Abstract
The current study aimed to investigate the mediating role of cognitive attentional syndrome (CAS) and distress tolerance in the relationship between health-related metacognitions and coronavirus anxiety. The sample of this study consisted of 462 participants (381 female). Participants voluntarily completed self-report questionnaires on each of the variables mentioned above. The results of the structural modeling analysis showed that health-related metacognitions have a significant effect on the mediator variable of distress tolerance and CAS. Also, health-related metacognitions had a direct effect on coronavirus anxiety. Also, based on the results of the bootstrap test, it can be argued that health-related metacognitive beliefs, apart from their direct effect, play an important role in coronavirus anxiety, with CAS acting as a mediator. This study provides insights into the relationships among metacognitive beliefs, coronavirus anxiety, CAS, and distress tolerance. In particular, dysfunctional metacognitive beliefs, including an individual's beliefs about the uncontrollability of disease-related thoughts, are risk factors that could negatively affect mental health, leading to coronavirus anxiety. In addition, the association of dysfunctional beliefs with maladaptive behaviors resulting from the cognitive attentional syndrome is also involved in predicting and causing coronavirus anxiety. Given the insignificant role of emotional distress tolerance in the psychopathology of COVID-19 anxiety, the findings emphasize the importance of cognitive factors in this context.
Keywords: Health-related metacognitions, Coronavirus anxiety, Cognitive attentional syndrome, Distress tolerance
Introduction
In late 2019, an outbreak of COVID-19 (caused by the coronavirus SARS-CoV-2) was observed in Wuhan, China. The infection quickly spread to other areas of China (Chen et al., 2020; Zhao & Chen, 2020; Zhu et al., 2020) and triggered a global public health emergency (Enitan et al., 2020; Lai et al., 2019; World Health Organization, 2020a). Iran is now one of the most impacted countries experiencing the Sixths pandemic wave (Tehran Times, 2022). According to official data, there were 2,396,204 confirmed cases of COVID-19 and 69,574 fatalities in Iran between 3rd January 2020 and 26th April 2021 (World Health Organization, 2020b).
According to the present body of knowledge on COVID-19, some psychological elements are stronger at causing and intensifying anxiety associated with this coronavirus (ADAA, 2020; Chi tam et al., 2020; Jungmann & Witthöft, 2020), which can result in major health concerns (Gallagher et al., 2020; Lee, Jobe, et al., 2020; Mazza et al., 2020; McKay et al., 2020). As mental strain is expected to persist throughout the pandemic, more studies on pandemic-related psychological issues are needed (Lee, Mathis, et al., 2020). A recent study conducted during the fourth wave of the pandemic by using a national survey (Akbari et al., 2021c, 2021d) revealed that Iranians had experienced psychological distress due to the COVID-19. The authors have found that distress intolerance has predicted psychological distress, partially mediated by psychological flexibility. The significant mediation was independent of demographic factors (age, gender, marital status, and educational level) and fear of COVID-19, mindfulness, and satisfaction with life. The authors concluded that despite the mentioned variables, accepting and using unpleasant emotions as fuel to achieve valued goals rather than avoiding them would mitigate the psychological distress during the pandemic.
Some researchers have found that fear and anxiety about COVID-19 are associated with higher rates of anxiety and depression symptoms (Ahmed et al., 2020; Ahorsu et al., 2020; Jungmann & Witthoft, 2020; Lee, Mathis, et al., 2020; Lee, 2020b; Taylor & Asmundson, 2020; Wang et al., 2020; Akbari et al., 2021d). The heightened anxiety and depressive symptoms are associated with health anxiety (HA; Nikčević et al., 2021). It refers to psychological distress when a person thinks he/she is ill or will become ill (Creed et al., 2018). This is a constant anxiety that most people will experience during the pandemic. This state can be affected by metacognitions about health, which reflect one's cognitions regarding health-related cognitions responsible for various emotional disorders (Leahy et al., 2018; Yilmaz et al., 2015). Metacognitive beliefs concerning uncontrollability and danger of thoughts can predict symptoms of health anxiety (Brown et al., 2019; Gutierrez et al., 2020; Rachor & Penney, 2020); suggesting that beliefs about the power of thoughts to cause illness and a feeling of inability to stop the thinking would elevate the health anxiety through threat interpretation of thoughts (Melli et al., 2018).
Metacognitive beliefs can activate and maintain what Wells and Matthews (1994) refer to as the Cognitive Attentional Syndrome (CAS), which is one of the factors that contribute to an increase in anxiety and depression symptoms (Fergus et al., 2012; Fergus & Scullin., 2017; Kowalski et al., 2019). The CAS consists of three components: rumination and worry, repetitive negative thinking, and focusing attention on threats, as well as coping behaviors and strategies (e.g., thought suppression, thought and situation avoidance, or substance and alcohol use; Papageorgiou & Wells, 2009; Sica et al., 2007; Spada et al., 2015; Wells, 2009).
Typically, the CAS is activated to address unwanted negative intrusive thoughts (Wells, 2009); in COVID, what if I got infected? The CAS is made up of chains of verbal thought, such as excessive worry about getting sick; a pattern of putting the focus on the threat, which includes scanning the body for signs of illness and excessive body checking; and coping strategies that have negative consequences, such as looking up illnesses on the internet or trying to block out thoughts of illness. Rather than putting an end to negative thinking, the CAS encourages it, leading to the perception that illness is present. COVID-19 anxiety also can be harmonized with this perspective as a form and an indication of health anxiety.
