Abstract
Revision anterior cruciate ligament (ACL) reconstruction is a technically demanding procedure, and the surgeon should be prepared to address bone tunnel osteolysis, concurrent meniscal, ligamentous, or cartilage lesions, and limb malalignment. ACL revision can typically be done in one procedure, but it may need to be staged if there is poor previous tunnel positioning or excessive tunnel osteolysis. Bone grafting of the tunnels can be accomplished in several ways, including autograft, allograft, or bone substitutes. Currently, no consensus is available regarding the optimal choice of bone graft material for bone tunnel augmentation in revision ACL reconstruction. Bone graft substitute for tunnel augmentation has been showed to have good histologic, radiographic, and intraoperative integration, comparable to that of autologous bone. In this Technical Note, the technical details of arthroscopic treatment of attenuated anterior cruciate ligament graft with enlarged bone tunnels are described. The tunnels are debrided arthroscopically and filled up with PRO-DENSE injectable regenerative graft.
Technique Video
Arthroscopic treatment of attenuated anterior cruciate ligament graft with enlarged bone tunnels of the right knee. The patient is in the supine position. The anterolateral portal is the viewing portal, and the anteromedial portal is the working portal. The lax anterior cruciate ligament (ACL) is resected. The femoral bone tunnel is debrided, and the tunnel wall is microfractured. The tibial bone tunnel is debrided with the ACL reamer, while the articular opening is covered with an arthroscopic curette. The tibial bone tunnel is further debrided with an arthroscopic shaver and burr via the tunnel. The fluid irrigation is switched off and the subsequent steps are performed under dry arthroscopy. The femoral and tibial bone tunnels are filled up with injectable regenerative graft.
Introduction
Approximately 4% to 13% of all primary anterior cruciate ligament (ACL) reconstruction needs revision.1 Revision ACL reconstruction is a technically demanding procedure, and the surgeon should be prepared to address bone tunnel osteolysis, concurrent meniscal, ligamentous, or cartilage lesions, and limb malalignment.2 ACL revision can typically be done in one procedure but may need to be staged if there is poor previous tunnel positioning or excessive tunnel osteolysis.2
Anteroposterior and lateral images can be evaluated for tibial and femoral tunnel placement (Fig 1). ACL tunnels can be in an accurate location without need for redirection, in an inaccurate location requiring redirection through native bone, or in an inaccurate location requiring redirection through a preexisting tunnel. The latter group may require bone grafting of existing tunnels before revision tunnel placement.1, 2, 3 Moreover, measurements of 15 mm are consistent with notable tunnel osteolysis and makes a primary fixation of the graft either impossible or at least very difficult.1,2,4 The tunnel-enlargement phenomenon occurs primarily with hamstring autografts, suspension fixation devices, and absorbable implants, and it commonly progresses within 24 weeks postoperatively.5, 6, 7 The prevalence of tunnel enlargement ranges from 25% to 100% in femoral tunnels and 29% to 100% in tibial tunnels after ACL reconstruction.6 The mechanism of tunnel enlargement is not well understood; mechanical and biological factors have been suggested as the etiology of tunnel enlargement.5 Biological factors include osteolytic cytokines that enter the space between the graft and the bone through the synovial fluid. Mechanical factors include longitudinal graft motion by extra-cortical femoral fixation (bungee effect), transverse graft motion (windshield-wiper effect), improper graft placement, higher initial graft tension and accelerated rehabilitation.8
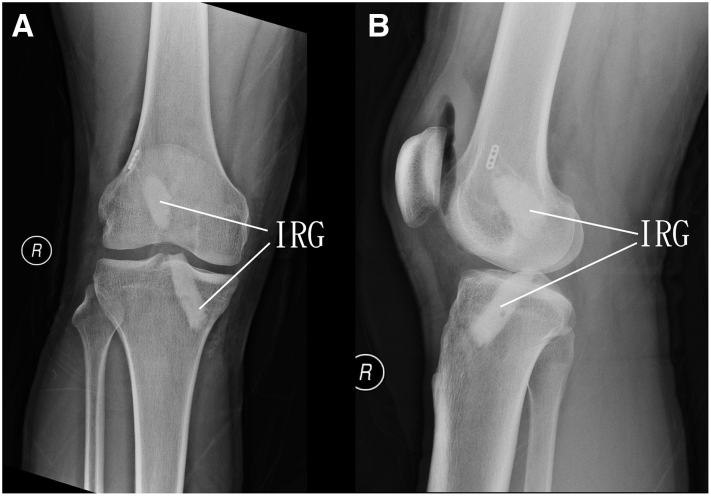
Fig. 1.
