Abstract
Background
Despite improvements, disparities in breast cancer care have led to an inequitable distribution of treatment delays and worse outcomes among patients with breast cancer. This study aimed to quantify the contribution of mediators that may explain racial/ethnic disparities in breast cancer treatment delays.
Patients and Methods
We conducted a retrospective analysis of patients from the National Cancer Database with stage I–III breast cancer who underwent surgical resection. Mediation analyses estimated the extent to which racial/ethnic disparities in the distribution of patient characteristics account for racial/ethnic disparities in delayed treatment.
Results
Of the 1,349,715 patients with breast cancer included, 10%, 5%, and 4% were Black, Hispanic, and other non-white race/ethnicity, respectively. Multivariable models showed that patients in these racial/ethnic groups had 73%, 81%, and 24% increased odds of having a treatment delay relative to white patients. Mediation analyses suggested that 15%, 19%, and 15% of the treatment delays among Black, Hispanic, and other non-white race/ethnicity patients, respectively, are explained by disparities in education, comorbidities, insurance, and facility type. Therefore, if these mediators had been distributed equally among all races/ethnicities, a reduction of 15–19% in the delayed treatment disparities experienced by minority patients would have been observed. Academic facility type was the factor that could yield the largest reduction in time to treatment disparities, contributing to 8–13% of racial/ethnic disparities.
Conclusions
Patients with breast cancer who identified as Black, Hispanic, and other non-white races/ethnicities are exposed to longer treatment delays relative to white patients. Efforts to equalize mediators could remove substantial portions of racial/ethnic disparities in delayed treatment.
Breast cancer is the second leading cause of cancer death in women in the USA. Breast cancer outcomes have been steadily improving over the past three decades, with mortality rates decreasing by 40% from 1989 to 2017.1 Despite an overall improvement in breast cancer outcomes, previous research demonstrates racial/ethnic disparities in the distribution of this improvement. In 1990, breast cancer mortality rate in Black women was 11% greater than that of white women. By 2005, this disparity increased to a 38% relative difference in breast cancer mortality rates.3 The growing disparity in breast cancer outcomes of Black and white women reflects inequities in our healthcare system and the disproportionate lack of access to quality breast cancer treatment that Black patients experience. Furthermore, Black women with breast cancer are differentially exposed to social determinants of health including economic instability, lack of social support, inadequate transportation, and other barriers.
Research demonstrates that, while breast cancer outcomes are multifactorial, treatment delays are associated with decreased survival rates in disease stages I–III. This has been the subject of recent interest given delays in care experienced during the coronavirus disease 2019 (COVID-19) pandemic.4–6 Black women are at a significantly higher risk of experiencing delays in treatment than white women.6 A patient’s insurance and financial status also impact breast cancer treatment delays,7,8 and can reduce the opportunity of benefiting from early detection and intervention. Similar patterns may also be present for other racial/ethnic subgroups such as Hispanic and Asian patients.9
While previous research has identified a variety of factors that cause treatment delays, the mechanisms by which these factors lead to racial/ethnic disparities in breast cancer treatment delays have not been explicitly identified.10 An investigation of these pathways is necessary to identify areas for improvement in breast cancer care that can address racial/ethnic inequities at the population level. The objective of this study was to quantify the contribution of individual mediators that explain racial/ethnic disparities in delays to initial treatment following breast cancer diagnosis. We hypothesized that the distribution of socioeconomic and system-level factors would be different by race/ethnicity and thus could account for significant portions of the overall treatment delay disparities.
Patients and Methods
Data Source and Study Population
This Institutional Review Board exempt study analyzed data from the National Cancer Database (NCDB) Participant User Files. The study population included all patients ≥ 18 years of age from participating hospitals diagnosed with breast cancer between 2004 and 2017. Patients with stage I–III cancer who underwent surgery were included. Men, stage IV cancers, and those who did not receive surgery were excluded. Overall, 1,349,715 breast cancer cases met inclusion criteria. Analysis included demographic information, pathologic findings, and treatment modality, with specific emphasis on time to treatment.
