Abstract
Angiographically, a “dual LAD” is described as two distinct arteries supplying the vascular territory of the LAD in parts, identified as the short LAD/LAD1 and the long LAD/LAD2. Using an easy-to-understand three-step approach, Jariwala et al unveiled a novel classification strategy for dual LAD systems in an attempt to decrease ambiguity in diagnosis and management of the anomaly. As part of our research, we looked at a wide range of published cases and case series in the literature, and also those reported from our hospital. In our novel classification system, we divide dual LADs into three main groups based on their origin and vascular territory, each of which is further divided into subgroups based on the course of LAD1/LAD2 and the variable feature that is a distinguishing attribute of the type of anomaly to be specified.
A review of 144 publications in the world literature revealed 340 patients eligible for the study. The median age was 58.8 years (SD - 11.42; range - 29–89) with male predominance (3.3:1). Cases in Group I comprised 60.6% of the total cases, followed by Group II (36.2%), and Group III (3.2%). Subgroup I-A was the most common in terms of dual LAD, followed by subgroup II-A. Acute coronary syndrome (45.5%) and chronic coronary syndrome (55.8%) were the most common clinical presentations in patients with significant coronary artery disease (30.8%).
Keywords: Coronary angiography, Computed tomography angiography, Coronary artery disease, Coronary vessel anomalies, Double left anterior descending artery
Abbreviations: LAD, Left anterior descending artery; LMCA, Left main coronary artery; MDCT, Multidetector computed tomography; STEMI, ST-segment elevation myocardial infarction; NSTEMI, non-ST-segment elevation myocardial infarction; PTCA, Percutaneous transluminal coronary angioplasty; CABG, Coronay artery bypass surgery; CAD, Coronary artery disease; LCX, Left circumflex artery; RCA, Right coronary artery; RCS, Right coronary sinus
1. Introduction
Although the angiographic findings of the dual LAD system is considered as a typical variant of LAD, it should be labelled as a coronary anomaly when component/s of the dual LAD originate and/or courses anomalously.1 In order to prevent misunderstanding of coronary angiography, cardiac physicians and diagnosticians need to be aware of this significant coronary abnormality.2 From a therapeutic standpoint, categorising the dual LAD system is critical in order to better understand their pathophysiology and to imply optimal revascularization.3
To classify dual LAD, the previous overlapping numbering system of classification was replaced with a systematic novel classification using innovative nomenclature.4 For dual LAD systems, our classification not only has a simplistic approach to use but also has therapeutic implications.
Reclassification of all cases and case series of dual LAD described in the literature as well as our institutional cases was done based on a novel technique. This was dividing dual LAD into three distinct groups and subgroups as acknowledged by the “Indian Association of Cardiovascular-Thoracic Surgeons”.1
2. Material and methods
The cases reported in the literature between 1939 till the time of writing of this manuscript with dual LAD were included. The databases like MEDLINE, PubMed, EMBASE, Science Direct, Scopus, Google Scholar, Cochrane Library, and Crossref were used to identify the cases that had been published. The following search terms or keywords were used to search electronic databases: “Dual LAD;” “Duplication of LAD;” “Double LAD;” “Split LAD;” “Dual anterior interventricular artery;” “Dual origin of the left anterior descending artery from the left and right coronary arteries.” Reference lists of all identified journal articles have also been reviewed. To increase the sensitivity of the search results, the search strategy was customized to each database and no lower date or language restrictions were applied. ‘Google translate has been used to translate non-English articles.
We identified 161 articles related to dual LAD in the literature. We reviewed the case records of patients with dual LAD who were diagnosed at our centre from May 2018 to May 2021. Ethics permission and authorization was granted by the Ethics Committee of our Hospitals for a retrospective review of patient data. The authors independently reviewed all the collected journal articles about dual LAD. After fulfilling the inclusion/exclusion criteria for the diagnosis of dual LAD as indicated below, eligible patients were added based on angiographic data or autopsy findings.
2.1. Inclusion criteria
-
(I)
Age ≥19 years,
-
(II)
Description matching morphological features of ‘Dual LAD’,
-
(III)
Presence of other coronary anomalies,
2.2. Exclusion criteria
-
1.
Associated with congenital heart diseases.
-
2.
Publications without complete clinical descriptions and angiographical information were omitted.
Four more articles that described the association of dual LAD with corrected transposition of great arteries [C-TGA] and anomalous origin of LAD from pulmonary artery [ALCAPA] were also excluded.5, 6, 7, 8 Two titles without abstracts were excluded. 11 publications such as a letter to the editor, review articles, duplicates were also omitted (Fig. 1).
Fig. 1.
Procedure of screening of eligible publication based on inclusion and exclusion criteria. Our analysis comprised 144 out of 161 publications related to the dual LAD and the final assessment contained 340 patients which were reclassified using the novel classification. LAD = left anterior descending artery [Reproduced with permission].
The following data was extracted from eligible cases and recorded on a standard data extraction form: Authors, year of publication, age of patient/s, gender, clinical presentation, conventional angiography and/or MDCT coronary angiography findings, observations from autopsy studies of coronary anatomy, their numerical older classifications, final diagnosis and therapeutic strategies used. We also retrieved detailed angiographic or autopsy findings, such as the origin, course, and pattern of distribution of dual LAD, LAD1, and LAD2. In accordance with the novel classification of dual LAD,1 all of the recovered cases were reclassified, as detailed in the following section (Fig. 2):
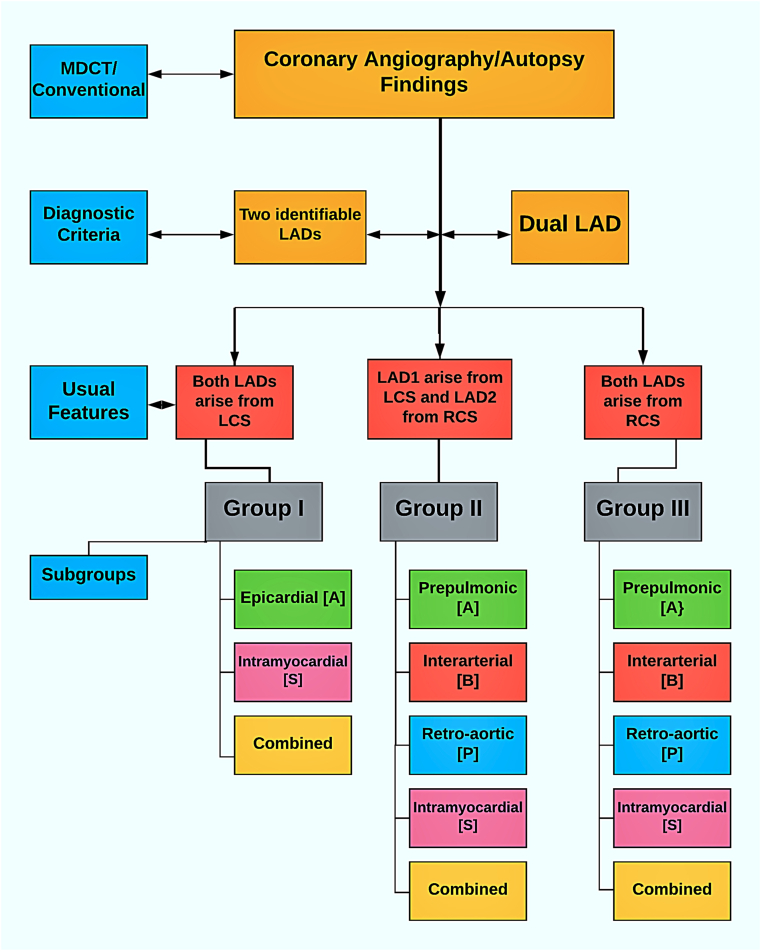
Fig. 2.
