This cohort study assesses whether the period after an ischemic stroke is associated with the risk of recurrent stroke in patients aged 66 years or older who are undergoing elective nonneurologic, noncardiac surgery.
Key Points
Question
Is the time elapsed since an ischemic stroke associated with an increased risk of recurrent stroke in older patients undergoing elective nonneurologic, noncardiac surgery?
Findings
In this cohort study of 5 841 539 patients, those who had a stroke within 30 days before surgery had an 8-fold higher risk of stroke compared with patients without a previous stroke. The risk of stroke significantly decreased at 90 days and did not decrease significantly thereafter.
Meaning
These findings suggest that waiting more than 90 days after a stroke may not reduce the risk of recurrent stroke in older patients undergoing elective nonneurologic, noncardiac surgery.
Abstract
Importance
Perioperative strokes are a major cause of death and disability. There is limited information on which to base decisions for how long to delay elective nonneurologic, noncardiac surgery in patients with a history of stroke.
Objective
To examine whether an association exists between the time elapsed since an ischemic stroke and the risk of recurrent stroke in older patients undergoing elective nonneurologic, noncardiac surgery.
Design, Setting, and Participants
This cohort study used data from the 100% Medicare Provider Analysis and Review files, including the Master Beneficiary Summary File, between 2011 and 2018 and included elective nonneurologic, noncardiac surgeries in patients 66 years or older. Patients were excluded if they had more than 1 procedure during a 30-day period, were transferred from another hospital or facility, were missing information on race and ethnicity, were admitted in December 2018, or had tracheostomies or gastrostomies. Data were analyzed May 7 to October 23, 2021.
Exposures
Time interval between a previous hospital admission for acute ischemic stroke and surgery.
Main Outcomes and Measures
Acute ischemic stroke during the index surgical admission or rehospitalization for stroke within 30 days of surgery, 30-day all-cause mortality, composite of stroke and mortality, and discharge to a nursing home or skilled nursing facility. Multivariable logistic regression models were used to estimate adjusted odds ratios (AORs) to quantify the association between outcome and time since ischemic stroke.
Results
The final cohort included 5 841 539 patients who underwent elective nonneurologic, noncardiac surgeries (mean [SD] age, 74.1 [6.1] years; 3 371 329 [57.7%] women), of which 54 033 (0.9%) had a previous stroke. Patients with a stroke within 30 days before surgery had higher adjusted odds of perioperative stroke (AOR, 8.02; 95% CI, 6.37-10.10; P < .001) compared with patients without a previous stroke. The adjusted odds of stroke were not significantly different at an interval of 61 to 90 days between previous stroke and surgery (AOR, 5.01; 95% CI, 4.00-6.29; P < .001) compared with 181 to 360 days (AOR, 4.76; 95% CI, 4.26-5.32; P < .001). The adjusted odds of 30-day all-cause mortality were higher in patients who underwent surgery within 30 days of a previous stroke (AOR, 2.51; 95% CI, 1.99-3.16; P < .001) compared with those without a history of stroke, and the AOR decreased to 1.49 (95% CI, 1.15-1.92; P < .001) at 61 to 90 days from previous stroke to surgery but did not decline significantly, even after an interval of 360 or more days.
Conclusions and Relevance
The findings of this cohort study suggest that, among patients undergoing nonneurologic, noncardiac surgery, the risk of stroke and death leveled off when more than 90 days elapsed between a previous stroke and elective surgery. These findings suggest that the recent scientific statement by the American Heart Association to delay elective nonneurologic, noncardiac surgery for at least 6 months after a recent stroke may be too conservative.
Introduction
More than 25 million patients undergo surgery each year in the US.1,2 The incidence of perioperative strokes in patients undergoing nonneurologic, noncardiac surgery is between 0.1% and 1%.3,4,5 Although perioperative strokes are uncommon, they can have a devastating impact and are the leading cause of disability in the US.6,7 According to the American Heart Association, the overall number of strokes will increase 2-fold by 2050,6 and the projected annual cost of stroke care in the US is expected to increase to $240 billion by 2030.8
The American Heart Association and American Stroke Association published a scientific statement in 2021 that advised delaying elective nonneurologic, noncardiac surgery at least 6 months and possibly as long as 9 months after a previous stroke to reduce the risk of recurrent stroke.9 This recommendation was based mainly on the results of a single retrospective analysis of 481 183 patients undergoing elective nonneurologic, noncardiac surgery that used data from a Danish national health care database.10 The risk of recurrent stroke was highest in patients undergoing surgery within 3 months of a previous stroke and leveled off at 9 months. In separate studies,11,12 the same research group found that the risk of postoperative stroke was also increased in patients with a recent stroke who underwent emergency nonneurologic, noncardiac surgery and aortic valve replacement. However, the results of these analyses may not be generalizable to the US population; compared with European nations, the US has a nearly 2-fold higher rate of obesity; a 50% higher rate of hospitalizations from preventable causes, such as diabetes and hypertension; and a lower life expectancy.13
The aim of this study was to examine whether the time elapsed since a previous acute ischemic stroke was associated with the risk of recurrent stroke in older patients undergoing elective nonneurologic, noncardiac surgery in the US. Because the 2021 scientific statement represents the consensus of clinical experts and is not a clinical practice guideline, formal evidence-based recommendations from the American Heart Association and American Stroke Association do not yet exist on how long to delay elective nonneurologic, noncardiac surgery after a previous stroke. This study could help to inform the development of future evidence-based recommendations in a clinical practice guideline regarding the optimal timing of surgery after a previous stroke.
Methods
Data Source
This cohort study used data from the 100% Medicare Provider Analysis and Review files, including the Master Beneficiary Summary File, between 2011 and 2018. These databases include beneficiary demographic information (age, sex, and self-reported race and ethnicity); payer information; International Classification of Diseases, Ninth Revision and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision diagnosis and procedure codes; source of admission; whether the admission was elective; discharge destination; and date of death. The institutional review board of the University of Rochester School of Medicine and Dentistry reviewed the proposal, determined that it met federal criteria for exemption, and waived the requirement for informed consent. The study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Study Sample
We included elective nonneurologic, noncardiac surgeries performed in patients 66 years and older (eFigure 1 in the Supplement). Patients who underwent more than 1 procedure during a 30-day period were excluded. We used the Agency for Healthcare Research and Quality Clinical Classifications Software to map International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and International Statistical Classification of Diseases, Tenth Revision, Procedure Coding System procedure codes into classes.14,15 We mapped ICD-9-CM and International Statistical Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnostic codes to Elixhauser comorbidity categories using the Elixhauser package in Stata (StataCorp LLC) based on algorithms created by Quan et al.16,17 We identified 7 466 389 hospital admissions for elective nonneurologic, noncardiac surgery between January 2013 and November 2018 (eFigure 1 in the Supplement). We excluded 1 418 438 patients younger than 66 years to have at least a 12-month lookback period for previous strokes. We excluded 51 160 patients transferred from another hospital or facility because these observations may have been incorrectly classified as elective admissions. We excluded 72 718 patients with missing information on race or ethnicity. We also excluded 59 396 patients admitted in December 2018 to have 30 days of follow-up after the index admission. In addition, we excluded 21 216 patients who underwent a second procedure within a 30-day period and excluded 1922 patients who underwent tracheostomies or gastrostomies because these procedures are more commonly performed in patients with a recent debilitating stroke who may be at particularly high risk for a recurrent stroke (ie, confounding by indication).10 The final analytic cohort consisted of 5 841 539 surgeries.
