Abstract
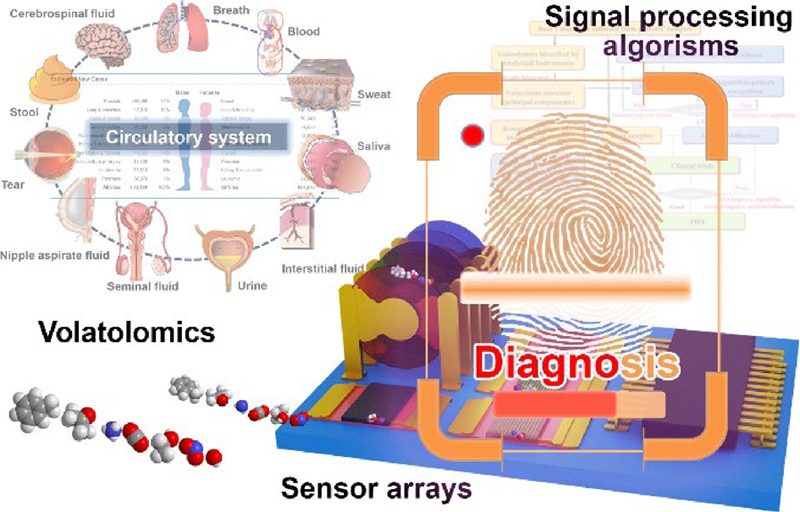
Various diseases increasingly challenge the health status and life quality of human beings. Volatolome emitted from patients has been considered as a potential family of markers, volatolomics, for diagnosis/screening. There are two fundamental issues of volatolomics in healthcare. On one hand, the solid relationship between the volatolome and specific diseases needs to be clarified and verified. On the other hand, effective methods should be explored for the precise detection of volatolome. Several comprehensive review articles had been published in this field. However, a timely and systematical summary and elaboration is still desired. In this review article, the research methodology of volatolomics in healthcare is critically considered and given out, at first. Then, the sets of volatolome according to specific diseases through different body sources and the analytical instruments for their identifications are systematically summarized. Thirdly, the advanced electronic nose and photonic nose technologies for volatile organic compounds (VOCs) detection are well introduced. The existed obstacles and future perspectives are deeply thought and discussed. This article could give a good guidance to researchers in this interdisciplinary field, not only understanding the cutting-edge detection technologies for doctors (medicinal background), but also making reference to clarify the choice of aimed VOCs during the sensor research for chemists, materials scientists, electronics engineers, etc.
Keywords: volatolomics, electronic nose, disease diagnosis, sensor, artificial olfaction, volatile organic compounds
Acknowledgements
This research is supported by National Numerical Windtunnel Project (No. NNW2020ZT2-A21), Marie Sklodowska-Curie Actions: Individual Fellowship (No. H2020-MSCA-IF) [898486], Key Research and Development Program of Shaanxi (Nos. 2022ZDLSF01-04 and 2020GXLH-Y-012), the National Natural Science Foundation of China (No. 81972488), and the Shenzhen Science and Technology Program (No. JCYJ20210324115209026).
Footnotes
Wenwen Hu, Weiwei Wu, and Yingying Jian contributed equally to this work.
Contributor Information
Yun Qian, Email: qianyun1985@zju.edu.cn.
Miaomiao Yuan, Email: mingshuiyao@gmail.com.
Mingshui Yao, Email: yuanmm3@mail.sysu.edu.cn.
References
- [1].GBD 2019 diseasesinjuries collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the global burden of disease study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Siegel R L, Miller K D, Fuchs H E, Jemal A. Cancer statistics, 2022. CA: Cancer J. Clin. 2022;72:7–33. doi: 10.3322/caac.21708. [DOI] [PubMed] [Google Scholar]
- [3].Gould M K, Huang B Z, Tammemagi M C, Kinar Y, Shiff R. Machine learning for early lung cancer identification using routine clinical and laboratory data. Am. J. Respir. Crit. Care Med. 2021;204:445–453. doi: 10.1164/rccm.202007-2791OC. [DOI] [PubMed] [Google Scholar]
- [4].Yang J S, Xu R Y, Wang C C, Qiu J D, Ren B, You L. Early screening and diagnosis strategies of pancreatic cancer: A comprehensive review. Cancer Commun. 2021;41:1257–1274. doi: 10.1002/cac2.12204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Acharya B, Acharya A, Gautam S, Ghimire S P, Mishra G, Parajuli N, Sapkota B. Advances in diagnosis of tuberculosis: An update into molecular diagnosis of Mycobacterium tuberculosis. Mol. Biol. Rep. 2020;47:4065–4075. doi: 10.1007/s11033-020-05413-7. [DOI] [PubMed] [Google Scholar]
- [6].Vandenberg O, Martiny D, Rochas O, van Belkum A, Kozlakidis Z. Considerations for diagnostic COVID-19 tests. Nat. Rev. Microbiol. 2021;19:171–183. doi: 10.1038/s41579-020-00461-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ito E, Iha K, Yoshimura T, Nakaishi K, Watabe S. Early diagnosis with ultrasensitive ELISA. Adv. Clin. Chem. 2021;101:121–133. doi: 10.1016/bs.acc.2020.06.002. [DOI] [PubMed] [Google Scholar]
- [8].Afzal A. Molecular diagnostic technologies for COVID-19: Limitations and challenges. J. Adv. Res. 2020;26:149–159. doi: 10.1016/j.jare.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Pagana K D, Pagana T J, Pagana T N. Mosby’s Diagnostic and Laboratory Test Reference. 14th ed. St. Louis: Elsevier; 2019. [Google Scholar]
- [10].Herring W. Learning Radiology: Recognizing the Basics. 4th ed. Philadelphia: Elsevier; 2019. [Google Scholar]
- [11].Lamoureux C, Hanna T N, Sprecher D, Weber S, Callaway E. Radiologist errors by modality, anatomic region, and pathology for 1.6 million exams: What we have learned. Emerg. Radiol. 2021;28:1135–1141. doi: 10.1007/s10140-021-01959-6. [DOI] [PubMed] [Google Scholar]
- [12].Velusamy, P.; Su, C. H.; Ramasamy, P.; Arun, V.; Rajnish, N.; Raman, P.; Baskaralingam, V.; Senthil Kumar, S. M.; Gopinath, S. C. B. Volatile organic compounds as potential biomarkers for noninvasive disease detection by nanosensors: A comprehensive review. Crit. Rev. Anal. Chem., in press, 10.1080/10408347.2022.2043145. [DOI] [PubMed]
- [13].Zhong W H, Zhang X Y, Zeng Y X, Lin D J, Wu J. Recent applications and strategies in nanotechnology for lung diseases. Nano Res. 2021;14:2067–2089. doi: 10.1007/s12274-020-3180-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Zhang, S.; Pang, J. B.; Li, Y. F.; Yang, F.; Gemming, T.; Wang, K.; Wang, X.; Peng, S.; Liu, X. Y.; Chang, B. et al. Emerging internet of things driven carbon nanotubes-based devices. Nano Res., in press, 10.1007/s12274-021-3986-7.
- [15].Ruddy E N, Carroll L A. Select the best VOC control strategy. Chem. Eng. Prog. 1993;89:28–35. [Google Scholar]
- [16].Kesselmeier J, Staudt M. Biogenic volatile organic compounds (VOC): An overview on emission, physiology and ecology. J. Atmos. Chem. 1999;33:23–88. doi: 10.1023/A:1006127516791. [DOI] [Google Scholar]
- [17].Kukkar D, Vellingiri K, Kaur R, Bhardwaj S K, Deep A, Kim K H. Nanomaterials for sensing of formaldehyde in air: Principles, applications, and performance evaluation. Nano Res. 2019;12:225–246. doi: 10.1007/s12274-018-2207-5. [DOI] [Google Scholar]
- [18].Zhang J, Tian Y H, Luo Z W, Qian C, Li W W, Duan Y X. Breath volatile organic compound analysis: An emerging method for gastric cancer detection. J. Breath Res. 2021;15:044002. doi: 10.1088/1752-7163/ac2cde. [DOI] [PubMed] [Google Scholar]
- [19].Zhong X H, Li D, Du W, Yan M Q, Wang Y, Huo D Q, Hou C J. Rapid recognition of volatile organic compounds with colorimetric sensor arrays for lung cancer screening. Anal. Bioanal. Chem. 2018;410:3671–3681. doi: 10.1007/s00216-018-0948-3. [DOI] [PubMed] [Google Scholar]
- [20].Buszewski B, Kęsy M, Ligor T, Amann A. Human exhaled air analytics: Biomarkers of diseases. Biomed. Chromatogr. 2007;21:553–566. doi: 10.1002/bmc.835. [DOI] [PubMed] [Google Scholar]
- [21].Zhu B, Wang H C. Diagnostics of Traditional Chinese Medicine. London: Singing Dragon; 2010. [Google Scholar]
- [22].Corradi M, Mutti A. News from the breath analysis summit 2011. J. Breath Res. 2012;6:020201. doi: 10.1088/1752-7155/6/2/020201. [DOI] [PubMed] [Google Scholar]
- [23].Dima A C, Balaban D V, Dima A. Diagnostic application of volatile organic compounds as potential biomarkers for detecting digestive neoplasia: A systematic review. Diagnostics. 2021;11:2317. doi: 10.3390/diagnostics11122317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Vishinkin R, Busool R, Mansour E, Fish F, Esmail A, Kumar P, Gharaa A, Cancilla J C, Torrecilla J S, Skenders G, et al. Profiles of volatile biomarkers detect tuberculosis from skin. Adv. Sci. 2021;8:2100235. doi: 10.1002/advs.202100235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].da Costa B R B, De Martinis B S. Analysis of urinary VOCs using mass spectrometric methods to diagnose cancer: A review. Clin. Mass Spectrom. 2020;18:27–37. doi: 10.1016/j.clinms.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Janssens E, van Meerbeeck J P, Lamote K. Volatile organic compounds in human matrices as lung cancer biomarkers: A systematic review. Crit. Rev. Oncol. Hematol. 2020;153:103037. doi: 10.1016/j.critrevonc.2020.103037. [DOI] [PubMed] [Google Scholar]
- [27].Van Malderen K, De Winter B Y, De Man J G, De Schepper H U, Lamote K. Volatomics in inflammatory bowel disease and irritable bowel syndrome. EBioMedicine. 2020;54:102725. doi: 10.1016/j.ebiom.2020.102725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Broza Y Y, Zhou X, Yuan M M, Qu D Y, Zheng Y B, Vishinkin R, Khatib M, Wu W W, Haick H. Disease detection with molecular biomarkers: From chemistry of body fluids to nature-inspired chemical sensors. Chem. Rev. 2019;119:11761–11817. doi: 10.1021/acs.chemrev.9b00437. [DOI] [PubMed] [Google Scholar]
