Abstract
Background and purpose
The influence of postoperative limping on patient satisfaction and amount of limping reduction following THA are not well documented. We (1) assessed if postoperative limping is associated with satisfaction 5 years after THA performed via the lateral or anterior approach; (2) evaluated the influence of surgical approach on amount of limping reduction following THA.
Patients and methods
We conducted a prospective cohort study of primary elective THAs performed in 2002–2013. Limping was assessed before and 5 years after surgery using the Harris Hip limping sub-score. Satisfaction was assessed at 5 years on a 5-point Likert scale. We compared proportions of satisfied patients among groups of limping. Evolution of limping before and after surgery was noted. Analyses were performed overall and stratified by pain and surgical approach. We used univariate and multivariate logbinomial regression models.
Results
1,257 patients were included (mean age 70 years). 81% had surgery via a lateral and 19% via an anterior approach. Before THA, 60% had moderate to severe limping and all reported pain. After THA, limping and pain improved; 9% of patients were dissatisfied. In multivariate analysis stratified on pain level, limping was associated with higher dissatisfaction. Similar results were obtained after lateral vs. anterior approach.
Interpretation
Postoperative limping impacts patient satisfaction after THA. The association varied by degree of limping and absence or presence of pain. It was independent of surgical approach. 5 years after THA occurrence of limping was largely reduced after both a lateral and an anterior approach, with low evidence of a greater reduction under an anterior approach.
Persistence of symptoms or occurrence of complications following total hip arthroplasty (THA) influences patient satisfaction, a complex subjective phenomenon influenced by several factors. The presence and severity of limping is one of them (1,2). Neuprez et al. found that the patient’s expectation to eliminate the preoperative limping thanks to the surgery was linked to satisfaction (3). Moreover, postoperative limping was associated with more unfulfilled expectations and could be a stigma of disability visible to all with an adverse psychological impact affecting patient satisfaction (3,4). Finally, limping could be related to the patient’s pain level impacting their level of mobility during daily life (4).
Several factors can cause postoperative limping: leg length discrepancy, nerve injury, weakness of the gluteal muscles, and surgical approach (5). Most common surgical approaches are posterior (PA), lateral (LA), and direct anterior approach (DAA) (6)—associated with different complication profiles (7-11). Limping has been among the first clinical signs of metal-on-metal prosthesis failure and may be used to monitor implant/provider performance (12-14). It has also been identified as a good predictor of postoperative patient-reported outcomes (15).
The impact of postoperative limping on patient satisfaction, pain, and function is sparsely documented. The main purpose of this study was thus to assess if limping 5 years after surgery is associated with patient satisfaction following primary elective THA performed through the DAA or LA. The secondary purpose was to evaluate the influence of surgical approach on the amount of limping following THA.
Patients and methods
Study design and setting
This study used a prospective register-based cohort from a large tertiary hospital. All patients undergoing primary elective THA for primary osteoarthritis (first hip only) between January 1, 2002 and December, 30, 2013 were eligible for the study. For main analyses we included all patients who had a complete preoperative and 5-year clinical follow-up assessment (Figure).
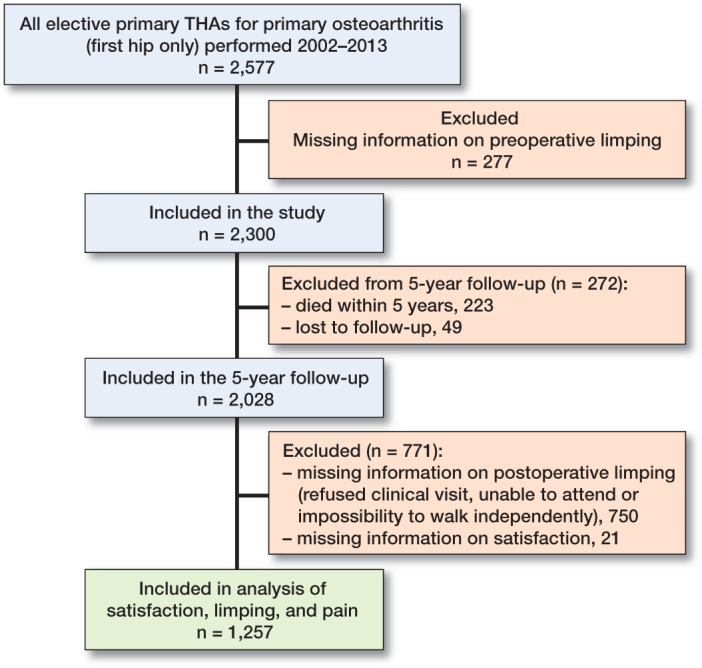
Flowchart for enrolment of the patient according to inclusion and exclusion criteria before, and five years after total hip arthroplasty (THA).