Flow diagram showing scheme of novel classification of dual LAD. The diagnosis of dual LAD is based on angiographic or autopsy findings of 2 arteries which supply the same vascular territory. Based on the origins of the LAD1 and LAD2 either completely from the LCS, LCS, and RCS, or exclusively from the RCS, dual LAD is categorized into one of the three groups. It is further sub-grouped based upon their four courses: Epicardial or Prepulmonic or Anterior (A); Inter-arterial or Between (B); Retro-aortic or Posterior (P); Intra-myocardial or Septal (S). LAD = left anterior descending artery; LCS = Left coronary sinus; RCS = Right coronary sinus [Reproduced with permission].
2.3. Method of novel classification of dual LAD
After the diagnosis is confirmed, one of the three groups is allocated to dual LAD: those which originate entirely from the left coronary sinus (Group I), those which originate partially from both the left and right coronary sinuses (Group II), and those which originate entirely from the right coronary sinus (Group III).
Dual LAD should be subclassified into one of four subgroups based on the course of the LAD2: anterior or epicardial (A), interarterial (B), septal or intramyocardial (S), and posterior or retro-aortic (P).
The course of either the LMCA [in group-III] or both LADs may be the same and is designated using a single subgroup alphabet, for example, Group I-A, Group II-A, and Group III-A.
If there is a separate course of both LADs, then use two subgroup alphabets to mark them together. The first alphabet refers to the path of LAD1 while the second alphabet refers to that of LAD2, for example, Group I-AS, Group II-AB, Group III-PA.
Variable feature of the dual LAD (type of anomaly) to be described after assigning to one of three groups (Fig. 3) and corresponding subgroup, for example, Group I – A: Separate origin of LAD1 and LAD2 from the LMCA and absence of the common LAD; Group II – B: Interarterial course of LAD2; Group III – PA: Retro aortic course of LAD1 and prepulmonic course of LAD2.
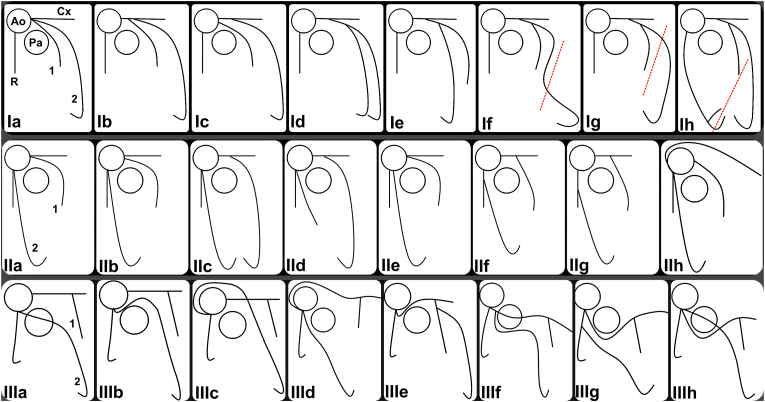
Fig. 3.
Schematic representation of various variable features (type of anomalies) incorporated under three groups of novel classification. Upper Panel (Group I): the absence of LMCA and common LAD and separate origin of LAD1 and LAD2 form LCS (Ia), the early origin of LAD1 from the LMCA which bifurcates into LAD2 and LCX (Ib), the separate origin of LAD1 from LCS (Ic), equal lengths of LAD1 and LAD2 (Id), reverse lengths of LAD1 and LAD2 (Ie), epicardial right ventricular course of LAD2 (If), epicardial left ventricular course of LAD2 (Ig), triple LAD anomaly wherein the inferior ventricular artery enters AIVS (Ih). Middle Panel (Group II): the absence of LMCA (IIa), the separate origin of LAD1 and LCX (IIb), equal lengths of LAD1 and LAD2 (IIC), reverse lengths of LAD1 and LAD2 (IId), the separate origin of RCA and LAD2 from RCS (IIe), the origin of LAD2 from the proximal segment of the RCA (IIf) and the mid-segment of the RCA (IIg), anomalous origin of the LCX from the RCS/RCS (IIh). Lower Panel (Group II/III): Epicardial Course of LAD1 and intramyocardial Course of LAD2 (IIIa); Epicardial Course of LAD1 and Interarterial course of LAD2 (IIIb); Epicardial Course of LAD1 and Retro aortic course of LAD2 (IIIc); Common origin of LAD2 and LMCA from the RCS wherein LMCA divides into LAD1 and LCX which takes retro aortic course while LAD2 continues epicardially (IIId); LMCA originated from the RCS, had interarterial course, which divided into LCX and LAD, and LAD divided into LAD1 in AIVS and LAD2 which ran epicardially on LV surface (IIIe); LMCA had a transseptal course before bifurcating into a LAD1, and LCX. The LAD2 had a prepulmonic course before entering the distal AIVS (IIIf); LAD1 and LCX were arising from the LMCA which originated from the RCS, Meanwhile, LAD2 was seen arising from the proximal RCA. Both vessels had epicardial course (IIIg); Single coronary artery in the RCS trifurcated into pre-pulmonic, short LMCA dividing into LAD1, LCX and a separate origin of a transseptal, LAD2 (IIIh). LAD = left anterior descending artery; LMCA = left main coronary artery; LCX = left circumflex artery; RCS = right coronary sinus; RCA = right coronary artery; AIVS = anterior interventricular sulcus [modified and reproduced with permission].
The IBM SPSS 16.0 software system (SPSS, Chicago, IL, USA) was used to conduct statistical analysis. Descriptive statistics were used to interpret the results, including means, median, mode, ranges, standard deviations, and percentages.