- [29].Krilaviciute A, Heiss J A, Leja M, Kupcinskas J, Hawick H, Brenner H. Detection of cancer through exhaled breath: A systematic review. Oncotarget. 2015;6:38643–38657. doi: 10.18632/oncotarget.5938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hakim M, Broza Y Y, Barash O, Peled N, Phillips M, Amann A, Haick H. Volatile organic compounds of lung cancer and possible biochemical pathways. Chem. Rev. 2012;112:5949–5966. doi: 10.1021/cr300174a. [DOI] [PubMed] [Google Scholar]
- [31].Broza Y Y, Vishinkin R, Barash O, Nakhleh M K, Haick H. Synergy between nanomaterials and volatile organic compounds for non-invasive medical evaluation. Chem. Soc. Rev. 2018;47:4781–4859. doi: 10.1039/C8CS00317C. [DOI] [PubMed] [Google Scholar]
- [32].Haick H, Broza Y Y, Mochalski P, Ruzsanyi V, Amann A. Assessment, origin, and implementation of breath volatile cancer markers. Chem. Soc. Rev. 2014;43:1423–1449. doi: 10.1039/C3CS60329F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Van den Velde S, Nevens F, Van Hee P, van Steenberghe D, Quirynen M. GC-MS analysis of breath odor compounds in liver patients. J. Chromatogr. B: Analyt. Technol. Biomed. Life Sci. 2008;875:344–348. doi: 10.1016/j.jchromb.2008.08.031. [DOI] [PubMed] [Google Scholar]
- [34].Lubes G, Goodarzi M. GC-MS based metabolomics used for the identification of cancer volatile organic compounds as biomarkers. J. Pharm. Biomed. Anal. 2018;147:313–322. doi: 10.1016/j.jpba.2017.07.013. [DOI] [PubMed] [Google Scholar]
- [35].Mentana A, Camele I, Mang S M, De Benedetto G E, Frisullo S, Centonze D. Volatolomics approach by HS-SPME-GC-MS and multivariate analysis to discriminate olive tree varieties infected by Xylella fastidiosa. Phytochem. Anal. 2019;30:623–634. doi: 10.1002/pca.2835. [DOI] [PubMed] [Google Scholar]
- [36].Choi M J, Oh C H. 2nd dimensional GC-MS analysis of sweat volatile organic compounds prepared by solid phase microextraction. Technol. Health Care. 2014;22:481–488. doi: 10.3233/THC-140807. [DOI] [PubMed] [Google Scholar]
- [37].Gruber B, Keller S, Groeger T, Matuschek G, Szymczak W, Zimmermann R. Breath gas monitoring during a glucose challenge by a combined PTR-QMS/GC×GC-TOFMS approach for the verification of potential volatile biomarkers. J. Breath Res. 2016;10:036003. doi: 10.1088/1752-7155/10/3/036003. [DOI] [PubMed] [Google Scholar]
- [38].Rudnicka J, Kowalkowski T, Ligor T, Buszewski B. Determination of volatile organic compounds as biomarkers of lung cancer by SPME-GC-TOF/MS and chemometrics. J. Chromatogr. B: Analyt. Technol. Biomed. Life Sci. 2011;879:3360–3366. doi: 10.1016/j.jchromb.2011.09.001. [DOI] [PubMed] [Google Scholar]
- [39].Stefanuto P H, Zanella D, Vercammen J, Henket M, Schleich F, Louis R, Focant J F. Multimodal combination of GC × GC-HRTOFMS and SIFT-MS for asthma phenotyping using exhaled breath. Sci. Rep. 2020;10:16159. doi: 10.1038/s41598-020-73408-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Yang J, Li Y J, Liu Q Q, Li L, Feng A Z, Wang T Y, Zheng S, Xu A D, Lyu J. Brief introduction of medical database and data mining technology in big data era. J. Evid. Based Med. 2020;13:57–69. doi: 10.1111/jebm.12373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Peng G, Tisch U, Adams O, Hakim M, Shehada N, Broza Y Y, Billan S, Abdah-Bortnyak R, Kuten A, Haick H. Diagnosing lung cancer in exhaled breath using gold nanoparticles. Nat. Nanotechnol. 2009;4:669–673. doi: 10.1038/nnano.2009.235. [DOI] [PubMed] [Google Scholar]
- [42].Liu K, Shang C D, Wang Z L, Qi Y Y, Miao R, Liu K Q, Liu T H, Fang Y. Non-contact identification and differentiation of illicit drugs using fluorescent films. Nat. Commun. 2018;9:1695. doi: 10.1038/s41467-018-04119-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Hu W W, Wan L T, Jian Y Y, Ren C, Jin K, Su X H, Bai X X, Haick H, Yao M S, Wu W W. Electronic noses: From advanced materials to sensors aided with data processing. Adv. Mater. Technol. 2019;4:1800488. [Google Scholar]
- [44].Broza Y Y, Zuri L, Haick H. Combined volatolomics for monitoring of human body chemistry. Sci. Rep. 2014;4:4611. doi: 10.1038/srep04611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Xu Z Q, Broza Y Y, Ionsecu R, Tisch U, Ding L, Liu H, Song Q, Pan Y Y, Xiong F X, Gu K S, et al. A nanomaterial-based breath test for distinguishing gastric cancer from benign gastric conditions. Br. J. Cancer. 2013;108:941–950. doi: 10.1038/bjc.2013.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Amal H, Ding L, Liu B B, Tisch U, Xu Z Q, Shi D Y, Zhao Y, Chen J, Sun R X, Liu H, et al. The scent fingerprint of hepatocarcinoma: In-vitro metastasis prediction with volatile organic compounds (VOCS) Int. J. Nanomedicine. 2012;7:4135–4146. doi: 10.2147/IJN.S32680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Xue R Y, Dong L, Zhang S, Deng C H, Liu T T, Wang J Y, Shen X Z. Investigation of volatile biomarkers in liver cancer blood using solid-phase microextraction and gas chromatography/mass spectrometry. Rapid Commun. Mass Spectrom. 2008;22:1181–1186. doi: 10.1002/rcm.3466. [DOI] [PubMed] [Google Scholar]
- [48].Hakim M, Billan S, Tisch U, Peng G, Dvrokind I, Marom O, Abdah-Bortnyak R, Kuten A, Haick H. Diagnosis of head-and-neck cancer from exhaled breath. Br. J. Cancer. 2011;104:1649–1655. doi: 10.1038/bjc.2011.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Peng G, Hakim M, Broza Y Y, Billan S, Abdah-Bortnyak R, Kuten A, Tisch U, Haick H. Detection of lung, breast, colorectal, and prostate cancers from exhaled breath using a single array of nanosensors. Br. J. Cancer. 2010;103:542–551. doi: 10.1038/sj.bjc.6605810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Phillips M, Altorki N, Austin J H M, Cameron R B, Cataneo R N, Kloss R, Maxfield R A, Munawar M I, Pass H I, Rashid A, et al. Detection of lung cancer using weighted digital analysis of breath biomarkers. Clin. Chim. Acta. 2008;393:76–84. doi: 10.1016/j.cca.2008.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Phillips M, Cataneo R N, Ditkoff B A, Fisher P, Greenberg J, Gunawardena R, Kwon C S, Rahbari-Oskoui F, Wong C. Volatile markers of breast cancer in the breath. Breast J. 2003;9:184–191. doi: 10.1046/j.1524-4741.2003.09309.x. [DOI] [PubMed] [Google Scholar]
- [52].Phillips M, Cataneo R N, Ditkoff B A, Fisher P, Greenberg J, Gunawardena R, Kwon C S, Tietje O, Wong C. Prediction of breast cancer using volatile biomarkers in the breath. Breast Cancer Res. Treat. 2006;99:19–21. doi: 10.1007/s10549-006-9176-1. [DOI] [PubMed] [Google Scholar]
- [53].Phillips M, Cataneo R N, Saunders C, Hope P, Schmitt P, Wai J. Volatile biomarkers in the breath of women with breast cancer. J. Breath Res. 2010;4:026003. doi: 10.1088/1752-7155/4/2/026003. [DOI] [PubMed] [Google Scholar]
- [54].Poli D, Carbognani P, Corradi M, Goldoni M, Acampa O, Balbi B, Bianchi L, Rusca M, Mutti A. Exhaled volatile organic compounds in patients with non-small cell lung cancer: Cross sectional and nested short-term follow-up study. Respir. Res. 2005;6:71. doi: 10.1186/1465-9921-6-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Fuchs P, Loeseken C, Schubert J K, Miekisch W. Breath gas aldehydes as biomarkers of lung cancer. Int. J. Cancer. 2010;126:2663–2670. doi: 10.1002/ijc.24970. [DOI] [PubMed] [Google Scholar]
- [56].Broza Y Y, Kremer R, Tisch U, Gevorkyan A, Shiban A, Best L A, Haick H. A nanomaterial-based breath test for short-term follow-up after lung tumor resection. Nanomedicine. 2013;9:15–21. doi: 10.1016/j.nano.2012.07.009. [DOI] [PubMed] [Google Scholar]
- [57].Gaspar E M, Lucena A F, Duro da Costa J, Chaves das Neves H. Organic metabolites in exhaled human breath—A multivariate approach for identification of biomarkers in lung disorders. J. Chromatogr. A. 2009;1216:2749–2756. doi: 10.1016/j.chroma.2008.10.125. [DOI] [PubMed] [Google Scholar]
- [58].Song G, Qin T, Liu H, Xu G B, Pan Y Y, Xiong F X, Gu K S, Sun G P, Chen Z D. Quantitative breath analysis of volatile organic compounds of lung cancer patients. Lung Cancer. 2010;67:227–231. doi: 10.1016/j.lungcan.2009.03.029. [DOI] [PubMed] [Google Scholar]
- [59].Barash O, Peled N, Hirsch F R, Haick H. Sniffing the unique “odor print” of non-small-cell lung cancer with gold nanoparticles. Small. 2009;5:2618–2624. doi: 10.1002/smll.200900937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Davies M P A, Barash O, Jeries R, Peled N, Ilouze M, Hyde R, Marcus M W, Field J K, Haick H. Unique volatolomic signatures of TP53 and KRAS in lung cells. Br. J. Cancer. 2014;111:1213–1221. doi: 10.1038/bjc.2014.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Chen X, Xu F J, Wang Y, Pan Y F, Lu D J, Wang P, Ying K J, Chen E G, Zhang W M. A study of the volatile organic compounds exhaled by lung cancer cells in vitro for breath diagnosis. Cancer. 2007;110:835–844. doi: 10.1002/cncr.22844. [DOI] [PubMed] [Google Scholar]
