Abstract
Introduction
Radiographers provide mobile radiography services for patients who are critically ill as well as patients isolated due to highly infectious diseases such as COVID-19. The pandemic has caused the demand for mobile radiography to increase. This study aims to understand the experience of radiographers performing mobile radiography during the COVID-19 pandemic to identify the success criteria and challenges faced.
Methodology
This study utilized a cross sectional online survey to obtain data. The online survey was disseminated to radiographers working in public hospitals who have performed mobile radiography from February 2020 to September 2021. The key sections explored in the survey are: (1) demographics, (2) operations, (3) adequacy of resources, and (4) success criteria. The answers were obtained in the form of multiple choice questions, Likert scales or free text.
Results
Radiographers reported a rise in mobile radiography workload as well as increased time required to perform an examination for COVID-19 patients. The factors identified for success criteria were: (1) infection control management, (2) resource management (3) modified techniques and (4) improved workflow. The challenges encountered were: (1) nature of exam, (2) juggling the demand for mobile imaging and (3) staff well-being.
Conclusion
As the COVID-19 situation is evolving, departments have to constantly refine policies and processes as well as ensure the provision of adequate resources such as manpower and personal protective equipment (PPE) so that radiographers feel supported and can perform their duties safely.
Implications for practice
This study has identified challenges that radiographers face in mobile radiography as well as the success criteria that can aid radiographers in their job.
Keywords: Radiography, Mobile radiography, Portable radiography, COVID-19, Pandemic
RÉSUMÉ
Introduction
Les radiographes fournissent des services de radiographie mobile aux patients gravement malades ainsi qu'aux patients isolés en raison de maladies hautement infectieuses comme la COVID-19. La pandémie a entraîné une augmentation de la demande de radiographie mobile. Cette étude vise à comprendre l'expérience des radiographes effectuant des radiographies mobiles pendant la pandémie de COVID-19 afin d'identifier les critères de réussite et les défis rencontrés.
Méthodologie
Cette étude a utilisé une enquête transversale en ligne pour obtenir des données. L'enquête en ligne a été diffusée aux radiographes travaillant dans des hôpitaux publics et ayant effectué des radiographies mobiles entre février 2020 et septembre 2021. Les sections clés explorées dans l'enquête sont : (1) les données démographiques, (2) les opérations, (3) l'adéquation des ressources et (4) les critères de réussite. Les réponses ont été obtenues sous forme de questions à choix multiples, d'échelles de Likert ou de texte libre.
Résultats
Les radiographes ont signalé une augmentation de la charge de travail en radiographie mobile ainsi qu'une augmentation du temps nécessaire pour effectuer un examen pour les patients COVID-19. Les facteurs identifiés pour les critères de réussite étaient : (1) la gestion du contrôle des infections, (2) la gestion des ressources (3) les techniques modifiées et (4) l'amélioration du flux de travail. Les défis rencontrés étaient : (1) la nature de l'examen, (2) jongler avec la demande d'imagerie mobile et (3) le bien-être du personnel.
Conclusion
Comme la situation liée à la COVID-19 évolue, les services doivent constamment affiner les politiques et les processus, ainsi que veiller à fournir des ressources adéquates, telles que la main-d'œuvre et les équipements de protection individuelle (EPI), afin que les radiographes se sentent soutenus et puissent accomplir leurs tâches en toute sécurité.
Implications pour la pratique
Cette étude a permis d'identifier les défis auxquels les radiographes sont confrontés en radiographie mobile ainsi que les critères de réussite qui peuvent aider les radiographes dans leur travail.