Arthroscopic treatment of attenuated anterior cruciate ligament graft with enlarged bone tunnels of the right knee. The patient is in supine position. Anteroposterior (A) and lateral (B) radiographs of the knee showed the position of the bone tunnels and degree of tunnel enlargement. FBT, femoral bone tunnel; TBT, tibial bone tunnel.
Literature supports proceeding with a bone grafting procedure in these situations before revision ACL reconstruction.1,2,4 The goal is to fill all bony defects and provide a fresh landscape for new tunnels. Bone grafting of the tunnels can be accomplished in several ways, including autograft, allograft, or bone substitutes.2 Currently, no consensus is available regarding the optimal choice of bone graft material for bone tunnel augmentation in revision ACL reconstruction.9 Autograft for bone tunnel grafting may be associated with a lower risk of revision ACL reconstruction graft failure compared with allograft bone.9,10 However, the autograft is usually harvested from the iliac crest, which is associated with a high morbidity rate.1 Alternatively, bone graft substitute for tunnel augmentation has been showed to have good histologic, radiographic, and intraoperative integration, comparable to that of autologous bone.1,11 The purpose of this Technical Note is to describe the details of arthroscopic treatment of attenuated anterior cruciate ligament graft with enlarged bone tunnels. The tunnels are debrided arthroscopically and filled up with PRO-DENSE injectable regenerative graft (Wright, Memphis, TN). It is indicated for recurrent laxity after ACL reconstruction with tunnel enlargements of 10-15 mm or more and/or previous tunnel position affecting placement of new tunnels.1, 2, 3 It is contraindicated if the recurrent laxity is associated with appropriately placed tunnels without excessive tunnel osteolysis or previous tunnels outside the trajectory for revision tunnels (Table 1).2 In these cases, 1-staged revision should be performed.9
Table 1.
Indications and Contraindications of Arthroscopic Treatment of Attenuated Anterior Cruciate Ligament Graft with Enlarged Bone Tunnels
| Indications | Contraindications |
|---|---|
|
|
Surgical Technique
Preoperative Planning and Patient Positioning
Detailed history of the symptoms and previous operation and clinical examination of the knee are important for decision making of revision surgery. Advanced imaging should be obtained in all patients with a history of ACL reconstruction and recurrent laxity. Magnetic resonance imaging (MRI) should be obtained to evaluate the status of the graft and provide a preliminary evaluation of the tunnel position and size. MRI can also be used to evaluate for concomitant chondral, meniscal, or ligamentous pathology.2,4 It does have limitations when evaluating the bony anatomy, and preexisting hardware can distort the images, making measurements difficult. Computed tomogram (CT) has been found to provide detailed evaluation of bony pathology, size of the bone tunnels, and any existing osteolysis.2,4 Tibial and femoral tunnel size should be measured on the preoperative CT scan for preoperative planning. Tunnel diameter should be measured at the widest visualized diameter on the axial, coronal, and sagittal planes.2,4
The patient is in supine position, and an ipsilateral thigh tourniquet is used to provide a bloodless surgical field. Fluid inflow is driven by gravity, an arthro-pump is not used, and a 4.0-mm, 30° arthroscope (Dyonics, Smith and Nephew, Andover, MA) is used.
Portal Placement
The procedure is performed via the anteromedial and anterolateral portals. The anterolateral portal is 1 cm above the knee joint line and just next to the patellar tendon in a palpable soft spot. The anteromedial portal is 1 cm above the joint line and 1 cm medial to the patellar tendon, also in a palpable soft spot.12 Five-millimeter skin incisions are made at the portal sites. The capsule is perforated by a hemostat.