- [62].Filipiak W, Sponring A, Filipiak A, Ager C, Schubert J, Miekisch W, Amann A, Troppmair J. TD-GC-MS analysis of volatile metabolites of human lung cancer and normal cells in vitro. Cancer Epidemiol. Biomarkers Prev. 2010;19:182–195. doi: 10.1158/1055-9965.EPI-09-0162. [DOI] [PubMed] [Google Scholar]
- [63].Amal H, Leja M, Funka K, Skapars R, Sivins A, Ancans G, Liepniece-Karele I, Kikuste I, Lasina I, Haick H. Detection of precancerous gastric lesions and gastric cancer through exhaled breath. Gut. 2016;65:400–407. doi: 10.1136/gutjnl-2014-308536. [DOI] [PubMed] [Google Scholar]
- [64].Hicks L C, Huang J Z, Kumar S, Powles S T, Orchard T R, Hanna G B, Williams H R T. Analysis of exhaled breath volatile organic compounds in inflammatory bowel disease: A pilot study. J. Crohns Colitis. 2015;9:731–737. doi: 10.1093/ecco-jcc/jjv102. [DOI] [PubMed] [Google Scholar]
- [65].Karban A, Nakhleh M K, Cancilla J C, Vishinkin R, Rainis T, Koifman E, Jeries R, Ivgi H, Torrecilla J S, Haick H. Programmed nanoparticles for tailoring the detection of inflammatory bowel diseases and irritable bowel syndrome disease via breathprint. Adv. Healthc. Mater. 2016;5:2339–2344. doi: 10.1002/adhm.201600588. [DOI] [PubMed] [Google Scholar]
- [66].Winlaw D S, Keogh A M, Schyvens C G, Spratt P M, Macdonald P S, Smythe G A. Increased nitric oxide production in heart failure. Lancet. 1994;344:373–374. doi: 10.1016/S0140-6736(94)91403-6. [DOI] [PubMed] [Google Scholar]
- [67].Pijls K E, Smolinska A, Jonkers D M A E, Dallinga J W, Masclee A A M, Koek G H, van Schooten F J. A profile of volatile organic compounds in exhaled air as a potential non-invasive biomarker for liver cirrhosis. Sci. Rep. 2016;6:19903. doi: 10.1038/srep19903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Chen S, Zieve L, Mahadevan V. Mercaptans and dimethyl sulfide in the breath of patients with cirrhosis of the liver. Effect of feeding methionine. J. Lab. Clin. Med. 1970;75:628–635. [PubMed] [Google Scholar]
- [69].Kaji H, Hisamura M, Saito N, Murao M. Gas chromatographic determination of volatile sulfur compounds in the expired alveolar air in hepatopathic subjects. J. Chromatogr. 1978;145:464–468. doi: 10.1016/S0378-4347(00)81377-8. [DOI] [PubMed] [Google Scholar]
- [70].Cikach F S, Jr., Tonelli A R, Barnes J, Paschke K, Newman J, Grove D, Dababneh L, Wang S H, Dweik R A. Breath analysis in pulmonary arterial hypertension. Chest. 2014;145:551–558. doi: 10.1378/chest.13-1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Mansoor J K, Schelegle E S, Davis C E, Walby W F, Zhao W X, Aksenov A A, Pasamontes A, Figueroa J, Allen R. Analysis of volatile compounds in exhaled breath condensate in patients with severe pulmonary arterial hypertension. PLoS One. 2014;9:e95331. doi: 10.1371/journal.pone.0095331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Phillips M, Cataneo R N, Condos R, Ring Erickson G A, Greenberg J, La Bombardi V, Munawar M I, Tietje O. Volatile biomarkers of pulmonary tuberculosis in the breath. Tuberculosis. 2007;87:44–52. doi: 10.1016/j.tube.2006.03.004. [DOI] [PubMed] [Google Scholar]
- [73].Tangerman A, Winkel E G. Extra-oral halitosis: An overview. J. Breath Res. 2010;4:017003. doi: 10.1088/1752-7155/4/1/017003. [DOI] [PubMed] [Google Scholar]
- [74].Avincsal M O, Altundag A, Ulusoy S, Dinc M E, Dalgic A, Topak M. Halitosis associated volatile sulphur compound levels in patients with laryngopharyngeal reflux. Eur. Arch. Otorhinolaryngol. 2016;273:1515–1520. doi: 10.1007/s00405-016-3961-1. [DOI] [PubMed] [Google Scholar]
- [75].Corradi M, Rubinstein I, Andreoli R, Manini P, Caglieri A, Poli D, Alinovi R, Mutti A. Aldehydes in exhaled breath condensate of patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2003;167:1380–1386. doi: 10.1164/rccm.200210-1253OC. [DOI] [PubMed] [Google Scholar]
- [76].Van Berkel J J B N, Dallinga J W, Möller G M, Godschalk R W L, Moonen E J, Wouters E F M, Van Schooten F J. A profile of volatile organic compounds in breath discriminates COPD patients from controls. Respir. Med. 2010;104:557–563. doi: 10.1016/j.rmed.2009.10.018. [DOI] [PubMed] [Google Scholar]
- [77].Paredi P, Kharitonov S A, Leak D, Ward S, Cramer D, Barnes P J. Exhaled ethane, a marker of lipid peroxidation, is elevated in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2000;162:369–373. doi: 10.1164/ajrccm.162.2.9909025. [DOI] [PubMed] [Google Scholar]
- [78].Aksenov A A, Gojova A, Zhao W X, Morgan J T, Sankaran S, Sandrock C E, Davis C E. Characterization of volatile organic compounds in human leukocyte antigen heterologous expression systems: A cell’s “chemical odor fingerprint”. ChemBioChem. 2012;13:1053–1059. doi: 10.1002/cbic.201200011. [DOI] [PubMed] [Google Scholar]
- [79].Halliwell B, Gutteridge J M, Cross C E. Free radicals, antioxidants, and human disease: Where are we now? J. Lab. Clin. Med. 1992;119:598–620. [PubMed] [Google Scholar]
- [80].Broza Y Y, Mochalski P, Ruzsanyi V, Amann A, Haick H. Hybrid volatolomics and disease detection. Angew. Chem., Int. Ed. 2015;54:11036–11048. doi: 10.1002/anie.201500153. [DOI] [PubMed] [Google Scholar]
- [81].Opitz P, Herbarth O. The volatilome-investigation of volatile organic metabolites (VOM) as potential tumor markers in patients with head and neck squamous cell carcinoma (HNSCC) J. Otolaryngol. Head Neck Surg. 2018;47:42. doi: 10.1186/s40463-018-0288-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Cauchi M, Weber C M, Bolt B J, Spratt P B, Bessant C, Turner D C, Willis C M, Britton L E, Turner C, Morgan G. Evaluation of gas chromatography mass spectrometry and pattern recognition for the identification of bladder cancer from urine headspace. Anal. Methods. 2016;8:4037–4046. doi: 10.1039/C6AY00400H. [DOI] [Google Scholar]
- [83].Guadagni R, Miraglia N, Simonelli A, Silvestre A, Lamberti M, Feola D, Acampora A, Sannolo N. Solid-phase microextraction-gas chromatography-mass spectrometry method validation for the determination of endogenous substances: Urinary hexanal and heptanal as lung tumor biomarkers. Anal. Chim. Acta. 2011;701:29–36. doi: 10.1016/j.aca.2011.05.035. [DOI] [PubMed] [Google Scholar]
- [84].Hanai Y, Shimono K, Matsumura K, Vachani A, Albelda S, Yamazaki K, Beauchamp G K, Oka H. Urinary volatile compounds as biomarkers for lung cancer. Biosci. Biotechnol. Biochem. 2012;76:679–684. doi: 10.1271/bbb.110760. [DOI] [PubMed] [Google Scholar]
- [85].Yang Q, Shi X Z, Wang Y, Wang W Z, He H B, Lu X, Xu G W. Urinary metabonomic study of lung cancer by a fully automatic hyphenated hydrophilic interaction/RPLC-MS system. J. Sep. Sci. 2010;33:1495–1503. doi: 10.1002/jssc.200900798. [DOI] [PubMed] [Google Scholar]
- [86].Banday K M, Pasikanti K K, Chan E C Y, Singla R, Rao K V S, Chauhan V S, Nanda R K. Use of urine volatile organic compounds to discriminate tuberculosis patients from healthy subjects. Anal. Chem. 2011;83:5526–5534. doi: 10.1021/ac200265g. [DOI] [PubMed] [Google Scholar]
- [87].Dospinescu V M, Tiele A, Covington J A. Sniffing out urinary tract infection—Diagnosis based on volatile organic compounds and smell profile. Biosensors. 2020;10:83. doi: 10.3390/bios10080083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Yang H, Kim D, Kim J, Moon D, Song H S, Lee M, Hong S, Park T H. Nanodisc-based bioelectronic nose using olfactory receptor produced in Escherichia coli for the assessment of the death-associated odor cadaverine. ACS Nano. 2017;11:11847–11855. doi: 10.1021/acsnano.7b04992. [DOI] [PubMed] [Google Scholar]
- [89].Probert C S J, Ahmed I, Khalid T, Johnson E, Smith S, Ratcliffe N. Volatile organic compounds as diagnostic biomarkers in gastrointestinal and liver diseases. J. Gastrointestin. Liver Dis. 2009;18:337–343. [PubMed] [Google Scholar]
- [90].Cummings J H. Short chain fatty acids in the human colon. Gut. 1981;22:763–779. doi: 10.1136/gut.22.9.763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].Yokoyama M T, Carlson J R. Microbial metabolites of tryptophan in the intestinal tract with special reference to skatole. Am. J. Clin. Nutr. 1979;32:173–178. doi: 10.1093/ajcn/32.1.173. [DOI] [PubMed] [Google Scholar]
