857 | 40,399 | 71 | (68-73) | 11,199 | 10,046 | 1115 | (1094-1136) | 1390 | 10,375 | 134 | (127-141) |
| Imprisonment | ||||||||||||||||
| Yes | 881 | 59620 | 15 | (14-16) | 17 | 306 | 56 | (35-89) | 113 | 76 | 1491 | (1240-1792) | 21 | 79 | 265 | (173-406) |
| No | 81,290 | 6947668 | 12 | (12-12) | 2846 | 40,140 | 71 | (68-74) | 11,119 | 9981 | 1114 | (1094-1135) | 1374 | 10,308 | 133 | (126-141) |
| Substance abuse | ||||||||||||||||
| Yes | 13,197 | 498,119 | 26 | (26-27) | 346 | 1873 | 185 | (166-205) | 938 | 454 | 2067 | (1939-2203) | 126 | 488 | 258 | (217-307) |
| No | 68,974 | 6,509,169 | 11 | (11-11) | 2517 | 38,574 | 65 | (63-68) | 10,294 | 9603 | 1072 | (1051-1093) | 1269 | 9899 | 128 | (121-135) |
| Supported psychiatric housing | ||||||||||||||||
| Yes | 267 | 14,791 | 18 | (16-20) | 11 | 68 | 163 | (90-294) | 39 | 16 | 2409 | (1760-3297) | … | … | … | … |
| No | 81,904 | 6,992,497 | 12 | (12-12) | 2852 | 40,379 | 71 | (68-73) | 11,193 | 10,041 | 1115 | (1094-1136) | … | … | … | … |
| Psychiatric admission | ||||||||||||||||
| Yes | 1723 | 21,534 | 80 | (76-84) | 75 | 115 | 655 | (522-821) | 99 | 3609 | 3609 | (2964-4395) | 13 | 31 | 416 | (241-716) |
| No | 80,448 | 6,985,754 | 12 | (11-12) | 2788 | 40,332 | 69 | (67-72) | 11,133 | 10,029 | 1110 | (1090-1131) | 1382 | 10,356 | 133 | (127-141) |
| Severe mental illness | ||||||||||||||||
| Yes | 9277 | 375,747 | 25 | (24-25) | 354 | 1699 | 208 | (188-231) | 1073 | 409 | 2622 | (2470-2784) | 118 | 444 | 266 | (222-318) |
| No | 72,894 | 6,631,541 | 11 | (11-11) | 2509 | 38,747 | 65 | (62-67) | 10,159 | 9648 | 1053 | (1033-1074) | 1277 | 9943 | 128 | (122-136) |
| Chronic medical condition | ||||||||||||||||
| Yes | 72,840 | 3,528,327 | 21 | (20-21) | 2611 | 16,741 | 156 | (150-162) | 8707 | 4066 | 2142 | (2097-2187) | 1120 | 4330 | 259 | (244-274) |
| No | 9331 | 3,478,961 | 3 | (3-3) | 252 | 23,705 | 11 | (9-12) | 2525 | 5991 | 421 | (405-438) | 275 | 6057 | 45 | (40-51) |
SARS-CoV-2 infection=severe acute respiratory syndrome coronavirus, Pyrs=person-years, MR=mortality rate, IR=incidence rate.
Person-years may not sum up to group total due to rounding.
Unadjusted rates per 1000 person-years.
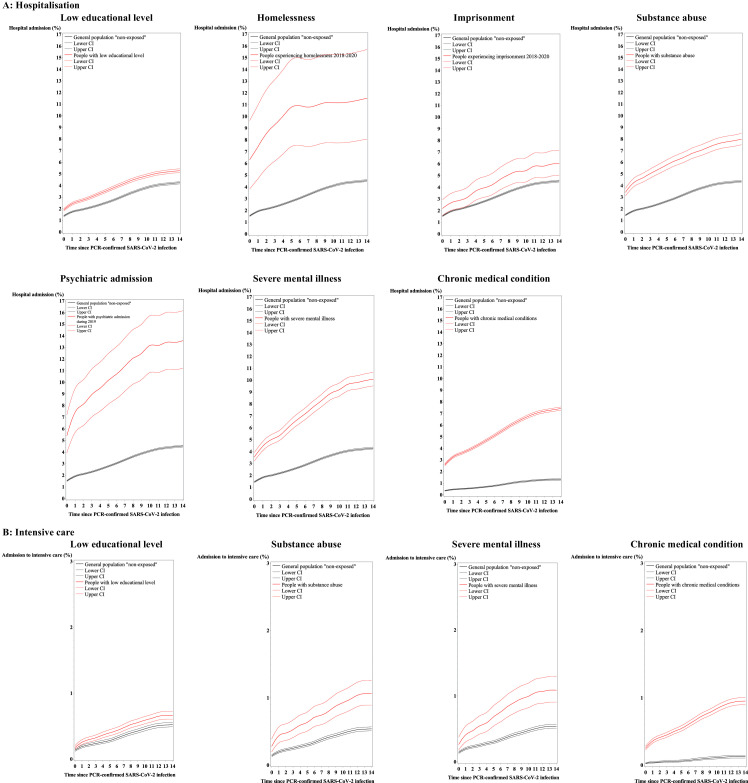
Hospitalisation
In all, 11,232 (4·5%) out of 249,924 individuals with PCR-confirmed SARS-CoV-2 infection were hospitalised within two weeks from their positive PCR-test. The cumulative probability of hospitalisation was increased for all the main population groups compared with non-exposed individuals from the background population (Figure 1). Among people experiencing homelessness, 11·6% (95% CI 8·1-15·7) were hospitalised. High cumulative probability was also found in individuals with severe psychiatric morbidity, especially for those with psychiatric admission (13·6%, 95% CI 11·2-16·2) (details of CIFs in Appendix, Supplementary table 4, p. 7).
