Abstract
Introduction:
Women are not usually taught about the menopause formally, and many general practitioners have relatively little training. The aim of this study was to explore perimenopausal women’s attitudes and knowledge of the menopause.
Method:
An online survey was designed to evaluate attitudes and knowledge of the menopause in women older than 40 years. The survey was generated with Qualtrics XM® and promoted via social media. In all, 3150 women started the survey. In this study, data from 947 perimenopausal women were analysed.
Results:
Regarding women’s attitudes to the menopause, 38.8% were accepting of it but more than 30% were dreading it. The women had experienced a number of menopause symptoms including mood swings (68.9%), brain fog (68.3%), and fatigue (66.8%). More than 90% of women had never been taught about the menopause at school, and more than 60% did not feel informed at all about the menopause. School was thought to be the best place for menopause education to start (83.6%). In all, 68.2% of women had only looked for information about the menopause as their symptoms started and they had talked to friends and used a variety of websites to look for information. When asked for their free-text views on the menopause, thematic analysis produced four themes: the overarching knowledge gap, the onset and impact of symptoms, perimenopause: the hidden phenomenon, and managing symptoms: differing schools of thought.
Conclusion:
Lack of education for women and their general practitioners is causing perimenopausal women to go through this important stage in their lives with a lack of knowledge and appropriate medical care. It is essential that women are taught about the menopause, from school onwards and that we offer health professionals appropriate training starting from the medical school curriculum.
Keywords: education, menopause, menopause symptoms, perimenopause, women’s health
Introduction
Perimenopause and menopause have affected approximately one billion women worldwide. 1 The number of women aged 45 and older in the United Kingdom is on an increasing upward trajectory. 2 It is estimated that there are currently in the region of 13 million perimenopausal or menopausal women in the United Kingdom, equating to around one-third of the entire female population. 3
Menopause is the permanent cessation of menses for 12 months. 4 Once 12 months is reached, the woman will be post-menopause. The perimenopause is an ill-defined time period before the woman has her final period 5 and is often associated with the start of a number of perimenopausal symptoms.
Globally, there has little formal teaching about the menopause at any stage of a women’s life and the media often present the menopause negatively. A consequence of this is that many women have little knowledge or awareness of what can be a very symptomatic life phase. Equally, many health professionals have not received adequate and up-to-date training on how to deal with the menopause. 6 Consequently, perimenopausal women often suffer in silence in the absence of education and knowledge. 7
Both women and health professionals have misconceptions about how hormonal changes relate to the biological and psychological conditions of menopause. 8 Consequently, many women have little awareness that the wide array of symptoms they may be experiencing are related to perimenopause or that these can manifest in a biological, psychological, or social context. A study in the UAE found that 67% of women had poor knowledge of the menopause, 9 and a study of 220 UK women found that women had little formal menopause education. 10 Due to this lack of awareness, they are less likely to seek or receive the medical assistance they require. 11
Many surveys related to the topic of menopause have been conducted but to our knowledge, none have explored women’s knowledge and attitudes with the aim of improving menopause education. This is especially important in the United Kingdom as in 2019 the Department for Education has made it mandatory for menopause education to be included in schools. 12 Using an online survey, we wanted to explore these issues so that we can effectively deliver menopause education.
Method
Ethics
Ethics approval was awarded by UCL Research Ethics Committee ID no: 9831/005. The selected sample population for the study were English-speaking women who were aged 40 and older at the time of entering the survey.
Research design
For this mixed-method, observational study, a 35-question, online survey was designed using the computer software Qualtrics XM® composed of 34 quantitative questions and one free-text question. The inclusion was any woman aged 40 and older.
There were three sections to the survey. The first was informed consent which contained information about why the survey was being conducted, what questions would be asked, and data protection. The respondent only continued to the next section if they consented. Sociodemographic information was required which included age; gender identity; sexual orientation; current relationship status; whether they have children, and if so, how many; highest educational qualification; field of work/study/trade; religion; ethnicity; and disability status. The third section explored the women’s individual experience, attitudes, and their learning about perimenopause and menopause.
One of the final questions asked ‘Have you had, or are you having, any of the symptoms below since becoming peri-menopausal or menopausal – tick all that apply’. The list of 52 symptoms was decided upon through extensive research and discussions with patients and clinicians. This question did not suggest that they were all menopausal symptoms. It was decided to put this question towards the end of the survey as we felt that if they were presented with this long list of symptoms at the start of the survey, it would taint their responses. It was possible that this question affected the final free text question.
The survey was validated by seeking advice from menopause advocates and using cognitive interviews with eight women. The eight women were interviewed while they completed the survey in a 1:1 meeting. As they went through the questions, it was discussed whether they could understand the question and whether the question required editing. Very few edits were needed at this stage. A soft launch was advertised on the Global Women Connected Facebook group (a group run by Professor Joyce Harper which discusses various women’s health issues) to check the functionality of the survey which was live on various social media platforms (Facebook, Twitter, LinkedIn, and Instagram) from 19 May 2021 to 26 May 2021. Data saturation was reached and evidenced during data analysis and confirmed during initial coding.
We asked women ‘which of the following stages do you think best describes you’. Not in the perimenopause/menopause, Peri-menopausal – still having periods with some peri-menopausal symptoms. Post-menopausal – not had a period for 1 year or more, I am not sure if I am peri-menopausal/menopausal, I do not currently have periods, so I am not sure whether I am peri-menopausal/menopausal. This made it possible for us to filter out perimenopause and post-menopause women. In this study, only the women who identified as perimenopausal are included, and the remaining data will be published subsequently. Thematic analysis was conducted by adopting the six-phase method suggested by Braun and Clarke. 13 The data were read and then re-read to enable immersion into the text. Second, meaningful and repeated units of text were identified, which were assigned codes, allowing more data to be identified and categorized into these codes. Third, the data were reviewed again by two others to ensure all codes had been identified and exhausted.
Results
Sociodemographic characteristics
A total of 3150 women started the survey and 947 described themselves as perimenopausal and were included in this analysis. Some respondents did not answer all the questions, and incomplete responses were included in the analysis. The demographic characteristics of these women included are in shown Table 1. The majority of the women in this study identified as female (919/947, 97.0%) and were married or in a civil partnership (633/947, 66.3%).
Table 1.
Demographic characteristics of the perimenopausal women of the study.
| n | Frequency (%) | |
|---|---|---|
| Age | ||
| 40–45 | 232 | 24.5 |
| 46–51 | 549 | 58.0 |
| 52–55 | 149 | 15.7 |
| >56 | 17 | 1.8 |
| Country of residence | ||
| United Kingdom | 830 | 87.7 |
| Other | 117 | 12.4 |
| Gender Identity | ||
| Female | 919 | 97.0 |
| Non-binary | 2 | 0.2 |
| Prefer not to say | 17 | 1.8 |
| Other | 9 | 1.0 |
| Sexual orientation | ||
| Heterosexual | 851 | 89.9 |
| Homosexual | 23 | 2.4 |
| Bisexual | 42 | 4.4 |
| Pansexual | 10 | 1.1 |
| Asexual | 3 | 0.3 |
| Prefer not to say | 18 | 1.9 |
| Relationship status | ||
| Single | 126 | 13.3 |
| In a relationship not cohabiting | 39 | 4.1 |
| In a relationship cohabiting | 129 | 13.6 |
| Married/civil partnership | 633 | 66.8 |
| Prefer not to say | 4 | 0.4 |
| Other | 5 | 0.5 |
| Widowed | 11 | 1.6 |
| Parity | ||
| 1 | 187 | 19.8 |
| 2 | 393 | 41.5 |
| 3 | 117 | 12.4 |
| 4 or more | 33 | 3.5 |
| I do not have children | 215 | 22.7 |
| Prefer not to say | 2 | 0.2 |
| Highest educational qualification | ||
| Secondary school | 41 | 4.3 |
| A level/College level | 110 | 11.6 |
| University undergraduate | 222 | 23.4 |
| University postgraduate | 500 | 52.8 |
| Other | 20 | 2.1 |
| Prefer not to say | 3 | 0.3 |
| Ethnicity | ||
| White-English/Welsh/Scottish/Northern Irish/British | 741 | 78.2 |
| White-Irish | 39 | 4.1 |
| Any other white background | 68 | 7.2 |
| Black/Black British-Caribbean | 3 | 0.3 |
| Any other Black/African/Caribbean background | 3 | 0.3 |
| Asian/Asian British-Indian | 13 | 1.4 |
| Arab | 1 | 0.1 |
| Latino | 3 | 0.3 |
| Mixed ethnic background | 13 | 1.4 |
| Any other ethnic group | 2 | 0.2 |
| Prefer not to say | 5 | 0.5 |
Women’s attitudes and experience of the menopause
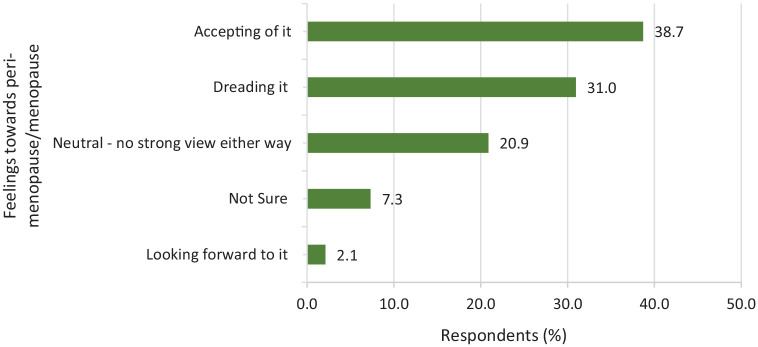
Women were asked how they felt about the perimenopause/menopause and were given five options: looking forward to it, accepting of it, neutral (no strong view either way), dreading it, not sure (Figure 1). In all, 61% of women were accepting, looking forward to, or feeling neutral about the menopause (578/947), but 31% were dreading it (292/947).
