Abstract
Background
Mental health problems are common among clinicians working in public hospitals even in the late stage of the COVID-19 pandemic. Network analysis is a novel approach to explore interactions between mental health problems at the symptom level. This study examined the network structure of comorbid depression and anxiety and their associations with quality of life (QOL) among hospital clinicians in China during the late stage of the COVID-19 pandemic.
Methods
A total of 4931 participants were recruited from October 13 to 22, 2020. The nine-item Patient Health Questionnaire (PHQ-9), seven-item Generalized Anxiety Disorder Scale (GAD-7), and the World Health Organization Quality of Life Questionnaire-Brief Version (WHOQOL-BREF) were used to measure depressive and anxiety symptoms, and QOL, respectively. Central and bridge symptoms were identified with centrality and bridge centrality indices, respectively. Network stability was examined using the case-dropping procedure.
Results
The prevalence of depression (defined as PHQ-9 total score ≥ 5) was 35.1 % [95 % confidence interval (CI) = 33.73–36.41 %)], the prevalence of anxiety (GAD-7 total score ≥ 5) was 32.5 % (95 % CI = 31.20–33.84 %), while the prevalence of comorbid depression and anxiety was 26.9 % (95 % CI = 25.7–28.2 %). “Impaired motor skills”, “Trouble relaxing” and “Uncontrollable worry” were the central symptoms in the whole depression-anxiety network. “Irritability”, “Feeling afraid” and “Sad mood” were the most key bridge symptoms linking depression and anxiety. Three symptoms (“Fatigue”, “Trouble relaxing” and “Nervousness”) were the most strongly and negatively associated with QOL. Neither gender nor the experiences of caring for COVID-19 patients was associated with network global strength, distribution of edge weights or individual edge weights.
Limitations
The causality between variables could not be established. Depressive and anxiety symptoms were assessed by self-report measures, which may result in recall bias and limitations in capturing clinical phenomena.
Conclusions
Both the central (i.e., “Impaired motor skills”, “Trouble relaxing” and “Uncontrollable worry”) and bridge symptoms (i.e., “Irritability”, “Feeling afraid” and “Sad mood”) identified in this network analysis should be targeted in specific treatment and preventive measures for comorbid depressive and anxiety symptoms among clinicians in the late stage of the pandemic. Furthermore, “Fatigue”, “Trouble relaxing” and “Nervousness” are key symptoms to address to improve clinicians' QOL.
Keywords: Depression, Anxiety, Clinicians, Network analysis, COVID-19
1. Introduction
Since the coronavirus disease 2019 (COVID-19) outbreak was first reported in China at the end of December 2019, it has emerged in >200 countries and territories by October 2021, with >236 million confirmed cases (World Health Organization, 2021). With strict public health measures and widespread use of vaccines, COVID-19 epidemic has been well-controlled since late 2020 in China, although occasional outbreaks caused by imported cases from overseas have continued to occur (Burki, 2020). The COVID-19 pandemic has had a negative mental health impact on vulnerable populations particularly healthcare workers resulting in an increased risk of psychiatric problems such as depression and anxiety (Lai et al., 2020; Pan et al., 2022; Tsamakis et al., 2020), as well as comorbid depression and anxiety (Baker et al., 2012; Frewen et al., 2013). Compared with depression or anxiety alone, comorbid depression and anxiety are associated with more severe health outcomes such as greater illness severity, higher risk of chronicity, and more severe functioning impairment (Groen et al., 2020; Liu et al., 2021; Zhou et al., 2017). Therefore, to reduce the likelihood of severe health outcomes, understanding the specific features of comorbid depression and anxiety is important. Moreover, as a widely used health outcome measure, quality of life (QOL) is a multidimensional concept associated with various factors such as physical and psychological health, social relationships, educational level, employment, sense of security and others (Pequeno et al., 2020; The WHOQOL Group, 1998). Both depression and anxiety are negatively associated with QOL (An et al., 2020; Angermeyer et al., 2002; Bodurka-Bevers et al., 2000; Fiorillo and Javed, 2021; Zhang et al., 2021); for example, a cross sectional study found that clinicians with depression had a lower QOL when comparing to those without depression during the COVID-19 pandemic (Zhang et al., 2021).
Recent studies found that psychiatric problems, such as depression and anxiety, are common among clinicians even in the late pandemic stage despite better containment during this period (Cai et al., 2021; Lorusso et al., 2020). Therefore, addressing the depression and anxiety among clinicians during the late stage of the pandemic is an important focus for both clinical practice and research (Tian et al., 2020; Zhao et al., 2021). Both depression and anxiety comprise a cluster of symptoms (Kroenke et al., 2001; Tyrer and Baldwin, 2006). However, most studies only assessed the severity of depression and anxiety, and their comorbidities using standalone total scores of standard scales, which do not reflect the associations and inter-relationships between individual symptoms.
Unlike traditional research approaches, network analysis could quantify the relationships between individual depressive and anxiety symptoms, which has been widely used in clinical research (Beard et al., 2016; Dalege et al., 2017; Epskamp et al., 2018; Marchetti, 2019; Van Borkulo et al., 2017). In the theory of network analysis, psychiatric syndromes and disorders are viewed as an interacting cluster of symptoms, which include nodes representing observed variables (e.g., depressive and anxiety symptoms). Different nodes are connected by edges that represent relationships between nodes (i.e., partial correlations) (Epskamp et al., 2018). The node centrality statistics (e.g., strength, expected influence (EI)) are used to measure nodes' characteristics and determine the central (influential) symptoms in the network (Beard et al., 2016). Central symptoms within a network model have the strongest associations with other symptoms. Since central symptoms may activate other symptoms, they may play a major role in the onset and/or maintenance of a psychiatric syndrome. Thus, targeting central symptoms in preventive measures and interventions may be more efficient (Borsboom and Cramer, 2013). Furthermore, network model provides a new approach to understanding the mechanism of psychiatric comorbidities (Cramer et al., 2010a; Cramer et al., 2010b). For instance, when an individual suffers from a psychiatric disorder, certain symptoms of this disorder may increase the risk of other disorders, which are regarded as bridge symptoms in the network model. Bridge symptoms in the network model may play a critical role in developing and perpetuating comorbidities, and also provide hints for clinicians for preventing and treating psychiatric comorbidities (Jones et al., 2019).
