Abstract
Using telehealth as a mode of service delivery has the potential to address some long-standing challenges in early intervention (EI) services such as waiting lists to access services. Yet, little is known about parent perceptions of telehealth in EI based on their lived experiences partnering with EI practitioners. The purpose of this study was to explore parent perceptions on using telehealth, especially on family-professional partnerships and coaching. Interviews were conducted with 15 parents of children receiving EI services via telehealth from June to August of 2021. Almost half of the participants reflected under-represented racial and ethnic backgrounds. Constant comparative analysis and emergent coding were used for data analysis. The findings showed that the advantages outnumbered the disadvantages regarding telehealth. Participants reported that telehealth provided a safe and flexible option and eliminated the wait to access EI services. However, participants identified some disadvantages to telehealth including telehealth precluded substantive interactions with therapists and limited access to technology. The findings also indicated that telehealth enhanced family-professional partnerships. Nearly all participants valued coaching during telehealth. Participants suggested initial supports to facilitate EI via telehealth, including stable internet access, telehealth training, and an initial in-person visit. Implications for research and practice are discussed.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10882-022-09853-w.
Keywords: Telehealth, Early intervention, Family, Perspective
A Qualitative Study Exploring Parental Perceptions of Telehealth in Early Intervention
Across the United States, over 400,000 children receive early intervention (EI) services (Early Childhood Technical Assistance Center, 2020). Provided under the Individuals with Disabilities Education Act (IDEA, 2004), EI services address delays in development among young (aged 0–3) children with developmental delays and disabilities and their families. EI services may include speech therapy, physical and occupational therapies, nutrition services, and other services based on the needs of the child and family (DEC of the CEC, 2014). EI is family-centered using everyday activities as the intervention context to create multiple opportunities for children to practice their target skills to facilitate their development (Fleming et al., 2011). The importance of EI cannot be overstated. When families receive EI services, their children are more likely to participate in toilet training, mealtime, and bedtime routines. Often, children demonstrate significantly improved developmental trajectories (Fuller & Kaiser, 2020; Noyes-Grosser et al., 2018) and parents report improved quality of life (Epley et al., 2011). Without EI, children often regress in their health, language, cognitive, social and emotional development (Barton et al., 2012).
As of January 10, 2021, there have been 88 million cases and 1.9 million deaths due to COVID-19 (World Health Organization, 2020). Because of the pandemic, all in-person EI visits were initially suspended across the country to minimize contagion for families and EI providers (Edelman, 2020). In respond to a rapid shift in service delivery, many EI providers began using telehealth to serve young children with disabilities or delays. Allowing children to receive EI services in a safe environment, telehealth is a mode of service delivery that utilizes telecommunications and information technology to provide access to health care such as assessment, diagnosis, intervention, consultation, supervision, and education (Nickelson, 1998; Zoder-Martell et al., 2020). Telehealth enables services to be provided remotely via synchronous auditory and visual methods (Richmond et al., 2017). Some research has examined the effectiveness of providing services via telehealth (e.g., Aashima et al., 2021; Behl et al., 2017; Bennell et al., 2021; Blaiser et al., 2013; Little et al., 2018; Tenforde et al., 2020). However, the majority of studies used researchers, not EI practitioners, to conduct interventions via telehealth (for a review, see Author, in progress). In some models, however, researchers used telehealth to train and coach EI practitioners. For example, in a cascaded coaching model, a researcher trains and coaches a practitioner who supports a caregiver to use strategies with their child; however, research about the cascaded coaching model and its generalizability is still limited (Meadan et al., 2020). It is important to explore the use of telehealth among EI practitioners and families. Given that telehealth may be an ongoing modality in EI beyond the COVID-19 pandemic (Early Childhood Technical Assistance Center, 2020), it is critical to understand parent perceptions of telehealth in EI based on their lived experiences. Thus, the purpose of this study was to explore parent experiences with telehealth in EI services.
At the most basic level, it is critical to explore parent perceptions of access to EI services via telehealth. In the US, many parents report that telehealth is acceptable and feasible (Wainer & Ingersoll, 2015; Wallisch et al., 2019). Salomone and Maurizio Arduino (2017) conducted a survey with 43 parents of young children with autism to examine the feasibility of parent coaching via telehealth. The findings showed that parents’ internet skills predicated their satisfaction with telehealth. However, such extant research focuses on parent perceptions after they have used telehealth in research studies (Ashburner et al., 2016; Behl et al., 2017). Such studies often rely on convenience samples of families who self-select to receive services via telehealth. The samples may not generalize to families who have no choice (e.g., families who live in remote areas where access to service providers is limited or non-existent) but to use telehealth to access services. If telehealth remains a modality for EI services following the COVID-19 pandemic, it is critical to have a more holistic understanding of parent perceptions of access to EI services via telehealth.
Given the importance of involving families in EI (Callanan et al., 2021; Hughes-Scholes & Gavidia-Payne, 2019), it is also important to characterize parent perceptions of family-professional partnerships in EI using telehealth. Regardless of service delivery modality, EI providers support parents to facilitate their child’s learning and development; these partnerships help build family capacity and increase family resilience (Friedman et al., 2012). When parents have strong partnerships with EI providers, parents report less stress and greater satisfaction with EI services (Bruder & Dunst, 2015). However, none of the extant literature has examined whether family-professional partnerships change in relation to the mode of service delivery. To this end, it is critical to explore how the quality of the family-professional partnerships may change in relation to telehealth.
Coaching is a critical tenet of EI and one of the strategies to foster family-professional partnerships (Akhbari Ziegler & Hadders-Algra, 2020). However, coaching is not uniform (Akhbari Ziegler & Hadders-Algra, 2020; Ives, 2008). Coaching is generally referred to include adult learning strategies to promote a parent’s ability to support child learning and development in daily activities (Rush & Shelden, 2020). Coaching elements may include joint planning, observation, action/practice, reflection, and reciprocal feedback (Akhbari-Ziegler & Hadders-Algra., 2020; Rush et al., 2011). Coaching is widely agreed to lead to improved child outcomes (Akamoglu & Meadan, 2018; Heidlage et al., 2020). Unfortunately, EI providers often spend the majority of their time conducting direct intervention (versus coaching) during in-person EI visits (Campbell & Sawyer, 2007). Indeed, there is a research-to-practice gap with regard to coaching and direct intervention (Romano & Schnurr, 2020). Telehealth may be able to resolve this gap as, without the ability to directly interact with the child, providers may be more likely to use coaching practices.
Finally, it is critical to identify supports which can help families engage in EI via telehealth. In a study of parent perceptions of telehealth, many families, especially Spanish-speaking families, anticipated that a lack of internet access may inhibit their ability to participate in telehealth (Yang et al., 2021). However, with the right supports, telehealth may also be a way to reduce service disparities. For example, many Latinx families face a shortage of Spanish-speaking EI providers (Williams et al., 2013). Telehealth may enable families to access interpreters since the interpreters will not need to be local. If needed supports (e.g., interpreters, stable internet) can be identified and provided to families, they can participate in telehealth—especially families from marginalized backgrounds—then telehealth may be a way to reduce such inequity.