Figure 1.
Cumulative incidence of hospital admission (a) and intensive care (b) after a PCR-confirmed SARS-CoV-2 infection.
| Hospital admissions (%) | Individuals with SARS-CoV-2 infection for analysis | ICU admissions (%) | Individuals with SARS-CoV-2 infection for analysis | |
|---|---|---|---|---|
| The Danish general population | 11,287 (4·5) | 249,924 | 1413 (0·6) | 251,497 |
| Low educational level | 3874 (5·3) | 73,803 | 493 (0·7) | 74,353 |
| Homelessness | 31 (11·5) | 269 | 17 (1·1) | 1583 |
| Imprisonment | 112 (6·0) | 1882 | 20 (1·1) | 1902 |
| Substance abuse | 944 (7·9) | 11,893 | 128 (1·1) | 12,137 |
| Supported psychiatric housing during | 39 (9·4) | 417 | … | … |
| Psychiatric admission | 100 (13·5) | 739 | 13 (1·7) | 766 |
| Severe mental illness | 1083 (10·0) | 10,819 | 119 (1·1) | 11,012 |
| Chronic medical condition | 9723 (7·4) | 131,846 | 1265 (1·0) | 133,299 |
In analyses adjusted for sex, age, and calendar time, all population groups had increased risk of hospitalisation following SARS-CoV-2 infection compared with non-exposed individuals in the background population. Overall, these results remained after further adjustments (except from psychiatric admission according to hospitalisation in the mutually adjusted model as it became statistically insignificant) (estimates in Appendix, Supplementary table 5-6, p. 8-9). Homelessness was associated with highest risk of hospitalisation (IRR 4·36, 95% CI 3·09-6·14), and individuals with supported psychiatric housing had almost 3-times higher risk of being hospitalised (IRR 2·79, 95% CI 2·04-3·83) than those in other living environments. People with a low educational level also had higher risk of hospitalisation than those with a higher educational level (IRR 1·44, 95% CI 1·38-1·50). We identified a statistically significant interaction between sex and any chronic medical conditionon on the multiplicative and additive scale. Males with chronic medical conditions had compared with males without a 2.04-times increased risk of death (95% CI 1.92-2.17) whereas the risk associated with chronic medical conditions was lower in females having a 1.77-times increased risk of death (95% CI 1.65-1.90) when compared with females without chronic medical conditions. Also, sex was found to modify the effect of severe mental illness on hospitalisation on the additive scale with higher relative excess risk for males than for females (Appendix, Supplementary table 7-8, p. 10-12).
Intensive care
Among individuals with SARS-CoV-2 infection, 1413 (0·6%) were admitted to intensive care. Overall, the probability of admission to intensive care after infection was somewhat increased for the population groups studied (Figure 1, Appendix, Supplementary table 9, p. 13). Highest cumulative probability of intensive care was found for people with psychiatric admission (1·7%, 95% CI 1·0-2·8). Among most of the other population groups (e.g., individuals experiencing homelessness or imprisonment) cumulative probability of intensive care treatment was found for 1%.
In the adjusted analyses of the risk of intensive care (Table 2), all population groups studied had elevated risk following SARS-CoV-2 infection (ranging from IRR of 1·32 to 3·12) compared with individuals not qualifying for the specific group studied. Among those experiencing homelessness, the risk was 3-times increased (95% CI, 1·29-7·52) and in those experiencing imprisonment it was 2.41-times increased (95% CI, 1·56-3·72). Overall, the increased IRRs remained after further adjustments including e.g. vaccination status and even after mutually adjustment of population groups (except from homelessness as the results became statistically insignificant in the further adjusted models (Appendix, Supplementary table 6, p. 9 and 10, p. 15)).
Table 2.
