Summary
This study evaluated the clinical characteristics of mental health of child and adolescent psychiatric patients during temporary school closure throughout the coronavirus 2019 (COVID-19) pandemic in Japan using the Questionnaire - Children with Difficulties (QCD) and other useful psychological rating scales. The participants were those who visited the Department of Child and Adolescent Psychiatry, Kohnodai Hospital. From those 1,463 participants, case and control groups were selected: 92 patients who visited the hospital during the temporary school closure from March 2020 to May 2020 (case group) and randomly sampled sex- and age-matched 92 patients during the pre-COVID period from April 2017 to March 2020 (control group). QCD is a parent-assessed questionnaire designed to evaluate the difficulties of children along the course of a day, right from waking up in the morning to retiring to bed at night. Lower scores indicate stronger difficulties. QCD scores were compared between the two groups in each of the following age groups: elementary school (6-12 years of age) and junior high school (12-15 years of age). In elementary school students, scores "during school" of QCD indicating functioning or disabilities during school hours were 3.31 ± 2.52 and 4.52 ± 2.33 in case group and control group, respectively (p < 0.05). In junior high school students, scores "Attention-Deficit Hyperactivity Disorder Rating Scale (ADHD-RS)" indicating ADHD symptoms were 16.78 ± 12.69 and 11.80 ± 10.40 in case group and control group, respectively (p < 0.05). The findings suggest that the closure of schools due to the pandemic might worsen difficulties among elementary school patients, and hyperactivity and impulsivity might increase among junior high school patients. The long-term impact of stress caused by school closure on child and adolescent psychiatric patients needs to be investigated in the future.
Keywords: Questionnaire - Children with Difficulties (QCD), clinical characteristics, during school, Attention-Deficit Hyperactivity Disorder Rating Scale (ADHD-RS), hyperactivity and impulsivity
Introduction
Coronavirus disease 2019 (COVID-19), which emerged in December 2019, turned into a pandemic and spread worldwide in 2020 (1). The social distancing measures adopted for preventing the spread of the infection disrupted the daily routine of people. According to United Nations Educational, Scientific and Cultural Organization (UNESCO), as of April 1, 2020, schools were suspended nationwide in 172 countries (2). In Japan, owing to the spread of COVID-19, school closures continued from March 2, 2020, to May 25, 2020. The children were forced to stay at home to curb the infection and were hence unable to lead normal lives. School is crucial to help maintain mental health function as a mental health system for children and adolescents with and without mental health issues (3-5).
COVID-19 is associated with psychiatric problems in several groups, including patients affected by the disease and clinicians who care for them (6,7). Furthermore, COVID-19 is linked to psychiatric symptoms in the general population of adults and children as well (8). Children who were quarantined at home experienced symptoms of anxiety, depression, and post-traumatic stress disorder (9,10). People with mental health disorders are especially vulnerable during times of crisis (11). The effects of COVID-19 on the mental state of general children have been examined, but how are children with mental problems affected?
There are some studies on the effects of temporary school closure on the mental health of children. An increased risk of emotional and behavioral problems was reported among adolescents in Indonesia (12). Children who were physically active during school closures had fewer behavioral problems. Children of parents with anxiety symptoms were at higher risk for emotional symptoms (13). Loneliness during school closures was associated with gaming addiction behaviors among young people (14). School closures due to the COVID-19 outbreak caused anxiety, depression, and stress in children (15). Children with poor academic performance were associated with higher risk of anxiety-related and obsessive compulsive disorder-related symptoms (16). In a study of Japanese elementary and junior high school students, the school closures disrupted their sleep rhythms, eating habits, and physical activity. As a result, children became less active and energetic, and found it harder to find things that interested them (17). The effects of temporary school closure on the mental state of general children have been examined, but how did the lives of children with mental problems change between temporary school closure compared to the pre- COVID period? In the normal period, the prevalence of bullying among children with Autism Spectrum Disorders (ASD) or attention-deficit hyperactivity disorder (ADHD) was high (18). Bullying was related to having ADHD, lower social skills, and some form of conversational disability (19).