3. Results
We studied 340 adult patients with dual LAD in this case series, 6 of whom registered from our hospital (of which three illustrated cases shown in Fig. 4; Fig. 1), and 334 cases were recorded in 144 publications including 4 autopsy and 11 radiological studies (see the Supplementary Material – list of cases published in the literature). A total of 6 large case series comprising more than 10 patients accounted for 181 dual LAD cases, of which the largest series was by Bozler et al. which included 56 cases,2 followed by Bae et al who reported 45 cases.18 Recently, Mehmet Seker, Sidhu, and Wander published data of 25 and 22 cases, respectively.19,20 The original description and classification by Spindola-Franco et al was based upon 23 cases.19 The autopsy case series by Nikolic et al. described 10 cases of Group I-AS [Intra-myocardial course].21 Small case series included 2 case reports having a cluster of 3 and 4 cases each9, 10, 11, 12 while 5 case reports constituted 2 cases each,13, 14, 15, 16, 17 the remaining 129 were single patient case reports.
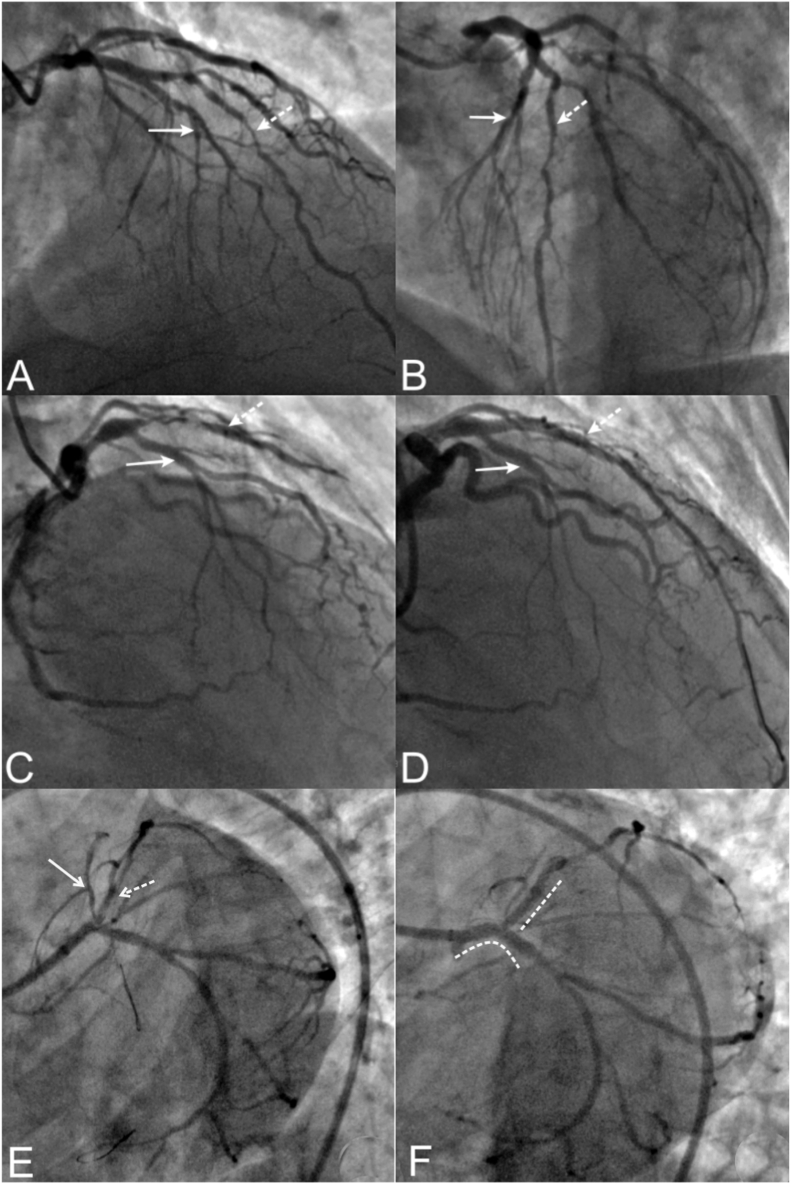
Fig. 4.
Coronary angiography of three illustrated cases form our institute demonstrating group I-A dual LAD. Case 1 (Panels A, B): Right anterior and left anterior oblique views revealed the Left main coronary artery bifurcated into the left anterior descending artery (LAD) and left circumflex artery (LCX). The LAD proper is divided into the LAD1 and LAD2. The LAD2 and LCX had significant atherosclerotic stenoses. The 1st diagonal branch also a significant lesion of its ostio-proximal segment which arose from the LAD1. LAD2 also gave rise to retrograde collateral (Rentrop grade 3) to the critically stenosed right coronary artery territory [Not shown]. The patient underwent coronary artery bypass surgery due to symptoms of effort angina and underlying triple vessel disease. Case 2 (Panels C, D): Right anterior oblique views demonstrated critical stenosis of the proximal segment of the LAD2 with thrombolysis in myocardial infarction (TIMI) II flow. LAD1 and other arteries were normal. Percutaneous coronary intervention with a drug-eluting stent could restore TIMI III flow and alleviate his symptom of exertion-induced angina. Case 3 (Panels E, F): Left anterior caudal view demonstrated separate origin of the LAD1 and LAD2 from the LMCA. The LAD1 was misinterpreted for the proper LAD and LAD2 was misinterpreted as a ramus intermidius branch. There was a significant stenoses of the ostio-proximal segments of LAD1, LAD2 and LCx. Patient underwent percutaneous coronary intervention of the LMCA using two stent strategy.
The demographic information, clinical presentations and therapeutic strategies are presented in Table 1. The overall mean age at initial diagnosis of dual LAD was 58.8 years [Median 59.3 years; Mode 60 years; Standard deviation 11.4; Range 29–89 years], compared to 57.9 years for single case reports, whereas it was 45.13 years for case series. Gender-related information has been extracted from 85.5% of cases. There was male predominance [77%], with a male: female ratio of 3.3:1.
Table 1.
Demographics, clinical presentations and therapeutic strategies of patients with dual LAD [n = 340].
| Variable | Average [Years] | Standard Deviation [Range] |
|---|---|---|
| Age | ||
| Overall | 58.80 | 11.4 [29–89] |
| Case series | 45.13 | 7.67 [22–56] |
| Case reports | 57.90 | 11.5 [29–89] |
| Numbers | Percentage | |
| Gender | 291 | 85.5 |
| Male | 224 | 77.0 |
| Female | 67 | 23.0 |
| Clinical Presentation | 175 | 52.1 |
| Stable angina | 54 | 30.8 |
| Unstable angina | 43 | 24.7 |
| STEMI | 29 | 16.6 |
| NSTEMI | 7 | 4.0 |
| Atypical chest pain | 16 | 9.1 |
| Heart failure | 10 | 5.7 |
| Miscellaneous | 16 | 9.1 |
| Coronary artery Disease | 276 | 81.2 |
| Present | 154 | 55.8 |
| Absent | 122 | 44.2 |
| Therapeutic Decision | 242 | 71.2 |
| Medical Management | 143 | 59.1 |
| PTCA | 57 | 23.6 |
| CABG | 42 | 17.3 |
Abbreviations: STEMI = ST-segment myocardial infarction, NSTEMI = non-ST-segment elevation myocardial infarction; PTCA = Percutaneous transluminal coronary angioplasty; CABG = Coronary artery bypass surgery.