Exposure and Outcome
Race/ethnicity was the exposure of interest, which was categorized as white, Black, Hispanic, or other non-white according to NCDB data. The other non-white category includes those who were not identified as white, Black, or Hispanic by the NCDB. The primary outcome was delayed treatment. Time to initial treatment is measured as the number of days from diagnosis to initiation of the first treatment. Time to initial treatment ≥ 42 days was considered delayed treatment. This variable was dichotomized at the upper quartile (top 25% of the distribution), with 25% of patients experiencing delays of ≥ 42 days. This is a data-driven approach since there are no guidelines or consensus panels that have defined a cutoff for delayed treatment following diagnosis.
Mediators and Confounders
Mediators analyzed in this study were income, education, comorbidity burden, insurance status, and academic facility status, which were dichotomized for the purpose of analysis. Zip code-level median income greater than or equal to US $48,000 (the median) was considered high; income less than US $48,000 was considered low. Education was determined by the percentage of individuals without a high school degree in each zip code. Zip codes with < 14% of residents without a high school degree were considered “high education.” Comorbidity burden was dichotomized according to the Charlson–Deyo Comorbidity score, with ≥ 1 being a high comorbidity burden. Insurance status was operationalized as either public (Medicaid, Medicare, or other government) or private. Academic facility status was split into patients who were treated at academic facilities and those who were not. Confounders included for analysis were age at diagnosis, American Joint Committee on Cancer stage at diagnosis, facility location, and rural residence. Facility location was determined by region of the USA, and rural residence was determined by US Department of Agriculture population data and defined as counties with a population of less than 2500 people. Methods developed by VanderWeele and Robinson were utilized to determine whether variables were confounders or mediators.10 VanderWeele and Robinson show that racial/ethnic disparities in treatment outcomes are caused by disparities in mediating factors rather than race/ethnicity itself.
Statistical Analysis
We examined the unadjusted association between race/ethnicity and baseline characteristics as well as delayed treatment using Pearson’s chi-square tests and analysis of variance as appropriate to the data. Separate multivariable analyses were conducted. First, we used logistic regression to examine the association between race/ethnicity and delayed treatment while only including confounders (but no mediators) in order to estimate the total effect (total disparity) of race/ethnicity on delayed treatment. Next, we evaluated the association between race/ethnicity and the five mediators as outcomes using five separate logistic regression models that adjusted for the confounders. Then, we fit a final logistic regression model to estimate the effect of each of the five mediators on delayed treatment while adjusting for race/ethnicity and the confounders. Mediators that were statistically significantly different between races/ethnicities and associated with delayed treatment were used to conduct a mediation analysis to partition the total effect of race/ethnicity into the effect explained by each mediator and the effect left over after equalizing the distribution of mediators. We used the SAS macro developed by Vanderweele and Valenti to conduct five separate mediation analyses.11 This method uses Judea Pearl’s mediation formula to estimate direct and indirect effects as well as the percent mediated, which represents the percentage of the outcome that would be reduced if the distributions of the mediators were equalized across exposure groups.12 Each mediation analysis yielded an estimate of the percent mediated and the total percent mediated was calculated by adding the five individual percent mediated estimates.
Results
The analysis cohort was composed of 1,349,715 patients with breast cancer, of whom 10%, 5%, and 4% were Black, Hispanic, and other non-white race/ethnicity, respectively. Overall, 52.1% of the study population had private insurance and 1.4% came from rural counties. The South Atlantic region contributed the greatest number of patients to this study (23%); 64.5% of patients had high level of household income, and 63% came from counties with higher levels of education (complete demographic data in Table 1). Prevalence of delayed treatment varied across racial/ethnic groups, ranging from 22% to 35.7%. Delayed treatment among the entire study population was 23.9%.
Table 1.