Risk of adverse outcomes in individuals with PCR-confirmed SARS-CoV-2 infection.
| Hospitalisation within 14 days |
Intensive care within 14 days |
Death within 60 days |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Population groups | IRR* | (95% CI) | P value | IRR* | (95% CI) | P value | MRR* | (95% CI) | P value |
| Low educational level | |||||||||
| Yes | 1·44 | (1·38-1·50) | <0·0001 | 1·59 | (1·42-1·78) | <0·0001 | 1·34 | (1·24-1·45) | <0·0001 |
| No | 1 | 1 | 1 | ||||||
| Homelessness | |||||||||
| Yes | 4·36 | (3·09-6·14) | <0·0001 | 3·12 | (1·29-7·52) | 0·033⁎⁎ | 8·17 | (3·66-18·25) | <0·0001 |
| No | 1 | 1 | 1 | ||||||
| Imprisonment | |||||||||
| Yes | 1·99 | (1·65-2·40) | <0·0001 | 2·41 | (1·56-3·72) | 0·00050 | 3·11 | (1·93-5·03) | <0·0001 |
| No | 1 | 1 | 1 | ||||||
| Substance abuse | |||||||||
| Yes | 1·52 | (1·42-1·62) | <0·0001 | 1·32 | (1·09-1·58) | 0·0048 | 2·10 | (1·88-2·36) | <0·0001 |
| No | 1 | 1 | 1 | ||||||
| Supported psychiatric housing | |||||||||
| Yes | 2·79 | (2·04-3·83) | <0·0001 | … | … | 2·88 | (1·59-5·21) | 0·0029 | |
| No | 1 | … | … | 1 | |||||
| Psychiatric admission | |||||||||
| Yes | 1·24 | (1·02-1·51) | 0·041⁎⁎ | 1·99 | (1·15-3·45) | 0·027⁎⁎ | 1·76 | (1·40-2·22) | <0·0001 |
| No | 1 | 1 | 1 | ||||||
| Severe mental illness | |||||||||
| Yes | 1·71 | (1·61-1·82) | <0·0001 | 1·52 | (1·26-1·84) | <0·0001 | 1·66 | (1·49-1·86) | <0·0001 |
| No | 1 | 1 | 1 | ||||||
| Chronic medical conditions | |||||||||
| Yes | 1·97 | (1·88-2·07) | <0·0001 | 1·88 | (1·63-2·18) | <0·0001 | 1·60 | (1·40-1·83) | <0·0001 |
| No | 1 | 1 | 1 | ||||||
SARS-CoV-2 infection=severe acute respiratory syndrome coronavirus 2, IRR=incidence rate ratio, ICU=intensive care unit, MRR=mortality rate ratio.
Adjusted for 5-year age groups, calendar time in months, and sex.
The p-value became > 0.05 (non-significant) when adjusting for multiple testing with Bonferroni correction made in relation to the eight tests for each of the three outcomes.
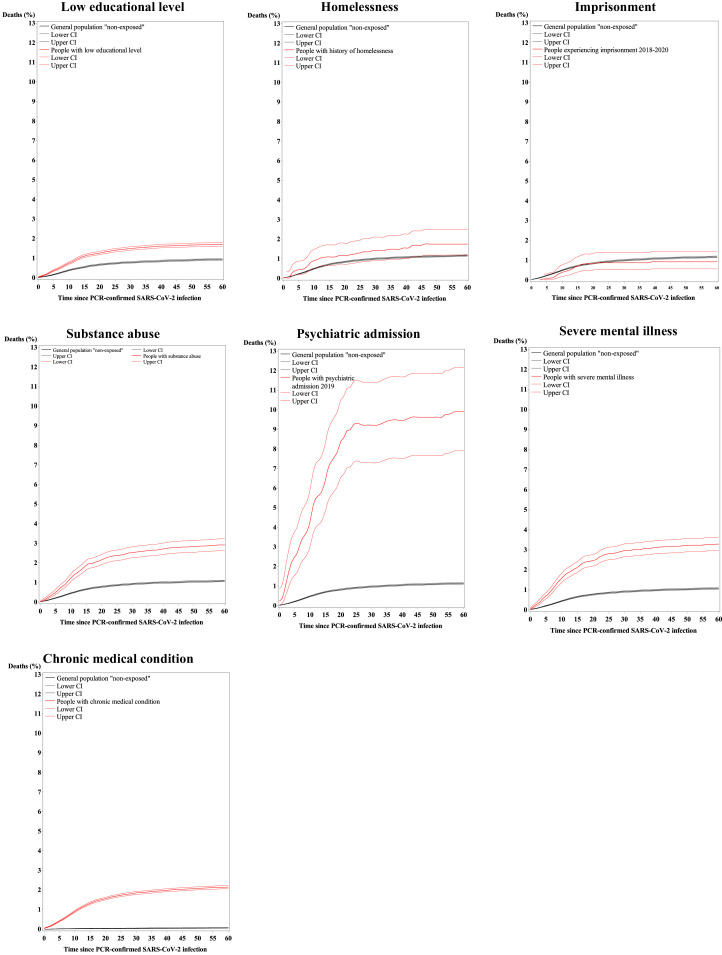
60-day mortality
Among all Danes with PCR-confirmed SARS-CoV-2 infection, 2864 (1·1%) died within 60 days after the positive test. Figure 2 shows a higher probability of dying for most of our selected population groups compared with non-exposed individuals (except from imprisonment and homelessness) (Appendix, Supplementary table 11, p. 16). Among individuals with severe psychiatric vulnerability, especially high probability of death was found for those with psychiatric admission (9·9%, 95% CI 7·9-12·2). See overall curves and results for supplementary groups and comparison groups in Appendix p. 16-17.