The primary outcome was whether a patient had an acute ischemic stroke during the index surgical admission or was rehospitalized within 30 days of the index surgical admission with a primary diagnosis of acute ischemic stroke. We used the present-on-admission indicator to identify perioperative strokes that occurred during the index surgical admission.18 The secondary outcomes were (1) 30-day all-cause mortality, (2) composite of acute ischemic stroke or death within 30 days, and (3) discharge to a nursing home or skilled nursing facility. We identified ischemic strokes using both ICD-9-CM (433-434.91) and ICD-10-CM (I63-I63.9) codes. The use of ICD-9-CM and ICD-10-CM diagnostic codes for acute stroke has been previously validated and shown to have a sensitivity of 82% for ischemic stroke.19 The key independent variable was whether a patient was admitted with a primary diagnosis of ischemic stroke before the index surgical admission.
Statistical Analysis
Data were analyzed from May 7 to October 23, 2021. In the main analysis, we used a multivariable logistic regression model to ascertain whether there was an independent association between a previous stroke and perioperative stroke. The model controlled for age, sex, race and ethnicity, dual-eligibility status (eligible for both Medicare and Medicaid), whether a patient was living in the community or in a nursing home or skilled nursing facility before surgery, comorbidities, surgical procedure class, and year of admission. We specified the time interval between a previous stroke and the index surgery as a categorical variable: 30 days or fewer, 31 to 60 days, 61 to 90 days, 91 to 180 days, 181 to 360 days, and 361 to 720 days. The reference category was patients with no previous stroke within the 720-day lookback period. We specified the time interval as a categorical variable because previous research showed that the association of the time elapsed between a previous stroke and surgery with the risk of a recurrent perioperative stroke was nonlinear.10 We then separately reestimated this model using each of the secondary outcomes: death or stroke within 30 days, death within 30 days, and discharge to a nursing home or skilled nursing facility. We characterized the association between time interval and risk of adverse outcome using adjusted odds ratios (AORs) and adjusted rates. Patients with missing data (only 1% of the analytic cohort) were excluded from the secondary analysis.
We conducted a series of subgroup analyses to examine whether the findings were, in part, a function of the risk of surgery. Rather than dividing surgeries arbitrarily into risk categories based on expert consensus,20 we used a regression-based approach to categorize surgeries into low-, intermediate-, and high-risk groups based on the risk of death (eTable 1 in the Supplement). We first reestimated the baseline model for 30-day mortality using logistic regression modeling, in which we specified the surgical procedure classes as fixed effects, and then estimated the adjusted risk for each surgical procedure class. After examining the distribution of the procedural risk of mortality, we divided the procedure classes into 3 groups based on the risk of 30-day mortality: 0.5% or less, more than 0.5% to 1.0%, and more than 1.0%. We then separately estimated stratified regression models for the main outcome and for the secondary outcomes for each of the 3 procedure risk categories. After excluding patients with fractures, we performed a subgroup analysis in patients who underwent elective knee and hip arthroplasties. Because of sample size considerations, we specified the time interval between a previous stroke and the index surgery as a categorical variable: 90 days or fewer, 91 to 180 days, 181 to 360 days, and 361 to 720 days for the low-risk surgery and orthopedic cohorts.
All statistical analyses were performed using Stata/MP, version 17.0 (StataCorp LLC). We used cluster robust variance estimators to account for the clustering of observations within hospitals in the nonhierarchical regression models. The threshold for statistical significance was a 2-sided P < .05.
Results
Patient Population
The study was based on 5 841 539 surgeries (patients had a mean [SD] age of 74.1 [6.1] years; 3 371 329 [57.7%] were women and 2 470 210 [42.3%] men; and 1.5% were Asian, 6.2% Black, 4.6% Hispanic, 0.4% American Indian or Alaska Native, 86.8% non-Hispanic White, and 0.6% other individuals [“other” was listed as such in the databases; no additional data are available for that category]), of which 54 033 (0.9%) were in patients with a previous stroke (Table). Patients with a history of strokes were slightly older than those without such a history (age 76.0 vs 74.1 years), more likely to be men (52.8% vs 42.2%), and more likely to have dual-eligibility status (11.8% vs 7.5%). Patients with a history of stroke were also more likely than those with no history of stroke to have had congestive heart failure (13.4% vs 5.9%), cardiac arrhythmias (30.4% vs 16.9%), valvular disease (10.9% vs 5.7%), peripheral vascular disease (26.6% vs 7.8%), and kidney failure (17.4% vs 9.8%). Patients with a history of stroke vs those with no previous stroke were less likely to undergo surgery with a low risk of mortality (39.6% vs 57.5%) and more likely to undergo surgery with a higher risk of mortality (39.3% vs 19.8%).
Table. Patient Characteristics.