Outcomes
Main outcome was the satisfaction of the patients 5 years after THA. Patients were specifically asked by questionnaire, “Are you satisfied with the result of your hip surgery?” Response categories were: dissatisfied (1), somewhat dissatisfied (2), somewhat satisfied (3), satisfied (4), or very satisfied (5).
The main variables of interest were limping and pain, which were physician-assessed before and 5 years after THA. Limping was evaluated using the corresponding item from the Harris Hip Score (HHS categories: none, slight, moderate, and severe) (16). Pain was evaluated using the HHS pain sub-score (categories no pain, occasional, mild, moderate, and severe or extremely severe pain).
Other data collection
All data was extracted from the Geneva Arthroplasty Registry (17). Assessed baseline data was: age at surgery, sex, BMI, ASA score, Charnley disability grade (grade A, B, C) (18), diabetes, hypertension, ischemic cardiac disease, smoking status, diagnosis, type of fixation (uncemented, hybrid, cemented), and surgical approach used (lateral vs. anterior approach), and duration of the hip symptoms. Variables assessed 5 years after surgery consisted of: hip abductor strength using the Medical Research Council Manual Muscle Testing scale (MMT) evaluated by the surgeon (scored using a M0 [No muscle activation] to M5 [Muscle activation against examiner’s full resistance, full range of motion]) (19), leg-length discrepancy in centimeters evaluated by the surgeon, and the use of cane or walking aid evaluated with the HHS assistance sub-score (categories: none, cane for long distance, cane most of the time, one crutch, two crutches, two crutches, or incapacity to walk).
Statistics
Patient characteristics and clinical outcomes (satisfaction, limping, hip pain) were described as mean (SD) for quantitative variables and counts and percentages for qualitative variables.
The primary objective was to assess if limping 5 years postoperative was associated with patient satisfaction 5 years after THA. To address this issue, reported patient satisfaction was dichotomized into either reporting a higher level of satisfaction (including “very satisfied,” “satisfied”) labelled “satisfied” or reporting a poor or medium level of satisfaction (including “somewhat satisfied,” “somewhat dissatisfied,” “dissatisfied”) labelled “dissatisfied.” Proportions of satisfied patients were then compared among groups of limping (none vs. slight vs. moderate to severe) using univariate and multivariate logbinomial regression models. In the multivariate model, limping effect was adjusted for sex, age (≥ 70 vs. < 70) and BMI (≥ 30 vs. < 30). Analyses were stratified by pain level (none, slight/occasional, moderate/severe). A similar analysis was also performed in subgroups of surgical approach (LA vs. DAA) as a sensitivity analysis without stratifying for pain level.
The secondary objective was to compare the influence of surgical approach on limping 5 years after THA (none vs. slight to severe). Risk of limping was compared between the 2 groups (DAA vs. LA) using univariate and multivariate log-binomial regression models. In the multivariate model, surgery effect was adjusted for degree of preoperative limping, sex, age, and BMI. Whether preoperative duration of hip symptoms, postoperative pain, hip abductor strength (dichotomized in: ≥ M4–M5 vs. < M4), leg-length discrepancy (dichotomized in: none between –1 cm and +1 cm vs. > +1 cm or < –1 cm) and walking with cane (dichotomized in: no [none] vs. yes [cane for long distance, cane most of the time, 1 crutch, 2 crutches, 2 crutches, or incapacity to walk]) were associated with postoperative limping was evaluated with a chi-square test as post-hoc analyses.
Statistical significance was assessed at a 2-sided 0.05 level for all analyses. All analyses were performed using STATA software, version 13.1 (StataCorp LP, College Station, TX, USA).
Ethics, funding, data sharing, and potential conflicts of interest
The registry data collection was approved by the local ethics committee (CCER Geneva, no. PB_2017-00164, Switzerland). All the data used in this study is retrieved from the Geneva Arthroplasty Registry. The patient consent for data collection was obtained and protected in the registry. Institutional financial support was received for the registry from the “Fondation pour la recherche ostéoarticulaire.” Interested researchers may request access to data from DH. None of the authors report any conflict of interest.
