Abstract
Study Objectives:
Whether short or insufficient sleep are risk factors for new-onset nocturnal gastroesophageal reflux (nGER).
Methods:
In this 10-year longitudinal study, adult general-population women in Uppsala, Sweden, answered questionnaires on sleep, nGER, and other conditions on 2 occasions. Participants at baseline totaled 6,790, while participants at follow-up totaled 4,925. “Short sleep” was defined as sleeping < 6 hours/night and “insufficient sleep” was defined as reporting an average actual sleep duration below 80% of the self-estimated need for sleep duration but without “short sleep.” nGER was defined as reporting heartburn or acid reflux after going to bed sometimes, often, or very often. The confounding factors—age, body mass index, physical activity, caffeine intake, smoking habits, alcohol dependence, depression, anxiety, and snoring—were defined from the questionnaire.
Results:
At baseline, 839 participants reported short sleep and 1,079 participants were defined as having insufficient sleep. Both participants with insufficient sleep and short sleep had nGER more often than those with sufficient sleep (26% vs 17% vs 10%, respectively). At follow-up, a new onset of nGER was twice as common among those with insufficient or short sleep at baseline and follow-up, compared with those with sufficient sleep at baseline and follow-up, even after adjusting for confounding factors (odds ratio 2.0 [1.5–2.8], P < .001).
Conclusions:
Insufficient sleep and short sleep are associated with nGER. Persistent insufficient and/or short sleep independently increases the risk of developing nGER over a 10-year follow-up. Women seeking treatment for nGER should be questioned about their sleep habits to identify insufficient sleep as a possible causative factor.
Citation:
Emilsson OI, Al Yasiry H, Theorell-Haglöw J, Ljunggren M, Lindberg E. Insufficient sleep and new onset of nocturnal gastroesophageal reflux among women: a longitudinal cohort study. J Clin Sleep Med. 2022;18(7):1731–1737.
Keywords: gastroesophageal reflux, sleep duration, insufficient sleep
BRIEF SUMMARY
Current Knowledge/Study Rationale: Insufficient sleep and nocturnal gastroesophageal reflux are common in the female general population. Experimental studies have shown that induced sleep deprivation increases gastroesophageal reflux, but it is unknown if insufficient sleep in the general population may cause gastroesophageal reflux.
Study Impact: In this study, we found that insufficient sleep is an independent risk factor for developing nocturnal gastroesophageal reflux among women. This negative association was seen even among women with normal sleep duration but with subjectively reported insufficient sleep. Women seeking health care for gastroesophageal reflux should be assessed for insufficient sleep, as insufficient sleep may be a modifiable risk factor for their gastroesophageal reflux.
INTRODUCTION
Insufficient sleep is common in the general population, with a reported prevalence of 7%–25%.1–3 Gastroesophageal reflux is another prevalent condition, with a reported prevalence of 10%–20%, and in a significant percentage of these cases nocturnal gastroesophageal reflux (nGER) is also present.4–6
Insufficient sleep can lead to poorer alertness and a decrease in general performance and it is associated with comorbidities such as diabetes, high blood pressure, asthma, obesity, coronary heart disease, and stroke.7,8 Notably, nGER may contribute to poorer quality of sleep, and studies from the general population have found an association between nGER and sleep induction, sleep maintenance, and daytime sleepiness.9–11 In addition, nGER is associated with the sleep-disrupting disease obstructive sleep apnea.12,13 Treating nGER may improve self-reported sleep quality, although objective sleep parameters appear to be unaffected.4
Interestingly, even though studies using polysomnography and simultaneous esophageal pH measurements have found that some reflux episodes induce changes in sleep stage or awakenings, the reflux episodes are preceded even more frequently by sleep stage changes or awakenings.14–17 A recent small interventional study found that reflux episodes, measured by esophageal pH, were significantly increased after a night of induced sleep deprivation.18 Together, this indicates that insufficient sleep could increase the risk of nGER. However, no studies have evaluated whether this applies to insufficient sleep in the general population. Moreover, it is unclear if this association is only acute and transient, or if it is also long lasting.
The definition of insufficient sleep in epidemiological studies is often based solely on reported sleep duration, usually as less than 6 hours a night.8 However, this measurement does not take account of the individual variation in sleep need.3 For this reason, some studies have adapted a sleep sufficiency index, defined as the actual sleep duration percentage of sleep need.3
Our aim was to investigate whether insufficient sleep is a risk factor for developing nocturnal reflux among females in the general population. For this purpose, we used a population-based female cohort with a 10-year follow-up and considered both sleep duration and the sleep sufficiency index for the definition of insufficient sleep.
