Abstract
Injuries to the posterolateral corner (PLC) of the knee are uncommon, and usually associated with other ligamentous injuries. A combined posterior cruciate ligament (PCL) and PLC tear is the most frequent combination. Several studies describe anatomic reconstructive techniques using an open approach with large incisions and extensive exploration of the posterolateral structures. This Technical Note describes an all-arthroscopic technique as a safe and efficient treatment of combined PCL and PLC instability using the trans-septal approach.
Key Words: instability, knee trauma, multi-ligament knee injury, posterolateral corner, sports injury
Technique Video
All-arthroscopic treatment of combined PCL and PLC instability using the trans-septal approach is shown in a right knee in the supine position.
Introduction
Injuries to the posterolateral corner (PLC) of the knee are uncommon, and are usually associated with other ligamentous injuries.1 Approximately 60% of posterior cruciate ligament (PCL) injuries are associated with tears of the PLC structures.2 These injuries typically occur in the setting of a multiligament knee injury; therefore, the diagnosis and surgical reconstruction can be extremely challenging.3
Classically, anatomic techniques use an open-approach with a large lateral incision, extensive exploration of the posterolateral structures, identification of the peroneal nerve and capsulotomy.4,5 Arthroscopic assessment of the posterior compartments of the knee is challenging due to the proximity of the neurovascular bundle. This study describes an all-arthroscopic technique for the treatment of combined PCL and PLC instability.
Surgical Technique
This Technical Note presents an all-arthroscopic technique for the treatment of combined PCL and PLC instability (Video 1). The pearls and pitfalls, advantages, and disadvantages are presented in Tables 1 and 2.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls | |
|---|---|---|
| Trans-septal approach | Posterolateral and posteromedial portals should be well established. Shaver faces toward the scope (anterior) in order to avoid any popliteal neurovascular bundle injury The PCL tibial attachment exposure can be completely achieved by detaching the posterior capsule from the PCL for more than 10 mm downward from the articular surface. In addition to a direct visualization, a fluoroscopic examination is recommended to confirm the location of the tip of the guidewire before overdrilling it with a reamer. |
Creating the posterior portals using the light source to transilluminate the skin incision, which avoids neurovascular injury Gentle removal of the central-inferior septum is important to avoid iatrogenic injury to the middle genicular vessels. The retained PCL tibial attachment is useful for setting the orientation of the center of the PCL tibial attachment. |
| PCL/ PT tunnel creation | The PCL tibial attachment exposure can be completely achieved by detaching the posterior capsule from the PCL for more than 10 mm downward from the articular surface. | Carefully keep the cutting surface of the shaver in the anteroinferior direction, facing the bone and away from neurovascular bundle. |
|
Graft fixation |
The tension of the ACL provides relatively accurate information about the reduction of the knee joint. | While fixing the PCL graft, maintain the tibia reduced by pulling the proximal tibia anteriorly, while the knee is flexed at 90°. |
ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
Table 2.
Advantages and Disadvantages
| Advantages |
| Less morbidity |
| Trans-septal approach is safe and provides direct visualization of the footprints. |
| Anatomic reconstruction |
| Less risk of tibial tunnel malpositioning |
| Less exposure and tourniquet time may lead to low infection rates. |
| Disadvantages |
| Significant learning curve in trans-septal approach |
| Risk of vascular injury to the popliteal and the lateral inferior genicular arteries |
| More demanding to identify insertion sites of the posterolateral corner structures arthroscopically than when performing an open procedure |
Patient Setup
The patient is placed supine on the operating table in the standard arthroscopy position with a lateral post, just proximal to the knee, at the tourniquet level. A foot roll prevents the hip from externally rotating and maintains 90° of knee flexion.