Frequent activation of the CAS by catastrophic misinterpretations of physical symptoms can underlie sustained worry (Bailey & Wells, 2015a), which causes the persistence of negative emotions and negative self-appraisal in some individuals (Fergus & Bardeen, 2013; Fergus et al., 2012), cumulating the levels of anxiety and depression (Fergus et al., 2013; Kowalski et al., 2019). As this deplorable state persists, not all people may be able to bear and endure it, which refers to an individual's perceived ability to endure negative emotions and is one of the cognitive-emotional factors that influence the development of mental and emotional distress (Ranney et al., 2020), namely, distress tolerance (DT; Leyro et al., 2016).
Research shows that lower levels of DT are associated with a higher risk for clinically-relevant levels of depression (Felton et al., 2019;), anxiety (Lee et al., 2018), anxiety sensitivity (Sauer et al., 2020), and symptoms of PTSD (Liu et al., 2020; Wright et al., 2020; Zegel et al., 2020). These findings suggest that DT may play a key role in developing anxiety in general (Laposa et al., 2015). Associated behaviors with low DT may lead to persistent anxiety symptoms (Wright et al., 2020), triggered by the COVID-19 pandemic eternity (Sauer et al., 2020; Wright et al., 2020); People with low DT who feel inefficacy to tolerate negative internal state, for example, by thinking that COVID-19-related thoughts are uncontrollable and dangerous, are motivated to escape from internal states which intensifies anxiety.
Although several studies support the prominent role of distress tolerance in anxiety, this construct has received little exploration in the literature on health anxiety (Fergus et al., 2015; Keough et al., 2010; Sauer et al., 2020). Overall, we consider COVID-19 anxiety as an indication of health anxiety; thus, we believe that the anxiety of being infected with COVID-19 can be influenced by metacognitions about health, such as I cannot get rid of thinking about COVID-19 and I cannot stop it. However, we hypothesized that distress tolerance could mediate this path, as people who cannot tolerate the caused distress by the mentioned metacognitions may feel a higher level of COVID-19 anxiety. Moreover, we hypothesized that cognitive attentional syndrome could mediate the relationship between metacognitions about health and COVID-19 anxiety, given that fixed attention on the metacognitions would elevate the level of COVID-19 anxiety.
Methods
Participants
This study used a convenience sample of 462 participants. 82.5% were female (381 females; Mean age = 33.31, SD = 9.88) and 17.5% were male (81 males; Mean age = 34.62, SD = 9.72). In terms of education, 5% had some undergraduate education, 16% had a diploma, 27.18% had a bachelor's degree, 43.7% had a master's degree, and 12% had a doctoral degree. Concerning employment status, 54% were employed, 39% were unemployed, and 7% had lost their jobs because of the COVID-19 pandemic.
Measures
Coronavirus Anxiety Scale (CAS)
The Coronavirus Anxiety Scale (CAS) is a valid, unidimensional scale developed by Lee (2020a) that assesses the physiological responses of dysfunctional fear and anxiety associated with the COVID-19 virus. It is validated in Persian (Mohammadpour et al., 2020) and demonstrated good psychometric properties with Chronbach's alpha of 0.82. This scale consists of five items (e.g., "I felt paralyzed or frozen when I thought about or was exposed to information about the coronavirus"). Then, participants were assessed according to the 5-point scale (0 = none/never, 4 = almost every day for the past two weeks) on how often each anxiety symptom occurred (e.g., "I had trouble falling or staying asleep because I was thinking about the coronavirus"). Also, this scale has acceptable internal consistency reliability, structure, and concurrent validity. The cut score of this scale is ≥ 9, with 90% sensitivity and 85% specificity. The Cronbach's alpha in the original study was 0.92 and for the current study was 0.79.
The Metacognitions about Health Questionnaire (MCQ-HA; Bailey & Wells, 2015a, 2015b)
This tool was developed based on the widely-used, 30-item Metacognitions Questionnaire (MCQ-30; Wells & Cartwright-Hatton, 2004). Unlike the MCQ-30, the MCQ-HA assesses the metacognitive beliefs associated with health anxieties. This scale consists of 14 items with a 4-point Likert response from 1 ("I do not agree") to 4 ("I strongly agree"). Based on the initial analysis by the parent study (Bailey and Wells, 2015a; 2015b), the following items were created: (1) beliefs about biased thinking (e.g., "Thinking the worse about symptoms will keep me safe"); (2) beliefs that thoughts cause illness ("Worrying about illness is likely to make it happen"); (3) beliefs about the uncontrollability of thoughts (e.g., "Dwelling on thoughts of illness is uncontrollable"). Studies have shown that this scale has acceptable internal consistency and discriminant and convergent validity. In the study by Bailey and Wells (2015c), the internal consistency of subscales with alpha scores is significant: beliefs that thoughts cause illness = 0.82, beliefs about biased thinking = 0.81, and beliefs that thoughts are uncontrollable = 0.80. The Persian version of MCQ-HA (Akbari, 2019) has shown good internal consistency of 0.87. Also, in the current study, Cronbach's alphas of the total scale were 0.74.
The Cognitive Attentional Syndrome Scale (CAS-1; Wells, 2009)
The CAS-1 is a 16-item scale developed to assess the activation of cognitive-attentional symptoms (Wells, 2009). This scale measures the frequency of persistent thinking styles, dysfunctional coping strategies, and the extent of metacognitive beliefs about these strategies (Fergus et al., 2012, 2013). The first two items are questions about the frequency of rumination, worry, and threat monitoring. These are rated on a scale of 0 to 8. The other six items are related to maladaptive behaviors used to cope with negative emotions and thoughts (e.g., "I could make myself sick by worrying") and are rated from 0 to 8. The final subscale (8 items) assesses individuals' metacognitive beliefs about the CAS. However, to avoid inflation of associations between variables (metacognitions about health and CAS), the positive and negative generic metacognitions embedded in CAS-I were removed from the analysis. A high score of CAS-1 indicates an increase in the level of CAS activation. Additionally, CAS-1 has high internal compatibility (Cronbach’s alpha = 0.86; Fergus et al., 2012). The Persian version (Farrokhi & Sohrabi, 2017) also has shown good psychometric properties with Chronbach's alpha of 0.82; the latter in the current study for the whole scale was 0.88.