This study aimed to evaluate the clinical characteristics of the child and adolescent psychiatric patients in the period of temporary school closure during COVID-19. Temporary school closure during COVID-19 is expected to have some effect on difficulties in their daily life.
Participants and Methods
Study design and setting
The present study used data from Registry Study of Child and Adolescent Mental Health in Japan (http://www. ncgmkohnodai.go.jp/subject/100/200/opt10018111401. pdf). The participants comprised patients who visited Department of Child and Adolescent Psychiatry, Kohnodai Hospital, National Center for Global Health and Medicine, between April 2017 and May 2020 for the first time. A retrospective case-control design was utilized to evaluate patients' daily lives throughout temporary school closure during the COVID-19 pandemic. First, the participants were allocated to one of the following two groups: patients who visited the hospital during the temporary school closure from March 2020 to May 2020 and patients who visited the hospital from April 2017 to March 2020. Second, patients with incomplete data and preschool patients were excluded from the former group. They were case group. The same number of sex- and age-matched patients with case group was randomly sampled from the latter group. They were control group. The two groups were compared in each age category: elementary school patients (6-12 years of age) and junior high school patients (12-15 years of age). The Questionnaire - Children with Difficulties (QCD) is a parent-assessed questionnaire designed to evaluate difficulties in a child's functioning during specific periods of the day (20). The QCD scores were compared between case and control groups. Furthermore, five other psychological rating scales were used for the comparison, namely, Tokyo Autistic Behavior Scale (TABS) (21), Attention- Deficit Hyperactivity Disorder Rating Scale (ADHD-RS) (22), Oppositional Defiant Behavior Inventory (ODBI) (23), Depression Self-Rating Scale for Children (DSRS) (24), and Spence Children's Anxiety Scale (SCAS) (25).
The study protocol was approved by Ethical Committee of National Center for Global Health and Medicine (NCGM-G-003603-00) (Tokyo, Japan) and was conducted in accordance with the tenets of Declaration of Helsinki. There was no written or verbal informed consent because informed consent was obtained from all participants as per Ethical Guidelines for Medical and Health Research Involving Human Subjects of Japan. The guidelines state that, "it is not always necessary to obtain informed consent from study participants. However, researchers must publish information on the implementation of the study, including the purpose of the study for observational studies only using past clinical records and not human tissue samples". The purpose, methods, and analyses of the study and the details on how to refuse participation were posted in the hospital outpatient clinic. In addition, the data were anonymized throughout the study period. Information from this study may contain potentially identifiable patient information, and data sharing is restricted by Ethical Committee of National Center for Global Health and Medicine based on Ethical Guidelines for Medical and Health Research Involving Human Subjects of Japan. However, the data can be accessed by contacting Ethical Committee of National Center for Global Health and Medicine.
Recruitment of participants
This study comprised Japanese patients who visited our department between April 2017 and May 2020. We allowed consultation of patients < 15 years of age at the initial visit. Psychologists and psychiatrists designed the initial interview forms, which included the demographic characteristics of the patients and clinical implications. Subsequently, the questionnaires were constructed using QCD, TABS, ADHD-RS, ODBI, DSRS, and SCAS. Professionals specializing in child and adolescent psychiatry diagnosed and treated all patients according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) (26). Patients with a moderate-to-severe intellectual disability according to DSM-5, organic brain disease, drug-induced psychiatric disease, traumatic brain injury, and genetic syndromes were referred to other medical institutions and were excluded from this study.
Measurement tools
QCD: This questionnaire consists of a total of 20 questions designed to assess the child's daily life functioning or disabilities along the course of a day, right from waking up in the morning to retiring to bed at night (Supplemental Appendix 1, https://www. globalhealthmedicine.com/site/supplementaldata. html?ID=48). This form is filled out by caregivers. Each item is provided with a score of 0-3, and a score of 0 indicates the most severe condition (20). The reliability and validity of this questionnaire have been established (27).
TABS: This tool is rated by the child's caretaker to assess the behavior of children with ASD. The tool comprises 39 items that are provisionally grouped into the following four areas: interpersonal-social relationship, language-communication, habit-mannerism, and others. Each item has a score of 0-2, and the highest possible total score is 78. The higher the score, the stronger are the autistic characteristics (21).