Patient demographics. All p-values represent a chi-square test except for age, which represents analysis of variance
| All Patients | White | Black | Hispanic | Other non-white | ||
|---|---|---|---|---|---|---|
| Demographic | N (%) | N (%) | N (%) | N (%) | N (%) | |
| Total | 1,349,715 | 1,099,383 (81.45) | 138,937 (10.29) | 60,369 (4.47) | 51,026 (3.78) | |
| Mean age at diagnosis [SD] | 62.8 | 63.48 [12.21] | 60.50 [11.78] | 59.16 [11.85] | 58.82 [11.65] | |
| Diagnosis to Treatment | ||||||
| Greater than 42 days | 323,085 (23.9) | 241,942 (22.0) | 45,039 (32.4) | 21,555 (35.7) | 14,549 (28.5) | |
| Less than or equal to 42 | 1,026,630 (76.1) | 857,441 (78.0) | 93,898 (67.6) | 38,814 (64.3) | 36,477 (71.5) | |
| Insurance | ||||||
| Private insurance | 703,292 (52.1) | 571,930 (52.0) | 69,660 (50.1) | 30,768 (50.9) | 31,317 (61.4) | |
| Public insurance | 646,423 (47.9) | 527,453 (48.0) | 69,277 (49.9) | 29,601 (49.1) | 19,709 (38.6) | |
| Urban/rural zip code | ||||||
| Urban/metro | 1,331,188 (98.6) | 1,082,552 (98.5) | 137,731 (9.1) | 60,262 (99.8) | 50,643 (99.3 | |
| Rural | 18,527 (1.4) | 16,831 (1.5) | 1206 (0.9) | 107 (0.2) | 383 (0.7) | |
| Facility region | ||||||
| New England | 84,866 (6.3) | 76,659 (7.0) | 3681 (2.7) | 2642 (4.4) | 1884 (3.7) | |
| Middle Atlantic | 209,453 (15.5) | 167,257 (15.2) | 22,346 (16.1) | 10,500 (17.4) | 9,350 (18.3) | |
| South Atlantic | 306,135 (22.7) | 236,752 (21.5) | 51,234 (36.9) | 11,005 (18.2) | 7144 (14.0) | |
| East North Central | 235,250 (17.4) | 202,967 (18.5) | 23,505 (16.9) | 4369 (7.2) | 4409 (8.7) | |
| East South Central | 82,725 (6.1) | 69,507 (6.3) | 12,213 (8.8) | 375 (0.6) | 630 (1.2) | |
| West North Central | 110,451 (8.2) | 102,427 (9.3) | 5301 (3.8) | 930 (1.5) | 1793 (3.5) | |
| West South Central | 98,515 (7.3) | 71,722 (6.5) | 13,111 (9.4) | 10,538 (17.5) | 3144 (6.2) | |
| Mountain | 58,395 (4.3) | 51,043 (4.6) | 1231 (0.9) | 4173 (6.9) | 1948 (3.82) | |
| Pacific | 163,925 (12.2) | 121,049 (11.0) | 6,315 (4.5) | 15,837 (26.3) | 20,724 (40.6) | |
| Stage at diagnosis | ||||||
| Stage I | 842,465 (62.4) | 706,355 (64.3) | 72,486 (52.2) | 33,360 (55.3) | 30,264 (59.3) | |
| Stage II | 408,515 (30.3) | 318,969 (29.0) | 51,197 (36.8) | 21,336 (35.3) | 17,013 (33.3) | |
| Stage III | 98,735 (7.32) | 74,059 (6.7) | 15,254 (11.0) | 5673 (9.4) | 3749 (7.34) | |
| Charleson–Deyo | ||||||
| ≥ 1 | 244,648 (18.1) | 189,492 (17.2) | 35,337 (25.4) | 11,749 (19.5) | 8070 (15.8) | |
| 0 | 1,105,067 (81.9) | 909,891 (82.8) | 103,600 (74.6) | 48,620 (80.5) | 42,956 (84.2) | |
| Average zip code Household income | ||||||
| Greater than/equal to 48,000 | 869,999 (64.5) | 742,472 (67.5) | 53,686 (38.6) | 33,350 (55.2) | 40,491 (79.4) | |
| Less than 48,000 | 479,716 (35.5) | 356,911 (32.5) | 85,251 (61.4) | 27,019 (44.8) | 10,535 (20.7) | |
| Zip code rate without HS degree attainment | ||||||
| < 14% | 844,070 (62.5) | 745,363 (67.8) | 46,481 (33.5) | 20,278 (33.6) | 31,948 (62.6) | |
| ≥ 14% | 505,645 (37.5) | 354,020 (32.2) | 92,456 (66.5) | 40,091 (66.4) | 19,078 (37.4) | |
| Academic treatment | ||||||
| Yes | 401,028 (29.7) | 303,237 (26.6) | 56,164 (40.4) | 21,788 (36.1) | 19,839 (38.9) | |
| No | 948,687 (70.3) | 796,146 (72.4) | 82,773 (59.6) | 38,581 (63.9) | 31,187 (61.1) |
In adjusted models, patients identified as Black, Hispanic, and other non-white race/ethnicity had increased odds of experiencing treatment delays when compared with white patients (Table 2). Black [odds ratio (OR) = 1.73, 95% confidence interval (CI) = 1.71–1.75], Hispanic [OR = 1.81, 95% CI = 1.78–1.84], and other non-white [OR = 1.24, 95% CI = 1.2–1.26] patients had 73%, 81%, and 24% increased odds of having treatment delay relative to white patients. Racial/ethnic inequities in treatment delays are reflected in these increased odds, with the largest effect seen in the Hispanic population.