Figure 1.
Women were asked how they felt about perimenopause/menopause.
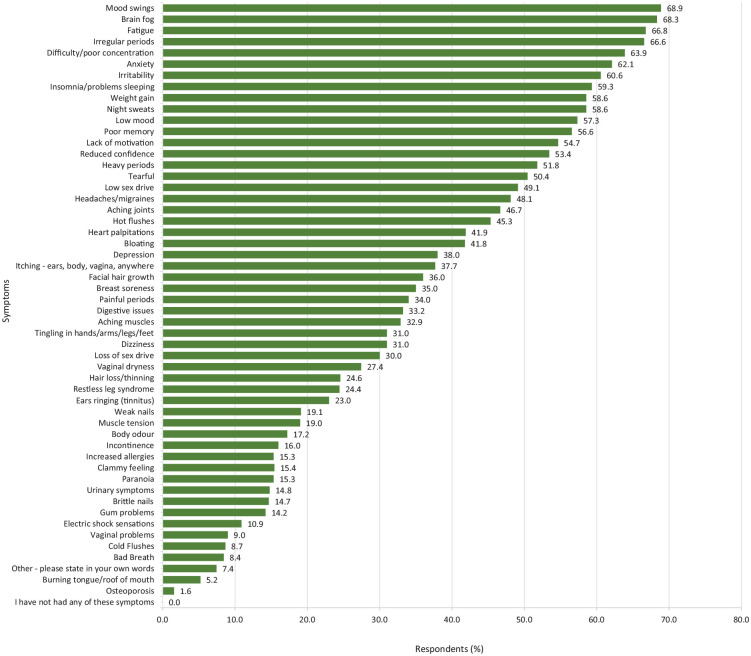
Women were asked if they had had, or if they were having, any symptoms since becoming perimenopausal and they could tick all that applied (Figure 2). The most common symptoms were mood swings (68.9%, 620/900), brain fog (68.3%, 615/900), fatigue (66.8%, 601/900), irregular periods (66.6%, 599/900), and difficulty concentrating (63.9%, 575/900). Night sweats were reported by 58.6% (527/900) and hot flashes by 45.3% (408/900). Low sex drive was noted in 49.1% (442/900) and loss of sex desire in 30.0% (270/900). If put together, 79.1% of women reported effects on their desire for sex. Vaginal dryness was noted in 27.4% (247/900) and vaginal problems in 9.0% (81/900).
Figure 2.
Women were asked if they had had, or if they were having, any of the symptoms below since becoming perimenopausal and could tick all that applied.
Menopause knowledge and education
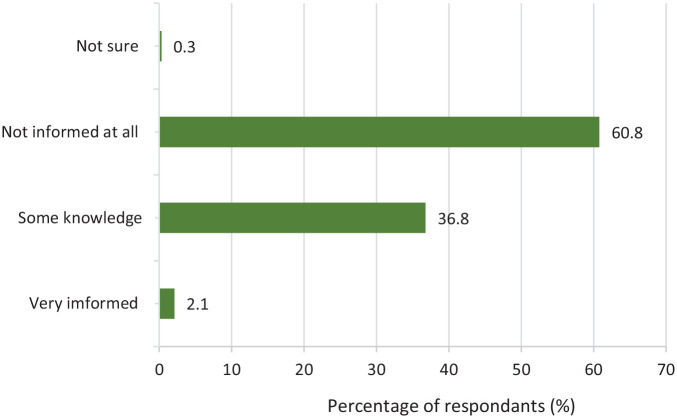
Women were asked if they had been taught about the menopause at school and were given three options: not at all, some basic information, and very detailed – 90.2% (812/900) said not at all and 9.8% (88/900) said some basic information. None had been taught very detailed information.
Women were asked how informed they felt about the perimenopause/menopause before the age of 40 with the option to choose: very informed, some knowledge, not informed at all, and not sure (Figure 3). More than 60% felt not informed at all (547/900).
Figure 3.
How informed the women felt about the perimenopause/menopause before the age of 40.
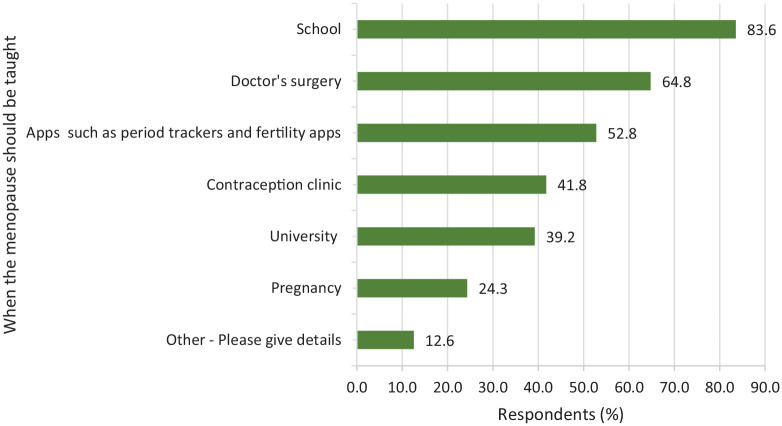
Women were asked when they thought the menopause should be taught and were given a list of options: school, university, doctors surgery, contraception clinic, apps such as period trackers and fertility apps, pregnancy, and other and could tick all that applied (Figure 4). Most respondents wanted the menopause to be taught at school (83.6%, 752/900), doctors’ surgery (64.8%, 583/900), and through apps (52.8%, 475/900).
Figure 4.
Women were asked, when do you think the menopause should be taught? Respondents could tick more than one option.
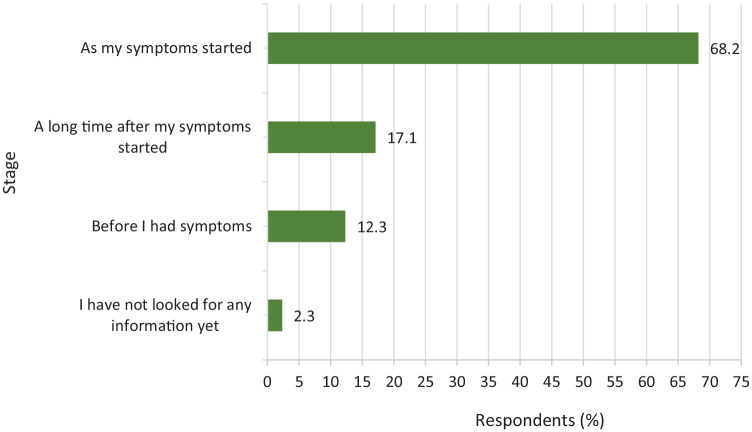
Women were asked if they had started to look for this information, and when did they look for it (Figure 5). Most respondents looked for information as their symptoms started 68.2% (614/900), with only 12.3% (111/900) looking before their symptoms.
