Abstract
Given the global increase in air pollution and its crucial role in human health, as well as the steep rise in prevalence of metabolic syndrome (MetS), a better understanding of the underlying mechanisms by which environmental pollution may influence MetS is imperative. Exposure to air pollution is known to impact DNA methylation, which in turn may affect human health. This paper comprehensively reviews the evidence for the hypothesis that the effect of air pollution on the MetS is mediated by DNA methylation in blood. First, we present a summary of the impact of air pollution on metabolic dysregulation, including the components of MetS, i.e., disorders in blood glucose, lipid profile, blood pressure, and obesity. Then, we provide evidence on the relation between air pollution and endothelial dysfunction as one possible mechanism underlying the relation between air pollution and MetS. Subsequently, we review the evidence that air pollution (PM, ozone, NO2 and PAHs) influences DNA methylation. Finally, we summarize association studies between DNA methylation and MetS. Integration of current evidence supports our hypothesis that methylation may partly mediate the effect of air pollution on MetS.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13148-022-01301-y.
Keywords: Epigenetics, DNA methylation, Metabolic syndrome, Air pollution
Background
Air pollution is a well-known health problem worldwide leading to increased morbidity and mortality [1]. Air pollution has been associated with several human diseases including metabolic disorders [1]. While the association between air pollution and metabolic syndrome (MetS) is well established, the exact underlying mechanism(s) explaining this relation remains to be elucidated. Here, we review the associations between air pollution and MetS-related traits, between air pollution and DNA methylation, and between DNA methylation and MetS (Additional file 1: Table S1). Finally, we integrate the evidence and propose that DNA methylation potentially mediates the effect of air pollution on MetS.
Measurement of air pollution
Six popular air pollutants are known as ‘criteria air pollutants’ including ozone (O3), particulate matter (PM), carbon monoxide (CO), sulfur dioxide (SO2), lead, and nitrogen dioxide (NO2) (Table 1). The air quality index (AQI) is based on daily measurement of all criteria pollutants except lead. Most methods for measurement of gaseous air pollutants use in situ continuous monitors for hourly averaged concentrations. PMs are typically measured using combined sampling systems over a 24-h period with defined inlets, pumps, sampler surfaces, etc. (Additional file 1: Table S2) [2]. Polycyclic aromatic hydrocarbons (PAHs) are another group of chemicals widely distributed in the atmosphere that also constitute an important source of air pollution (Table 1). PAHs are ubiquitous environmental pollutants that are formed during the incomplete burning of coal, oil, gas, and tobacco. PAHs generated from these sources can bind to or form small particles in the air [3].
Table 1.
Major sources of ambient air pollutants
| Pollutant | Major sources |
|---|---|
| Ozone (O3) | Formed from nitrogen oxide species and volatile organic compounds by human activities (largely the combustion of fossil fuel) |
| Particulate matter (PM) | Naturally occurring, originates from volcanoes, dust storms, forest and grassland fires, living vegetation, and sea spray. Human activities, such as the burning of fossil fuels in vehicles, power plants, and various industrial processes also generate significant amounts of aerosols |
| Carbon monoxide (CO) | Is a product of fuel combustion such as natural gas, coal, or wood. Vehicular exhaust contributes to the majority of carbon monoxide in the atmosphere |
| Sulfur dioxide (SO2) | Is produced by volcanoes and in industrial processes. Combustion of coal and petroleum generates sulfur dioxide, as they often contain sulfur compounds |
| Lead | Ore and metals processing and piston engine aircraft operating on leaded aviation fuel. Other sources include waste incinerators, utilities, and lead–acid battery manufacturers. The highest lead concentration in air is usually found near lead smelters |
| Nitrogen dioxide (NO2) | Nitrogen dioxide is expelled from high-temperature combustion and is also produced during thunderstorms by electric discharge |
| Polycyclic aromatic hydrocarbons (PAHs) | Are formed during the incomplete burning of coal, oil, gas, and tobacco |
Data retrieved from Wikipedia and United States Environmental Protection Agency Web site (www.epa.gov)
The International Agency for Research on Cancer (IARC) Working Group on the Evaluation of Carcinogenic Risk to Humans has provided a complete list of methods for the measurement of air pollutants [4]. There are a number of challenges and concerns related to exposure assessment for ambient air pollution in general and actual PM exposure specifically, especially in regions where there is little air quality monitoring. In large-scale epidemiological studies of PM and health, ambient fixed-location monitors are used to assign exposure. Then, the associations with different health outcomes are estimated using single-pollutant regression models. While this approach provides a general framework for estimating associations between air pollution and health, ambient monitors are often sparse and some of them do not provide daily measurement. Also, there might be some instrument or sampling errors. In order to enrich the limited data, integrative techniques such as the Data Integration Model for Air Quality (DIMAQ) have been developed, which provide estimates of exposures to PM2.5 at a high resolution. This method incorporates different data sources including ground measurements, satellite remote sensing, population estimates, topography, and information on local monitoring networks and measures of specific air pollution indices from chemical transport models. Dedicated methods for estimating exposure–risk relationships such as the integrated exposure–response function (IER) have been developed, which estimates the relative risk for a disease caused by air pollution exposure from PM2.5 [5, 6].