Several studies have applied network analysis on the characteristics of depression and anxiety in various populations. For example, a study reported that “fatigue” was the central and bridge symptom in the network structure of depression and anxiety among migrant Filipino domestic workers (Garabiles et al., 2019). In another study conducted in psychiatric patients, “sad mood” and “worry” were identified as the central symptoms in the network model (Beard et al., 2016). Since the patterns and features of mood syndromes are strongly influenced by socioeconomic contexts and environmental factors (Compton et al., 2006; Kleinman, 2004), it is crucial to examine the network structure of depressive and anxiety symptoms separately in different settings and populations. Additionally, no network analysis on the association between QOL and depressive and anxiety symptoms among clinicians during the pandemic has been reported, although this is important to develop effective strategies to improve QOL in this population.
To date, no studies on comorbid depressive and anxiety symptoms (depression and anxiety hereafter) in clinicians in the late stage of the COVID-19 pandemic have been published using the network model, which gave us the impetus to conduct this study. The study objectives were to investigate the network structure of comorbid depression and anxiety among hospital clinicians during the late stage of the pandemic in China, and to explore the relationships between QOL and depressive and anxiety symptoms.
2. Methods
2.1. Study design and settings
This was a cross-sectional study on the mental health status of clinicians conducted by the National Clinical Research Center for Mental Disorders of China with the support of the Beijing Hospital Authority from October 13 to 22, 2020 in Beijing China. Due to risk of contagion, face-to-face interviews were not conducted during the COVID-19 pandemic. Like other studies (Lai et al., 2020; Sun et al., 2020), WeChat-imbedded “Questionnaire Star” program was adopted to collect data based on consecutive sampling. WeChat is a widely used smartphone-based social communication application with >1.2 active billion users per month in China. All clinicians in Beijing needed to register personal health status using WeChat each week during the pandemic, therefore, all were presumably WeChat users. Eligibility inclusion criteria included: 1) aged 18 years or older; 2) clinicians working in public hospitals in Beijing; 3) able to understand the content of assessment. The study protocol was centrally approved by the ethics committee of Beijing Anding Hospital. A Quick Response code (QR Code) linked to the study introduction and invitation, and the access to questionnaire was designed and adopted. The QR code was distributed to all public hospitals in Beijing by the National Clinical Research Center for Mental Disorders of China, and all clinicians working in these hospitals were invited to participate in this study. After providing the electronic written informed consent, participants could access the data collection form and questionnaire by scanning the QR code using their smartphone.
2.2. Measurements
Severity of depressive symptoms was measured using the Chinese version of the nine-item Patient Health Questionnaire (PHQ-9) (Kroenke et al., 2001). Each item was scored from “0” (not at all) to “3” (nearly every day), with a higher score indicating more severe depressive symptoms. The PHQ-9 has been well-validated in the Chinese populations (Wang and Chen, 2014; Zhang et al., 2013). Severity of anxiety symptoms was measured using the Chinese version of the 7-item Generalized Anxiety Disorder Scale (GAD-7) (Garabiles et al., 2020; Spitzer et al., 2006), which comprises 7 items with each scored from “0” (not at all) to “3” (nearly every day), and higher scores indicate more severe anxiety symptoms. A PHQ-9 total score of ≥5 was considered as "having depression", a GAD-7 total score of ≥5 was considered as "having anxiety", while those with both PHQ-9 total score of ≥5 and GAD-7 total score of ≥5 were considered as "having comorbid depression and anxiety". Global quality of life (QOL) was measured by the first two items of the World Health Organization Quality of Life Questionnaire-brief version (WHOQOL-BREF) (Skevington et al., 2004; The WHOQOL Group, 1998). Higher total scores indicate higher QOL. The Chinese version of the WHOQOL-BREF has been validated in Chinese populations with good sensitivity and specificity (Xia et al., 2012; Yang et al., 2006).
2.3. Statistical analyses
2.3.1. Network estimation
The comorbid depression and anxiety network analysis was performed using R software (R Core Team, 2020). The polychoric correlations between all the PHQ-9 and GAD-7 items were calculated based on the Graphical Gaussian Model (GGM) with the graphic least absolute shrinkage and selection operator (LASSO) and Extended Bayesian Information Criterion (EBIC) model in the R package “qgraph” (Epskamp et al., 2018; Epskamp et al., 2012). The expected influence (EI) was calculated to determine the central (influential) symptoms in the network (Beard et al., 2016). For each node, EI represented the summed weight of all its edges, including positive and negative associations with its immediate neighbor nodes in the network, i.e., EI considered the sign of the association connecting two nodes (i.e., negative vs. positive partial correlation) by summing the magnitude of the edges connected to the node. The role of a symptom as a bridge between depression and anxiety communities was also assessed in this study using the bridge expected influence (bEI) of each symptom. The bEI of one node is the summed edge weights to the nodes of all other symptoms, which reflects the importance of an individual symptom linking two clusters of psychiatric symptoms or two psychiatric disorders (Cramer et al., 2010b; Jones et al., 2021). Furthermore, the predictability of each node was estimated using the package “mgm” (Haslbeck and Waldorp, 2015). Predictability was defined as the variance in a node that is explained by all other nodes in the network. Moreover, the flow network of QOL, depression and anxiety was estimated.
2.3.2. Network stability
To further assess the accuracy of the network, the bootstrap method in the “bootnet” package was used to investigate the stability of centrality and bridge centrality indices based on three procedures. First, the accuracy of edge-weights was estimated by computing confidence intervals (CIs) with non-parametric bootstrapping method (Chernick, 2011). Then, the primary dataset was resampled randomly to create new datasets from which the 95 % CIs were calculated. Second, the correlation stability coefficient (CS-C) was calculated to assess the stability of the EI centrality using subset bootstraps (Costenbader and Valente, 2003). The CS-C represented the maximum proportion of samples that could be removed, such that with 95 % probability the correlation between original centrality indices could reach at least 0.7 (Epskamp et al., 2018). Generally, the CS-C should not be <0.25, and preferably above 0.5. Third, bootstrapped difference tests were performed to evaluate differences in the network's properties (Epskamp and Fried, 2018). This test relied on 95 % CIs, to determine if two edge-weights or two node centrality indices significantly differed from one-another.