- [92].Lee J H, Karamychev V N, Kozyavkin S A, Mills D, Pavlov A R, Pavlova N V, Polouchine N N, Richardson P M, Shakhova V V, Slesarev A I, et al. Comparative genomic analysis of the gut bacterium Bifidobacterium longum reveals loci susceptible to deletion during pure culture growth. BMC Genomics. 2008;9:247. doi: 10.1186/1471-2164-9-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Ahmed I, Greenwood R, de Lacy Costello B, Ratcliffe N M, Probert C S. An investigation of fecal volatile organic metabolites in irritable bowel syndrome. PLoS One. 2013;8:e58204. doi: 10.1371/journal.pone.0058204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [94].Bannaga A S, Farrugia A, Arasaradnam R P. Diagnosing inflammatory bowel disease using noninvasive applications of volatile organic compounds: A systematic review. Expert Rev. Gastroenterol. Hepatol. 2019;13:1113–1122. doi: 10.1080/17474124.2019.1685873. [DOI] [PubMed] [Google Scholar]
- [95].Homann N. Alcohol and upper gastrointestinal tract cancer: The role of local acetaldehyde production. Addict. Biol. 2001;6:309–323. doi: 10.1080/13556210020077028. [DOI] [PubMed] [Google Scholar]
- [96].Studer S M, Orens J B, Rosas I, Krishnan J A, Cope K A, Yang S, Conte J V, Becker P B, Risby T H. Patterns and significance of exhaled-breath biomarkers in lung transplant recipients with acute allograft rejection. J. Heart Lung Transplant. 2001;20:1158–1166. doi: 10.1016/S1053-2498(01)00343-6. [DOI] [PubMed] [Google Scholar]
- [97].Tisch U, Schlesinger I, Ionescu R, Nassar M, Axelrod N, Robertman D, Tessler Y, Azar F, Marmur A, Aharon-Peretz J, et al. Detection of Alzheimer’s and Parkinson’s disease from exhaled breath using nanomaterial-based sensors. Nanomedicine. 2013;8:43–56. doi: 10.2217/nnm.12.105. [DOI] [PubMed] [Google Scholar]
- [98].Paredi P, Kharitonov S A, Barnes P J. Elevation of exhaled ethane concentration in asthma. Am. J. Respir. Crit. Care Med. 2000;162:1450–1454. doi: 10.1164/ajrccm.162.4.2003064. [DOI] [PubMed] [Google Scholar]
- [99].Olopade C O, Zakkar M, Swedler W I, Rubinstein I. Exhaled pentane levels in acute asthma. Chest. 1997;111:862–865. doi: 10.1378/chest.111.4.862. [DOI] [PubMed] [Google Scholar]
- [100].Hunt J F, Erwin E, Palmer L, Vaughan J, Malhotra N, Platts-Mills T A E, Gaston B. Expression and activity of pH-regulatory glutaminase in the human airway epithelium. Am. J. Respir. Crit. Care Med. 2002;165:101–107. doi: 10.1164/ajrccm.165.1.2104131. [DOI] [PubMed] [Google Scholar]
- [101].Ashutosh K. Nitric oxide and asthma: A review. Curr. Opin. Pulm. Med. 2000;6:21–25. doi: 10.1097/00063198-200001000-00005. [DOI] [PubMed] [Google Scholar]
- [102].Kharitonov S A, Yates D, Robbins R A, Barnes P J, Logan-Sinclair R, Shinebourne E A. Increased nitric oxide in exhaled air of asthmatic patients. Lancet. 1994;343:133–135. doi: 10.1016/S0140-6736(94)90931-8. [DOI] [PubMed] [Google Scholar]
- [103].Persson M G, Gustafsson L E, Zetterström O, Agrenius V, Ihre E. Single-breath nitric oxide measurements in asthmatic patients and smokers. Lancet. 1994;343:146–147. doi: 10.1016/S0140-6736(94)90935-0. [DOI] [PubMed] [Google Scholar]
- [104].Montuschi P, Corradi M, Ciabattoni G, Nightingale J, Kharitonov S A, Barnes P J. Increased 8-isoprostane, a marker of oxidative stress, in exhaled condensate of asthma patients. Am. J. Respir. Crit. Care Med. 1999;160:216–220. doi: 10.1164/ajrccm.160.1.9809140. [DOI] [PubMed] [Google Scholar]
- [105].Horváth I, Donnelly L E, Kiss A, Kharitonov S A, Lim S, Chung K F, Barnes P J. Combined use of exhaled hydrogen peroxide and nitric oxide in monitoring asthma. Am. J. Respir. Crit. Care Med. 1998;158:1042–1046. doi: 10.1164/ajrccm.158.4.9710091. [DOI] [PubMed] [Google Scholar]
- [106].Marom O, Nakhoul F, Tisch U, Shiban A, Abassi Z, Haick H. Gold nanoparticle sensors for detecting chronic kidney disease and disease progression. Nanomedicine. 2012;7:639–650. doi: 10.2217/nnm.11.135. [DOI] [PubMed] [Google Scholar]
- [107].Simenhoff M L, Burke J F, Saukkonen J J, Ordinario A T, Doty R, Dunn S. Biochemical profile of uremic breath. N. Engl. J. Med. 1977;297:132–135. doi: 10.1056/NEJM197707212970303. [DOI] [PubMed] [Google Scholar]
- [108].Altomare D F, Di Lena M, Porcelli F, Trizio L, Travaglio E, Tutino M, Dragonieri S, Memeo V, de Gennaro G. Exhaled volatile organic compounds identify patients with colorectal cancer. Br. J. Surg. 2013;100:144–150. doi: 10.1002/bjs.8942. [DOI] [PubMed] [Google Scholar]
- [109].McCurdy M R, Sharafkhaneh A, Abdel-Monem H, Rojo J, Tittel F K. Exhaled nitric oxide parameters and functional capacity in chronic obstructive pulmonary disease. J. Breath Res. 2011;5:016003. doi: 10.1088/1752-7155/5/1/016003. [DOI] [PubMed] [Google Scholar]
- [110].Dekhuijzen P N, Aben K K, Dekker I, Aarts L P, Wielders P L, Van Herwaarden C L, Bast A. Increased exhalation of hydrogen peroxide in patients with stable and unstable chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 1996;154:813–816. doi: 10.1164/ajrccm.154.3.8810624. [DOI] [PubMed] [Google Scholar]
- [111].Balfour-Lynn I M, Laverty A, Dinwiddie R. Reduced upper airway nitric oxide in cystic fibrosis. Arch. Dis. Child. 1996;75:319–322. doi: 10.1136/adc.75.4.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [112].Thomas S R, Kharitonov S A, Scott S F, Hodson M E, Barnes P J. Nasal and exhaled nitric oxide is reduced in adult patients with cystic fibrosis and does not correlate with cystic fibrosis genotype. Chest. 2000;117:1085–1089. doi: 10.1378/chest.117.4.1085. [DOI] [PubMed] [Google Scholar]
- [113].Kamboures M A, Blake D R, Cooper D M, Newcomb R L, Barker M, Larson J K, Meinardi S, Nussbaum E, Rowland F S. Breath sulfides and pulmonary function in cystic fibrosis. Proc. Natl. Acad. Sci. USA. 2005;102:15762–15767. doi: 10.1073/pnas.0507263102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [114].Galassetti P R, Novak B, Nemet D, Rose-Gottron C, Cooper D M, Meinardi S, Newcomb R, Zaldivar F, Blake D R. Breath ethanol and acetone as indicators of serum glucose levels: An initial report. Diabetes Technol. Ther. 2005;7:115–123. doi: 10.1089/dia.2005.7.115. [DOI] [PubMed] [Google Scholar]
- [115].Novak B J, Blake D R, Meinardi S, Rowland F S, Pontello A, Cooper D M, Galassetti P R. Exhaled methyl nitrate as a noninvasive marker of hyperglycemia in type 1 diabetes. Proc. Natl. Acad. Sci. USA. 2007;104:15613–15618. doi: 10.1073/pnas.0706533104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [116].Pelli M A, Trovarelli G, Capodicasa E, De Medio G E, Bassotti G. Breath alkanes determination in ulcerative colitis and Crohn’s disease. Dis. Colon Rectum. 1999;42:71–76. doi: 10.1007/BF02235186. [DOI] [PubMed] [Google Scholar]
- [117].Kokoszka J, Nelson R L, Swedler W I, Skosey J, Abcarian H. Determination of inflammatory bowel disease activity by breath pentane analysis. Dis. Colon Rectum. 1993;36:597–601. doi: 10.1007/BF02049868. [DOI] [PubMed] [Google Scholar]
- [118].Phillips M, Boehmer J P, Cataneo R N, Cheema T, Eisen H J, Fallon J T, Fisher P E, Gass A, Greenberg J, Kobashigawa J, et al. Prediction of heart transplant rejection with a breath test for markers of oxidative stress. Am. J. Cardiol. 2004;94:1593–1594. doi: 10.1016/j.amjcard.2004.08.052. [DOI] [PubMed] [Google Scholar]
- [119].Hiroshi K, Masaya H, Nariyoshi S, Makoto M. Evaluation of volatile sulfur compounds in the expired alveolar gas in patients with liver cirrhosis. Clin. Chim. Acta. 1978;85:279–284. doi: 10.1016/0009-8981(78)90305-4. [DOI] [PubMed] [Google Scholar]
- [120].Tangerman A, Meuwese-Arends M T, van Tongeren J H M. A new sensitive assay for measuring volatile sulphur compounds in human breath by Tenax trapping and gas chromatography and its application in liver cirrhosis. Clin. Chim. Acta. 1983;130:103–110. doi: 10.1016/0009-8981(83)90263-2. [DOI] [PubMed] [Google Scholar]
- [121].Hisamura M. Quantitative analysis of methyl mercaptan and dimethyl sulfide in human expired alveolar gas and its clinical application: Study in normal subjects and patients with liver diseases. J. Jpn. Soc. Intern. Med. 1979;68:1284–1292. doi: 10.2169/naika.68.1284. [DOI] [PubMed] [Google Scholar]
- [122].Lee J, Ngo J, Blake D, Meinardi S, Pontello A M, Newcomb R, Galassetti P R. Improved predictive models for plasma glucose estimation from multi-linear regression analysis of exhaled volatile organic compounds. J. Appl. Physiol. 2009;107:155–160. doi: 10.1152/japplphysiol.91657.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [123].Miekisch W, Schubert J K, Noeldge-Schomburg G F E. Diagnostic potential of breath analysis—Focus on volatile organic compounds. Clin. Chim. Acta. 2004;347:25–39. doi: 10.1016/j.cccn.2004.04.023. [DOI] [PubMed] [Google Scholar]
- [124].Nakhleh M K, Amal H, Awad H, Gharra A, Abu-Saleh N, Jeries R, Haick H, Abassi Z. Sensor arrays based on nanoparticles for early detection of kidney injury by breath samples. Nanomedicine. 2014;10:1767–1776. doi: 10.1016/j.nano.2014.06.007. [DOI] [PubMed] [Google Scholar]