Figure 5.
If they had looked for information about the perimenopause/menopause, when had they started to look for information.
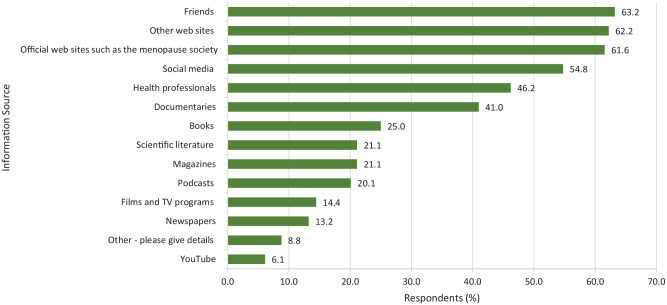
Women were asked if they had specifically looked for information about the menopause in any of these ways and they could tick all that applied (Figure 6). The three top answers were friends (569/900, 63.2%), websites (560/900, 62.2%), and official websites such as the menopause society (554/900, 61.8%).
Figure 6.
Women were asked if they had specifically looked for information about the menopause in any of these ways and could tick all that applied.
Qualitative analysis
Women were asked if they would like to tell us anything about their views of perimenopause/menopause in their own words. A total of 545 women gave answers. Four themes were identified: the overarching knowledge gap, the onset and impact of symptoms, perimenopause: the hidden phenomenon, and managing symptoms: differing schools of thought.
The knowledge gap
This was a major theme that many women spoke about. There were two main areas of the women’s lived experience that were pivotally affected by lack of education; their personal lack of education and their general practitioner’s (GP) lack of education.
Their personal lack of education
The women were angry that they had reached this point in their lives without any knowledge of how perimenopause would affect them. They talked about their woeful lack of preparedness which made them feel disempowered and caused them to lose confidence both in themselves and in their bodies. A number of them stated they had never even heard the word perimenopause before. They used language such as ‘disgraceful’ and ‘shocking’ in reference to the paucity of information that exists and many of the women called for earlier teaching in schools.
We aren’t informed enough. I’d never even heard the word perimenopause until I spoke to a nurse. I genuinely thought my menopause started when my periods stopped. I’ve been having symptoms and suffering in silence for 2 years. #29
I think we should be taught from a young age not only about our periods, sex, boys, girls, etc but what to expect when we are older at least if it were touched upon earlier. #675
Other than hot flushes, most of the women were entirely unaware of the wide array of symptoms and so did not connect them to the perimenopause. Some said that they had learned about some symptoms since reading the list in our survey. They reported a broad range of mental, emotional, and physical symptoms that had caused profound changes in them. Symptoms that were mentioned included anxiety, rage, suicidal thoughts, restless legs, facial hair growth, weight gain, and numerous others. Many of the women felt that they were going mad, especially when their GPs had no idea what was wrong with them and only offered antidepressants or selective serotonin reuptake inhibitors’ (SSRI), which the women knew were incorrect, in many cases.
Self-directed learning
A large number of the women were so frustrated with their lack of knowledge that they had engaged in self-directed learning. They had used a variety of methods including books, media, and websites. Some were worried about the quality of the information available while others managed to access more reliable online sources such as the National Institute for Health Care Excellence (NICE) guidelines, which some of the women took with them on visits to their GP.
Conversely, many of the women preferred to avoid the difficult hunt for information online as they said this led them down all sorts of ‘rabbit holes’. Many felt better assured knowing that others were having similar experiences and preferred to rely on friends, family, or work colleagues as their sources of information.
I have had more info from colleagues of the same age who have recommended alternatives than anything I have read. #139
Educating early is a must. Women spend around 1/3 of their life with reduced hormones and support is not available readily enough. It seems women have to seek out answers for themselves, many don’t because of lack of knowledge . . . #106
Regardless of how skilled the women were at researching, they said that navigating the route to access menopause information proved to be difficult and that they did not know where to look. Most of the women were educated to postgraduate level and even those with science or medical backgrounds such as nurses were at a loss as to how they could access the information they needed.
I consider myself well informed (because in physiology, PhD and work in research) – but I find it hard to know where to look for information. #100
Confusion with pre-existing conditions
A number of the women found it difficult to distinguish between the symptoms of perimenopause and the symptoms of their pre-existing conditions. The conditions they spoke of included premenstrual dysphoric disorder (PMDD), polycystic ovarian syndrome (PCOS), and deep vein thrombosis (DVT), among others. They wanted clarity on which symptoms were perimenopause related and which were not. In some cases, they felt that either condition made the other worse. They had questions that were unanswered and there was no information available to help them, even from their GP.
I have PCOS, there is practically no information available about PCOS and the menopause. I have kind of worked out for myself that my more regular periods might be a perimenopause symptom as my excessively high oestrogen levels fall into a more normal range. My GP has absolutely no idea about PCOS and menopause symptoms . . . I have no idea if there are any extra things I should be trying to manage as the PCOS and menopause interact. #690
Another area of confusion was the potential side effects or contra-indications of the medications they were already taking. They wanted to know how their present medication might interact with HRT or whether it would preclude them from being prescribed hormone replacement therapy (HRT) at all. The women were taking medications for aura migraines, asthma, anaemia, and they questioned the effect that either would have on the other. They commonly referred to the absence of GP’s knowledge and they found it difficult to find information anywhere. They felt unsupported to greater or lesser degrees.
I have a chronic illness so it is hard to see where that ends and the menopause begins. I have had doctors be very dismissive though I have increasingly problematic hormonal cycle related, devastating low mood depression. I have felt bereft of hope and suicidal. Hard to get taken seriously at all. Also very hard with tingling sensations and aches and pains as these are so easily dismissed. #81
In some cases, the women’s pre-existing conditions led to a need for a ‘tailor-made’ HRT prescription. Again, due to the lack of medical knowledge, many women were massively disappointed when they would go to their GP, hopeful of feeling supported, but their GP had no idea what to prescribe for them. As a result, some of the women felt as though they had no choice but to pay for help from the private sector.
I have had to pay for help, which concerns me because I have asked my own GP several times and I am also a well informed doctor. I have a history of DVT so I know I am high risk for traditional artificial oestrogen but it’s so massively disappointing that I have to pay £300+ to access decent advice and prescriptions which I know myself I could deliver to my own patients via the NHS. #729
Educating men and boys
A large part of the women’s lived experience was affected by the lack of perimenopause awareness in the people around them. Many referred to men’s attitudes that exist today, as sexist social norms that continue to reinforce shameful stereotypes of the menopausal woman. The women felt that men and boys should be taught menopausal awareness, so that they could appreciate the hardships of their loved ones and colleagues, to become fully supportive of their suffering.
It is men that need proper education as they make going through it worse with their constant judgements and constantly knocking women as if they are mad rather than suffering proper ailments. #599
Men need to be educated too . . . comics need to stop – the suffering is accepted as ‘nagging old moany women’. Pretty sure it would be taken more seriously if men had to go through it too. #639
Their GP’s lack of education
The women clearly expressed their disbelief and distress in the face of their GP’s limited education. Their angst was evident in their stories of repeated, unsuccessful attempts to find out what was wrong with them and to understand why they were suffering unexplained symptoms. They resoundingly complained that their GP lacked awareness of perimenopause/menopause and how disappointed they were when their GP consultations would lead to an unsatisfactory end, without even a mention of perimenopause or menopause. In this way, the women would repeatedly come away from their GP feeling increasingly abandoned, unsupported, and would be left reeling with confusion, as though they were going mad.
