Abstract
Background
Due to the emergence of COVID-19, many countries have started mass immunization programs. To date, no cases of optic neuritis following COVID-19 vaccination have been reported in the literature.
Case presentation
Objective: Here, we report 2 cases of unilateral optic neuritis after vaccination against COVID-19 using the Sinopharm vaccine (Sinopharm Group Co. Ltd, China).
Design
The clinical history, examination, and test findings of two individuals with unilateral optic neuritis associated with the timing of COVID-19 vaccination were described and further analyzed.
Setting
Two patients developed optic neuritis after receiving the COVID-19 vaccine. One patient developed optic neuritis 6 weeks after the first dose and 3 weeks after the second dose. The other patient developed optic neuritis 3 weeks after the first dose. Participants: Two female patients, aged 21 and 39 years.
Result
The patients were successfully treated with intravenous methylprednisolone pulse therapy. Both patients had typical manifestations of optic neuritis and their visual acuity recovered fully after treatment. The second of these patients was positive for anti-myelin oligodendrocyte glycoprotein antibodies (MOG).
Conclusion
Optic neuritis is a potential adverse effect after vaccination against the coronavirus disease (COVID-19).
Supplementary Information
The online version contains supplementary material available at 10.1007/s10633-022-09880-0.
Keywords: COVID-19 vaccine, Optic neuritis, Case report
Background
Cases of optic neuritis after vaccination have been published in the medical literature, including those resulting after vaccination against influenza, tuberculosis and other infectious diseases [1]. One case of acute thyroiditis and bilateral optic neuritis following SARS-CoV-2 vaccination has been reported [2]. As more people get vaccinated, concerns about neurological complications associated with COVID-19 vaccines are escalating [3]. Here, we report two cases of unilateral optic neuritis after receiving a vaccination against COVID-19 (Sinopharm Group Co. Ltd, China) for the first time.
Case presentation
Case 1
The patient was a 21-year-old female who presented with blurred vision in the right eye with ocular rotation pain 6 weeks after the first dose and 3 weeks after the second dose of the COVID-19 vaccine. The patient was diagnosed at an external hospital as having optic neuritis in the right eye and was treated with a peribulbar injection of tretinoin (2 mg). Following treatment, her ocular rotation pain and visual acuity improved slightly. Subsequently, the patient sought medical attention at the Ophthalmology Center of Zhuhai People's Hospital on June 5, 2021. Her ocular examination results were as follows. Vod 0.6 (no improvement by correction); Vos 1.0; NCT: 14.0 mmHg in the right eye 15.0 mmHg in the left eye; RAPD (+) in the right eye; and slit lamp microscopy showed blurred optic disc margin with congestion and edema in the right eye. No significant abnormalities were evident in the left eye. FFA showed early hyperfluorescence leakage and late enhancement of the right optic papilla (Fig. 1A and B). OCT of the right eye showed significant thickening of the RNFL. Automatic static perimetry (Humphrey 24-2) showed the presence of a central scotoma in the right eye (Fig. 2). The pattern visual evoked potential (PVEP) showed decreased amplitude in the right eye (Fig. 4A). MRI of the head showed a small ischemic focus in the left frontal lobe (no treatment was recommended after consultation with a cerebrovascular physician). The orbital MRI scan showed no significant abnormalities. The patient’s serum anti-aquaporin-4 (AQP4) antibody, anti-myelin basic protein antibody (MBP) and anti-myelin oligodendrocyte glycoprotein antibody (MOG) were all negative. The diagnosis of optic neuritis in the right eye was confirmed. Treatment using 800 mg methylprednisolone was given for pulse therapy as an intravenous bolus for 3 days, and then oral prednisone was used with gradual dose reduction until discontinuation. Papillary congestion and edema in the right eye gradually resolved until the optic disk boundary became clear. The patient’s visual acuity recovered to 0.8 in 1 week and 1.0 after 1 month (Fig. 3).