Results
Study population (Table 1 and Supplementary data)
Table 1. Baseline characteristics of patients undergoing primary total hip arthroplasty (THA). Values are count (%) unless otherwise specified.
| Factor | Included patients n = 1,257 |
|---|---|
| Women | 765 (61) |
| Age at operation, mean (SD) | 70.5 (8.9) |
| BMI, mean (SD) | 27.3 (4.8) |
| ASA score | |
| 1–2 | 1,037 (83) |
| 3–4 | 220 (17) |
| Comorbidities | |
| Diabetes | 117 (9) |
| Hypertension | 652 (52) |
| Ischemic cardiac disease | 94 (7) |
| Smoking status | |
| Never | 825 (67) |
| Former | 206 (16) |
| Current | 191 (15) |
| Unknown | 35 (2) |
| Charnley disability grade | |
| A | 399 (33) |
| B | 430 (32) |
| C | 405 (35) |
| Missing | 23 |
| Surgical approach | |
| Lateral | 1,023 (81) |
| Anterior | 234 (19) |
| Type of fixation | |
| Hybrid THA | 872 (69) |
| Uncemented THA | 355 (28) |
| Cemented THA | 30 (3) |
Between 2002 and 2013, 2,577 patients had undergone an elective primary THA for primary osteoarthritis (first hip) in our center, of whom a 5-year follow-up visit has been obtained in 1,257 patients (Figure). Patients excluded from the analysis did not differ substantially from those who were included except for a slightly higher age and ASA scores, which is consistent with the fact that for inclusion they had to survive until the 5-year clinical visit (Table 1 and Supplementary data). Briefly, patients included in the study were female (61%), and mean age was 70.5 years (SD 8.9) with a BMI of 27.3 (SD 4.8) (Table 1). Surgery was performed via LA (81%) or DAA (19%). The orthopedic rehabilitation scheme was the same for all patients. It consisted of early mobilization on day 1 after surgery (walking with crutches) supervised by a physiotherapist followed by daily sessions with the physiotherapist on how to walk with canes, go up and down stairs, and pick up an object from the ground.
HHS, limping, and pain before and 5 years after surgery
Before undergoing THA, mean HHS was 51 (SD 15), 747 patients (60%) had moderate to severe limping and all suffered some pain, with about 2 expressing severe or extremely severe pain (Table 2). 5 years after THA, HHS, limping, and pain improved. Mean HHS increased to 89 (SD 14), 879 patients (70%) had no longer any limping, and 838 (67%) no longer suffered any pain. Among those with limping 5 years after THA, 78/127 patients (61%) reported some degree of pain, whereas among those without limping 341/1,130 patients reported pain (30%; p < 0.001).
Table 2. Degree of limping and pain and Harris hip score prior to and 5 years after THA (n = 1,257). Values are count (%) unless otherwise specified.
| Before surgery | 5 years after surgery | |
|---|---|---|
| Harris Hip Limping | ||
| None | 129 (10) | 879 (70) |
| Slight | 381 (30) | 251 (20) |
| Moderate | 550 (44) | 101 (8) |
| Severe | 197 (16) | 26 (2) |
| Hip pain | ||
| None | 0 (0) | 838 (67) |
| Occasional | 54 (4) | 265 (21) |
| Mild | 94 (7) | 72 (6) |
| Moderate | 540 (43) | 64 (5) |
| Severe or extremely severe | 569 (46) | 18 (1) |
| Harris hip score total, mean (SD) | 51 (15) | 89 (14) |
Impact of limping on patient satisfaction
Overall, 1,144 patients (91%) were satisfied with the result of their surgery while 113 (9%) reported a poor or medium level of satisfaction (dissatisfied patients) (Table 3). Limping was statistically significantly associated with dissatisfaction.
Table 3. Degree of postoperative limping and patient satisfaction 5 years after surgery. Values are count (%).
| All patients n = 1,257 | Satisfied n = 1,144 | Dissatisfied n = 113 | |
|---|---|---|---|
| Limping | |||
| None | 879 (70) | 844 (74) | 35 (31) |
| Slight | 251 (20) | 219 (19) | 32 (28) |
| Moderate | 101 (8) | 66 (6) | 35 (31) |
| Severe | 26 (2) | 15 (1) | 11 (10) |
The magnitude of the association varied by degree of limping and degree of pain (Table 4). Among patients without pain (n = 838), 23 were dissatisfied (2.7%) and the presence of slight and of moderate to severe limping was associated with dissatisfaction (adjusted RRslight = 5.3, 95% CI 1.8–16 and adjusted RRmoderate to severe = 18, CI 6.9–46). In patients with concomitant slight or occasional pain (n = 337), 49 patients were dissatisfied (15%), and the presence of slight and of moderate to severe limping was associated with dissatisfaction (adjusted RRslight = 1.2, CI 0.7–2.4 and adjusted RRmoderate to severe = 3.6, CI 2.0–6.5). In patients with concomitant moderate or severe pain (n = 82), 41 patients were dissatisfied and the presence of slight and of moderate to severe limping was associated with dissatisfaction (adjusted RRslight = 2.1, CI 1.1–3.8 and adjusted RRmoderate to severe = 2.0, CI 1.2–3.3). The magnitude of the influence of limping on dissatisfaction decreased with increasing pain level.