Figure 2.
Cumulative incidence of death after a PCR-confirmed SARS-CoV-2 infection.
| Deaths (%) | Individuals with SARS-CoV-2 infection for analysis | |
|---|---|---|
| The Danish general population | 2864 (1·1) | 251,570 |
| Low educational level | 1242 (1·7) | 74,382 |
| Homelesness | 27 (1·7) | 1585 |
| Imprisonment | 17 (0·9) | 1905 |
| Substance abuse | 346 (2·9) | 12,154 |
| Supported psychiatric housing | 11 (2·6) | 428 |
| Psychiatric admission | 75 (9·8) | 767 |
| Severe mental illness | 354 (3·2) | 11,019 |
| Chronic medical condition | 2796 (2·1) | 133,366 |
In adjusted analyses in people with SARS-CoV-2 infection, people experiencing homelessness had the highest risk of death (MRR 8·17, 95% CI 3·66-18·25) (Table 2). The mortality was also 3-times increased for imprisonment (95% CI 1·93-5·03). Of the population groups with psychiatric vulnerability, all groups had elevated mortality risk compared with non-exposed individuals. Individuals with supported psychiatric housing had almost 3-times increased risk (MRR 2·88, 95% CI 1·59-5·21) compared with those with other living circumstances in the general population. The MRR found for low educational level was 1·34 (95% CI 1·24-1·45) compared with a higher educational level. Results remained after full adjustment (except from supported psychiatric housing that became statistically insignificant in the mutually adjusted model (Appendix, Supplementary table 6 and 12, p. 9, 18)). We identified modification on the association between substance abuse, psychiatric admission, severe mental illness, and chronic medical conditions, respectively, on death by sex on the additive scale. The effect of these population groups with increased risk of death was relatively higher among males than females. No statistically significant interactions between sex and population group on the multiplicative scale were identified (Appendix, Supplementary table 13-14, p. 19-21).
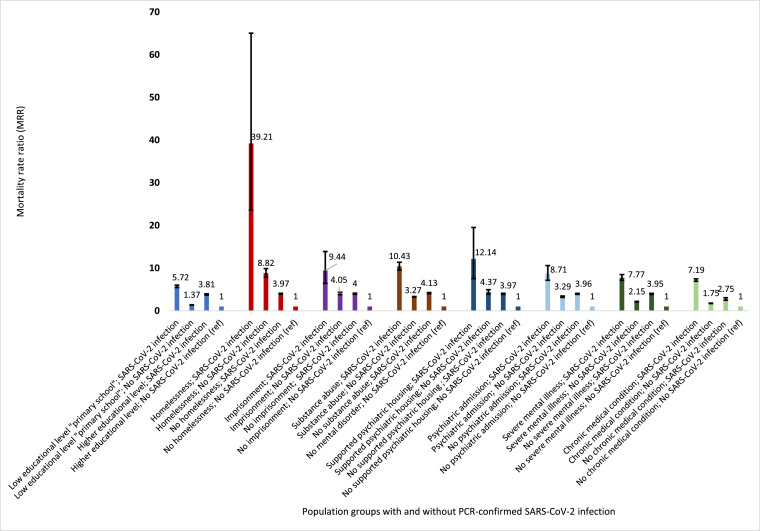
All-cause follow-up mortality
All population groups had excess mortality independent of PCR-confirmed SARS-CoV-2 infection status during the study period (Figure 3). Based on the analysis of the combined effect of the specific population group and PCR-confirmed SARS-CoV-2 infection status we found a 39-times increased mortality rate in individuals experiencing homelessness who also had SARS-CoV-2 infection when compared with those without homelessness experiences and without a PCR-confirmed SARS-CoV-2 infection (MRR: 39·21, 95% CI 23·63-65·06) with slightly higher risk after full adjustment, i.e. country of origin, living area, and vaccination status (MRR: 41·24, 95% CI 24·84-68·44). People experiencing homelessness with no positive PCR-test had a MRR of 8·82 (95% CI, 7·87-9·89), whereas those with SARS-CoV-2 infection without experiences of homelessness had a MRR of 3·97 (95% 3·85-4·10) when compared to individuals with absence of both of these conditions. Adjustment for e.g. vaccination (model 2) resulted in minor changes in estimates (Appendix, Supplementary table 15, p. 22). A confirmed SARS-CoV-2 infection was associated with an additional 4-times increased risk of dying in people experiencing homelessness (the SARS-CoV-2 infection-related mortality risk is illustrated in Appendix, Supplementary Figure 4, p. 23). Individuals with supported psychiatric housing with a positive test for SARS-CoV-2 infection had a MRR of 12·14 (95% CI 7·54-19·52), which was similar to most other of the population groups although slightly higher than for people with low educational level (Figure 3, Appendix, Supplementary table 15, p. 22).
Figure 3.
Risk of all-cause mortality by population groups combined with PCR-confirmed SARS-CoV-2 infection status.