With COVID-19, the nature of service delivery is changing. While little extant research has examined parent perceptions of telehealth in EI, research has shown that parents of children with disabilities value telehealth in other modes of service delivery (Wainer & Ingersoll, 2015; Wallisch et al., 2019). Further, even after the COVID-19 pandemic, many states plan to continue to offer telehealth as a mode of service delivery (Early Childhood Technical Assistance Center, 2020) due to its cost-effectiveness and feasibility (Ashburner et al., 2016; Cason, 2009). Thus, it is critical to explore parent perceptions of telehealth in EI. This study had four research questions: (1) How do parents describe their experiences accessing EI services via telehealth?; (2) How do parents describe their partnerships with providers during telehealth?; (3) How do parents describe coaching during telehealth?; and (4) According to parents, what initial supports would help facilitate EI via telehealth?
Method
Participants
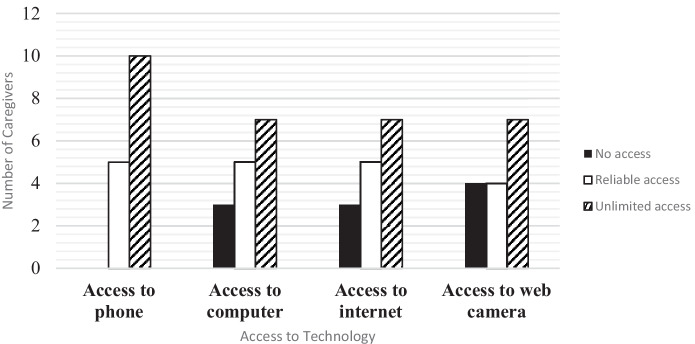
To be included in the study, each participant had to be a parent of a child who received EI services via telehealth and provided informed consent prior to engaging in the study. All participants were from a Midwestern state. Interviews were conducted with 15 parents of children receiving EI services via telehealth. The sample was racially diverse with 46.7% (n = 7) of the participants reflecting under-represented racial and ethnic backgrounds. Most participants were females (n = 14, 93.3%) and had completed some college or higher level of education (n = 11, 73.3%). The mean age of participants was 36.5 years (SD = 7.03). On average, the children of the participants were 27.6 months old (SD = 6.59). Also, nearly half of the participants had limited access to technology (see Fig. 1). On average, participants’ children received 3.25 services (range: 2-5). See Table 1.
Fig. 1.
Caregivers access to different types of technologies
Table 1.
Participant Demographics
| Participant | Age | Education | Income | Race or Ethnicity | Child gender | Child age (months) |
Child disability | Services received |
|---|---|---|---|---|---|---|---|---|
| Amy | 32 | Graduate Degree | > $100,000 | Asian | Male | 36 | DD | ST; DT; OT |
| Caroline | 53 | 4-year Degree | –- | –- | Male | 23 | SLI; DD | ST; DT; OT |
| Emily | 39 | Graduate Degree | $70-$99,999 | Black | Male | 24 | ASD | ST; DT; OT; PT; Nutrition |
| Helen | 35 | Graduate Degree | > $100,000 | White | Male | 14 | DD | ST; DT; OT; PT; Nutrition |
| Jenny | 33 | High school | $70-$99,999 | White | Female | 24 | DD | ST; OT |
| Katie | 25 | High school | $50-$69,999 | Latina | Male | 24 | SLI: DD; OI | ST; DT: OT; PT |
| Karen | – | Some College | $50-$69,999 | White | Male | 24 | Health Condition | ST; OT; PT; Nutrition |
| Lucy | 39 | Graduate Degree | > $100,000 | White | Male | 24 | SLI | ST; OT; PT |
| Nancy | 39 | High school diploma | $15-$29,999 | White | Male | 24 | ID; SLI; DD | DT; OT |
| Prisha | 33 | 4-year Degree | $70–99,999 | Asian | Male | 29 | DD; visual impairment | ST; DT; OT |
| Sally | 35 | Some College | $30-$49,999 | White | Female | 24 | SLI; | ST; DT |
| Sarah | 37 | 4-year Degree | $70-$99,999 | White | Male | 36 | ASD; DD | ST; DT; OT |
| Maria | 25 | High school | $15-$29,999 | Latina | Female | 36 | SLI | ST; DT; OT |
| Leticia | 44 | Some College | $30-$49,999 | Latina | Female | 36 | - | DT; OT; PT |
| Juana | 42 | Some College | $15-$29,999 | Latina | Female | 36 | - |
All participant names are pseudonyms. SLI Speech/language Impairment, ASD Autism Spectrum Disorder, DD Developmental Delay, ID Intellectual Disability, OI Orthopedic Impairment, OT Occupational Therapy, DT Developmental Therapy, ST Speech Therapy, PT Physical Therapy
Recruitment
To recruit participants, the authors shared the recruitment flyer with community agencies who served families of children receiving EI services. All recruitment materials were available in English and Spanish. Participants were recruited from June to August of 2021. At the time of recruitment, the midwestern state in which this study took place had COVID-19 in-person restrictions to EI services. If participants were interested in the study, they contacted the research team. The team members shared information about the study. If an individual agreed to participate and met the inclusionary criteria, then the individual completed the consent form. Each participant received a $20 gift card for their participation. Specifically, each participant received a $10 gift card after the interview and a $10 gift card after the member check. Recruitment was ongoing until we reached a redundancy of themes (Bowen, 2008).
Procedures
This study was approved by the University Institutional Review Board. Data were collected via a demographic questionnaire and a semi-structured interview protocol. The participants selected the time, date, and mode (i.e., phone call or Zoom platform) for the interview. Most interviews (n = 9; 60%) were conducted over Zoom. Notably, Zoom is HIPPA compliant (McGill & Fiddler, 2021). Extant literature has suggested that in-person, phone and Zoom interviews may generate similar results (Gray et al., 2020; Sturges & Hanrahan, 2004).
At the beginning of each interview, the interviewer introduced themselves and shared their personal and professional relation to EI and disability. Additionally, the interviewer shared the purpose of the study, explained the consent form, and asked participants if they had any questions. During the interview, descriptive field notes (e.g., the interviewer recorded the tone of the participant) were taken. Additionally, to document the insights of the interviewer, reflective field notes were completed during and after the interview. Each interview lasted between 15 and 57 min (M = 30.93; SD = 11.89). All interviews were audio-recorded and transcribed verbatim, culminating in 177 single-spaced pages of transcripts. To ensure accuracy of transcripts and to check for fidelity to the interview protocol, the authors listened to the recordings along with each transcript. Fidelity was 100%.
Altogether, three interviews were conducted in Spanish. Each interview was transcribed verbatim by native Spanish speakers. After each interview was transcribed in Spanish, the interviews were translated into English and then back-translated into Spanish. The forward/back translation method is commonly used with interviews recorded in another language (Brislin, 1970).