I had very little idea of the range of symptoms of the peri-menopause. I knew about hot flushes and I didn’t have those so couldn’t work out what was happening to me. I honestly thought I was going mad. I also really struggled to get any help from my GP – two male GPs dismissed my symptoms and said it’s a phase every woman goes through . . . #28
Incorrect medical advice
There were numerous reports where the women’s consultations highlighted their GP’s lack of education in matters of perimenopause/menopause. As a result, the women commonly reported being misinformed which resulted in their having to return several times following inaccurate diagnoses and/or incorrect prescriptions. The women shared many frightening examples where they knew their mental health issues were perimenopause/menopause-related, that is, depression or anxiety, but the GP would refuse to listen. Instead, the women felt undermined and disrespected by their GP’s insistence on prescribing antidepressants or SSRIs.
Symptoms not recognized by GP, who has prescribed Sertraline for ‘mood symptoms’. I am not taking them, because my low mood reflects hormonal changes, and it is not consistent or like depression. I have requested HRT for current and future health, but the GP has refused it. I have the NICE guidelines to inform GP practice of this peri menopausal gaslighting and mis-prescribing. #163
The women were bemused when they were given incorrect explanations by their GP. For example, they were told that they could not be perimenopausal because they were too young, or that the menopause was not possible in their 40s, or because they were still menstruating. Many of them knew they had been misinformed and this fuelled their concerns that they could not trust their GP. They reported how they were recommended blood tests that did not reveal perimenopausal status and so were dismissed, or simply not believed. Some also felt frustrated after being sent for various tests including magnetic resonance imaging (MRI) and computed tomography (CT) scans, which came back negative, and the women were brushed off, despite experiencing perimenopausal symptoms.
I’ve had so many tests in the last two years for heart palpitations, ectopic beats, etc and nobody suggested this might be caused by the menopause. I’ve suffered from bouts of terrible dizziness. Nobody suggested it might be menopause. My migraines got so much worse I had to see a neurologist, even she didn’t suggest it might be menopause. I had to have a scan because of bloating and abdominal pain, and have terrible adenomyosis, and the radiologist said maybe a coil might help. This led to more discussions around perimenopause incidentally, and now I’m on HRT and finally feel more like me that I have in years. So many doctors and none mentioned menopause once. Yet I was over 45. It’s just wrong. #456
The upshot of scenarios such as these left the women exhausted and lacking confidence in their doctors. Some of them chose to point out that their GP was a woman, as though hoping this would avail them satisfactory advice, yet they felt equally unsupported. Many felt the only option was to pay for private treatment.
While sadly few, it is noteworthy to point out that some of the woman reported positive experiences with their medical professional.
. . . I was treated for anxiety and stress for a long time until I went back to complain about severe night sweats and I was lucky that a youngish woman doctor was on the ball – I had blood tests that confirmed I had hrt patches and coil and within 3 months felt nearly myself again. #566
The onset and impact of the symptoms
Being unprepared regarding the symptoms of the menopause led to two subthemes: being surprised by the onset of symptoms, and the impact of the symptoms.
Surprised by the onset of symptoms
Arising from their lack of education, many of the women were surprised by the unexpected onset of perimenopausal symptoms and they were equally shocked by the vague nature of the onset. Unaware, some spoke of living with the symptoms for long periods of time before they ‘joined the dots’. Likewise, a number of the women only realized their symptoms were linked to perimenopause when ticking the list of 52 symptoms in our survey.
The lack of information is shocking, I didn’t know the symptoms so didn’t join the dots until I spoke to a friend! We are both nurses, and we didn’t know! #438
The symptoms hit me like a truck about 3 years ago and I wasn’t prepared at all. #307
The women’s reports of the gradual nature of how the symptoms ‘crept up’ on them was illustrative of the many different combinations and individual symptoms that they experienced; either all of a sudden or on an accumulative basis. These symptoms ranged from the most common such as hot flushes, night sweats, and brain fog.
I am astonished at the range of symptoms and the impact they had on me and how ill prepared I was. I had anxiety, lack of sex drive, fuzzy hands, memory loss, low confidence, brain fog and so on, the fatigue I felt for years shocked me to the core. The migraines were debilitating and I reached the point of feeling my life was pointless and I added no value. #76
The women did not expect to have symptoms in their early 40s or even as early as age 35. They said they felt totally underprepared. The combination of the unpredictability and the surprise of the onset brought a devastating blow to some of the women. One woman spoke of having fallen off a hormonal cliff and said that having to come to terms with the unanticipated impact on their fertility was particularly difficult. They were thrust into a process of bereaving their ability to have children and spoke of having to deal with feelings of loss or grief at the sudden end of their fertile years.
If I had been more aware of what the symptoms were, and had had more of an understanding from my GP when I went with increasingly heavy/clotting periods at 40/41, then I feel I would have realised what was happening and looked to treat those symptoms much earlier. I have found it particularly difficult, not having children, as you realise that the whole reason for women having the presence of a menstrual cycle is to be fertile and produce children. So knowing that it is all going to end without feeling it was ‘useful’ in any way is hitting quite hard. #759
In many cases, they were brushed off by their GP saying ‘no, you’re too young’. The women suggested that perimenopause should be routinely discussed at their health checks to remove some of the mystery that surrounds perimenopause and to help allay the shock of the onset.
The impact of the symptoms
The women’s voices included undertones of the biopsychosocial elements influencing their lived experience of perimenopause. They described their mental, emotional and physical symptoms and how the effects of those spilled from their personal and interpersonal lives, and beyond, into their working lives. Some examples of this were anxiety about being a competent parent, worries about maintaining competency in their work, or relationship breakdown.
It’s impacted my relationship with my husband and I’m now battling to save my marriage all because of perimenopause!! #734
I lived with severe symptoms for 18 months – I was exhausted and unable to focus on my job, and felt that I no longer had the capability to do my work. #575
When the analysis delved into the consequences of the symptoms they were expressing, it was possible to appreciate the whole-person effect of perimenopause. For example, when the women said they were suffering hot flushes or night sweats, many expressed that they were confused by what was happening to them. It was as though they were residing in changing bodies, with no knowledge or understanding as to why this was the case. In a number of instances, their internal confusion impacted their sense of self-worth, to the extent that they would profoundly lose confidence.
My confidence and sense of self worth was on the floor and the tears I have cried, I have lost count of #76
It’s totally taken over my well being. Whilst I don’t feel unwell, I’m very aware my whole body and mind are different. I have different sensations in my bones, muscles and head. The tinnitus is constant and the other symptoms just happen at different intervals. #727
The women’s narratives were illustrative of how perimenopause and its symptoms had the potential to become terrifying, and intricately enmeshed in their beings, to the point of disabling their normal functioning and causing embarrassing situations.
It’s terrifying. The sudden mood changes are the worse- I have had shouting matches with strangers! Not like me at all. I have a lot more sympathy toward teenage boys when they’re learning to cope with anger. It’s not something I’ve had to learn until now. #518
The ongoing state of confusion often had the women questioning their sanity.
They spoke of issues around their mental health, including brain fog, feeling they were getting premature dementia or that they were going mad. For some, the mental impact was so extreme that they spoke of ending their lives.
I feel desperate that I might kill myself . . . The healthcare system should be set up to allow professionals the time to properly look after women and for them to monitor their health so support can be offered proactively at the right time . . . I have been frighteningly close to walking into traffic so I can end my life. Instead of feeling supported, I have been left to piece together a diagnosis . . . to say I feel let down is a massive understatement. #218
In contrast to the striking prevalence of the women’s negativity towards the impact of symptoms, some were positive. Some were ready to embrace the new life stage and expressed pleasure that their periods would stop. In some cases, they looked forward to the hormonal changes and were hopeful that the onset would make their current conditions, such as endometriosis and fibroids, less problematic.
Another of the joys of being female but looking forward to not being bothered with periods any more! It’s a beautiful phase of life – like the autumn – a season in life when there is change but moving onto new things! #668
Perimenopause: the hidden phenomenon
Some of the women spoke out about the secrecy that enshrouds perimenopause and called for open discussion for the purpose of increasing awareness and raising the profile of this hidden phenomenon. Some referred to the stigma of all issues related to perimenopause and the marginalizing effect this has had on their lives. The women’s voices were collectively indignant that ‘half the population’ go through perimenopause yet rather than being celebrated as a natural biological milestone, the taboo engrafts a culture of secrecy and isolation, where they are left to suffer in silence.