Air pollution as a global health problem
Air pollution has become a global health problem. The World Health Organization Global Burden of Disease (GBD) Comparative Risk Assessment study estimates the burden of disease attributable to air pollution in terms of deaths and disability-adjusted life years (DALY). The GBD Study from 2015 [7] reports ambient PM2.5 (particulate matter with a diameter ≤ 2.5 μm) as the fifth-ranking mortality risk factor in 2015, which amounts to about 4.2 million deaths, and 103.1 million DALYs in 2015 and it found an increasing trend of deaths attributable to ambient PM2.5 from 1990 to 2015. This could be because of rising levels of pollution and increasing number of deaths from non-communicable disease (NCDs) in the largest low-income and middle-income countries with growing populations. Except the two recent years being impacted by COVID-19 lockdown, increasing air pollution since 2016 has been reported in many countries [8–10] (Fig. 1). Moreover, WHO reports that 91% of the global population live in places exceeding air quality guidelines. Mortality and morbidity are mostly related to cardiovascular and respiratory outcomes [7–11]. To further investigate AP attributable mortality, we retrieved the AP attributable death rate per cause from WHO Global Health Observatory (data were available for 2016), alongside with their air quality using the PM2.5 index (in the same year, i.e., 2016, from the same database). AP attributable death rates for the top five countries with the highest PM2.5 index are given in Table 2. GBD Study 2015 also ranks ambient ozone as the 34th risk factor for global deaths and 42nd risk factor for DALYs which amounts to causing 254,000 deaths globally and a loss of 4.1 million DALYs in 2015.
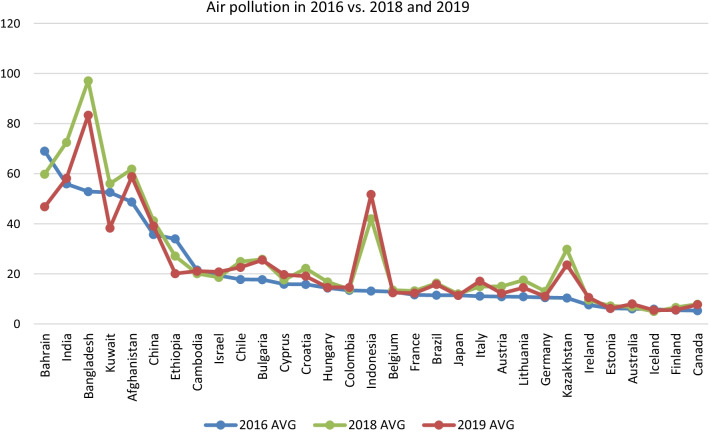
Fig. 1.
Average air pollution (PM2.5) across 31 countries where data were available for all three time spots of 2016, 2018, and 2019. WHO GHO repository (https://www.who.int/data/gho/data/indicators/indicator-details/GHO/concentrations-of-fine-particulate-matter-(pm2-5)) and IQair Web site (https://www.iqair.com) are used to retrieve average air quality indices (AVG). P values of one-tailed paired T tests for 2016 vs. 2018, and 2019 measures were 0.0028 and 0.067, respectively
Table 2.