| Characteristic | Patients, No. (%) | |
|---|---|---|
| No previous stroke (n = 5 787 506) | Previous stroke (n = 54 033) | |
| Time to previous stroke | ||
| No strokes within 720 d | 5 787 506 (100.0) | NA |
| 361-720 d | NA | 25 262 (46.8) |
| 181-360 d | NA | 14 675 (27.2) |
| 91-180 d | NA | 7611 (14.1) |
| 61-90 d | NA | 2612 (4.8) |
| 31-60 d | NA | 2356 (4.4) |
| ≤30 d | NA | 1517 (2.8) |
| Age, y | ||
| Mean (SD) | 74.1 (6.1) | 76.0 (6.5) |
| 66-69 | 1 596 091 (27.6) | 10 042 (18.6) |
| 70-74 | 1 772 999 (30.6) | 14 805 (27.4) |
| 75-79 | 1 293 199 (22.3) | 13 563 (25.1) |
| 80-84 | 732 002 (12.6) | 9432 (17.5) |
| ≥ 85 | 393 215 (6.8) | 6191 (11.5) |
| Sex | ||
| Female | 3 345 805 (57.8) | 25 524 (47.2) |
| Male | 2 441 701 (42.2) | 28 509 (52.8) |
| Race and ethnicity | ||
| Asian | 85 301 (1.5) | 580 (1.1) |
| Black | 359 390 (6.2) | 4424 (8.2) |
| Hispanic | 264 544 (4.6) | 2248 (4.2) |
| American Indian or Alaska Native | 21 646 (0.4) | 202 (0.4) |
| Non-Hispanic White | 5 021 418 (86.8) | 46 326 (85.7) |
| Othera | 35 207 (0.6) | 253 (0.5) |
| Dual eligibility | 433 586 (7.5) | 6383 (11.8) |
| Transfer from nursing home or skilled nursing facility | 11 711 (0.2) | 491 (0.9) |
| Comorbidities | ||
| Congestive heart failure | 340 168 (5.9) | 7261 (13.4) |
| Cardiac arrythmias | 979 309 (16.9) | 16 400 (30.4) |
| Valvular disease | 327 886 (5.7) | 5891 (10.9) |
| Pulmonary circulation disorders | 89 860 (1.6) | 1430 (2.6) |
| Peripheral vascular disease | 453 313 (7.8) | 14 395 (26.6) |
| Hypertension | ||
| Uncomplicated | 3 559 013 (61.5) | 35 069 (64.9) |
| Complicated | 714 135 (12.3) | 11 410 (21.1) |
| Chronic pulmonary disease | 1 060 027 (18.3) | 13 239 (24.5) |
| Diabetes | ||
| Uncomplicated | 1 037 323 (17.9) | 12 915 (23.9) |
| Complicated | 347 019 (6.0) | 6331 (11.7) |
| Hypothyroidism | 1 041 768 (18.0) | 8927 (16.5) |
| Kidney failure | 567 872 (9.8) | 9381 (17.4) |
| Liver disease | 132 168 (2.3) | 1435 (2.7) |
| Peptic ulcer disease | 36 226 (0.6) | 415 (0.8) |
| AIDS or HIV | 20 039 (0.3) | 334 (0.6) |
| Lymphoma | 28 220 (0.5) | 298 (0.6) |
| Metastatic cancer | 164 638 (2.8) | 1565 (2.9) |
| Solid tumor without metastasis | 777 688 (13.4) | 8581 (15.9) |
| Rheumatoid arthritis | 278 877 (4.8) | 2445 (4.5) |
| Coagulopathy | 161 175 (2.8) | 2031 (3.8) |
| Obesity | 1 084 111 (18.7) | 7392 (13.7) |
| Weight loss | 113 039 (2.0) | 2199 (4.1) |
| Fluid and electrolyte disorder | 631 752 (10.9) | 8442 (15.6) |
| Blood loss anemia | 51 804 (0.9) | 763 (1.4) |
| Deficiency anemia | 99 587 (1.7) | 1308 (2.4) |
| Alcohol abuse | 63 182 (1.1) | 862 (1.6) |
| Drug abuse | 42 412 (0.7) | 513 (0.9) |
| Psychoses | 22 337 (0.4) | 356 (0.7) |
| Depression | 721 894 (12.5) | 7456 (13.8) |
| Surgical risk mortality | ||
| Low (≤0.5%) | 3 330 180 (57.5) | 21 419 (39.6) |
| Intermediate (>0.5%-1.0%) | 1 312 297 (22.7) | 11 396 (21.1) |
| High (>1.0%) | 1 145 029 (19.8) | 21 218 (39.3) |
| Surgical procedure classes | ||
| Laminectomy | 509 666 (8.8) | 4360 (8.1) |
| Thyroidectomy | 25 294 (0.4) | 301 (0.6) |
| Tonsillectomy | 2791 (0) | 32 (0.1) |
| Lobectomy or pneumonectomy | 164 591 (2.8) | 2201 (4.1) |
| Peripheral vascular bypass | 106 136 (1.8) | 4891 (9.1) |
| Embolectomy or endarterectomy of lower limbs | 96 870 (1.7) | 4082 (7.6) |
| Procedures on spleen | 23 916 (0.4) | 187 (0.3) |
| Colostomy | 35 109 (0.6) | 544 (1.0) |
| Ileostomy | 48 332 (0.8) | 618 (1.1) |
| Gastrectomy | 65 223 (1.1) | 505 (0.9) |
| Small-bowel resection | 33 069 (0.6) | 322 (0.6) |
| Colorectal resection | 317 491 (5.5) | 3729 (6.9) |
| Appendectomy | 32 474 (0.6) | 292 (0.5) |
| Cholecystectomy | 107 351 (1.9) | 1414 (2.6) |
| Inguinal or femoral hernia repair | 23 114 (0.4) | 371 (0.7) |
| Hernia repair, other | 164 202 (2.8) | 1411 (2.6) |
| Exploratory laparotomy | 7925 (0.1) | 127 (0.2) |
| Lysis of adhesions | 205 433 (3.5) | 1994 (3.7) |
| Resection or removal of urinary obstruction | 50 579 (0.9) | 1177 (2.2) |
| Nephrectomy | 114 033 (2.0) | 1091 (2.0) |
| Kidney transplant | 1293 (0) | 10 (0) |
| Transurethral resection of the prostate | 54 858 (0.9) | 1137 (2.1) |
| Open prostatectomy | 127 313 (2.2) | 627 (1.2) |
| Oophorectomy | 137 611 (2.4) | 1106 (2.0) |
| Other operation on ovaries | 5498 (0.1) | 50 (0.1) |
| Hysterectomy | 129 088 (2.2) | 946 (1.8) |
| Repair of cystocele and rectocele | 31 226 (0.5) | 183 (0.3) |
| Arthroplasty, knee | 1 942 181 (33.6) | 11 547 (21.4) |
| Hip replacement | 1 031 160 (17.8) | 7085 (13.1) |
| Arthroplasty, other than hip or knee | 342 124 (5.9) | 2691 (5.0) |
| Amputation of lower extremity | 68 844 (1.2) | 3011 (5.6) |
| Spinal fusion | 687 917 (11.9) | 5458 (10.1) |
| Outcomes | ||
| 30-d Stroke | 19 066 (0.3) | 1411 (2.6) |
| 30-d Mortality | 45 193 (0.8) | 1315 (2.4) |
| Death or stroke, 30-d | 62 210 (1.1) | 2616 (4.8) |
| Discharge to nursing home or skilled nursing facility | 1 430 611 (24.7) | 19 929 (36.9) |
Abbreviation: NA, not applicable.
The other category was listed as such in the databases; no additional data are available for that category.
Unadjusted Outcomes
The incidence of perioperative stroke in patients with a previous stroke vs without stroke was 2.6% vs 0.3% (Table). Fifty percent of the strokes in the perioperative 30-day period that required hospital readmission occurred within 7 days of the index surgical admission (eFigure 2 in the Supplement). In patients with a stroke within 30 days before surgery, the risk of perioperative stroke was higher (unadjusted odds ratio [OR], 18.86; 95% CI, 15.23-23.35; P < .001) than in patients without a previous stroke (Figure 1). Patients with a stroke within 30 days before surgery vs those without a previous stroke had a higher risk of 30-day mortality (unadjusted OR, 9.94; 95% CI, 8.20-12.05; P < .001), composite of stroke or mortality (unadjusted OR, 12.94; 95% CI, 11.10-15.08; P < .001), or discharge to a nursing home or skilled nursing facility (unadjusted OR, 2.68; 95% CI, 2.42-2.98; P < .001).
Figure 1. Risk of Major Adverse Events and Discharge to Nursing Home or Skilled Nursing Facility Stratified by Time to Previous Stroke.