Introduction
Coronavirus disease-2019 (COVID-19) is an acute infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1 The first case of COVID-19 was reported in Singapore on 23 January 2020 and community transmission was soon reported on 7 February 2020.2 As of 30 October 2021, Singapore has reported a total of 195,211 COVID-19 cases and a total death toll of 394.3 Singapore has since experienced several waves of COVID-19 with this study taking place in the middle of the wave experienced from late August 2021 to November 2021, which saw 91,146 Covid cases in the month of October.4 Due to its transmissibility and its mortality on certain vulnerable groups, COVID-19 presented new challenges to the healthcare system.5 , 6 Stresses to the healthcare system include managing the influx of COVID-19 patients and ensuring the continuation of health care services.7
Imaging is a key feature in the diagnosis, treatment and management for COVID-19 patients. Chest radiographs (CXR) are the most commonly ordered imaging test for both suspected and confirmed COVID-19 cases. The benefits of a chest radiograph in comparison to other imaging modalities such as a computed tomography (CT) scan include its ease of access, speed and cost effectiveness.8 , 9 The CXR is able to identify signs of pneumonia in COVID-19 patients and can predict the onset of severe disease.10 To prevent nosocomial transmission of COVID-19, the chest radiographs are commonly obtained via mobile radiography. In mobile radiography, radiographers bring the mobile radiography machine to the patient's bedside to acquire the chest radiographs.11
Before COVID-19, radiographers provided mobile radiography services for patients who are critically ill and patients isolated due to communicable diseases. The rise of COVID-19 cases has seen an increased demand and stress on radiographers as more mobile radiography orders were made for suspected and confirmed COVID-19 patients. Swift changes in protocol had to be made in radiography departments to cope with the increased workload while protecting staff and other patients from COVID-19. Such measures include team segregation, modifications to workflow and use of personal protective equipment (PPE).12
The effect of the overwhelming mobile radiography requests following increased COVID-19 patient admissions had put the radiographers under tremendous pressure to balance the responsibilities between delivering timely imaging services and maintaining strict infection control measures. As radiography departments adapt to the pandemic, guidelines and protocols are frequently refined, which was also another stress contributor to radiographers. Despite the presence of literature on the operations of radiology during the pandemic, there is a dearth of specific insights into the experience of radiographers providing mobile radiography services.
As a year had passed since the emergence of COVID-19 in Singapore, this research aims to understand the unique experience and challenges of mobile radiography faced by radiographers. This exploratory study will help to identify the success criteria and challenges faced by radiographers. Success criteria would be defined as measures that are able to assist and enable radiographers to provide mobile radiography services during the pandemic. It is hopeful that the interventions proposed on the issues raised will assist in streamlining the processes for mobile radiographers and increase future preparedness against pandemics.
Methodology
Study design
This study utilized a cross-sectional online survey design. The questions were designed to understand the experience of radiographers performing mobile radiography and challenges faced. The questionnaire was written in English and composed of 29 close-ended questions with 5 open-ended questions to capture deeper qualitative information that is unique to each participant's experience (Supplementary Material 1). The 4 key sections of the survey are: (1) demographics, (2) operations, (3) adequacy of resources, and (4) success criteria.
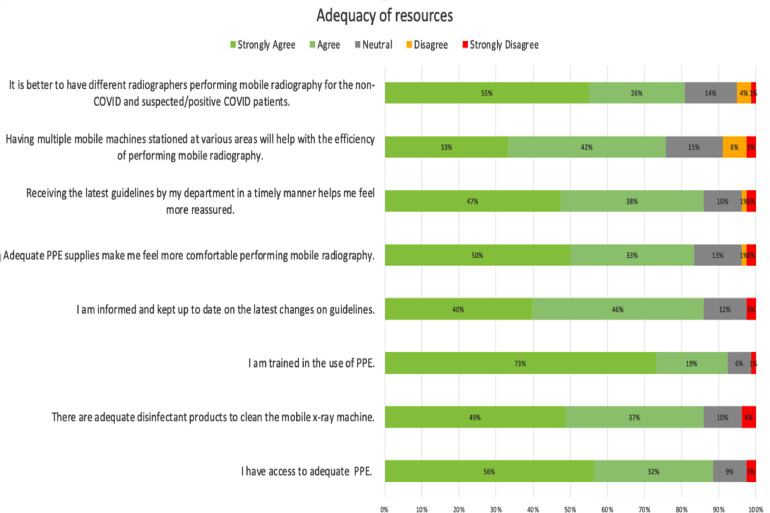
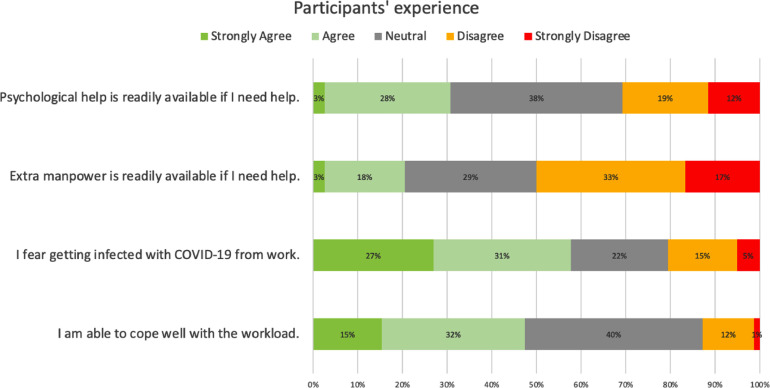
Questions regarding the adequacy of resources and participants’ experience were asked in the form of Likert scale questions, with a scale of 1-5, from 1- strongly disagree, 2-disagree, 3- neutral, 4- agree, to 5- strongly agree (Fig. 2 and 3).