Table 4. Influence of postoperative limping on patient satisfaction 5 years after surgery, stratified by pain level.
| 5 years after surgery | All patients | Satisfied n = 1,144 | Dissatisfied n = 113 | Crude RR (CI) | Adjusted c RR ( CI ) |
|---|---|---|---|---|---|
| n (%) a | n (%) b | n (%) b | |||
| No pain | 838 | 815 | 23 | ||
| No limping | 661 (79) | 654 (99) | 7 (1) | 1 | 1 |
| Slight limping | 117 (14) | 111 (95) | 6 (5) | 4.8 (1.7–14) | 5.4 (1.8–16) |
| Moderate/severe limping | 60 (7) | 50 (83) | 10 (14) | 16 (6.2–40) | 18 (6.9–46) |
| Slight/occasional pain | 337 | 288 | 49 | ||
| No limping | 194 (58) | 174 (90) | 20 (10) | 1 | 1 |
| Slight limping | 108 (32) | 93 (86) | 15 (14) | 1.3 (0.7–2.5) | 1.3 (0.7–2.4) |
| Moderate/severe limping | 35 (10) | 21 (60) | 14 (40) | 3.9 (2.2–6.9) | 3.6 (2.0–6.5) |
| Moderate/severe pain | 82 | 41 | 41 | ||
| No limping | 24 (29) | 16 (67) | 8 (33) | 1 | 1 |
| Slight limping | 26 (32) | 15 (58) | 11 (42) | 1.3 (0.6–2.6) | 2.1 (1.1–3.8) |
| Moderate/severe limping | 32 (39) | 10 (31) | 22 (69) | 1.1 (0.6–2.1) | 2.0 (1.2–3.3) |
RR = Risk ratio; CI = 95% confidence intervals
Column percentages.
Row percentages.
Adjusted for age, sex, BMI.
The association between postoperative limping and patient satisfaction was similar in patients operated on with the lateral and the anterior approach in the adjusted analyses (Table C, see Supplementary data).
Impact of surgical approach on limping 5 years after surgery
Overall, patients of both groups (LA vs. DAA) shared similar characteristics, except for their mean age (71 vs. 69 years) and a higher proportion of Charnley B in the lateral approach group (37% vs. 26%). 5 years after THA, satisfaction and pain were similar in both groups, but the risk of postoperative limping was 30% higher (RR = 1.3, CI 1.0–1.6) with the lateral approach. In multivariable analysis, this decreased slightly and the confidence interval included 1 (adjusted RR = 1.2, 0.98–1.6), (Table 2, Supplementary data, and Table 5).
Table 5. Influence of surgical approach on limping 5 years after THA.
| 5 years after surgery | All patients | Postoperative limping | Crude RR (CI) | Adjusted c RR (CI) | |
|---|---|---|---|---|---|
| no n = 1,144 | Yes n = 113 | ||||
| n (%) a | n (%) b | n (%) b | |||
| Surgery approach | 1,257 | 879 (70) | 378 (30) | ||
| Anterior | 234 (19) | 177 (76) | 57 (24) | 1 | 1 |
| Lateral | 1023 (81) | 702 (69) | 321 (31) | 1.3 (1.0–1.6) | 1.2 (0.9–1.6) |
Footnotes: see Table 4.
Impact of preoperative duration of symptoms, postoperative pain, hip abductor strength, and leg length discrepancy on limping 5 years after surgery
5 years after THA, limping was associated with higher pain, lower hip abductor strength, greater leg length discrepancy, and walking with cane. No association was found between postoperative limping and duration of hip symptoms before THA (Table 6).