METHODS
Population and study design
The current study used data from the population-based cohort Sleep and Health in Women, a 10-year prospective, observational study that was initiated in 2000 with a questionnaire sent out to randomly selected women above the age of 20 in the city of Uppsala, Sweden, where 7,051 women participated at baseline (response rate 71.6%).19 Of these participants, 5,193 also participated in the 10-year follow-up.20 For cross-sectional analysis, data from the baseline population were used, where 6,790 women had data on sleep duration and the estimated need for sleep. For the prospective analysis, follow-up data were added from the longitudinal part of the Sleep and Health in Women study, in which 4,925 women had answered questions about sleep duration at follow-up.
Definitions and categorization of sleep sufficiency and sleep duration
Both at baseline and at follow-up, the women answered 2 questions relating to sleep duration in hours: “How many hours do you sleep each night on average?” (habitual sleep duration), and “How many hours sleep per night do you estimate you need to be rested?” (estimated need for sleep). The questions used in this study were identical at baseline and follow-up. Based on the answers, the sleep sufficiency index (SSI)3 was calculated, defined as “habitual sleep duration” divided by “estimated need for sleep.” The strength of the SSI is that it may be independent of the individual sleep need, which varies considerably between individuals.3
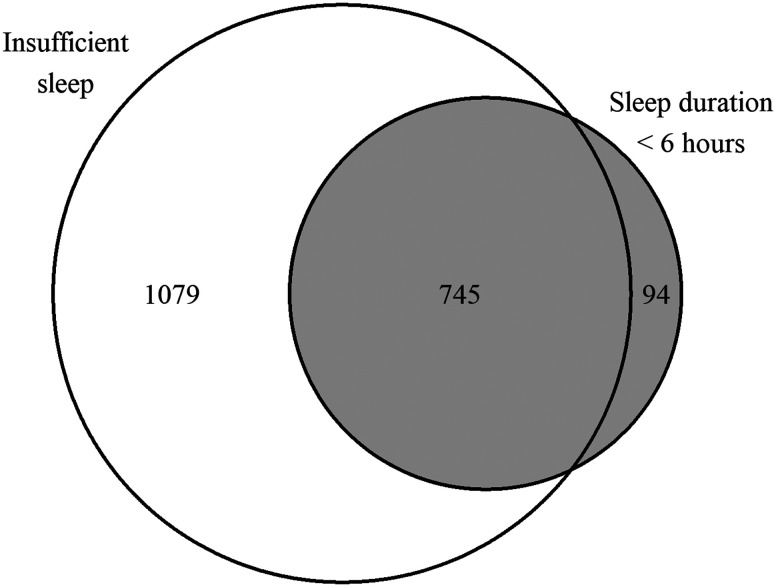
The women were divided into 3 groups. First, those with sleep duration of ≥ 6 hours and with an SSI of ≥ 0.8 were defined as having “sufficient sleep” (n = 4,872). Second, those with an SSI of < 0.8 but with sleep duration of ≥ 6 hours were defined as having “insufficient sleep” (n = 1,079). Third, those reporting sleep duration of < 6 hours were defined as having “short sleep,” irrespective of SSI (n = 839) (Figure 1).
Figure 1. Venn diagram of participants with insufficient sleep and sleep duration below 6 hours at baseline.
Participants in the gray area were defined as having short sleep, while participants in the white area were defined as having insufficient sleep (defined as a sleep sufficiency index of < 0.8).
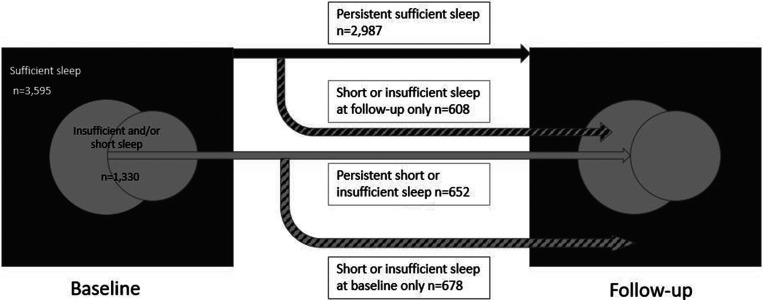
For the prospective analyses, a measurement reflecting sleep duration and SSI transition over time was constructed from both baseline and follow-up data (Figure 2). For this measurement, all the participants reporting sleep duration of < 6 hours and/or an SSI of < 0.8 were defined as having “short or insufficient sleep,” while participants reporting sleep duration of ≥ 6 hours and with an SSI of ≥ 0.8 were defined as having “sufficient sleep.” Participants defined as having short or insufficient sleep at both baseline and follow-up were defined as “Persistent short or insufficient sleep” (n = 652). Participants reporting short or insufficient sleep only at baseline were defined as “short or insufficient sleep only at baseline” (n = 678). Subjects reporting short or insufficient sleep only at follow-up were defined as “short or insufficient sleep only at follow-up” (n = 608). Participants with sufficient sleep at baseline and follow-up were defined as “persistent sufficient sleep” (n = 2,987).