Distress Tolerance Scale (DTS; Simmons & Gaher, 2005)
This questionnaire is a 15-item distress tolerance self-assessment index. The DTS is scored on a 5-point scale: (5) strongly disagree, (4) mildly disagree, (3) agree and disagree equally, (2) mildly agree, and (1) strongly agree. The items in this scale measure distress tolerance based on an individual's ability to cope with emotional distress, mental assessment of distress, attention to negative emotions if they occur, and regulatory actions to relieve distress. High scores on this scale indicate high distress tolerance. Alpha coefficients for these subscales in the original study were 0.72, 0.82, 0.78, 0.70, and 0.82 for the whole scale. This scale has also been found to have good standard validity and initial convergence (Simmons & Gaher, 2005). The Persian version (Akbari et al. 2021b) has demonstrated sound psychometric properties with Chronbach's alpha of 0.89, and in the current study, it is for the whole scale was 0.80.
Procedure
The current research was carried out according to the Helsinki Declaration of 1989. Participants were invited to participate in the current study via advertisements on digital applications (WhatsApp and Telegram). A web link was sent to the mentioned applications. A link was supplied with information on the current study purpose on the first page. After agreeing to participate, how to complete the surveys, demographic information, and a pack of questionnaires became available to the respondents by confirming the consent form. Individuals were required to be at least 18 years old to participate in this study. All participants volunteered and were not compensated; also, they were assured that their answers would be confidential as they could fill out the questionnaires anonymously.
Data Analysis
Data were analyzed using SPSS version 25 for Windows (IBM SPSS Statistics) and LISREL 8.80 (Jöreskog & Sörbom, 2006). Correlations were used to assess the relationships between the variables in the current study. Second, structural equation modeling was used to assess the proposed model. The bootstrap was also used to test the mediational path (iteration number = 2000). The model fit was evaluated through the Chi-square index (χ2), comparative fit index (CFI), normed fit index (NFI), incremental fit index (IFI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR). An adequate fit was indicated by values < 5 for 2/df, values > 0.9 for CFI, NFI and IFI; in addition, values equal to or < 0.08 (values < 0.06 are more appropriate) for the RMSEA and SRMR represent an adequate fit (Kline, 2015).
Results
Descriptive Statistics
See Table 1 for descriptive statistics, including the mean, standard deviation, skewness, and the kurtosis of the research variables.
Table 1.
Correlation matrix and descriptive indices of research variables
| Variables | 1 | 2 | 3 | 4 | M | SD | Skewness | Kurtosis | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | MCQ-HA | 1 | 27.97 | 6.51 | 0.243 | − 0.116 | |||
| 2 | DTS | 0.445** | 1 | 46.52 | 10.92 | − 0.144 | − 0.251 | ||
| 3 | CAS-1 | 0.502** | 0.455** | 1 | 87.16 | 29.44 | − 0.559 | − 0.117 | |
| 4 | Coronavirus Anxiety | 0.425** | 0.375** | 0.462** | 1 | 6.96 | 3.217 | 1.165 | 1.195 |
n = 461
MCQ-HA Metacognitions about Health Questionnaire, DTS The Distress Tolerance Scale, CAS-1 The Cognitive Attentional Syndrome Scale
**p < .001
Assumptions of Structural Equation Modeling
Before evaluating the structural model of the research, the assumptions of structural equation modeling were first examined. The skewness of the variables is in the range of 0.742 to 1.957, and kurtosis falls in the range of − 1.100 to 4.743. Chou and Bentler (1995) consider the cut-off point of ± 3 to be appropriate for the amount of skewness. For the cut-off point of the kurtosis, values greater than ± 10 are problematic for this index (Kline, 2011). The relative multivariate kurtosis index, which is calculated to evaluate the assumption of multivariate normality, was 1.29. Bentler (1998) believes that multivariate normality is achieved if the value of this index is less than 3.
Preliminary studies showed that the data is suitable for structural equation modeling using the maximum likelihood estimation method (Table 1).
Measurement Model
Before evaluating the structural model, the fit indices for the measurement model were calculated. The measurement model identifies the relationship between the observable and latent variables. The evaluation was done using confirmatory factor analysis, and the fit indices of the measurement model presented in Table 2 show a very good fit. Thus, the evaluation of the structural model indicates an acceptable fit.
Table 2.