The figure shows the mortality rate ratio of all-cause death during the study period by population groups: 1) low educational level, 2) homelessness, 3) imprisonment, 4) substance abuse, 5) supported psychiatric housing, 6) psychiatric admission, 7) severe mental illness, and 8) chronic medical condition with and without PCR-confirmed SARS-CoV-2 infection. First column shows the combined risk of exposure and SARS-CoV-2 infection, second column shows the risk associated with the population group without PCR-confirmed SARS-CoV-2 infection, third column shows the risk associated with PCR-confirmed SARS-CoV-2 infection in individuals not qualifying for the specific population group, and fourth column the reference group i.e. people without qualifying for the specific population group and without a PCR-confirmed SARS-CoV-2 infection. Estimates are adjusted for 5-year age groups, calendar time in months, and sex.
SARS-CoV-2 infection and PCR-testing
Lower cumulative probability of a PCR-confirmed SARS-CoV-2 infection was found for all population groups (except for low educational level, for which it was higher) compared with the general population not part of the specific population group (Appendix, Supplementary table 16 and Supplementary Figure 5a-b, p. 24-26).
After adjustment for age, calendar time, and sex, most population groups still had reduced risk of PCR-confirmed SARS-CoV-2 infection (except for low educational level, psychiatric admission, and chronic medical conditions with slightly increased risk) (Appendix, Supplementary table 17, p. 27). Homelessness was associated with substantially lower risk of confirmed infection (IRR 0·61, 95% CI 0·54-0·69) compared with individuals in the general population without such experiences.
Furthermore, most of the population groups also had lower odds of having a PCR-test during the study period (except for psychiatric admission associated with slightly increased odds) Appendix, Supplementary table 18, p. 28). People experiencing homelessness had an OR of 0·48 (95% CI, 0·46-0·51).
Discussion
In this Danish nationwide, register-based cohort study based on 4,412,382 individuals from Feb 27, 2020 to Oct 15, 2021, clear associations between both experiences of social deprivation (i.e. from low educational level to homelessness and imprisonment) and psychiatric severe vulnerability (i.e. substance abuse, supported psychiatric housing, psychiatric admission, and severe mental illness) with all adverse health outcomes were identified. Even mutually adjustment of all other population groups did not change the result considerably. Experience of homelessness was linked to the highest risk of all adverse outcomes with 4-times increased risk of hospitalisation, 3-times increased risk of intensive care, 8-times increased risk of death after a positive test for SARS-CoV-2 infection. A 41-times increased risk of all-cause death after adjustment was found for individuals experiencing homelessness and having PCR-confirmed SARS-CoV-2 infection during the study period compared with individuals without homelessness and without PCR-confirmed SARS-CoV-2 infection in the Danish general population. Supported psychiatric housing was associated with almost 3-times increased risk of both hospitalisation and death after PCR-confirmed SARS-CoV-2 infection compared with people in other living facilities. Indication of sex as a modifier on the risk of hospitalisation and death was found for some of the population groups suggesting that males had higher risk as compared to females.
Our study is the largest and most representative study to date of adverse SARS-CoV-2 infection-related outcomes among socially marginalised and psychiatrically vulnerable subpopulations. Due to access to nationwide registers with the possibility of optimal linkage between Danish registers and complete follow-up information we were able to study absolute and relative risks related to PCR-confirmed SARS-CoV-2 infection during around 20 months follow-up and to adjust for several important confounders, including vaccination against SARS-CoV-2 infection.
Our results confirm previous findings, primarily from other countries, of increased risk of adverse health outcomes associated with homelessness,14,20 psychiatric disorders including substance abuse,11,12,21,39 and chronic medical conditions.13 The high risk of morbidity and mortality in people experiencing homelessness, imprisonment, and individuals with psychiatric disorders might be explained by high proportions of underlying medical conditions.10,16,21,34 It is also likely that the individuals living in vulnerable living environments are affected by multiple exclusionary experiences, as well as undiagnosed and untreated disorders, and that these complex needs contribute to the severe health outcomes.16 Furthermore, these groups also had lower odds for being PCR-tested. Thus, the detection of a SARS-CoV-2 infection might be postponed, which could lead to increased risk of hospitalisation and intensive care. In the Danish general population, people are often routinely tested for SARS-CoV-2 infection due to work conditions or other activities that would require a negative PCR-test.22 Consequently, early detection of infection is more likely.