Absolutely need more information and should be talked about more. Women suffer in silence and it is a topic that people don’t feel comfortable talking about. It’s like you have to hide it as it is so socially unacceptable for women to admit they are getting older! #296
Overall, the women took the position as though calling out those with outdated views. Their voices were demonstrative of a collective of women pushing back against the historical and societal othering of the stereotypical ‘aging, sweaty’ woman undergoing perimenopause/menopause. They were fed up with the shame, indignity, and humiliation that has been overtly or covertly directed towards them, and generations before them.
. . . men. . . make going through it worse with their constant judgements and constantly knocking women as if they are mad rather than suffering proper ailments. #599
We should change the narrative from that of a shameful process that represents all the negatives of being female and ageing. The message is of something to be quiet about, that you’re ‘past it’ not just in terms of fertility, or that you’re a mad old woman, constantly losing your temper and sweating. The latter might be true, but it should be a process that is normalized so that we can seek help without feeling like we’ve failed somehow. #356
Some of the women’s feminist leanings came through in this theme more than the other themes. In this way, they spoke of the different expectations they believed men would have in the event of being similarly situated. There was a palpable feeling of their unease with the long-standing patriarchal influence and medicalisation of perimenopause and menopause. The women expressed how the age-old dogma of keeping women’s health issues ‘under wraps’ has created a way of life where they are hesitant in sharing their suffering, even with their closest family members.
If this was affecting men there would be drive through windows handing out HRT. Enough with the patriarchal control of women’s bodies. #577
It’s simply not discussed enough . . . It made me embarrassed to discuss it with my family and friends as you don’t want to appear ‘old’ or less of a women because you can’t have children. It makes me feel really sad when I think about the impact it’s had on me. I’m grateful to be able to share these thoughts now and grateful you are doing a study, it needs to be talked about more openly. #55
The overarching lack of perimenopause education also infiltrated the women’s workplace and some felt entirely misunderstood and unsupported during their suffering at work. They expressed how there is an expectation to remain silent about any perimenopause/menopause issues they may have while doing their job. They reported people rolling their eyes if they tried to talk about it and that any suffering was seen as a sign of weakness. They alluded to the unspoken rule where matters of perimenopause/menopause are to be kept hidden. They said that having to battle symptoms that they did not understand, while there was no appreciation for what they were going through, impacted their confidence. Many felt that their competence was compromised due to the lack of support, and some had to leave their job.
The loss of confidence and the feeling of wanting to hide from people at work is very debilitating. I seem to manage having a dippy day at home but at work it panics me and makes me feel as if I can’t do my job. #570
I wish it wasn’t so taboo and work colleagues/family not roll their eyes when you try and talk about it. #574
The women reflected on the impact of the taboo and stigma on their careers. They compared their partner’s work experience at the same stage of their careers, compounded by the draining effect of perimenopause. In contrast to their partner’s experience, they spoke of the combined juggle of work, running the family, and perimenopause. This combination made them feel side-lined into accepting fewer challenging positions.
Society still expects women to melt away into the background. By their mid-forties most men are nailing their careers, and yet women frequently feel self doubt at the prospect of managing the menopause, family life and a demanding career. This shouldn’t be happening and it is costing the economy as women are not sufficiently supported to stay in/take on demanding roles. #877
Many of the women called for the education of employers and colleagues, to enable understanding of perimenopause/menopause in the workplace. They called for open discussion and measures to be put in place such as well-being initiatives and policies that would enable them to do their work, without the judgement and criticisms of others. One of the women had set up a menopause support group at work, and another created guidelines to make reasonable adjustments for female staff members.
It is disappointing the lack of knowledge of many professionals and peers, as such I have had to educate myself. As a headteacher I have created policy and guidelines to make reasonable adjustments for female staff members. #133
The taboo and stigma of all perimenopause/menopause matters were apparent in the women’s homelives as they would refer to their loneliness and said they had no-one to talk to. There were many references to opening the discussion at home and talking about it more with family and loved ones to dispel the taboo. One of the women spoke of how their vaginal symptoms impacted their sex life and how their lack of communication almost wrecked their marriage. Another of the women expressed their working as a team with their partner by saying ‘my husband and I decided to go privately’, however, the women’s silence, behind closed doors, was more prevalent within the narratives.
. . . My husband didn’t have a clue either – bit of an awkward conversation, made me feel washed up and passed it when he’s just fine. Feels very unfair. No-one speaks about the impact on your sex life and these issues have nearly caused me and my husband to separate. #843
Managing symptoms: differing schools of thought
Their narratives are rich with stories of the many barriers and their convoluted routes to find ways of managing their symptoms. Some chose to go on HRT and have been delighted, some have stopped using HRT due to side effects, or simply chose not to opt for HRT. Some have bypassed the biomedical route in the pursuit of natural alternatives or lifestyle changes, and some have chosen not to treat their perimenopause but to accept it as a natural life phase.
Requesting HRT
Some of the women were trying to get HRT and some were already on it. In either case, many spoke of their difficulties and the barriers they encountered in the process of trying to get a prescription.
Some women were annoyed by the lack of knowledge at almost every turn of their quest to obtain HRT. They explained how this made it difficult for them to navigate a complicated medical system while undergoing their own, confusing symptoms. Many told of their long-lived and complicated journeys during which they endured symptoms for up to 10 years, before reaching a prescription for HRT. Some of the women chose to persist, and some chose not.
At 45 after numerous doctors and hospital appointments I was fitted with the mirena coil to stop my continuous period and sent on my way with no mention of perimenopause. I now learn that was the start of it and lots of symptoms and doctors visits (several visits each year thinking I was completely falling apart!) have followed over the following 8 years which have taken their toll with no mention of oestrogen deficiency. After being prompted by a friend I started research and am now on HRT. Very annoyed at the lack of help. #893
On numerous occasions, the women were ignored, not believed, or refused HRT, due to their GP’s lack of perimenopausal knowledge. To ease their laborious journey, many embarked on self-directed learning and went to their GP armed with their own research such as the NICE guidelines for menopause. In some cases, they told their GP what to prescribe and as a result, they were given the wrong prescription.
The lack of information and support from health professionals is distressing. I had to do my own research on HRT to recommend to my GP who openly acknowledged that he doesn’t have a clue about the menopause. Not surprisingly I asked him to prescribe the wrong medication, which he did since he didn’t know anything about it. Finding the right HRT has taken me years, with serious health and personal consequences. #202
Some women were given the right prescription and they found that HRT changed their lives for the better. They were overjoyed and said it relieved all of their symptoms and gave them back a quality of life they had been missing.
. . .I did a lot of research before seeing my GP about HRT. I have been using HRT for two years and it has changed my life. I have better sleep, better energy, more confidence, ability to think critically and clearly, my body no longer feels heavy and slow, my outlook is brighter and I feel more like a normal human being! I feel really angry that there continues to be a prevalence of mis information about HRT and ongoing stigma about using it. It is a life saver and a life changer. #575
The women felt it was very hit and miss as to whether their GP would have sufficient knowledge to meet their perimenopausal needs and also whether that would avail them of the HRT which was best suited to them. Many had decided to pay for private treatment in the hope of a more satisfying experience.
I don’t feel like a visit to the GP would help me, I would most likely get prescribed a generic HRT, no tests would be done and I’d be told ‘let’s see how you get on with this’. I’m planning to go privately to seek help for a more tailored approach rather than a trial and error method that NHS offers. #846
Not wishing to take HRT
Many said they were unsure about going on HRT and harboured negative views. Often this hesitancy was connected either to the historic controversy connecting HRT with cancer or they felt they could not trust any NHS (National Health Service) guidance. Some felt that they wanted a natural approach to this time of their lives.
. . . I have no real knowledge about HRT but still feel it’s a risky option after the cancer scares of the early 2000’s. #468
I talked to a nurse at my GP surgery when I was having a smear. She told me I was too young to be peri menopausal. I was 45. It was so ignorant. It made me mistrustful of any NHS driven conversation . . . #898
Some had tried HRT and said that the side effects prevented them from continuing. They spoke of having bad migraines or really bad premenstrual syndrome (PMS) among other symptoms.