Fit indices for measurement and structural model
| Chi-square | DF | X2/DF | RMSEA | SRMR | CFI | NFI | GFI | |
|---|---|---|---|---|---|---|---|---|
| Measurement model | 182.66 | 55 | 3.32 | 0.068 | 0.056 | 0.97 | 0.97 | 0.94 |
| Structural model | 141.84 | 39 | 3.63 | 0.076 | 0.058 | 0.97 | 0.95 | 0.95 |
Structural Model
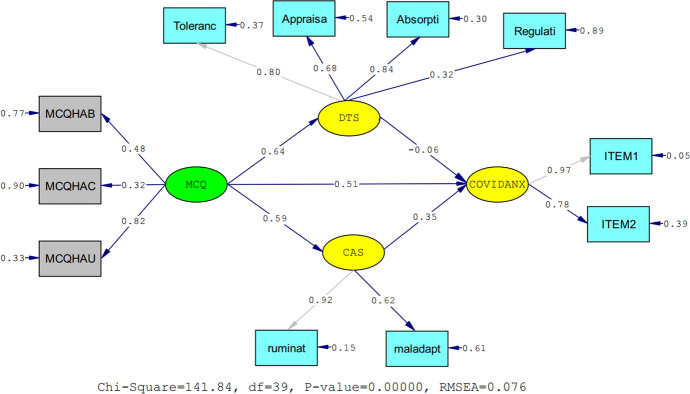
Figure 1 illustrates the structural model with standardized coefficients using bootstrapping technique. As can be seen, health-related metacognitive beliefs as an independent variable with standard coefficients of 0.65 and 0.67, respectively, significantly affect the mediator variable of distress tolerance and cognitive attentional syndrome. Also, with a standardized coefficient of 0.57, health-related metacognitive beliefs significantly affect coronavirus anxiety. On the other hand, distress tolerance as a mediator variable, with a standardized coefficient of -0.04, has no significant effect on coronavirus anxiety. Meanwhile, cognitive attentional syndrome as a mediator variable, with a standardized coefficient of 0.22, significantly affects the coronavirus anxiety variable (Fig. 1). Overall, these results indicate that the present model can explain 50% of the variance of coronavirus anxiety. Therefore, it can be concluded that health-related metacognitive beliefs significantly affect coronavirus anxiety directly and through the cognitive attentional syndrome (see Table 3).
Fig. 1.
Structural model of research with standardized coefficients. MCQ = Metacognitions About Health, CAS = Cognitive Attentional Syndrome Scale, DTS = Distress Tolerance Scale; CORANX = Coronavirus Anxiety Scale. ITEM 1 and ITEM 2 are created for coronavirus anxiety scale using item parceling method, so each one corresponds to the one parcel
Table 3.
Bootstrap test results for mediator effects
| Independent variable | Mediator variable | Dependent variable | Bootstrap limits | Standard error | Effect Size | p-value | |
|---|---|---|---|---|---|---|---|
| Upper limit | lower limit | ||||||
| MCQ-HA | Distress tolerance | Coronavirus anxiety | 0.043 | − 0.122 | 0.050 | − 0.039 | 0.431 |
| MCQ-HA | Cognitive attentional syndrome | Coronavirus anxiety | 0.269 | 0.145 | 0.038 | 0.207 | 0.001 |
Discussion
This study aimed to investigate the mediating role of the cognitive attentional syndrome and distress tolerance in the relationship between health-related metacognitive beliefs and coronavirus anxiety. The results showed that cognitive attentional syndrome, the maladaptive behaviors that people use to cope with their negative feelings and thoughts, has a high impact on the formation and development of coronavirus anxiety.
The present study's findings indicate that metacognitive beliefs related to health are important, influential factors in the development of COVID-19 anxiety. It suggests that the constant, repetitive ruminations around the potential development of disease are a strong predictor of coronavirus anxiety. This finding is consistent with previous research that has shown that metacognitive beliefs, especially the uncontrollability of thoughts that people have about their health, predict the symptoms of health anxiety (Barenbrügge et al., 2013; Brown et al., 2019; Hashemi et al., 2020; Kaur et al., 2011; Melli et al., 2018; Rachor & Penney, 2020; Ramos-Cejudo & Salguero, 2017; Wells, 2013).
Furthermore, the results suggest that metacognitive beliefs about health are partly involved in developing coronavirus anxiety in individuals through the activation and maintenance of the cognitive attentional syndrome. Coronavirus anxiety arises from repetitive negative thinking associated with worry, rumination, and inappropriate control strategies. According to the metacognitive model of health anxiety, this anxiety arises from repetitive negative thoughts about the disease. These results harmonize with previous studies that found that metacognitive beliefs are an important factor in developing health anxiety and that metacognitions about biased thinking can independently affect health anxiety (Rachor & Penney, 2020); Thus, metacognitive beliefs about health are not only related to health anxiety in general, but also with coronavirus anxiety, as demonstrated by our findings.
Based on the result, it can be argued that health-related metacognitive beliefs, apart from their direct association with COVID-19 anxiety, have a significant indirect effect on the COVID-19 anxiety with the mediating role of the cognitive attentional syndrome; The first time being examined in the current study. Among the components of the CAS, rumination, worry, and other maladaptive behaviors and strategies that people adopt when faced with threats, also play a major part in coronavirus anxiety. These findings are consistent with studies by Bailey and Wells that showed that the CAS maintains and exacerbates the trend of worrying and ruminating about the potential disease that can predict health anxiety (Bailey and Wells, 2015a, 2015b); This is the same with metacognitive beliefs, CAS is not only related with health anxiety in general, but also with coronavirus anxiety, as shown by our findings.
However, health-related metacognitive beliefs mediated by distress tolerance had no significant effect on coronavirus anxiety which was against our proposed theoretical model. Some authors have argued that distress tolerance can play an important role in the formation and persistence of some mental disorders (Robinson et al., 2019). Also, studies on COVID-19 have suggested that lower distress tolerance is associated with an increased risk of depression, anxiety, and PTSD symptoms (Liu et al., 2020; Wright et al., 2020). Yet, our findings showed that distress tolerance did not significantly influence the formation of coronavirus-related anxiety. In particular, the current data are consistent with Sauer et al.'s (2020) findings, which showed that distress tolerance does not affect the development of health and coronavirus anxiety. Our study and Sauer et al.'s (2020) study both used a self-report measure of emotional DT; however, if a measure focusing on the behavioral component of DT was used, future research might find a significant pattern. However, our findings suggest that COVID-19 anxiety may develop regardless of how a person can tolerate negative emotional states; it is more cognitive and about persisting on chains of maladaptive thinking and worry. There may be another cause for the insignificant link between emotional DT and coronavirus anxiety in the tested model despite the significant bivariate correlation between these two variables. It may be due to the inclusion of metacognitive beliefs as a predictor of DT in the model. Considered as a whole, additional research is required to determine whether DT types (e.g., behavioral) would alter the results and, if not, whether metacognitive beliefs are more relevant than distinct types of DT.