2.3.3. Network comparison
As recommended in previous studies (Lai et al., 2020; Zhang et al., 2020), we investigated whether the network characteristics differed between male and female participants, and between clinicians with and without experiences of caring for COVID-19 patients. The Network Comparison Test (NCT) was performed to assess differences in the network structure (e.g., distributions of edge weights), global strength (e.g., the absolute sum of all edge weights of the networks), and each edge between the two networks (i.e., females vs. males; those with experiences of caring for COVID-19 vs. those without experiences of caring for COVID-19) using Holm-Bonferroni correction of p values due to multiple tests (Van Borkulo et al., 2017). These tests were performed with the R-package “NetworkComparisonTest” version 2.0.1 (van Borkulo et al., 2016).
3. Results
3.1. Study sample
Of a total of 5230 were invited to participate in the study, 4931 fulfilled the study entry criteria and completed the assessment (1095 males and 3836 females). The overall prevalence of depression (defined as PHQ-9 total score ≥ 5) was 35.1 % [95 % confidence interval (CI) = 33.73–36.41 %], the prevalence of anxiety (GAD-7 total score ≥ 5) was 32.5 % (95 % CI = 31.20–33.84 %), while the prevalence of comorbid depression (PHQ-9 total score ≥ 5) and anxiety (GAD-7 total score ≥ 5) was 26.9 % (95 % CI = 25.7–28.2 %). The mean age of participants was 36.5 years [standard deviation (SD) = 8.40 years], and mean PHQ-9 score was 3.75 (SD = 4.12), and mean GAD-7 score was 3.17 (SD = 3.40). Mean scores of the PHQ-9 and GAD-7 with their SDs, skewness, and kurtosis are shown in Table S1.
3.2. Network structure
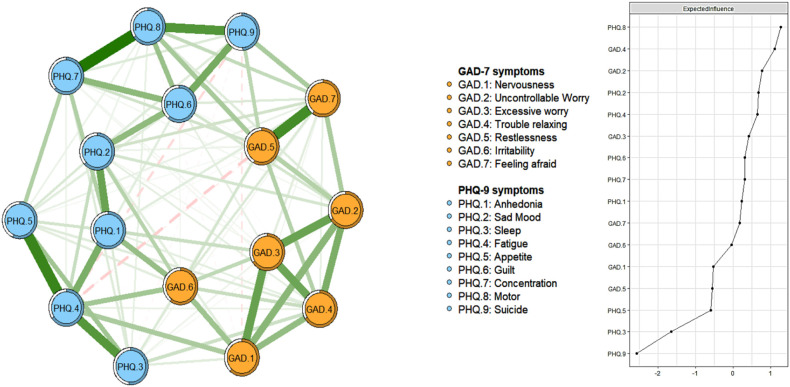
Fig. 1 shows the network structure of depression and anxiety in hospital clinicians during the late stage of the COVID-19 pandemic. The predictability of each symptom is shown as ring-shaped pie charts. The mean predictability was 0.61, indicating that on average 61 % of each node's variance could be accounted for by neighboring nodes. The network model indicates that the connection between GAD.5 (“Restlessness”) and GAD.7 (“Feeling afraid”) was the strongest positive edge in the anxiety community, followed by the edges between GAD.1 (“Nervousness”) and GAD.3 (“Excessive worry”), and between GAD.2 (“Uncontrol worry”) and GAD.3 (“Excessive worry”). In the depression community, the edge between PHQ.7 (“Concentration”) and PHQ.8 (“Motor”) was the strongest one, followed by the edges between nodes PHQ.4 (“Fatigue”) and PHQ.5 (“Appetite”) and between nodes PHQ.8 (“Motor”) and PHQ.9 (“Suicide”).
Fig. 1.
Network structure of depression and anxiety in clinicians during the late stage of the COVID-19 pandemic.
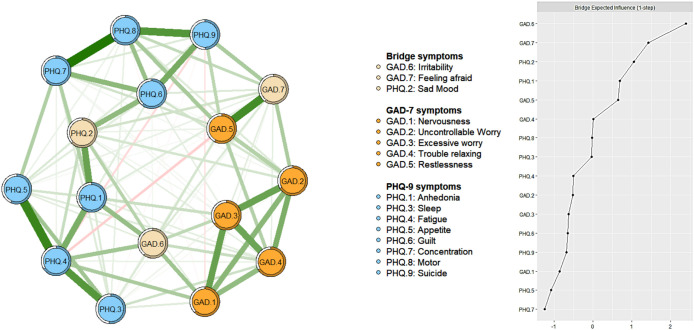
For centrality index EI, the node PHQ.8 (“Motor”) had the highest EI centrality, followed by the nodes GAD.4 (“trouble relaxing”) and GAD.2 (“Uncontrollable worry”) in the whole network (Fig. 1 right part), indicating that the three symptoms are important and influential for understanding the structure of the depression and anxiety network model among hospital clinicians. For bridge EI, GAD.6 (“Irritability”), GAD.7 (“Feeling afraid”) and PHQ.2 (“Sad mood”) were the most key bridge symptoms linking depression and anxiety communities (Fig. 2 ). In the depression and anxiety network structure, the connection between GAD.6 (“Irritability”) and PHQ.4 (“Fatigue”) (average edge weight = 0.137) was the strongest edge, followed by the connections between GAD.5 (“Restlessness”) and PHQ.8 (“Motor”) (average edge weight = 0.128), and between GAD.7 (“Feeling afraid”) and PHQ.9 (“Suicide”) (average edge weight = 0.125). Moreover, there was a negative connection between GAD.5 (“Restlessness”) and PHQ.4 (“Fatigue”) (Fig. 2, Supplementary Table S2).
Fig. 2.