The procedure should begin with a thorough diagnostic arthroscopy to evaluate the articular cartilage, menisci, and tunnel placement, as well as prior hardware locations and the presence of scar tissue, a cyclops lesion, or notch overgrowth.4
Resection of the Lax Anterior Cruciate Ligament
The anterolateral portal is the viewing portal and the anteromedial portal is the working portal. The lax anterior cruciate ligament graft is resected from its tibial insertion toward its femoral insertion with an arthroscopic radiofrequency wand (Smith and Nephew, Andover, MA) (Fig 2). Caution should be paid not to injure the posterior cruciate ligament.
Fig 2.
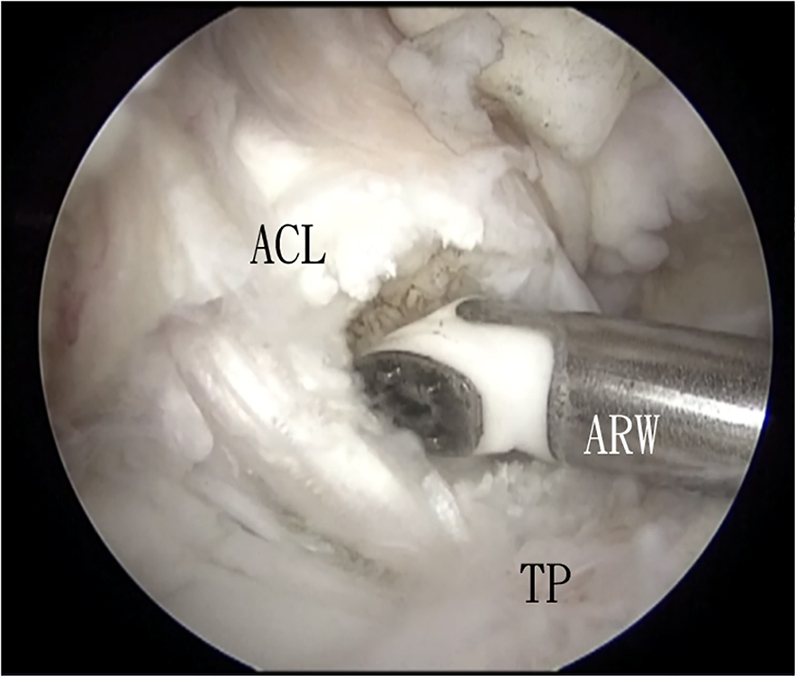
Arthroscopic treatment of attenuated anterior cruciate ligament graft with enlarged bone tunnels of the right knee. The patient is in supine position. The anterolateral portal is the viewing portal and the anteromedial portal is the working portal. The lax anterior cruciate ligament graft is resected from its tibial insertion toward its femoral insertion with an arthroscopic radiofrequency wand. ACL, anterior cruciate ligament; ARW, arthroscopic radiofrequency wand; TP, tibial plateau.
Debridement of the Femoral Bone Tunnel
The anterolateral portal is the viewing portal and the anteromedial portal is the working portal. When the anterior cruciate ligament is traced proximally, the femoral bone tunnel can be identified. The fibrous tissue of the tunnel is curetted and resected with arthroscopic curette (Arthrex, Naples, FL), arthroscopic shaver (Dyonics, Smith and Nephew) and arthroscopic radiofrequency wand (Fig 3). After clearance of the soft tissue, the tunnel wall is microfractured with an arthroscopic awl (Smith and Nephew, Andover, MA).
Fig 3.

Arthroscopic treatment of attenuated anterior cruciate ligament graft with enlarged bone tunnels of the right knee. The patient is in supine position. The anterolateral portal is the viewing portal, and the anteromedial portal is the working portal. The fibrous tissue of the tunnel is curetted and resected with arthroscopic curette. AC, arthroscopic curette; FBT, femoral bone tunnel.
Debridement of the Tibial Bone Tunnel
The anterolateral portal is the viewing portal. The previous surgical scar for tibial bone is incised. A guide pin is inserted through the tibial bone tunnel to the knee joint. The tip of the guide wire is covered with the arthroscopic curette, which is inserted via the anteromedial portal. The tibial tunnel is debrided by drilling with an ACL reamer along the guide pin. Coverage of the guide pin by the curette can prevent accidental injury to the articular cartilage during reaming of the tibial tunnel. The tibial tunnel is further debrided with the arthroscopic shaver, which is inserted via the distal tibial cortical opening of the bone tunnel. After all the fibrous tissue is removed, the sclerotic wall of the tunnel is debrided with an arthroscopic burr (Dyonics, Smith and Nephew) (Fig 4).