Our findings of reduced risk of PCR-confirmed SARS-CoV-2 infection in individuals with psychiatric disorders correspond with a few previous studies.40,41 We had expected the homeless shelters and supported psychiatric housing facilities to be epicentres similarly to long-term care facilities.42 Whereas we found lower odds for having a PCR-test in most of the vulnerable groups, other studies found psychiatric disorders to be associated with more frequently testing.40,41 Our results of lower rates of confirmed infection, also in the socially marginalised groups, could be explained by a lower willingness to be tested, reduced access to tests, or a preference for rapid tests. A Danish cross-sectional study in pre-print reported lower self-reported testing for SARS-CoV-2 infection in people experiencing homelessness (60%) than in homeless shelter workers (80%) (p<0·001) and a seroprevalence of 6-7% in these groups. This study found a 2.3-times higher SARS-CoV-2 seroprevalence in people experiencing homelessness compared with a sample of around 18,500 Danish blood donors aged 17-69 years, which was used as a proxy for the Danish general population (P<0·001).43 This indicates under-ascertainment of cases. Studies from other countries have reported higher risks of SARS-CoV-2 infection and a higher seroprevalence in people experiencing homelessness8,14,20 or psychiatric disorders.21,44 Infection rates, testing frequency, study designs, and exposures vary between studies and make comparison difficult. Our results of lower PCR-confirmed infection in people living in homeless shelters and supported psychiatric housing facilities in Denmark could also be explained by a strong focus on infection mitigation and prevention strategies including hand hygiene practice, self-isolation, social distancing, and staff training on infection prevention strategies. A Danish study in pre-print reported that almost all people experiencing homelessness and homeless shelter workers follow one or more of the national guidelines of SARS-CoV-2 infection prevention.43 There might also be fewer social interactions among socially and psychiatrically vulnerable groups than in the general population. Such mitigation strategies as well as single-room accommodation and comprehensive and rapid testing have been suggested as important factors for obtaining reduced risk of infections and adverse outcomes in homeless populations.8,14,45 Spending much time outdoors was reported to be a positive factor in socially marginalised populations.8
In Denmark, people have universal tax-funded access to the health care system and vaccines, and the vaccine acceptance rates have been high in the general population.46 However, it should be noticed that the vaccine uptake in vulnerable population groups has been substantially lower than in the general population, especially in the socially marginalised population groups.7 Mass testing and tracing of contacts have been important tools in the mitigation of the pandemic in Denmark.22 Variations in the political handling of the pandemic and in public health and health system capacity between high-income countries should be noticed.47 Thus, it might be difficult to generalise our results to other countries. However, due to a well-established safety net, sufficient treatment facilities during the pandemic, and a strong public health capacity with a high capacity of PCR-testing for SARS-CoV-2,22,47 we would expect the marginalised and deprived individuals to be less vulnerable than in other high-income countries e.g. the UK and the USA.
This study has limitations. The definitions of homelessness, imprisonment, and supported psychiatric housing included current and previous experiences during 2018-2020. We cannot know whether people were in these vulnerable positions exactly at the time of the infection or the outcome. Estimates of morbidity and mortality are expected to be conservative. Also, in a few analyses, the number of cases were low. Details of specific test patterns were outside the scope of this study, but this might explain some of the differences in SARS-CoV-2 infection-related outcomes between groups. Furthermore, we were not able to adjust for some potential confounders, e.g. risk awareness, access to hygiene facilities, social interactions, and undiagnosed disorders. We did not include death as competing risk in the regression models analysing morbidity. However, since death is a relatively rare event, this would not change the result, but could lead to a slightly overestimation of hospitalisation and intensive care.
Our results corroborate the state of inequality in health during the COVID-19 pandemic, even in a high-income country like Denmark with a well-established safety net. This calls for increased attention to address vulnerable communities and population groups in pandemic planning as well as practical mitigation strategies, including infection prevention. High-income societies need to have more focus on socially deprived and psychiatrically vulnerable population groups.
Contributors
MN obtained funding of the study. MN, SFN, TML, MO, CH, SE, MB, and KM designed the study. SFN, CH, and MO had full access to all data in the study and verify the underlying data. SFN takes responsibility for the integrity of the data and the accuracy of the data analyses. SFN analysed the data with supervision from TML. All authors interpreted the data. SFN drafted the manuscript. All authors critically revised the manuscript.
Ethics approval and consent to participate
The study was approved by the Danish Data Protection Agency, and data access was agreed by Statistics Denmark and the Danish Health Data Authority. Approval by the Ethics Committee and written informed consent were not required for register-based projects, cf. LBK nr 1338 af 01/09/2020, §10 Bekendtgørelse af lov om videnskabsetisk behandling af sundhedsvidenskabelige forskningsprojekter og sundhedsdatavidenskabelige forskningsprojekter [Act no. 1338 of 1 September 2020, section 10 on research ethics for administration of health scientific research projects and health data scientific research projects]. All data were de-identified and not recognizable at an individual level.
Data sharing statement
The data that support the findings of this study are available from Statistics Denmark. The data access requires the completion of a detailed application form from the Danish Data Protection Agency, the Danish National Board of Health and Statistics Denmark. For more information on accessing the data, see https://www.dst.dk/en.
Declaration of interests
We declare no competing interests. As a governmental institution, Statens Serum Institut is involved in the national vaccine distribution chain; receiving, storing and distributing vaccines to doctors and vaccine centres within Denmark.
Acknowledgements
This study was funded by a grant from the Novo Nordisk Foundation to MN (grant number NFF20SA0063142).
The Danish Departments of Clinical Microbiology (KMA) and Statens Serum Institut carried out laboratory analyses, registration, and release of the national SARS-CoV-2 surveillance data for the present study.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanepe.2022.100421.