All the documented cases have been categorized as per our novel classification as shown in Table 2 (Fig. 5). Group I [n = 206; 60.6%] was the largest, followed by Group II [n = 123; 36.2%] and Group III cases [n = 11; 3.2%] were lowest in numbers. Further detailed sub-analysis showed that group I-A [n = 181; 53.2%] was a common presentation of dual LAD followed by group II-A [n = 99; 29.1%]. Group I-AS [n = 25; 7.35%] has been significantly greater than II-AB [n = 13; 3.8%] and II-AS [n = 9; 2.6%] while only two cases (0.6%) of II-AP have been reported. In Group III, aberrant morphological patterns of III-PA dual LAD were most often detected in four cases (1.2%), followed by three cases of III-AB (0.9%). Two cases of group III-SA cases accounted for 0.6% of all cases, whereas isolated cases of groups III-A and III-AS accounted for 0.3% each.
Table 2.
Frequency and distribution of groups and subgroups, variable features (type of anomaly) of dual LAD as per novel classification. Abbreviations: LAD = Left anterior descending artery; LMCA = Left main coronary artery; LCX = Left circumflex artery; RCS = Right coronary sinus; RCA = Right coronary artery; AIVS = Anterior interventricular sulcus; LV = Left ventricle; UC = Unclassified.
| Novel Classification |
Source |
Pictorial Depiction |
Older Classification |
N |
% |
||
|---|---|---|---|---|---|---|---|
| Groups (N,%) | Subgroups | Variable Features (Type of anomaly) | |||||
| Group I (N = 206; 60.6%) |
I-A | Absence of LMCA/common LAD and separate origin of LAD1 and LAD2 form LMCA/LCS. | Soman23; Jariwala et al1 | Fig. 3; Panel Ia | I | 181 | 53.2 |
| Early origin of LAD1 from the LMCA which bifurcates into LAD2 and LCX. | Dhanse et al24; Subban et al25 | Fig. 3; Panel Ib | VII | ||||
| Separate origin of LAD1 from LCS. | Şeker M20; Shizukuda Y et al26 | Fig. 3; Panel Ic | UC | ||||
| Equal/reverse lengths of LAD1 and LAD2. | Sayin MR et al16 | Fig. 3; Panel Id/Ie | UC, XIII | ||||
| Epicardial right ventricular course of LAD2. | Spindola-Franco et al4; Bozlar et al2 | Fig. 3; Panel If | II | ||||
| Epicardial left ventricular course of LAD2. | Spindola-Franco et al4; Bozlar et al2; | Fig. 3; Panel Ig | I | ||||
| Triple LAD anomaly wherein the inferior ventricular artery enters the distal AIVS. | Bozlar et al2; Jariwala et al22 | Fig. 3; Panel Ih | IX | ||||
| I-AS | Epicardial course of LAD1 and intramyocardial course of LAD2 | Spindola-Franco et al4; Bozlar et al2 | Fig. 4 | III | 25 | 7.35 | |
|
Group II (N = 123; 36.2%) |
II-A | Presence of LMCA and origin of LAD2 from common ostium on the RCS. | Moulton et al26 |
Fig. 3; Panel IIa |
V variant | 99 | 29.1 |
| Absence of LMCA and separate origin of LAD1 and LCX and separate origin of LAD2 from RCS. | Manchanda et al28 | Fig. 3; Panel IIb | V | ||||
| Equal lengths of LAD1 and LAD2 | El Tallawi et al29 |
Fig. 3; Panel IIc |
UC | ||||
| Reverse lengths of LAD1 and LAD2 | Cho et al30 |
Fig. 3; Panel IId |
IV variant | ||||
| Separate origin of RCA and LAD2 from RCS | Manchanda et al28; Deora et al31; Prasad A et al32; Celik et al33 | Fig. 3; Panel IIe | V, VI, VIa, X | ||||
| Origin of LAD2 from the proximal segment of the RCA | Spindola-Franco et al4;Maroney et al34 |
Fig. 3; Panel IIf |
IV, VI | ||||
| Origin of LAD2 from the mid-segment of the RCA | Bozlar et al2 |
Fig. 3; Panel IIg |
VIII | ||||
| Anomalous origin of the LCX from the RCS/RCS | Bali et al23; Bittner et al14; Chang et al24; Daralammouri et al25; Turkoglu et al26 |
Fig. 3; Panel IIh |
IV | ||||
| II-AB | Epicardial Course of LAD1 and Interarterial course of LAD2 | Deora et al35 | Fig. 3; Panel IIIb | VI, VIa | 13 | 3.8 | |
| II-AS | Epicardial Course of LAD1 and Intramyocardial Course of LAD2 | Manchanda et al28 | Fig. 4; Panel IIIa | V, VII | 9 | 2.6 | |
| II-AP | Epicardial Course of LAD1 and Retro aortic course of LAD2 | Yokokawa et al39;Panduranga et al40 | Fig. 3; Panel IIIc | V | 2 | 0.6 | |
|
Group III (N = 11; 3.2%) |
III-PA | Common origin of LAD2 and LMCA from the RCS wherein LMCA divides into LAD1 and LCX which takes retro aortic course while LAD2 continues epicardially. | Barbaryan et al41; Lee et al42; Vora43; Bozlar et al2 | Fig. 3; Panel IIId | VIII | 4 | 1.2 |
| III-AB | LMCA originated from the RCS, had interarterial course, which divided into LCX and LAD, and LAD divided into LAD1 in AIVS and LAD2 which ran epicardially on LV surface. | Agarwal et al13; Tuncer et al44; Bozlar et al2 | Fig. 3; Panel IIIe | V, VI | 3 | 0.9 | |
| III-SA | LMCA had a transseptal course before bifurcating into a LAD1, and LCX. The LAD2 had a prepulmonic course before entering the distal AIS. | Al-Umairi et al45; Pandey et al46 | Fig. 3; Panel IIIf | XII | 2 | 0.6 | |
| III-A | LAD1 and LCX were arising from the LMCA which originated from the RCS, Meanwhile, LAD2 was seen arising from the proximal RCA. Both vessels had epicardial course | Cingoz et al47 | Fig. 3; Panel IIIg | UC | 1 | 0.3 | |
| III -AS | Single coronary artery in the RCS trifurcated into pre-pulmonic, short LMCA dividing into LAD1, LCX and a separate origin of a transseptal, LAD2. | Desimone et al48 | Fig. 3; Panel IIIh | XI | 1 | 0.3 | |
Fig. 5.
Graphical representation of the frequency of three groups and their subgroups of dual LAD as per novel classification. Group I – A dual LAD has been more frequent followed by Group II-A. Other subgroups have been less common and were documented sporadically. LAD = Left anterior descending artery.