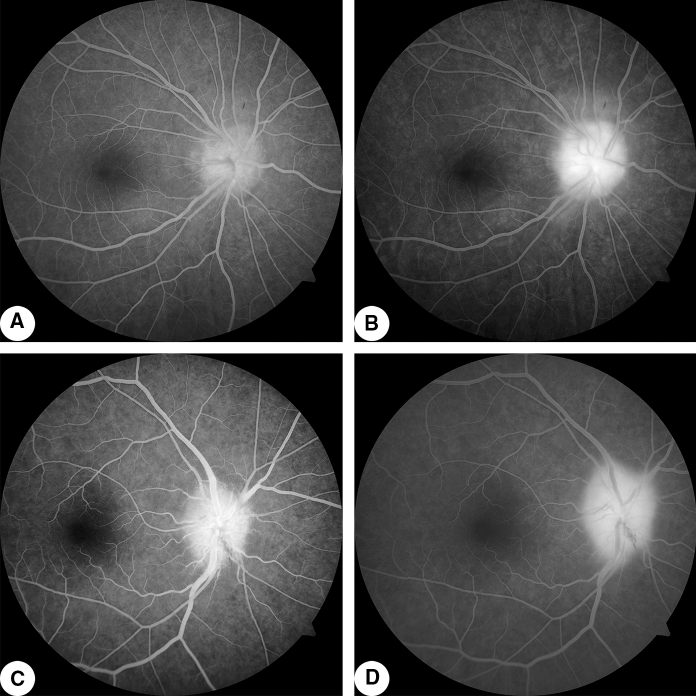
Fig. 1.
Fluorescein fundus angiogram A Case 1: early-stage right eye angiogram (0:00:29.4) with hyperfluorescence of dilated capillaries on the surface of the optic papilla; B Case 1: late angiogram (0:05:11.2) with hyperfluorescence of the whole optic papilla. C Case 2: early right eye angiogram (0:01:32.3) with hyperfluorescence of the optic papilla; D Case 2: late angiogram (0:08:25.5) with markedly enhanced fluorescence of the optic papilla
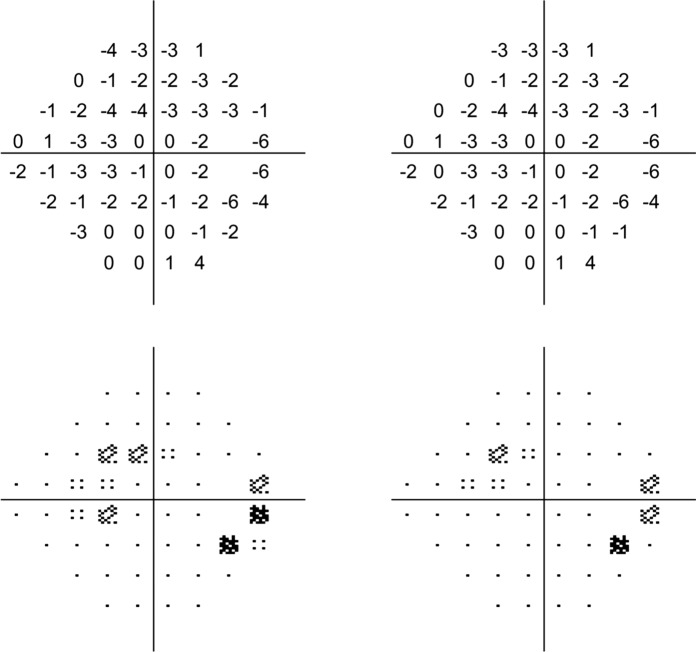
Fig. 2.
Automatic static perimetry (Humphrey 24-2) in case 1 shows the presence of a central dark spot in the right eye
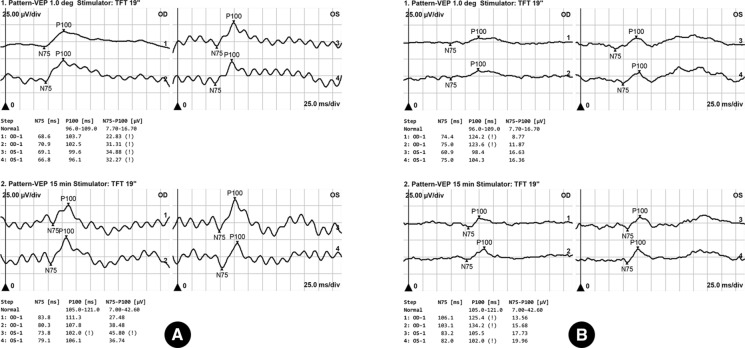
Fig. 4.