Table 2.
Total effect of race/ethnicity on treatment delay. Odds of having treatment initiation greater than 42 days after diagnosis by race/ethnicity using white patients as a comparator group
| Race | Odds ratio of delayed treatment (> 42 days) | 95% CI |
|---|---|---|
| Black versus white | 1.73 | 1.71–1.75 |
| Hispanic versus white | 1.81 | 1.78–1.84 |
| Other non-white versus white | 1.24 | 1.21–1.26 |
When compared with the white reference group, patients of all comparator races/ethnicities were more likely to receive treatment at an academic facility, have lower education levels, have public insurance, and have underlying comorbidities at the time of diagnosis. Black and Hispanic patients were more likely to have lower income than white patients (OR = 0.54, 95% CI = 0.53–0.55; OR = 0.97, 95% CI = 0.95–0.99, respectively) (Table 3).
Table 3.
Results of mediation analysis between race/ethnicity and treatment delay greater than 42 days after diagnosis
| Mediators stratified by race/ethnicity | Association between race and mediator, OR (95% CI) | % of total effect attributable to mediator (true) (%) | % of total effect attributable to mediator (false) (%) |
|---|---|---|---|
| Black versus white | |||
| Education | 0.38 (038–0.39) | 4 | 5 |
| Comorbidities | 1.64 (1.62–1.66) | 0 | 0 |
| Private insurance status | 0.66 (0.65–0.67) | 0 | 0 |
| Academic treatment | 1.67 (1.66–1.70) | 11 | 10 |
| Hispanic versus white | |||
| Education | 0.24 (0.24–0.25) | 11 | 5 |
| Comorbidities | 1.27 (1.25–1.30) | 0 | 0 |
| Private insurance status | 0.50 (0.48–0.51) | 0 | 0 |
| Academic treatment | 1.60 (1.57–1.63) | 8 | 7 |
| Other non-white versus white | |||
| Education | 0.59 (0.57–0.60) | 2 | 1 |
| Comorbidities | 1.21 (1.09–1.45) | 0 | 0 |
| Private insurance status | 0.79 (0.77–0.81) | 0 | 0 |
| Academic treatment | 1.76 (1.72–1.79) | 13 | 16 |
Analysis of mediators independent of race/ethnicity and confounders demonstrated that all mediators of interest were associated with delayed treatment (Table 4). Mediators associated with lower odds of delayed treatment include higher levels of education (OR = 0.91, 95% CI = 0.90–0.92) and private insurance (OR = 0.81, 95% CI = 0.80–0.82). Mediators associated with higher odds of delayed treatment include higher income (OR = 1.02, 95% CI = 1.01–1.03), higher comorbidity burden (OR = 1.15, 95% CI = 1.14–1.16), and treatment at an academic facility (OR = 1.49, 95% CI = 1.48–1.50). Higher income was unexpectedly associated with higher odds of delayed treatment. Since Black and Hispanic patients were less likely to have higher income, the income variable cannot be one of the reasons why Black and Hispanic patients had delayed treatment. Thus, income cannot be a mediator. However, all other proposed mediators meet the criteria and assumptions for being mediators.