- [125].Ulanowska A, Kowalkowski T, Trawińska E, Buszewski B. The application of statistical methods using VOCs to identify patients with lung cancer. J. Breath Res. 2011;5:046008. doi: 10.1088/1752-7155/5/4/046008. [DOI] [PubMed] [Google Scholar]
- [126].Filipiak W, Filipiak A, Sponring A, Schmid T, Zelger B, Ager C, Klodzinska E, Denz H, Pizzini A, Lucciarini P, et al. Comparative analyses of volatile organic compounds (VOCs) from patients, tumors and transformed cell lines for the validation of lung cancer-derived breath markers. J. Breath Res. 2014;8:027111. doi: 10.1088/1752-7155/8/2/027111. [DOI] [PubMed] [Google Scholar]
- [127].Rudnicka J, Walczak M, Kowalkowski T, Jezierski T, Buszewski B. Determination of volatile organic compounds as potential markers of lung cancer by gas chromatography-mass spectrometry versus trained dogs. Sens. Actuators B: Chem. 2014;202:615–621. doi: 10.1016/j.snb.2014.06.006. [DOI] [Google Scholar]
- [128].Poli D, Goldoni M, Corradi M, Acampa O, Carbognani P, Internullo E, Casalini A, Mutti A. Determination of aldehydes in exhaled breath of patients with lung cancer by means of on-fiber-derivatisation SPME—GC/MS. J. Chromatogr. B: Analyt. Technol. Biomed. Life Sci. 2010;878:2643–2651. doi: 10.1016/j.jchromb.2010.01.022. [DOI] [PubMed] [Google Scholar]
- [129].Kischkel S, Miekisch W, Sawacki A, Straker E M, Trefz P, Amann A, Schubert J K. Breath biomarkers for lung cancer detection and assessment of smoking related effects—Confounding variables, influence of normalization and statistical algorithms. Clin. Chim. Acta. 2010;411:1637–1644. doi: 10.1016/j.cca.2010.06.005. [DOI] [PubMed] [Google Scholar]
- [130].Wehinger A, Schmid A, Mechtcheriakov S, Ledochowski M, Grabmer C, Gastl G A, Amann A. Lung cancer detection by proton transfer reaction mass-spectrometric analysis of human breath gas. Int. J. Mass Spectrom. 2007;265:49–59. doi: 10.1016/j.ijms.2007.05.012. [DOI] [Google Scholar]
- [131].Phillips M, Gleeson K, Hughes J M B, Greenberg J, Cataneo R N, Baker L, McVay W P. Volatile organic compounds in breath as markers of lung cancer: A cross-sectional study. Lancet. 1999;353:1930–1933. doi: 10.1016/S0140-6736(98)07552-7. [DOI] [PubMed] [Google Scholar]
- [132].Callol-Sanchez L, Munoz-Lucas M A, Gomez-Martin O, Maldonado-Sanz J A, Civera-Tejuca C, Gutierrez-Ortega C, Rodriguez-Trigo G, Jareno-Esteban J. Observation of nonanoic acid and aldehydes in exhaled breath of patients with lung cancer. J. Breath Res. 2017;11:026004. doi: 10.1088/1752-7163/aa6485. [DOI] [PubMed] [Google Scholar]
- [133].Phillips M, Cataneo R N, Cummin A R C, Gagliardi A J, Gleeson K, Greenberg J, Maxfield R A, Rom W N. Detection of lung cancer with volatile markers in the breath. Chest. 2003;123:2115–2123. doi: 10.1378/chest.123.6.2115. [DOI] [PubMed] [Google Scholar]
- [134].Oguma T, Nagaoka T, Kurahashi M, Kobayashi N, Yamamori S, Tsuji C, Takiguchi H, Niimi K, Tomomatsu H, Tomomatsu K, et al. Clinical contributions of exhaled volatile organic compounds in the diagnosis of lung cancer. PLoS One. 2017;12:e0174802. doi: 10.1371/journal.pone.0174802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [135].Phillips M, Altorki N, Austin J H M, Cameron R B, Cataneo R N, Greenberg J, Kloss R, Maxfield R A, Munawar M I, Pass H I, et al. Prediction of lung cancer using volatile biomarkers in breath. Cancer Biomark. 2007;3:95–109. doi: 10.3233/CBM-2007-3204. [DOI] [PubMed] [Google Scholar]
- [136].D’Amico A, Pennazza G, Santonico M, Martinelli E, Roscioni C, Galluccio G, Paolesse R, Di Natale C. An investigation on electronic nose diagnosis of lung cancer. Lung Cancer. 2010;68:170–176. doi: 10.1016/j.lungcan.2009.11.003. [DOI] [PubMed] [Google Scholar]
- [137].Bajtarevic A, Ager C, Pienz M, Klieber M, Schwarz K, Ligor M, Ligor T, Filipiak W, Denz H, Fiegl M, et al. Noninvasive detection of lung cancer by analysis of exhaled breath. BMC Cancer. 2009;9:348. doi: 10.1186/1471-2407-9-348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [138].Yu H, Xu L, Wang P. Solid phase microextraction for analysis of alkanes and aromatic hydrocarbons in human breath. J. Chromatogr. B: Analyt. Technol. Biomed. Life Sci. 2005;826:69–74. doi: 10.1016/j.jchromb.2005.08.013. [DOI] [PubMed] [Google Scholar]
- [139].Fu X A, Li M X, Knipp R J, Nantz M H, Bousamra M. Noninvasive detection of lung cancer using exhaled breath. Cancer Med. 2014;3:174–181. doi: 10.1002/cam4.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [140].Broza Y Y, Har-Shai L, Jeries R, Cancilla J C, Glass-Marmor L, Lejbkowicz I, Torrecilla J S, Yao X L, Feng X L, Narita A, et al. Exhaled breath markers for nonimaging and noninvasive measures for detection of multiple sclerosis. ACS Chem. Neurosci. 2017;8:2402–2413. doi: 10.1021/acschemneuro.7b00181. [DOI] [PubMed] [Google Scholar]
- [141].Ionescu R, Broza Y, Shaltieli H, Sadeh D, Zilberman Y, Feng X L, Glass-Marmor L, Lejbkowicz I, Müllen K, Miller A, et al. Detection of multiple sclerosis from exhaled breath using bilayers of polycyclic aromatic hydrocarbons and single-wall carbon nanotubes. ACS Chem. Neurosci. 2011;2:687–693. doi: 10.1021/cn2000603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [142].Tisch U, Aluf Y, Ionescu R, Nakhleh M, Bassal R, Axelrod N, Robertman D, Tessler Y, Finberg J P M, Haick H. Detection of asymptomatic nigrostriatal dopaminergic lesion in rats by exhaled air analysis using carbon nanotube sensors. ACS Chem. Neurosci. 2012;3:161–166. doi: 10.1021/cn200093r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [143].Assady S, Marom O, Hemli M, Ionescu R, Jeries R, Tisch U, Abassi Z, Haick H. Impact of hemodialysis on exhaled volatile organic compounds in end-stage renal disease: A pilot study. Nanomedicine. 2014;9:1035–1045. doi: 10.2217/nnm.13.85. [DOI] [PubMed] [Google Scholar]
- [144].Humad S, Zarling E, Clapper M, Skosey J L. Breath pentane excretion as a marker of disease activity in rheumatoid arthritis. Free Radic. Res. Commun. 1988;5:101–106. doi: 10.3109/10715768809066917. [DOI] [PubMed] [Google Scholar]
- [145].Phillips M, Sabas M, Greenberg J. Increased pentane and carbon disulfide in the breath of patients with schizophrenia. J. Clin. Pathol. 1993;46:861–864. doi: 10.1136/jcp.46.9.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [146].Wang C S, Dong R, Wang X Y, Lian A L, Chi C J, Ke C F, Guo L, Liu S S, Zhao W, Xu G W, et al. Exhaled volatile organic compounds as lung cancer biomarkers during one-lung ventilation. Sci. Rep. 2014;4:7312. doi: 10.1038/srep07312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [147].Di Lena M, Porcelli F, Altomare D F. Volatile organic compounds as new biomarkers for colorectal cancer: A review. Colorectal Dis. 2016;18:654–663. doi: 10.1111/codi.13271. [DOI] [PubMed] [Google Scholar]
- [148].Macfarlane G T, Cummings J H, Macfarlane S, Gibson G R. Influence of retention time on degradation of pancreatic enzymes by human colonic bacteria grown in a 3-stage continuous culture system. J. Appl. Bacteriol. 1989;67:521–527. doi: 10.1111/j.1365-2672.1989.tb02524.x. [DOI] [PubMed] [Google Scholar]
- [149].Woodmansey E J. Intestinal bacteria and ageing. J. Appl. Microbiol. 2007;102:1178–1186. doi: 10.1111/j.1365-2672.2007.03400.x. [DOI] [PubMed] [Google Scholar]
- [150].Navaneethan U, Parsi M A, Lourdusamy D, Grove D, Sanaka M R, Hammel J P, Vargo J J, Dweik R A. Volatile organic compounds in urine for noninvasive diagnosis of malignant biliary strictures: A pilot study. Dig. Dis. Sci. 2015;60:2150–2157. doi: 10.1007/s10620-015-3596-x. [DOI] [PubMed] [Google Scholar]
- [151].Silva C L, Passos M, Câmara J S. Investigation of urinary volatile organic metabolites as potential cancer biomarkers by solidphase microextraction in combination with gas chromatography-mass spectrometry. Br. J. Cancer. 2011;105:1894–1904. doi: 10.1038/bjc.2011.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [152].Wang D C, Wang C S, Pi X, Guo L, Wang Y, Li M J, Feng Y, Lin Z W, Hou W, Li E Y. Urinary volatile organic compounds as potential biomarkers for renal cell carcinoma. Biomed. Rep. 2016;5:68–72. doi: 10.3892/br.2016.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [153].Silva C L, Passos M, Câmara J S. Solid phase microextraction, mass spectrometry and metabolomic approaches for detection of potential urinary cancer biomarkers—A powerful strategy for breast cancer diagnosis. Talanta. 2012;89:360–368. doi: 10.1016/j.talanta.2011.12.041. [DOI] [PubMed] [Google Scholar]
- [154].Nam H, Chung B C, Kim Y, Lee K, Lee D. Combining tissue transcriptomics and urine metabolomics for breast cancer biomarker identification. Bioinformatics. 2009;25:3151–3157. doi: 10.1093/bioinformatics/btp558. [DOI] [PubMed] [Google Scholar]