Figure 2. Flow chart for the definition of study groups for prospective analysis.
At baseline, 1,824 participants had a sleep sufficiency index of < 0.8, while 839 participants reported short sleep duration (< 6 hours) (Figure 1). Of the 1,824 participants with a sleep sufficiency index of < 0.8, 745 were included in the group with short sleep duration, while the remaining 1,079 participants reported sleep duration of ≥ 6 hours and were categorized as having insufficient sleep for the further cross-sectional analysis.
Definition of nocturnal gastroesophageal reflux
At both baseline and follow-up, nGER was defined using the following question: “How often do you experience heartburn or acid reflux after going to bed?”. Participants answered on a 5-point scale (never–rarely–sometimes–often–very often). Participants answering sometimes, often, or very often were categorized as having nGER. Participants reporting nGER at follow-up but not at baseline were considered to have new-onset nGER.11
Definitions and categorization of covariates
Prior to analysis, a directed acyclic graph (a diagram displaying assumptions about the relationship between variables) was used to identify potential confounders.21 The identified confounders were age, body mass index (BMI), physical activity, caffeine intake, smoking habits, alcohol consumption, and snoring. All of these were available and self-reported from the baseline questionnaire.
BMI was calculated as weight divided by height squared (kg/m2). Delta-BMI as a measure of change in BMI over time was defined as BMI at follow-up minus BMI at baseline.
Physical activity levels were categorized into 3 groups. “Low physical activity” was defined as spending most free time doing stationary activities, such as reading books or watching television. “Moderate physical activity” was defined as reporting a minimum of 4 hours of moderate physical activity a week, such as cycling or walking. “High physical activity” was defined as spending a minimum of 3 hours a week on physically challenging activities, such as swimming or running.22,23
Caffeine intake was categorized into 3 groups: “0 cups a day,” “1–2 cups a day,” and “3 or more cups a day.”9 Smoking habits were categorized into 3 groups: “current smokers,” “former smokers,” and “never smokers.” Alcohol dependence was defined as 2 or more positive responses to the 4 questions from the Cutting down, Annoyance by criticism, Guilty feeling and Eye opener (CAGE) questionnaire.24 Depression and anxiety were defined from the Hospital Anxiety and Depression Scale (HADS).25 A score from 8–10 was defined as possible depression or anxiety on each respective subscale, and a score above 10 was defined as probable depression or anxiety. Snoring was assessed using the question: “How often do you snore loudly and disturbingly?” Participants answered on a 5-point scale (never–rarely–sometimes–often–very often). Participants answering sometimes, often, or very often were defined as snorers.11
Participants were asked to state how severe their problems were regarding daytime sleepiness. Participants answered on a 5-point scale (no problems–small–moderate–severe–very severe). Those who answered that they had severe or very severe problems were defined as having daytime sleepiness.26
Statistical analysis
The main exposure in this study was sleep sufficiency variables and the outcome was nGER. Both cross-sectional and prospective analyses were performed.
Descriptive and cross-sectional analysis
In the cross-sectional descriptive analysis of baseline data, common descriptive statistics were used and a Venn diagram was drawn to explore the association between insufficient sleep and short sleep duration. Descriptive data were presented as the median and interquartile range for nonnormally distributed continuous variables; the mean and standard deviation for normally distributed continuous variables and n (%) for categorical variables. Associations between insufficient sleep and nGER were analyzed using the chi-square test for unadjusted analysis, and multiple logistic regression was used for adjusted analysis (based on the a priori defined model from the directed acyclic graph, as described above).