Data Collection
Demographic Questionnaire
The demographic questionnaire collected information about participants: age, gender, race and ethnicity, number of children with and without disabilities, EI services the child received and preferred modality for EI services (i.e., in-person, telehealth, telephone). The questionnaire also included questions about access to technology (Fitton et al., 2017).
Interview Protocol
The interview protocol was developed utilizing extant literature about EI and telehealth (e.g., Wallisch et al., 2019; Yang et al., 2021). Experts in qualitative methodology, EI, and telehealth as well as parents of children with disabilities reviewed the protocol and provided feedback. Minor revisions (e.g., small changes to the wording of questions) were made based on their feedback. The finalized interview protocol was piloted with a parent of children with disabilities who received EI via telehealth. Based on the pilot, further revisions were made to the interview protocol (e.g., changes to the order of questions). See Appendix A for the protocol.
Researcher Identity
All authors have at least five years of experience working with children with disabilities and partnering with families. Since the authors have experience working with families of young children with disabilities, this can be a strength because they are familiar with the experiences of families. Additionally, two authors have family members with disabilities who received EI services. As such, they are familiar with the experiences of receiving EI services. Futhermore, one author is Latina and a native Spanish speaker. Accordingly, she is familiar with the Latinx culture and was able to interview participants in their native language. One author has experience providing services to young children via telehealth.
Data Analysis
To analyze the transcripts, the research team used constant comparative analysis (Glaser & Strauss, 1967) and emergent coding (Patton, 2002). First, to familiarize themselves with the data, each research team member read each transcript multiple times (Tesch, 1990). Then, they individually coded three interviews using a line-by-line approach. Specifically, each piece of data (i.e., line of transcripts) was compared with each research team member’s coded data, highlighted, and annotated with a specific phrase (Creswell, 2003). Then, each new piece of data was compared with the previously coded data to check if the data reflected a new idea or could be an existing code. A line could have multiple codes if multiple concepts were present. Then, the researchers met to compare codes and resolve any differences (e.g., naming of codes) until a consensus was met. This stage of coding resulted in 72 codes. Then, the team met to compare the codes for redundancy and created a codebook. With the codebook, the coding team returned to the transcripts and independently coded the data again. The team met to discuss their codes and coded the remaining 12 interviews.
The team grouped the codes into categories and organized the categories into themes. To ensure internal homogeneity and external heterogeneity, categories were refined and confirmed (Braun & Clarke, 2006) by combining categories (e.g., “safest mode”, “convenient”, and “reduced health concerns”) with overlapping data into a larger category (e.g., “Telehealth provided a safe option to access EI services”), which reflected deeper analysis of thematic development. During the final stage of data analysis, a total of 27 categories were organized into four main themes with 13 supporting themes (e.g., “Advantage: Telehealth provided a safe option to access EI services”). After all transcripts were coded, the team discussed and confirmed the codes, categories, and themes.
Credibility and Trustworthiness
To ensure credibility and trustworthiness, the authors conducted first- and second-level member checks, peer debriefing, and had personal connections to the topic of study (Brantlinger et al., 2005). First-level member checks were conducted at the end of each interview. Specifically, the interviewer offered a summary of the interview to each participant; no participant offered changes. Second-level member checks were used to authenticate the analysis (Brantlinger et al., 2005). Specifically, after reading a transcript, a summary of the interview was developed and it was sent to participants to determine the summary’s accuracy. Of the 15 participants, three participants added information to their summary. Additionally, the authors participated in weekly peer debriefing. During these meetings, the team discussed data analysis and the interpretation of results. Finally, the authors’ personal connections to children with disabilities and their families, ensured they valued the experiences of families receiving EI services. To address biases and the values of the authors, researcher reflexivity was conducted.
Results
Accessing EI Services Through Telehealth
Advantage: Telehealth Provided a Safe Option to Access EI Services
In the context of the COVID-19 pandemic, 13 participants reported being grateful that telehealth was an option to receive EI services. Specifically, participants reported that they liked the convenience of telehealth as it allowed the families to stay home and safe without worrying about contacting COVID-19. Karen was the mother of a 2-year-old son with a history of brain bleeding, leukemia, and seizures. Through EI, her son received all services via telehealth. She reported that telehealth gave her “The ability to have more comfort and safeness due to the world, and my son's condition, with leukemia.” Similarly, Sally, the mother of a 2-year-old son with a speech-language impairment, appreciated the safety afforded by telehealth. She reported, “The visits allow us to see someone in-person without actually having to be in-person.”
Advantage: Telehealth Eliminated the Wait for EI Services
Twelve participants reported that, without telehealth, they may not have received any EI services. At the time of the interview, many families were waiting for EI in-person services due to the statewide shortages of EI providers. Sarah, the mother of a 3-year-old son with autism, was waiting for speech therapy (ST), occupational therapy (OT), and developmental therapy (DT). Solely because of telehealth, she reported being able to receive those services: “I would rather have some therapies than none. We were already on a long waitlist… So, it [telehealth] just gave us the opportunity to even do therapy where if it weren't for that I don't think we would have been able to have services, or we would have had to wait so long that there really would have been a huge opportunity cost.”
Advantage: Telehealth Made Access to EI Services More Flexible
Ten participants reported that access to EI services was more flexible because of telehealth. Katie was the mother of a 2-year-old child with a speech-language impairment, developmental delay, and orthopedic impairment. She reported: “Sometimes, I have things come up–doctor's appointments or stuff like that–and it [telehealth] was a little bit more flexible. If I couldn't do that day, or we could switch it out for another day or, you know, making an earlier or later time.” Other participants commented on the flexibility in location provided by telehealth. Caroline, the mother of a 2-year-old boy with a speech-language impairment and developmental delay, explained: “We're out visiting or something like that, he [son] could have his visits somewhere else. Just have his device with me or log in on someone else's device. Like one day we were in the car, and I just set it up.”
Advantage and Disadvantage: Nuanced Family Participation in EI Services
Eleven participants reported being very involved in EI services via telehealth. During telehealth sessions, participants reported fulfilling roles such as “instructor” and “facilitator” so their child could participate in EI. Karen reported being more involved in telehealth (versus in-person) services: “[I am] making sure that I fully understand what I needed to do for my child, because I was acting as the therapist, to make sure everything was described properly. She [provider] not only is trying to instruct the child. She's making sure that I do it correctly.” Similarly, Jenny, the mother of a daughter with developmental delay who received OT and ST, stated: “It's on me to redirect her [daughter]. [Over telehealth], they [the therapists] are not physically able to do anything. So, it's me as a parent having to understand that I have to get her [daughter] to do this thing.” In tandem with their high involvement, participants reported challenges. Specifically, participants reported that managing their children’s behaviors during the telehealth session in addition to trying to listen to the therapist was difficult. Amy, the mother of a 3-year-old boy with developmental delays, stated: “It's just a little more to manage with like the phone and or even the laptop and the screen and just kind of managing both his behaviors and also like doing actual therapy.”