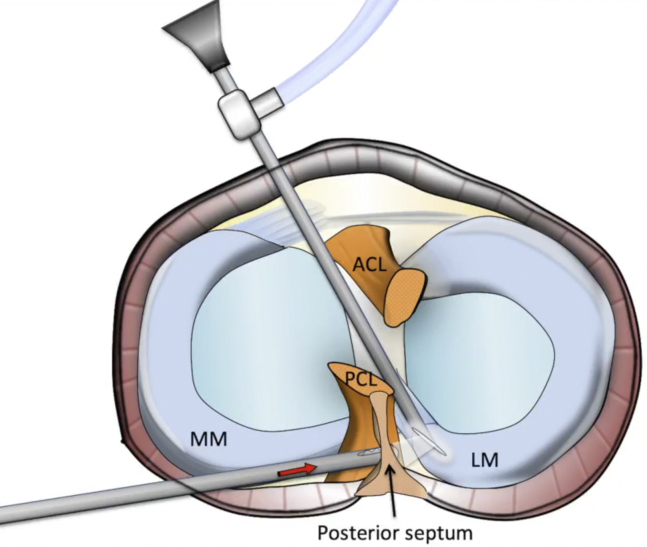
Trans-septal approach and posterior portals
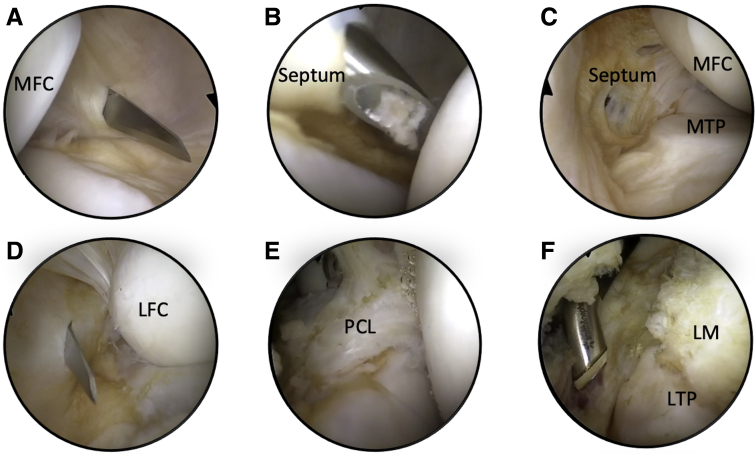
Initially, a routine arthroscopic examination of the knee joint is performed through the standard anterolateral and anteromedial portals. A trans-septal approach, as described by Ahn et al.,6 is used to gain access between the medial and lateral posterior compartments (Fig 1). After making a posteromedial portal, a shaver is introduced with the tip in contact with the medial side of the septum facing anteriorly, away from the popliteal neurovascular bundle (Fig 2, A-D). The septum is then released until the shaver is visible in the posterolateral compartment. The posterolateral compartment can then be accessed via the posteromedial portal, and a posterolateral portal can be performed under direct arthroscopic visualization using transillumination of the skin. Portal placement is posterior to the lateral collateral ligament (LCL) and popliteus tendon (PT) at the level of the joint line for access to the PT and fibular head. The shaver is inserted into the posterolateral portal to resect the septum to the level of the PCL (Fig 2E). A radio frequency device is inserted through the posterolateral portal to separate the posterolateral capsule from the posterior horn of the lateral meniscus for 2 cm to visualize the popliteal sulcus (Fig 2F). The lateral meniscus, the popliteus, the posterior capsule, and proximal tibiofibular capsule are identified. The posterior capsule and gastrocnemius muscle fibers are seen distally, and the space between the popliteus and gastrocnemius is opened. After the synovium is removed with a shaver, the popliteus musculotendinous junction is identified (Fig 2F).
Fig 1.
Transeptal approach illustration. ACL, anterior cruciate ligament; LM, lateral meniscus; MM, medial meniscus; PCL, posterior cruciate ligament. Red arrow shows shaver facing anteriorly toward the posterior septum, while black arrow shows the posterior septum.
Fig 2.
Arthroscopic images showing the making of the posteromedial portal (A), septum debridement with the shaver (B) , the view of the septum hole, with the arthroscope inserted in the posteromedial portal (C), the making of the posterolateral portal (D), the identification of the tibial posterior cruciate ligament remnant stump (E), and the opening of the popliteus sulcus window (F).
PCL/ PT tunnel creation
With the arthroscope in the posteromedial portal, the shaver is introduced from the posterolateral portal to reach the PCL tibial footprint. The PCL tibial attachment site is exposed by detaching the posterior capsule from the PCL for more than 10 mm downward from the articular surface. The cutting surface of the shaver is kept in an anteroinferior direction, facing the bone, to avoid damaging the posterior neurovascular structures. The hook of the PCL tibial guide is introduced through the anteromedial portal toward the PCL tibial footprint. A guidewire is introduced at the hamstring insertion site, until its tip appears in the PCL footprint under direct visualization. A fluoroscopic examination confirms the location of the tip of the guidewire before overdrilling with a 9-mm cannulated reamer. To protect the neurovascular structures, a curette is placed over the wire tip. Using a suture passer, the surgeon inserts a looped Ethibond suture (Ethicon, Somerville, NJ) through the tunnel and pulled out through the anterolateral portal.