Network structure of depression and anxiety showing bridge symptoms in clinicians during the late stage of the COVID-19 pandemic
3.3. Network stability
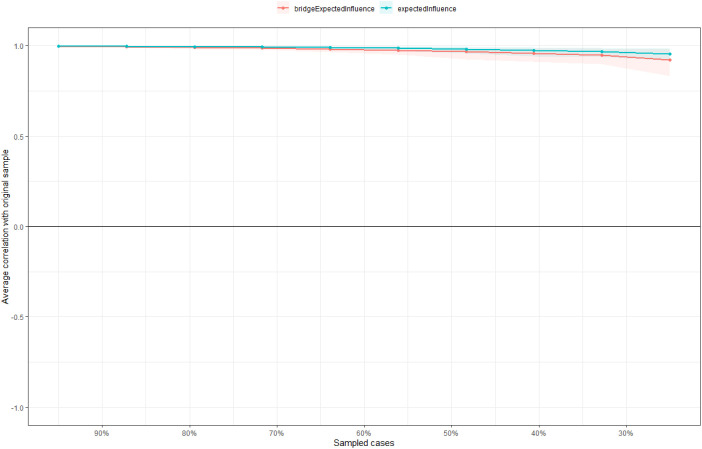
The centrality of EI had an excellent level of stability (i.e., CS-coefficient = 0.75), which indicates that when 75 % of the sample was dropped, the structure of the network did not significantly change (Fig. 3 ). The results of the bootstrap 95 % CI for edges and bootstrapped differences tests for edge weight are shown in supplementary Fig. S1, and the results of estimation of edge weight difference by bootstrapped difference test are shown in supplementary Fig. S2. The bootstrap difference test shows that most of the comparisons between edge weights are statistically significant (Supplementary Fig. S3).
Fig. 3.
The stability of centrality and bridge centrality indices using case-dropping bootstrap.
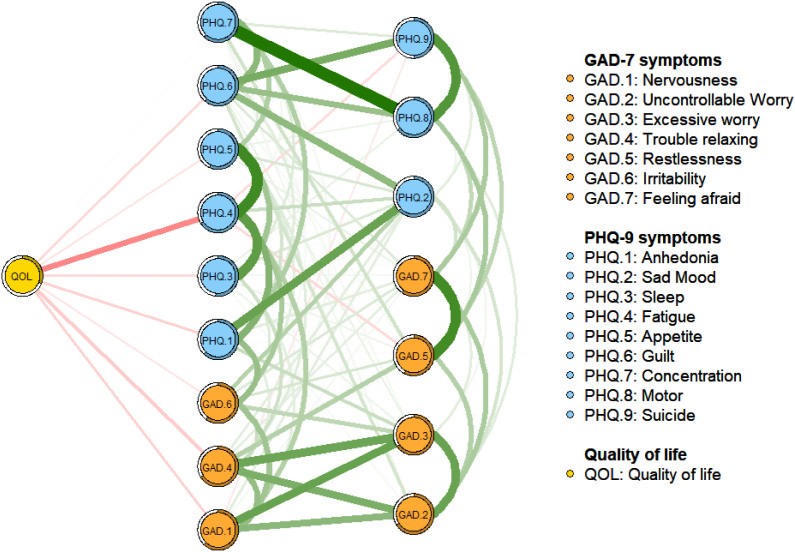
3.4. Flow network of quality of life (QOL)
Following previous studies (An et al., 2020; Hacimusalar et al., 2020), as a widely used health outcome, depression and anxiety was negatively associated with QOL in hospital clinicians. Of the individual symptoms, the node PHQ.4 (“Fatigue”) had the strongest negative association with QOL (average edge weight = −0.15), followed by the GAD.4 (“Trouble relaxing”) (average edge weight = −0.06) and GAD.1 (“Nervousness”) (average edge weight = −0.06) (Fig. 4 ).
Fig. 4.
Flow network of quality of life.
3.5. The confounding effects of age, gender, and experiences caring for COVID-19 patients on the depression and anxiety network model
Previous findings (Cai et al., 2020; Chew et al., 2020; Pappa et al., 2020) indicated that gender, age and the experiences of caring for COVID-19 patients were significantly associated with depression and anxiety in clinicians. Based on previous studies (Dalege et al., 2017; Marchetti, 2019), the depression and anxiety network model and structure indexes were re-estimated after controlling for age, gender and the experiences of caring for COVID-19 patients as covariates. The adjusted network model after controlling for covariates was significantly correlated with the original one (r = 0.66, 95 % CI = [−0.22, 0.69]; p < 0.05) (Supplementary Fig. S4), suggesting that the covariates did not significantly affect the network model.
3.6. Network comparison tests for gender and the experiences caring for COVID-19 patients
The comparison of network models between female (n = 3836) and male (n = 1095) clinicians did not find significant differences in the network global strength (network strength: 8.28 in male participants; 7.92 in female participants; S = 0.35, p = 0.159), and edge weights (M = 0.11, p = 0.272; Supplementary Figs. S5 and S6). Similarly, the comparison of network structure between clinicians with (n = 2055) and without (n = 2876) the experiences of caring for COVID-19 patients did not find significant differences in the network global strength (network strength: 7.94 in clinicians with the experiences of caring for COVID-19 patients; 7.93 in those without the experiences; S: 0.01, p = 0.971), and edge weights (M = 0.09, p = 0.63; Supplementary Figs. S7 and S8).
4. Discussion
To best of our knowledge, this was the first study that characterized the network structure of comorbid depressive and anxiety, and their associations with QOL in Chinese hospital clinicians (N = 4931) during the late stage of the COVID-19 pandemic. In this study, “Impaired motor skills” was the most central symptom in the depression and anxiety network, followed by “Trouble relaxing” and “Uncontrollable worry”. As such, these symptoms are important and influential in terms of understanding the structure of the depression and anxiety network model in this population. Furthermore, “Irritability”, “Feeling afraid” and “Sad mood” were the key bridge symptoms linking depression and anxiety in this sample. We also found that “Fatigue”, “Trouble relaxing” and “Nervousness” were negatively associated with QOL among clinicians.