Fig. 2.
Adequacy of resources.
Fig. 3.
Participants’ experience.
The survey was piloted with eight participants from one of the study centres who have experience in mobile radiography. The participants were invited to perform the survey and give their feedback regarding the clarity of the questions.
An online survey design was chosen as it would enable us to reach a wider range of participants. The survey link was disseminated to radiographers working in public hospitals in Singapore. The managers of radiography departments were contacted to assist in sending the online survey link to radiographers in their department. There was no coercion involved.
All radiographers who performed mobile radiography from February 2020 to September 2021 were invited to participate in the survey. The survey was opened for a period of one month between 13 September 2021 to 13 October 2021. Radiographers who were still undergoing training in mobile radiography were excluded due to their lack of experience, this was done through a statement in the participant information sheet informing those under training not to participate. No identifiable information was collected in the survey. Participation in the survey was voluntary and participants were able to exit the survey at any time without consequences.
The online questionnaire was created through FormSG (GovTech, SG), a secure and encrypted website that will enable the responses to be stored securely.
No funding was received for this study and the authors declare no conflict of interest.
Exemption from a full ethical review was approved by Singhealth Centralised Institutional Review Board (CIRB) as no identifiable details were collected in the survey.
Data analysis
The results were analysed with Excel Version 16.55. Descriptive statistics were performed for quantitative questions. Thematic analysis was used for open ended questions to identify patterns in qualitative data to better understand participants' experience. Two members of the research team were responsible for the thematic analysis. The contents of the free text response were organised into codes and those that formed a pattern were grouped to create themes.
Results
Demographics
A total of 78 radiographers participated in the survey, of which 53 (68.0%) were female while 25 (32%) were male. Majority [56% (44)] of the participants were in the age bracket between 25 to 29 years. The participants mean years of radiography experience was 4.45 years. Between February 2020 to September 2021, the average number of weeks that the participants have been rostered to perform mobile radiography was 16 weeks.
Operations
The questions under operations were meant to understand the nature, workflow and protocols that the participants experienced. The mean number of mobile radiographs performed in a day was 15.4. Most [88% (66)] radiographers performed mobile radiography alone while those that did not had two people involved.
Besides performing mobile radiography, 81% (63) of radiographers performing mobile radiography had to simultaneously cover other areas of operation such as the Accident and Emergency (A&E), inpatient services or operating theatre. As most hospitals had more than one building in the compound, 85% of radiographers provide coverage between different buildings as well. 77% (60) of radiographers perform mobile radiography for both COVID and non-COVID wards concurrently.
Workload
When asked how the workload has changed, 96% of the participants reported an increase in workload. 64% of radiographers also reported an increase in the number of orders for other body parts besides chest and abdominal x-rays. For those who reported an increase in orders for other body parts, 94% felt that it made the job harder. In the free text response, participants reported increased fatigue and challenges which include limitations in ward space and difficulty in positioning the patient.