Table 4.
Effect of mediator on outcome variable (delay in treatment initiation greater than 42 days)
| Mediator | Association between mediator and outcome, OR (95% CI) |
|---|---|
| Income | 1.02 (1.01–1.03) |
| Education | 0.91 (0.90–0.92) |
| Comorbidities | 1.15 (1.14–1.16) |
| Private insurance status | 0.81 (0.80–0.82) |
| Academic treatment | 1.49 (1.48–1.50) |
Mediation analyses suggested that, if the distribution of education, comorbidity burden, insurance status, and facility type of all patients reflected those of white patients, 15%, 20%, and 15% of the treatment delay that Black, Hispanic, and other non-white race/ethnicity patients experience, respectively, could be eliminated. Treatment at an academic facility was the largest mediating factor, accounting for 11%, 8%, and 13% of the disparity in delayed time to treatment among Black, Hispanic, and other non-white race/ethnicity patients, respectively.
Discussion
In this study of 1,349,715 women, we demonstrate that Black, Hispanic, and other non-white race/ethnicity women are more likely than white women to experience breast cancer treatment delays, and we use mediation analysis to explore the factors that contribute to these inequities. Our findings are consistent with findings of previous research and support a need for such disparities to be acknowledged. Existing disparities research considers race/ethnicity as a factor associated with an outcome without identifying intervenable variables that cause these disparities to exist.10,11 In this study, we considered the importance of temporal ordering of variables to partition out causes of disparities in treatment delays. Identifying factors that contribute to disparities in treatment delays provides opportunities for intervention and improvement in breast cancer care.
The mediating factors of delayed treatment explored were education, comorbidities, insurance, and treatment at an academic facility. Per our analysis, these mediators together accounted for 15%, 19%, and 15% of treatment delays experienced by Black, Hispanic, and other non-white race/ethnicity patients, respectively. Identifying the contribution that each of these factors makes to treatment delays provides valuable information for reducing these delays via targeted intervention strategies. Further investigation is needed to determine the remaining 81–85% of the mediation. Many of the remaining factors may be variables not captured by NCDB or variables that cannot be readily intervened upon. It is interesting to note that income was not a mediator because higher income was unexpectedly associated with higher delays in treatment. While our study cannot elucidate the specific reasons why this was observed, one possible explanation is that higher-income patients likely have more options for treatment plans and may undergo additional imaging, biopsies, and second opinion consultations.
Treatment at an academic facility was the mediator with the greatest contribution to treatment delays across the three comparator races/ethnicities. This requires further exploration of why academic facilities treat a greater number of minority patients and why treatment at these facilities contributes to delayed treatment. Addressing this mediating factor at the system and hospital level requires additional information about the association between academic facilities and treatment delays. One possible reason for this association is the inherent delay in the referral process for patients diagnosed at outside hospitals. Additionally, the greater volume of complex cases treated at academic facilities might contribute to longer treatment delays. While academic facilities are associated with better oncologic and long-term outcomes, recent evidence suggests that academic facilities experienced greater patient volume growth than did community hospitals.13–17 These trends in greater patient volume may exacerbate racial/ethnic disparities in treatment delays. It is unclear whether academic facilities are aware of these disparities and the extent to which systemic barriers may be leading to treatment delays among disadvantaged populations.
It is likely that disparities in breast cancer outcomes, such as mortality and quality of life, reflect disparities in time to treatment along with screening rates, stage at diagnosis, and other factors of breast cancer treatment. Therefore, the mediating factors of time to treatment described in this study likely contribute to disparities in overall breast cancer outcomes. Further research is necessary to explore other mediating factors in breast cancer disparities in order to design and implement policy changes and interventions that address these disparities. It remains unclear which factors are easiest to intervene upon by individual physicians, for example.