In the depression and anxiety network model, psychomotor symptoms such as impaired motor skills (“Motor”), inability to relax (“Trouble relaxing”), and uncontrollable worry were the central symptoms among Chinese clinicians during the late stage of the COVID-19 pandemic. This was consistent with the results of a previous study conducted in the Chinese general population during the COVID-19 pandemic (Wang et al., 2020). However, previous studies found that other depressive symptoms, such as “Sad mood” and “Too much worry”, were also the most central symptoms among psychiatric patients (Beard et al., 2016), while “Fatigue”, “Too much worry” and “Sad mood” were the core symptoms among Filipino domestic workers (Garabiles et al., 2019). These inconsistent findings indicate the discrepancy of central symptoms between different study samples and between different study periods. During the late stage of the pandemic, uncertainty remained due to the rapid spread of SARS-CoV-2 Delta variant globally, necessitating the continuation of strict public health measures (He et al., 2021). Hospital clinicians were deployed to provide clinical services and conduct mass rapid nucleic acid test for the population in high-risk areas. Therefore, the heavy workload and high level of stress for clinicians persisted, coupled with quarantine measures such as reduced outdoor physical exercises and recreational activities. Furthermore, clinicians might worry about the risk of infection to themselves, their family members, and colleagues because of the highly contagious variant (Cai et al., 2020) and the limited protective effects of the COVID-19 vaccines. All these factors could increase the risk of psychomotor symptoms such as impaired motor skills, inability to relax, and uncontrollable worry. In the network theory, central symptoms play important roles in maintaining the psychopathology network, hence treating those symptoms could help to ameliorate the relevant psychopathology (Belzer and Schneier, 2004; Cramer et al., 2010a).
Anxiety and depression are commonly co-occurring disorders (Kalin, 2020). A global survey found that 45.7 % of participants with lifetime major depressive disorder had a lifetime history of one or more anxiety disorder (Ferro, 2016). The results from Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study showed that 53 % of those with major depression had significant anxiety (Fava et al., 2004). According to previous neurobiological studies (Etkin and Schatzberg, 2011; Kovner et al., 2019), anxiety and depressive disorders have common changes in prefrontal limbic pathways involved in emotion regulation mechanisms at the brain circuit level. Several meta-analyses also revealed that common structural and functional changes in brain circuits underlying emotion regulation (Etkin and Schatzberg, 2011), executive function (Goodkind et al., 2015), and cognitive control (McTeague et al., 2017) in both anxiety and depression. Further, alterations in prefrontal limbic pathways (Kovner et al., 2019; McTeague et al., 2020) and serotonergic projections arising from the raphe nuclei are associated with both depression and anxiety (An et al., 2016). Moreover, depression is associated with a single nucleotide polymorphisms-heritability of 12–14 %, indicating substantial genetic overlap with anxiety (Purves et al., 2017). From the neuroendocrinological perspective, dysfunctional hypothalamic–pituitary–adrenal (HPA) axis and elevated cortisol are considered common to both depression and anxiety (Chen et al., 2017; Tafet and Nemeroff, 2020).
The network analysis revealed that bridge symptoms connecting depressive and anxiety communities included “Irritability” (becoming easily annoyed or irritable), “Feeling afraid” (feeling afraid as if something awful might happen) and “Sad mood” (feeling down, depressed or hopeless) in clinicians. Our findings are consistent with previous findings (Garabiles et al., 2019; Jones et al., 2021; Wang et al., 2020). For instance, “Irritability” was the bridge symptom in depression and anxiety network model among the general population (Wang et al., 2020), while “Sad mood” was the bridge symptom in depression and anxiety network model in Filipino domestic workers during the COVID-19 pandemic (Garabiles et al., 2019; Jones et al., 2021). Even during the late stage of the COVID-19 pandemic, clinicians had to wear personal protective equipment (PPE) that might result in physical discomfort and difficulty breathing (Salazar de Pablo et al., 2020), all of which could cause irritability among clinicians. Moreover, a study found that “Uncertainty about when the epidemic will be under control” and “Worry about inflicting COVID-19 on family” were the most stressful feelings among clinicians during the pandemic (Hummel et al., 2021), which could isolate clinicians from their families and reduce their social supports (Braquehais et al., 2020). All these factors may trigger feelings of being afraid, depressed or hopeless. In network theory, if bridge symptoms that link comorbid syndromes/disorders could be improved (i.e., “burning the bridges” between syndromes/disorders), the psychiatric comorbidities could be reduced (Jones et al., 2018). Therefore, intervention focusing on these bridge symptoms could reduce the co-occurring depression and anxiety among clinicians. It should be noted that bridge and central symptoms between studies are often not the same in different study samples. For example, compared to our findings, a study conducted among patients with both depression and anxiety found that “psychomotor agitation” or “retardation” was the strongest bridge symptom connecting anxiety and depression clusters, followed by “concentration problems” and “restlessness” (Kaiser et al., 2021). In another study conducted in psychiatric patients, “sad mood” and “worry” were identified as the central symptoms in the network model (Beard et al., 2016).
QOL is a concept that includes a person's physical condition, psychological state, level of independence, social relationships, environment and spirituality (Bonomi et al., 2000). In this study, compared with other symptoms, “Fatigue”, “Trouble relaxing” and “Nervousness” had strong negative associations with QOL in clinicians, which is consistent with previous findings (Jin et al., 2021). Jin et al. (Jin et al., 2021) reported that clinicians with fatigue had significantly lower QOL compared with those without. Other studies found that clinicians reporting higher level of psychological stress and burnout had an increased risk of substance abuse and suicide, especially when they were dealing with huge work demands, illness, deaths, interpersonal conflicts and lack of knowledge or support during public health crisis (e.g., outbreaks of infectious diseases (Aiken et al., 2002; Su et al., 2009)), all of which could lower QOL.
The strength of this study included the large sample size and use of the network approach to visualize comorbid depressive and anxiety symptoms in clinicians. However, several limitations should be noted. First, this was a cross-sectional study, therefore the causality between variables could not be established. Future longitudinal studies are warranted. Second, depressive and anxiety symptoms were assessed by self-report measures, which may result in recall bias and limitations in capturing clinical phenomena (Coughlin, 1990). Third, the central symptoms and bridge symptoms identified in this study may not be generalized to other groups during other stages of the pandemic.
