Abstract
Background:
The 2015 HIV outbreak in Indiana associated with prescription opioid injection coupled with rising rates of hepatitis C, especially in areas with long-standing opioid abuse, have raised concerns about prescription opioid injection. However, research on this topic is limited. We assessed trends in treatment admissions reporting injection, smoking, and inhalation abuse of prescription opioids and examined characteristics associated with non-oral routes of prescription opioid abuse in the U.S.
Methods:
Prescription opioid abuse treatment admissions in the 2004–2013 Treatment Episode Data Set were used to calculate counts and percentages of prescription opioid treatment admissions reporting oral, injection, or smoking/inhalation abuse overall, by sex, age, and race/ethnicity. Multivariable multinomial logistic regression was used to identify demographic and substance use characteristics associated with injection or smoking/inhalation abuse.
Results:
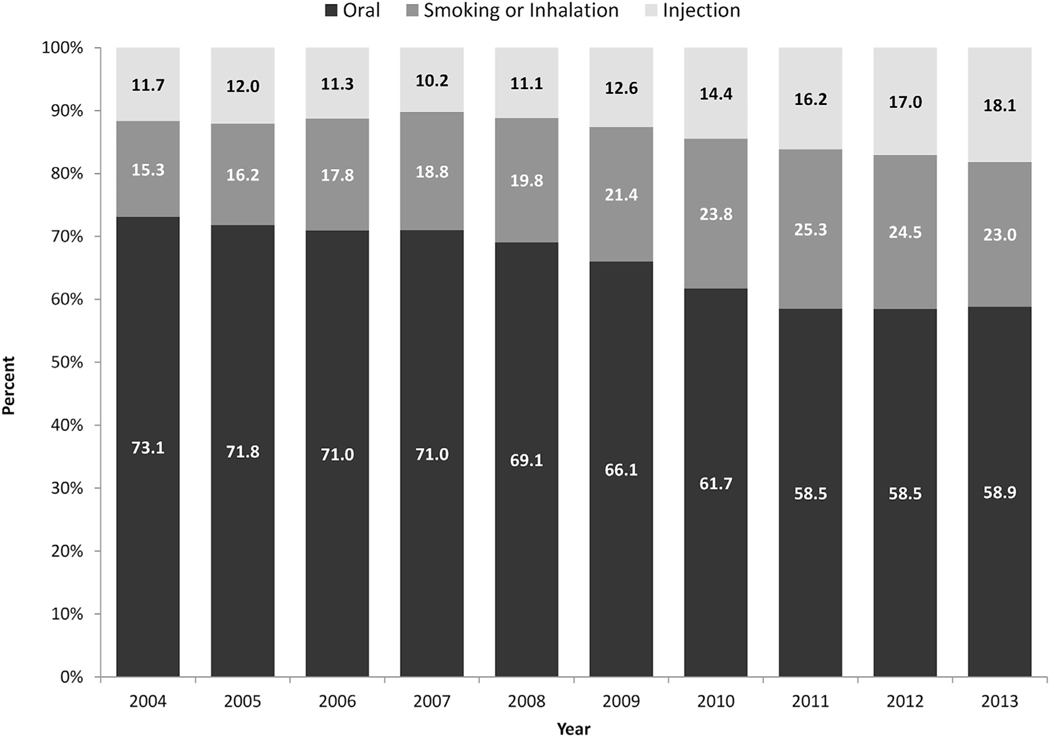
From 2004–2013, oral abuse decreased from 73.1% to 58.9%; injection abuse increased from 11.7% to 18.1%; and smoking/inhalation abuse increased from 15.3% of admissions to 23.0%. Among treatment admissions, the following were associated with injection abuse: male sex, 18–54 year-olds, non-Hispanic whites, non-Hispanic other, homeless or dependent living, less than full-time work, living in the Midwest or South, ≥1 prior treatment episodes, younger age of first opioid use, and reporting use of cocaine/crack, marijuana, heroin, or methamphetamine.
Conclusions:
The proportion of treatment admissions reporting prescription opioid injection and smoking/inhalation abuse increased significantly in the U.S. between 2004 and 2013. Expanding prevention efforts as well as access to medication-assisted treatment and risk reduction services for people who inject drugs is urgently needed.
Keywords: Prescription opioid, Injection, Abuse, Overdose
1. Introduction
The United States is in the midst of an epidemic of opioid-related morbidity and mortality (Paulozzi et al., 2011; Rudd et al., 2016; U.S. Department of Health and Human Services (DHHS), 2013). Prior research has found that non-oral routes of abuse such as inhaling, snorting, smoking, and injecting are common among different groups misusing prescription opioids (Black et al., 2013; Davis and Johnson, 2008; Havens et al., 2007; McCabe et al., 2007, 2009; Surratt et al., 2011; Young et al., 2010). Non-oral routes of abuse provide faster drug delivery and onset compared to oral use, thereby intensifying the reinforcing, euphoric effects of opioids and increasing vulnerability to addiction (Compton and Volkow, 2006; Katz, 2008). In addition, non-oral routes, especially injecting, are associated with greater severity of drug abuse and use disorder and increase the risk for overdose (Black et al., 2013; Katz, 2008; Surratt et al., 2011).
Research reflects that people who abuse opioids over time often move from less dangerous routes, such as oral abuse, to more dangerous routes, such as injection (Black et al., 2013). Multiple qualitative studies describe a trajectory from oral opioid abuse to inhalation or smoking and then injection of prescription opioids and in some cases concurrent or subsequent injection of heroin or other illicit opioids (Inciardi et al., 2009; Lankenau et al., 2012; Mars et al., 2014; Mateu-Gelabert et al., 2014; Peavy et al., 2012; Pollini et al., 2011). Injection may be the most dangerous route of abuse as it is associated with substantial health consequences, such as injection-related endocarditis, infectious disease transmission, increased risk for overdose, emergency department visits, and mortality (Black et al., 2013; Havens et al., 2007; Lankenau et al., 2015; Peters et al., 2016; Ronan and Herzig, 2016; Silva et al., 2013; Surratt et al., 2011; Young et al., 2010; Zibbell et al., 2014, 2015).