Fig 4.
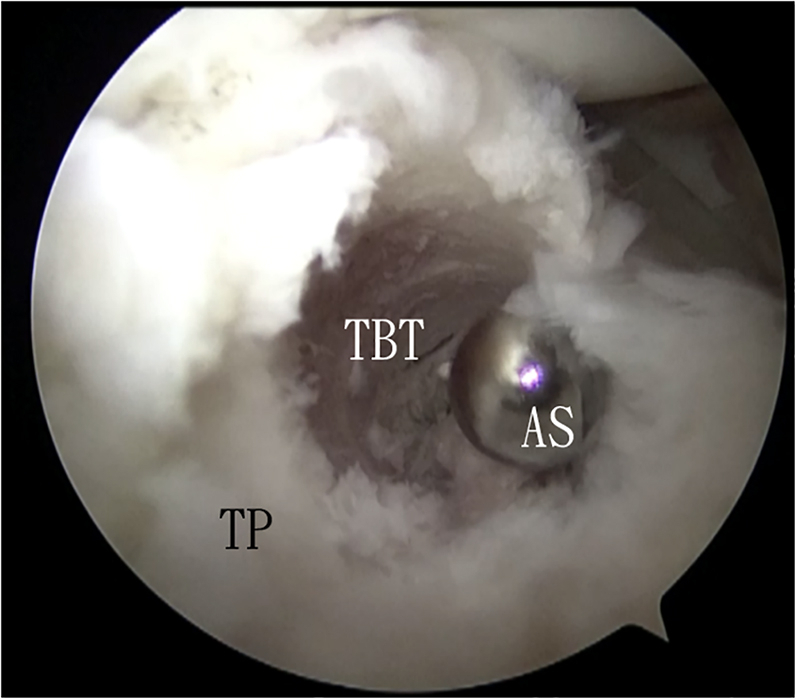
Arthroscopic treatment of attenuated anterior cruciate ligament graft with enlarged bone tunnels of the right knee. The patient is in the supine position. The anterolateral portal is the viewing portal, and the tibial bone tunnel is the working portal. The tibial tunnel is debrided with the arthroscopic shaver. AS, arthroscopic shaver; TBT, tibial bone tunnel; TP, tibial plateau.
The fluid irrigation is switched off, and the subsequent steps are performed under dry arthroscopy.
Fill Up the Femoral Bone Tunnel with PRO-DENSE Injectable Regenerative Graft
The anterolateral portal is the viewing portal and the anteromedial portal is the working portal. The delivery needle (Wright, Memphis, TN) is inserted into the femoral bone tunnel, and the tunnel is filled up by the PRO-DENSE Injectable Regenerative Graft (Wright) (Fig 5).
Fig 5.
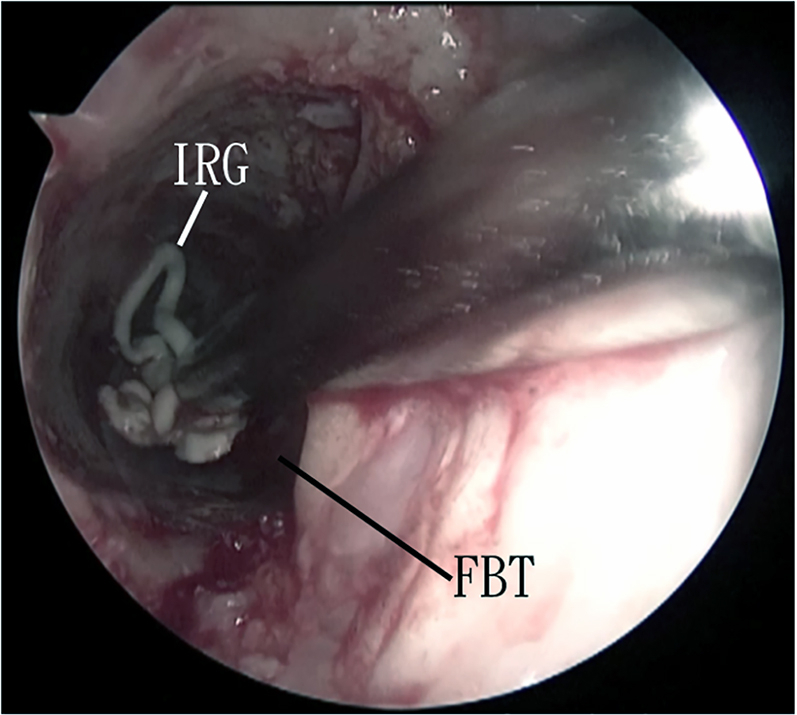
Arthroscopic treatment of attenuated anterior cruciate ligament graft with enlarged bone tunnels of the right knee. The patient is in the supine position. The anterolateral portal is the viewing portal, and the anteromedial portal is the working portal. The delivery needle is inserted into the femoral bone tunnel, and the tunnel is filled up by the PRO-DENSE injectable regenerative graft. FBT, femoral bone tunnel; IRG, injectable regenerative graft.