Case 1: PVEP A showed prolonged P100 wave latency and decreased amplitude in the right eye. Case 2: PVEP B showed prolonged P100 wave latency and decreased amplitude
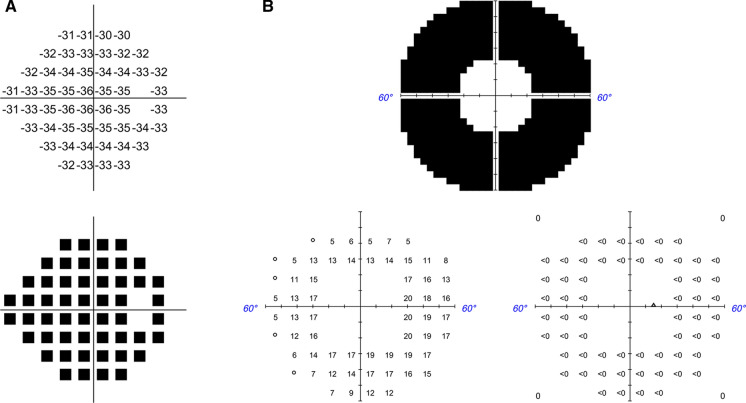
Fig. 3.
Case 2 automatic perimetry (Humphrey 24-2 (A) and 60-4 (B)) showing centripetal narrowing of the visual field in the right eye
Case 2
The patient was a 38-years-old female who was seen at the Ophthalmology Center of Zhuhai People's Hospital on June 7, 2021, for sudden onset of blurred vision in the right eye, 3 weeks after the first dose of the COVID-19 vaccine. Her ocular examination results were as follows. Vod FC/1 m (accurate light localization in all directions, no improvement in correction); Vos 1.0; NCT: 15.0 mmHg in the right eye and 15.0 mmHg in the left eye; RAPD (+) in the right eye; and slit lamp microscopy showed blurred borders of the right optic disc with congestion and edema. No significant abnormalities were seen on examination of the left eye. Color fundoscopy photographs of the right eye showed an indistinct boundary of the optic papilla with disc congestion and edema and retinal vein thickening. FFA showed hyper-fluorescence leakage of the right optic papilla in the early stage and enhancement in the late stage (Fig. 1C and D). OCT of the right eye showed significant thickening of the RNFL thickness. The pattern visual evoked potential (PVEP) showed prolonged P100 wave latency and decreased amplitude (Fig. 4B). Automatic static perimetry (Humphrey 24-2 and 60-4) showed centripetal narrowing of the visual field (Fig. 3). The orbital CT showed hypointense thickening of the right optic nerve, with no significant abnormalities on cranial CT. The patient’s serum anti-aquaporin 4 (AQP4) antibody and anti-myelin basic protein antibody (MBP) were negative, and anti-myelin oligodendrocyte glycoprotein antibody (MOG) was positive (+) 1:32. The diagnosis of optic neuritis in the right eye was confirmed. The patient was given 1000 mg methylprednisolone intravenously as shock therapy for 3 days, and then treatment was changed to oral prednisone with gradual dose reduction until discontinuation. Papillary congestion and edema in the right eye gradually resolved until the optic disk boundary become clear. The patient’s visual acuity recovered to 0.6 in 1 week and 1.0 after 1 month.
Discussion
The development of vaccines has greatly contributed to public health worldwide, significantly reducing morbidity and mortality from infectious diseases. However, vaccines are also a powerful stimulant of the immune system and theoretically have the potential to induce or exacerbate immune disorders by manifesting as abnormal serological markers of the immune system, or clinically as autoimmune diseases [4]. Cases of optic neuritis following vaccination have been reported in the literature. As yet, there is insufficient evidence to prove a causal relationship between vaccination and optic neuritis [5].