Importantly, the risk for certain negative health effects may be higher for prescription opioid injection compared to injection of other drugs. Studies have found that prescription opioid injection remains a risk factor for HCV even after accounting for injection of other drugs, including heroin. This increased risk is likely a result of factors such as the process of preparing the oral prescription opioid for injection (Lankenau et al., 2015; Zibbell et al., 2014). In addition, aspects of prescription opioid formulations, including other active and inactive ingredients such as talc can increase risk for injection-related skin complications and complications related to intranasal abuse (Katz et al., 2011; Lake and Kennedy, 2016; Roux et al., 2011; Roy et al., 2011; Vosler et al., 2014).
The recent outbreak of 181 HIV cases in Indiana associated with injection of the prescription opioid oxymorphone coupled with several years of rising rates of HCV, especially in areas with long-standing problems of prescription opioid abuse, have refocused concerns on prescription opioid injection (Peters et al., 2016; Suryaprasad et al., 2014; Zibbell et al., 2015). Despite these pressing concerns, there is limited data on the population of people misusing prescription opioids via non-oral routes in the U.S. In particular, there is a paucity of data on trends related to drug routes of abuse and the characteristics of those engaging in non-oral routes of abuse. Characterizing these populations and how they have changed over time, as well as identifying risk factors associated with non-oral routes of abuse, in particular injection abuse, are fundamental steps to informing targeted policy, programmatic initiatives, and future research efforts.
2. Materials and methods
2.1. Data source
Data are from the 19,009,159 treatment admissions reported in the 2004 through 2013 Treatment Episode Data Set (TEDS) public use files (Substance Abuse and Mental Health and Services Administrations (Substance Abuse and Mental Health Services Administration, 2016). TEDS, reported annually by the Substance Abuse and Mental Health Services Administration, provides demographic and substance use characteristics of substance use treatment admissions among people 12 years and older to state-licensed or certified substance abuse treatment centers that receive federal public funding. TEDS represents a compilation of data collected through the individual data collection systems of the state agencies for substance use treatment. The data are publically available and primarily include substance use and demographic measures (Substance Abuse and Mental Health Services Administration, 2015).
2.2. Substance use measures
TEDS captures data on the primary, secondary, and tertiary substances of abuse and the usual route of abuse for each substance among treatment admissions. This study focused on the 1,260,151 treatment admissions where the primary substance of abuse was prescription opioids (non-prescription methadone and other opiates and synthetic opioids not including heroin). Usual route of abuse for prescription opioids was recoded into three groups: 1) oral; 2) injection; and 3) smoking or inhalation (1.0% of admissions reported other non-oral/non-injection route of abuse and are included in this group). Additional substance use measures included: 1) the number of previous substance use treatment episodes (i.e., distinct previous treatment admissions): 0, 1, 2, or 3 or more; 2) self-reported age of first abuse of prescription opioid analgesics: 14 years old or younger, 15–17, 18–20, 21–24, 25–29, 30–39, or 40 years or older; and 3) other substances abused in additional to the primary substance reported at treatment admission: alcohol, cocaine or crack, marijuana, heroin, methamphetamine, and benzodiazepines.
2.3. Demographic measures
Demographic measures include: 1) sex: male or female; 2) age group: 12–17, 18–24, 25–34, 35–44, 45–54, or 55 and over; 3) race/ ethnicity: non-Hispanic white, non-Hispanic black, non-Hispanic other, or Hispanic; 4) living arrangement: independent living (living alone or with others without supervision), dependent living (living in a supervised setting such as a residential institution, halfway house or group home, and children under age 18 living with parents, relatives, or guardians or in foster care), or homeless (no fixed address, includes shelters); 5) employment status: full-time (working 35 h or more each week), part-time (working less than 35 h per week), unemployed (looking for work during the past 30 days or on layoff from job), or not in labor force (not looking for work during past 30 days or a student, homemaker, disabled, retired, or inmate of an institution); and 6) U.S. census region: Northeast, Midwest, South, or West.
2.4. Data analysis
First, annual number and percentage of prescription opioid abuse treatment admissions reporting oral, injection, and smoking or inhalation as the usual route of abuse were calculated overall, by sex, age group, and race/ethnicity group for 2004 through 2013. Second, the percentage of prescription opioid analgesic treatment admissions reporting injection as the usual route of abuse was calculated by U.S. census region for each year for 2004 through 2013.
Joinpoint regression (v 4.2.0.2) was used to assess trends for each of the percentages calculated above. Joinpoint assesses changes in trends by incorporating point estimates and their standard errors and tests a regression model using a Monte Carlo permutation method with no joinpoints (i.e., changes in trends occurring during the assessed time period) against alternative models to determine whether and where more joinpoints should be added (Kim et al., 2000). For this analysis, the trend over the full study time period overall and for demographic groups were examined. A p value of <0.05 was considered statistically significant.
Finally, a multivariable multinomial logistic regression was conducted to identify characteristics associated with injection or smoking or inhalation as the usual route of prescription opioid abuse compared to oral abuse. The demographic and substance use measures defined above were included in the model. Results are presented as adjusted relative risk ratios and associated 95% confidence intervals. Multicollinearity was assessed using variance inflation factors and was not identified in the final model. Data analyses were conducted with STATA version 14.0 (Stata Corp. College Station, TX).
3. Results
Treatment admissions for primary prescription opioid abuse increased from 58,125 in 2004–193,600 in 2011 and then declined to 153,870 in 2013. The number of treatment admissions reporting oral abuse as the usual route of opioid abuse increased from 42,489 in 2004–90,574 in 2013, a 113.2% increase; injection abuse increased 311.9% from 6774 admissions in 2004–27,903 in 2013; and smoking or inhalation abuse increased 299.4% from 8862 admissions in 2004–35,393 in 2013.
Fig. 1 presents the percentage of treatment admissions by usual route of abuse between 2004 and 2013. The percentage of admissions reporting injection abuse increased from 11.7% in 2004–18.1% in 2013–a 54.7% relative increase. For smoking or inhalation abuse, the percentage of primary prescription opioid abuse treatment admissions increased from 15.3% in 2004–23.0% in 2013–a 50.3% relative increase. In contrast to non-oral routes of abuse, the percentage of admissions reporting oral abuse declined from 73.1% in 2004–58.9% in 2013–a 19.4% decrease.
Fig. 1.
Routes of Abuse among Primary Prescription Opioid Abuse Treatment Admissions by Year, United States, 2004–2013.