Ambient air pollution attributable death rate by cause (per 100,000 population, age-standardized) for top 5 polluted regions in 2016 (based on PM2.5 concentration in ug/m3), where WHO data were available for both PM2.5 and outcomes
| Location | PM2.5 | COPD | Trachea, bronchus, lung cancers | Lower respiratory infections | Stroke | IHD | Total |
|---|---|---|---|---|---|---|---|
| Niger | 93.18 | 10.96 | 0.22 | 58.26 | 20.59 | 34.95 | 125 |
| Nepal | 81.57 | 28.88 | 4.39 | 19.67 | 17.41 | 42.01 | 112.4 |
| Qatar | 80.8 | 3.13 | 3.39 | 4.05 | 4.12 | 31.7 | 46.4 |
| Mauritania | 74.13 | 6.73 | 0.28 | 35.95 | 13.55 | 31.63 | 88.15 |
| Egypt | 72.31 | 10.2 | 2.3 | 11.25 | 19.38 | 61.9 | 105 |
Data are retrieved from Global Health Observatory (GHO)—WHO, 2016. PM2.5: particulate matter with a diameter ≤ 2.5 μm; COPD: chronic obstructive pulmonary disease; IHD: ischemic heart disease
Air pollution and metabolic syndrome
MetS is characterized by the clustering of cardiometabolic risk factors. There are different definitions of MetS most of which are quite similar apart from some differences in the cutoffs of the components. The shared feature of all definitions is that MetS is considered as the coexistence of at least three out of five components including abdominal obesity, disorders in fasting blood glucose, triglycerides, blood pressure, and HDL cholesterol [12, 13]. MetS is a known predisposing factor for a number of chronic, non-communicable diseases of which type 2 diabetes and cardiovascular diseases are the most important [14]. As such MetS is an important public health concern. Several predisposing factors are shown to modify the risk of MetS, including (but not limited to) genetic factors, diet, physical activity, smoking, education, age, sex, race, ethnicity, socioeconomic status, and urban-versus-rural residence [15]. Hence, like any other complex trait, MetS is a consequence of both genetic and environmental factors such as air pollution, and their complex interaction [16]. Several lines of evidence indicate that exposure to air pollutants has a crucial role in the development and progress of MetS both in adults and in children [17–19]. One potential consideration in cross-sectional association studies of air pollution and MetS is the possible confounding effect of socioeconomic status. Like MetS, air pollution exposure may also relate in part to socioeconomic status. However, studies on this relationship are not conclusive [20, 21]. There is some evidence of a nonlinear relationship between air pollution and MetS, where socioeconomic status seems to intensify the association, but does not explain it entirely [22, 23]. However, longitudinal studies in which air pollution exposure precedes MetS occurrence without any significant individual changes in socioeconomic status during follow up strengthen the hypothesis [24, 25]. A narrative review in firefighters showed association of air pollutants and MetS in World Trade Center (WTC)-exposed Fire Department of New York. This study found that exposure to particulate matter provokes pulmonary and systemic inflammation. Systemic inflammation leads to the development of MetS and cardiopulmonary disease, such as chronic obstructive pulmonary disease and cardiovascular disease. Individuals with these conditions are more susceptible to the inflammatory effects of PM exposure, which can aggravate their conditions [26].
Some cross-sectional studies in adults documented that exposure to ambient air pollutants is independently associated with risk of MetS and related chronic diseases [27, 28]. The observed associations between air pollution exposure and MetS were sensitive to MetS definitions. Regarding the MetS components, strongest associations were observed with impaired fasting glycemia, and positive but weaker associations with hypertension and waist-circumference-based obesity. Cardiometabolic effects of air pollution may be majorly driven by impairment of glucose homeostasis and, to a lesser extent, visceral adiposity [28]. In a nationwide study on 1,413 children with a mean (SD) age of 14.81 (2.48) years, we showed that those living in areas with higher air pollution had higher levels of MetS components including increased systolic blood pressure, fasting blood glucose, and triglycerides, as well as lower levels of HDL-C. The results remained significant even after adjustment for confounding factors including age, sex, and anthropometric measures, as well as for dietary and physical activity habits [29]. In a previous study, we have shown that exposure to air pollutants increases the risk of underlying MetS components [17] which is in line with longitudinal studies [15]. Additionally, we have recently shown for the first time that independent of weight status, exposure of children to PAHs is significantly associated with two components of MetS, namely triglycerides and fasting blood glucose. This study can partly explain, why not all obese persons have a higher risk for all MetS components, and why some normal-weight individuals do show these risk factors. Hence, this study provided confirmatory evidence of the role of exposure to air pollutants in the development of MetS and its components [30]. In this review, we will take a closer look at the association of air pollution with MetS and will explore possible mechanisms explaining this association.