Longitudinal analysis
For the longitudinal analysis, the outcome was new-onset nGER. All the confounders except for delta-BMI were defined from baseline data. For the analysis of new-onset nGER at follow-up, participants reporting nGER at baseline were excluded (n = 589) and the data were analyzed using the chi-square test for unadjusted analysis, while multiple logistic regression was used for adjusted analysis (based on an a priori–defined model from the directed acyclic graph, as described previously). In addition, a second analysis of the association between sleep insufficiency and nGER was performed on longitudinal data using multiple logistic regression, where participants reporting short sleep (< 6 hours) at baseline or follow-up were excluded.
The statistical analysis was performed in STATA, version 16.1 for Windows (StataCorp, College Station, TX). A P value below .05 was considered statistically significant.
Ethical approval
Informed consent was obtained from all the participants, and ethical approval was obtained from the Ethics Committee at the Medical Faculty at Uppsala University (Dnr 99486 and Dnr 2009/379).
RESULTS
Baseline characteristics
Participants with insufficient sleep were younger, while those with short sleep were older than those with sufficient sleep. Among participants with insufficient sleep and short sleep duration, smoking, depression, and anxiety were more common, the physical activity level was lower, snoring was slightly more common, and daytime sleepiness much more common, compared with participants with sufficient sleep. BMI, coffee consumption, and alcohol dependence were similar in all 3 groups (Table 1).
Table 1.
Baseline characteristics.
| Sufficient Sleep (Sleep Duration ≥ 6 h/night, SSI ≥ 0.8) (n = 4,872) | Insufficient Sleep (Sleep Duration ≥ 6 h/night, SSI < 0.8) (n = 1,079) | Short Sleep (Sleep Duration < 6 h/night, any SSI) (n = 839) | |
|---|---|---|---|
| Age, y | 43 (29 – 57) | 37 (27 – 50) | 53 (39 – 67) |
| BMI, kg/m2 | 24.0 ± 4.0 | 24.0 ± 4.1 | 24.9 ± 4.6 |
| Never smokers | 3,017 (62.3%) | 607 (56.7%) | 466 (56.1%) |
| Former smokers | 1,077 (22.2%) | 243 (22.7%) | 202 (24.3%) |
| Current smokers | 748 (15.5%) | 220 (20.6%) | 162 (19.5%) |
| Alcohol dependence | 262 (5.6%) | 83 (8.0%) | 42 (5.5%) |
| No coffee intake | 226 (4.7%) | 55 (5.1%) | 29 (3.5%) |
| 1–2 cups a day | 1,355 (28.1%) | 300 (28.0%) | 218 (26.3%) |
| 3 or more cups a day | 3,241 (67.2%) | 715 (66.8%) | 581 (70.2%) |
| Low physical activity | 792 (16.4%) | 237 (22.2%) | 211 (25.7%) |
| Moderate physical activity | 3,003 (62.2%) | 632 (59.2%) | 503 (61.3%) |
| High physical activity | 1,032 (21.4%) | 199 (18.6%) | 106 (12.9%) |
| No depression | 4,233 (90.1%) | 822 (79.2%) | 579 (73.0%) |
| Possible depression | 339 (7.2%) | 146 (14.1%) | 143 (18.0%) |
| Probable depression | 125 (2.7%) | 70 (6.7%) | 71 (9.0%) |
| No anxiety | 3,465 (73.4%) | 554 (52.6%) | 413 (51.5%) |
| Possible anxiety | 797 (16.9%) | 264 (25.1%) | 178 (22.2%) |
| Probable anxiety | 456 (9.7%) | 235 (22.3%) | 211 (26.3%) |
| Snoring | 1,158 (24.4%) | 285 (26.8%) | 234 (29.5%) |
| Daytime sleepiness | 384 (8.0%) | 288 (27.1%) | 255 (31.3%) |
Data are presented as the median and interquartile range for non–normally distributed continuous variables, the mean and standard deviation for normally distributed continuous variables, and n (%) for categorical variables. Sufficient sleep is defined as sleeping ≥ 6 hours/night and having an SSI of ≥ 0.8. Insufficient sleep is defined as sleeping ≥ 6 hours/night but having an SSI of < 0.8. Short sleep is defined as sleeping < 6 hours/night. BMI = body mass index, SSI = sleep sufficiency index.
Cross-sectional analysis—insufficient sleep and nGER at baseline
The prevalence of nGER in women with insufficient sleep was twice as high compared with those with sufficient sleep (Table 2). In women with short sleep, the prevalence of nGER was nearly 3 times as high compared with those with sufficient sleep (Table 2). After adjusting for confounding factors, both insufficient sleep and short sleep were significantly associated with nGER (Table 3).