Data on the severity of CAD were recorded in 81.2% [n = 276] of the cases from the coronary angiography descriptions in the publications. In 55.8% [n = 154] of cases, the associated significant coronary artery disease was reported. We had relevant data on clinical manifestations of patients with underlying dual LAD anomalies for only 52.1% [n = 175] of cases. The most common clinical presentation was acute coronary syndrome in 45.5% of cases, with unstable angina being the most common clinical presentation in 24.7% [n = 43], followed by STEMI in 16.6% [n = 29], while NSTEMI in 4.0% [n = 7]. The chronic coronary syndrome (stable angina) was the second most common clinical presentation in 30.8% [n = 54] of patients, while 9.1% [n = 16] experienced atypical chest discomfort. In 5.7% [n = 10] of cases, heart failure was the initial presentation. A miscellaneous group that was asymptomatic with a positive stress test, evaluations for cardiac, non-cardiac surgery, or arrhythmias comprised of 9.1% [n = 16] of the cases.
Information on the recommended or successfully completed therapeutic strategies has been obtained from 71.2% [n = 242] of the cases. Medical management was advocated in the majority of cases [n = 143; 59.1%]. The revascularization was done in 40.9% of cases in which PTCA [n = 57; 23.6%] outnumbered CABG [n = 42; 17.3%].
Additional coronary anomalies have been reported in 6.2% [n = 21] of the total cases. Anomalous origin of LCX for the RCS/RCA was most common in 12 cases 14,23, 24, 25, 26, while 2 cases had an aberrant origin/continuation as an obtuse marginal branch of LAD1. There were 5 cases of inter-coronary communication/anastomosis14,27 and 2 cases of associated hyperdominant LAD.1
4. Discussion
Approximately 80% of the dual LAD anomalies are asymptomatic, with just 20% causing symptoms.27,28 Angiographically, a small or hypoplastic LAD (Type I) that does not reach the cardiac apex, has three distinct anatomical variations that must be considered:
-
1.
A long-dominant posterior descending branch of the right coronary artery may be present, feeding the apex and ending beyond the apex in the AIVS, designated as ‘super dominant RCA’.22
-
2.
A long parallel diagonal branch can occur, descending parallel to the LAD but not entering the AIVS, designated as ‘parallel LAD’.1
-
3.
A ‘dual LAD’ could be in existence and its awareness and recognition is important for several reasons as discussed below in Table 3 (Fig. 6).
Table 3.
Clinical and therapeutic implications of the dual LAD based on angiographic presentation.
| Sr. No. | Angiographic presentation (Conventional and/or MDCT) | Original Classification | Novel classification | Clinical/Therapeutic implications |
|---|---|---|---|---|
| General implications | ||||
| 1 | Intramyocardial course of LAD15 | III | Group I-AS Group II-AS Group III-AS |
If myocardial perfusion SPECT imaging demonstrates no evidence of ischemia, these cases should be managed medically. |
| 2 | Occlusion of LAD135 | All cases of Dual LADs | Group I Group II Group III |
Echocardiography: Correspond to isolated RWMA of the septal wall. |
| 3 | Occlusion of LAD235 | Echocardiography: Demonstrate the antero-apical RWMAs with a normal septal wall. | ||
| 4 | Premature termination of LAD with nonperfused mid and/or distal territory of LAD without the presence of the collateral circulation36 | IV | Group II | The existence of another component of the LAD should be explored. |
| 5 | LAD2 emerging from the RCS/RCA37 | IV | Group II | Misdiagnosed as a branch of the conus. The presence of septal and diagonal branches distinguishes it as LAD. |
| 6 | Prepulmonary course of LAD238 | IV, VIII, X, XI | Group II-A Group III-PA |
It is fallacious to believe that LAD2 originating from RCS with less tortuosity and fewer branches is more resistant to atherosclerosis. |
| Interventional Implications | ||||
| 1 | Occlusion of the common LAD prior the division to the LAD1 and LAD235 | I | Group I | The primary PCI of the LAD1 did not alleviate chest pain or ST-segment elevation. Repeat angiography showed the presence of an occluded LAD2, and repeat intervention restored flow into the LAD2 and improved symptoms and ECG. |
| 2 | Trifurcation lesion involving LAD1 & LAD2 and large parallel diagonal branch39 | I | Group I-A | Authors in this index case performed triple kissing balloon angioplasty. |
| 3 | CTO intervention of the LAD240 | I | Group I-A | Retrograde approach via septal perforators should not attempted. |
| 4 | Thrombotic occlusion of the common LAD41 | I | Group I-A | After re-establishing the flow, the lesion included the bifurcation of LAD1 and LAD2 of equal size, necessitating the culotte technique during primary PCI. |
| 5 | LAD1 misinterpreted as LAD occlusion in acute anterior wall myocardial infarction29,42 | IV | Group II | Especially, in the absence of a retrograde flow, one should look for a separate coronary artery flowing from the RCA – ‘Missing Artery’. |
| Surgical Implications | ||||
| 1 | Prepulmonic course of the LAD217 | IV, VIII, X, XI | Group II-A Group III-PA |
With volume overload (atrial septal abnormalities, tricuspid regurgitations, etc.) it is at risk of damage to the LAD2 during median sternotomy. |
| 2 | Intramyocardial course of the LAD1.43 |
III | Group I-AS | A challenging revascularization due to its higher position in the anterior interventricular groove makes it more difficult to graft. Knowledge about the dual LAD variant allows for more accurate placement of arteriotomies during revascularization. |
| 3 | Interarterial course of LAD2.38,44 | V, VI, VII | Group II-AB Group III-AB |
1. It is attributed to sudden cardiac death and, consequently, is an indication of surgical repair if myocardial ischemia or prior syncope is documented. 2. Important to be detected before these cardiac procedures since failure to do so can result in accidental surgical excision of the anomalous blood vessel during the procedure. |
| 4 | Significant stenoses of LAD1 and LAD2 (12,39,40). | All cases of Dual LADs | Group I Group II Group III |
The LAD1 provides the blood supply mainly to the septal wall, and the LAD2 largely provides the anterior left ventricular wall. Thus, surgical revascularization therapies, such as CABG, may require revascularization of both LADs |
| 5 | Abnormal origin of the LCX from RCS.47 | IV | Group II | It raises the risk of inadvertent vascular compression during surgery during mitral and aortic valve replacement. |
Abbreviations: CABG = Coronary atery bypass surgery; ECG = Electrocardiogram; LAD = left anterior descending artery; LMCA = left main coronary artery; LCX = left circumflex artery; PCI = Percutaneous coronary intervention; RCS = right coronary sinus; RCA = right coronary artery; RWMA = Regional wall motion abnormality; SPECT = Single photon emission computed tomography.
Fig. 6.