The PLC tibial tunnel is performed after locating the musculotendinous junction on the posterior aspect of the tibia and identifying the insertion site of the PT on the tibia. The ACL femoral drill guide (Arthrex, Naples, FL) is inserted through the posterolateral portal (video). The tip of the guide is placed in the middle of the PT insertion site on the tibia at the level of the tip of the fibula.7 The anterior starting point of the drill guide is located between the lateral edge of the tibial tuberosity and the medial edge of Gerdy’s tubercle. A guidewire is inserted in an anteroposterior direction through the guide, and then overdrilled to a 7-mm tunnel. A curette is placed over the tip for protection. Another looped Ethibond suture (Ethicon) is inserted through the tunnel with the suture passer and retrieved through the lateral incision.
The PLC femoral tunnel is initially made by introducing the arthroscope from the anterolateral portal into the lateral gutter. A guidewire is placed in the middle of the femoral footprint of the PT, ∼18.5 mm distally to the LCL insertion site. The femoral socket is overdrilled with a 7-mm reamer to a depth of 25 mm for the PT. A FiberStick (Arthrex) is then inserted through the lateral incision, and the loop is grasped and pulled out to the femur, leaving the FiberStick filling the entire PT tunnel from its exit in the tibia to its entry into the femur.
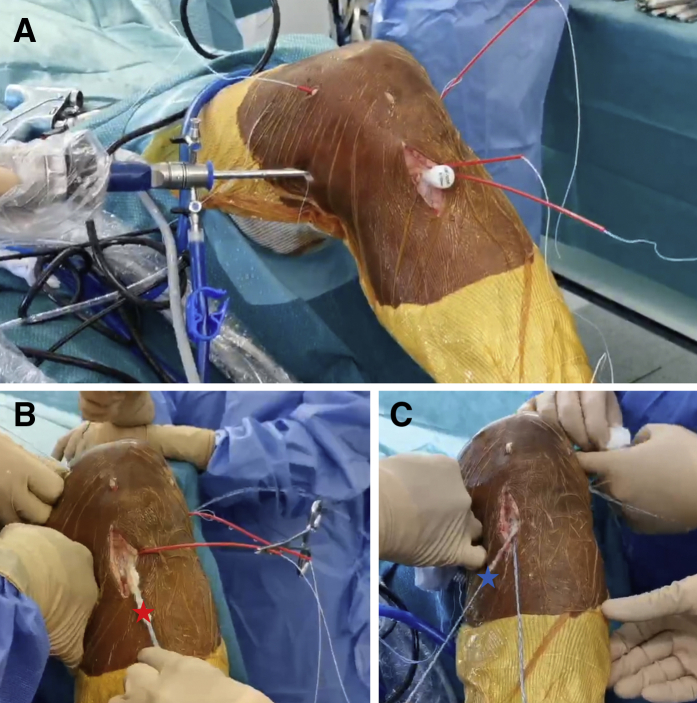
The PCL femoral attachment is located 10 mm posterior to the distal border of the articular cartilage of the medial femoral condyle. At this location, a guidewire is inserted using the drill guide, piercing the medial femoral condylar cortex. The femoral tunnel is reamed from outside-in using a Flipcutter (Arthrex). The retained PCL fibers at the femoral attachment are preserved as much as possible. Similar to the PLC, a FiberStick is used to grasp the loop and pull it out to the femur, leaving the FiberStick filling the PCL tunnel from its exit in the tibia to its entry into the femur (Fig 3A).
Fig 3.
Graft passage. (A) Two FiberStick filling the entire length of the tunnels (PCL [posterior cruciate ligament] and PT [popliteus tendon]) just before the passage of the respective grafts. (B) PCL graft passage (red star denotes PCL graft). (C) PT graft passage (black star denotes PT graft).
Graft Passage and Fixation
The PCL is reconstructed using a tibialis posterior allograft, and the PT, a double gracilis autograft. The grafts are prepared to pass through a 7-mm tunnel after tubularizing the tendon ends. Maintaining the knee in 90° of flexion, with the arthroscope placed in the anterolateral portal, the suture attached to the tibialis posterior allograft is tied to the PCL suture loop and pulled into Yesthe posterior aspect of the joint through the tibial tunnel, passing anteriorly along the superior border of the fibers of the PCL remnant and exiting through the femoral tunnel (Fig 3B). Then, the same procedure is done in the PT tunnel with the double gracilis autograft, pulling the graft from the tibia, passing through the joint and exiting in the femur (Fig 3C). At this point, the arthroscope is placed in the posterolateral compartment, and the graft passage is confirmed.