Disadvantage: Telehealth Precluded Substantive Interactions with Therapists
Six participants reported that telehealth made it difficult for them and their children to meaningfully interact with EI providers. Emily, the mother of a 2-year-old boy with autism, was worried about the limited socialization with her providers. She stated, “I don't think it [telehealth] worked well for him cause she [the provider] didn't really have that interaction with him”. The limited engagement between the provider and the child may be due to the child losing focus and being disinterested in appearing on a screen. Caroline, a mother of a son with speech- language impairments and developmental delays, stated: “It was hard to grasp his [son’s] attention and engage with them [providers]. When they [providers] were in-person, it's like he was engaging. He loved it. He was able to focus on one thing and has a little bit more patience. Once the pandemic hit, we went to the Video therapy [telehealth]. It was a bit harder because he had to learn how to stay still and focused so he had to increase his patience level and stuff. It was kinda difficult [for him] to engage with them.” Notably, participants reported that child engagement increased over time. Leticia, the mother of a 3-year-old daughter with developmental delay, noticed this shift in their child. She shared: “Because she [daughter] didn't want to, at the beginning she didn't want to be in front of the screen much, but later the therapists told me to let her go and she would go by herself and when she saw that I was sitting down, she would go and sit with me and then the girls [therapists] would start talking to her. They [therapist] would start telling her, she would show her a book. She started to like it more, she would run and she would sit down and little by little she started to like that.”
Disadvantage: Limited Access to Technology Made Access to Telehealth Difficult
Only three participants reported lacking technology to participate in telehealth. Specifically, some participants reported limited: devices, stable internet, digital literacy and/or online platforms. Maria, the mother of a 3-year-old daughter with a speech-language impairment, was frustrated that their telehealth was interrupted frequently because of unreliable internet access. She reported: “We didn't have a good connection. Well, we didn't have internet services here at home then. We had get to internet service to have this better connection.” Similarly, Caroline, the mother of a child with developmental delays, said: “With speech [therapy], there's a lot of lip reading involved and things like that and there's just so much….‘What was that? I couldn't hear.’ A lot of times, it's almost every time, it's a bad connection.”
Regarding access to devices and online platforms, five participants had to locate devices to use and, because of their lack of access, reported limited digital literacy. Emily, the mother of a boy with autism, stated: “I do know that not all parents, not all parents know how to work technology. Not all parents know [how to use the] iPad, or iPhones with FaceTime. So, maybe for those parents, you know, maybe like a loaner laptop or something could have been provided.” Regarding platforms, some participants faced challenges with the online platforms (e.g. Zoom, Google Meets, etc.). Karen used Zoom during telehealth. She reported: “The only thing I didn't like was the Zoom… There was a time limit… Sometimes after the session is done, we just talk about how things were or talk about other things in general… The thing is with Zoom it will cut you off at a certain time, and it will end the call."
Mixed Perceptions of Family-Professional Partnerships
Positive Family-Professional Partnerships
All participants reported positive partnerships. They characterized their providers as: engaged, good listeners, supportive, caring, patient, helpful, flexible, and experienced. Put simply, Nancy reported: “I think they [providers] did a really awesome job of helping me with what we need to do with [my son].” Additionally, all participants reported positive communication with their providers during telehealth. Participants often spoke about well-established communication preferences such as texts, emails, and phone calls to build trust. Prisha, the mother of a child with cerebral palsy, reported: “The good thing about telehealth was, they [providers] were available anytime, because there were lots of doubts [about] doing live video visits [telehealth]. It's different from in-person. But then I could text them [therapists] anytime… and they replied right away. I think they were available [the] whole day because they also knew since it's online, everything is online so she might have some doubt on how to do this exercise with my child. They were like explaining and making videos and then sending it to me. So, they taught me everything.” Similarly, Jenny, the mother of a daughter with developmental delay, reported: “If I have questions I can reach out [to my therapists] throughout the week. [They] can always get back to me and had kind of like building that support structure for me personally, has really helped me be able to then in turn, become a support structure for my own child instead of relying on them [therapists] to be that for her.”
Frustrating Partnerships with Professionals
Two participants reported being frustrated with their providers because the providers asked them to purchase materials for telehealth sessions. Helen, the mother of a son with a developmental delay, reported: “[The speech therapist] recommending things for me to buy that I'm not going to buy because I already had one and gave it away prior. We have other things we can do. I don't need to buy this one thing. Stop talking about it.” Similarly, Caroline, the mother of a child with developmental delays, reported feeling frustrated with her providers because: “I have to go and get my own stuff or make it for the video visits.” In addition, two participants were frustrated that providers did not notify them to prepare materials before the sessions. Juana, the mother of a child with developmental delays, reported: “Maybe they would tell me [what] we're going to play next week. We're going to interact with this pasta, with rice or can you have some cubes, some blocks or can you have a paper and we can color. If they [providers] told me that, I could prepare.”
Coaching
Parents valued coaching
Fourteen participants valued coaching during telehealth. Participants reported that coaching enabled them to learn how to embed therapeutic strategies into daily activities. Jenny, the mother of a child with developmental delays, reported: “[Providers] have made me become more hands on with my daughter. So, instead of having someone sit in my home and work with her, I'm working with her through instruction and I think that's really awesome. It's made me a lot more comfortable doing that throughout our entire day instead of just that hour we're on the [telehealth] session.” Moreover, participants reported that coaching was clear, structured, and individualized. Amy, the mother of a child with a developmental delay, reported: “She [provider] would give me some feedback on trying to do these things with him, and we would do an activity [for] like 5–10 min. We would also build up his attention. So, she was giving me strategies to try to get him to stick with one activity a little longer because he kinda [was] bouncing a little bit from activity to activity. At the end of it, she would also wrap it up and say ‘These are the things we talked about’ and [give me] a little bit of homework in terms of what to work on next time and some home programs.” Notably, one participant reported receiving coaching even when an interpreter was present. Leticia, reported: “The therapists didn't speak Spanish, but the way they interpreted, it was very good. Very good communication and everything they [the interpreters] told me, I understood them. I was never left with a question.”
Some Frustration with Coaching Strategies
Although the majority of participants were positive about coaching during telehealth, two participants reported it was stressful and frustrating to receive coaching. Helen, the mother of twin boys with developmental delays, was frustrated about the coaching without feedback. She said: “Like we're talking to them [speech therapist and nutritionist] a lot, but it doesn't feel like we're involved. It feels more like we're just reporting things and taking in information, so it feels a lot more frustrating.” Similarly, Emily, the mother of a 2 year old boy with autism, said: “In the face of people [in-person visits], they [providers] can actually show you and model things. They have the object there and see how the child reacts with [the object]. But in the telehealth visits, you don’t have that… it will say that your child needs three months of therapy to get to this next milestone in the face-to-face therapy. For the telehealth therapy, it would need to be six months instead of three [months].”