The NHS gynaecologist I eventually got a referral to put me on HRT that gave me the heaviest periods I’ve ever experienced, and really bad PMS when I had to take progesterone. I went back to her but she wasn’t very helpful. I’m on combined HRT now, having done my own research and suggested this particular one, but it only helps with the physical symptoms. I’ve booked with a Harley St specialist because I can’t go on like this. #789
The women told how the poor accessibility to any women’s health services was another dissuading factor in their decision against HRT. Many of the women were fed up with feeling lost amid the lack of support and called for changes to the healthcare system that would make women’s health services more easily available to them. They made suggestions such as reviewing the healthcare system to allow professionals the time to properly monitor women’s health. Others suggested support groups in GP practices or menopause clinics.
There needs to be accessible support. Menopause clinics that are branded as women’s wellness for a more holistic view. Or is it something that can be included in family planning? Not all GPs are equipped to give support, information and appropriate medication. Few of us can afford private obgyn. #855
. . . it can be quite frightening without knowing why you’re feeling this way. More education for GP’s to have these conversations with women is necessary. Have they considered menopause clinics, support groups with in GP practices? #505
Adding to the women’s sense of caution, the variability of the information in the media seemed to exacerbate HRT hesitancy among them. One woman went so far as to say the media portrayal of HRT was fearsome. Another woman said they were fed up with HRT propaganda and in this way, many were generally disappointed by the media bias where the portrayal of HRT was either positive or negative, with little neutrality. It was also acknowledged that more balanced media exposure was on the increase.
The issues around HRT feel very politicised . . . I struggle to find any ‘neutral’ information about it. Articles are either very pro-HRT or very anti. #767
I think that all the recent publicity would have worried me, as it gives the impression that all women will have severe symptoms unless we take HRT – which is not the case for me or most of my friends. #359
Natural alternatives and lifestyle changes
Some women did not want perimenopause or menopause to be medicalized and they refuted suggestions that it is a hormone deficiency that must be corrected with medication. They were proactive in their approach to perimenopause and were striving to be supportive of the changes within them. They preferred to uphold these changes as part of an inevitable life phase that is to be embraced, so they could actively enhance their lived experience.
I feel offended by the implication that menopause is a hormone deficiency syndrome. I think this is a misogynistic, patriarchal view even though it is often perpetuated by women. It is a difficult life stage for many people, but a natural process and women should not be regarded as deficient or broken in some way. #50
Menopause is the period of biological and a liberating phase of my life. My goal is to ride this phase with all the love and compassion and liberation I can give myself, maybe getting older was something I have always looked forward to . . . #482
The general mission of these women was to seek the information that would avail them of the optimum passage through the perimenopause/menopause. They seemed resigned that they could not rely on their GP for support and were determined to find their answers for themselves. They often referred to the lack of knowledge and were resentful that no help or advice was available to deal with their bodily changes such as weight gain. They were also unimpressed that information on diet, nutrition, or exercise was not readily available to help with many of these changes. Their preferred approach was to adopt lifestyle changes that would act to minimize their suffering.
If we were provided with advice about how to reduce symptoms such as exercise or walking, I would have had more motivation to do these things. #192
Want free advice about nutrition and exercise – how to get rid of tummy as previously tried and tested routines no longer work. #175
Some of the women preferred to try alternative therapies such as herbal medicine, homoeopathy, and naturopathy, and they were pleased with the results. They felt that this helped with hot flushes and some other symptoms. Some found social media sites useful but most felt frustrated at the paucity of information on complementary therapies and alternatives and asked for more guidance as to these other options that are out there.
With homeopathy, life is much easier and symptoms are minimal now – delighted to be breezing through it. A friend is still on HRT at age of 80 – I’m sorry but this is just plain wrong #668
Most literature I’ve seen seems to avoid alternative approaches or herbal alternatives. I have found the social media sites celebrating older women helpful in resetting my mindset and positive mental approach. #139
Discussion
To our knowledge, this is the first UK survey that has asked women their attitudes and knowledge of the menopause with the aim of improving menopause education. Through this quantitative and qualitative analysis, it is clear that menopause education needs to start in schools and continue throughout a woman’s life and that menopause education should be embedded in GP training. All women should have access to a suitably qualified doctor. Women should be fully informed when entering this key stage of their life and should also have confidence that they will be offered appropriate treatment.
Women’s attitudes to the menopause
In the United Kingdom, there has been no formal education about the menopause, so it is hardly surprising that although 40% of women in this survey were accepting of the menopause, 30% were dreading it. In the United Kingdom, the media have been mostly presenting a negative view of the menopause, such as recently portrayed in three TV documentaries. There is no doubt that many women will have physical and psychological symptoms. Hopefully, education will ensure women understand menopause symptoms and treatments before they reach perimenopause, rather than entering this stage of their lives in the dark about what it involves.
The question that asked ‘Have you had, or are you having, any of the symptoms below since becoming peri-menopausal or menopausal – tick all that apply’ listed 52 symptoms. The list was compiled from various sources 14 and added to after extensive discussions with menopause experts, menopause advocates, and women. The question did not say that all 52 were menopause symptoms and this list may cause some debate. Certainly, we have presented the most comprehensive list of suggested menopause symptoms to date, and some may argue that some of these symptoms may not be caused by the menopause. But we wanted to know what women thought. Certainly, further research needs to be conducted into symptoms that women experience around the time of the menopause.
The majority of symptoms the women reported were psychological issues such as mood swings, brain fog, irritability, poor concentration, poor memory, low mood, lack of motivation, reduced confidence, and anxiety, all of which may have a profound effect on women’s quality of life. Women may start to question many areas of their lives, from relationships to their careers. Some women will be living in a household where their children are going through puberty, which has many of the same symptoms as the menopause. Realizing that some of these feelings may be due to the menopause can be a comfort to many women. It is also important to determine if the symptoms were menopausal or due to other underlying health conditions.
The World Health Organization (WHO) has defined sexual health as a state of physical, emotional mental, and social well-being related to sexuality. Women in this survey complained of a low sex drive (49.1%) and loss of sex drive (30%). Vaginal dryness was noted in 27.4%. The latter is an unusual feature in perimenopausal women and more one of the post-menopause. This brings to the fore problems around arousal and lubrication rather than lack of local oestrogen as a cause. The figures in this survey suggest that sexual dissatisfaction is prevalent among peri-menopausal women and healthcare providers should be pro-active in eliciting this.
The qualitative analysis illustrated how many women were totally unaware that the symptoms they were experiencing were menopausal. The onset of symptoms caused shock and bewilderment which often had a significant impact on their lives.
Women in our survey were angry and shocked about how little they knew about symptoms. Herbert et al. 15 studied Australian women, and they also described the women’s lack of awareness of menopausal symptoms as ‘shocking’ and found a virtually complete absence of knowledge as to the possible long-term health effects of the menopause. A cross-sectional study of Chinese women showed that some had knowledge of the menopause but very little awareness, with most women believing that the symptoms of menopause do not need to be treated. 16 Larroy et al. 17 used the Menopause Rating Scale (MRS) 18 to assess and group symptoms into categories such as somatic, psychological, urogenital, physical, anxiety and depression, sexuality, and social. They concluded that perimenopausal symptoms led to a deterioration in women’s quality of life.
Women’s education
Being suitably informed about perimenopause/menopause matters would significantly improve women’s quality of life. 11 We found that a high proportion of women did not have any menopause education at school and that, before the age of 40, the majority had not felt informed at all. Seeing that most women had only looked for information about the menopause when their symptoms had started, or a long time after their symptoms had started, many were entering the perimenopause with no idea of what symptoms might be menopause-related and how to deal with them. In 1999, an evaluation was conducted on a health intervention used to explore the knowledge and impact of the menopause among a group of middle-aged women. A significant part of the group felt that being in the project had positively influenced their experience of the menopause and that being empowered with knowledge had helped them cope better, both emotionally and practically. 19
Without formal education, some women had resorted to self-learning but were finding it difficult to navigate reliable sources of information. They reported that talking to friends was the main way they self-learnt, followed by websites, such as the British Menopause Society (BMS). It is important for websites such as these to be aware that the public will view them, and it would be useful to make the information easily accessible and evidence based.