After the femoral attachment of the PCL the graft has been fixed with a button (Arthrex), the tibia is reduced by pulling the proximal tibia anteriorly, while the knee is flexed at 90°. The tension of the ACL provides information regarding the reduction of the knee joint, while it is evaluated with a probe.6 While keeping the knee in a reduced position, the graft is fixed to the tibia with another button. Finally, while applying an anterior load to the graft at 90° of flexion and internal rotation, the PT graft is fixed in the femur and in the tibia with cannulated bioabsorbable interference screws. The popliteus sulcus window is closed with a 25° hook (QuickPass Lasso, Arthrex) loaded with a no. 0 absorbable monofilament suture.
Postoperative
The postoperative rehabilitation program follows the protocol developed by Edson and Fanelli.8 A PCL brace is used to minimize gravitational forces on the tibia, while the patient is supine. The brace is locked in extension during ambulation, and the patient is allowed to partially weight bear with crutches for 6 weeks. The patient is allowed to start prone, passive knee flexion to 90° immediately. After 6 weeks, progressive weight bearing, as tolerated, is allowed with crutches and the brace unlocked. Closed kinetic chain exercises, range of motion, core strengthening, and attainment of a normal gait pattern are the goals from 6 to 12 weeks postoperatively. Isolated hamstring exercises are not allowed for 6 months, and the brace is worn full time for 1 year.
Discussion
This technique provides an alternative to an open approach for combined PCL and PLC reconstruction, demonstrating to be a safe and efficient technique and restoring external tibial rotation stability as effectively as the traditional open approach. This is an encouraging message, since surgery involving PLC instability combined with other ligamentous injuries has been reported as technically demanding, with possible unsatisfactory outcomes.3,9
This technique is less morbid compared to the traditional open approach. In our experience, it has proven to be superior, respecting the anatomy with less complications. More clinical studies are needed to verify this comparison.
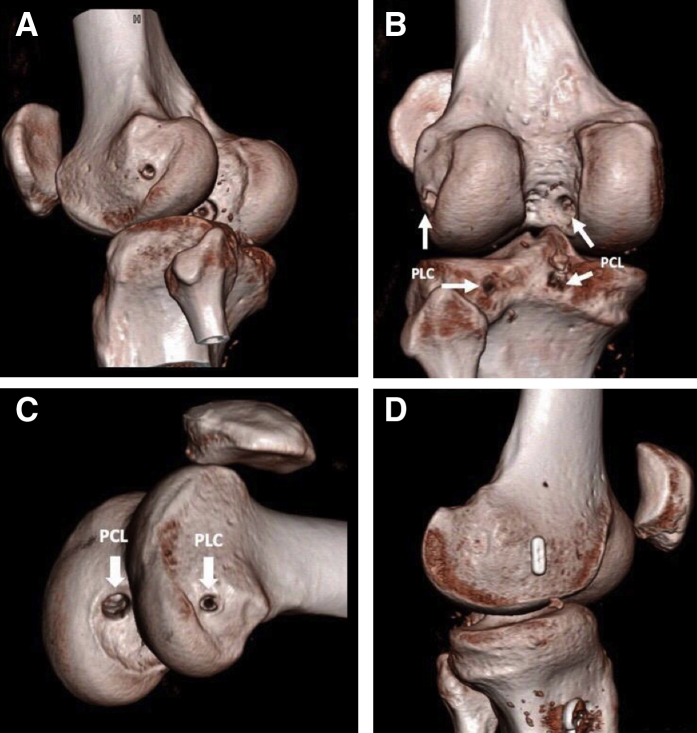
In PCL reconstructions, problems, such as poor visualization of the tibial attachment, malposition of the tibial tunnel, and risk of any serious neurovascular injury may lead to poor outcomes. In the presented technique, such as previously described by Freychet et al.,10 the use of the trans-septal approach allows an excellent visual field and improves exposure of the PCL tibial attachment site. This method decreases the risk of injuring the posterior neurovascular structures and provides an accurate transtibial tunnel while preserving the distal tibial stump of the PCL (Fig 4).
Fig 4.
CT Scan control showing a good positioning of the tunnels, respecting the anatomy of PCL and PT original attachments. (A) Inferolateral view with both posterior cruciate ligament (PCL) and posterolateral corner (PLC) tunnels. (B) Posterior view with both PCL and PLC tunnels (white arrows). (C) Lateral view with both PCL and PLC tunnels (white arrows). (D) Medial view.