Table 6. Duration of hip symptoms prior to THA and postoperative hip pain, hip abductor strength, leg length discrepancy, and walking with cane or not, according to postoperative limping. Values are count (%).
| Factor | All | Postoperative limping | p-value | |
|---|---|---|---|---|
| none to slight n = 1,130 | Moderate to severe n = 127 | |||
| At baseline | ||||
| Duration of hip symptoms | 0.4 | |||
| < 1 year | 224 | 199 (19) | 25 (21) | |
| 1–2 years | 429 | 394 (37) | 35 (29) | |
| 2–5 years | 343 | 303 (28) | 40 (33) | |
| > 5 years | 193 | 173 (16) | 20 (17) | |
| Missing | 68 | 61 | 7 | |
| 5 years after surgery | ||||
| Hip pain | < 0.001 | |||
| None/occasional | 838 | 778 (69) | 60 (47) | |
| Mild/moderate | 337 | 302 (27) | 35 (28) | |
| Severe/extreme | 82 | 50 (4) | 32 (25) | |
| Missing | 0 | 0 | 0 | |
| Hip abductor strength | < 0.001 | |||
| ≥ M4–M5 | 988 | 906 (96) | 82 (85) | |
| < M4 | 48 | 34 (7) | 14 (15) | |
| Missing | 221 | 190 | 31 | |
| Leg length discrepancy | 0.009 | |||
| None | 785 | 720 (80) | 65 (68) | |
| > 1 cm or < –1 cm | 211 | 181 (20) | 30 (32) | |
| Missing | 261 | 229 | 32 | |
| Walking with cane | < 0.001 | |||
| No | 1,158 | 1,059 (94) | 99 (78) | |
| Yes | 97 | 69 (6) | 28 (22) | |
| Missing | 2 | 2 | 0 | |
Discussion
Our study shows a negative influence of postoperative limping on patient satisfaction in patients with and without pain. The influence of limping on dissatisfaction decreased with increasing pain level. The association between limping and satisfaction 5 years postoperatively was independent of surgical approach. Moreover, 5 years after THA the occurrence of limping was largely reduced after both lateral and anterior surgical approaches. The latter led to a greater reduction in limping occurrence.
We observed that 30% of patients presented limping to any degree after primary elective THA. Mancuso et al. (4) in a prospective cohort study of 487 patients found a similar proportion (31%) 4 years after THA. Limping was assessed by telephone interview. The authors reported that patients with limping had more unfulfilled expectations. This is in accordance with our finding that patients with postoperative limping were more dissatisfied than those without. The presence of pain postoperatively is a well-known important contributor to dissatisfaction after THA (20). This was also the case in our cohort. Because limping and pain are intertwined, we evaluated the relationship between limping and satisfaction by level of pain. In those without pain the presence of limping led to substantially greater dissatisfaction, which hints at a direct association.
Another important finding of this study concerns the influence of the surgical approach on the presence of limping 5 years after surgery. Postoperative limping was more frequent after the lateral approach compared with the anterior approach (any degree 31% vs. 24%; moderate to severe 11% vs. 5%). This is in accordance with Amlie et al. (21) who conducted a cross-sectional study (survey) 1–3 years after primary THA to evaluate the influence of surgical approach on patient-reported outcomes and complications, among them patient-reported limping. 25% of their patients operated on via a lateral approach reported limping compared with 12% and 13% after an anterior and posterolateral approach (21,22). This difference may be due to the surgical technique itself, with a greater potential for muscle damage with the lateral approach (21,23-25). In general, postoperative limping may be caused by trochanter pain, unequal lower limb length, lack of offset restoration or/and nerve injury, or insufficiency of the gluteal muscle (26,27). Nevertheless, the association between limping and satisfaction was similar for both surgical approaches.
Weakness of the hip muscles can result in abnormal gait patterns and functional disability with lateral bending of the trunk. Nankaku et al. hypothesized that the preoperative gluteus medius muscle atrophy, rather than hip abductor strength, was the best predictor of postoperative limping in the frontal plane after THA (28). In accordance with these results, we observed that some patients with limping 5 years after surgery had weaker hip abductor strength and/or presence of leg length discrepancy. These 2 factors may be related to the presence of limping and may therefore influence gait abilities and functionalities. Weakness of the hip abductor muscles may be a direct cause of Trendelenburg gait (29) and leg-length discrepancy is known to have an effect on the gait asymmetry, lower back pain, and joint compensations with an increase in oxygen consumption due to these gait impairments (30). The previously mentioned factors are important to co-evaluate, and an understanding of the etiology of the limping is essential to manage and prevent it.
To our knowledge this is the largest prospective cohort study of THA patients in whom limping was assessed before and 5 years after surgery. Limping is so far sparsely documented in large cohort/registry-based studies, which most often rely on patient-reported outcome measures (PROM) to evaluate postoperative symptoms, and in most of the currently used PROMs (exception Oxford Hip Score) limping is not included. Even if collected, the individual item results of PROMs are rarely presented.