Initial Supports to Facilitate EI via Telehealth
Stable Internet Access
Nine participants reported wanting stable internet access. Helen reported that, to access EI via telehealth, she had to upgrade her internet connection. She stated, “We actually had a little bit of a problem [with the internet connection] for a little while. Then, we upgraded our Wi-Fi and it stopped being an issue.” Accordingly, participants recommended providing families with access to stable internet. Helen further reported, “So, like that probably would be needed, making sure they [families] have internet.”
Telehealth Training
Twelve participants reported wanting training about telehealth. The training could include navigating online platforms (e.g., Zoom) and receiving an overview of telehealth (e.g., expectations and structure). Leticia reported it would be helpful for parents to participate in a training related to navigating online platforms because, “There are many of us that don’t know much about the technology and sometimes we don’t know [how] to use it or how to log-in. I know it was difficult for me.” Participants also reported wanting a brief training to provide an orientation to telehealth. Lucy explained that parents should have, “A little bit more direction like how to get the best out of the video visits [telehealth] you know like what to expect…Maybe a little more guidance on the behavior aspect of [the child] and the expectations for the video visits.”
Initial In-Person Visit
Two participants reported wanting an initial in-person visit. They reported that an initial in-person visit would help establish rapport between the family and the provider before receiving EI services via telehealth. Karen reported that an initial in-person meeting would be helpful for the parent to share information about the child. She stated, “Have a meet and greet and review the child’s levels, strengths, and weaknesses. Without the child there and [for the therapist to say] ‘Ok, this is what we’re going to do [during the sessions]’.” Similarly, Lucy reported, “In the beginning, it’s kind of hard. I felt like there wasn't a definitive plan in place. I feel like the first couple of sessions were kind of very, very confusing. Because he [son] doesn't really have a definitive diagnosis. What is he going to benefit from the most? … Once we kind of figured out then it was more smooth sailing. I think it would be so much easier if it was like in person at first and then we went to live video [telehealth].”
Discussion
In this study, we explored the perceptions of 15 parents of children who received EI services via telehealth. We had four main findings: advantages to accessing EI services via telehealth outnumbered the disadvantages; high-quality family-professional partnerships persevered during telehealth sessions; coaching was used during telehealth sessions; and logistical barriers need to be overcome to improve access to telehealth.
There were advantages and disadvantages to accessing EI services via telehealth. Overall, the advantages outnumbered the disadvantages. Notably, the advantages were not only COVID-19-specific but also may address some long-standing challenges in EI. For example, prior to COVID-19, the EI service system often struggled to meet the demand for EI services due to limited providers (Fenikil´e et al., 2015) and high costs (Little et al., 2018), leaving many families waiting for services. From this study, families reported being able to access EI only because of the telehealth modality. Indeed, research has demonstrated that 87% more children could receive therapy services if telehealth is an option (Cason et al., 2012). To ensure families can access telehealth, it may be helpful to have ways for troubleshooting technical issues such as delays in the audio transmission (Lee et al., 2015) as well as strategies for therapists to provide telehealth such as providing extra wait time (Lerman et al., 2020). Altogether, the advantages may outweigh the disadvantages in providing EI services via telehealth.
The other advantages were consistent with extant literature. Families often experience travel burdens when accessing services (Kogan et al., 2008). However, when services are offered via telehealth (versus in-person), families save mileage and experience reduced costs (Heitzman-Powell et al., 2013). This study complements the extant literature showing that the flexibility of telehealth was appreciated by families. This study also extends the literature suggesting that lived experience with receiving EI services via telehealth may change family perceptions of telehealth. Although Yang et al. (2021) found that caregivers preferred in-person (versus telehealth) EI visits prior to COVID-19, the pandemic (and corresponding shift to telehealth) may change parent perceptions to be more inclined to choose telehealth over in-person EI services.
For the most part, high-quality family-professional partnerships persevered during telehealth sessions. This finding is consistent with previous studies (Baharav & Reiser, 2010; Gibbs & Toth-Cohen, 2011; Vismara et al., 2012) that telehealth enhanced family-professional partnerships. The findings suggest that participants received support, coaching, and strengths-based information from their providers during telehealth sessions – key components of family-centered practices (DEC of the CEC, 2014). However, a few participants were frustrated their partnerships especially when they had to purchase materials for telehealth sessions. To this end, bagless therapy may be appropriate (Williams & Ostrosky, 2020). Bagless therapy means that the therapist only uses items in the home. Therapists may adapt household materials that are available and embed outcomes into naturally occurring everyday routines for children and families (Crawford & Weber, 2014). Thus, families can still implement EI strategies in everyday routines without relying on purchasing new materials or using materials brought by a therapist. Practitioners may consider using bagless therapy across modalities to strengthen family-professional partnerships.
While there was some frustration, coaching was used during telehealth sessions. Coaching delivered via telehealth has been demonstrated to improve child participation and parenting self-efficacy (Little et al., 2018), and be highly acceptable to families (Wallisch et al., 2019). The current study extends the literature by suggesting that practitioners can engage in coaching during EI sessions via telehealth. Of note, some providers used direct intervention rather than coaching. Because EI is family-centered, providers should consider relying on coaching more than direct intervention (Friedman et al., 2012). To be effective, EI providers need to strengthen their knowledge and skills about how to collaborate with and coach caregivers during the sessions to build caregiver capacity rather than conducting direct therapy. This finding reinforces that the research-to-practice gap with coaching may persist, even in telehealth sessions. Indeed, this finding may reflect that some EI providers struggle with coaching parents (Douglas et al., 2020). In particular, EI providers may find it difficult to coach parents in telehealth sessions due to the greater reliance on verbal stimuli. Similarly, some parents may be struggle to respond to the provider’s verbal instructions via telehealth. To this end, providers could send parents written instructions before the telehealth sessions. Providers also can work with parents to review the prior video-recorded sessions and provide feedback. More research and professional development may be needed for EI providers to improve coaching strategies.
Logistical barriers need to be overcome to improve access to telehealth. This study showcases that, while telehealth may resolve some inequity in accessing EI services, it also exacerbates some disparities. For example, rural families and underserved families may not have access to high-speed internet and digital literacy for using telehealth (Rideout & Katz, 2016). By providing devices, data plans, and training, such families may be able to access EI services via telehealth. This finding further extends the literature by suggesting that only providing a device may be insufficient to overcome disparities. In addition to devices, an initial in-person visit may be helpful to detect and resolve potential technological problems such as camera position, adequacy of Internet speed, compatibility of hardware and sofeware, and the assurance of direct and stable Internet connection (Lerman et al., 2020). Morevoer, training may be needed to enhance the digital literacy of the family. Notably, such training should be individualized to each family’s needs (Fraser et al., 2017).