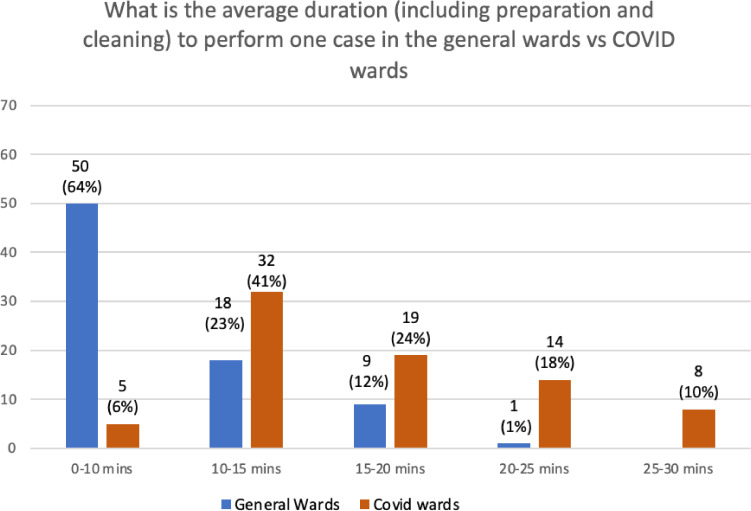
Participants were also asked to indicate the average time taken to perform an X-ray in the general ward compared to COVID-19 wards. When comparing the self-reported estimated timing, there was an increase in the average duration (Fig. 1 ). The majority of participants (64%) reported that they could complete a case in the general ward within 10 minutes while the majority (41%) required between 10 to 15 minutes to complete a case for suspected or confirmed COVID-19 cases. 85% of respondents noted that the increase in duration for suspected or confirmed COVID-19 cases made mobile radiography more challenging.
Fig. 1.
Comparison of the average duration to perform a case in the general ward compared to suspected/confirmed COVID-19 cases.
Success criteria and challenges
The response from questions relating to the adequacy of resources, participants’ experience and free text questions were used in generating the factors for success criteria and identifying challenges faced.
The factors identified for success criteria were: (1) infection control management, (2) resource management (3) modified techniques and (4) improved workflow. The challenges encountered were: (1) nature of exam, (2) juggling the demand for mobile imaging and (3) staff well-being.
Success criteria
Infection control management
In Fig. 2 , the majority of participants (79%) strongly agreed that they were trained in the use of PPE and 56% strongly agreed that they had access to adequate personal protective equipment (PPE). 49% strongly agreed that there were adequate disinfectant products to clean the mobile radiography machine.
83% of the respondents agreed that the provision of adequate personal protective equipment ensured that they feel comfortable performing mobile radiography for COVID-19 patients. 86% of participants reported that they were informed and kept up to date on the latest changes in guidelines and most agreed (85%) that receiving the latest updates on guidelines in a timely manner helped them to feel assured.
“Management always keep us updated on the guidelines to safely control the situation.” (Rad 9)
A small number of participants expressed concern and confusion when guidelines were not clear.
“I'm not sure if the wards that are on lock down….. Do we do those cases or wait for the isolation team to do?.” (Rad 64)
Resource management
With regards to allocation of resources, 72% felt that having multiple machines stationed at various areas in the hospital would help in the efficiency of performing mobile radiography.
“We can deploy a [dedicated] portable machine to [these] isolation wards… Less effort for the radiographer pushing the machine up and down and maybe cleaning it one time is enough.” (Rad 5)
Most participants felt that the use of additional equipment, together with their strategic placement, were beneficial in their mobile radiography experience. To enhance their performance, some participants suggested:
“Addition of laptop terminals for on-the-go registration of add on cases”. (Rad 59)
In terms of manpower, 81% felt that it would be beneficial to assign different radiographers to perform mobile radiography for COVID-19 patients. Radiographers can also be better supported by an increase in staff deployment. This allowed for the concept of a “clean” and “dirty” radiographer, to separate the coverage between general wards and covid cases, and to cope with the increased workload.
“One dirty who is positioning the patient, one clean who is only touching the machine.” (Rad 39)
“It helps to have two persons covering mobile radiography, one for clean cases while another for ‘dirty’ cases.” (Rad 58)
“Activation of [other] radiographers if workload is too much.” (Rad 47)
Modified technique
Many participants have identified new techniques such as exposing through glass and using a detector stand to help them perform X-rays more effectively. The technique of exposing through glass minimises direct contact between the covid positive patient and the radiographer.