- [155].Khalid T, Aggio R, White P, De Lacy Costello B, Persad R, Al-Kateb H, Jones P, Probert C S, Ratcliffe N. Urinary volatile organic compounds for the detection of prostate cancer. PLoS One. 2015;10:e0143283. doi: 10.1371/journal.pone.0143283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [156].Wang M G, Xie R J, Jia X B, Liu R C. Urinary volatile organic compounds as potential biomarkers in idiopathic membranous nephropathy. Med Princ. Pract. 2017;26:375–380. doi: 10.1159/000478782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [157].Abaffy T, Möller M, Riemer D D, Milikowski C, DeFazio R A. A case report-volatile metabolomic signature of malignant melanoma using matching skin as a control. J. Cancer Sci. Ther. 2011;3:140–144. doi: 10.4172/1948-5956.1000076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [158].Abaffy T, Duncan R, Riemer D D, Tietje O, Elgart G, Milikowski C, Defazio R A. Differential volatile signatures from skin, naevi and melanoma: A novel approach to detect a pathological process. PLoS One. 2010;5:e13813. doi: 10.1371/journal.pone.0013813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [159].Allardyce R A, Hill A L, Murdoch D R. The rapid evaluation of bacterial growth and antibiotic susceptibility in blood cultures by selected ion flow tube mass spectrometry. Diagn. Microbiol. Infect. Dis. 2006;55:255–261. doi: 10.1016/j.diagmicrobio.2006.01.031. [DOI] [PubMed] [Google Scholar]
- [160].Boots A W, Smolinska A, van Berkel J J B N, Fijten R R R, Stobberingh E E, Boumans M L L, Moonen E J, Wouters E F M, Dallinga J W, Van Schooten F J. Identification of microorganisms based on headspace analysis of volatile organic compounds by gas chromatography-mass spectrometry. J. Breath Res. 2014;8:027106. doi: 10.1088/1752-7155/8/2/027106. [DOI] [PubMed] [Google Scholar]
- [161].Preti G, Thaler E, Hanson C W, Troy M, Eades J, Gelperin A. Volatile compounds characteristic of sinus-related bacteria and infected sinus mucus: Analysis by solid-phase microextraction and gas chromatography-mass spectrometry. J. Chromatogr. B: Analyt. Technol. Biomed. Life Sci. 2009;877:2011–2018. doi: 10.1016/j.jchromb.2009.05.028. [DOI] [PubMed] [Google Scholar]
- [162].Zscheppank C, Wiegand H L, Lenzen C, Wingender J, Telgheder U. Investigation of volatile metabolites during growth of Escherichia coli and Pseudomonas aeruginosa by needle trap-GC-MS. Anal. Bioanal. Chem. 2014;406:6617–6628. doi: 10.1007/s00216-014-8111-2. [DOI] [PubMed] [Google Scholar]
- [163].Kunze N, Göpel J, Kuhns M, Jünger M, Quintel M, Perl T. Detection and validation of volatile metabolic patterns over different strains of two human pathogenic bacteria during their growth in a complex medium using multi-capillary column-ion mobility spectrometry (MCC-IMS) Appl. Microbiol. Biotechnol. 2013;97:3665–3676. doi: 10.1007/s00253-013-4762-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [164].Shestivska V, Nemec A, Dřevínek P, Sovová K, Dryahina K, Španěl P. Quantification of methyl thiocyanate in the headspace of Pseudomonas aeruginosa cultures and in the breath of cystic fibrosis patients by selected ion flow tube mass spectrometry. Rapid Commun. Mass Spectrom. 2011;25:2459–2467. doi: 10.1002/rcm.5146. [DOI] [PubMed] [Google Scholar]
- [165].Neerincx A H, Geurts B P, Habets M F J, Booij J A, van Loon J, Jansen J J, Buydens L M C, van Ingen J, Mouton J W, Harren F J M, et al. Identification of Pseudomonas aeruginosa and Aspergillus fumigatus mono- and co-cultures based on volatile biomarker combinations. J. Breath Res. 2016;10:016002. doi: 10.1088/1752-7155/10/1/016002. [DOI] [PubMed] [Google Scholar]
- [166].Schöller C, Molin S, Wilkins K. Volatile metabolites from some gram-negative bacteria. Chemosphere. 1997;35:1487–1495. doi: 10.1016/S0045-6535(97)00209-9. [DOI] [PubMed] [Google Scholar]
- [167].Filipiak W, Sponring A, Baur M M, Filipiak A, Ager C, Wiesenhofer H, Nagl M, Troppmair J, Amann A. Molecular analysis of volatile metabolites released specifically by staphylococcus aureus and pseudomonas aeruginosa. BMC Microbiol. 2012;12:113. doi: 10.1186/1471-2180-12-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [168].Bean H D, Dimandja J M D, Hill J E. Bacterial volatile discovery using solid phase microextraction and comprehensive two-dimensional gas chromatography-time-of-flight mass spectrometry. J. Chromatogr. B: Analyt. Technol. Biomed. Life Sci. 2012;901:41–46. doi: 10.1016/j.jchromb.2012.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [169].Shestivska V, Španěl P, Dryahina K, Sovová K, Smith D, Musílek M, Nemec A. Variability in the concentrations of volatile metabolites emitted by genotypically different strains of Pseudomonas aeruginosa. J. Appl. Microbiol. 2012;113:701–713. doi: 10.1111/j.1365-2672.2012.05370.x. [DOI] [PubMed] [Google Scholar]
- [170].Carroll W, Lenney W, Wang T S, Španěl P, Alcock A, Smith D. Detection of volatile compounds emitted by Pseudomonas aeruginosa using selected ion flow tube mass spectrometry. Pediatr. Pulmonol. 2005;39:452–456. doi: 10.1002/ppul.20170. [DOI] [PubMed] [Google Scholar]
- [171].Yu K S, Hamilton-Kemp T R, Archbold D D, Collins R W, Newman M C. Volatile compounds from Escherichia coli O157:H7 and their absorption by strawberry fruit. J. Agric. Food Chem. 2000;48:413–417. doi: 10.1021/jf990576b. [DOI] [PubMed] [Google Scholar]
- [172].Storer M K, Hibbard-Melles K, Davis B, Scotter J. Detection of volatile compounds produced by microbial growth in urine by selected ion flow tube mass spectrometry (SIFT-MS) J. Microbiol. Methods. 2011;87:111–113. doi: 10.1016/j.mimet.2011.06.012. [DOI] [PubMed] [Google Scholar]
- [173].Maddula S, Blank L M, Schmid A, Baumbach J I. Detection of volatile metabolites of Escherichia coli by multi capillary column coupled ion mobility spectrometry. Anal. Bioanal. Chem. 2009;394:791–800. doi: 10.1007/s00216-009-2758-0. [DOI] [PubMed] [Google Scholar]
- [174].Guamán A V, Carreras A, Calvo D, Agudo I, Navajas D, Pardo A, Marco S, Farré R. Rapid detection of sepsis in rats through volatile organic compounds in breath. J. Chromatogr. B: Analyt. Technol. Biomed. Life Sci. 2012;881–882:76–82. doi: 10.1016/j.jchromb.2011.12.001. [DOI] [PubMed] [Google Scholar]
- [175].Chippendale T W E, Španěl P, Smith D. Time-resolved selected ion flow tube mass spectrometric quantification of the volatile compounds generated by E. coli JM109 cultured in two different media. Rapid Commun. Mass Spectrom. 2011;25:2163–2172. doi: 10.1002/rcm.5099. [DOI] [PubMed] [Google Scholar]
- [176].Bianchi F, Careri M, Mangia A, Mattarozzi M, Musci M, Concina I, Falasconi M, Gobbi E, Pardo M, Sberveglieri G. Differentiation of the volatile profile of microbiologically contaminated canned tomatoes by dynamic headspace extraction followed by gas chromatography-mass spectrometry analysis. Talanta. 2009;77:962–970. doi: 10.1016/j.talanta.2008.07.061. [DOI] [PubMed] [Google Scholar]
- [177].Umber B J, Shin H W, Meinardi S, Leu S Y, Zaldivar F, Cooper D M, Blake D R. Gas signatures from Escherichia coli and Escherichia coli-inoculated human whole blood. Clin. Transl. Med. 2013;2:13. doi: 10.1186/2001-1326-2-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [178].Elgaali H, Hamilton-Kemp T R, Newman M C, Collins R W, Yu K S, Archbold D D. Comparison of long-chain alcohols and other volatile compounds emitted from food-borne and related gram positive and gram negative bacteria. J. Basic Microbiol. 2002;42:373–380. doi: 10.1002/1521-4028(200212)42:6<373::AID-JOBM373>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- [179].Zhu J J, Bean H D, Kuo Y M, Hill J E. Fast detection of volatile organic compounds from bacterial cultures by secondary electrospray ionization-mass spectrometry. J. Clin. Microbiol. 2010;48:4426–4431. doi: 10.1128/JCM.00392-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [180].Saranya R, Aarthi R, Sankaran K. Simple and specific colorimetric detection of Staphylococcus using its volatile 2-[3-acetoxy-4,4,14-trimethylandrost-8-en-17-yl] propanoic acid in the liquid phase and head space of cultures. Appl. Microbiol. Biotechnol. 2015;99:4423–4433. doi: 10.1007/s00253-015-6573-6. [DOI] [PubMed] [Google Scholar]
- [181].Martin H J, Turner M A, Bandelow S, Edwards L, Riazanskaia S, Thomas C L P. Volatile organic compound markers of psychological stress in skin: A pilot study. J. Breath Res. 2016;10:046012. doi: 10.1088/1752-7155/10/4/046012. [DOI] [PubMed] [Google Scholar]
- [182].Ara K, Hama M, Akiba S, Koike K, Okisaka K, Hagura T, Kamiya T, Tomita F. Foot odor due to microbial metabolism and its control. Can. J. Microbiol. 2006;52:357–364. doi: 10.1139/w05-130. [DOI] [PubMed] [Google Scholar]
- [183].Yamazaki S, Hoshino K, Kusuhara M. Odor associated with aging. Anti-Aging Med. 2010;7:60–65. doi: 10.3793/jaam.7.60. [DOI] [Google Scholar]