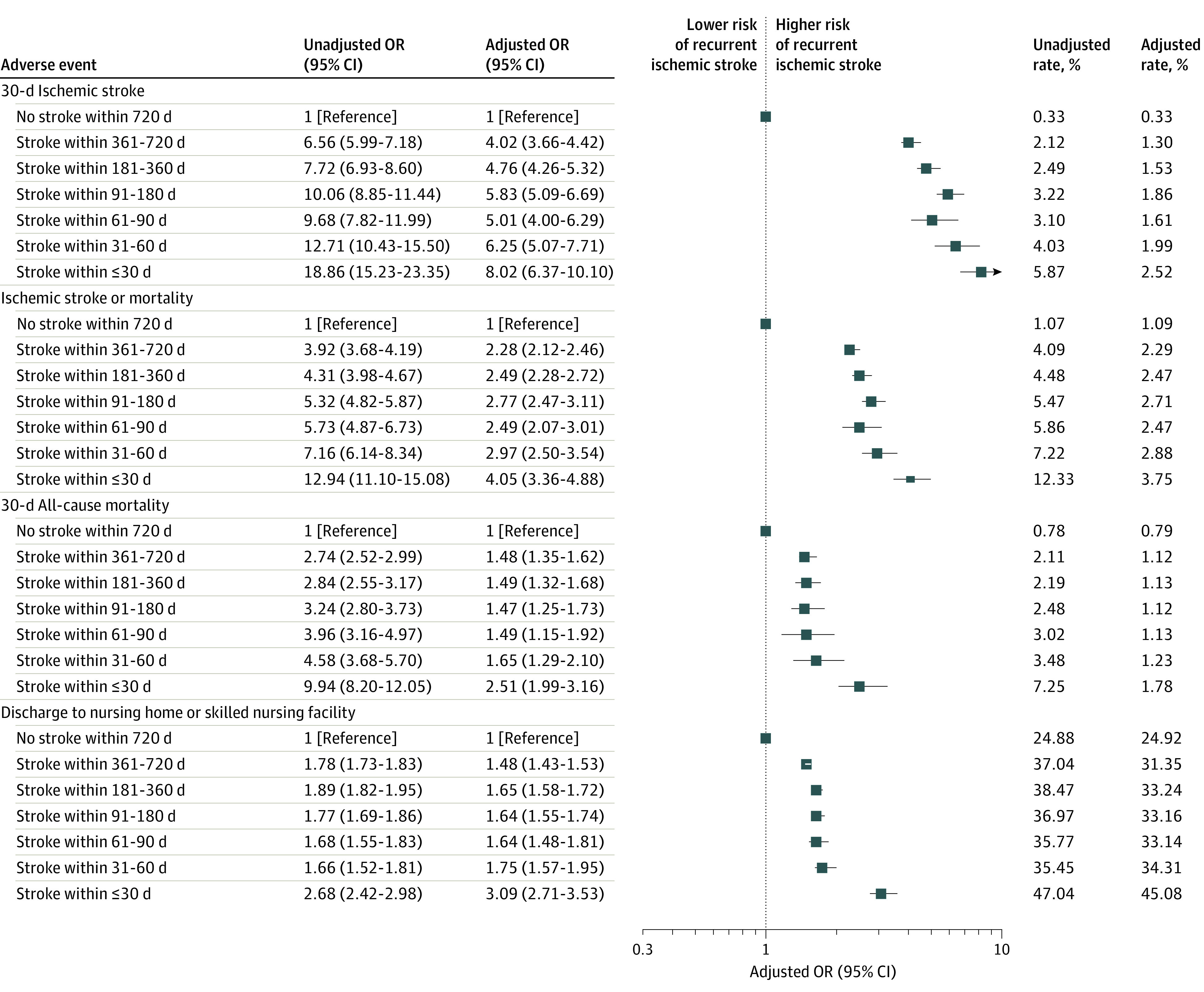
Odds ratios (ORs) were adjusted for age, sex, race and ethnicity, dual-eligibility status, transfer from a nursing home or skilled nursing facility, comorbidities, surgical procedure class, and year of admission. Error bars indicate the 95% CIs.
Adjusted Outcomes
After adjusting for age, sex, race and ethnicity, dual-eligibility status, transfer from a nursing home or skilled nursing facility, comorbidities, surgical procedure class, and year of admission, patients with a history of stroke 30 days or fewer before surgery had higher odds of recurrent stroke within 30 days after surgery (AOR, 8.02; 95% CI, 6.37-10.10; P < .001) than patients without a previous stroke (Figure 1; eTable 2 in the Supplement). The adjusted odds of stroke were not significantly different at an interval of 61 to 90 days between previous stroke and index surgery (AOR, 5.01; 95% CI, 4.00-6.29; P < .001) compared with 181 to 360 days (AOR, 4.76; 95% CI, 4.26-5.32; P < .001). The adjusted rate of stroke was 2.52% in patients with a history of stroke within 30 days of surgery compared with 0.33% in patients without a previous stroke (adjusted risk difference, 2.19%; 95% CI, 1.64-2.74; P < .001) (Figure 1).
The adjusted odds of 30-day all-cause mortality were higher (AOR, 2.51; 95% CI, 1.99-3.16; P < .001) in patients who underwent surgery within 30 days of a previous stroke compared with patients without a history of stroke. The odds of 30-day mortality decreased to 1.49 (95% CI, 1.15-1.92; P < .001) when the time interval between previous stroke and index surgery increased to 61 to 90 days but did not decrease further even when the time interval increased to 361 to 720 days (AOR, 1.48; 95% CI, 1.35-1.62; P < .001). The adjusted rate of 30-day mortality was 1.78% in patients undergoing surgery within 30 days of a previous stroke compared with 0.79% in patients without a history of stroke (adjusted risk difference, 0.99%; 95% CI, 0.63%-1.34%; P < .001).
The adjusted odds of discharge to a nursing home or skilled nursing facility were higher in patients who underwent surgery within 30 days of a previous stroke (AOR, 3.09; 95% CI, 2.71-3.53; P < .001) compared with patients without a previous stroke. The risk of discharge to a nursing home or skilled nursing facility decreased after 30 days but remained elevated for patients with a stroke more than 360 days before surgery. The adjusted rate of discharge to a nursing home or skilled nursing facility was 45.08% in patients undergoing surgery within 30 days of a previous stroke compared with 24.92% in patients without a history of stroke (adjusted risk difference, 20.16%; 95% CI, 17.56-22.76; P < .001).
The results of the subgroup analyses suggested that the risk of postoperative stroke leveled off when the time interval from a previous stroke was greater than 90 days for high-risk surgery (>1.0% risk of mortality) (Figure 2). The adjusted odds of stroke were not significantly different at 61 to 90 days (AOR, 3.61; 95% CI, 2.61-4.98; P < .001) compared with 181 to 360 days (AOR, 3.37; 95% CI, 2.85-3.99; P < .001). The risk of stroke did not appear to level off in patients undergoing intermediate- or low-risk surgery or hip and knee replacements (Figure 3 and Figure 4; eFigure 3 in the Supplement).