Schematic representation of therapeutic implications of dual LAD. There are therapeutic implications for general (inter-arterial course, myocardial bridging, misdiagnosis as a conus branch, differential regional wall motion abnormalities), interventional management (Percutaneous coronary transluminal angioplasty) for bifurcation lesion involving LAD1 and LAD2, and surgical management (Coronary artery bypass surgery) should aim for complete revascularization in case of significant coronary artery disease involving common LAD or LAD1 and LAD2) or presurgical identification of prepulmonary course of LAD2 to prevent inadvertent iatrogenic injury. LAD = Left anterior descending artery.
As observed by Spindola-Franco et al. (57 years) and Sidhu and Wander (56.77 years), the average age of our patients was 58.8 years and the average age of case reports was 57.8 years, which was in line with our findings. One reason for this might be because these studies were done on populations of patients with CAD, the most common reason for coronary angiography. In the case series, the average age was 45.13 years, with two radiological case series including much younger people. Most earlier case studies by Spindola-Franco et al.4 had a male to female ratio of 2.8:1, whereas Bozlar et al.2 reported a ratio of 2.23:1, indicating that men outweighed females like in our experience (3.3:1).
Among the 73.9% and 4.3% of the patients that Spindola-Franco et al. found to be Type I and Type II dual LAD cases, our new categorization of these cases placed them in Group I-A [78.2%].4 According to the earlier classification, Type III dual LAD was reclassified in our study to Group I-AS with a frequency of 7.3%. A total of 5% of patients had Group I-AS dual LADs detected by Bozlar et al., 4.6% by Sidhu and Wander and 13% by Spindola-Franco et al., whereas Nikolic et al. recorded exclusively 10 specific cases of intra-myocardial dual LADs.2,4,19,21
Group II accounted for 36.2% of all cases, with isolated instances documented in individual case reports accounting for the majority [n = 99; 80.5%]. Çanga et al. reported four Group II cases, whereas Tuncer et al. and Montero-Cabezas et al. documented three cases each, and the other five authors documented two cases each.2,4,9, 10, 11,14,15,20 The second-most common morphological type was Group II-A, which accounted for 36.2% of all cases and 81% of Group II cases. Bozler et al. detected just two instances of Group III dual LADs in their case series, with the rest being rare occurrences accounting for 3.2% of all cases reported as case reports of unique types of double LAD.2
Coronary artery anomalies seldom produce symptoms. It is difficult to identify whether an atherosclerotic CAD is present and whether this abnormality accelerates the atherosclerosis. Non-invasive studies of the affected artery and coronary angiography may provide divergent outcomes in patients with severe CAD and coronary artery anomalies.23 In a case series by Sidhu and Wander, the significant CAD was 68.1%19 while we found it to be 55.8% as we had a cluster of case series that had a younger and middle-aged group of patients. The therapeutic decisions were available in 71.2% of publications. The majority of patients [59.1%] underwent medical management while revascularization was advocated in 40.9% of cases in the form of PTCA [23.6%] and CABG [17.3%]. A unique case series described by Sajja et al shows four patients with dual LAD who underwent successful CABG.12
Though courses of anomalous coronary arteries are benign, the awareness of the inter-arterial route between the aortic root and the pulmonary artery is crucial. Its link to sudden death is due to myocardial ischemia caused by proximal intramural segment compression, which necessitates surgical intervention.45,10 Hence, MDCT is more 3D omniplanar than conventional coronary angiography in establishing the specific origin, course and even interconnections with other cardiac structures of aberrant coronary arteries. To make use of the novel classification, it is critical to analyse cardiac imaging with MDCT while establishing a reperfusion strategy for dual LAD. In our research, 61% of patients employed MDCT to validate dual LAD results. Nevertheless, the utilisation of MDCT in real-world practise is on the rise.25,26
5. Limitations of study
Clustering most dual LAD cases in the literature and elaborating on their demographics, clinical manifestation and implications on the management according to a novel classification suggested by us was the first step. The primary drawback of our research was its retrospective nature, with data collected focusing on previous case reports/series. Other drawbacks were a lack of a structured standard reporting system and that of complete data such as demographics, clinical presentation and therapeutic options. We included a broad range of publications, such as autopsy reports, with the primary purpose of categorizing them into a novel classification. We were unable to gather information on the prevalence of atherosclerosis in the various groups with dual LADs in order to compare them to the general population. We included articles that did not provide information on clinical presentation and treatment regimens since our main purpose was to reclassify previously reported patients with dual LAD. To look for further information, such as a proclivity for atherosclerosis in dual LAD and its therapeutic benefits, we require particular prospective trials that are randomised controlled studies compared to normal controls.
6. Conclusion
We came up with a novel classification for dual LAD in order to standardise the diagnosis and treatment of the dual LAD systems. A comprehensive investigation incorporating findings from multiple cardiac imaging modalities, such as conventional and MDCT angiographies, is required for the identification and diagnosis of this uncommon coronary artery abnormality. The majority of dual LAD variations and accompanying anomalies are associated with a benign course of the aberration, but the malignant course of the anomalous vessels, as well as associated CAD, must be acknowledged. Recognizing this abnormality, on the other hand, is crucial for full revascularization in the case of existing CAD and the prevention of sudden cardiac death.
Informed consent
Informed consent was obtained from a participant included in the study, and additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Competing/conflict of interests
As an author, I declare that there is no financial or non-financial conflict/competing of interests. This manuscript has not been submitted to any journal before for publication as a part or complete version. I give complete consent and rights to the journal for its publication. Informed consent was obtained from a participant included in the study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Funding
There is no source of funding for this article.
Author contribution statement
All the authors contributed to Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Software; Supervision; Validation; Roles/Writing - original draft; Writing - review & editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ihj.2022.04.002.
Contributor Information
Pankaj Jariwala, Email: Pankaj_jariwala@hotmail.com.