Fill up the Tibial Bone Tunnel With PRO-DENSE Injectable Regenerative Graft
The anterolateral portal is the viewing portal. The tibial bone tunnel is dried up with peanut swab via its distal tibial cortical opening and then, the delivery needle is inserted in the bone tunnel. The tibial bone tunnel is filled up by the PRO-DENSE Injectable Regenerative Graft, while the articular opening of the bone tunnel is covered with a bone curette of appropriate size via the anteromedial portal in order to avoid excessive leakage of the graft into the knee joint (Fig 6, Fig 7, Video 1, and Table 2).
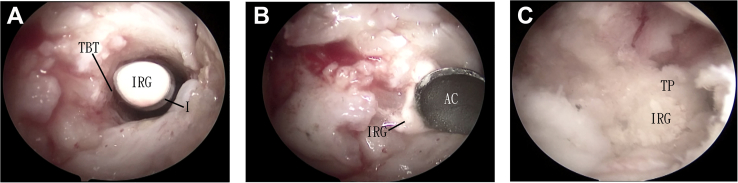
Fig 6.
Arthroscopic treatment of attenuated anterior cruciate ligament graft with enlarged bone tunnels of the right knee. The patient is in the supine position. The anterolateral portal is the viewing portal and the anteromedial portal and tibial bone tunnel are the working portals. (A) The delivery needle loaded with PRO-DENSE Injectable Regenerative Graft is inserted into the tibial bone tunnel. (B) A bone curette of appropriate size is inserted via the anteromedial portal to over the articular opening of the bone tunnel during injection of the graft. (C) The tibial tunnel is filled up with the graft up to the level of tibial plateau. IRG, injectable regenerative graft; AC, arthroscopic curette; TBT, tibial bone tunnel; TP, tibial plateau.
Fig 7.
Arthroscopic treatment of attenuated anterior cruciate ligament graft with enlarged bone tunnels of the right knee. The patient is in the supine position. The anterolateral portal is the viewing portal, and the anteromedial portal is the working portal. Postoperative anterolateral (A) and lateral (B) radiographs showed that the femoral and tibial bone tunnels are filled up with the injectable regenerative graft (IRG).
Table 2.
Pearls and Pitfalls of Arthroscopic Treatment of Attenuated Anterior Cruciate Ligament Graft With Enlarged Bone Tunnels
| Pearls | Pitfalls |
|---|---|
|
|
Discussion
In two-staged revision ACL reconstruction, a CT scan may be performed 3-6 months after the initial procedure to evaluate the integration of the graft and assess readiness for the second stage of the revision.1,4 Two-staged revision usually requires an average delay of 4-6 months to allow for the bone defect to heal, likely subjecting patients to a prolonged period of knee instability and, thus adding to the risk of meniscal injury, additional deterioration of muscle strength, and osteochondrosis.1,3 In order to avoid these potential risks, 1-staged revision is preferable whenever possible.