- [184].Gallagher M, Wysocki C J, Leyden J J, Spielman A I, Sun X, Preti G. Analyses of volatile organic compounds from human skin. Br. J. Dermatol. 2008;159:780–791. doi: 10.1111/j.1365-2133.2008.08748.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [185].Abaffy T, Möller M G, Riemer D D, Milikowski C, DeFazio R A. Comparative analysis of volatile metabolomics signals from melanoma and benign skin: A pilot study. Metabolomics. 2013;9:998–1008. doi: 10.1007/s11306-013-0523-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [186].Campbell L F, Farmery L, George S M C, Farrant P B J. Canine olfactory detection of malignant melanoma. BMJ Case Rep. 2013;2013:bcr2013008566. doi: 10.1136/bcr-2013-008566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [187].D’Amico A, Bono R, Pennazza G, Santonico M, Mantini G, Bernabei M, Zarlenga M, Roscioni C, Martinelli E, Paolesse R, et al. Identification of melanoma with a gas sensor array. Skin Res. Technol. 2008;14:226–236. doi: 10.1111/j.1600-0846.2007.00284.x. [DOI] [PubMed] [Google Scholar]
- [188].Kwak J, Gallagher M, Ozdener M H, Wysocki C J, Goldsmith B R, Isamah A, Faranda A, Fakharzadeh S S, Herlyn M, Johnson A T C, et al. Volatile biomarkers from human melanoma cells. J. Chromatogr. B: Analyt. Technol. Biomed. Life Sci. 2013;931:90–96. doi: 10.1016/j.jchromb.2013.05.007. [DOI] [PubMed] [Google Scholar]
- [189].Pickel D, Manucy G P, Walker D B, Hall S B, Walker J C. Evidence for canine olfactory detection of melanoma. Appl. Anim. Behav. Sci. 2004;89:107–116. doi: 10.1016/j.applanim.2004.04.008. [DOI] [Google Scholar]
- [190].Dormont L, Bessière J M, Cohuet A. Human skin volatiles: A review. J. Chem. Ecol. 2013;39:569–578. doi: 10.1007/s10886-013-0286-z. [DOI] [PubMed] [Google Scholar]
- [191].Barzantny H, Schröder J, Strotmeier J, Fredrich E, Brune I, Tauch A. The transcriptional regulatory network of Corynebacterium jeikeium K411 and its interaction with metabolic routes contributing to human body odor formation. J. Biotechnol. 2012;159:235–248. doi: 10.1016/j.jbiotec.2012.01.021. [DOI] [PubMed] [Google Scholar]
- [192].Marshall J, Holland K T, Gribbon E M. A comparative study of the cutaneous microflora of normal feet with low and high levels of odour. J. Appl. Bacteriol. 1988;65:61–68. doi: 10.1111/j.1365-2672.1988.tb04318.x. [DOI] [PubMed] [Google Scholar]
- [193].Natsch A, Derrer S, Flachsmann F, Schmid J. A broad diversity of volatile carboxylic acids, released by a bacterial aminoacylase from axilla secretions, as candidate molecules for the determination of human-body odor type. Chem. Biodivers. 2006;3:1–20. doi: 10.1002/cbdv.200690015. [DOI] [PubMed] [Google Scholar]
- [194].De Giovanni N, Fucci N. The current status of sweat testing for drugs of abuse: A review. Curr. Med. Chem. 2013;20:545–561. doi: 10.2174/0929867311320040006. [DOI] [PubMed] [Google Scholar]
- [195].Holmberg M, Winquist F, Lundström I, Gardner J W, Hines E L. Identification of paper quality using a hybrid electronic nose. Sens. Actuators B: Chem. 1995;27:246–249. doi: 10.1016/0925-4005(94)01595-9. [DOI] [Google Scholar]
- [196].Ulmer H, Mitrovics J, Noetzel G, Weimar U, Göpel W. Odours and flavours identified with hybrid modular sensor systems. Sens. Actuators B: Chem. 1997;43:24–33. doi: 10.1016/S0925-4005(97)00161-5. [DOI] [Google Scholar]
- [197].Pardo M, Kwong L G, Sberveglieri G, Brubaker K, Schneider J F, Penrose W R, Stetter J R. Data analysis for a hybrid sensor array. Sens. Actuators B: Chem. 2005;106:136–143. doi: 10.1016/j.snb.2004.05.045. [DOI] [Google Scholar]
- [198].Li C L, Chen Y F, Liu M H, Lu C J. Utilizing diversified properties of monolayer protected gold nano-clusters to construct a hybrid sensor array for organic vapor detection. Sens. Actuators B: Chem. 2012;169:349–359. doi: 10.1016/j.snb.2012.05.009. [DOI] [Google Scholar]
- [199].Lu H L, Lu C J, Tian W C, Sheen H J. A vapor response mechanism study of surface-modified single-walled carbon nanotubes coated chemiresistors and quartz crystal microbalance sensor arrays. Talanta. 2015;131:467–474. doi: 10.1016/j.talanta.2014.08.027. [DOI] [PubMed] [Google Scholar]
- [200].Zetola N M, Modongo C, Matsiri O, Tamuhla T, Mbongwe B, Matlhagela K, Sepako E, Catini A, Sirugo G, Martinelli E, et al. Diagnosis of pulmonary tuberculosis and assessment of treatment response through analyses of volatile compound patterns in exhaled breath samples. J. Infect. 2017;74:367–376. doi: 10.1016/j.jinf.2016.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [201].Cho Y S, Jung S C, Oh S. Diagnosis of bovine tuberculosis using a metal oxide-based electronic nose. Lett. Appl. Microbiol. 2015;60:513–516. doi: 10.1111/lam.12410. [DOI] [PubMed] [Google Scholar]
- [202].Wu C S, Du L P, Wang D, Zhao L H, Wang P. A biomimetic olfactory-based biosensor with high efficiency immobilization of molecular detectors. Biosens. Bioelectron. 2012;31:44–48. doi: 10.1016/j.bios.2011.09.037. [DOI] [PubMed] [Google Scholar]
- [203].Chen X, Cao M F, Li Y, Hu W J, Wang P, Ying K J, Pan H M. A study of an electronic nose for detection of lung cancer based on a virtual SAW gas sensors array and imaging recognition method. Meas. Sci. Technol. 2005;16:1535–1546. doi: 10.1088/0957-0233/16/8/001. [DOI] [Google Scholar]
- [204].Mazzone P J, Hammel J, Dweik R, Na J, Czich C, Laskowski D, Mekhail T. Diagnosis of lung cancer by the analysis of exhaled breath with a colorimetric sensor array. Thorax. 2007;62:565–568. doi: 10.1136/thx.2006.072892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [205].Janzen M C, Ponder J B, Bailey D P, Ingison C K, Suslick K S. Colorimetric sensor arrays for volatile organic compounds. Anal. Chem. 2006;78:3591–3600. doi: 10.1021/ac052111s. [DOI] [PubMed] [Google Scholar]
- [206].Vincent T A, Gardner J W. A low cost MEM based NDIR system for the monitoring of carbon dioxide in breath analysis at ppm levels. Sens. Actuators B: Chem. 2016;236:954–964. doi: 10.1016/j.snb.2016.04.016. [DOI] [Google Scholar]
- [207].Meng Z, Stolz R M, Mendecki L, Mirica K A. Electrically-transduced chemical sensors based on two-dimensional nanomaterials. Chem. Rev. 2019;119:478–598. doi: 10.1021/acs.chemrev.8b00311. [DOI] [PubMed] [Google Scholar]
- [208].Paolesse R, Nardis S, Monti D, Stefanelli M, Di Natale C. Porphyrinoids for chemical sensor applications. Chem. Rev. 2017;117:2517–2583. doi: 10.1021/acs.chemrev.6b00361. [DOI] [PubMed] [Google Scholar]
- [209].Shehada N, Cancilla J C, Torrecilla J S, Pariente E S, Brönstrup G, Christiansen S, Johnson D W, Leja M, Davies M P A, Liran O, et al. Silicon nanowire sensors enable diagnosis of patients via exhaled breath. ACS Nano. 2016;10:7047–7057. doi: 10.1021/acsnano.6b03127. [DOI] [PubMed] [Google Scholar]
- [210].Cao L A, Yao M S, Jiang H J, Kitagawa S, Ye X L, Li W H, Xu G. A highly oriented conductive MOF thin film-based Schottky diode for self-powered light and gas detection. J. Mater. Chem. A. 2020;8:9085–9090. doi: 10.1039/D0TA01379J. [DOI] [Google Scholar]
- [211].Yuan H Y, Tao J F, Li N X, Karmakar A, Tang C H, Cai H, Pennycook S J, Singh N, Zhao D. On-chip tailorability of capacitive gas sensors integrated with metal-organic framework films. Angew. Chem., Int. Ed. 2019;58:14089–14094. doi: 10.1002/anie.201906222. [DOI] [PubMed] [Google Scholar]
- [212].Sun Z B, Yu S H, Zhao L L, Wang J F, Li Z F, Li G. A highly stable two-dimensional copper (II) organic framework for proton conduction and ammonia impedance sensing. Chem. Eur. J. 2018;24:10829–10839. doi: 10.1002/chem.201801844. [DOI] [PubMed] [Google Scholar]
- [213].Yao M S, Li W H, Xu G. Metal-organic frameworks and their derivatives for electrically-transduced gas sensors. Coord. Chem. Rev. 2021;426:213479. doi: 10.1016/j.ccr.2020.213479. [DOI] [Google Scholar]
- [214].Pauling L, Robinson A B, Teranishi R, Cary P. Quantitative analysis of urine vapor and breath by gas—liquid partition chromatography. Proc. Natl. Acad. Sci. USA. 1971;68:2374–2376. doi: 10.1073/pnas.68.10.2374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [215].Amal H, Haick H. Point of care breath analysis systems. In: Llobet E, editor. Advanced Nanomaterials for Inexpensive Gas Microsensors. Cambridge, MA: Elsevier; 2020. pp. 315–334. [Google Scholar]
- [216].Nakhleh M K, Badarny S, Winer R, Jeries R, Finberg J, Haick H. Distinguishing idiopathic Parkinson’s disease from other parkinsonian syndromes by breath test. Parkinsonism Relat. Disord. 2015;21:150–153. doi: 10.1016/j.parkreldis.2014.11.023. [DOI] [PubMed] [Google Scholar]