In conclusion, central symptoms (i.e., “Impaired motor skills”, “Trouble relaxing” and “Uncontrollable worry”) and bridge symptoms (i.e., “Irritability”, “Feeling afraid” and “Sad mood”) identified in this network of comorbid depression and anxiety should be targeted in specific treatment and preventive measures for comorbid depressive and anxiety symptoms in Chinese hospital clinicians in the late stage of the pandemic. For example, cognitive behavioral therapy (CBT) targeting these symptoms using behavioral activation and cognitive restructuring could be beneficial for clinicians with comorbid depression and anxiety (Björgvinsson et al., 2014). Additionally, government and healthcare agencies need to address depression and anxiety in hospital clinicians in the late stage of the COVID-19 pandemic with effective interventions. Furthermore, “Fatigue”, “Trouble relaxing” and “Nervousness” are important symptoms to address to improve QOL.
CRediT authorship contribution statement
Study design: Yu-Tao Xiang, Sha Sha.
Data collection, analysis and interpretation: Chee H. Ng, Yu Jin, Tengfei Tian, Sixiang Liang, Zhe Wang, Yinqi Liu, Qinge Zhang, Ling Zhang.
Drafting of the manuscript: Yu Jin, Yu-Tao Xiang.
Critical revision of the manuscript: Teris Cheung, Zhaohui Su.
Approval of the final version for publication: all co-authors.
Role of the funding source
There is no funding for this research.
Declaration of competing interest
None.
Acknowledgements
We thank the trade union of Beijing Municipal Administration of Hospitals and all staff who supplied this study. Meanwhile, we would like to thank Mr. Changshun Xu, deputy director of Beijing Municipal Administration of Hospitals, Mr. Cunliang Wang, vice chairman of the trade union of Beijing Municipal Administration of Hospitals, and Mr. Yan Li, the trade union of Beijing Municipal Administration of Hospitals for their work to this study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jad.2022.06.051.
Appendix A. Supplementary data
Supplementary material
References
- Aiken L.H., Clarke S.P., Sloane D.M., Sochalski J., Silber J.H. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- An Y., et al. Mirtazapine exerts an anxiolytic-like effect through activation of the median raphe nucleus-dorsal hippocampal 5-HT pathway in contextual fear conditioning in rats. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2016;70:17–23. doi: 10.1016/j.pnpbp.2016.04.014. [DOI] [PubMed] [Google Scholar]
- An Y., et al. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J. Affect. Disord. 2020;276:312–315. doi: 10.1016/j.jad.2020.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angermeyer M.C., Holzinger A., Matschinger H., Stengler-Wenzke K. Depression and quality of life: results of a follow-up study. Int J Soc Psychiatry. 2002;48(3):189–199. doi: 10.1177/002076402128783235. [DOI] [PubMed] [Google Scholar]
- Baker A.L., Thornton L.K., Hiles S., Hides L., Lubman D.I. Psychological interventions for alcohol misuse among people with co-occurring depression or anxiety disorders: a systematic review. J. Affect. Disord. 2012;139(3):217–229. doi: 10.1016/j.jad.2011.08.004. [DOI] [PubMed] [Google Scholar]
- Beard C., et al. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychol. Med. 2016;46(16):3359–3369. doi: 10.1017/S0033291716002300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belzer K., Schneier F.R. Comorbidity of anxiety and depressive disorders: issues in conceptualization, assessment, and treatment. J. Psychiatr. Pract. 2004;10(5):296–306. doi: 10.1097/00131746-200409000-00003. [DOI] [PubMed] [Google Scholar]
- Björgvinsson T., et al. Effectiveness of cognitive behavior therapy for severe mood disorders in an acute psychiatric naturalistic setting: a benchmarking study. Cogn. Behav. Ther. 2014;43(3):209–220. doi: 10.1080/16506073.2014.901988. [DOI] [PubMed] [Google Scholar]
- Bodurka-Bevers D., et al. Depression, anxiety, and quality of life in patients with epithelial ovarian cancer. Gynecol. Oncol. 2000;78(3):302–308. doi: 10.1006/gyno.2000.5908. [DOI] [PubMed] [Google Scholar]
- Bonomi A.E., Patrick D.L., Bushnell D.M., Martin M. Validation of the United States' version of the World Health Organization quality of life (WHOQOL) instrument. J. Clin. Epidemiol. 2000;53(1):1–12. doi: 10.1016/s0895-4356(99)00123-7. [DOI] [PubMed] [Google Scholar]
- van Borkulo C., et al. 2016. Package ‘NetworkComparisonTest’. [Google Scholar]
- Borsboom D., Cramer A.O. Network analysis: an integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Braquehais M.D., et al. The impact of the COVID-19 pandemic on the mental health of healthcare professionals. QJM. 2020 doi: 10.1093/qjmed/hcaa207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burki T. China's successful control of COVID-19. Lancet Infect. Dis. 2020;20(11):1240–1241. doi: 10.1016/S1473-3099(20)30800-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Q., et al. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: a case-control study. J. Affect. Disord. 2020;275:210–215. doi: 10.1016/j.jad.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai H., et al. Prevalence of problematic internet use and its association with quality of life among undergraduate nursing students in the later stage of COVID-19 pandemic era in China. Am. J. Addict. 2021;30(6):585–592. doi: 10.1111/ajad.13216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C., et al. The exercise-glucocorticoid paradox: how exercise is beneficial to cognition, mood, and the brain while increasing glucocorticoid levels. Front. Neuroendocrinol. 2017;44:83–102. doi: 10.1016/j.yfrne.2016.12.001. [DOI] [PubMed] [Google Scholar]
- Chernick M.R. John Wiley & Sons; 2011. Bootstrap Methods: A Guide for Practitioners and Researchers. [Google Scholar]
- Chew N.W.S., et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton W.M., Conway K.P., Stinson F.S., Grant B.F. Changes in the prevalence of major depression and comorbid substance use disorders in the United States between 1991–1992 and 2001–2002. Am. J. Psychiatry. 2006;163(12):2141–2147. doi: 10.1176/ajp.2006.163.12.2141. [DOI] [PubMed] [Google Scholar]
- Costenbader E., Valente T.W. The stability of centrality measures when networks are sampled. Soc. Networks. 2003;25(4):283–307. [Google Scholar]