3.1. Oral prescription opioid abuse by demographic characteristics
Table 1 reports the trends in the number and percent of primary opioid abuse treatment admissions by usual routes of abuse by sex, age group, and race/ethnicity. For males, oral abuse declined from 69.4% of treatment admissions in 2004–55.6% in 2013. Among females, the percentage declined from 77.3% to 62.5%. With the exception of treatment admissions among people aged 55 years or older, oral abuse declined across all other age groups, although the magnitude of the decline varied. The 55 year and older age group consistently had the highest percentage of treatment admissions reporting oral abuse as the usual route of abuse, ranging from 84.5% to 87.3% each year. Oral abuse was lowest among 18–24 year olds throughout the study period, ranging from 41.9% to 58.5% each year. Among race/ethnicity groups, non-Hispanic whites experienced the most consistent and sharpest decline in oral abuse, decreasing from 73.6% in 2004–57.3% in 2013, whereas oral abuse among non-Hispanic blacks increased from 72.2% in 2004–78.8% in 2013. The non-Hispanic other race/ethnicity group consistently had the lowest percentage of treatment admissions reporting oral abuse.
Table 1.
Routes of Abuse among Primary Prescription Opioid Abuse Treatment Admissions by Select Demographic Groups by Year, United States, 2004–2013.
| 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | |
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Overall | 58,125 | 69,939 | 83,411 | 98,792 | 122,613 | 144,272 | 166,474 | 193,600 | 169,055 | 153,870 |
| Usual Route of Abuse Oral | ||||||||||
| N (%) | 42,489 (73.1) | 50,209 (71.8) | 59,191 (71.0) | 70,148 (71.0) | 84,712 (69.1) | 95,297 (66.1) | 102,739 (61.7) | 113,307 (58.5) | 98,923 (58.5) | 90,574 (58.9)* |
| Sex | ||||||||||
| male | 21,235 (69.4) | 25,571 (68.4) | 30,308 (67.8) | 35,578 (67.7) | 42,432 (65.5) | 47,901 (62.3) | 51,689 (58.2) | 56,931 (55.4) | 49,235 (54.9) | 45,186 (55.6)* |
| female | 21,239 (77.3) | 24,626 (75.8) | 28,871 (74.6) | 34,555 (74.8) | 42,268 (73.2) | 47,387 (70.3) | 51,036 (65.8) | 56,359 (62.1) | 49,678 (62.6) | 45,376 (62.5)* |
| Age, years | ||||||||||
| 12–17 | 662 (63.1) | 799 (65.7) | 841 (62.2) | 1,039 (64.1) | 1,497 (62.3) | 1,740 (59.0) | 1,586 (54.3) | 1,528 (51.1) | 1,098 (50.4) | 811 (52.7) |
| 18–24 | 7,516 (58.0) | 9,688 (58.5) | 11,763 (57.8) | 14,448 (57.4) | 17,847 (55.9) | 20,376 (51.8) | 22,076 (47.1) | 22,255 (42.5) | 17,704 (41.9) | 14,174 (42.6)* |
| 25–34 | 13,531 (72.1) | 16,488 (70.3) | 20,306 (69.0) | 25,344 (69.7) | 32,453 (68.0) | 38,093 (65.8) | 42,402 (61.4) | 48,338 (58.0) | 42,895 (57.6) | 39,526 (56.6)* |
| 35–44 | 11,952 (80.6) | 12,821 (79.3) | 14,373 (79.6) | 15,866 (80.0) | 17,624 (78.2) | 18,835 (76.3) | 19,464 (72.7) | 21,747 (70.3) | 19,604 (69.1) | 19,184 (68.2)* |
| 45–54 | 7,318 (83.7) | 8,478 (82.7) | 9,685 (83.6) | 10,756 (84.6) | 11,968 (84.1) | 12,495 (83.2) | 12,902 (81.2) | 14,263 (79.8) | 12,617 (78.5) | 11,581 (77.5)* |
| 55 and older | 1,510 (85.3) | 1,935 (85.0) | 2,223 (84.5) | 2,695 (87.3) | 3,323 (87.2) | 3,758 (86.1) | 4,309 (86.5) | 5,176 (85.7) | 5,005 (86.2) | 5,298 (85.3) |
| Race/Ethnicity | ||||||||||
| Non-Hispanic White | 35,021 (73.6) | 40,970 (72.0) | 50,374 (71.1) | 65,505 (71.0) | 72,356 (68.8) | 80,287 (65.6) | 87,468 (61.1) | 95,262 (57.3) | 82,526 (57.1) | 74,155 (57.3)* |
| Non-Hispanic Black | 1,910 (72.2) | 2,079 (73.4) | 2,542 (76.0) | 2,898 (81.1) | 3,457 (82.2) | 4,069 (81.0) | 4,393 (79.8) | 5,868 (78.7) | 5,517 (78.6) | 5,742 (78.8)* |
| Non-Hispanic Other | 995 (61.8) | 1,245 (58.3) | 1,565 (61.8) | 1,987 (59.9) | 2,343 (59.5) | 2,806 (55.7) | 3,027 (53.8) | 3,439 (56.5) | 3,372 (54.3) | 3,408 (55.6)* |
| Hispanic | 1,474 (78.7) | 2,024 (78.0) | 2,592 (79.0) | 3,027 (80.3) | 3,938 (79.0) | 4,737 (75.4) | 5,432 (70.2) | 6,353 (67.8) | 6,313 (67.9) | 6,190 (68.9)* |
| Injection N (%) | 6,774 (11.7) | 8,422 (12.0) | 9,400 (11.3) | 10,094 (10.2) | 13,637 (11.1) | 18,164 (12.6) | 24,042 (14.4) | 31,264 (16.2) | 28,780 (17.0) | 27,903 (18.1)* |
| Sex | ||||||||||