Appendix. Supplementary materials
References
- 1.World Health Organization . 2021. WHO Coronavirus (Covid-19) Dashboard.https://covid19.who.int/ Accessed 8 September 2021. [Google Scholar]
- 2.Creech CB, Walker SC, Samuels RJ. SARS-CoV-2 Vaccines. JAMA. 2021 doi: 10.1001/jama.2021.3199. [DOI] [PubMed] [Google Scholar]
- 3.Haas EJ, Angulo FJ, McLaughlin JM, et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet. 2021;397:1819–1829. doi: 10.1016/S0140-6736(21)00947-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barda N, Dagan N, Ben-Shlomo Y, et al. Safety of the BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Setting. N Engl J Med. 2021 doi: 10.1056/NEJMoa2110475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lazarus JV, Ratzan SC, Palayew A, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27:225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Curtis HJ, Inglesby P, Morton CE, et al. Trends and clinical characteristics of COVID-19 vaccine recipients: a federated analysis of 57.9 million patients’ primary care records in situ using OpenSAFELY. Br J General Practice. 2022;72:e51–e62. doi: 10.3399/BJGP.2021.0376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nilsson SF, Laursen TM, Osler M, et al. Vaccination against SARS-CoV-2 infection among vulnerable and marginalised population groups in Denmark: A nationwide population-based study. Lancet Regional Health - Europe. 2022;16 doi: 10.1016/j.lanepe.2022.100355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roederer T, Mollo B, Vincent C, et al. Seroprevalence and risk factors of exposure to COVID-19 in homeless people in Paris, France: a cross-sectional study. Lancet Public Health. 2021 doi: 10.1016/S2468-2667(21)00001-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsai J, Wilson M. COVID-19: a potential public health problem for homeless populations. Lancet Public Health. 2020;5:e186–e187. doi: 10.1016/S2468-2667(20)30053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aldridge RW, Story A, Hwang SW, et al. Morbidity and mortality in homeless individuals, prisoners, sex workers, and individuals with substance use disorders in high-income countries: a systematic review and meta-analysis. Lancet. 2018;391:241–250. doi: 10.1016/S0140-6736(17)31869-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ceban F, Nogo D, Carvalho IP, et al. Association between mood disorders and risk of COVID-19 infection, hospitalization, and death: a systematic review and meta-analysis. JAMA Psychiatry. 2021;78:1079–1091. doi: 10.1001/jamapsychiatry.2021.1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vai B, Mazza MG, Delli Colli C, et al. Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis. Lancet Psychiatry. 2021;8:797–812. doi: 10.1016/S2215-0366(21)00232-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mohsenpour A, Bozorgmehr K, Rohleder S, Stratil J, Costa D. SARS-Cov-2 prevalence, transmission, health-related outcomes and control strategies in homeless shelters: systematic review and meta-analysis. EClinicalMedicine. 2021 doi: 10.1016/j.eclinm.2021.101032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.De Hert M, Mazereel V, Detraux J, Van Assche K. Prioritizing COVID-19 vaccination for people with severe mental illness. World Psychiatry. 2021;20:54–55. doi: 10.1002/wps.20826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tweed EJ, Thomson RM, Lewer D, et al. Health of people experiencing co-occurring homelessness, imprisonment, substance use, sex work and/or severe mental illness in high-income countries: a systematic review and meta-analysis. J Epidemiol Community Health. 2021;75:1010–1018. doi: 10.1136/jech-2020-215975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mazereel V, Van Assche K, Detraux J, De Hert M. COVID-19 vaccination for people with severe mental illness: why, what, and how? Lancet Psychiatry. 2021;8:444–450. doi: 10.1016/S2215-0366(20)30564-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Picker LJ, Dias MC, Benros ME, et al. Severe mental illness and European COVID-19 vaccination strategies. Lancet Psychiatry. 2021;8:356–359. doi: 10.1016/S2215-0366(21)00046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mosites E, Parker EM, Clarke KEN, et al. Assessment of SARS-CoV-2 infection prevalence in homeless shelters - four U.S. Cities, March 27-April 15, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:521–522. doi: 10.15585/mmwr.mm6917e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richard L, Booth R, Rayner J, Clemens KK, Forchuk C, Shariff SZ. Testing, infection and complication rates of COVID-19 among people with a recent history of homelessness in Ontario, Canada: a retrospective cohort study. CMAJ Open. 2021;9:E1–E9. doi: 10.9778/cmajo.20200287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang QQ, Kaelber DC, Xu R, Volkow ND. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatry. 2020:1–10. doi: 10.1038/s41380-020-00880-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hansen CH, Michlmayr D, Gubbels SM, Mølbak K, Ethelberg S. Assessment of protection against reinfection with SARS-CoV-2 among 4 million PCR-tested individuals in Denmark in 2020: a population-level observational study. Lancet. 2021;397:1204–1212. doi: 10.1016/S0140-6736(21)00575-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pedersen CB. The danish civil registration system. Scand J Public Health. 2011;39:22–25. doi: 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- 24.Schmidt M, Pedersen L, Sorensen HT. The Danish civil registration system as a tool in epidemiology. Eur J Epidemiol. 2014;29:541–549. doi: 10.1007/s10654-014-9930-3. [DOI] [PubMed] [Google Scholar]
- 25.Nielsen SF, Hjorthøj CR, Erlangsen A, Nordentoft M. Psychiatric disorders and mortality among people in homeless shelters in Denmark: a nationwide register-based cohort study. Lancet. 2011;377:2205–2214. doi: 10.1016/S0140-6736(11)60747-2. [DOI] [PubMed] [Google Scholar]
- 26.Nilsson SF, Nordentoft M, Fazel S, Laursen TM. Homelessness and police-recorded crime victimisation: a nationwide, register-based cohort study. Lancet Public Health. 2020;5:e333–e341. doi: 10.1016/S2468-2667(20)30075-X. [DOI] [PubMed] [Google Scholar]
- 27.The Danish Ministry of Social Affairs. Consolidation Act on Social Services. 2015. http://www.english.sm.dk/media/14900/consolidation-act-on-social-services.pdf2018.