- Coughlin S.S. Recall bias in epidemiologic studies. J. Clin. Epidemiol. 1990;43(1):87–91. doi: 10.1016/0895-4356(90)90060-3. [DOI] [PubMed] [Google Scholar]
- Cramer A.O., Waldorp L.J., van der Maas H.L., Borsboom D. Comorbidity: a network perspective. Behav Brain Sci. 2010;33(2–3):137–150. doi: 10.1017/S0140525X09991567. discussion 150–193. [DOI] [PubMed] [Google Scholar]
- Cramer A.O., Waldorp L.J., Van Der Maas H.L., Borsboom D. Complex realities require complex theories: refining and extending the network approach to mental disorders. Behav. Brain Sci. 2010;33(2–3):178. [Google Scholar]
- Dalege J., Borsboom D., van Harreveld F., van der Maas H.L.J. Network analysis on attitudes: a brief tutorial. Soc. Psychol. Personal. Sci. 2017;8(5):528–537. doi: 10.1177/1948550617709827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S., Fried E.I. 2018. Package ‘bootnet’. [Google Scholar]
- Epskamp S., Cramer A.O., Waldorp L.J., Schmittmann V.D., Borsboom D. Qgraph: network visualizations of relationships in psychometric data. J. Stat. Softw. 2012;48(4):1–18. [Google Scholar]
- Epskamp S., Borsboom D., Fried E.I. Estimating psychological networks and their accuracy: a tutorial paper. Behav. Res. Methods. 2018;50(1):195–212. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etkin A., Schatzberg A.F. Common abnormalities and disorder-specific compensation during implicit regulation of emotional processing in generalized anxiety and major depressive disorders. Am. J. Psychiatry. 2011;168(9):968–978. doi: 10.1176/appi.ajp.2011.10091290. [DOI] [PubMed] [Google Scholar]
- Fava M., et al. Clinical correlates and symptom patterns of anxious depression among patients with major depressive disorder in STAR* D. Psychol. Med. 2004;34(7):1299–1308. doi: 10.1017/s0033291704002612. [DOI] [PubMed] [Google Scholar]
- Ferro M.A. Major depressive disorder, suicidal behaviour, bipolar disorder, and generalised anxiety disorder among emerging adults with and without chronic health conditions. Epidemiol. Psychiatr. Sci. 2016;25(5):462–474. doi: 10.1017/S2045796015000700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorillo A., Javed A. Education and training in psychiatry in low- and middle-income countries during and after the COVID-19 pandemic. Asia Pac. Psychiatry. 2021;13(4) doi: 10.1111/appy.12500. [DOI] [PubMed] [Google Scholar]
- Frewen P.A., Schmittmann V.D., Bringmann L.F., Borsboom D. Perceived causal relations between anxiety, posttraumatic stress and depression: extension to moderation, mediation, and network analysis. Eur. J. Psychotraumatol. 2013;4 doi: 10.3402/ejpt.v4i0.20656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garabiles M.R., Lao C.K., Xiong Y., Hall B.J. Exploring comorbidity between anxiety and depression among migrant filipino domestic workers: a network approach. J. Affect. Disord. 2019;250:85–93. doi: 10.1016/j.jad.2019.02.062. [DOI] [PubMed] [Google Scholar]
- Garabiles M.R., et al. Psychometric validation of PHQ-9 and GAD-7 in Filipino migrant domestic workers in Macao (SAR), China. J. Pers. Assess. 2020;102(6):833–844. doi: 10.1080/00223891.2019.1644343. [DOI] [PubMed] [Google Scholar]
- Goodkind M., et al. Identification of a common neurobiological substrate for mental illness. JAMA Psychiatry. 2015;72(4):305–315. doi: 10.1001/jamapsychiatry.2014.2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groen R.N., et al. Comorbidity between depression and anxiety: assessing the role of bridge mental states in dynamic psychological networks. BMC Med. 2020;18(1):308. doi: 10.1186/s12916-020-01738-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacimusalar Y., Kahve A.C., Yasar A.B., Aydin M.S. Anxiety and hopelessness levels in COVID-19 pandemic: a comparative study of healthcare professionals and other community sample in Turkey. J. Psychiatr. Res. 2020;129:181–188. doi: 10.1016/j.jpsychires.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslbeck J., Waldorp L.J. arXiv; 2015. mgm: Estimating Time-varying Mixed Graphical Models in High-dimensional Data. preprint arXiv:1510.06871. [Google Scholar]
- He L., et al. Risk factors for anxiety and depressive symptoms in doctors during the coronavirus disease 2019 pandemic. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.687440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummel S., et al. Mental health among medical professionals during the COVID-19 pandemic in eight european countries: cross-sectional survey study. J. Med. Internet Res. 2021;23(1) doi: 10.2196/24983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin Y., et al. Prevalence of fatigue and its association with quality of life among frontline clinicians in ophthalmology and otolaryngology departments during the COVID-19 pandemic. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.678917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones P.J., Mair P., Riemann B.C., Mugno B.L., McNally R.J. A network perspective on comorbid depression in adolescents with obsessive-compulsive disorder. J. Anxiety Disord. 2018;53:1–8. doi: 10.1016/j.janxdis.2017.09.008. [DOI] [PubMed] [Google Scholar]
- Jones P.J., Ma R., McNally R.J. Bridge centrality: a network approach to understanding comorbidity. Multivariate Behav Res. 2019:1–15. doi: 10.1080/00273171.2019.1614898. [DOI] [PubMed] [Google Scholar]
- Jones P.J., Ma R., McNally R.J. Bridge centrality: a network approach to understanding comorbidity. Multivariate Behav Res. 2021;56(2):353–367. doi: 10.1080/00273171.2019.1614898. [DOI] [PubMed] [Google Scholar]
- Kaiser T., Herzog P., Voderholzer U., Brakemeier E.L. Unraveling the comorbidity of depression and anxiety in a large inpatient sample: network analysis to examine bridge symptoms. Depress. Anxiety. 2021;38(3):307–317. doi: 10.1002/da.23136. [DOI] [PubMed] [Google Scholar]
- Kalin N.H. The critical relationship between anxiety and depression. Am. Psychiatr. Assoc. 2020:365–367. doi: 10.1176/appi.ajp.2020.20030305. [DOI] [PubMed] [Google Scholar]
- Kleinman A. Culture and depression. N. Engl. J. Med. 2004;351(10):951–953. doi: 10.1056/NEJMp048078. [DOI] [PubMed] [Google Scholar]