Figure 2. Risk of Major Adverse Events and Discharge to Nursing Home or Skilled Nursing Facility Stratified by Time to Previous Stroke in Patients Undergoing Surgical Procedures With High Risk of Mortality (>1.0%).
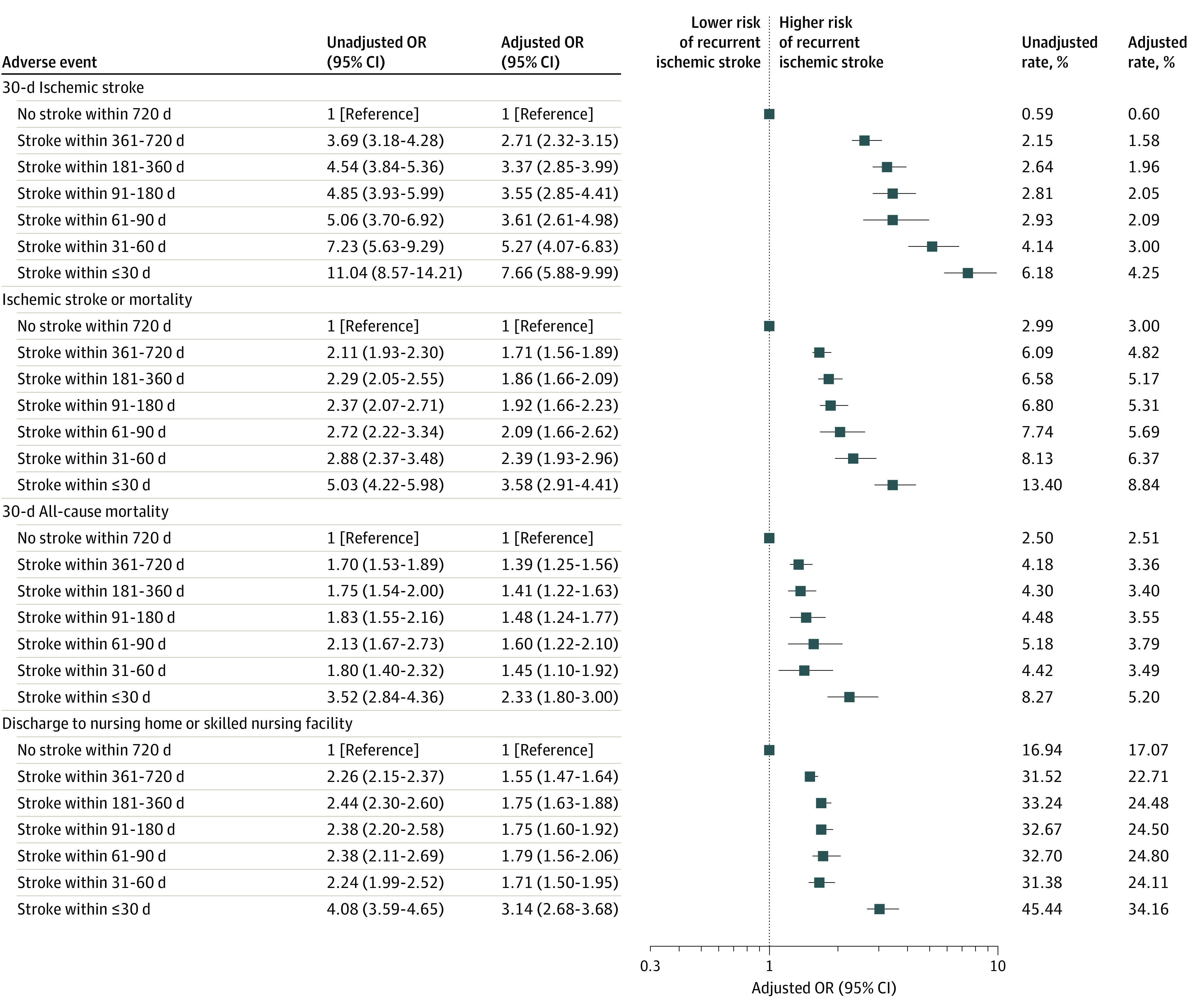
Odds ratios (ORs) were adjusted for age, sex, race and ethnicity, dual-eligibility status, transfer from a nursing home or skilled nursing facility, comorbidities, surgical procedure class, and year of admission. Error bars indicate the 95% CIs.
Figure 3. Risk of Major Adverse Events and Discharge to Nursing Home or Skilled Nursing Facility Stratified by Time to Previous Stroke in Patients Undergoing Surgical Procedures With Intermediate Risk of Mortality (>0.5%-1.0%).
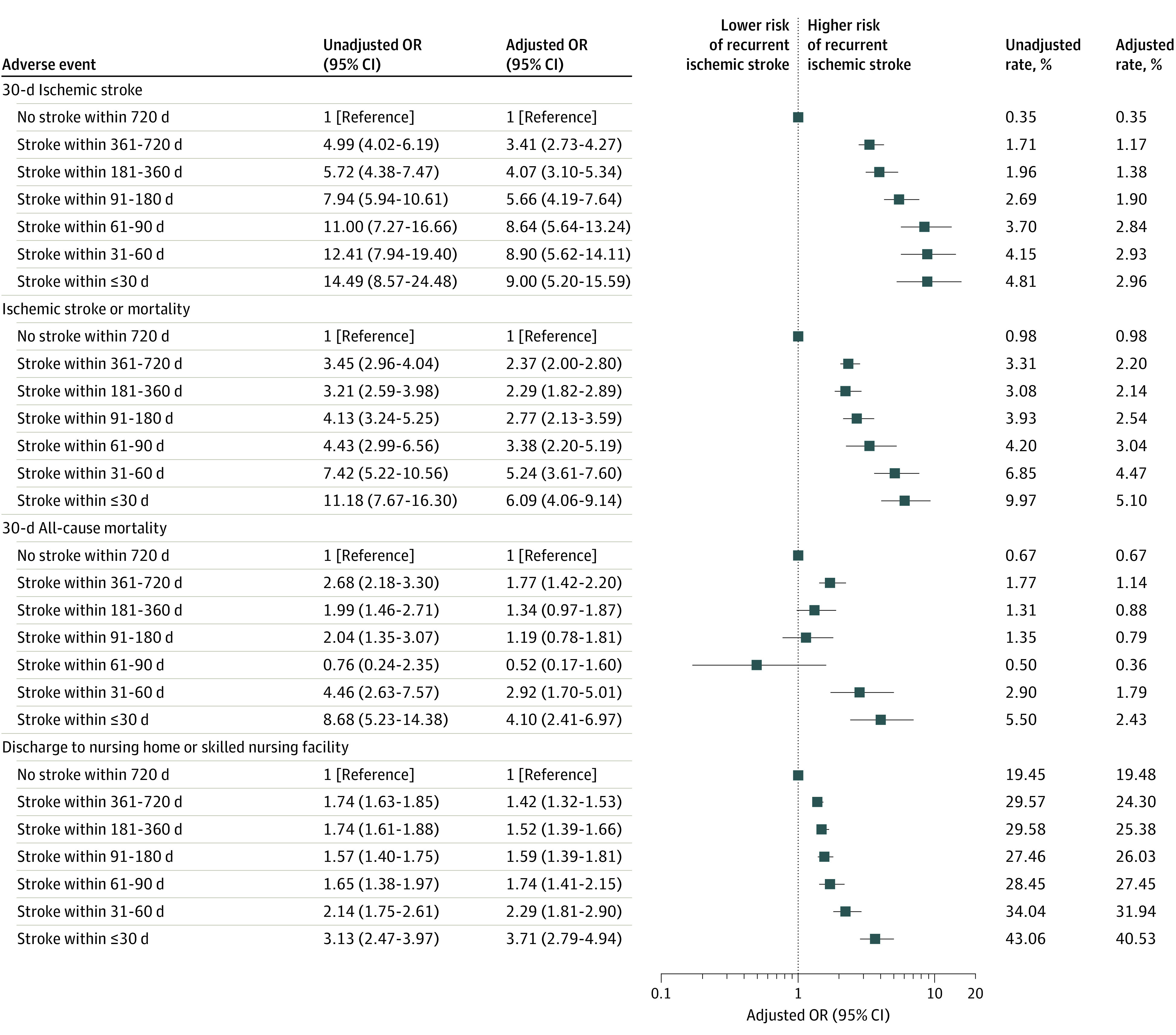
Odds ratios (ORs) were adjusted for age, sex, race and ethnicity, dual-eligibility status, transfer from a nursing home or skilled nursing facility, comorbidities, surgical procedure class, and year of admission. Error bars indicate the 95% CIs.