| male | 3,922 (12.8) | 4,833 (12.9) | 5,417 (12.1) | 5,647 (10.8) | 7,808 (12.1) | 10,390 (13.5) | 13,653 (15.4) | 17,370 (16.9) | 16,079 (17.9) | 15,188 (18.7)* |
| female | 2,845 (10.4) | 3,587 (11.0) | 3,982 (10.3) | 4,440 (9.6) | 5,827 (10.1) | 7,772 (11.5) | 10,385 (13.4) | 13,889 (15.3) | 12,697 (16.0) | 12,714 (17.5)* |
| Age, years | ||||||||||
| 12–17 | 66 (6.3) | 73 (6.0) | 70 (5.2) | 68 (4.2) | 142 (5.9) | 228 (7.7) | 243 (8.3) | 265 (8.9) | 184 (8.5) | 120 (7.8) |
| 18–24 | 1,939 (15.0) | 2,403 (14.5) | 2,656 (13.1) | 3,084 (12.3) | 4,280 (13.4) | 6,102 (15.5) | 8,061 (17.2) | 10,236 (19.5) | 8,721 (20.7) | 7,454 (22.4)* |
| 25–34 | 2,457 (13.1) | 3,167 (13.5) | 3,789 (12.9) | 4,135 (11.4) | 5,791 (12.1) | 7,892 (13.6) | 10,820 (15.7) | 14,914 (17.9) | 14,068 (18.9) | 14,311 (20.5)* |
| 35–44 | 1,413 (9.5) | 1,706 (10.6) | 1,667 (9.2) | 1,724 (8.7) | 2,115 (9.4) | 2,514 (10.2) | 3,216 (12.0) | 3,894 (12.6) | 3,939 (13.9) | 4,110 (14.6)* |
| 45–54 | 816 (9.3) | 955 (9.3) | 1,015 (8.8) | 921 (7.3) | 1,081 (7.6) | 1,169 (7.8) | 1,382 (8.7) | 1,543 (8.6) | 1,542 (9.6) | 1,480 (9.9) |
| 55 and older | 83 (4.7) | 118 (5.2) | 203 (7.7) | 162 (5.3) | 228 (6.0) | 259 (5.9) | 320 (6.4) | 412 (6.8) | 326 (5.6) | 428 (6.9) |
| Race/Ethnicity | ||||||||||
| Non-Hispanic White | 5,662 (11.9) | 6,990 (12.3) | 8,153 (11.5) | 8,888 (10.4) | 12,002 (11.4) | 15,843 (13.0) | 21,182 (14.8) | 27,908 (16.8) | 25,866 (17.9) | 25,025 (19.3)* |
| Non-Hispanic Black | 195 (7.4) | 205 (7.2) | 271 (8.1) | 200 (5.6) | 237 (5.6) | 326 (6.5) | 360 (6.5) | 478 (6.4) | 449 (6.4) | 426 (6.1) |
| Non-Hispanic Other | 226 (14.0) | 280 (13.1) | 364 (14.4) | 423 (12.7) | 469 (11.9) | 653 (13.0) | 818 (14.5) | 904 (14.9) | 918 (14.8) | 940 (15.3) |
| Hispanic | 149 (8.0) | 230 (8.9) | 237 (7.2) | 254 (6.7) | 393 (7.9) | 600 (9.6) | 857 (11.1) | 1,148 (12.2) | 1,168 (12.6) | 1,056 (11.8) |
| Smoking or Inhalation N (%) | 8,862 (15.3) | 11,308 (62.0) | 14,820 (17.8) | 18,550 (18.8) | 24,264 (19.8) | 30,811 (21.4) | 39,693 (23.8) | 49,029 (25.3) | 41,352 (24.5) | 35,393 (23.0)* |
| Sex | ||||||||||
| male | 5,463 (17.8) | 7,006 (18.7) | 8,960 (20.1) | 11,314 (21.5) | 14,564 (22.5) | 18,581 (24.2) | 23,487 (26.4) | 28,540 (27.8) | 24,383 (27.2) | 20,856 (25.7)* |
| female | 3,396 (12.4) | 4,296 (13.2) | 5,857 (15.1) | 7,229 (15.6) | 9,689 (16.8) | 12,228 (18.2) | 16,200 (20.9) | 20,479 (22.6) | 16,962 (21.4) | 14,532 (20.0)* |
| Age, years | ||||||||||
| 12–17 | 322 (30.7) | 344 (28.3) | 442 (32.7) | 513 (31.7) | 765 (31.8) | 980 (33.2) | 1,094 (37.4) | 1,200 (40.1) | 895 (41.1) | 607 (39.5)* |
| 18–24 | 3,501 (27.0) | 4,474 (27.0) | 5,935 (29.2) | 7,628 (30.3) | 9,778 (30.7) | 12,837 (32.7) | 16,730 (35.7) | 19,916 (38.0) | 15,803 (37.4) | 11,632 (35.0)* |
| 25–34 | 2,787 (14.8) | 3,805 (16.2) | 5,335 (18.1) | 6,906 (19.0) | 9,484 (19.9) | 11,944 (20.6) | 15,828 (22.9) | 20,108 (24.1) | 17,438 (23.4) | 15,943 (22.9)* |
| 35–44 | 1,470 (9.9) | 1,643 (10.2) | 2,020 (11.2) | 2,240 (11.3) | 2,787 (12.4) | 3,350 (13.6) | 4,077 (15.2) | 5,277 (17.1) | 4,831 (17.0) | 4,843 (17.2)* |
| 45–54 | 605 (6.9) | 819 (8.0) | 883 (7.6) | 1,033 (8.1) | 1,189 (8.4) | 1,351 (9.0) | 1,611 (10.1) | 2,077 (11.6) | 1,908 (11.9) | 1,886 (12.6)* |
| 55 and older | 177 (10.0) | 223 (9.8) | 205 (7.8) | 230 (7.5) | 261 (6.9) | 349 (8.0) | 353 (7.1) | 451 (7.5) | 477 (8.2) | 482 (7.8) |
| Race/Ethnicity | ||||||||||
| Non-Hispanic White | 6,929 (14.6) | 8,906 (15.7) | 12,368 (17.5) | 15,886 (18.6) | 20,768 (19.8) | 26,223 (21.4) | 34,608 (24.2) | 43,015 (25.9) | 36,136 (25.0) | 30,315 (23.4)* |
| Non-Hispanic Black | 540 (20.4) | 549 (19.4) | 531 (15.9) | 477 (13.3) | 514 (12.2) | 626 (12.5) | 751 (13.6) | 1,106 (14.8) | 1,057 (15.1) | 1,049 (15.1)* |
| Non-Hispanic Other | 390 (24.2) | 612 (28.6) | 605 (23.9) | 909 (27.4) | 1,125 (28.6) | 1,576 (31.3) | 1,785 (31.7) | 1,740 (28.6) | 1,918 (30.9) | 1,781 (29.1)* |
| Hispanic | 250 (13.4) | 341 (13.1) | 451 (13.8) | 487 (12.9) | 651 (13.1) | 949 (15.1) | 1,444 (18.7) | 1,875 (20.0) | 1,819 (19.6) | 1,744 (19.4)* |
p value for trend is statistically significant at p < 0.05.