Our study has limitations. First, only 50% of the patients who were eligible have been included in this study, therefore our results might not be generalizable to the entire population of patients presenting for THA. The second limitation was that our study included a smaller number of patients with an anterior compared with a lateral surgical approach. This is due to the fact that the lateral approach has been used since 2002 whereas the anterior approach was introduced in 2008. Third, no objective information was available concerning the gait functionality of these patients before and after THA, including quantitative measurements such as trunk movement, range of motion of the lower limb joints during gait, or measurement of the hip and knee muscle forces before and after THA. However, limping was physician-assessed and not patient-reported. Fourth, patients were operated upon by multiple orthopedic surgeons, reflecting the clinical practice of a University Hospital with a large number of surgeries, and different types of prosthesis, techniques, and surgeon experience levels. And finally, the number of patients in the subgroup with postoperative limping and absence of pain was small, leading to large confidence intervals.
In conclusion, our findings indicate that the presence of limping after THA contributes to patient dissatisfaction. The strength of the association varies by severity of limping and absence or presence of concomitant pain.
CB and AL retrieved the data. AL, ABM, and AP contributed to the statistical analyses. ABM, AP, and AL wrote the initial manuscript, and all authors critically revised the manuscript.
The authors would like to thank all Geneva Arthroplasty Registry staff for their continuous work and effort to keep updated the registry. They would also like to thank all the surgeons and patients who have contributed to the registry.
Acta thanks Marketta Henriksson for help with peer review of this study.
Supplementary data
Supplementary Table A.
Baseline characteristics prior to total hip arthroplasty (THA) according to patient eligibility. Values are count (%) unless otherwise specified
| Eligible n = 2,577 | Included n = 1 257 | Excluded n = 1320 | |
|---|---|---|---|
| Women | 1,531 (59) | 765 (61) | 766 (58) |
| Age at operation, mean (SD) | 71.2 (9.6) | 70.5 (8.9) | 71.8 (10) |
| BMI, mean (SD) ASA score | 27.2 (4.8) | 27.3 (4.8) | 27.1 (4.9) |
| 1–2 | 2,038 (79) | 1,037 (83) | 1,001 (76) |
| 3–4 | 539 (21) | 220 (17) | 319 (24) |
| Co-morbidities | |||
| Diabetes | 265 (10) | 117 (9) | 148 (11) |
| Hypertension | 1,408 (55) | 652 (52) | 756 (57) |
| Ischemic heart disease | 218 (8) | 94 (7) | 124 (9) |
| Smoking status | |||
| Never | 1,640 (64) | 825 (67) | 815 (62) |
| Former | 463 (17) | 206 (16) | 257 (19) |
| Current | 401 (16) | 191 (15) | 210 (16) |
| Unknown | 73 (3) | 35 (2) | 38 (3) |
| Charnley disability grade | |||
| A | 829 (33) | 399 (33) | 430 (34) |
| B | 803 (32) | 430 (32) | 373 (30) |
| C | 866 (35) | 405 (35) | 461 (36) |
| Missing | 79 | 23 | 56 |
| Surgical approach | |||
| Lateral | 1,951 (77) | 1,023 (81) | 928 (73) |
| Anterior | 570 (23) | 234 (19) | 336 (27) |
| Other | 56 | 56 | |
| Surgical intervention | |||
| Hybrid THA | 1,747 (68) | 872 (69) | 875 (66) |
| Uncemented THA | 753 (29) | 355 (28) | 396 (30) |
| Cemented THA | 77 (3) | 30 (3) | 47 (4) |
Supplementary Table B.
Satisfaction, limping, pain and Harris Hip Score prior to and 5 years after total hip arthroplasty (THA) by surgical approach (N = 1,257). Values are count (%) unless otherwise specified
| Preoperative | Postoperative | |||
|---|---|---|---|---|
| lateral approach | anterior approach | lateral approach | anterior approach | |
| Satisfaction | ||||
| Very satisfied | – | – | 744 (73) | 168 (72) |
| Satisfied | – | – | 188 (18) | 44 (19) |
| Somewhat satisfied | – | – | 65 (6) | 19 (8) |
| Somewhat dissatisfied | – | – | 21 (2) | 2 (0.8) |
| Dissatisfied | – | – | 5 (1) | 1 (0.2) |
| Harris Hip Limping | 1,023 (81) | 234 (19) | 1,023 (81) | 234 (19) |
| None | 79 (8) | 50 (21) | 702 (69) | 177 (76) |
| Slight | 315 (31) | 66 (29) | 206 (20) | 45 (19) |
| Moderate | 470 (46) | 80 (34) | 90 (9) | 11 (4.5) |
| Severe | 159 (15) | 38 (16) | 25 (2) | 1 (0.5) |
| Hip pain | ||||
| No pain | 0 (0) | 0 (0) | 688 (67) | 150 (64) |
| Pain (any level) | 1,023 (100) | 234 (100) | 335 (33) | 84 (36) |
| Harris Hip score | ||||
| total, mean (SD) | 51 (15) | 51 (15) | 88 (14) | 91 (13) |
Supplementary Table C. Limping and patient satisfaction 5 years after THA using the lateral approach.