Figure 4. Risk of Major Adverse Events and Discharge to Nursing Home or Skilled Nursing Facility Stratified by Time to Previous Stroke in Patients Undergoing Surgical Procedures With Low Risk of Mortality (≤0.5%).
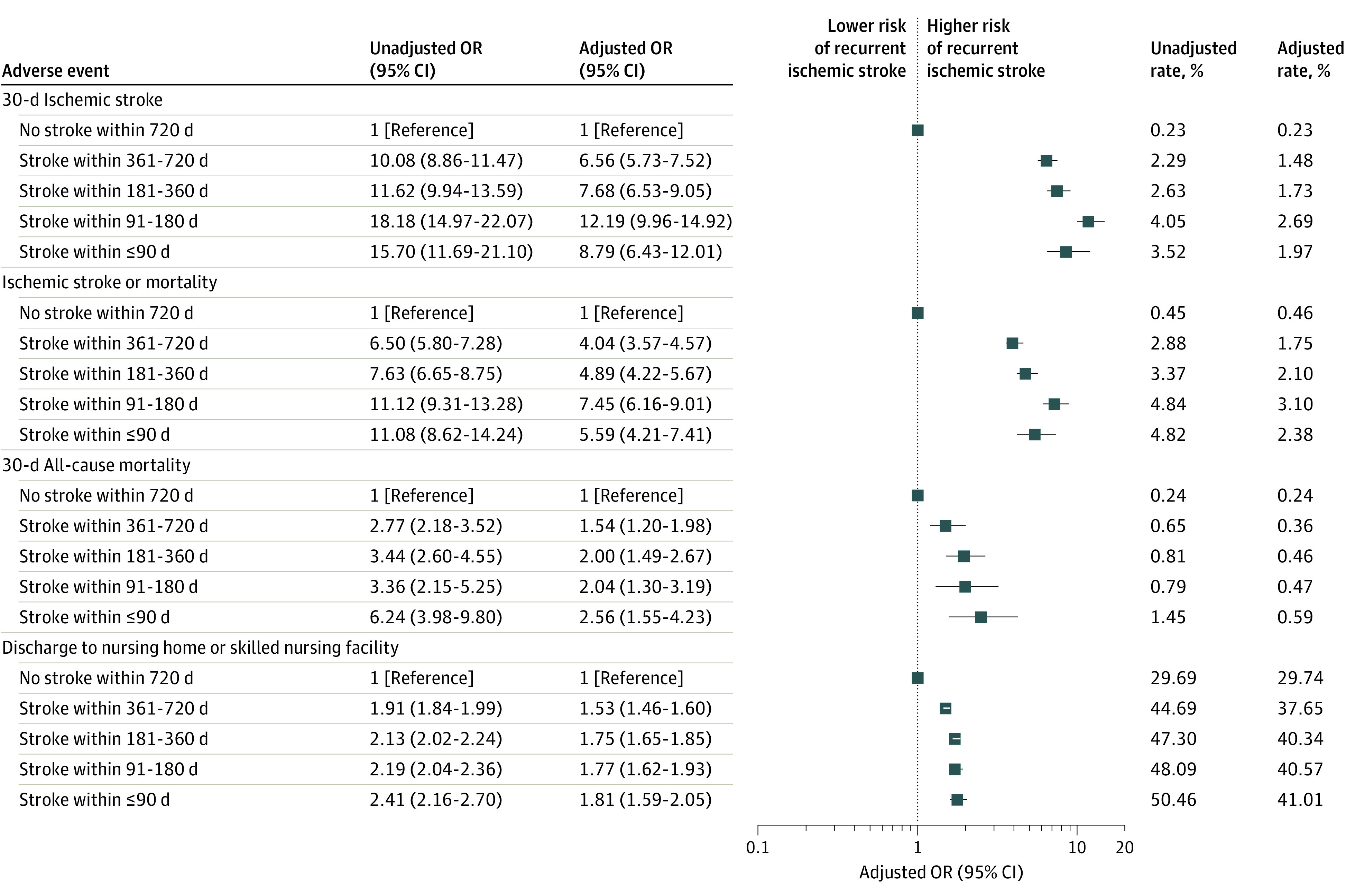
Odds ratios (ORs) were adjusted for age, sex, race and ethnicity, dual-eligibility status, transfer from a nursing home or skilled nursing facility, comorbidities, surgical procedure class, and year of admission. Error bars indicate the 95% CIs.
Discussion
Using national data on 5.8 million Medicare beneficiaries from 2011 to 2018, we found that patients with a history of stroke within 30 days of elective nonneurologic, noncardiac surgery had an 8-fold higher risk of acute ischemic stroke, a 2.5-fold higher risk of all-cause mortality, and a 3-fold higher risk of discharge to a nursing home or skilled nursing facility compared with patients without a history of stroke. The risk of recurrent stroke in patients with a previous stroke leveled off after 90 days but was still 5-fold higher compared with patients without such a history. The risk of death also leveled off after 90 days, but the rate was still 50% higher than in patients without a previous stroke.