3.2. Injection prescription opioid abuse by demographic characteristics
The percentage of male treatment admissions reporting injection abuse of opioids fluctuated between 10.8% and 12.9% in 2004 through 2007 and then increased in each subsequent year to a high of 18.7% in 2013. Similarly, among females, the percentage ranged from 9.6% to 11.0% between 2004 and 2007 and then increased each year to a high of 17.5% in 2013. The 18–24 year old and 25–34 year old age groups experienced the most consistent increases in injection opioid abuse among treatment admissions, particularly after 2007. In 2013, 22.4% of primary opioid abuse treatment admissions among 18–24 year olds and 20.5% of admissions among 25–34 year olds reported injection as the usual route of abuse. Among race/ethnicity groups, non-Hispanic whites experienced the only significant increase in the percentage of treatment admissions reporting injection abuse, increasing from 11.9% in 2004–19.3% in 2013.
3.3. Smoking or inhalation prescription opioid abuse by demographic characteristics
Among prescription opioid abuse treatment admissions, increases in smoking or inhalation abuse occurred among males and females, people aged 12–17, 18–24, 25–34, 35–44, and 45–54 year olds, and non-Hispanic whites, Non-Hispanic other, and Hispanics. Smoking or inhalation abuse declined among non-Hispanic blacks.
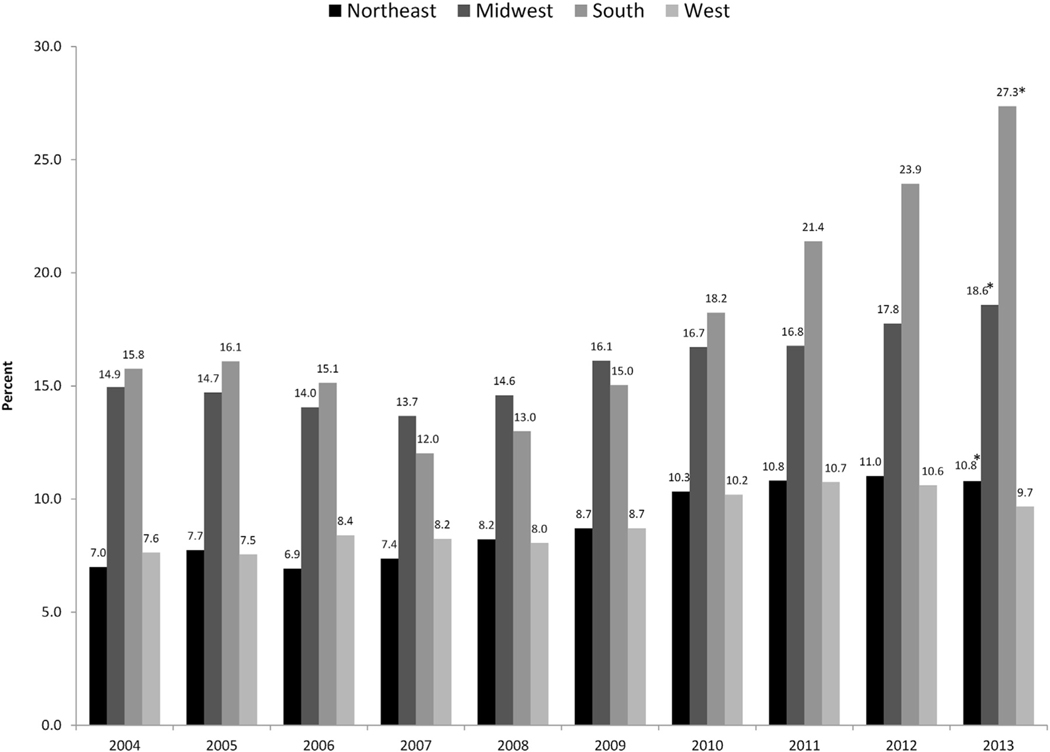
3.4. Injection abuse by U.S. census region
There was wide variation in the percentage of primary prescription opioid abuse treatment admissions reporting injection as the usual route of abuse across U.S. census regions (Fig. 2). The Northeast and West regions had the lowest percentage of treatment admissions reporting prescription opioid injection as the primary route of abuse. The percentage of admissions in the Midwest and South regions were similar in 2004 through 2008, however, after 2008, the percentage of admissions reporting injection of opioids as the usual route of abuse in the South increased substantially faster than in the Midwest region. In 2013, 27.3% of primary prescription opioid abuse treatment admission in the South reported injection as the usual route of abuse compared to 18.6% in the Midwest, 10.8% in the Northeast, and 9.7% in the West.
Fig. 2.
Injection as the Usual Route of Abuse among Primary Prescription Opioid Abuse Treatment Admissions by Census Region, United States, 2004–2013.
3.5. Multivariable multinomial logistic regression analysis
Table 2 provides the results from the multivariable multinomial logistic regression analysis. Relative risk for injection abuse among treatment admissions was greater between 2009 and 2013 compared to 2004, with the highest relative risk in 2013. Characteristics associated with increased relative risk of injection as the usual route of opioid abuse compared to oral abuse among treatment admissions included: being male, people age 18–54 years, non-Hispanic whites, non-Hispanic other, the homeless, dependent living, working less than full-time, living in the Midwest or South, having a prior substance abuse treatment episode, initiating opioid abuse at an earlier age, reporting cocaine or crack, marijuana, heroin, or methamphetamine use at treatment admission. In general, characteristics associated with smoking or inhalation abuse compared to oral abuse among treatment admissions were similar to those for injection abuse. Noted exceptions include increased relative risk among younger treatment admissions, treatment admissions in the Northeast, and treatment admissions reporting methamphetamine or benzodiazepine use at time of admission.
Table 2.