| 5 years after surgery | All patients | Satisfied n = 1,144 | Dissatisfied n = 113 | Crude RR (CI) | Adjusted c RR ( CI ) |
|---|---|---|---|---|---|
| n (%) a | n (%) b | n (%) b | |||
| Lateral approach | |||||
| Limping | 1,023 | 932 (91) | 91 (9) | ||
| None | 702 (70) | 678 (96) | 24 (4) | 1 | 1 |
| Slight | 206 (20) | 180 (87) | 26 (13) | 3.7 (2.2–6.3) | 3.5 (2.1–6.0) |
| Moderate/severe | 115 (10) | 74 (64) | 41 (36) | 10 (6.6–17) | 10 (6.3– 16) |
| Anterior approach | |||||
| Limping | 234 | 212 (91) | 22 (9) | ||
| None | 177 (75) | 166 (96) | 11 (4) | 1 | 1 |
| Slight | 45 (19) | 39 (87) | 6 (13) | 2.2 (0.84–5.5) | 2.7 (1.1–6.7) |
| Moderate/severe | 12 (6) | 7 (58) | 5 (42) | 6.7 (2.8–16) | 11 (5.1–25) |
RR = Risk ratio; CI = 95% confidence intervals
Column percentages.
Row percentages.
Adjusted for age, sex, BMI.
References
- 1.Roder C, Vogel R, Burri L, Dietrich D, Staub L P. Total hip arthroplasty: leg length inequality impairs functional outcomes and patient satisfaction. BMC Musculoskelet Disord 2012; 13: 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kahlenberg C A, Nwachukwu B U, Schairer W W, Steinhaus M E, Cross M B. Patient satisfaction reporting after total hip arthroplasty: a systematic review. Orthopedics 2017; 40(3): e400-e4. [DOI] [PubMed] [Google Scholar]
- 3.Neuprez A, Delcour J P, Fatemi F, Gillet P, Crielaard J M, Bruyere O, et al. Patients’ expectations impact their satisfaction following total hip or knee arthroplasty. PloS One 2016; 11(12): e0167911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mancuso C A, Jout J, Salvati E A, Sculco T P. Fulfillment of patients’ expectations for total hip arthroplasty. J Bone Joint Surg Am 2009; 91(9): 2073-8. [DOI] [PubMed] [Google Scholar]
- 5.Horstmann T, Listringhaus R, Brauner T, Grau S, Mundermann A. Minimizing preoperative and postoperative limping in patients after total hip arthroplasty: relevance of hip muscle strength and endurance. Am J Phys Med Rehabil 2013; 92(12): 1060-9. [DOI] [PubMed] [Google Scholar]
- 6.Palan J, Beard D J, Murray D W, Andrew J G, Nolan J. Which approach for total hip arthroplasty: anterolateral or posterior? Clin Orthop Relat Res 2009; 467(2): 473-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berstock J R, Blom A W, Beswick A D. A systematic review and metaanalysis of complications following the posterior and lateral surgical approaches to total hip arthroplasty. Ann R Coll Surg Engl 2015; 97(1): 11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pincus D, Jenkinson R, Paterson M, Leroux T, Ravi B. association between surgical approach and major surgical complications in patients undergoing total hip arthroplasty. JAMA 2020; 323(11): 1070-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenlund S, Broeng L, Holsgaard-Larsen A, Jensen C, Overgaard S. Patient-reported outcome after total hip arthroplasty: comparison between lateral and posterior approach. Acta Orthop 2017; 88(3): 239-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flevas D A, Tsantes A G, Mavrogenis A F. Direct anterior approach total hip arthroplasty revisited. JBJS Rev 2020; 8(4): e0144. [DOI] [PubMed] [Google Scholar]
- 11.Hoskins W, Bingham R, Lorimer M, Hatton A, de Steiger R N. Early rate of revision of total hip arthroplasty related to surgical approach: an analysis of 122,345 primary total hip arthroplasties. J Bone Joint Surg Am 2020; 102(21): 1874-82. [DOI] [PubMed] [Google Scholar]
- 12.Berber R, Khoo M, Cook E, Guppy A, Hua J, Miles J, et al. Muscle atrophy and metal-on-metal hip implants: a serial MRI study of 74 hips. Acta Orthop 2015; 86(3): 351-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matharu G S, Berryman F, Dunlop D J, Judge A, Murray D W, Pandit H G. Has the threshold for revision surgery for adverse reactions to metal debris changed in metal-on-metal hip arthroplasty patients? A cohort study of 239 patients using an adapted risk-stratification algorithm. Acta Orthop 2019; 90(6): 530-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith A J, Dieppe P, Vernon K, Porter M, Blom A W, National Joint Registry of E, et al. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales. Lancet 2012; 379(9822): 1199-204. [DOI] [PubMed] [Google Scholar]