Table 2.
Prevalence of nGER at baseline by sleep sufficiency categories.
| nGER | P | |
|---|---|---|
| Sufficient sleep (n = 4, 872) | 478 (9.9%) | Reference |
| Insufficient sleep (and ≥ 6 hours/night sleep) (n = 1,079) | 181 (16.9%) | < .001 |
| Short sleep (< 6 hours/night) (n = 839) | 217 (26.1%) | < .001 |
nGER = nocturnal gastroesophageal reflux.
Table 3.
ORs (with 95% CIs) for nGER at baseline by insufficient sleep.
| nGER | ||
|---|---|---|
| Unadjusted OR (95% CI) | Adjusted OR (95% CI) | |
| Sufficient sleep | 1.00 | 1.00 |
| Insufficient sleep (and ≥ 6 hours/night sleep) | 1.85 (1.54–2.23) | 1.62 (1.31–1.99) |
| Short sleep (< 6 hours/night) | 3.22 (2.69–3.86) | 2.32 (1.87–2.88) |
Unadjusted analysis and analysis adjusted for age, body mass index, smoking status, caffeine consumption, alcohol dependence, physical activity level, depression, anxiety, and snoring. CI = confidence interval, nGER = nocturnal gastroesophageal reflux, OR = odds ratio.
Prospective analysis—insufficient sleep and nGER at follow-up
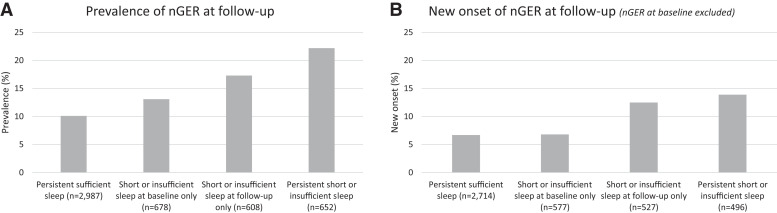
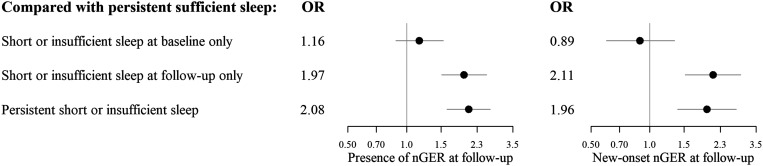
Women with persistent insufficient or short sleep displayed the highest prevalence of nGER at follow-up, followed by those with insufficient or short sleep only at follow-up (Figure 3). Among participants without nGER at baseline (n = 4,314), new-onset nGER at follow-up was most frequent among those with insufficient or short sleep at follow-up, irrespective of baseline status (Figure 3). Having insufficient or short sleep only at follow-up, or having persistent insufficient or short sleep, were both associated with prevalent or new-onset nGER, after adjusting for confounding factors (Figure 4).
Figure 3. Insufficient sleep and nGER at follow-up.
(A) Prevalence of nGER at follow-up by reported sleep duration and sleep sufficiency index transitions. (B) New onset of nGER at follow-up by reported sleep duration and sleep sufficiency index transitions. nGER = nocturnal gastroesophageal reflux.
Figure 4. Adjusted ORs with 95% confidence intervals for the presence and new onset of nGER at follow-up by reported sleep duration at baseline and follow-up.
ORs are adjusted for age, BMI at baseline and delta-BMI, physical activity, caffeine intake, smoking habits, alcohol consumption, depression, anxiety, and snoring. The analysis of new-onset nGER excluded women with nGER at baseline. BMI = body mass index, nGER = nocturnal gastroesophageal reflux, OR = odds ratio.
A secondary analysis, adjusted for confounding factors and based only on participants with normal sleep duration (≥ 6 hours) at both baseline and follow-up, showed that insufficient sleep only at follow-up (n = 389), but not persistent insufficient sleep (n = 232), was associated with increased odds of prevalent nGER, compared with persistent sufficient sleep (n = 2,987) (adjusted odds ratio [95% confidence interval]: 1.81 [1.29–2.52]; 1.42 [0.93–2.17], respectively). However, when studying new-onset nGER, insufficient sleep only at follow-up (n = 342) was associated with new-onset nGER, but it was nonsignificant for persistent insufficient sleep (n = 186), compared with persistent sufficient sleep (n = 2,714) (adjusted odds ratio [95% confidence interval]: 2.02 [1.36–3.00]; 1.41 [0.79–2.51], respectively).