Kartik Jadhav, Email: drkartik303@gmail.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Jariwala P., Jadhav K.P., Koduganti S. Dual left anterior descending artery: diagnostic criteria and novel classification. Indian J Thorac Cardiovasc Surg. 2020 Aug 2 doi: 10.1007/s12055-020-01102-z. http://link.springer.com/10.1007/s10832-007-9069-7 [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bozlar Uğur, Şahin Uğurel Mehmet, Sarı Sebahattin, Akgün Veysel, Fatih Örs M.T. Prevalence of dual left anterior descending artery variations in CT angiography. Diagn Interventional Radiol. 2015;21(1):34–41. doi: 10.5152/dir.2014.14275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Uekita H., Miura S., Yamaguchi O., et al. A rare anomaly of LAD mimicking CTO. J Cardiol Case. 2014;9(1):11–14. doi: 10.1016/j.jccase.2013.08.011. [Internet], Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spindola-Franco H., Grose R., Solomon N. Dual left anterior descending coronary artery: angiographic description of important variants and surgical implications. Am Heart J. 1983;105(3):445–455. doi: 10.1016/0002-8703(83)90363-0. [DOI] [PubMed] [Google Scholar]
- 5.Salachas A., Achenbach K., Liberatos G., Hatzioannidis V., Goudevenos I., Sideris D. Isolated corrected transposition of great arteries and double left anterior descending artery originating from the left and right coronary artery: a rare combination of coronary artery anomaly and congenital heart disease. Angiology. 1996;47(1):67–72. doi: 10.1177/000331979604700110. [DOI] [PubMed] [Google Scholar]
- 6.Lama N., Patris MA V.P. European Society of Cardiovascular Radiology. 2019. An exceptional complex coronary anomaly . Is this the new variant in Dual LAD classification system; pp. 1–14. [Google Scholar]
- 7.Vohra A., Narula H. Dual left anterior descending artery with anomalous origin of long LAD from pulmonary artery - rare coronary anomaly detected on computed tomography coronary angiography. Indian J Radiol Imag. 2016;26(2) doi: 10.4103/0971-3026.184423. http://www.ncbi.nlm.nih.gov/pubmed/27413266%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4931778 [Internet] 201–5. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nakamae K., Ichihara Y., Morita K., Niinami H. Surgical management for dual left anterior descending artery with anomalous origin of left coronary artery from pulmonary artery: a case report. Gen Thorac Cardiovasc Surg. 2021 Jan 1;69(1):94–96. doi: 10.1007/s11748-020-01377-4. [DOI] [PubMed] [Google Scholar]
- 9.Montero-Cabezas J.M., Tohamy A.M., Karalis I., Delgado V., Schalij M.J. The descending septal artery: description of this infrequent coronary anatomical variant in three different clinical scenarios. Rev Esp Cardiol. 2015;68(11):1029–1031. doi: 10.1016/j.rec.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 10.Tuncer C., Batyraliev T., Yilmaz R., Gokce M., Eryonucu B., Koroglu S. Origin and distribution anomalies of the left anterior descending artery in 70,850 adult patients: multicenter data collection. Cathet Cardiovasc Interv. 2006;68(4):574–585. doi: 10.1002/ccd.20858. [DOI] [PubMed] [Google Scholar]
- 11.Çanga Y., Güvenç T.S., Karatas M.B., et al. Clinical presentation and outcomes in type IV dual left anterior descending artery anomaly. Int Med Appl Sci. 2016;8(1):32–36. doi: 10.1556/1646.8.2016.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sajja L.R., Farooqi A., Shaik M.S., Yarlagadda R.B., Baruah D.K., Pothineni R.B. Dual left anterior descending coronary artery: surgical revascularization in 4 patients. Tex Heart Inst J/ 2000;27(3):292–296. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=101083&tool=pmcentrez&rendertype=abstract from the Texas Heart Institute of St Luke’s Episcopal Hospital, Texas Children’s Hospital [Internet] Available from: [PMC free article] [PubMed] [Google Scholar]
- 13.Agarwal P.P., Kazerooni E.A. Dual left anterior descending coronary artery: CT findings. Am J Roentgenol. 2008;191(6):1698–1701. doi: 10.2214/AJR.08.1193. [DOI] [PubMed] [Google Scholar]
- 14.Bittner V., Nath H.P., Cohen M., Soto B. Dual connection of the left anterior descending coronary artery to the left and right coronary arteries. Cathet Cardiovasc Diagn. 1989;16(3):168–172. doi: 10.1002/ccd.1810160306. [DOI] [PubMed] [Google Scholar]
- 15.Reuben Ilia H.G., MG Mid left anterior descending coronary artery originating from the right coronary artery. Vol. 33. Int J Cardiol. 1991;33:162–165. doi: 10.1016/0167-5273(91)90165-l. 1991, 162–5. [DOI] [PubMed] [Google Scholar]
- 16.Sayin M.R., Akpinar I., Karabag T., Dogan S.M., Aydin M. Atypical type of dual left anterior descending coronary artery. J Cardiol Case. 2013;8(1):e39–e41. doi: 10.1016/j.jccase.2013.03.009. [Internet], Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spałek M., Stępień-Wałek A., Paszkiewicz J., Wożakowska-Kapłon B. Double left anterior descending artery: congenital anomaly or normal variant of coronary arteries? Cardiol J. 2017 Aug 23;24(4):445–446. doi: 10.5603/CJ.2017.0090. https://journals.viamedica.pl/cardiology_journal/article/view/47504 [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 18.Young Jin Bae, Kwang Soo Cha, Jin Gon Park, et al. Dual left anterior descending coronary artery: incidence, angiographic features and clinical significance in the era of revascularization. Kor Circul J. 2000;30(9) 1092–8. [Google Scholar]
- 19.Sidhu N.S., Wander G.S. Prevalence and characteristics of dual left anterior descending artery in adult patients undergoing coronary angiography. Future Cardiol. 2019;15(6):425–435. doi: 10.2217/fca-2019-0052. [DOI] [PubMed] [Google Scholar]
- 20.Şeker M. Prevalence and morphologic features of dual left anterior descending artery subtypes in coronary CT angiography. Radiol Med. 2020;125(3):247–256. doi: 10.1007/s11547-019-01124-7. [Internet], Available from: [DOI] [PubMed] [Google Scholar]
- 21.Nikolić S., Živković V., Gačić Manojlović E., Milovanović P., Djonić D., Djurić M. Does the myocardial bridge protect the coronary from atherosclerosis? A comparison between the branches of the dual-left anterior descending coronary artery type 3: an autopsy study. Atherosclerosis. 2013;227(1):89–94. doi: 10.1016/j.atherosclerosis.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 22.Jariwala P., Sunnadkal R. Type 9 dual left anterior descending artery or triple left anterior descending artery anomaly: a rare anomaly. J Indian Acad Echocardiogr Cardiovasc Imag. 2019;3(2):99. http://www.jiaecho.org/text.asp?2019/3/2/99/265760 [Internet] Available from: [Google Scholar]