Same as primary ACL reconstruction, anatomic graft placement and stable initial fixation of a revision ACL graft should be achieved in the revision ACL reconstruction.3 Bone tunnel enlargement and incorrect positioning of the tunnels in the primary ACL reconstruction can potentially compromise fixation of the revision ACL graft.1,3 Careful preoperative planning is very important for success of the revision surgery.7 The presence of significant tunnel enlargement and/or possibility of confluence of previous bone tunnels and the planned new tunnels indicate the need of a 2-staged revision.
Accurate bone tunnel filling in a 2-staged anterior cruciate ligament revision is indubitably fundamental for a successful outcome.10 Autograft bone is frequently used, but it requires longer operative time and is associated with donor-site morbidity.9,10 Use of allografts may solve these problems, but their use is associated with high costs and strict regulatory limitations.10 Use of bone substitutes can avoid donor site morbidity associated with traditional autograft harvesting, and it has comparable outcomes in terms of lamellar bone formation and integration within the tunnels, allowing a correct tunnel placement during revision surgery.1,10 They can be used to fill bone tunnels in an easier and faster way, and their use is associated with fewer postoperative complications, such as pain and local hematoma.10 In this reported technique, an injectable regenerative graft is used. It is based on combinations of the fast dissolving calcium sulfate and the stronger and more slowly remodeling calcium phosphate compounds. This might enhance vascular infiltration and replacement of the graft by new bone, while providing osteoconductive and mechanical support.13,14 Moreover, its initial stability after setting can avoid dropping of the graft from the femoral bone tunnel into the knee joint by the effect of gravity.4
This minimally invasive technique has the advantage of less soft tissue trauma, better cosmetic result, less wound complications, shorter operative time, and avoidance of bone graft donor site morbidity. The potential risks of this technique include unhealed bone tunnels, injury to the posterior cruciate ligament and articular cartilage (Table 3). This is not technically demanding and can be attempted by the averaged knee arthroscopists.
Table 3.
Advantages and Risks of Arthroscopic Treatment of Attenuated Anterior Cruciate Ligament Graft With Enlarged Bone Tunnels
| Advantages | Risks |
|---|---|
|
|
Footnotes
Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic treatment of attenuated anterior cruciate ligament graft with enlarged bone tunnels of the right knee. The patient is in the supine position. The anterolateral portal is the viewing portal, and the anteromedial portal is the working portal. The lax anterior cruciate ligament (ACL) is resected. The femoral bone tunnel is debrided, and the tunnel wall is microfractured. The tibial bone tunnel is debrided with the ACL reamer, while the articular opening is covered with an arthroscopic curette. The tibial bone tunnel is further debrided with an arthroscopic shaver and burr via the tunnel. The fluid irrigation is switched off and the subsequent steps are performed under dry arthroscopy. The femoral and tibial bone tunnels are filled up with injectable regenerative graft.
References
- 1.von Recum J., Gehm J., Guehring T., et al. Autologous bone graft versus silicate-substituted calcium phosphate in the treatment of tunnel defects in 2-stage revision anterior cruciate ligament reconstruction: A prospective, randomized controlled study with a minimum follow-up of 2 years. Arthroscopy. 2020;36:178–185. doi: 10.1016/j.arthro.2019.07.035. [DOI] [PubMed] [Google Scholar]
- 2.Miller M.D., Kew M.E., Quinn C.A. Anterior cruciate ligament revision reconstruction. J Am Acad Orthop Surg. 2021;29:723–731. doi: 10.5435/JAAOS-D-21-00088. [DOI] [PubMed] [Google Scholar]
- 3.Yoon K.H., Kim J.S., Park S.Y., Park S.E. One-stage revision anterior cruciate ligament reconstruction: Results according to preoperative bone tunnel diameter. Five to fifteen-year follow-up. J Bone Joint Surg Am. 2018;100:993–1000. doi: 10.2106/JBJS.17.01044. [DOI] [PubMed] [Google Scholar]