DISCUSSION
In this study of adult women from the general population in Sweden, cross-sectional analysis revealed that participants who had insufficient sleep at baseline had nGER approximately twice as frequently as those with sufficient sleep. This pattern was also seen among participants with insufficient sleep with sleep duration of ≥ 6 hours/night. The longitudinal analysis found that participants with insufficient or short sleep either only at follow-up or persistently had double the odds of new-onset nGER. The results were consistent after adjusting for confounding variables.
As previously mentioned, our definition of insufficient sleep, based on a low ratio between actual sleep duration and perceived needed sleep duration, is thought to contain information regarding both quality of sleep and sleep duration.3 In this study, insufficient sleep was very common among women with short sleep duration. However, more than half the group of women reporting insufficient sleep reported normal sleep duration (≥ 6 hours/night). This suggests that, among women categorically defined as having sufficient sleep (≥ 6 hours/night), a significant proportion perceive a need for a longer sleep to feel properly rested.
The association between insufficient sleep and nGER was somewhat stronger among participants with short sleep duration, but it was nonetheless also significant among women with insufficient sleep and normal sleep duration. Our results therefore support the hypothesis that we need to take account of more factors than actual sleep duration when studying the effects of insufficient sleep.
In the present study, we found that insufficient sleep may also be a risk factor for developing nGER among women in the general population. Interestingly, those with new onset of insufficient or short sleep had a similar or higher new onset of nGER than those with persistent sleep impairment. A recent experimental study, where induced sleep deprivation was shown to lead to nGER among healthy individuals, further supports a possible causal association.18 Interestingly, only 2 nights of sleep deprivation were sufficient to induce a clear increase in esophageal acid exposure. This increase in acid exposure induced by sleep deprivation, possibly from more frequent transient relaxations in the lower esophageal sphincter, may explain why nGER increases among women with insufficient sleep. Further, short sleep has been shown to lead to visceral hyperalgesia and may therefore aggravate nGER symptoms.27
The observation that sleep deprivation appears to induce nGER relatively quickly18 may explain why the frequency of new-onset nGER was similarly increased among participants with persistently insufficient sleep and new onset of insufficient sleep. This is further supported by our finding that those with persistent insufficient or short sleep had a somewhat higher prevalence of nGER at follow-up than those with insufficient or short sleep only at follow-up, while new-onset nGER was similar in these 2 groups or even higher among those with insufficient or short sleep only at follow-up. In other words, among participants reporting persistently insufficient sleep, those at risk of developing nGER may have already developed nGER at baseline and therefore been excluded from the analysis of new-onset nGER.
Strengths and weaknesses
One of the main strengths of this study was the large population studied in a prospective manner. The detailed nature of the questionnaires enabled adjustments for relevant confounders, which further enhanced the validity of the results. However, some methodological issues need to be addressed. First, even though the prospective nature of this study with a 10-year follow-up was valuable, the fact that we only had data from 2 time points 10 years apart reduces the certainty of interpretations regarding the direction of the association between insufficient sleep and nGER. Second, no objective measurements were performed in this study, which impairs the validity of the definitions of nGER and insufficient sleep.28 Polysomnography and esophageal pH measurements would have been valuable in order to objectively measure sleep parameters and nGER, respectively, but this was not possible in this study due to the size of the cohort. We also lacked more detailed information on gastroesophageal reflux in general, which hindered our ability to study the significance of other aspects of reflux, such as use of proton pump inhibitor, Barrett’s esophagus, and daytime reflux. Third, all the data collected were self-reported, which may increase the risk of recall bias. Lastly, the populations in this study comprised only adult females, making the conclusions only generalizable to adult women.
Despite these limitations, this study has some clinical relevance. First, this study implies that insufficient sleep is an independent risk factor for the development of nGER, and the development of nGER may come soon after the occurrence of insufficient sleep. Second, this study implies that experiencing insufficient sleep (defined by a ratio of < 0.8 between actual sleep duration and estimated need for sleep) may be of clinical or public health interest, as it is associated with negative outcomes, even though actual sleep duration was ≥ 6 hours. In our cohort, most women with insufficient sleep reported a habitual sleep duration of at least 6 hours/night, indicating that a significant group of participants with insufficient sleep would have been missed if they were only defined by short sleep duration.
Previous studies have found that nGER may impair sleep quality.9,10,17,23,24 According to our data, impaired sleep might then provoke nGER, thus potentially creating a vicious circle.