The systemic inequities demonstrated by this study parallel the inequities seen throughout the COVID-19 pandemic. Individuals of minority races/ethnicities experienced higher rates of both SARS-CoV-2 infection and SARS-CoV-2-related death when compared with non-Hispanic white individuals. These disproportionate rates of infection and death reflect systemic inequities in our healthcare system and the social determinants of health that contribute to such inequities.18 Additionally, the COVID-19 pandemic caused both intentional and consequential treatment delays in cancer care, prolonging breast cancer treatment for many patients. Hispanic patients were more likely to experience delayed cancer treatment during the COVID-19 pandemic when compared with white patients.19 The COVID-19 pandemic has brought to light many of the inequities in our healthcare system reflected in this study, further solidifying the importance of determining the mediating factors that contribute to such inequities. The benefit of determining these mediating factors is that they can serve as a guide for targeted interventions and allocation of resources to improve care delivery. Interventions may include close follow-up with care coordinators to address any practical barriers to timely treatment. Once interventions are put into place, program evaluation methods are required to determine the efficacy of these interventions. A repeat analysis of breast cancer treatment delay after interventions are deployed may help monitor and reduce these inequities. Because interventions are likely to take place at the institutional level, this may require an individualized analysis of a particular institution and may not be captured with the NCDB.
This study is not without limitations. Primarily, limitations inherent to retrospective study design and the use of large databases, such as selection bias and confounding, should be considered. Limitations of the NCDB include possible selection bias, coding errors, incomplete data, and missing variables that may be relevant to mediation analysis. For example, variables such as income and education are measured at the zip code level and not at the patient level, which could have led to measurement error and bias. The limitations of the NCDB, specifically incomplete data and missing variables, are likely contributors to the fact that the mediators in our study accounted for just 15–19% of treatment delays. Further, we were able to measure system-wide inequities, but we are unable to assess racial/ethnic bias or discrimination experienced by patients. Strengths of this study include the use of mediation analysis to assess factors contributing to treatment delays as well as the large number of patients included in the analysis.
Conclusions
This study confirms that patients who identify as Black, Hispanic, or other non-white race/ethnicity are more likely to experience delayed breast cancer treatment than white patients. Mediation analysis demonstrates that intermediate factors have an impact on treatment delays. These findings suggest that social determinants of health continue to explain inequitable breast cancer treatment and outcomes. In addition to the five mediators that we have evaluated, further investigation of other mediating factors will enable targeted interventions at the system, hospital, and individual level to reduce or eliminate racial/ethnic disparities. This will prompt individual physicians and hospital systems to be more in tune with racial/ethnic disparities allowing them to implement interventions on a patient per patient basis.
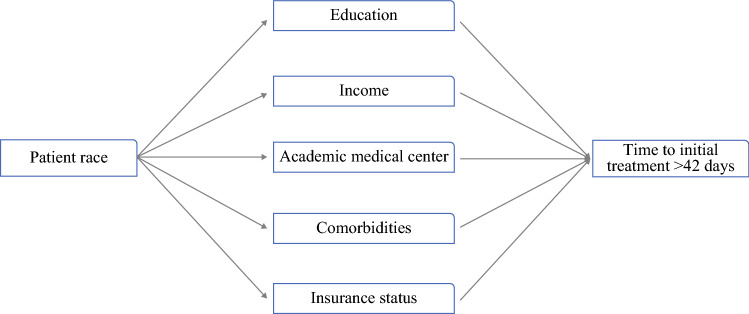
Fig. 1.
Causal directed acyclic graph of proposed mediators involved in racial/ethnic disparities in delayed initial treatment
Funding
None.