“Minimising the time taken to gown and de-gown for each patient by performing CXRs through a door.” (Rad 49)
Improved workflow
To enhance efficiency in performing mobile radiography, several participants also mentioned collaborating with COVID wards to improve the process such as clearly demarcating floors, dedicating ward space for X-ray and grouping of COVID cases.
“COVID wards [allocated] one room for us radiographers to perform the CXR for their mobile patients.” (Rad 18)
“Different timings for portable CXRs for covid patients and general morning round patients. Splitting up the workload allows the machine to have sufficient battery to perform.” (Rad 62)
When COVID wards failed to collate cases, one radiographer commented:
“It is tiresome having to don the PPE over and over again and going back to the same ward in a short period of time.” (Rad 58)
Participants preferred the use of swab status to determine eligibility for mobile X-ray.
“If possible, to request for mobile X-rays only if really needed and patient has been cleared or confirmed of COVID case. There are cases where COVID status is pending and full contact precaution is taken for that particular case. [Confirmation of COVID-status helps] prevent wastage and minimise mobile radiographer resources.” (Rad 50)
A new mandatory pregnancy test protocol for all female patients of child-bearing age who needed mobile X-ray was also found to be helpful.
“This way we do not have to waste time ascertaining the pregnancy status of the patients in the rooms, and the potential for miscommunication or inaccurate verbal consent is reduced.” (Rad 63)
Challenges
Nature of exam
Before the pandemic, mobile radiography was mainly limited to chest radiographs and occasionally abdominal radiographs. Chest X-rays are considered relatively simple examinations to perform and only one image is required. The scatter radiation associated with a chest X-ray is also very low, which is why it is suitable to be performed in the ward. As movement out of the ward for COVID-19 positive patients had to be limited to prevent nosocomial infection, radiography departments increased the acceptance for other body regions.
This increases the difficulty for radiographers as imaging for other body regions might require multiple images and the patient's cooperation in maintaining the position. Complex examinations may also require the use of additional equipment such as positioning sponges and a detector holder which have to be brought along with the mobile machine.
“It's quite challenging to attend to a patient who has a COVID infection and yet is not cooperative and is very stiff. Positioning is difficult given that I am the only one in the room doing the procedure…” (Rad 9)
“Space limitation in the wards is a big challenge when doing other body parts such as horizontal beam lateral (HBL) hip.” (Rad 49)
“It also requires more logistics, such as positioning sponges and support, that end up getting exposed to COVID as well and our machine doesn't have a lot of space to place all of them.” (Rad 52)
“Exposure factors for some body parts may also be limited by the portable x-ray machine.” (Rad 63)
Several participants also raised concerns over radiation safety, especially when performing examinations other than chest X-rays in the ward.
“Furthermore, when these COVID patients are in the ward with other COVID patients, doing other complex X-rays that require more than 2 exposures may also mean exposing other patients in that ward.” (Rad 76)
Juggling the demand for mobile imaging
Under normal circumstances, radiographers perform mobile X-rays for critically ill patients or patients who require urgent medical attention. However, radiographers now face increased stress as they juggle X-ray requests from Covid wards and intensive care units. Although radiographers are trained to identify and prioritise urgent cases, this becomes difficult to achieve when there are multiple requests for urgent X-rays.
Most participants mentioned how numerous clinicians insisted on the urgency of their cases, making it harder to accurately prioritise truly urgent cases.
“It's challenging to juggle these cases especially when the nurses and doctors insist that their cases should be prioritised as urgent.” (Rad 58)
“Having 5 calls for patients requiring urgent portable CXR in a 15 minutes period. Ended up missing out on performing imaging for the one patient who required it the most; the patient passed away before I could reach.” (Rad 43)
When participants were asked for areas for improvement, the majority suggested the need for more appropriate orders for mobile radiography, where ward staff should only request mobile X-ray services for COVID or critically ill patients who are unable to be brought down to the imaging room. Such measures will allow radiographers to attend to patients who really require an urgent X-ray in a timely manner.