Conclusion
This Technical Note described an all-arthroscopic technique for the treatment of combined PCL and PLC instability. We are facing an evolution in the treatment of posterolateral knee instability, always characterized as a morbid surgery, and with modest functional outcomes.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: Y.L. reports personal fees from Arthrex, Smith & Nephew, Stryker, and Biomet, outside the submitted work. B.S.-C. reports personal fees from Arthrex, outside the submitted work. C.G. reports grants from Arthrex, outside the submitted work. B.A.L. reports grants from Arthrex, outside the submitted work. L.G. reports grants from Arthrex, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
All-arthroscopic treatment of combined PCL and PLC instability using the trans-septal approach is shown in a right knee in the supine position.
References
- 1.LaPrade R.F., Wentorf F.A., Fritts H., Gundry C., Hightower C.D. A prospective magnetic resonance imaging study of the incidence of posterolateral and multiple ligament injuries in acute knee injuries presenting with a hemarthrosis. Arthroscopy. 2007;23:1341–1347. doi: 10.1016/j.arthro.2007.07.024. [DOI] [PubMed] [Google Scholar]
- 2.Petrillo S., Volpi P., Papalia R., Maffulli N., Denaro V. Management of combined injuries of the posterior cruciate ligament and posterolateral corner of the knee: a systematic review. Br Med Bull. 2017;123:47–57. doi: 10.1093/bmb/ldx014. [DOI] [PubMed] [Google Scholar]
- 3.Levy B.A., Stuart M.J., Whelan D.B. Posterolateral instability of the knee: Evaluation, treatment, results. Sports Med Arthrosc Rev. 2010;18:254–262. doi: 10.1097/JSA.0b013e3181f88527. [DOI] [PubMed] [Google Scholar]
- 4.Blackman A.J., Engasser W.M., Krych A.J., Stuart M.J., Levy B.A. Fibular head and tibial-based (2-tailed) posterolateral corner reconstruction. Sports Med Arthrosc Rev. 2015;23:44–50. doi: 10.1097/JSA.0000000000000041. [DOI] [PubMed] [Google Scholar]
- 5.Strobel M.J., Schulz M.S., Petersen W.J., Eichhorn H.J. Combined anterior cruciate ligament, posterior cruciate ligament, and posterolateral corner reconstruction with autogenous hamstring grafts in chronic instabilities. Arthroscopy. 2006;22:182–192. doi: 10.1016/j.arthro.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Ahn J.H., Chung Y.S., Oh I. Arthroscopic posterior cruciate ligament reconstruction using the posterior trans-septal portal. Arthroscopy. 2003;19:101–107. doi: 10.1053/jars.2003.50017. [DOI] [PubMed] [Google Scholar]
- 7.Frosch K.H., Akoto R., Heitmann M., Enderle E., Giannakos A., Preiss A. Arthroscopic reconstruction of the popliteus complex: Accuracy and reproducibility of a new surgical technique. Knee Surg Sports Traumatol Arthrosc. 2015;23:3114–3120. doi: 10.1007/s00167-014-3000-y. [DOI] [PubMed] [Google Scholar]
- 8.Edson C.J., Fanelli G.C., Beck J.D. Rehabilitation after multiple-ligament reconstruction of the knee. Sports Med Arthrosc Rev. 2011;19:162–166. doi: 10.1097/JSA.0b013e31821918b2. [DOI] [PubMed] [Google Scholar]
- 9.Noyes F.R., Barber-Westin S.D., Albright J.C. An analysis of the causes of failure in 57 consecutive posterolateral operative procedures. Am J Sports Med. 2006;34:1419–1430. doi: 10.1177/0363546506287743. [DOI] [PubMed] [Google Scholar]
- 10.Freychet B., Sonnery-Cottet B., Dutra Vieira T., Sanders T.L., Kennedy N.I., Krych A.J., Stuart M.J., Levy B.A. Arthroscopic identification of the knee posterolateral corner structures: Technical Note–Part 2. Arthrosc Tech. 2020;9:e1985–e1992. doi: 10.1016/j.eats.2020.08.033. 019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
All-arthroscopic treatment of combined PCL and PLC instability using the trans-septal approach is shown in a right knee in the supine position.
All-arthroscopic treatment of combined PCL and PLC instability using the trans-septal approach is shown in a right knee in the supine position.