To conclude, dysfunctional metacognitive beliefs, including an individual's beliefs about the uncontrollability of disease-related thoughts, act as a risk factor that has a detrimental effect on mental health and leads to anxiety disorders such as health anxiety (i.e., coronavirus anxiety). In addition, the association of dysfunctional beliefs with maladaptive behaviors resulting from cognitive attentional syndrome is also involved in predicting coronavirus anxiety. These results suggest that individuals with highly dysfunctional beliefs about their illness and health are more likely to ruminate. Subsequently, these individuals engage in destructive maladaptive behaviors to eliminate dysfunctional thoughts, which increases their anxiety and entanglement in this cycle. Moreover, it should be noted that we have used emotional DT measures, which, by non-significant mediating role of DT, stress the importance of other types of DT (Akari et al., 2021a; for a review), such as tolerance of physical sensations, tolerance of ambiguity and uncertainty, and tolerance of frustration; by using any related measures to the different type of DT, future studies might shed light on different pattern than ours and extend on our understanding on the possible role of DT in the context of COVID-19.
Due to the widespread prevalence of this epidemic, the duration since its onset, the exhausting conditions of quarantine, and the problems it has caused (Cao et al., 2020; Fiorillo et al., 2020; Luo et al., 2020), paying special attention to COVID-19 anxiety during this period and even after is necessary. To alleviate psychological distress and reduce anxiety, we need to apply interventions to correct dysfunctional metacognitive beliefs, such as Metacognitive Therapy (Wells, 2009). The current study's significance would be in demonstrating that COVID-19 anxiety has more cognitive than emotional aspects; thus, clinicians may like to place a greater emphasis on the cognitive component of COVID-19 anxiety, as emotional distress tolerance was not found to underlie the association between metacognitions about health and COVID-19 anxiety. It appears that assisting clients in overcoming worry, maladaptive coping strategies, and maladaptive metacognition about health would reduce COVID-19 anxiety.
However, all findings should be interpreted in light of the limitations. The first limitation of this study is the self-report form of the scales, which does not allow comorbidities and acute psychological disorders to be investigated. Second, the present study has a cross-sectional design; thus, the reported results show relationships, and the causal relationships between variables cannot be concluded. Also, the overrepresentation of females in the current study may restrict the generalizations of the findings to males. Future studies might want to target the clinical population or a more gender-balanced sample using a longitudinal or multi-wave measurements design to overcome the mentioned limitations and to expand our understanding of the relationship between metacognitions about health and COVID-19 anxiety, with more focus on the maintaining and exacerbating role of the cognitive attentional syndrome as the underlying mechanism of the aforementioned.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
The authors confirm that the data supporting the findings of this study are available.
Declaration
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could influence the work reported in this paper.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- ADAA. (2020). Coronavirus anxiety—Helpful expert tips and resources. Anxiety and Depression Association of America, ADAA. Retrieved 22nd May, 2020, from https://adaa.org/finding-help/coronavirus-anxiety-helpfulresources.
- Ahmed, M. Z., Ahmed, O., Aibao, Z., Hanbin, S., Siyu, L., & Ahmad, A. (2020). The epidemic of COVID-19 in China and associated psychological problems. Asian Journal of Psychiatry, 51, 102092. 10.1016/j.ajp.2020.102092. [DOI] [PMC free article] [PubMed]
- Ahorsu, D. K., Lin, C. Y., Imani, V., Saffari, M., Griffiths, M. D., & Pakpour, A. H. (2020). The fear of COVID-19 scale: Development and initial validation. International Journal of Mental Health and Addiction, 1–9.10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed]
- Akbari, M. (2019). Students' health anxiety prediction based on the emotional inflexibility, metacognitions about health, and anxiety sensitivity. Contemporary Psychology,25, (Suppl.), 69–74.
- Akbari, M., Hosseini, Z. S., Seydavi, M., Zegel, M., Zvolensky, M. J., & Vujanovic, A. A. (2021a). Distress tolerance and posttraumatic stress disorder: A systematic review and meta-analysis. Cognitive behaviour therapy, 1–30. [DOI] [PubMed]
- Akbari M, Disabato D, Seydavi M, Zamani E. The Persian personalized psychological flexibility index (P-PPFI): Psychometric properties in a general population sample of Iranians. Journal of Contextual Behavioral Science. 2021;22:32–43. doi: 10.1016/j.jcbs.2021.09.004. [DOI] [Google Scholar]
- Akbari, M., Seydavi, M., & Zamani, E. (2021c). The mediating role of personalized psychological flexibility in the association between distress intolerance and psychological distress: A national survey during the fourth waves of COVID-19 pandemic in Iran. Clinical Psychology & Psychotherapy, 1–11. 10.1002/cpp.2685. [DOI] [PMC free article] [PubMed]
- Akbari M, Seydavi M, Zamani E, Nikčević AV, Spada MM. The Persian COVID-19 Anxiety Syndrome Scale (C-19ASS): Psychometric properties in a general community sample of Iranians. Clinical Psychology & Psychotherapy. 2021 doi: 10.1002/cpp.2686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey R, Wells A. Metacognitive beliefs moderate the relationship between catastrophic misinterpretation and health anxiety. Journal of Anxiety Disorders. 2015;34:8–14. doi: 10.1016/j.janxdis.2015.05.005. [DOI] [PubMed] [Google Scholar]
- Bailey, R., & Wells, A. (2015b) Development and initial validation of a measure of metacognitive beliefs in health anxiety: The MCQHA. Psychiatry Research, 230(3), 871–877. (ISSN 01651781). [DOI] [PubMed]
- Bailey R, Wells A. Illness beliefs in predicting health anxiety: An evaluation of the metacognitive versus the cognitive models. The Australian Psychological Society. 2015 doi: 10.1111/cp.12078. [DOI] [Google Scholar]
- Barenbrügge J, Glöckner-Rist A, Rist F. Positive and negative Metakognitionen über Krankheitssorgen. Psychotherapeut. Psychotherapeut. 2013;58(6):560–568. doi: 10.1007/s00278-013-1016-2. [DOI] [Google Scholar]
- Brown, R. J., Skelly, N., Chew-Graham, C. A. (2019). Online health research and health anxiety: a systematic review and conceptual integration, Clinical Psychology Science and Practice, 27(2). 10.1111/cpsp.12299.
- Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, Hi L, Sheng C, Cai Y, Li X, Wang J, Zhang Z. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):6–15. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi Tam, C., Sun, S. H., Yang, X., Li, X., Zhou, Y., & Shen, Z. (2020). Psychological distress among HIV healthcare providers during the COVID-19 pandemic in China: Mediating roles of institutional support and resilience. AIDS and Behavior, 21, 1–9. 10.1007/s10461-020-03068-w. [DOI] [PMC free article] [PubMed]
- Chou CP, Bentler PM. Estimates and tests in structural equation modeling. In: Hoyle RH, editor. Structural equation modeling: Concepts, issues, and applications. Sage Publications Inc; 1995. pp. 37–55. [Google Scholar]
- Creed F, Tomenson B, Chew-Graham C, Macfarlane G, McBeth J. The associated features of multiple somatic symptom complexes. Journal of Psychosomatic Research. 2018;112:1–8. doi: 10.1016/j.cbpra.2006.01.005. [DOI] [PubMed] [Google Scholar]
- Enitan SS, Ibeh IN, Oluremi AS, Olayanju AO, Itodo GE. The 2019 novel coronavirus outbreak: Current crises, controversies, and global strategies to prevent a pandemic. International Journal of Pathogen Research. 2020;4(1):1–16. doi: 10.9734/ijpr/2020/v4i130099. [DOI] [Google Scholar]
- Farrokhi H, Sohrabi F. Investigating reliability, validity and factor structure of the persian version of the cognitive attentional syndrome (CAS-1) Journal of Analytical-Cognitive Psychology. 2017;8(30):9–15. [Google Scholar]
- Felton, J. W., Strutz, K. L., McCauley, H. L., Poland, C. A., Barnhart, K. J., Lejuez, C. W. (2019). Delay Discounting interacts with distress tolerance to predict depression and alcohol use disorders among individuals receiving inpatient substance use services. International Journal of Mental Health and Addiction, 18(5), 1416–1421. 10.1007/s11469-019-00163-5. [DOI] [PMC free article] [PubMed]
- Fergus TA, Bardeen JR. Anxiety sensitivity and intolerance of uncertainty: Evidence of incremental specificity about health anxiety. Personality and Individual Differences. 2013;55:640–644. doi: 10.1016/j.paid.2013.05.016. [DOI] [Google Scholar]
- Fergus TA, Bardeen JR, Orcutt HK. Attentional control moderates the relationship between activation of the cognitive attentional syndrome and symptoms of psychopathology. Personality and Individual Differences. 2012;53:213–217. doi: 10.1016/J.PAID.2012.03.017. [DOI] [Google Scholar]
- Fergus TA, Bardeen JR, Orcutt HK. Examining the specific facets of distress tolerance that are relevant to health anxiety. Journal of Cognitive Psychotherapy. 2015;29:32–44. doi: 10.1891/0889-8391.29.1.32. [DOI] [PubMed] [Google Scholar]
- Fergus TA, Scullin MK. The cognitive attentional syndrome is associated with sleep difficulties in a community sample. Behavioral Sleep Medicine. 2017;15(5):410–420. doi: 10.1080/15402002.2016.1141771. [DOI] [PubMed] [Google Scholar]
- Fergus TA, Valentiner DP, McGrath PB, Gier-Lonsway S, Jencius S. The cognitive attentional syndrome: Examining relations with mood and anxiety symptoms and distinctiveness from psychological inflexibility in a clinical sample. Psychiatry Research. 2013;210:215–219. doi: 10.1016/J.PSYCHRES.2013.04.020. [DOI] [PubMed] [Google Scholar]
- Fiorillo A, Sampogna G, Giallonardo V, Del Vecchio V, Luciano M, Albert U, Carmassi C, Carra G, Cirulli F, DellOsso B, Giulia Nanni M, Pompili M, Sani G, Tortorella A, Volpe U. Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: Results from the COMET collaborative network. European Psychiatry. 2020;63(1):e87. doi: 10.1192/j.eurpsy.2020.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher, M. W., Zvolensky, M. J., Long, L. J., Rogers, A. H., & Garey, L. (2020). The impact of Covid-19 experiences and associated stress on anxiety, depression, and functional impairment in American adults. Cognitive Therapy and Research, 1–9. 10.1007/s10608-020-10143-y. [DOI] [PMC free article] [PubMed]
- Gutierrez, R., Hirani, T., & Curtis, L. (2020). Metacognitive beliefs mediate the relationship between anxiety sensitivity and traits of obsessive-compulsive symptoms. BMC Psychology, 8(1), 40. 10.1186/s40359-020-00412-6. [DOI] [PMC free article] [PubMed]
- Hashemi SGH, Hosseinnezhad SH, Dini S, Griffiths MD, Lin CY, Pakpour AH. The mediating effect of the cyberchondria and anxiety sensitivity in the association between problematic internet use, metacognition beliefs, and fear of COVID-19 among the Iranian online population. Heliyon. 2020 doi: 10.1016/j.heliyon.2020.e05135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jöreskog, K. G., & Sörbom, D. (2006). LISREL 8.8 for windows [computer software]. Scientific Software International Inc
- Jungmann, S. M., & Witthoft, M. (2020). Health anxiety, cyberchondria, and coping in the current COVID-19 pandemic: Which factors are related to coronavirus anxiety?. Journal of Anxiety Disorders. 10.1016/j.janxdis.102239. [DOI] [PMC free article] [PubMed]
- Kaur A, Butow P, Thewes B. Do metacognitions predict attentional bias in health anxiety? Cognitive Therapy and Research. 2011;35:575–580. doi: 10.1007/s10608-011-9387-6. [DOI] [Google Scholar]
- Keough ME, Riccardi CJ, Timpano KR, Mitchell MA, Schmidt NB. Anxiety symptomatology: The association with distress tolerance and anxiety sensitivity. Behavior Therapy. 2010;41(4):567–574. doi: 10.1016/j.beth.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline, R. B. (2011). Methodology in the social sciences. Principles and practice of structural equation modeling (3rd ed.). Guilford Press.