“Nurses in all wards should implement a strict policy on ordering if they really need an urgent portable x-ray […] or until the swab is released.” (Rad 9)
“For ward staff to not use lack of manpower as an excuse for not fetching (clean) patients down to x-ray room, as radiography staff is also [facing a] lack of manpower and may neglect actual STAT cases that need mobile radiography.” (Rad 62)
Staff well-being
Participants expressed fatigue due to the increased workload, insufficient manpower, larger area of coverage and more time-consuming procedures. Only 47% of the respondents agreed that they were able to cope well with the workload. When asked if extra manpower was readily available when they required help, 50% of the participants disagreed with that statement (Fig. 3 ).
“With increased positive patients, there isn't really time for mobile radiographers to sit down and vet cases. It's more of your colleagues just telling you there's another patient and you just go ahead and do.” (Rad 60)
“Sometimes I take more time to clean/disinfect than doing the patients’ x-rays.” (Rad 55)
“Going an entire afternoon shift without sitting down longer than the 15 minutes dedicated to post processing. (Rad 41)
Some participants also mentioned the additional discomfort of wearing PPE.
“Blurry vision from the goggles and difficulty breathing through the N95 mask.” (Rad 73)
“Hot and sweaty to wear the PPE in a non-airconditioned covid ward.” (Rad 30)
Several participants also mentioned the fear of getting infected due to longer exposure time with covid patients. Despite agreeing that there was training and access to adequate PPE and disinfectant products, most of the participants (58%) fear getting infected with COVID-19 from the workplace (Fig. 3).
“Uncooperative patients sometimes increase time of exposure to patients. Especially when there is no nurse available to assist and help.” (Rad 61)
“Most patients also do not wear masks and they keep on coughing hard, even though you wear a complete set of PPE, subconsciously it is very scary to risk yourself.” (Rad 9)
Discussion
Most research on the radiographer's experience during COVID-19 focuses on radiographers as a whole.13., 14., 15. To the best of our knowledge, there was no research specifically to explore the experiences of radiographers performing mobile radiography in hospitals during the COVID-19 pandemic. This study is the first qualitative study that evaluates the success criteria and challenges faced by radiographers. Our findings show that infection control, resource management and modification of routine radiographic practices are key measures in the success of mobile radiography. On the other hand, challenges include increased workload and stress on radiographers.
Effective communications are essential during the pandemic. Streamlined communication channels between ward staff and radiographers are crucial to ensure radiographers are kept up to date on the latest COVID-19 situation, infection control guidelines and patient's infectious status.13 Unclear guidelines will place radiographers at risk of exposure to COVID-19 and cause fear when handling COVID-19 patients.16 On top of that, work efficiency will be reduced as more time is needed to clarify the situation before delivering service. Therefore, quick dissemination with correct information is vital to maintain a safe working environment and optimise efficiency.
The provision of adequate PPE and disinfectant products are key in providing a safe environment for radiographers to perform their duty. The adequacy of resources may alleviate radiographers anxiety, allowing them to feel safer and comfortable while performing mobile radiography. Following the experience of SARS, MOH recommended that agencies maintain a 3 to 6 month stockpile in preparation for a pandemic.17 Thus, it is important for departments to monitor stocks closely and prepare alternate supply chains to ensure there are sufficient PPE.
Enhancement of infection control measures such as segregation of both mobile radiographic units and staff to minimise cross contamination between patients and staff are noted as common practices in Singapore.18 , 19 The mobile radiographic units are segregated into ‘clean’ and ‘dirty’ units where the ‘dirty’ units are designated for use in high-risk areas (COVID-19 related cases). Radiographers are also similarly segregated into ‘clean’ and ‘dirty’ teams with the ‘dirty’ teams performing mobile radiography for high risk areas. While most of the respondents feel that it is better to have different radiographers performing mobile radiography for ‘clean’ and ‘dirty’ patients, not all hospitals practice this, with 77% of respondents providing coverage between different wards. This can be attributed to the lack of manpower in the department and worsened by the increase in demand for mobile radiography services. Radiography teams are at risk of being understaffed when radiographers fall ill with respiratory symptoms and are issued with 5 days of medical leave as per the Ministry of Health (MOH) guidelines.20 The number of radiographers performing mobile radiography remains the same despite the dramatic increase in COVID-19 cases due to manpower crunch.