The two patients reported in this paper had symptoms, signs, and ophthalmologic examination results consistent with the diagnosis of typical optic neuritis, and both had rapid and marked improvement in vision after high-dose glucocorticoid intravenous pulse therapy. The two cases reported here were both vaccinated with the inactivated vaccine from Sinopharm. Our two female patients were previously fit, had no history of any chronic disease, had no significant abnormalities based on routine blood count, erythrocyte sedimentation, 4-item viral tests, immunoglobulins, and ANA immune markers on admission, had no systemic symptoms such as fever or rash, and had no significant evidence of existing infection or noninfectious inflammation. There is no clear evidence to prove a causal relationship between COVID-19 vaccination and optic neuritis. From what has been reported in the Chinese and international literature, the development of optic neuritis after COVID-19 vaccination is rare. However, several cases of neuromyelitis optical spectrum disorder have been reported following COVID-19 vaccination [6, 7].
Another concern to be noted is that the onset of the two cases reported was several weeks after vaccination, and serum AQP4 antibody and MBP antibody were negative in both cases, while the MOG antibody was positive (+) 1:32 in case 2. The neurologist was consulted who suggested further cervicothoracic MRI, but the patient declined the imaging. As such, it remained unclear whether the patient had demyelinating lesions.
Conclusion
Optic neuritis is a potential adverse effect after vaccination against the coronavirus disease (COVID-19).
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Author contribution
All authors contribute equally to the article.
Funding
This study was supported by grants from the Science and Technology Foundation of Zhuhai (ZH3310200025PJL) and the Cultivation Project of Zhuhai People's Hospital (2019PY-22).
Declarations
Conflict of interest
The authors certify that there is no affiliations or financial interest with authorship, research or publication in this article.
Informed consent
Written informed consent was obtained from the patients for publication of this case report and any accompanying images.
Statement of human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of Zhuhai People’s Hospital(Zhuhai Hospital Affiliated with Jinan University) and with the 1964 Helsinki Declaration and its later amendments.
Statement on the welfare of animals
This article does not contain any studies with animals performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jiajun Wang, Sumin Huang and Zhijian Yu have contributed equally to this work.
References
- 1.De Giacinto C, Guaglione E, Leon PE, et al. Unilateral optic neuritis: a rare complication after measles-mumps-rubella vaccination in a 30-year-old woman. Case Rep Ophthalmol Med. 2016;2016:8740264. doi: 10.1155/2016/8740264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leber HM, Sant'Ana L, Konichi da Silva NR et al (2021) Acute thyroiditis and bilateral optic neuritis following sars-cov-2 vaccination with coronavac: a case report. Ocul Immunol Inflamm 1–7 [DOI] [PubMed]
- 3.Goss AL, Samudralwar RD, Das RR, et al. Ana investigates: Neurological complications of covid-19 vaccines. Ann Neurol. 2021;89(5):856–857. doi: 10.1002/ana.26065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jakimovski D, Weinstock-Guttman B, Ramanathan M et al (2020) Infections, vaccines and autoimmunity: a multiple sclerosis perspective. Vaccines (Basel) 8(1) [DOI] [PMC free article] [PubMed]
- 5.Baxter R, Lewis E, Fireman B, et al. Case-centered analysis of optic neuritis after vaccines. Clin Infect Dis. 2016;63(1):79–81. doi: 10.1093/cid/ciw224. [DOI] [PubMed] [Google Scholar]
- 6.Chen S, Fan XR, He S, et al. Watch out for neuromyelitis optica spectrum disorder after inactivated virus vaccination for covid-19. Neurol Sci. 2021;42(9):3537–3539. doi: 10.1007/s10072-021-05427-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Helmchen C, Buttler GM, Markewitz R et al (2021) Acute bilateral optic/chiasm neuritis with longitudinal extensive transverse myelitis in longstanding stable multiple sclerosis following vector-based vaccination against the sars-cov-2. J Neurol 1–6 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.