Limitations
Despite providing an important jumping-off point, this study had a few limitations. First, due to its participants, this study has limited transferability. For example, this study was conducted in one midwestern state which had not offered EI services via telehealth prior to the COVID-19 pandemic. Other states which offered services via telehealth prior to COVID-19 may have families with different experiences. Second, because of the timing of this project, it is difficult to disentangle how the pandemic may have influenced participant responses. Research is needed during non-pandemic times to explore parent perceptions of telehealth. Third, this study reflected only one interview with each family. Findings suggest that their experiences with telehealth may change over time. Longitudinal data would be helpful to develop a more holistic understanding of their lived experiences with telehealth. Fourth, EI may include applied behavior analysis (ABA) services. However, in this study, none of our participants’ children received ABA via telehealth.
Directions for Future Research
There are many directions for future research. First, it is important to explore how parent experiences and background may impact their characterization and perceptions of EI via telehealth. In this study, we did not identify any patterns between parents who had previously received in-person services and parents who had only received services via telehealth. However, there may be differences depending on prior experiences. Indeed, while this study suggests that parents liked telehealth upon receiving it, other studies have found that parents who have only received in-person EI services do not prefer telehealth (Yang et al., 2021). Further, this study suggests that digital literacy may influence perceptions of telehealth. Indeed, digital literacy may impact parent perceptions of the efficacy of telehealth (Camden & Silva, 2021). In addition to prior experience and digital literacy, there may be other experiences and backgrounds which further influence parent perceptions of telehealth. Future research should identify such characteristics so targeted interventions can be developed to support families in receiving EI services via telehealth. There is also a need for observational research to understand how coaching practices may differ in telehealth (versus in-person) settings. This study suggested that many families enjoyed coaching; however, some providers were not coaching families during EI sessions. By observing EI sessions both in-person and via telehealth, there can be a comparison of the frequency of coaching strategies (e.g., guided practice with feedback; Rush & Shelden, 2020). Such observational data can help pinpoint similarities and differences in coaching between modalities and inform professional development to increase the use of coaching.
Implications for Practice
Practitioners should consider identifying solutions to overcome barriers in accessing EI services via telehealth. Many barriers were logistical (e.g., stable internet access; the need for devices and online platforms). Such logistical concerns point to service disparities with respect to socioeconomic status. Provider agencies may consider offering data plans to families who do not have consistent internet access. Providers may also consider offering a technology loan program so families can borrow devices to participate in telehealth sessions. Such solutions may help address barriers to access especially among marginalized families. As discussed in previous section, bagless therapy is one of other implications for practice align with prior research about in-person EI visits that can use in Telehealth. The use of telehealth as a service delivery modality for EI is in its infancy. Few studies have examined its use within the context of a statewide program. Based on this study, it is important to provide more training and support to providers on the use of coaching strategies in telehealth with families to empower their capacity and competence.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Appendix A Interview Protocol
-
Describe the Early Intervention services your child received before the COVID-19 pandemic. What types of services and how were they delivered?
Probe: How often?
Probe: Describe the interaction between each provider, caregiver, and child
-
How did you decide whether to participate in telehealth?
Probe: What questions did you have about telehealth?
Probe: How did your service coordinator and/or other EI Professionals discuss telehealth with you? Was coaching ever discussed?
Probe: Did you receive any materials about telehealth? If so, what was their effect?
-
Describe the Early Intervention services you receive now. What types of services and how are they delivered?
Probe: How often?
Probe: Describe the interaction between each provider, caregiver, and child
What expectations did you have for your providers during telehealth?
What expectations do providers have for you and your child during telehealth?
-
What do you like about telehealth?
Probe: What’s been going well?
Probe: Does that happen across all services?
-
What are some challenges you have experienced with telehealth?
Probe: Does that happen across all services?
Probe: How have you and/or the IFSP team addressed these challenges?
-
What support or resources do you think would make telehealth a better experience for families in general?
Probe: Would it be helpful to be able to record telehealth sessions?
Probe: Would it be helpful to include a training session of how to setup and use the online platform, which will be used for telehealth?
Probe: Would monthly calls for troubleshooting be helpful?
When in-person services become more available, how will you decide whether to return to in-person visits or keep live video visits?
Authors’ Contribution
All authors contributed to the study conception, design, and interpretation of results. Data analysis was performed by W. C. Cheung, J. Aleman-Tovar, A. N. Johnston, and M. M. Burke. The first draft of the manuscript was written by W. C. Cheung, J. Aleman-Tovar, A. N. Johnston, and M. M. Burke, and M. M. Burke and L. M. Little commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
The authors did not receive support from any organization for the submitted work.
Compliance with Ethical Standards
Ethics Approval
This study was approved by the University Institutional Review Board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to Participants
Written informed consent was obtained prior to the interview.
Competing Interests
All authors (W. C. Cheung, J. Aleman-Tovar, A. N. Johnston, L. M. Little, & M. M. Burke) declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Aashima N, M., & Sharma, R. A review of patient satisfaction and experience with telemedicine: A virtual solution during and beyond COVID-19 pandemic. Telemedicine and e-Health. 2021;27(12):1325–1331. doi: 10.1089/tmj.2020.0570. [DOI] [PubMed] [Google Scholar]
- Akamoglu Y, Meadan H. Parent-implemented language and communication interventions for children with developmental delays and disabilities: A scoping review. Review Journal of Autism and Developmental Disorders. 2018;5(3):294–309. doi: 10.1007/s40489-018-0140-x. [DOI] [Google Scholar]
- Akhbari Ziegler S, Hadders-Algra M. Coaching approaches in early intervention and paediatric rehabilitation. Developmental Medicine & Child Neurology. 2020;62(5):569–574. doi: 10.1111/dmcn.14493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashburner J, Vickerstaff S, Beetge J, Copley J. Remote versus face-to-face delivery of early intervention programs for children with autism spectrum disorders: Perceptions of rural families and service providers. Research in Autism Spectrum Disorders. 2016;23:1–14. doi: 10.1016/j.rasd.2015.11.011. [DOI] [Google Scholar]
- Baharav E, Reiser C. Using telepractice in parent training in early autism. Telemedicine and e-Health. 2010;16(6):727–731. doi: 10.1089/tmj.2010.0029. [DOI] [PubMed] [Google Scholar]
- Barton ML, Dumont-Mathieu T, Fein D. Screening young children for autism spectrum disorders in primary practice. Journal of Autism and Developmental Disorders. 2012;42(6):1165–1174. doi: 10.1007/s10803-011-1343-5. [DOI] [PubMed] [Google Scholar]
- Behl DD, Blaiser K, Cook G, Barrett T, Callow-Heusser C, Brooks BM, Dawson P, Quigley S, White KR. A multisite study evaluating the benefits of early intervention via telepractice. Infants & Young Children. 2017;30(2):147–161. doi: 10.1097/IYC.0000000000000090. [DOI] [Google Scholar]
- Bennell KL, Lawford BJ, Metcalf B, Mackenzie D, Russell T, van den Berg M, Crowther S, Aiken J, Fleming J, Hinman RS. Physiotherapists and patients report positive experiences overall with telehealth during the COVID-19 pandemic: A mixed-methods study. Journal of Physiotherapy. 2021;67(3):201–209. doi: 10.1016/j.jphys.2021.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaiser KM, Behl D, Callow-Heusser C, White KR. Measuring costs and outcomes of tele-intervention when serving families of children who are deaf/hard-of-hearing. International Journal of Telerehabilitation. 2013;5(2):3–17. doi: 10.5195/ijt.2013.6129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen GA. Naturalistic inquiry and the saturation concept: A research note. Qualitative Research. 2008;8:137–152. doi: 10.1177/1468794107085301. [DOI] [Google Scholar]
- Brantlinger E, Jimenez R, Klingner J, Pugach M, Richardson V. Qualitative studies in special education. Exceptional Children. 2005;71(2):195–207. doi: 10.1177/001440290507100205. [DOI] [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- Brislin RW. Back-translation for cross-cultural research. Journal of Cross-Cultural Psychology. 1970;1(3):185–216. doi: 10.1177/135910457000100301. [DOI] [Google Scholar]
- Bruder MB, Dunst CJ. Parental judgments of early childhood intervention personnel practices: Applying a consumer science perspective. Topics in Early Childhood Special Education. 2015;34(4):200–210. doi: 10.1177/0271121414522527. [DOI] [Google Scholar]
- Callanan, J., Signal, T., & McAdie, T. (2021). Involving parents in early intervention: therapists’ experience of the parent child relationally informed-early intervention (PCRI-EI) model of practice. International Journal of Disability, Development and Education, 1–14.