- 23.Bali H.K., Chattree K., Bali S.K., Chauhan H.K.C., Shukla C.P. PCI in a case of dual (type IV) LAD with anomalous origin of the LCx from RCA. J Saudi Heart Assoc. 2014;26(1):43–46. doi: 10.1016/j.jsha.2013.07.003. [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chang C.J., Cheng N.J., Ko Y.S., Ko Y.L., Chiang C.W. Dual left anterior descending coronary artery and anomalous aortic origin of the left circumflex coronary artery: a rare and complicated anomaly. Am Heart J. 1997;133(5):598–601. doi: 10.1016/s0002-8703(97)70157-1. [DOI] [PubMed] [Google Scholar]
- 25.Daralammouri Y., Ghannam M., Lauer B. New congenital coronary artery anomaly - double supply of single left anterior descending coronary artery from the left and right coronary sinuses: a case report. J Med Case Rep. 2016;10(1):1–3. doi: 10.1186/s13256-016-1003-7. [Internet], Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Turkoglu S., Balcioglu S., Ozdemir M. Type IV dual left anterior descending artery associated with anomalous origin of the left circumflex coronary artery from the right coronary artery: a case report. J Invasive Cardiol. 2008;20(12):669–670. [PubMed] [Google Scholar]
- 27.Moreno-Martínez F.L., Cuesta J., Rivero F., Alfonso F., Benedicto A., Pozo-Osinalde E. Y-shaped dual left anterior descending artery or coronary collateral circulation? Rev Española Cardiol. 2019 Apr;72(4):346–348. doi: 10.1016/j.rec.2018.05.009. https://linkinghub.elsevier.com/retrieve/pii/S188558571830197X (English Edition) [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 28.Angelini P. Coronary artery anomalies: an entity in search of an identity. Circulation. 2007;115(10):1296–1305. doi: 10.1161/CIRCULATIONAHA.106.618082. [DOI] [PubMed] [Google Scholar]
- 29.Puranik A., Nair G., Vijayraghavan R. A rare scenario of stenosed type IV dual LAD with normal myocardial perfusion scan. World J Nucl Med. 2012;11(1):28. doi: 10.4103/1450-1147.98744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Al-Umairi R.S., Al-Kindi F.A., Al-Tai S.A. A new variant of dual left anterior descending artery anomaly type XI. Sultan Qaboos Univ Med J. 2018;18(3):e386–e388. doi: 10.18295/squmj.2018.18.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yokokawa T., Watanabe K., Sakamoto T., Ohwada T., Takeishi Y. Importance of multi-detector computed tomography for percutaneous coronary intervention in a patient with type V dual left anterior descending artery. J Cardiol Case. 2012;6(4) doi: 10.1016/j.jccase.2012.06.010. [Internet], e100–2. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matsumoto M., Yokoyama K., Yahagi T., et al. Double left anterior descending artery arising from right and left sinus of Valsalva in patient with acute coronary syndrome. Int J Cardiol. 2011;149(1) doi: 10.1016/j.ijcard.2009.03.049. [Internet] e40–2. Available from: [DOI] [PubMed] [Google Scholar]
- 33.Yamanaka O., Hobbs R.E. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn. 1990;21(1):28–40. doi: 10.1002/ccd.1810210110. [DOI] [PubMed] [Google Scholar]
- 34.Cruz C., McLean D., Janik M., Raggi P., Zafari A.M. A rare coincidence of two coronary anomalies in an adult. Cardiol Res Pract. 2010;1(1) doi: 10.4061/2010/376067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Deora S., Kumar T., Shah S.C., Patel T. Reporting a novel variant of type VI dual left anterior descending artery: a rare coronary anomaly. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2015-211128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ferreira R.d.e.S.A., Santos J.L.A.d.o.s., Greguolo C., Fabris J.F., Pinto M.D.A., Antônio R.S. Intervenção coronária percutânea primária em paciente com artéria descendente anterior dupla. Rev Bras Cardiol Invas. 2015;23(1):66–69. doi: 10.1016/j.rbciev.2014.12.002. [Internet] Available from: [DOI] [Google Scholar]
- 37.Shiraki Teruo, Saito Daiji, Murata Katsutoshi, et al. A case with hypoplastic left anterior descending coronary artery and developed conus branch. Shinzo. 1997;29(4):313–317. [Google Scholar]
- 38.Celik M., Iyisoy A., Celik T. A coronary artery anomaly: type IV dual left anterior descending artery. Cardiovasc J Afr. 2010;21(4):223–224. doi: 10.5830/cvja-2010-032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Belostotsky V., Veljanovska L., Hristov N., Mitrev Z. Dual left anterior descending artery distribution. Interact Cardiovasc Thorac Surg. 2010;10(4):648–649. doi: 10.1510/icvts.2009.221820. [DOI] [PubMed] [Google Scholar]
- 40.Formica F., Corti F., Colombo V., Monica G., Paolini G. Dual left anterior descending coronary artery from right aortic sinus: report of a case of recurrent unstable angina after CABG. Heart Surg Forum. 2005;8(5):299–301. doi: 10.1532/HSF98.20051112. [DOI] [PubMed] [Google Scholar]
- 41.Oral D., Berkalp B., Pamir G., Ömürlü K., Erol Ç. Significance of dual left anterior descending coronary artery in interventional cardiology: a case report. Angiology. 1996;47(8):825–829. doi: 10.1177/000331979604700812. [DOI] [PubMed] [Google Scholar]
- 42.Cakar M.A., Gunduz H., Vatan M.B., Akdemir R. Anterior myocardial infarction in a patient with dual left anterior descending coronary artery. J Cardiovasc Med (Hagerstown, Md) 2012;13(3):203–204. doi: 10.2459/JCM.0b013e3283511fd0. [DOI] [PubMed] [Google Scholar]
- 43.Cusco J.A., Delehanty J.M., Ling F.S. Trifurcation triple balloon angioplasty in a dual left anterior descending coronary artery: the “ménage à trois” revisited. Cathet Cardiovasc Diagn. 1996;38(2):214–217. doi: 10.1002/(SICI)1097-0304(199606)38:2<214::AID-CCD22>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 44.Rigatelli G., Roncon L., Giordan M., Oliva L., Milan T., Cardaioli P. Primary angioplasty with DES-supported culottes stenting to revascularizing a dual left anterior descending coronary artery. Int J Cardiol. 2007;114(2):2005–2006. doi: 10.1016/j.ijcard.2006.07.130. [DOI] [PubMed] [Google Scholar]
- 45.Celik T., Bozlar U., Ozturk C., et al. A new anomaly of the left anterior descending artery: type X dual LAD. Indian Heart J. 2015;67 doi: 10.1016/j.ihj.2015.09.004. [Internet], S14–7. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yavuz T., Nazlı C., Öcal A., Ibrisim E., Kutsal A. Surgically revascularized dual LAD. Int J Cardiovasc Imag. 2004;20(1):71–74. doi: 10.1023/b:caim.0000013153.94737.9b. [DOI] [PubMed] [Google Scholar]
- 47.Cho J.S., Kim J., Yoon S.P. Dual left anterior interventricular coronary artery with a rare course in a Korean. Anat Cell Biol. 2015;48(2):144–146. doi: 10.5115/acb.2015.48.2.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bitigen A., Erkol A., Oduncu V., Akgün T., Mansuroglu D., Ozdemir N. Atherosclerosis in type IV dual left anterior descending artery and anomalous aortic origin of the left circumflex artery in association with rheumatic valve disease: a case report. Heart Surg Forum. 2007;10(4):E276–E278. doi: 10.1532/HSF98.20071026. http://www.ncbi.nlm.nih.gov/pubmed/17599874 [Internet] Available from: [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.