Multivariable Multinomial Logistic Regression Analysis Comparing Risk Factors for Injection or Smoking or Inhalation Abuse As Usual Route of Abuse Compared to Oral Abuse among Primary Prescription Opioid Abuse Treatment Admissions, United States, 2004–2013.
| Injection Abuse versus Oral Abuse | Smoking or Inhalation Abuse versus Oral Abuse | |
|---|---|---|
| Characteristic | Relative Risk Ratio (95% Confidence Interval) | Relative Risk Ratio (95% Confidence Interval) |
|
| ||
| Year | ||
| 2004 | Ref | Ref |
| 2005 | 0.96 (0.92–1.00) | 1.15 (1.10–1.19)* |
| 2006 | 0.92 (0.88–0.96)* | 1.26 (1.22–1.31)* |
| 2007 | 0.82 (0.79–0.86)* | 1.16 (1.12–1.20)* |
| 2008 | 0.90 (0.87–0.94)* | 1.22 (1.18–1.26)* |
| 2009 | 1.05 (1.01–1.09)* | 1.38 (1.34–1.43)* |
| 2010 | 1.26 (1.22–1.31)* | 1.65 (1.60–1.70)* |
| 2011 | 1.34 (1.30–1.39)* | 1.74 (1.69–1.80)* |
| 2012 | 1.45 (1.40–1.50)* | 1.74 (1.69–1.80)* |
| 2013 | 1.77 (1.71–1.83)* | 1.77 (1.72–1.83)* |
| Sex | ||
| Female | Ref | Ref |
| Male | 1.38 (1.36–1.40)* | 1.35 (1.34–1.37)* |
| Age, years | ||
| 12–17 | Ref | Ref |
| 18–24 | 2.85 (2.68–3.04)* | 1.00 (0.96–1.03) |
| 25–34 | 2.16 (2.03–2.30)* | 0.56 (0.54–0.58)* |
| 35–44 | 1.60 (1.50–1.71)* | 0.37 (0.36–0.39)* |
| 45–54 | 1.33 (1.24–1.42)* | 0.25 (0.24–0.27)* |
| 55 and over | 1.07 (0.98–1.15) | 0.20 (0.19–0.21)* |
| Race/Ethnicity | ||
| Hispanic | Ref | Ref |
| Non-Hispanic White | 1.44 (1.40–1.49)* | 1.41 (1.37–1.44)* |
| Non-Hispanic Black | 0.57 (0.54–0.60)* | 1.01 (0.98–1.05) |
| Non-Hispanic Other | 1.70 (1.62–1.77)* | 2.44 (2.36–2.53)* |
| Living Arrangement | ||
| Independent | Ref | Ref |
| Dependent | 1.27 (1.25–1.29)* | 1.05 (1.04–1.07)* |
| Homeless | 1.73 (1.69–1.77)* | 1.14 (1.12–1.17)* |
| Employment Status | ||
| Full-time employment | Ref | Ref |
| Part-time employment | 1.28 (1.24−1.32)* | 1.05 (1.03–1.08)* |
| Not in labor force | 1.37 (1.34–1.40)* | 0.92 (0.90–0.93)* |
| Unemployed | 1.69 (1.65–1.72)* | 1.07 (1.06–1.09)* |
| U.S. Census Region | ||
| Northeast | Ref | Ref |
| Midwest | 1.65 (1.62–1.68)* | 0.47 (0.46–0.48)* |
| South | 2.15 (2.12–2.19)* | 0.70 (0.69–0.70)* |
| West | 0.89 (0.87–0.91) | 0.52 (0.51–0.53)* |
| Number of Prior Substance Abuse Treatment Episodes | ||
| 0 | Ref | Ref |
| 1 | 1.18 (1.17–1.20)* | 1.04 (1.03–1.05)* |
| 2 | 1.44 (1.42–1.47)* | 1.06 (1.04–1.07)* |
| 3 or more | 1.79 (1.76–1.82)* | 1.02 (1.00–1.03)* |
| Age of First Use of Prescription Opioids, years | ||
| Less than 14 | Ref | Ref |
| 15–17 | 0.99 (0.96–1.01) | 1.07 (1.04–1.09)* |
| 18–20 | 0.85 (0.83–0.87)* | 1.05 (1.03–1.07)* |
| 21–24 | 0.74 (0.72–0.76)* | 0.97 (0.95–0.99)* |
| 25–29 | 0.65 (0.64–0.67)* | 0.86 (0.84–0.88)* |
| 30–39 | 0.58 (0.57–0.60)* | 0.79 (0.77–0.81)* |
| 40 and over | 0.44 (0.42–0.46)* | 0.72 (0.69–0.74)* |
| Substance Reported At Admission± | ||
| Alcohol | 0.87 (0.85–0.88)* | 0.92 (0.91–0.93)* |
| Cocaine or Crack | 1.71 (1.68–1.74)* | 1.29 (1.27–1.31)* |
| Marijuana | 1.09 (1.07–1.10)* | 1.27 (1.25–1.28)* |
| Heroin | 1.88 (1.84–1.92)* | 1.48 (1.46–1.51)* |
| Methamphetamine | 2.21 (2.15–2.26)* | 0.95 (0.92–0.98)* |
| Benzodiazepines | 0.98 (0.96–1.00)* | 1.02 (1.01–1.04)* |
4. Discussion
This study found large shifts from oral abuse of prescription opioids towards non-oral routes of abuse among admissions to substance use treatment between 2004 and 2013. The largest percentage change occurred among treatment admissions reporting injection as their usual route of prescription opioid abuse, increasing from 11.7% of primary prescription opioid abuse admissions in 2004–18.1% of admissions in 2013 – a 55% relative increase. Further, the absolute number of admissions reporting injection as the usual route of abuse increased more than 300% during the study period. These shifts portend continued increases in opioid injection-related harms in the U.S.
Among prescription opioid abuse treatment admissions, the significant increases in prescription opioid injection among those in the South along with increases among non-Hispanic white admissions, and admissions aged 18–34 years old parallel rising rates of HCV in the U.S.; HCV reports between 2006 and 2012 show the largest increases occurring east of the Mississippi River, particularly in states in central Appalachia heavily impacted by prescription opioid abuse, and often among non-Hispanic whites less than 30 years of age from more rural and suburban areas (Suryaprasad et al., 2014; Zibbell et al., 2015). In particular, the increases in non-oral routes of abuse among non-Hispanic white treatment admissions correspond with the substantial research documenting the disproportionate impact of the opioid epidemic on this population (U.S. Department of Health and Human Services, 2013; Paulozzi et al., 2011; Paulozzi, 2012; Rudd et al., 2016; Suryaprasad et al., 2014; Zibbell et al., 2015).