- 28.FEANTSA. ETHOS - Eurpoean Typology on Homelessness and Housing Exclusion. 2005. https://www.feantsa.org/en/toolkit/2005/04/01/ethos-typology-on-homelessness-and-housing-exclusion. Accessed 21 March 2022.
- 29.Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish national patient registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. doi: 10.2147/CLEP.S91125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Public Health. 2011;39:54–57. doi: 10.1177/1403494810395825. [DOI] [PubMed] [Google Scholar]
- 31.Pottegård A, Schmidt SAJ, Wallach-Kildemoes H, Sørensen HT, Hallas J, Schmidt M. Data Resource Profile: The Danish National Prescription Registry. Int J Epidemiol. 2017;46:798-F. doi: 10.1093/ije/dyw213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Board of Health . 2020. The Registry of Drug Abusers Undergoing Treatment.https://sundhedsdatastyrelsen.dk/da/registre-og-services/om-de-nationale-sundhedsregistre/sygdomme-laegemidler-og-behandlinger/stofmisbrugere-i-behandling Accessed 5 March 2021. [Google Scholar]
- 33.National Board of Health . 2020. The National Registry of Alcohol Treatment.https://sundhedsdatastyrelsen.dk/da/registre-og-services/om-de-nationale-sundhedsregistre/sygdomme-laegemidler-og-behandlinger/alkoholbehandlingsregisteret Accessed 5 March 2021. [Google Scholar]
- 34.Momen NC, Plana-Ripoll O, Agerbo E, et al. Association between mental disorders and subsequent medical conditions. N Engl J Med. 2020;382:1721–1731. doi: 10.1056/NEJMoa1915784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Voldstedlund M, Haarh M, Mølbak K. The Danish microbiology database (MiBa) 2010 to 2013. Euro Surveill. 2014;19 doi: 10.2807/1560-7917.es2014.19.1.20667. [DOI] [PubMed] [Google Scholar]
- 36.Knol MJ, VanderWeele TJ. Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol. 2012;41:514–520. doi: 10.1093/ije/dyr218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aalen OO, Johansen S. An empirical transition matrix for non-homogeneous markov chains based on censored observations. Scand J Stat. 1978;5:141–150. [Google Scholar]
- 38.Gray RJ. A class of k-sample tests for comparing the cumulative incidence of a competing risk. Annals Statistics. 1988;16:1141–1154. [Google Scholar]
- 39.Pottegård A, Kristensen KB, Reilev M, et al. Existing data sources in clinical epidemiology: the Danish COVID-19 Cohort. Clin Epidemiol. 2020;12:875–881. doi: 10.2147/CLEP.S257519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van der Meer D, Pinzón-Espinosa J, Lin BD, et al. Associations between psychiatric disorders, COVID-19 testing probability and COVID-19 testing results: findings from a population-based study. BJPsych Open. 2020;6:e87. doi: 10.1192/bjo.2020.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tzur Bitan D, Krieger I, Kridin K, et al. COVID-19 prevalence and mortality among schizophrenia patients: a large-scale retrospective cohort study. Schizophr Bull. 2021;47:1211–1217. doi: 10.1093/schbul/sbab012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McMichael TM, Currie DW, Clark S, et al. Epidemiology of Covid-19 in a long-term care facility in king county, Washington. N Engl J Med. 2020;382:2005–2011. doi: 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Röthlin Eriksen AR, Fogh K, Hasselbalch RB, et al. SARS-CoV-2 antibody prevalence among homeless people, sex workers and shelter workers in Denmark: a nationwide cross-sectional study. medRxiv. 2021:2021.05.07.21256388. [DOI] [PMC free article] [PubMed]
- 44.Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8:130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lewer D, Braithwaite I, Bullock M, et al. COVID-19 among people experiencing homelessness in England: a modelling study. Lancet Respir Med. 2020;8:1181–1191. doi: 10.1016/S2213-2600(20)30396-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.The Danish Health Authority . 2021. Status of the Epidemic in Denmark.https://www.sst.dk/en/English/Corona-eng/Status%20of%20the%20epidemic Accessed 23 September 2021. [Google Scholar]
- 47.Han E, Tan MMJ, Turk E, et al. Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. Lancet. 2020;396:1525–1534. doi: 10.1016/S0140-6736(20)32007-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.