ADHD-RS: This is an 18-item tool used by the child's caretaker to assess ADHD symptoms (22). Takayanagi et al. standardized Japanese version of ADHD-RS, which includes two factors: hyperactivity/impulsiveness and inattention. Each item is provided with a score of 0-3, and a total score of 54 indicates a condition of the highest severity (28).
ODBI: This comprises 18 questions covering DSM-IV-TR diagnostic criteria for ADHD, Oppositional Defiant Disorder (ODD), and conduct disorder. Each item is provided with a score of 0-3, and a total score of 54 indicates the highest severity. Participants with ODBI scores > 20 are considered to have ODD (23).
DSRS: This is a self-rating scale for depression in childhood. The 18-item scale was established based on a 37-item inventory associated with major depressive syndromes. Each item is provided with a score of 0-2, and a total score of 36 suggests the highest severity (24). Denda investigated Japanese children and adolescents, and the results showed that a cutoff score of 15 can be used to demonstrate the risk of depression (29).
SCAS: This questionnaire can evaluate the symptoms of various anxiety disorders, particularly social phobia, obsessive-compulsive disorder, and panic disorder/ agoraphobia. The 38-question test can be filled out by the child or the parent. Each item is provided with a score of 0-3, and a score of 114 is suggestive of the most severe condition (25). The internal consistency and test-retest reliability was satisfied in Japanese children and adolescents (30).
Statistical analysis
Mann-Whitney U test was employed to compare the continuous variables between the two groups. All statistical tests were two-tailed, and p-values < 0.05 were considered statistically significant. The analyses were performed using the Easy R Package, version 1.40 (31).
Results
Participants and Descriptive Data
Figure 1 depicts the flowchart of the participants. From April 2017 to May 2020, 1463 patients consulted our department. From March 2020 to May 2020, which corresponds to the temporary school closure period, 103 patients came for consultation; from April 2017 to March 2020, 1360 patients came for consultation. When we excluded those with incomplete data and preschool patients, case group consisted of 92 patients, and control group consisted of 92 randomly sampled sex- and age-matched patients.
Figure 1.
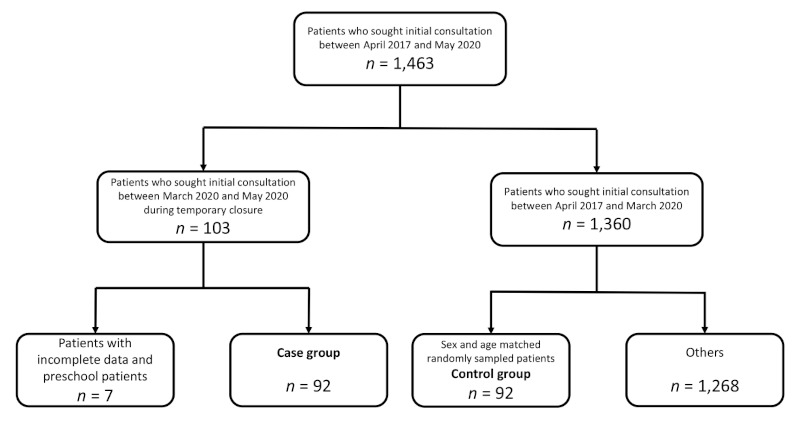
The flowchart of the participants.
Of the 92 patients, 42 were elementary school students (27 males, 15 females) and 50 were junior high school students (21 males, 29 females). The average age of the elementary school students was 9.29 ± 1.70 years (range, 6-12 years). The average age of the junior high school students was 13.32 ± 0.71 years (range, 12-15 years). Tables 1 and 2 present the clinical characteristics of elementary and junior high school students, respectively (both case and control groups). Each parameter was a result of Mann-Whitney U test.
In elementary school students, total scores of QCD were 24.26 ± 11.83 and 28.69 ± 8.69 in case group and control group, respectively. In junior high school students, total scores of QCD were 26.82 ± 12.11 and 24.96 ± 12.29 in case group and control group, respectively. Tables 3 and 4 present the QCD scores of elementary and junior high school students, respectively. Each parameter was the result of Mann-Whitney U test.