- Kline, R. B. (2015). Principles and practice of structural equation modeling. Guilford publications.
- Kowalski J, Wypych M, Marchewka A, Dragan M. Neural correlates of cognitive-attentional syndrome: an fmri study on repetitive negative thinking induction and resting-state functional connectivity. Frontiers in Psychology. 2019 doi: 10.3389/fpsyg.2019.00648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. International Journal of Antimicrobial Agents. 2019;55(3):105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laposa JM, Collimore KC, Hawley LL, Rector NA. Distress tolerance in OCD and anxiety disorders, and its relationship with anxiety sensitivity and intolerance of uncertainty. Journal of Anxiety Disorders. 2015;33:8–14. doi: 10.1016/j.janxdis.2015.04.003. [DOI] [PubMed] [Google Scholar]
- Leahy RL, Wupperman P, Edwards E, Shivaji SS, Molina N. Metacognition and emotional schemas: Effects on depression and anxiety. International Journal of Cognitive Therapy. 2018 doi: 10.1007/s41811-018-0035-8. [DOI] [Google Scholar]
- Lee, S. A. (2020a). Replication analysis of the coronavirus anxiety scale. The Journal of Psychiatry and Neurological Sciences, 33.
- Lee SA. How much "Thinking" about COVID-19 is clinically dysfunctional? Brain, Behavior, and Immunity. 2020;87:97–98. doi: 10.1016/j.bbi.2020.04.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SA, Jobe MC, Mathis AA, Gibbons JA. Incremental validity of coronaphobia: Coronavirus anxiety explains depression, generalized anxiety, and death anxiety. Journal of Anxiety Disorders. 2020;74:102268. doi: 10.1016/j.janxdis.2020.102268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SA, Mathis AA, Jobe MC, Pappalardo EA. Clinically significant fear and anxiety of COVID-19: A psychometric examination of the Coronavirus Anxiety Scale. Psychiatry Research. 2020;290:113112. doi: 10.1016/j.psychres.2020.113112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SA, Park CL, Russell BS. Does distress tolerance interact with trait anxiety to predict challenge or threat appraisals? Personality and Individual Differences. 2018;132:14–19. doi: 10.1016/j.paid.2018.05.014. [DOI] [Google Scholar]
- Leyro, T. M., Zvolensky, M. J., & Bernstein, A. (2016). Distress tolerance and psychopathological symptoms and disorders: a review of the empirical literature among adults. Psychological Bulletin, 136, 576. 10.1037/a0019712. [DOI] [PMC free article] [PubMed]
- Liu, C. H., Zhang, E., Wong, G. T. F., Hyun, S., Hahm, H. C. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Research. 290, 113172. 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed]
- Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Research. 2020;291:113190. doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza C, Ricci E, Biondi S, Colasanti M, Ferracuti S, Napoli C, Roma P. A nationwide survey of psychological distress among Italian people during the COVID-19. International Journal of Environmental Research and Public Health. 2020;17(9):3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay, D., Yang, H., Elhai, J., & Asmundson, G. (2020). Anxiety regarding contracting COVID-19 related to interoceptive anxiety sensations: The moderating role of disgust propensity and sensitivity. Journal of Anxiety Disorders, 102233. 10.1016 /j. janxdis.2020.102233. [DOI] [PMC free article] [PubMed]
- Melli G, Bailey R, Carraresi C, Poli A. Metacognitive beliefs as a predictor of health anxiety in a self-reporting Italian clinical sample. Clinical Psychology & Psychotherapy. 2018;25(2):263–271. doi: 10.1002/cpp.2159. [DOI] [PubMed] [Google Scholar]
- Mohammadpour, M., Ghorbani, V., Moradi, S., Khaki, Z., Foroughi, A. A., & Rezaei, M. R. (2020). Psychometric properties of the Iranian version of the coronavirus anxiety scale. Iranian Journal of Psychiatry and Clinical Psychology, 26(3), 374–387. http://ijpcp.iums.ac.ir/article-1-3270-fa.html
- Nikčević AV, Marino C, Kolubinski DC, Leach D, Spada MM. Modelling the contribution of the Big Five personality traits, health anxiety, and COVID-19 psychological distress to generalised anxiety and depressive symptoms during the COVID-19 pandemic. Journal of Affective Disorders. 2021;15:578–594. doi: 10.1016/j.jad.2020.10.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papageorgiou C, Wells A. A prospective test of the clinical metacognitive model of rumination and depression. International Journal of Cognitive Therapy. 2009;2:123–131. doi: 10.1521/ijct.2009.2.2.123. [DOI] [Google Scholar]