Declarations
Conflict of interest
None.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Centers for Disease Control and Prevention. An Update on Cancer Deaths in the United States. CDCBreast Cancer. 2021
- 2.DeSantis CE, Ma J, Gaudet MM, et al. Breast cancer statistics, 2019. CA Cancer J Clin. 2019;69(6):438–451. doi: 10.3322/caac.21583. [DOI] [PubMed] [Google Scholar]
- 3.Orsi JM, Margellos-Anast H, Whitman S. Black-White health disparities in the United States and Chicago: a 15-year progress analysis. Am J Public Health. 2010;100(2):349–356. doi: 10.2105/AJPH.2009.165407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khorana AA, Tullio K, Elson P, et al. Time to initial cancer treatment in the United States and association with survival over time: an observational study. PLoS ONE. 2019;14(3):e0213209. doi: 10.1371/journal.pone.0213209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bleicher RJ, Ruth K, Sigurdson ER, et al. Time to surgery and breast cancer survival in the United States. JAMA Oncol. 2016;2(3):330–339. doi: 10.1001/jamaoncol.2015.4508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cone EB, Marchese M, Paciotti M, et al. Assessment of time-to-treatment initiation and survival in a cohort of patients with common cancers. JAMA Netw Open. 2020;3(12):e2030072. doi: 10.1001/jamanetworkopen.2020.30072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sheppard VB, Oppong BA, Hampton R, et al. Disparities in breast cancer surgery delay: the lingering effect of race. Ann Surg Oncol. 2015;22(9):2902–2911. doi: 10.1245/s10434-015-4397-3. [DOI] [PubMed] [Google Scholar]
- 8.Yedjou CG, Tchounwou PB, Payton M, et al. Assessing the racial and ethnic disparities in breast cancer mortality in the United States. Int J Environ Res Public Health. 2017;14(5):E486. doi: 10.3390/ijerph14050486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blazek A, O’Donoghue C, Terranella S, et al. Impact of inequities on delay in breast cancer management in women undergoing second opinions. J Surg Res. 2021;268:445–451. doi: 10.1016/j.jss.2021.06.084. [DOI] [PubMed] [Google Scholar]
- 10.VanderWeele TJ, Robinson WR. On causal interpretation of race in regressions adjusting for confounding and mediating variables. Epidemiology. 2014;25(4):473–484. doi: 10.1097/EDE.0000000000000105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Valeri L, VanderWeele TJ. Mediation analysis allowing for exposure–mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros: Correction to Valeri and VanderWeele (2013) Psychol Methods. 2013;18(4):474–474. doi: 10.1037/a0035596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pearl J. The causal mediation formula—a guide to the assessment of pathways and mechanisms. Prev Sci. 2012;13(4):426–436. doi: 10.1007/s11121-011-0270-1. [DOI] [PubMed] [Google Scholar]
- 13.Shulman LN, Palis BE, McCabe R, et al. Survival as a quality metric of cancer care: use of the National Cancer Data Base to assess hospital performance. J Oncol Pract. 2018;14(1):e59–e72. doi: 10.1200/JOP.2016.020446. [DOI] [PubMed] [Google Scholar]
- 14.Wolfson JA, Sun C-L, Wyatt LP, Hurria A, Bhatia S. Impact of care at comprehensive cancer centers on outcome: results from a population-based study. Cancer. 2015;121(21):3885–3893. doi: 10.1002/cncr.29576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pfister DG, Rubin DM, Elkin EB, et al. Risk adjusting survival outcomes in hospitals that treat patients with cancer without information on cancer stage. JAMA Oncol. 2015;1(9):1303–1310. doi: 10.1001/jamaoncol.2015.3151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Birkmeyer NJO, Goodney PP, Stukel TA, Hillner BE, Birkmeyer JD. Do cancer centers designated by the National Cancer Institute have better surgical outcomes? Cancer. 2005;103(3):435–441. doi: 10.1002/cncr.20785. [DOI] [PubMed] [Google Scholar]
- 17.Frosch ZAK, Illenberger N, Mitra N, et al. Trends in patient volume by hospital type and the association of these trends with time to cancer treatment initiation. JAMA Netw Open. 2021;4(7):e2115675. doi: 10.1001/jamanetworkopen.2021.15675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alcendor DJ. Racial disparities-associated COVID-19 mortality among minority populations in the US. J Clin Med. 2020;9(8):2442. doi: 10.3390/jcm9082442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schmidt AL, Bakouny Z, Bhalla S, et al. Cancer care disparities during the covid-19 pandemic: covid-19 and cancer outcomes study. Cancer Cell. 2020;38(6):769–770. doi: 10.1016/j.ccell.2020.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]