Outcome Data
In elementary school students, there were no significant differences in TABS, ADHD-RS, ODBI, DSRS, and SCAS scores between the two groups (Table 1).
Table 1. Clinical characteristics of elementary school students.
| Variables | Case, % (n = 42) | Control, % (n = 42) | Effect Size | p value |
|---|---|---|---|---|
| Age (mean ± standard deviation) | 9.29 ± 1.70 | 9.29 ± 1.70 | - | - |
| Male sex (%) | 64.3 (n = 27) | 64.3 (n = 27) | - | - |
| TABS score | 17.86 ± 10.80 | 16.45 ± 9.69 | 0.14 | NS |
| ADHD-RS | 20.64 ± 13.79 | 19.98 ± 11.02 | 0.05 | NS |
| ODBI | 24.12 ± 17.24 | 26.40 ± 14.86 | 0.14 | NS |
| DSRS | 11.93 ± 5.27 | 13.71 ± 6.09 | 0.31 | NS |
| SCAS | 29.02 ± 19.22 | 33.88 ± 18.85 | 0.26 | NS |
Score ranges: Age, 6-12 years old. TABS (Tokyo Autistic Behavior Scale): 0-78 points. ADHD-RS (ADHD-Rating Scale): 0-54 points. ODBI (Oppositional Defiant Behavior Inventory): 0-54 points. DSRS (Depression Self-Rating Scale for Children): 0-36 points. SCAS (Spence Children's Anxiety Scale): 0-114 points.
In junior high school students, there were no significant differences in TABS, ODBI, DSRS, and SCAS scores between the two groups. Scores "ADHD-RS" indicating ADHD symptoms were 16.78 ± 12.69 and 11.80 ± 10.40 in case group and control group, respectively (p < 0.05) (Table 2).
Table 2. Clinical characteristics of junior high school students.
| Variables | Case, % (n = 50) | Control, % (n = 50) | Effect Size | p value |
|---|---|---|---|---|
| Age (mean ± standard deviation) | 13.32 ± 0.71 | 13.32 ± 0.71 | - | - |
| Male sex (%) | 42.0 (n = 21) | 42.0 (n = 21) | - | - |
| TABS score | 13.0 ± 11.49 | 10.5 ± 9.26 | 0.24 | NS |
| ADHD-RS | 16.78 ± 12.69 | 11.80 ± 10.40 | 0.43 | p < 0.05 |
| ODBI | 17.68 ± 13.52 | 19.00 ± 14.06 | 0.10 | NS |
| DSRS | 15.74 ± 8.37 | 16.52 ± 8.00 | 0.10 | NS |
| SCAS | 35.38 ± 23.39 | 34.02 ± 21.00 | 0.06 | NS |
Score ranges: Age, 12-15 years old. TABS (Tokyo Autistic Behavior Scale): 0-78 points. ADHD-RS (ADHD-Rating Scale): 0-54 points. ODBI (Oppositional Defiant Behavior Inventory): 0-54 points. DSRS (Depression Self-Rating Scale for Children): 0-36 points. SCAS (Spence Children's Anxiety Scale): 0-114 points.
In elementary school students, scores "during school" of QCD indicating functioning or disabilities during school hours were 3.31 ± 2.52 and 4.52 ± 2.33 in case group and control group, respectively (p < 0.05) (Table 3).
Table 3. The QCD scores of elementary school students.
| QCD | Case, % (n = 42) | Control, % (n = 42) | Effect Size | p value |
|---|---|---|---|---|
| Total | 24.26 ± 11.83 | 28.69 ± 8.69 | 0.43 | NS |
| Morning | 6.00 ± 3.12 | 6.62 ± 3.12 | 0.20 | NS |
| During school | 3.31 ± 2.52 | 4.52 ± 2.33 | 0.50 | p < 0.05 |
| After school | 3.55 ± 2.41 | 4.57 ± 2.50 | 0.42 | NS |
| Evening | 5.50 ± 3.48 | 6.00 ± 2.59 | 0.16 | NS |
| Night | 2.62 ± 2.67 | 2.83 ± 2.33 | 0.08 | NS |
| Overall behavior | 3.29 ± 1.99 | 4.14 ± 1.42 | 0.49 | NS |
Score ranges: QCD (Questionnaire: Children with Difficulties): 0-60 points.