- 4.Kew M.E., Miller M.D., Werner B.C. Chapter 5: Techniques for ACL revision reconstruction. Sports Med Arthrosc Rev. 2020;28:e11–e17. doi: 10.1097/JSA.0000000000000262. [DOI] [PubMed] [Google Scholar]
- 5.Lee D.K., Kim J.H., Lee S.S., et al. Femoral tunnel widening after double-bundle anterior cruciate ligament reconstruction with hamstring autograft produces a small shift of the tunnel position in the anterior and distal direction: Computed tomography-based retrospective cohort analysis. Arthroscopy. 2021;37:2554–2563.e1. doi: 10.1016/j.arthro.2021.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Yue L., DeFroda S.F., Sullivan K., Garcia D., Owens B.D. Mechanisms of bone tunnel enlargement following anterior cruciate ligament reconstruction. JBJS Rev. 2020;8 doi: 10.2106/JBJS.RVW.19.00120. [DOI] [PubMed] [Google Scholar]
- 7.Sauer S., Lind M. Bone tunnel enlargement after ACL reconstruction with hamstring autograft is dependent on original bone tunnel diameter. Surg J (N Y) 2017;3:e96–e100. doi: 10.1055/s-0037-1603950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taketom S. Editorial Commentary: Tunnel widening after anterior cruciate ligament reconstruction may increase laxity and complicate revision. Arthroscopy. 2021;37:2564–2566. doi: 10.1016/j.arthro.2021.04.013. [DOI] [PubMed] [Google Scholar]
- 9.Salem H.S., Axibal D.P., Wolcott M.L., et al. Two-stage revision anterior cruciate ligament reconstruction. A systematic review of bone graft options for tunnel augmentation. Am J Sports Med. 2020;48:767–777. doi: 10.1177/0363546519841583. [DOI] [PubMed] [Google Scholar]
- 10.Kon E., Di Matteo B. Editorial Commentary: Bone tunnel grafting for two-stage anterior cruciate ligament revision and the meaning of life for an arthroscopic surgeon. Arthroscopy. 2020;36:186–188. doi: 10.1016/j.arthro.2019.09.038. [DOI] [PubMed] [Google Scholar]
- 11.von Recum J., Schwaab J., Guehring T., Grutzner P.A., Schnetzke M. Bone incorporation of silicate-substituted calcium phosphate in 2-stage revision anterior cruciate ligament reconstruction: A histologic and radiographic study. Arthroscopy. 2017;33:819–827. doi: 10.1016/j.arthro.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 12.Ward B.D., Lubowitz J.H. Basic knee arthroscopy Part 2: Surface anatomy and portal placement. Arthrosc Tech. 2013;2:e501–e502. doi: 10.1016/j.eats.2013.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Larsson S., Hannink G. Injectable bone-graft substitutes: Current products, their characteristics and indications, and new developments. Injury. 2011;42:S30–S34. doi: 10.1016/j.injury.2011.06.013. [DOI] [PubMed] [Google Scholar]
- 14.Li C.C.H., Lui T.H. Management of bone cyst of talar body by endoscopic curettage, nanofracture and bone graft substitute. Arthrosc Tech. 2021;10:e1985–e1993. doi: 10.1016/j.eats.2021.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic treatment of attenuated anterior cruciate ligament graft with enlarged bone tunnels of the right knee. The patient is in the supine position. The anterolateral portal is the viewing portal, and the anteromedial portal is the working portal. The lax anterior cruciate ligament (ACL) is resected. The femoral bone tunnel is debrided, and the tunnel wall is microfractured. The tibial bone tunnel is debrided with the ACL reamer, while the articular opening is covered with an arthroscopic curette. The tibial bone tunnel is further debrided with an arthroscopic shaver and burr via the tunnel. The fluid irrigation is switched off and the subsequent steps are performed under dry arthroscopy. The femoral and tibial bone tunnels are filled up with injectable regenerative graft.
Arthroscopic treatment of attenuated anterior cruciate ligament graft with enlarged bone tunnels of the right knee. The patient is in the supine position. The anterolateral portal is the viewing portal, and the anteromedial portal is the working portal. The lax anterior cruciate ligament (ACL) is resected. The femoral bone tunnel is debrided, and the tunnel wall is microfractured. The tibial bone tunnel is debrided with the ACL reamer, while the articular opening is covered with an arthroscopic curette. The tibial bone tunnel is further debrided with an arthroscopic shaver and burr via the tunnel. The fluid irrigation is switched off and the subsequent steps are performed under dry arthroscopy. The femoral and tibial bone tunnels are filled up with injectable regenerative graft.