Koyuncu et al. 11 conducted an evaluation of the effectiveness of health education on menopause symptoms, knowledge, and attitude. Based in Turkey, this study included 52 women for a health intervention comprising three, 30-min sessions to impart information about the menopause, menopause-related health problems that can arise, and methods to assist with the prevention of those potential problems. At the end of the study, the women reported a decrease in the somatic and psychological subdimensions of the menopausal symptom evaluation scale and positive changes in their level of knowledge about menopause.
The women in our survey also stressed that it is key that men and boys are educated about the menopause so that they can understand what women are experiencing. There may be households where teenagers are going through puberty and the mother is going through the menopause, both of which present with similar psychological issues. It is also highly likely that some schoolteachers are going through the menopause. In the United Kingdom, including menopause education in the Personal, Social, Health and Economic (PSHE) Education curriculum will enable the education of boys and girls. 12
GP education
GPs are usually the first point of contact between a clinician and a woman facing menopausal symptoms. 6 In our survey we found that lack of perimenopausal/menopausal education for GPs was significant and had profound effects on the women. They suggested that their GP’s approach was coloured by the perception that perimenopausal symptoms were an isolated, biological event. 20 Some no longer trusted their doctor or the NHS. There was an over-reliance on diagnostic blood tests although these have been deemed to be unhelpful. 21 Findings of a 2018 survey suggested that medical professionals tend to find the emotional or sexual aspects of menopause more difficult to discuss than physical symptoms. 22 Overall, there was a widespread feeling of lack of support. As a consequence, medical gaslighting was inferred. 23 Medical gaslighting is a term used increasingly in Western medicine by those experiencing invalidation, dismissive, and unsatisfactory care. 24
In 2020, an American study exploring important gaps across various medical disciplines found that only 12 of 177 medical trainees felt suitably equipped to manage those undergoing menopause. 25 Another American study stated the lack of menopause education for medical students and trialled a 2-year menopause curriculum. 26 They found that structured menopause education adequately prepared the students to purposefully engage with those experiencing menopause.
The BMS is a non-profit organization established in 1989 which aims to educate, inform, and guide healthcare professionals on menopause and all aspects of post-reproductive health via lectures, conferences, courses, meetings, and exhibitions. 27 It has recently been reported that there are only about 143 BMS accredited menopause specialists and that due to a lack of menopause knowledge, medical professionals are obtaining menopause information from untrustworthy sources. 28 This was reflected in our survey since women reported that clinical management of their perimenopausal symptoms was unreliable and they often took the information, such as the NICE guidelines, to their doctors’ appointments.
Some studies have indicated that the initial findings of the 2002 Women’s Health Initiative study are still being primarily used by some medical practitioners as the basis for their advice regarding HRT to their patients although there have been further recent studies and re-analysis of the existing data with contrasting results.2,29 Some women found it difficult to get HRT and others found it was prescribed too freely. It is important for GPs to be able to advise women about all the options to treat menopause symptoms and to tailor treatment on an individual level. The need for this is clearly shown by the rise in private menopause clinical services.
Many women said they had received GP prescriptions for SSRIs or antidepressants. Prescribed medication generally resulted in compromised ability to discern which symptoms were perimenopausal and which were side effects of medication. For example, low sexual function was reported which could be either a symptom of perimenopause/menopause or a side effect of antidepressants. 30
A concerted and joined-up approach to increasing menopause education for GPs would significantly improve perimenopausal/menopausal women’s health care experience. It is critical that GP training is up to date and equips the GPs with all the necessary tools to treat menopausal symptoms and support patients in their journey during the menopausal transition by offering them evidence-based advice to help them make informed decisions. Several approaches have been suggested including mandatory training courses for primary and secondary care health professionals as well more menopause-focused educational content for trainee doctors and medical students. In 2014, the Chief Medical Officer, Dame Sally Davies, included an entire chapter in her annual report focussing on the psychosocial factors of menopause and its impact on work and personal lives. 31 Access to healthcare professionals who can both embrace and provide evidence-based advice and care to their patients during the menopausal transition is key. This would ensure that women receive the help if and when they need it as menopausal symptoms can deteriorate the quality of work, increase absence days and the overall impact the economy hugely.
In the United Kingdom, the BMS and the Faculty of Sexual and Reproductive Health (FSRH) are currently working hard to deliver training programmes for GPs as well as for women’s health specialists but funding is an issue. The Institute of Psychosexual Medicine is working alongside the Royal College of Obstetrics and Gynaecology (RCOG) and FSRH to highlight sexual difficulties among this group of women and ensure this is addressed appropriately.
Perimenopause: the hidden phenomenon
The findings in this study have demonstrated that there is much confusion and uncertainty around all aspects of perimenopause/menopause. A historic taboo, combined with the over arching lack of education and knowledge has rendered perimenopause ‘hidden’ and menopause-related matters to be considered private. This secrecy that enshrouds perimenopause and menopause has the capacity to permeate many areas of women’s lives including family, friends, and the workplace. It is hoped that increased education will bring the menopause to the forefront of conversations. Pop-up events such Menopause Café also helps as it gets the conversation started at ground level and raises awareness of the impact of menopause. 32
It is encouraging that menopause in the workplace appears to be a rising priority for employers. The majority of menopausal symptoms may affect a woman’s ability to work, and women also reported that they felt the menopause had affected their opportunity for promotion. Working in an environment that does not understand the menopause could be very stressful. The Office of National Statistics 33 data shows that menopausal women are the fastest growing working population with 8 in 10 menopausal women working. 34 In the United Kingdom, there is a national campaign to help employers understand menopause in the workplace. 35 This new focus of companies and institutions will provide improved working conditions as more companies continue to instigate policies and procedures to support their midlife employees.
Limitations
As with any survey, this study is limited to the responses of the people who completed it who were mostly educated to postgraduate level and were of white/British ethnicity, thereby compromising diversity. As a result, we are repeating this survey aiming at women from specific ethnicities, starting with black women. Promoting surveys on social media gives a bias to the social media followers of the person advertising the survey. Also, the survey was limited to women aged 40 and older. A survey for women aged 40 and younger was launched in February 2022.
In addition, education curricula and training of doctors are likely to vary significantly in different countries and some of the findings of this survey may not be applicable to women from different countries. Indeed, the narrative around the menopause and treatments is very variable in different countries (personal communications with people in other countries).
It may also be argued that women who had negative menopause experiences are more likely to complete a menopause survey, which may be the reason so many women reported negative views of the menopause. Either way, it is important to listen to the narratives of these women.
Our study demonstrated the lack of knowledge among women and the need for menopause education based on a large online survey. The findings of this survey are supportive of the changes announced for the UK education system, 12 UK Women’s Health Strategy, 36 and the development of menopause in the workplace strategies. From the announcement in 2021 of the UK government's Women’s Health Strategy, 36 almost 100,000 individuals and 400 organizations responded to the 2021 call for evidence. The strategy will be published in 2022, and central to the strategy will be to help women throughout their life course 37 which reflects the changing health issues of women throughout their lives, which includes adolescence, the fertile years, and post menopause.
Conclusion
This study provides valuable information to help develop menopause education and will be able to feed into the UK strategies. Women’s voices, healthcare policies and services, information and education, health in the workplace and research, evidence, and data are key themes. When educated, many women will still experience menopause symptoms, but they will enter this key stage of their lives fully informed about the symptoms and treatment options.
Supplemental Material
Supplemental material, sj-docx-1-whe-10.1177_17455057221106890 for An online survey of perimenopausal women to determine their attitudes and knowledge of the menopause by Joyce C Harper, Samantha Phillips, Rina Biswakarma, Ephia Yasmin, Ertan Saridogan, Sheila Radhakrishnan, Melanie C Davies and Vikram Talaulikar in Women’s Health
Acknowledgments
We would like to thank all the people who gave us advice in developing this survey including Angela Hindhaugh (Behing the woman), Rachel Lankester (Magnificent midlife), Elizabeth Ellis (Paustivity and know your menopause), and Jackie Lynch (the Happy Menopause).
Footnotes
Author contribution(s): Joyce C Harper: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Software; Supervision; Validation; Writing – original draft.
Samantha Phillips: Conceptualization; Methodology; Validation; Writing – original draft.
Rina Biswakarma: Data curation; Formal analysis.
Ephia Yasmin: Writing – review & editing.
Ertan Saridogan: Writing – review & editing.
Sheila Radhakrishnan: Writing – review & editing.