In junior high school students, there were no significant differences in the QCD scores between the two groups in either the main category or the subcategories (Table 4).
Table 4. The QCD scores of junior high school students.
| QCD | Case, % (n = 50) | Control, % (n = 50) | Effect Size | p value |
|---|---|---|---|---|
| Total | 26.82 ± 12.11 | 24.96 ± 12.29 | 0.15 | NS |
| Morning | 6.06 ± 3.37 | 5.40 ± 3.52 | 0.19 | NS |
| During school | 3.92 ± 2.63 | 4.00 ± 2.56 | 0.03 | NS |
| After school | 4.08 ± 2.58 | 3.88 ± 2.54 | 0.08 | NS |
| Evening | 5.14 ± 3.01 | 4.48 ± 3.32 | 0.21 | NS |
| Night | 4.28 ± 2.62 | 3.74 ± 2.61 | 0.21 | NS |
| Overall behavior | 3.44 ± 1.84 | 3.46 ± 1.98 | 0.01 | NS |
Score ranges: QCD (Questionnaire: Children with Difficulties): 0-60 points.
Discussion
This is the first study to evaluate the daily life functioning or disabilities of child and adolescent psychiatric patients along the course of a day in the period of temporary school closure during COVID-19. No articles were found in the PubMed title search that contain all the words "closure", "patient", and "COVID".
In elementary school students, the subcategory score "during school" of QCD was significantly lower in case group than in control group. "During school" included the following questions: "Does your child like going to school"? "Can your child behave in class as other children do"? and "Does your child have friends who accept him/her at school"? A score of 0 means "completely disagree", and a score of 3 means "completely agree". Parents might have given low scores because schools did not function during the temporary closure. The closure of schools due to the pandemic might worsen difficulties among elementary school patients. 41.0% of elementary school students and 84.3% of junior high school students used the Internet on their own smartphones, with the usage rate increasing with age (32). Therefore, parents of children attending junior high school might have given the same score as in normal times because their children were connected with their friends online. Parents of school-refusing adolescents had lower levels of parental self-efficacy than parents of school-attending adolescents (33). As another reason why parents gave low evaluation, it could be a burden for parents have their children stay at home even if it is for the temporary closure. Patients were affected by temporary school closure and out of shape during "during school".
In junior high school students, there were no significant differences in the QCD scores between the two groups. The total score of ADHD-RS was significantly higher in case group than in control group. As a previous study had suggested that ADHD symptoms were positively associated with perceived stress (34), patients in the age group of junior high school might have been frustrated by the temporary school closure as it prevented them from socializing with their peers. No diagnosis has been made as this is the initial consultation, but it might be that many children are diagnosed with ADHD. This result might suggest that hyperactivity and impulsivity are increasing but not affecting daily life functioning. In a previous study using QCD, 298 children with ADHD faced greater difficulties, particularly in the evening compared with the community controls (35). Furthermore, these difficulties were related to the severity of ADHD symptoms (35). Due to the small sample size, no statistically significant differences were found, but parents may have difficulties in the evening.
The present study has some limitations to consider. First, measurement bias might have existed. Data were registered after the initial consultation. Additional information might have been obtained after further examinations. Second, a selection bias may exist because of several reasons. There were only 92 participants who belonged to case group. Due to the small sample size, the results might be subject to random errors. Further, the small sample size might have contributed to no significant differences in the proportion. The study did not represent the overall situation associated with child and adolescent psychiatric patients throughout the temporary school closure during COVID-19 because it was conducted in a single district. Finally, the results of this study confirmed the association between the child and adolescent psychiatric patients and the daily life functioning or disabilities throughout the temporary school closure during COVID-19, but not the causality. An investigation of the effects of each of the two factors, i.e., temporary school closure and COVID-19 pandemic, on daily life functioning or disabilities is a future challenge.