- Kovner R., Oler J.A., Kalin N.H. Cortico-limbic interactions mediate adaptive and maladaptive responses relevant to psychopathology. Am. J. Psychiatry. 2019;176(12):987–999. doi: 10.1176/appi.ajp.2019.19101064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., et al. Comorbid anxiety and depression, depression, and anxiety in comparison in multi-ethnic community of West China: prevalence, metabolic profile, and related factors. J. Affect. Disord. 2021;298:381–387. doi: 10.1016/j.jad.2021.10.083. [DOI] [PubMed] [Google Scholar]
- Lorusso D., Ray-Coquard I., Oaknin A., Banerjee S. Clinical research disruption in the post-COVID-19 era: will the pandemic lead to change? ESMO Open. 2020;5(5) doi: 10.1136/esmoopen-2020-000924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchetti I. Hopelessness: a network analysis. Cogn. Ther. Res. 2019;43(3):611–619. [Google Scholar]
- McTeague L.M., et al. Identification of common neural circuit disruptions in cognitive control across psychiatric disorders. Am. J. Psychiatry. 2017;174(7):676–685. doi: 10.1176/appi.ajp.2017.16040400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McTeague L.M., et al. Identification of common neural circuit disruptions in emotional processing across psychiatric disorders. Am. J. Psychiatry. 2020;177(5):411–421. doi: 10.1176/appi.ajp.2019.18111271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan X., et al. Prevalence of mental health problems and associated risk factors among military healthcare workers in specialized COVID-19 hospitals in Wuhan, China: a cross-sectional survey. Asia Pac. Psychiatry. 2022;14(1) doi: 10.1111/appy.12427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S., et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pequeno N.P.F., Cabral N.L.A., Marchioni D.M., Lima S., Lyra C.O. Quality of life assessment instruments for adults: a systematic review of population-based studies. Health Qual. Life Outcomes. 2020;18(1):208. doi: 10.1186/s12955-020-01347-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purves K.L., et al. Vol. 203844. BioRxiv; 2017. The Common Genetic Architecture of Anxiety Disorders. [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2020. R: A Language and Environment for Statistical Computing. [Google Scholar]
- Salazar de Pablo G., et al. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J. Affect. Disord. 2020;275:48–57. doi: 10.1016/j.jad.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skevington S.M., Lotfy M., O'Connell K.A. The World Health Organization's WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual. Life Res. 2004;13(2):299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Su J.A., Weng H.H., Tsang H.Y., Wu J.L. Mental health and quality of life among doctors, nurses and other hospital staff. Stress Health. 2009;25(5):423–430. [Google Scholar]
- Sun D., et al. Psychological impact of 2019 novel coronavirus (2019-nCoV) outbreak in health workers in China. Epidemiol. Infect. 2020;148 doi: 10.1017/S0950268820001090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tafet G.E., Nemeroff C.B. Pharmacological treatment of anxiety disorders: the role of the HPA axis. Frontiers in Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.00443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The WHOQOL Group Development of the World Health Organization WHOQOL-BREF quality of life assessment. WHOQOL Group. Psychol. Med. 1998;28(3):551–558. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- Tian T., et al. Mental health burden of frontline health professionals treating imported patients with COVID-19 in China during the pandemic. Psychol. Med. 2020:1–2. doi: 10.1017/S0033291720002093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsamakis K., et al. COVID-19 pandemic and its impact on mental health of healthcare professionals. Exp. Ther. Med. 2020;19(6):3451–3453. doi: 10.3892/etm.2020.8646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyrer P., Baldwin D. Generalised anxiety disorder. Lancet. 2006;368(9553):2156–2166. doi: 10.1016/S0140-6736(06)69865-6. [DOI] [PubMed] [Google Scholar]
- Van Borkulo C.D., et al. Vol. 10. 2017. Comparing Network Structures on Three Aspects: A Permutation Test. Manuscript submitted for publication. [DOI] [PubMed] [Google Scholar]
- Wang X.Q., Chen P.J. Population ageing challenges health care in China. Lancet. 2014;383(9920):870. doi: 10.1016/S0140-6736(14)60443-8. [DOI] [PubMed] [Google Scholar]
- Wang Y., Hu Z., Feng Y., Wilson A., Chen R. Changes in network centrality of psychopathology symptoms between the COVID-19 outbreak and after peak. Mol. Psychiatry. 2020;25(12):3140–3149. doi: 10.1038/s41380-020-00881-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2021. WHO Coronavirus (COVID-19) Dashboard. [Google Scholar]
- Xia P., Li N., Hau K.T., Liu C., Lu Y. Quality of life of chinese urban community residents: a psychometric study of the mainland Chinese version of the WHOQOL-BREF. BMC Med. Res. Methodol. 2012;12:37. doi: 10.1186/1471-2288-12-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang S.C., Kuo P.W., Wang J.D., Lin M.I., Su S. Development and psychometric properties of the dialysis module of the WHOQOL-BREF Taiwan version. J. Formos. Med. Assoc. 2006;105(4):299–309. doi: 10.1016/s0929-6646(09)60121-2. [DOI] [PubMed] [Google Scholar]
- Zhang Y.L., et al. Validity and reliability of patient health Questionnaire-9 and patient health Questionnaire-2 to screen for depression among college students in China. Asia Pac. Psychiatry. 2013;5(4):268–275. doi: 10.1111/appy.12103. [DOI] [PubMed] [Google Scholar]
- Zhang W.R., et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 2020;89(4):242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H.H., et al. Depression and its relationship with quality of life in frontline psychiatric clinicians during the COVID-19 pandemic in China: a national survey. Int. J. Biol. Sci. 2021;17(3):683–688. doi: 10.7150/ijbs.56037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y.J., et al. Mental health status and quality of life in close contacts of COVID-19 patients in the post-COVID-19 era: a comparative study. Transl. Psychiatry. 2021;11(1):505. doi: 10.1038/s41398-021-01623-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y., et al. Comorbid generalized anxiety disorder and its association with quality of life in patients with major depressive disorder. Sci. Rep. 2017;7:40511. doi: 10.1038/srep40511. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material