CONCLUSIONS
Insufficient sleep, with or without short sleep duration (< 6 hours/night), was associated with a higher prevalence of nGER among adult women. Having persistent insufficient sleep, as well as a persistent short sleep duration, increased significantly the risk of developing nGER over 10 years. These associations were similar after adjusting for confounding factors. It is therefore clinically important to identify insufficient sleep, even in the setting of normal sleep time, to interfere with and hinder negative complications such as nGER. Also, patients seeking treatment for nGER should be questioned about their sleep habits to identify insufficient sleep as a possible causative factor.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. Work for this study was performed at the Department of Medical Sciences, Respiratory, Allergy, and Sleep Research, Uppsala University, Sweden. This study was supported by grants from Agreement on Medical Training and Clinical Research (ALF), Uppsala University; The Swedish Heart-Lung Foundation; and The Bror Hjerpstedt Foundation. The authors report no conflicts of interests.
ABBREVIATIONS
- BMI
body mass index
- nGER
nocturnal gastroesophageal reflux
- SSI
sleep sufficiency index
REFERENCES
- 1. Liu Y , Wheaton AG , Chapman DP , Cunningham TJ , Lu H , Croft JB . Prevalence of healthy sleep duration among adults—United States, 2014 . MMWR Morb Mortal Wkly Rep. 2016. ; 65 ( 6 ): 137 – 141 . [DOI] [PubMed] [Google Scholar]
- 2. Liljenberg B , Almqvist M , Hetta J , Roos BE , Agren H . The prevalence of insomnia: the importance of operationally defined criteria . Ann Clin Res. 1988. ; 20 ( 6 ): 393 – 398 . [PubMed] [Google Scholar]
- 3. Broman JE , Lundh LG , Hetta J . Insufficient sleep in the general population . Clin Neurophysiol. 1996. ; 26 ( 1 ): 30 – 39 . [DOI] [PubMed] [Google Scholar]
- 4. Gerson LB , Fass R . A systematic review of the definitions, prevalence, and response to treatment of nocturnal gastroesophageal reflux disease . Clin Gastroenterol Hepatol. 2009. ; 7 ( 4 ): 372 – 378, quiz 367 . [DOI] [PubMed] [Google Scholar]
- 5. Bruley des Varannes S , Errieau G , Tessier C . [Two thirds of patients with gastroesophageal reflux have nocturnal symptoms: survey by 562 general practitioners of 36,663 patients] . Presse Med. 2007. ; 36 ( 4 Pt 1 ): 591 – 597 . [DOI] [PubMed] [Google Scholar]
- 6. Farup C , Kleinman L , Sloan S , et al . The impact of nocturnal symptoms associated with gastroesophageal reflux disease on health-related quality of life . Arch Intern Med. 2001. ; 161 ( 1 ): 45 – 52 . [DOI] [PubMed] [Google Scholar]
- 7. Abrams RM . Sleep deprivation . Obstet Gynecol Clin North Am. 2015. ; 42 ( 3 ): 493 – 506 . [DOI] [PubMed] [Google Scholar]
- 8. Anothaisintawee T , Reutrakul S , Van Cauter E , Thakkinstian A . Sleep disturbances compared to traditional risk factors for diabetes development: Systematic review and meta-analysis . Sleep Med Rev. 2016. ; 30 : 11 – 24 . [DOI] [PubMed] [Google Scholar]
- 9. Shaker R , Castell DO , Schoenfeld PS , Spechler SJ . Nighttime heartburn is an under-appreciated clinical problem that impacts sleep and daytime function: the results of a Gallup survey conducted on behalf of the American Gastroenterological Association . Am J Gastroenterol. 2003. ; 98 ( 7 ): 1487 – 1493 . [DOI] [PubMed] [Google Scholar]
- 10. Mody R , Bolge SC , Kannan H , Fass R . Effects of gastroesophageal reflux disease on sleep and outcomes . Clin Gastroenterol Hepatol. 2009. ; 7 ( 9 ): 953 – 959 . [DOI] [PubMed] [Google Scholar]
- 11. Hägg SA , Emilsson ÖI , Franklin K , Janson C , Lindberg E . Nocturnal gastroesophageal reflux increases the risk of daytime sleepiness in women . Sleep Med. 2019. ; 53 : 94 – 100 . [DOI] [PubMed] [Google Scholar]