Conclusion
This study evaluated the clinical characteristics of the child and adolescent psychiatric patients throughout the temporary school closure during COVID-19. In line with the retrospective case-control design, the participants were allocated to one of the following two groups: those who visited the hospital during temporary school closure (case group) and randomly sampled sex-and age-matched patients (control group). Psychiatric outpatients of elementary school showed difficulties during school time due to temporary school closure throughout the COVID-19 pandemic. In psychiatric outpatients of junior high school, the total score of ADHD-RS was significantly higher in the case group than in the control group. Further investigations are warranted to study the impact of long-term stress experienced by child and adolescent psychiatric patients due to the school closure.
Funding: This work was supported in part by Grants-in- Aid for Research from the National Center for Global Health and Medicine (20A3001). The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors have no conflicts of interest to disclose.
References
- 1. World Health Organization. Director-General's remarks at the media briefing on 2019-nCoV on 11 February 2020. http://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 (accessed January 9, 2022).
- 2. United Nations Educational, Scientific and Cultural Organization. Education: From disruption to recovery, COVID-19 Impact on Education, Visualize evolution over time. https://en.unesco.org/covid19/educationresponse (accessed January 9, 2022).
- 3. Burns BJ, Costello EJ, Angold A, Tweed D, Stangl D, Farmer EM, Erkanli A. Children's mental health service use across service sectors. Health Aff (Millwood). 1995; 14:147-159. [DOI] [PubMed] [Google Scholar]
- 4. Donohue JM, Miller E. COVID-19 and school closures. JAMA. 2020; 324:845-847. [DOI] [PubMed] [Google Scholar]
- 5. Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. 2020; 4:421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Xiang Y, Jin Y, Cheung T. Joint international collaboration to combat mental health challenges during the coronavirus disease 2019 pandemic. JAMA Psychiatry. 2020; 77:989-990. [DOI] [PubMed] [Google Scholar]
- 7. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus Disease 2019. JAMA Netw Open. 2020; 3:e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Holmes EA, O'Connor RC, Pe r r y VH, e t a l. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020; 7:547-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Xie X, Xue Q, Zhou Y, Zhu K, Liu Q, Zhang J, Song R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020; 174:898-900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tang W, Hu T, Hu B, Jin C, Wang G, Xie C, Chen S, Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J Affect Disord. 2020; 274:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kelly BD. Coronavirus disease: challenges for psychiatry. Br J Psychiatry. 2020; 217:352-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wiguna T, Anindyajati G, Kaligis F, Ismail RI, Minayati K, Hanafi E, Murtani BJ, Wigantara NA, Putra AA, Pradana K. Brief research report on adolescent mental well-being and school closures during the COVID-19 pandemic in Indonesia. Front Psychiatry. 2020; 11:598756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Liu Q, Zhou Y, Xie X, Xue Q, Zhu K, Wan Z, Wu H, Zhang J, Song R. The prevalence of behavioral problems among school-aged children in home quarantine during the COVID-19 pandemic in china. J Affect Disord. 2021; 279:412-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zhu S, Zhuang Y, Lee P, Li JC, Wong PWC. Leisure and problem gaming behaviors among children and adolescents during school closures caused by COVID-19 in Hong Kong: quantitative cross-sectional survey study. JMIR Serious Games. 2021; 9:e26808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tang S, Xiang M, Cheung T, Xiang Y. Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent-child discussion. J Affect Disord. 2021; 279:353-360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McKune SL, Acosta D, Diaz N, Brittain K, Beaulieu DJ, Maurelli AT, Nelson EJ. Psychosocial health of school-aged children during the initial COVID-19 safer-at-home school mandates in Florida: a cross-sectional study. BMC Public Health. 