Our findings underscore the need to expand access to comprehensive risk reduction services such as access to sterile syringes, needles and other injection equipment, HIV and HCV testing and linkages to care, naloxone for overdose reversal, and medication-assisted treatment for opioid use disorders. The recent increases in heroin use and overdose linked to people who first started misusing prescription opioids and the rapidly expanding practice of non-pharmaceutical fentanyl being mixed with or sold as heroin leading to high numbers of overdoses, point to the extraordinary urgency of bringing these interventions to scale. This is particularly pressing in the South where more than 1 in 4 admissions in 2013 reported injection abuse. Prior research indicates limited access to medication-assisted treatment and syringe services programs in the South (Des Jarlais et al., 2013; Jones et al., 2015). Further emphasizing the urgency of action in this area, a recent study found that 150 of the 220 counties (68.2%) in the U.S. deemed most vulnerable to the rapid dissemination of HIV or HCV infections among people who inject drugs were counties in the South (Van Handel et al., 2016).
The finding that treatment admissions who started abusing prescription opioids at earlier ages were at increased risk for injection and other non-oral routes of abuse highlight the significance of implementing prevention programs that address prescription opioid abuse risk and protective factors. Spoth et al. (2013) demonstrated the long-term effectiveness of brief universal preventive interventions that can be implemented during middle school to reduce prescription opioid abuse. Investments to enable more widespread adoption of these early interventions among adolescents and young adults are needed. In addition, although the majority of people receiving prescription opioids take them as directed, given the well-documented relationship between increased inappropriate prescribing of prescription opioids and subsequent rise in abuse and overdose among nonmedical users of prescription opioids, efforts to improve the uptake of clinical practice guidelines on appropriate opioid prescribing, such as the recently released Centers for Disease Control and Prevention’s Guideline for Prescribing Opioids for Chronic Pain, (Dowell et al., 2016) and the implementation and routine use of prescription drug monitoring programs to aid clinical decision-making and to identify problematic use of prescription opioids and other controlled medications are needed.
4.1. Limitations
The study is subject to several limitations. First, TEDS comprises a significant proportion of all admissions to substance abuse treatment in the US; however, it does not capture all admissions. TEDS includes admissions at facilities that are licensed or certified by a state substance abuse agency or are administratively tracked for other reasons. Second, the primary, secondary, and tertiary substances of abuse reported to TEDS are those substances that led to the treatment episode and not necessarily a complete enumeration of all drugs used at the time of admission. Third, in many states TEDS data may include multiple admissions for the same patient. Therefore, the data in this study represent admissions and not patients. Despite these limitations, to our knowledge, this is the first study to examine in-depth national-level trends and characteristics associated with non-oral routes of prescription opioid abuse.
4.2. Conclusions
Injection and other non-oral routes of abuse among people admitted to substance use treatment for prescription opioid abuse increased significantly in the U.S. between 2004 and 2013. Given the growing concerns over health consequences related to opioid injection, actions are urgently needed to strengthen opioid abuse prevention policies and programs and expand the availability of medication-assisted treatment and comprehensive risk reduction services for people who inject drugs.
Role of the funding source
This study was jointly sponsored by the Office of the Assistant Secretary for Planning and Evaluation of the U.S. Department of Health and Human Services and the Centers for Disease Control and Prevention. The sponsors supported the authors who were responsible for preparation, review, and approval of the manuscript and the decision to submit the manuscript for publication. The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation and review of the manuscript; or decision to submit the manuscript for publication. The sponsors reviewed and approved the manuscript.
Footnotes
Conflict of interest
The authors report no conflicts.
References
- Black RA, Trudeau KJ, Cassidy TA, Budman SH, Butler SF, 2013. Associations between public health indicators and injecting prescription opioids by prescription opioid abusers in substance abuse treatment. J. Opioid Manag 9, 5–17. [DOI] [PubMed] [Google Scholar]
- Compton WM, Volkow ND, 2006. Abuse of prescription drugs and the risk of addiction. Drug Alcohol Depend. 83, S4–S7. [DOI] [PubMed] [Google Scholar]
- Davis WR, Johnson BD, 2008. Prescription opioid use, misuse, and diversion among street drug users in New York City. Drug Alcohol Depend. 92, 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Des Jarlais DC, Nugent A, Solberg A, Feelemyer J, Mermin J, Holtzman D, 2013. Syringe service programs for persons who inject drugs in urban, suburban, and rural areas–United States, 2013. Morb. Mortal. Wkly. Rep 64, 1337–1341. [DOI] [PubMed] [Google Scholar]
- Dowell D, Haegerich TM, Chou R, 2016. CDC guideline for prescription opioids for chronic pain -United States, 2016. MMWR. Recomm. Rep 65. (NoRR-1), Retrieved on 17 November 2016 from: 10.15585/mmwr.rr6501e1. [DOI] [PubMed] [Google Scholar]
- Havens JR, Walker R, Leukefeld CG, 2007. Prevalence of opioid analgesic injection among rural nonmedical opioid analgesic users. Drug Alcohol Depend. 87, 98–102. [DOI] [PubMed] [Google Scholar]
- Inciardi JA, Surratt HL, Cicero TJ, Beard RA, 2009. Prescription opioid abuse and diversion in an urban community: the results of an ultrarapid assessment. Pain Med. 10, 537–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Campopiano M, Baldwin G, McCance-Katz E, 2015. National and state treatment need and capacity for opioid agonist medication-assisted treatment. Am. J. Public Health 105, e55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz N, Dart RC, Bailey E, Trudeau J, Osgood E, Paillard F, 2011. Tampering with prescription opioids: nature and extent of the problem, health consequences, and solutions. Am. J. Drug Alcohol Abuse 37, 205–217. [DOI] [PubMed] [Google Scholar]
- Katz N, 2008. Abuse-deterrent opioid formulations: are they a pipe dream? Curr. Rheumatol. Rep 10, 11–18. [DOI] [PubMed] [Google Scholar]
- Kim HJ, Fay MP, Feuer EJ, Midthune DN, 2000. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med 19, 335–351. [DOI] [PubMed] [Google Scholar]