- 12. Gislason T , Janson C , Vermeire P , et al . Respiratory symptoms and nocturnal gastroesophageal reflux: a population-based study of young adults in three European countries . Chest. 2002. ; 121 ( 1 ): 158 – 163 . [DOI] [PubMed] [Google Scholar]
- 13. Emilsson OI , Janson C , Benediktsdóttir B , Júlíusson S , Gíslason T . Nocturnal gastroesophageal reflux, lung function and symptoms of obstructive sleep apnea: results from an epidemiological survey . Respir Med. 2012. ; 106 ( 3 ): 459 – 466 . [DOI] [PubMed] [Google Scholar]
- 14. Mello-Fujita L , Roizenblat S , Frison CR , et al . Gastroesophageal reflux episodes in asthmatic patients and their temporal relation with sleep architecture . Braz J Med Biol Res. 2008. ; 41 ( 2 ): 152 – 158 . [DOI] [PubMed] [Google Scholar]
- 15. Suzuki M , Saigusa H , Kurogi R , et al . Arousals in obstructive sleep apnea patients with laryngopharyngeal and gastroesophageal reflux . Sleep Med. 2010. ; 11 ( 4 ): 356 – 360 . [DOI] [PubMed] [Google Scholar]
- 16. Ing AJ , Ngu MC , Breslin AB . Obstructive sleep apnea and gastroesophageal reflux . Am J Med. 2000. ; 108 ( 4, suppl 1 ): 120 – 125 . [DOI] [PubMed] [Google Scholar]
- 17. Shepherd K , Ockelford J , Ganasan V , Holloway R , Hillman D , Eastwood P . Temporal relationship between night-time gastroesophageal reflux events and arousals from sleep . Am J Gastroenterol. 2020. ; 115 ( 5 ): 697 – 705 . [DOI] [PubMed] [Google Scholar]
- 18. Yamasaki T , Quan SF , Fass R . The effect of sleep deficiency on esophageal acid exposure of healthy controls and patients with gastroesophageal reflux disease . Neurogastroenterol Motil. 2019. ; 31 ( 12 ): e13705 . [DOI] [PubMed] [Google Scholar]
- 19. Svensson M , Lindberg E , Naessen T , Janson C . Risk factors associated with snoring in women with special emphasis on body mass index: a population-based study . Chest. 2006. ; 129 ( 4 ): 933 – 941 . [DOI] [PubMed] [Google Scholar]
- 20. Spörndly-Nees S , Åsenlöf P , Theorell-Haglöw J , Svensson M , Igelström H , Lindberg E . Leisure-time physical activity predicts complaints of snoring in women: a prospective cohort study over 10 years . Sleep Med. 2014. ; 15 ( 4 ): 415 – 421 . [DOI] [PubMed] [Google Scholar]
- 21. Shrier I , Platt RW . Reducing bias through directed acyclic graphs . BMC Med Res Methodol. 2008. ; 8 ( 1 ): 70 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lindberg E , Berne C , Franklin KA , Svensson M , Janson C . Snoring and daytime sleepiness as risk factors for hypertension and diabetes in women—a population-based study . Respir Med. 2007. ; 101 ( 6 ): 1283 – 1290 . [DOI] [PubMed] [Google Scholar]
- 23. Lissner L , Bengtsson C , Björkelund C , Wedel H . Physical activity levels and changes in relation to longevity. A prospective study of Swedish women . Am J Epidemiol. 1996. ; 143 ( 1 ): 54 – 62 . [DOI] [PubMed] [Google Scholar]
- 24. Ewing JA . Detecting alcoholism. The CAGE questionnaire . JAMA. 1984. ; 252 ( 14 ): 1905 – 1907 . [DOI] [PubMed] [Google Scholar]
- 25. Snaith RP . The Hospital Anxiety and Depression Scale . Health Qual Life Outcomes. 2003. ; 1 ( 1 ): 29 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Theorell-Haglöw J , Åkerstedt T , Schwarz J , Lindberg E . Predictors for development of excessive daytime sleepiness in women: a population-based 10-year follow-up . Sleep. 2015. ; 38 ( 12 ): 1995 – 2003 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Schey R , Dickman R , Parthasarathy S , et al . Sleep deprivation is hyperalgesic in patients with gastroesophageal reflux disease . Gastroenterology. 2007. ; 133 ( 6 ): 1787 – 1795 . [DOI] [PubMed] [Google Scholar]
- 28. Miller CB , Gordon CJ , Toubia L , et al . Agreement between simple questions about sleep duration and sleep diaries in a large online survey . Sleep Health. 2015. ; 1 ( 2 ): 133 – 137 . [DOI] [PubMed] [Google Scholar]