Melanie C Davies: Writing – review & editing.
Vikram Talaulikar: Writing – original draft; Writing – review & editing.
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Joyce Harper is author of Your Fertile Years and founder of Reproductive Health at Work.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Joyce C Harper  https://orcid.org/0000-0001-6364-2367
https://orcid.org/0000-0001-6364-2367
Supplemental material: Supplemental material for this article is available online.
References
- 1. Hoga L, Rodolpho J, Gonçalves B, et al. Women’s experience of menopause: a systematic review of qualitative evidence. JBI Database System Rev Implement Rep 2015; 13(8): 250–337. [DOI] [PubMed] [Google Scholar]
- 2. National Institute for Health Care Excellence (NICE). Menopause: diagnosis and management [Internet]. NICE, 2015, https://www.nice.org.uk/guidance/ng23 [PubMed] [Google Scholar]
- 3. Local Government Association. Menopause factfile, 2021, https://www.local.gov.uk/our-support/workforce-and-hr-support/wellbeing/menopause/menopause-factfile
- 4. World Health Organization (WHO). Research on the menopause in the 1990s: report of a WHO scientific group. World Health Organ Tech Rep Ser 1996; 866: 1–107. [PubMed] [Google Scholar]
- 5. Santoro N. Perimenopause: from research to practice. J Womens Health (Larchmt) 2016; 25(4): 332–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. General practice (GP) Health Careers, https://www.healthcareers.nhs.uk/explore-roles/doctors/roles-doctors/general-practice-gp
- 7. Brown L, Brown V, Judd F, et al. It’s not as bad as you think: menopausal representations are more positive in postmenopausal women. J Psych Obst Gynecol 2018; 39(4): 281–288. [DOI] [PubMed] [Google Scholar]
- 8. Gracia CR, Freeman EW. Onset of the menopause transition: the earliest signs and symptoms. Obstet Gynecol Clin North Am 2018; 45(4): 585–597. [DOI] [PubMed] [Google Scholar]
- 9. Hamid S, Al-Ghufli FR, Raeesi HA, et al. Women’s knowledge, attitude and practice towards menopause and hormone replacement therapy: a facility based study in Al-Ain, United Arab Emirates. J Ayub Med Coll Abbottabad 2014; 26(4): 448–454. [PubMed] [Google Scholar]
- 10. Bakouei F, Basirat Z, Salmalian H, et al. Assessment of women’s awareness level about symptoms and complications of menopause and methods to their prevention. J Local Global Health Sci 2013; 2013: 1. [Google Scholar]
- 11. Koyuncu T, Unsal A, Arslantas D. Evaluation of the effectiveness of health education on menopause symptoms and knowledge and attitude in terms of menopause. J Epidemiol Glob Health 2018; 8(1–2): 8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Department for Education. Statutory guidance: relationships education. Relationships and Sex Education (RSE) and Health Education [Internet]. GOV.UK, 2019, https://www.gov.uk/government/publications/relationships-education-relationships-and-sex-education-rse-and-health-education/relationships-and-sex-education-rse-secondary
- 13. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology 2006; 3(2): 77–101. [Google Scholar]
- 14. Atkinson C, Beck V, Brewis J, et al. Menopause and the workplace: new directions in HRM research and HR practice. Human Resource Management Journal 2021; 31(1): 49–64. [Google Scholar]
- 15. Herbert D, Bell RJ, Young K, et al. Australian women’s understanding of menopause and its consequences: a qualitative study. Climacteric 2020; 23(6): 622–628. [DOI] [PubMed] [Google Scholar]
- 16. Jin F, Tao M, Teng Y, et al. Knowledge and attitude towards menopause and hormone replacement therapy in Chinese women. Gynecol Obstet Invest 2015; 79(1): 40–45. [DOI] [PubMed] [Google Scholar]
- 17. Larroy C, Marin Martin C, Lopez-Picado A, et al. The impact of perimenopausal symptomatology, sociodemographic status and knowledge of menopause on women’s quality of life. Arch Gynecol Obstet 2020; 301(4): 1061–1068. [DOI] [PubMed] [Google Scholar]
- 18. Heinemann K, Ruebig A, Potthoff P, et al. The Menopause Rating Scale (MRS) scale: a methodological review. Health Qual Life Out 2004; 2(1): 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hunter M, O’Dea I. An evaluation of a health education intervention for mid-aged women: five year follow-up of effects upon knowledge, impact of menopause and health. Patient Educ Couns 1999; 38(3): 249–255. [DOI] [PubMed] [Google Scholar]
- 20. de Salis I, Owen-Smith A, Donovan JL, et al. Experiencing menopause in the UK: the interrelated narratives of normality, distress, and transformation. J Women Aging 2018; 30(6): 520–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Burger H, Woods NF, Dennerstein L, et al. Nomenclature and endocrinology of menopause and perimenopause. Expert Rev Neurother 2007; 7(11, Suppl.): S35–S43. [DOI] [PubMed] [Google Scholar]
- 22. Utian WH, Schiff I. NAMS-gallup survey on women’s knowledge, information sources, and attitudes to menopause and hormone replacement therapy. Menopause 2018; 25(11): 1172–1179. [DOI] [PubMed] [Google Scholar]
- 23. Sebring JCH. Towards a sociological understanding of medical gaslighting in western health care. Sociol Health Illn 2021; 43: 1951–1964. [DOI] [PubMed] [Google Scholar]
- 24. Hamoda H, Morris E, Marshall M, et al. BMS, RCOG, RCGP, FSRH, FOM and FPH position statement in response to the BMA report ‘challenging the culture on menopause for doctors’ – August 2020. Post Reprod Health 2021; 27(2): 123–125. [DOI] [PubMed] [Google Scholar]
- 25. Kling JM, MacLaughlin KL, Schnatz PF, et al. Menopause management knowledge in postgraduate family medicine, internal medicine, and obstetrics and gynecology residents: a cross-sectional survey. Mayo Clin Proc 2019; 94(2): 242–253. [DOI] [PubMed] [Google Scholar]
- 26. Christianson MS, Washington CI, Stewart KI, et al. Effectiveness of a 2-year menopause medicine curriculum for obstetrics and gynecology residents. Menopause 2016; 23(3): 275–279. [DOI] [PubMed] [Google Scholar]
- 27. British Menopause Society, 2021, https://thebms.org.uk/
- 28. Mander T. Working doctors and their menopause. Post Reprod Health 2020; 26(3): 119. [DOI] [PubMed] [Google Scholar]
- 29. Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the women’s health initiative randomized controlled trial. J Am Med Assoc 2002; 288(3): 321–333. [DOI] [PubMed] [Google Scholar]
- 30. Simon JA, Davis SR, Althof SE, et al. Sexual well-being after menopause: an international menopause society white paper. Climacteric 2018; 21(5): 415–427. [DOI] [PubMed] [Google Scholar]
- 31. Davies SC. Annual Report of the Chief Medical Officer, 2015. ‘The Health of the 51%: Women’. London: Department of Health, 2015. [Google Scholar]
- 32. Menopause café, https://www.menopausecafe.net/
- 33. Office of National Statistics, 2018, https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/employmentandemployeetypes/bulletins/uklabourmarket/september2018
- 34. Faculty of Occupational Medicine, 2021, http://www.fom.ac.uk/health-at-work-2/information-for-employers/dealing-with-health-problems-in-the-workplace/advice-on-the-menopause
- 35. Menopause in the workplace, 2021, https://menopauseintheworkplace.co.uk/menopause-at-work/menopause-and-work-its-important/
- 36. Women’s Health Strategy, 2020, https://www.gov.uk/government/publications/our-vision-for-the-womens-health-strategy-for-england
- 37. Our visions for the women’s health strategy for England, 2021, https://www.gov.uk/government/publications/our-vision-for-the-womens-health-strategy-for-england/our-vision-for-the-womens-health-strategy-for-england
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-whe-10.1177_17455057221106890 for An online survey of perimenopausal women to determine their attitudes and knowledge of the menopause by Joyce C Harper, Samantha Phillips, Rina Biswakarma, Ephia Yasmin, Ertan Saridogan, Sheila Radhakrishnan, Melanie C Davies and Vikram Talaulikar in Women’s Health