- Camden, C., & Silva, M. (2021). Pediatric telehealth: Opportunities created by the COVID-19 and suggestions to sustain its use to support families of children with disabilities. Physical & Occupational Therapy in Pediatrics, 41(1), 1–17. [DOI] [PubMed]
- Campbell PH, Sawyer LB. Supporting learning opportunities in natural settings through participation-based services. Journal of Early Intervention. 2007;29:287–305. doi: 10.1177/105381510702900402. [DOI] [Google Scholar]
- Cason J. A pilot telerehabilitation program: Delivering early intervention services to rural families. International Journal of Telerehabilitation. 2009;1(1):29. doi: 10.5195/ijt.2009.6007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cason J. Telehealth opportunities in occupational therapy through the Affordable Care Act. American Journal of Occupational Therapy. 2012;66(2):131–136. doi: 10.5014/ajot.2012.662001. [DOI] [PubMed] [Google Scholar]
- Crawford, M. J., & Weber, B. (2014). Early intervention every day! Embedding activities in daily routines for young children and their families. Brookes.
- Creswell, J. W. (2003). A framework for design. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches, 9–11.
- Division for Early Childhood of the Council for Exceptional Children. (2014). DEC recommended practices in early intervention/early childhood special education 2014. http://www.dec-sped.org/recommendedpractices
- Douglas SN, Meadan H, Kammes R. Early interventionists’ caregiver coaching: A mixed methods approach exploring experiences and practices. Topics in Early Childhood Special Education. 2020;40(2):84–96. doi: 10.1177/0271121419829899. [DOI] [Google Scholar]
- Early Childhood Technical Assistance Center. (2020). https://ectacenter.org/
- Edelman, L. (2020). Planning for the Use of Video Conferencing for Early Intervention Home Visits during the COVID-19 Pandemic. https://ectacenter.org/~pdfs/topics/disaster/Planning_for_the_Use_of_Video_Conferencing_in_EIduring_COVID-19_Pandemic.pdf
- Epley PH, Summers JA, Turnbull AP. Family outcomes of early intervention: Families’ perceptions of need, services, and outcomes. Journal of Early Intervention. 2011;33(3):201–219. doi: 10.1177/1053815111425929. [DOI] [Google Scholar]
- Fenikil´e, T. S., Ellerbeck, K., Filippi, M. K., & Daley, C. M. Barriers to autism screening in family medicine practice: A qualitative study. Primary Health Care Research & Development. 2015;16(4):356–366. doi: 10.1017/S1463423614000449. [DOI] [PubMed] [Google Scholar]
- Fitton L, Bustamante KN, Wood C. The social validity of telepractice among Spanish-Speaking caregivers of English learners: An examination of moderators. International Journal of Telerehabilitation. 2017;9(2):13. doi: 10.5195/ijt.2017.6227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming JL, Sawyer LB, Campbell PH. Early intervention providers’ perspectives about implementing participation-based practices. Topics in Early Childhood Special Education. 2011;30(4):233–244. doi: 10.1177/0271121410371986. [DOI] [Google Scholar]
- Fraser, S., Mackean, T., Grant, J., Hunter, K., Towers, K., & Ivers, R. (2017). Use of telehealth for health care of indigenous peoples with chronic conditions: A systematic review. Rural Remote Health, 17(3):4205. 10.22605/RRH4205 [DOI] [PubMed]
- Friedman M, Woods J, Salisbury C. Caregiver coaching strategies for early intervention providers: Moving toward operational definitions. Infants & Young Children. 2012;25:62–82. doi: 10.1097/IYC.0b013e31823d8f12. [DOI] [Google Scholar]
- Fuller EA, Kaiser AP. The effects of early intervention on social communication outcomes for children with autism spectrum disorder: A meta-analysis. Journal of Autism and Developmental Disorders. 2020;50(5):1683–1700. doi: 10.1007/s10803-019-03927-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbs V, Toth-Cohen S. Family-centered occupational therapy and telerehabilitation for children with autism spectrum disorders. Occupational Therapy in Health Care. 2011;25(4):298–314. doi: 10.3109/07380577.2011.606460. [DOI] [PubMed] [Google Scholar]
- Glaser, B. G., & Strauss, A. L. (1967). The discovery of grounded theory: Strategies for qualitative research. Aldine.
- Gray LM, Wong-Wylie G, Rempel., G. R., & Cook, K. Expanding qualitative research interviewing strategies: Zoom video communications. The Qualitative Report. 2020;25(5):1292–1301. [Google Scholar]
- Heidlage JK, Cunningham JE, Kaiser AP, Trivette CM, Barton EE, Frey JR, Roberts MY. The effects of parent-implemented language interventions on child linguistic outcomes: A meta-analysis. Early Childhood Research Quarterly. 2020;50:6–23. doi: 10.1016/j.ecresq.2018.12.006. [DOI] [Google Scholar]
- Heitzman-Powell, L. S., Buzhardt, J., Rusinko, L. C., & Miller, T. M. (2013). Formative evaluation of an ABA outreach training program for parents of children with autism in remote areas. Focus on Autism and Other Developmental Disabilities 29(1), 23-28 1088357613504992.
- Hughes-Scholes CH, Gavidia-Payne S. Early childhood intervention program quality: Examining family-centered practice, parental self-efficacy and child and family outcomes. Early Childhood Education Journal. 2019;47(6):719–729. doi: 10.1007/s10643-019-00961-5. [DOI] [Google Scholar]
- Individuals with Disabilities Education Improvement Act [IDEA]. (2004). 20 U.S.C 1400 et seq.