2021; 21:603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Saito M, Kikuchi Y, Lefor AK, Hoshina M. Mental health in Japanese children during school closures due to the COVID-19. Pediatr Int. 2022; 64:e14718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hellström L. A systematic review of polyvictimization among children with attention deficit hyperactivity or autism spectrum disorder. Int J Environ Res Public Health. 2019; 16:2280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sterzing PR, Shattuck PT, Narendorf SC, Wagner M, Cooper BP. Bullying involvement and autism spectrum disorders: prevalence and correlates of bullying involvement among adolescents with an autism spectrum disorder. Arch Pediatr Adolesc Med. 2012; 166:1058-1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Goto T, Yamashita Y, Usami M, Takahashi M, Saito K. A tool for the assessment of daily life functioning of children "Questionnaire-children with Difficulties (QCD)". Japanese Journal of Pediatrics. 2011; 64:99-106. (in Japanese) [Google Scholar]
- 21. Kurita H, Miyake Y. The reliability and validity of the Tokyo Autistic Behaviour Scale. Jpn J Psychiatry Neurol. 1990; 44:25-32. [DOI] [PubMed] [Google Scholar]
- 22. DuPaul GJ, Power TJ, Anastopoulos AD, Reid R. ADHD rating Scale-IV: Checklists, norms, and clinical interpretation. The Guilford Press. 1998. [Google Scholar]
- 23. Burns GL, Desmul C, Walsh JA, S i l p a k i t C, Ussahawanitchakit P. A multitrait (ADHD-IN, ADHD-HI, ODD toward adults, academic and social competence) by multisource (mothers and fathers) evaluation of the invariance and convergent/discriminant validity of the Child and Adolescent Disruptive Behavior Inventory with Thai adolescents. Psychol Assess. 2009; 21:635-641. [DOI] [PubMed] [Google Scholar]
- 24. Birleson P. The validity of depressive disorder in childhood and the development of a self-rating scale: a research report. J Child Psychol Psychiatry. 1981; 22:73-88. [DOI] [PubMed] [Google Scholar]
- 25. Spence SH. A measure of anxiety symptoms among children. Behav Res Ther. 1998; 36:545-566. [DOI] [PubMed] [Google Scholar]
- 26. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychological Association; 2013. [Google Scholar]
- 27. Usami M, Sasayama D, Sugiyama N, Hosogane N, Kim S, Yamashita Y, Kodaira M, Watanabe K, Iwadare Y, Sawa T, Saito K. The reliability and validity of the Questionnaire ‒ Children with Difficulties (QCD). Child Adolesc Psychiatry Ment Health. 2013; 7:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Takayanagi N, Yoshida S, Yasuda S, Adachi M, Kaneda- Osato A, Tanaka M, Masuda T, Kuribayashi M, Saito M, Nakamura K. Psychometric properties of the Japanese ADHD-RS in preschool children. Res Dev Disabil. 2016; 55:268-278. [DOI] [PubMed] [Google Scholar]
- 29. Denda K, Kako Y, Kitagawa N, Koyama T. Assessment of depressive symptoms in Japanese school children and adolescents using the Birleson Depression Self-Rating Scale. Int J Psychiatry Med. 2006; 36:231-241. [DOI] [PubMed] [Google Scholar]
- 30. Ishikawa S, Sato H, Sasagawa S. Anxiety disorder symptoms in Japanese children and adolescents. J Anxiety Disord. 2009; 23:104-111. [DOI] [PubMed] [Google Scholar]
- 31. Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant. 2013; 48:452-458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cabinet Office, Government of Japan. Survey Survey on the Internet Usage Environment for Youth, Part 2: Results of the Survey, Chapter 1 Results of the Survey on Youth, Section 1: Usage of Internet Connection Devices. https://www8.cao.go.jp/youth/youth-harm/chousa/r02/net-jittai/pdf-index.html (accessed January 9, 2022). (in Japanese) .
- 33. Carless B, Melvin GA, Tonge BJ, Newman LK. The role of parental self-efficacy in adolescent school-refusal. J Fam Psychol. 2015; 29:162-170. [DOI] [PubMed] [Google Scholar]
- 34. Combs MA, Canu WH, Broman-Fulks JJ, Rocheleau CA, Nieman DC. Perceived stress and ADHD symptoms in adults. J Atten Disord. 2015; 19:425-434. [DOI] [PubMed] [Google Scholar]
- 35. Usami M, Okada T, Sasayama D, Iwadare Y, Watanabe K, Ushijima H, Kodaira M, Sugiyama N, Iwadare Y, Sawa T, Saito K. What time periods of the day are concerning for parents of children with attention deficit hyperactivity disorder? PLoS One. 2013; 8:e79806. [DOI] [PMC free article] [PubMed] [Google Scholar]