- 15.Huber M, Kurz C, Leidl R. Predicting patient-reported outcomes following hip and knee replacement surgery using supervised machine learning. BMC Med Inform Decis Mak 2019; 19(1): 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahomed N N, Arndt D C, McGrory B J, Harris W H. The Harris hip score: comparison of patient self-report with surgeon assessment. J Arthroplasty 2001; 16(5): 575-80. [DOI] [PubMed] [Google Scholar]
- 17.Lübbeke A, Silman A J, Barea C, Prieto-Alhambra D, Carr A J. Mapping existing hip and knee replacement registries in Europe. Health Policy 2018; 122(5): 548-57. [DOI] [PubMed] [Google Scholar]
- 18.Charnley J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg Br 1972; 54(1): 61-76. [PubMed] [Google Scholar]
- 19.Naqvi U, Sherman A. Muscle strength grading. Treasure Island, FL: StatPearls; 2022. [PubMed] [Google Scholar]
- 20.Okafor L, Chen A F. Patient satisfaction and total hip arthroplasty: a review. Arthroplasty 2019; 1(1): 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amlie E, Havelin L I, Furnes O, Baste V, Nordsletten L, Hovik O, et al. Worse patient-reported outcome after lateral approach than after anterior and posterolateral approach in primary hip arthroplasty: a crosssectional questionnaire study of 1,476 patients 1–3 years after surgery. Acta Orthop 2014; 85(5): 463-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Demos H A, Rorabeck C H, Bourne R B, MacDonald S J, McCalden R W. Instability in primary total hip arthroplasty with the direct lateral approach. Clin Orthop Relat Res 2001(393): 168-80. [DOI] [PubMed] [Google Scholar]
- 23.Pongcharoen B, Chaichubut K. Limping following primary total hip replacement: comparison of 3 surgical approaches. JB JS Open Access 2019; 4(2): e0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mjaaland K E, Kivle K, Svenningsen S, Nordsletten L. Do postoperative results differ in a randomized trial between a direct anterior and a direct lateral approach in THA? Clin Orthop Relat Res 2019; 477(1): 145-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Svensson O, Skold S, Blomgren G. Integrity of the gluteus medius after the transgluteal approach in total hip arthroplasty. J Arthroplasty 1990; 5(1): 57-60. [DOI] [PubMed] [Google Scholar]
- 26.Khan T, Knowles D. Damage to the superior gluteal nerve during the direct lateral approach to the hip: a cadaveric study. J Arthroplasty 2007; 22(8): 1198-200. [DOI] [PubMed] [Google Scholar]
- 27.Bahl J S, Nelson M J, Taylor M, Solomon L B, Arnold J B, Thewlis D. Biomechanical changes and recovery of gait function after total hip arthroplasty for osteoarthritis: a systematic review and meta-analysis. Osteoarthritis Cartilage 2018; 26(7): 847-63. [DOI] [PubMed] [Google Scholar]
- 28.Nankaku M, Ikeguchi R, Goto K, So K, Kuroda Y, Matsuda S. Hip external rotator exercise contributes to improving physical functions in the early stage after total hip arthroplasty using an anterolateral approach: a randomized controlled trial. Disabil Rehabil 2016; 38(22): 2178-83. [DOI] [PubMed] [Google Scholar]
- 29.Elbuluk A M, Coxe F R, Schimizzi G V, Ranawat A S, Bostrom M P, Sierra R J, et al. Abductor deficiency-induced recurrent instability after total hip arthroplasty. JBJS Rev 2020; 8(1): e0164. [DOI] [PubMed] [Google Scholar]
- 30.Chen G, Nie Y, Xie J, Cao G, Huang Q, Pei F. Gait analysis of leg length discrepancy-differentiated hip replacement patients with developmental dysplasia: a midterm follow-up. J Arthroplasty 2018; 33(5): 1437-41. [DOI] [PubMed] [Google Scholar]