- Ives Y. What is' coaching'? An exploration of conflicting paradigms. International Journal of Evidence Based Coaching & Mentoring. 2008;6(2):100–113. [Google Scholar]
- Kogan MD, Strickland BB, Blumberg SJ, Singh GK, Perrin JM, van Dyck PC. A national profile of the health care experiences and family impact of autism spectrum disorder among children in the United States, 2005–2006. Pediatrics. 2008;122(6):e1149–e1158. doi: 10.1542/peds.2008-1057. [DOI] [PubMed] [Google Scholar]
- Lee, J. F., Schieltz, K. M., Suess, A. N., Wacker, D. P., Romani, P. W., Lindgren, S. D., Kopelman, T.G., & Dalmau, Y. C. P. (2015). Guidelines for developing telehealth services and troubleshooting problems with telehealth technology when coaching parents to conduct functional analyses and functional communication training in their homes. Behavior Analysis in Practice, 8, 190–200. 10.1007/s4061 7–014–0031–2. [DOI] [PMC free article] [PubMed]
- Lerman, D. C., O'Brien, M. J., Neely, L. C., Call, N. A., Tsami, L., Schieltz, K. M., Berg, W. K., Graber, J., Huang, P., Kopelman, T., & Cooper-Brown, L. (2020). Remote coaching of caregivers via telehealth: Challenges and potential solutions. Journal of Behavioral Education, 29(2), 195–221. 10.1007/s10864-020-09378-2 [DOI] [PMC free article] [PubMed]
- Little LM, Pope E, Wallisch A, Dunn W. Occupation-based coaching by means of telehealth for families of young children with autism spectrum disorder. American Journal of Occupational Therapy. 2018;72(2):275–286. doi: 10.5014/ajot.2018.024786. [DOI] [PubMed] [Google Scholar]
- McGill, M., & Fiddler, K. (2021). A user's guide for understanding and addressing telepractice technology challenges via ZOOM (Vol. 6, No. 2, pp. 494-499). American Speech-Language-Hearing Association.
- Meadan H, Chung MY, Sands MM, Snodgrass MR. The cascading coaching model for supporting service providers, caregivers, and children. The Journal of Special Education. 2020;54(2):113–125. doi: 10.1177/0022466919884070. [DOI] [Google Scholar]
- Nickelson, D. W. (1998). Telehealth and the evolving health care system: Strategic opportunities for professional psychology. Professional Psychology: Research and Practice, 29(6), 527–535. 10.1037/0735-7028.29.6.527.
- Noyes-Grosser DM, Elbaum B, Wu Y, Siegenthaler KM, Cavalari RS, Gillis JM, Romanczyk RG. Early intervention outcomes for toddlers with autism spectrum disorder and their families. Infants & Young Children. 2018;31(3):177–199. doi: 10.1097/IYC.0000000000000121. [DOI] [Google Scholar]
- Patton MQ. Qualitative research and evaluation methods. Sage; 2002. [Google Scholar]
- Richmond T, Peterson C, Cason J, Billings M, Terrell EA, Lee ACW, Towey M, Parmanto B, Saptano A, Cohn ER, Brennan D. American Telemedicine Association’s principles for delivering telerehabilitation services. International Journal of Telerehabilitation. 2017;9(2):63–67. doi: 10.5195/ijt.2017.6232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rideout, V., & Katz, V.S. (2016). Opportunity for All? Technology and Learning in Lower-income families. The Joan Ganz Cooney Center at Sesame Workshop.
- Romano M, Schnurr M. Mind the gap: Strategies to bridge the research-to-practice divide in early intervention caregiver coaching practices. Topics in Early Childhood Special Education. 2020 doi: 10.1177/0271121419899163. [DOI] [Google Scholar]
- Rush, D. D., & Sheldon, M. L. (2020). The early childhood coaching handbook. Brookes.
- Rush, D., Shelden, M., & Dunn, W. (2011). The early childhood coaching handbook. Brookes.
- Salomone E, Maurizio Arduino G. Parental attitudes to a telehealth parent coaching intervention for autism spectrum disorder. Journal of Telemedicine and Telecare. 2017;23(3):416–420. doi: 10.1177/1357633X16642067. [DOI] [PubMed] [Google Scholar]
- Sturges JE, Hanrahan KJ. Comparing telephone and face-to-face qualitative interviewing: A research note. Qualitative Research. 2004;4(1):107–118. doi: 10.1177/1468794104041110. [DOI] [Google Scholar]
- Tenforde, A. S., Borgstrom, H., Polich, G., Steere, H., Davis, I. S., Cotton, K., O’Donnell, M., & Silver, J. K. (2020). Outpatient physical, occupational, and speech therapy synchronous telemedicine: a survey study of patient satisfaction with virtual visits during the COVID-19 pandemic. American Journal of Physical Medicine & Rehabilitation. [DOI] [PMC free article] [PubMed]
- Tesch, R. (1990). Qualitative. Research: Analysis Types and Software. 10.4324/9781315067339 [DOI]
- Vismara LA, Young GS, Rogers SJ. Telehealth for expanding the reach of early autism training to parents. Autism Research and Treatment. 2012 doi: 10.1155/2012/121878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wainer AL, Ingersoll BR. Increasing access to an ASD imitation intervention via a telehealth parent training program. Journal of Autism and Developmental Disorders. 2015;45(12):3877–3890. doi: 10.1007/s10803-014-2186-7. [DOI] [PubMed] [Google Scholar]
- Wallisch A, Little L, Pope E, Dunn W. Parent perspectives of an occupational therapy telehealth intervention. International Journal of Telerehabiltation. 2019;11(1):15–22. doi: 10.5195/ijt.2019.6274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams CS, Ostrosky MM. What about MY TOYS? Common questions about using a bagless approach in early intervention. Young Exceptional Children. 2020;23(2):76–86. doi: 10.1177/1096250619829739. [DOI] [Google Scholar]
- Williams ME, Perrigo JL, Banda TY, Matic T, Goldfarb FD. Barriers to accessing services for young children. Journal of Early Intervention. 2013;35(1):61–74. doi: 10.1177/1053815113507111. [DOI] [Google Scholar]
- World Health Organization. (2020). Coronavirus disease (COVID-19) weekly epidemiological update and weekly operational update. www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
- Yang HW, Burke M, Isaacs S, Rios K, Schraml-Block K, Aleman-Tovar J, Tompkins J, Swartz R. Family perspectives toward using telehealth in early intervention. Journal of Developmental and Physical Disabilities. 2021;33(2):197–216. doi: 10.1007/s10882-020-09744-y. [DOI] [Google Scholar]
- Zoder-Martell KA, Markelz AM, Floress MT, Skriba HA, Sayyah LE. Technology to facilitate telehealth in applied behavior analysis. Behavior Analysis in Practice. 2020;13(3):596–603. doi: 10.1007/s40617-020-00449-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.