- Lake S, Kennedy MC, 2016. Health outcomes associated with illicit prescription opioid injection: a systematic review. J. Addict. Dis 35, 73–91. [DOI] [PubMed] [Google Scholar]
- Lankenau SE, Teti M, Silva K, Jackson Bloom J, Harocopos A, Treese M, 2012.Initiation into prescription opioid misuse amongst young injection drug users. Int. J. Drug Policy 23, 37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lankenau SE, Kecojevic A, Silva K, 2015. Associations between prescription opioid injection and Hepatitis C virus among young injection drug users. Drugs 22, 35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars SG, Bourgois P, Karandinos G, Montero F, Ciccarone D, 2014. Every ‘never’ I ever said came true: transitions from opioid pills to heroin injecting. Int. J. Drug Policy 25, 257–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mateu-Gelabert P, Guarino H, Jessell L, Teper A, 2014. Injection and sexual HIV/ HCV risk behaviors associated with nonmedical use of prescription opioids among young adults in New York City. J. Subst. Abuse Treat 48, 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Cranford JA, Boyd CJ, Teter CJ, 2007. Motives, diversion and routes of administration associated with nonmedical use of prescription opioids. Addict. Behav 32, 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Boyd CJ, Cranford JA, Teter CJ, 2009. Motives for non-medical use of prescription opioids among high school seniors in the United States: self-treatment and beyond. Arch. Pediatr. Adolesc. Med 163, 739–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulozzi LJ, Jones CM, Mack KA, Rudd RA, 2011. Vital signs: overdoses of prescription opioid pain relievers–United States, 1999–2008. Morb. Mortal. Wkly. Rep 60, 1487–1492. [PubMed] [Google Scholar]
- Paulozzi LJ, 2012. Prescription drug overdoses: a review. J. Saf. Res 43, 283–289. [DOI] [PubMed] [Google Scholar]
- Peavy KM, Banta-Green CJ, Kingston S, Hanrahan M, Merrill JO, Coffin PO, 2012. Hooked on prescription-type opiates prior to using heroin: results from a survey of syringe exchange clients. J. Psychoact. Drugs 44, 259–265. [DOI] [PubMed] [Google Scholar]
- Peters PJ, Pontones P, Hoover KW, Patel MR, Galang RR, Shields J, Blosser SJ, Spiller MW, Combs B, Switzer WM, Conrad C, Gentry J, Khudyakov Y, Waterhouse D, Owen SM, Chapman E, Roseberry JC, McCants V, Weidle PJ, Broz D, Samandari T, Mermin J, Walthall J, Brooks JT, Duwve JM, 2016. HIV infection linked to injection use of oxymorphone in Indiana, 2014–2015. N. Engl. J. Med 375, 229–239. [DOI] [PubMed] [Google Scholar]
- Pollini RA, Banta-Green CJ, Cuevas-Mota J, Metzner M, Teshale E, Garfein RS, 2011. Problematic use of prescription-type opioids prior to heroin use among young heroin injectors. Subst. Abuse Rehabil 2, 173–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronan MV, Herzig SJ, 2016. Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002–2012. Health Aff. (Millwood) 35, 832–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roux R, Carrieri MP, Keijzer L, Dasgupta N, 2011. Reducing harm from injecting pharmaceutical tablet or capsule material by injecting drug users. Drug Alcohol Rev. 30, 287–290. [DOI] [PubMed] [Google Scholar]
- Roy E, Arruda N, Bourgois P, 2011. The growing popularity of prescription opioid injection in downtown Montreal: new challenges for harm reduction. Subst. Use Misuse 46, 1142–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd RA, Aleshire N, Zibbell JE, Gladden RM, 2016. Increase in drug and opioid overdose deaths–United States, 2000–2014. Morb. Mortal. Wkly. Rep 64, 1378–1382. [DOI] [PubMed] [Google Scholar]
- Silva K, Schrager SM, Kecojevic A, Lankenau SE, 2013. Factors associated with history of non-fatal overdose among young nonmedical users of prescription drugs. Drug Alcohol Depend. 125, 104–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Trudeau L, Shin C, Ralston E, Redmond C, Greenberg M, Feinberg M, 2013. Longitudinal effects of universal preventive intervention on prescription drug misuse: three randomized controlled trials with late adolescents and young adults. Am. J. Public Health 103, 665–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality, 2015. Treatment Episode Data Set (TEDS): 2003–2013. National Admissions to Substance Abuse Treatment Services. BHSIS Series S-75, HHS Publication No. (SMA.) 15–4934. Rockville, MD. [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2016. Treatment Episode Data Set Admissions Public Use Files. Retrieved on 15 March 2016 from: http://wwwdasis.samhsa.gov/dasis2/teds.htm.
- Surratt H, Kurtz SP, Cicero TJ, 2011. Alternate routes of administration and risk for HIV among prescription opioid abusers. J. Addict. Dis 30, 334–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suryaprasad AG, White JZ, Xu F, Eichler BA, Hamilton J, Patel A, Hamdounia SB, Church DR, Barton K, Fisher C, Macomber K, Stanley M, Guilfoyle SM, Sweet K, Liu S, Iqbal K, Tohme R, Sharapov U, Kupronis BA, Ward JW, Holmberg SD, 2014. Emerging epidemic of hepatitis C virus infections among young nonurban persons who inject drugs in the United States, 2006–2012. Clin. Infect. Dis 59, 1411–1419. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, 2013. Addressing Prescription Drug Abuse in the United States: Current Activities and Future Opportunities. Retrieved on 7 November 2016 from: http://www.cdc.gov/drugoverdose/pdf/hhs_prescription_drug_abuse_report_09.2013.pdf.
- Van Handel MM, Rose CE, Hallisey E, Kolling JL, Zibbell JE, Lewis B, Bohm MK, Jones CM, Flanagan BE, Siddiqi AE, Iqbal K, Dent AL, Mermin JH, McCray E, Ward JW, Brooks JT, 2016. County-level vulnerability assessment for rapid dissemination of HIV or HCV infections among persons who inject drugs, United States. J. Acquir. Immun. Defic. Syndr 73, 323–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vosler PS, Ferguson BJ, Contreras JL, Wang EW, Schaitkin BM, Lee S, 2014. Clinical and pathologic characteristics of intranasal abuse of combined opioidacetaminophen medications. Int. Forum Allergy Rhinol 4, 839–844. [DOI] [PubMed] [Google Scholar]
- Young AM, Havens JR, Leukefeld CG, 2010. Route of administration for illicit prescription opioids: a comparison of rural and urban drug users. Harm Reduct. J 7, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zibbell JE, Hart-Malloy R, Barry J, Fan L, Flanigan C, 2014. Risk factors for HCV infection among young adults in rural New York who inject prescription opioid analgesics. Am. J. Public Health 104, 2226–2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zibbell JE, Iqbal K, Patel RC, Suryaprasad A, et al. , 2015. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤ 30 years–Kentucky, Tennessee, Virginia, and West Virginia, 2006–2012. Morb. Mortal. Wkly. Rep 64, 53–58. [PMC free article] [PubMed] [Google Scholar]