With more mobile radiography requests along with the extra time needed to perform an X-ray for suspected or confirmed COVID-19 patients, measures such as the deployment of additional mobile radiographic units and radiographers to various locations are essential in aiding radiographers. Radiographers are then able to deliver X-ray services more efficiently as the extra effort to push the machine from one place to another has been eliminated. Therefore, optimisation of radiographer manpower with re-deployment of radiographers from outpatient or other subspecialties to higher risk areas (mobile radiography) will help to ease the stress and balance the workload.
Although the rising radiological requests are unavoidable during the pandemic, the appropriateness of these requests as a key success criterion is still lacking. Appropriate radiological requests will enable timely imaging to the right patients while balancing the workload. An implementation of request guidelines that better empowers radiographers to flag out inappropriate requests may help make mobile radiography more successful by optimising scarce resources, especially during this trying time.
Limitations
Limitations to the study include the use of an online survey, where responses were only captured via multiple choice questions and limited free text questions. While an online survey is useful in reaching a wide range of participants and obtaining response at a faster rate, this may limit the depth of response achievable as compared to a focus group interview. Furthermore, the method of disseminating the online survey through radiography managers may inhibit higher participation rates as we did not pressure them to re-distribute the survey link to obtain more responses.
As this is a cross sectional study, the data only captured the participant's experience during the period of the survey which might change as the situation of the pandemic evolves. Further research could be done using a longitudinal methodology to implement and investigate the effects of workflow changes that may benefit radiographers performing mobile radiography during a pandemic.
Conclusion
The COVID-19 pandemic has seen an increase in demand for mobile radiography services resulting in operational challenges due to manpower constraints and additional stress and anxiety amongst radiographers. Radiography departments have enacted new workflows and policies to cope with the rising COVID-19 cases. Challenges to radiographers include the increase in orders for both standard chest radiographs and non-routine cases with increased complexity, while having to abide with infection control measures. As a result, radiographers reported feeling exhausted trying to juggle the demands while responding to urgent cases in a timely manner. Given these challenges, departments can support their staff by ensuring the adequate provision of PPE and ensuring that new updates are disseminated to their staff rapidly. Furthermore, constant evaluation of manpower requirements to facilitate staff deployment would be crucial in ensuring that there is adequate manpower to manage the demand for mobile radiography services.
Footnotes
Contributors: All authors contributed to the conception or design of the work, the acquisition, analysis, or interpretation of the data. All authors were involved in drafting and commenting on the paper and have approved the final version. Funding: This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Competing interests: All authors declare no conflict of interest. Ethical approval: Exemption from a full ethical review was approved by Singhealth Centralised Institutional Review Board (CIRB) as no identifiable details were collected in the survey.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jmir.2022.06.007.
Appendix. Supplementary materials
References
- 1.Lai C-C, Shih T-P, Ko W-C, Tang H-J, Hsueh P-R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents. 2020;55(3) doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coffman TM, Chan CM, Choong LH-L, Curran I, Tan HK, Tan CC. Perspectives on COVID-19 from Singapore: Impact on ESKD Care and Medical Education. J Am Soc Nephrol. 2020;31(10):2242LP–222245. doi: 10.1681/ASN.2020050721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ministry of Health Singapore. COVID-19 Situation Report. https://covidsitrep.moh.gov.sg