The findings of the present study provide additional evidence to support a recent scientific statement by the American Heart Association and the American Stroke Association to delay elective nonneurologic, noncardiac surgery in patients with a previous stroke.9 This recommendation was based on 1 nationwide cohort study conducted using enhanced administrative data on 481 183 patients aged 20 years or older from Denmark between 2005 and 2011.10 Jørgensen and colleagues10 reported a strong time-dependent association between the risk of perioperative stroke and a history of stroke, with the risk of stroke leveling off after 9 months from a previous stroke. We found evidence that the risk of stroke leveled off over time but after 90 days instead of 6 months. Jørgensen and colleagues10 also described a substantially higher risk of perioperative stroke compared with our findings. In particular, they reported 68-fold and 24-fold higher odds of stroke in patients undergoing elective surgery within 3 months and 3 to 6 months after a previous stroke, respectively. One possible explanation for the difference between these 2 studies is that our study cohort included only older patients, whereas the Danish cohort included patients aged 20 years and older. Thus, the reference population in the Danish study had a lower underlying risk of stroke, which could account for the large differences in odds ratios between the present study and the study by Jørgensen and colleagues.10 It is unclear why the risk of stroke leveled off sooner in our patient cohort.
Until recently, the focus of perioperative optimization in patients undergoing nonneurologic, noncardiac surgery has been to lower the risk of cardiac complications. Preserving brain function may be the next frontier in perioperative care.21 As many as 10% of patients aged 65 years or older undergoing nonneurologic, noncardiac surgery experience long-term cognitive decline.22 Improving perioperative brain health includes measures to prevent perioperative strokes and the associated cognitive and functional declines.23 Although the incidence of perioperative strokes is between 0.1% and 1%,3,4,5 the incidence of silent (covert) cerebral infarcts may be 7% or higher.24,25 Silent cerebral infarcts are associated with a 2-fold higher risk of cognitive decline at 1-year follow-up.25 The association between surgical timing and the risk of silent cerebral ischemia may be similar to what is observed for overt strokes. If so, then the impact of delaying elective surgery may be associated with absolute risk reductions that are much greater than those observed in the present study.
Limitations
This study has limitations. First, we did not examine whether the decline in the risk of perioperative stroke over time after surgery is greater than the decline in the risk of stroke over time had surgery not taken place.26 Jørgensen and colleagues27 attempted to address this variable in the Danish study by performing a simulation in which they assigned a fictive surgery date to patients in the database and then examined the risk of perioperative stroke in patients with previous stroke who underwent fictive surgery. In other words, they assigned a surgery date to patients who did not actually undergo surgery and then repeated the analysis to examine the association between the time interval from a previous stroke and the risk of a recurrent stroke after the patients underwent the fictive surgery (no surgery at all) on the assigned surgery date. Jørgensen and colleagues27 found that the decline in the risk of recurrent stroke was much greater in patients undergoing surgery than in patients undergoing fictive surgery. However, the patients undergoing fictive surgery were not risk matched to the patients in the study cohort who actually underwent surgery. From a practical standpoint, it would not be feasible to risk match patients with a previous stroke who underwent surgery to a group of fictive patients who did not undergo surgery using the Medicare inpatient claims data. The patients hospitalized with a medical condition (eg, pneumonia, heart failure) are acutely ill, whereas patients undergoing elective surgery are not acutely ill.
Second, because the present study is observational, the risk of perioperative stroke in patients with a recent stroke may be higher than we report. In particular, patients with more severe strokes may have avoided elective surgery altogether, leading us to underestimate the risk of perioperative stroke in patients with a history of stroke. This limitation is important because patients and their physicians might decide that the adjusted rates of stroke reported in this study are low enough to proceed with elective surgery. The findings are based on data from self-selected patients who may not be representative of all patients who consider undergoing elective surgery after a previous stroke. It is plausible that patients with more severe strokes did not elect to pursue surgery. Therefore, the magnitude of risk associated with surgery after a stroke reported in the present study may represent the lower bound of risk when advising patients of the risk of a recurrent perioperative stroke. On the other hand, it is also possible that unobserved differences between patients with and without previous strokes could upwardly bias the strength of the association between previous strokes and perioperative strokes.
Third, it is possible that most of the strokes occurring during the perioperative period could have happened even had surgery not taken place. However, this outcome is unlikely because 50% of the strokes in the perioperative period occurred within 7 days of the index surgical admission, which suggests that these strokes were temporally associated with the surgery. Fourth, some of the difference in risk between patients with previous strokes that occurred further back in time (eg, 181-360 days) vs those with more recent strokes (eg, 61-90 days) could be owing to survivorship bias. In other words, those patients who survive 12 months and then undergo surgery are likely to be healthier (and therefore less likely to have a stroke) than the patients who have surgery 1 month after a stroke. Fifth, findings of the present study cannot be generalized to younger adults because our study is based on patients 66 years or older.
Sixth, we could not control for the use of antithrombotic therapy during the perioperative period. It is possible that the magnitude of the association between previous stroke and recurrent stroke was smaller in patients receiving optimal antithrombotic therapy. This area is important for future research. Seventh, because this study was not designed to compare the risk of stroke in patients with a previous stroke who underwent elective surgery and those who do not undergo elective surgery, findings of this study cannot aid patients in such decision-making.
Conclusions
The findings of this cohort study suggest that patients 66 years or older with a history of stroke have a higher risk of perioperative stroke and 30-day mortality compared with patients without previous stroke. The risk of stroke and death leveled off when more than 90 days elapsed between a previous stroke and elective surgery. These findings suggest that the recent scientific statement by the American Heart Association and American Stroke Association to delay elective nonneurologic, noncardiac surgery at least 6 months after a recent stroke may be too conservative. Additional studies using all-payer data are necessary to examine the role of surgical timing in patients younger than 66 years.