- Rachor GS, Penney AM. Exploring metacognitions in health anxiety and chronic pain: A cross-sectional survey. BMC Psychology. 2020 doi: 10.1002/da.20469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos-Cejudo J, Salguero JM. Negative metacognitive beliefs moderate the influence of perceived stress and anxiety in long-term anxiety. Psychiatry Research. 2017;250:25–29. doi: 10.1016/j.psychres.2017.01.056. [DOI] [PubMed] [Google Scholar]
- Ranney, R. M., Bing-Canar, H., Paltell, K. C., Tran, J. K., Berenz, E. C., & Vujanovic, A. A. (2020). Cardiovascular risk as a moderator of associations among anxiety sensitivity, distress tolerance, PTSD, and depression symptoms among trauma-exposed firefighters. Journal of Psychosomatic Research. 10.1016/j.jpsychores.2020.110269. [DOI] [PubMed]
- Robinson, M., Ross, J., Fletcher, S., Burns, C. R., Lagdon, S., & Armour, C. (2019).The mediating role of distress tolerance in the relationship between childhood maltreatment and mental health outcomes among university students. Journal of Interpersonal Violence, 1–25. 10.1177/0886260519835002. [DOI] [PubMed]
- Sauer KS, Jungmann SM, Witthöft M. Emotional and behavioral consequences of the COVID-19 pandemic: The role of health anxiety, intolerance of uncertainty, and distress (In)tolerance. Environmental Research and Public Health. 2020;17:7241. doi: 10.3390/ijerph17197241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sica C, Steketee G, Ghisi M, Chiri LR, Franceschini S. Metacognitive beliefs and strategies predict worry, obsessive-compulsive symptoms and coping styles: A preliminary prospective study on an Italian non-clinical sample. Clinical Psychology & Psychotherapy. 2007;14(4):258–268. doi: 10.1002/cpp.520. [DOI] [Google Scholar]
- Simons JS, Gaher RM. The distress tolerance scale: Development and validation of a self-report measure. Motivation and Emotion. 2005;29(2):83–102. doi: 10.1007/s11031-005-7955-3. [DOI] [Google Scholar]
- Spada MM, Caselli G, Nikčević AV, Wells A. Metacognition in addictive behaviours. Addictive Behaviors. 2015;44:9–15. doi: 10.1016/j.addbeh.2014.08.002. [DOI] [PubMed] [Google Scholar]
- Taylor S, Asmundson GJG. Life in a post-pandemic world: What to expect of anxiety-related conditions and their treatment. Journal of Anxiety Disorders. 2020;72:102231. doi: 10.1016/j.janxdis.2020.102231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tehran times. (2022). Iran in sixth wave of pandemic: Health minister. Retrived February 17, 2022, from https://www.tehrantimes.com/news/469545/Iran-in-sixth-wave-of-pandemic-health-minister.
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells A. (2013). Cognitive therapy of anxiety disorders: A practice manual and conceptual guide. John Wiley & Sons.
- Wells A. Metacognitive therapy for anxiety and depression. Guilford Press; 2009. [Google Scholar]
- Wells A, Hatton C. A short form of the metacognitions questionnaire: Properties of the MCQ-30. Behaviour Research and Therapy. 2004;42:385–396. doi: 10.1016/S0005-7967(03)00147-5. [DOI] [PubMed] [Google Scholar]
- Wells A, Matthews G. Attention and emotion: A clinical perspective. Lawrence Erlbaum Associates; 1994. [Google Scholar]
- World Health Organization. (2020a). Rolling updates on coronavirus disease (COVID-19): Events as they happen. World Health Organization https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-asthey-happen.
- World Health Organization. (2020b). WHO Coronavirus Disease (COVID-19) Dashboard. The latest statistics on corona patients and deaths in Iran on 24th April 2021.
- Wright CD, Nelson CI, Brumbaugh JT, McNeil D, W. The role of distress tolerance as a potential mechanism between anxiety sensitivity and Gut-Specific Anxiety. International Journal of Behavioral Medicine. 2020;27:717–725. doi: 10.1007/s12529-020-09912-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yilmaz AE, Gencoz T, Wells A. Unique contributions of metacognition and cognition to depressive symptoms. The Journal of General Psychology. 2015;142:23–33. doi: 10.1080/00221309.2014.964658. [DOI] [PubMed] [Google Scholar]
- Zegel, M., Rogers, A. H., Vujanovic, A. A., & Zvolensky, M. J. (2020). Alcohol use problems and opioid misuse and dependence among adults with chronic pain: The role of distress tolerance. Psychology of Addictive Behaviors. 10.1037/adb0000587. [DOI] [PubMed]
- Zhao, S., Chen, H. (2020). Modeling the epidemic dynamics and control of COVID-19 outbreak in China. Quantitative Biology (Beijing, China), 1–9. 10.1101/2020.02.27.20028639. [DOI] [PMC free article] [PubMed]
- Zhu H, Wei L, Niu P. The novel coronavirus outbreak in Wuhan, China. Global Health Research and Policy. 2020;5(1):6. doi: 10.1186/s41256-020-00135-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available.