- 4.Ministry of Health Singapore UPDATE ON LOCAL COVID-19 SITUATION. 31 OCT 2021 https://www.moh.gov.sg/news-highlights/details/update-on-local-covid-19-situation- Published 2021. (31-oct-2021) [Google Scholar]
- 5.Gandhi M, Yokoe DS, Havlir D V. Asymptomatic Transmission, the Achilles’ Heel of Current Strategies to Control Covid-19. N Engl J Med. 2020;382(22):2158–2160. doi: 10.1056/NEJMe2009758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wei WE, Li Z, Chiew CJ, Yong SE, Toh MP, Lee VJ. Presymptomatic Transmission of SARS-CoV-2 - Singapore, January 23-March 16, 2020. Morb Mortal Wkly Rep. 2020;69(14):411–415. doi: 10.15585/mmwr.mm6914e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tan T, Toh M, Vasoo S, et al. Coronavirus Disease 2019 (COVID-19): The Singapore Experience. A Review of the First Eight Months. Ann Acad Med Singapore. 2020;49:764–778. doi: 10.47102/annals-acadmedsg.2020306. [DOI] [PubMed] [Google Scholar]
- 8.Çinkooğlu A, Bayraktaroğlu S, Ceylan N, Savaş R. Efficacy of chest X-ray in the diagnosis of COVID-19 pneumonia: comparison with computed tomography through a simplified scoring system designed for triage. Egypt J Radiol Nucl Med. 2021;52(1):166. doi: 10.1186/s43055-021-00541-x. [DOI] [Google Scholar]
- 9.Goyal A, Tiwari R, Bagarhatta M, Ashwini B, Rathi B, Bhandari S. Role of portable chest radiography in management of COVID-19: Experience of 422 patients from a tertiary care center in India. Indian J Radiol Imaging. 2021;31(1):S94–S100. doi: 10.4103/ijri.IJRI_480_20. Suppl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tan BYQ, Chew NWS, Lee GKH, et al. Psychological Impact of the COVID-19 Pandemic on Health Care Workers in Singapore. Ann Intern Med. 2020;173(4):317–320. doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kobes KJ, Budau-Bymoen A, Thakur Y, Yong-Hing CJ. Multidisciplinary Development of Mobile Radiography Guidelines Reduced the Number of Inappropriate Mobile Exams in Patients Receiving Chest Radiographs in British Columbia. Can Assoc Radiol J. 2020;71(1):110–116. doi: 10.1177/0846537119888357. [DOI] [PubMed] [Google Scholar]
- 12.Tan BP, Lim KC, Goh YG, et al. Radiology Preparedness in the Ongoing Battle against COVID-19: Experiences from Large to Small Public Hospitals in Singapore. Radiol Cardiothorac Imaging. 2020;2(2) doi: 10.1148/ryct.2020200140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foley SJ, O'Loughlin A, Creedon J. Early experiences of radiographers in Ireland during the COVID-19 crisis. Insights Imaging. 2020;11(1):104. doi: 10.1186/s13244-020-00910-6. [DOI] [PMC free article] [PubMed]
- 14.Lewis S, Mulla F. Diagnostic radiographers’ experience of COVID-19, Gauteng South Africa. Radiogr (London, Engl 1995) 2021;27(2):346–351. doi: 10.1016/j.radi.2020.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shanahan MC, Akudjedu TN. Australian radiographers’ and radiation therapists’ experiences during the COVID-19 pandemic. J Med Radiat Sci. 2021;68(2):111–120. doi: 10.1002/jmrs.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tay YX, Tan C, Huang Y, Kwek SL, Wei Y-M, McNulty J. Get comfortable with being uncomfortable: Experiences from diagnostic radiographers a year into the COVID-19 pandemic. J Med imaging Radiat Sci. 2021;52(3):332–339. doi: 10.1016/j.jmir.2021.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chua AQ, Tan MMJ, Verma M, et al. Health system resilience in managing the COVID-19 pandemic: lessons from Singapore. BMJ Glob Heal. 2020;5(9) doi: 10.1136/bmjgh-2020-003317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Au-Yong P-SA, Peh W-M, Koh FH-X, et al. Perceptions of healthcare workers in high-risk areas of a Singapore hospital during COVID-19: a cross-sectional study. Singapore Med J. 2021;1(16) doi: 10.11622/smedj.2021046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sim WY, Chen RC, Aw LP, et al. How to safely and sustainably reorganise a large general radiography service facing the COVID-19 pandemic. Radiography. 2020;26(4):e303–e311. doi: 10.1016/j.radi.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ministry of Health Singapore Additional Pre-emptive Measures to Reduce Risk of Community Transmission. November 14, 2021 https://www.moh.gov.sg/news-highlights/details/additional-pre-emptive-measures-to-reduce-risk-of-community-transmission Published 2020. Accessed. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.