eFigure 1. Flow diagram describing selection of cases in the analytic cohort
eFigure 2. Temporal distribution of strokes after surgery
eFigure 3. Risk of major adverse events and discharge to skilled nursing facility stratified by time to previous stroke in patients undergoing total hip arthroplasties or total knee arthroplasties
eTable 1. Surgery mortality risk categories
eTable 2. Model coefficients for baseline analysis
References
- 1.Karaca Z, McDermott KW. High-volume invasive, therapeutic ambulatory surgeries performed in hospital-owned facilities, 2016. Agency for Healthcare Research and Quality. Updated September 2020. Accessed August 12, 2021. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb252-Invasive-Ambulatory-Surgeries-2016.jsp [PubMed]
- 2.Steiner CA, Karaca Z, Moore BJ, Imshaug MC, Pickens G. Surgeries in hospital-based ambulatory surgery and hospital inpatient settings, 2014. Agency for Healthcare Research and Quality . Updated July 2020. Accessed August 12, 2021. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb223-Ambulatory-Inpatient-Surgeries-2014.jsp [PubMed]
- 3.Bateman BT, Schumacher HC, Wang S, Shaefi S, Berman MF. Perioperative acute ischemic stroke in noncardiac and nonvascular surgery: incidence, risk factors, and outcomes. Anesthesiology. 2009;110(2):231-238. doi: 10.1097/ALN.0b013e318194b5ff [DOI] [PubMed] [Google Scholar]
- 4.Mashour GA, Shanks AM, Kheterpal S. Perioperative stroke and associated mortality after noncardiac, nonneurologic surgery. Anesthesiology. 2011;114(6):1289-1296. doi: 10.1097/ALN.0b013e318216e7f4 [DOI] [PubMed] [Google Scholar]
- 5.Smilowitz NR, Gupta N, Ramakrishna H, Guo Y, Berger JS, Bangalore S. Perioperative major adverse cardiovascular and cerebrovascular events associated with noncardiac surgery. JAMA Cardiol. 2017;2(2):181-187. doi: 10.1001/jamacardio.2016.4792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Virani SS, Alonso A, Aparicio HJ, et al. ; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2021 update: a report from the American Heart Association. Circulation. 2021;143(8):e254-e743. doi: 10.1161/CIR.0000000000000950 [DOI] [PubMed] [Google Scholar]
- 7.GBD 2017 US Neurological Disorders Collaborators . Burden of neurological disorders across the US from 1990-2017: a global burden of disease study. JAMA Neurol. 2021;78(2):165-176. doi: 10.1001/jamaneurol.2020.4152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ovbiagele B, Goldstein LB, Higashida RT, et al. ; American Heart Association Advocacy Coordinating Committee and Stroke Council . Forecasting the future of stroke in the United States: a policy statement from the American Heart Association and American Stroke Association. Stroke. 2013;44(8):2361-2375. doi: 10.1161/STR.0b013e31829734f2 [DOI] [PubMed] [Google Scholar]
- 9.Benesch C, Glance LG, Derdeyn CP, et al. ; American Heart Association Stroke Council; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Epidemiology and Prevention . Perioperative neurological evaluation and management to lower the risk of acute stroke in patients undergoing noncardiac, nonneurological surgery: a scientific statement from the American Heart Association/American Stroke Association. Circulation. 2021;143(19):e923-e946. doi: 10.1161/CIR.0000000000000968 [DOI] [PubMed] [Google Scholar]
- 10.Jørgensen ME, Torp-Pedersen C, Gislason GH, et al. Time elapsed after ischemic stroke and risk of adverse cardiovascular events and mortality following elective noncardiac surgery. JAMA. 2014;312(3):269-277. doi: 10.1001/jama.2014.8165 [DOI] [PubMed] [Google Scholar]
- 11.Andreasen C, Jørgensen ME, Gislason GH, et al. Association of timing of aortic valve replacement surgery after stroke with risk of recurrent stroke and mortality. JAMA Cardiol. 2018;3(6):506-513. doi: 10.1001/jamacardio.2018.0899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Christiansen MN, Andersson C, Gislason GH, et al. Risks of cardiovascular adverse events and death in patients with previous stroke undergoing emergency noncardiac, nonintracranial surgery: the importance of operative timing. Anesthesiology. 2017;127(1):9-19. doi: 10.1097/ALN.0000000000001685 [DOI] [PubMed] [Google Scholar]
- 13.Tikkanen R, Abrams MK. U.S. health care from a global perspective, 2019: higher spending, worse outcomes? The Commonwealth Fund. January 30, 2020. Accessed August 13, 2021.https://www.commonwealthfund.org/publications/issue-briefs/2020/jan/us-health-care-global-perspective-2019
- 14.Clinical Classifications Software (CCS) for ICD-9-CM. Agency for Healthcare Research and Quality. Updated March 6, 2017. Accessed April 1, 2021. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp
- 15.Clinical Classifications Software (CCS) for ICD-10-PCS (beta version). Agency for Healthcare Research and Quality. Updated November 5, 2019. Accessed April 1, 2021. https://www.hcup-us.ahrq.gov/toolssoftware/ccs10/ccs10.jsp
- 16.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130-1139. doi: 10.1097/01.mlr.0000182534.19832.83 [DOI] [PubMed] [Google Scholar]
- 17.Stagg VS. Elixhauser: Stata module to calculate Elixhauser index of comorbidity. Boston College Department of Economics. 2015. Accessed April 1, 2021. https://ideas.repec.org/c/boc/bocode/s458077.html
- 18.Krumholz HM, Coppi AC, Warner F, et al. Comparative effectiveness of new approaches to improve mortality risk models from Medicare claims data. JAMA Netw Open. 2019;2(7):e197314. doi: 10.1001/jamanetworkopen.2019.7314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCormick N, Bhole V, Lacaille D, Avina-Zubieta JA. Validity of diagnostic codes for acute stroke in administrative databases: a systematic review. PLoS One. 2015;10(8):e0135834. doi: 10.1371/journal.pone.0135834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Poldermans D, Bax JJ, Boersma E, et al. ; Task Force for Preoperative Cardiac Risk Assessment and Perioperative Cardiac Management in Non-cardiac Surgery; European Society of Cardiology (ESC) . Guidelines for pre-operative cardiac risk assessment and perioperative cardiac management in non-cardiac surgery. Eur Heart J. 2009;30(22):2769-2812. doi: 10.1093/eurheartj/ehp337 [DOI] [PubMed] [Google Scholar]
- 21.Peden CJ, Miller TR, Deiner SG, Eckenhoff RG, Fleisher LA; Members of the Perioperative Brain Health Expert Panel . Improving perioperative brain health: an expert consensus review of key actions for the perioperative care team. Br J Anaesth. 2021;126(2):423-432. doi: 10.1016/j.bja.2020.10.037 [DOI] [PubMed] [Google Scholar]
- 22.Vacas S, Cole DJ, Cannesson M. Cognitive decline associated with anesthesia and surgery in older patients. JAMA. 2021. 2021;326(9):863-864. doi: 10.1001/jama.2021.4773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peden CJ, Ghaferi AA, Vetter TR, Kain ZN. Perioperative health services research: far better played as a team sport. Anesth Analg. 2021;133(2):553-557. doi: 10.1213/ANE.0000000000005590 [DOI] [PubMed] [Google Scholar]
- 24.Mrkobrada M, Hill MD, Chan MTV, et al. Covert stroke after non-cardiac surgery: a prospective cohort study. Br J Anaesth. 2016;117(2):191-197. doi: 10.1093/bja/aew179 [DOI] [PubMed] [Google Scholar]
- 25.NeuroVISION Investigators . Perioperative covert stroke in patients undergoing non-cardiac surgery (NeuroVISION): a prospective cohort study. Lancet. 2019;394(10203):1022-1029. doi: 10.1016/S0140-6736(19)31795-7 [DOI] [PubMed] [Google Scholar]
- 26.Powers WJ. Time since stroke and risk of adverse outcomes after surgery. JAMA. 2014;312(18):1930. doi: 10.1001/jama.2014.13422 [DOI] [PubMed] [Google Scholar]
- 27.Jørgensen ME, Gislason GH, Andersson C. Time since stroke and risk of adverse outcomes after surgery—reply. JAMA. 2014;312(18):1930-1931. doi: 10.1001/jama.2014.13428 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Flow diagram describing selection of cases in the analytic cohort
eFigure 2. Temporal distribution of strokes after surgery
eFigure 3. Risk of major adverse events and discharge to skilled nursing facility stratified by time to previous stroke in patients undergoing total hip arthroplasties or total knee arthroplasties
eTable 1. Surgery mortality risk categories
eTable 2. Model coefficients for baseline analysis