- [217].Nardi-Agmon I, Abud-Hawa M, Liran O, Gai-Mor N, Ilouze M, Onn A, Bar J, Shlomi D, Haick H, Peled N. Exhaled breath analysis for monitoring response to treatment in advanced lung cancer. J. Thorac. Oncol. 2016;11:827–837. doi: 10.1016/j.jtho.2016.02.017. [DOI] [PubMed] [Google Scholar]
- [218].Kim S J, Choi S J, Jang J S, Cho H J, Kim I D. Innovative nanosensor for disease diagnosis. Acc. Chem. Res. 2017;50:1587–1596. doi: 10.1021/acs.accounts.7b00047. [DOI] [PubMed] [Google Scholar]
- [219].Schuermans V N E, Li Z Y, Jongen A C H M, Wu Z Q, Shi J Y, Ji J F, Bouvy N D. Pilot study: Detection of gastric cancer from exhaled air analyzed with an electronic nose in Chinese patients. Surg. Innov. 2018;25:429–434. doi: 10.1177/1553350618781267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [220].Hanson C W, 3rd, Thaler E R. Electronic nose prediction of a clinical pneumonia score: Biosensors and microbes. Anesthesiology. 2005;102:63–68. doi: 10.1097/00000542-200501000-00013. [DOI] [PubMed] [Google Scholar]
- [221].Kateb B, Ryan M A, Homer M L, Lara L M, Yin Y F, Higa K, Chen M Y. Sniffing out cancer using the JPL electronic nose: A pilot study of a novel approach to detection and differentiation of brain cancer. NeuroImage. 2009;47:T5–T9. doi: 10.1016/j.neuroimage.2009.04.015. [DOI] [PubMed] [Google Scholar]
- [222].Wu A Q, Wang W Q, Zhan H B, Cao L A, Ye X L, Zheng J J, Kumar P N, Chiranjeevulu K, Deng W H, Wang G E, et al. Layer-by-layer assembled dual-ligand conductive MOF nano-films with modulated chemiresistive sensitivity and selectivity. Nano Res. 2021;14:438–443. doi: 10.1007/s12274-020-2823-8. [DOI] [Google Scholar]
- [223].Campbell M G, Sheberla D, Liu S F, Swager T M, Dincă M. Cu3(hexaiminotriphenylene)2: An electrically conductive 2D metal-organic framework for chemiresistive sensing. Angew. Chem. 2015;127:4423–4426. doi: 10.1002/ange.201411854. [DOI] [PubMed] [Google Scholar]
- [224].Stolz R M, Mahdavi-Shakib A, Frederick B G, Mirica K A. Host-guest interactions and redox activity in layered conductive metal-organic frameworks. Chem. Mater. 2020;32:7639–7652. doi: 10.1021/acs.chemmater.0c01007. [DOI] [Google Scholar]
- [225].Yao M S, Zheng J J, Wu A Q, Xu G, Nagarkar S S, Zhang G, Tsujimoto M, Sakaki S, Horike S, Otake K, et al. A dual-ligand porous coordination polymer chemiresistor with modulated conductivity and porosity. Angew. Chem., Int. Ed. 2020;59:172–176. doi: 10.1002/anie.201909096. [DOI] [PubMed] [Google Scholar]
- [226].Fan Y, Zhang J, Shen Y, Zheng B, Zhang W N, Huo F W. Emerging porous nanosheets: From fundamental synthesis to promising applications. Nano Res. 2021;14:1–28. doi: 10.1007/s12274-020-3082-4. [DOI] [Google Scholar]
- [227].Donarelli M, Ottaviano L, Giancaterini L, Fioravanti G, Perrozzi F, Cantalini C. Exfoliated black phosphorus gas sensing properties at room temperature. 2D Mater. 2016;3:025002. doi: 10.1088/2053-1583/3/2/025002. [DOI] [Google Scholar]
- [228].Cho S Y, Koh H J, Yoo H W, Jung H T. Tunable chemical sensing performance of black phosphorus by controlled functionalization with noble metals. Chem. Mater. 2017;29:7197–7205. doi: 10.1021/acs.chemmater.7b01353. [DOI] [Google Scholar]
- [229].Yao M S, Otake K I, Xue Z Q, Kitagawa S. Concluding remarks: Current and next generation MOFs. Faraday Discuss. 2021;231:397–417. doi: 10.1039/D1FD00058F. [DOI] [PubMed] [Google Scholar]
- [230].Yao M S, Wang P, Gu Y F, Koganezawa T, Ashitani H, Kubota Y, Wang Z M, Fan Z Y, Otake K I, Kitagawa S. A comparative study of honeycomb-like 2D π-conjugated metal-organic framework chemiresistors: Conductivity and channels. Dalton Trans. 2021;50:13236–13245. doi: 10.1039/D1DT02323C. [DOI] [PubMed] [Google Scholar]
- [231].Meng Z, Stolz R M, Mirica K A. Two-dimensional chemiresistive covalent organic framework with high intrinsic conductivity. J. Am. Chem. Soc. 2019;141:11929–11937. doi: 10.1021/jacs.9b03441. [DOI] [PubMed] [Google Scholar]
- [232].Zhang H H, Gu C, Yao M S, Kitagawa S. Hybridization of emerging crystalline porous materials: Synthesis dimensionality and electrochemical energy storage application. Adv. Energy Mater. 2022;12:2100321. doi: 10.1002/aenm.202100321. [DOI] [Google Scholar]
- [233].Jian Y Y, Qu D Y, Guo L H, Zhu Y J, Su C, Feng H R, Zhang G J, Zhang J, Wu W W, Yao M S. The prior rules of designing Ti3C2Tx MXene-based gas sensors. Front. Chem. Sci. Eng. 2021;15:505–517. doi: 10.1007/s11705-020-2013-y. [DOI] [Google Scholar]
- [234].Kim S J, Koh H J, Ren C E, Kwon O, Maleski K, Cho S Y, Anasori B, Kim C K, Choi Y K, Kim J, et al. Metallic Ti3C2Tx MXene gas sensors with ultrahigh signal-to-noise ratio. ACS Nano. 2018;12:986–993. doi: 10.1021/acsnano.7b07460. [DOI] [PubMed] [Google Scholar]
- [235].Lee E, VahidMohammadi A, Prorok B C, Yoon Y S, Beidaghi M, Kim D J. Room temperature gas sensing of two-dimensional titanium carbide (MXene) ACS Appl. Mater. Interfaces. 2017;9:37184–37190. doi: 10.1021/acsami.7b11055. [DOI] [PubMed] [Google Scholar]
- [236].Yao M S, Xiu J W, Huang Q Q, Li W H, Wu W W, Wu A Q, Cao L A, Deng W H, Wang G E, Xu G. Van der Waals heterostructured MOF-on-MOF thin films: Cascading functionality to realize advanced chemiresistive sensing. Angew. Chem., Int. Ed. 2019;58:14915–14919. doi: 10.1002/anie.201907772. [DOI] [PubMed] [Google Scholar]
- [237].Yao M S, Tang W X, Wang G E, Nath B, Xu G. MOF thin film-coated metal oxide nanowire array: Significantly improved chemiresistor sensor performance. Adv. Mater. 2016;28:5229–5234. doi: 10.1002/adma.201506457. [DOI] [PubMed] [Google Scholar]
- [238].Lei G L, Lou C M, Liu X H, Xie J Y, Li Z S, Zheng W, Zhang J. Thin films of tungsten oxide materials for advanced gas sensors. Sens. Actuator B: Chem. 2021;341:129996. doi: 10.1016/j.snb.2021.129996. [DOI] [Google Scholar]
- [239].Liu X H, Zheng W, Kumar R, Kumar M, Zhang J. Conducting polymer-based nanostructures for gas sensors. Coord. Chem. Rev. 2022;462:214517. doi: 10.1016/j.ccr.2022.214517. [DOI] [Google Scholar]
- [240].Lou C M, Lei G L, Liu X H, Xie J Y, Li Z S, Zheng W, Goel N, Kumar M, Zhang J. Design and optimization strategies of metal oxide semiconductor nanostructures for advanced formaldehyde sensors. Coord. Chem. Rev. 2022;452:214280. doi: 10.1016/j.ccr.2021.214280. [DOI] [Google Scholar]
- [241].Zhang J, Liu X H, Neri G, Pinna N. Nanostructured materials for room-temperature gas sensors. Adv. Mater. 2016;28:795–831. doi: 10.1002/adma.201503825. [DOI] [PubMed] [Google Scholar]
- [242].Liu X H, Ma T T, Pinna N, Zhang J. Two-dimensional nanostructured materials for gas sensing. Adv. Funct. Mater. 2017;27:1702168. doi: 10.1002/adfm.201702168. [DOI] [Google Scholar]
- [243].Xu K, Fu C, Gao Z, Wei F, Ying Y, Xu C, Fu G. Nanomaterial-based gas sensors: A review. Instrum. Sci. Technol. 2018;46:115–145. doi: 10.1080/10739149.2017.1340896. [DOI] [Google Scholar]
- [244].Jin C G, Kurzawski P, Hierlemann A, Zellers E T. Evaluation of multitransducer arrays for the determination of organic vapor mixtures. Anal. Chem. 2008;80:227–236. doi: 10.1021/ac0715120. [DOI] [PubMed] [Google Scholar]
- [245].Jin C G, Zellers E T. Limits of recognition for binary and ternary vapor mixtures determined with multitransducer arrays. Anal. Chem. 2008;80:7283–7293. doi: 10.1021/ac8008912. [DOI] [PubMed] [Google Scholar]
- [246].Gutierrez-Osuna R, Hierlemann A. Adaptive microsensor systems. Annu. Rev. Anal. Chem. 2010;3:255–276. doi: 10.1146/annurev.anchem.111808.073620. [DOI] [PubMed] [Google Scholar]
- [247].Li Z, Askim J R, Suslick K S. The optoelectronic nose: Colorimetric and fluorometric sensor arrays. Chem. Rev. 2019;119:231–292. doi: 10.1021/acs.chemrev.8b00226. [DOI] [PubMed] [Google Scholar]
- [248].Zhao S X, Lei J C, Huo D Q, Hou C J, Luo X G, Wu H X, Fa H B, Yang M. A colorimetric detector for lung cancer related volatile organic compounds based on cross-response mechanism. Sens. Actuators B: Chem. 2018;256:543–552. doi: 10.1016/j.snb.2017.10.091. [DOI] [Google Scholar]
- [249].Lei J C, Hou C J, Huo D Q, Luo X G, Bao M Z, Li X, Yang M, Fa H B. A novel device based on a fluorescent cross-responsive sensor array for detecting lung cancer related volatile organic compounds. Rev. Sci. Instrum. 2015;86:025106. doi: 10.1063/1.4907628. [DOI] [PubMed] [Google Scholar]
- [250].Hou C J, Lei J C, Huo D Q, Song K, Li J J, Luo X G, Yang M, Fa H B. Discrimination of lung cancer related volatile organic compounds with a colorimetric sensor array. Anal. Lett. 2013;46:2048–2059. doi: 10.1080/00032719.2013.782550. [DOI] [Google Scholar]
- [251].Huo D Q, Xu Y H, Hou C J, Yang M, Fa H B. A novel optical chemical sensor based AuNR-MTPP and dyes for lung cancer biomarkers in exhaled breath identification. Sens. Actuators B: Chem. 2014;199:446–456. doi: 10.1016/j.snb.2014.03.114. [DOI] [Google Scholar]