Putative mediating mechanisms of air pollution exposure in the pathogenesis of MetS
Endothelial dysfunction, a systemic pathological state of the inner lining of blood vessels, is one of the contributors of the complex pathophysiology of MetS [16, 30]. The condition is defined as an imbalance between vasodilating and vasoconstricting substances acting on the endothelium. Endothelial dysfunction can be measured by its serum markers such as endothelin-1, vascular adhesion molecule, and intercellular adhesion molecule. It is also assessed by measuring flow-mediated dilation of the brachial artery by ultrasound [31].
We and others have shown that endothelial dysfunction is associated with air pollution [32–34]. Our study showed that healthy children and adolescents with higher exposure to air pollutants, notably PM, had higher levels of markers of endothelial dysfunction and a possible pro-coagulant state [32]. In another study on prepubescent boys, we found that living in air-polluted areas was significantly associated with attenuated endothelium-dependent brachial artery dilation, i.e., a known marker of endothelial dysfunction [35]. In both the above-mentioned studies, we noticed that the association of air pollutants with markers of endothelial dysfunction was independent of weight status or lifestyle of participants.
In a population-based cohort of 233 mother–neonate pairs, we found that exposure to ambient air pollution during pregnancy was associated with cord blood concentrations of surrogate markers of endothelial dysfunction including endothelin-1, vascular adhesion molecule, and intercellular adhesion molecule [36]. Collectively, these studies suggest that endothelial dysfunction may be a mediating mechanism between air pollution and MetS.
Another possible mediator of air pollution effects on MetS might be the production of reactive oxygen species (ROS). These agents can affect the methylation–demethylation circuit in the nucleus, by direct modifications of the methylated CpG sites or by altering expression of involved enzymes, which in turn can lead to systemic (mostly hypomethylation) and locus-specific epigenetic changes in DNA [1]. The interplay of the air pollution-induced ROS reagents with inflammation [34, 37, 38] can lead to a variety of pathologic conditions including MetS components such as dyslipidemia and glucose intolerance [37].
Epigenomics—DNA methylation
Epigenetics is a field that investigates alterations in the DNA molecule that do not change the DNA sequence, but that can lead to differences in gene expression levels and hence variations in health outcomes [39–41]. Epigenetic processes mainly include histone modifications and DNA methylation. DNA methylation in blood is the most widely investigated epigenetic factor [42] on which we will focus in this review. DNA methylation is a chemical modification of DNA through the addition of a methyl group to the DNA molecule, which mainly happens at cytosine–guanine dinucleotide (CpG) sites [43, 44]. Modification of DNA methylation at the promoter region of the gene will typically lead to changes in gene expression. That is why the study of alterations in DNA methylation is important in understanding complex mechanisms underlying multifactorial diseases and traits [45, 46].
DNA methylation analyses of the candidate genes are hypothesis-based investigations of the association between DNA methylation of a gene and a particular trait or disease. Although this is an appropriate design and requires smaller sample sizes than genome-wide studies, there are criticisms about the possibility of false positives and hence, poor replication of the results of such studies (also called type I error). Thanks to reductions in costs and availability of microarray technology, genome-wide investigations of DNA methylation markers are now possible. The hypothesis-free experimental design of epigenome-wide association study (EWAS) has been applied during the past few years to unravel epigenomic (i.e., DNA methylation) alterations underlying complex traits and diseases. The first genome-wide methylation array was the Illumina Infinium HumanMethylation27K BeadChip [47]. However, most EWAS studies so far have applied the Illumina Infinium HumanMethylation450K BeadChip array for their DNA methylation profiling. The latter measures the methylation levels of over 485,000 CpG sites per genome. The most recent methylation array covers over 850,000 methylation sites per sample and, given sufficient sample sizes to avoid false-negative results (type II error), promises a new wave of successful EWAS studies with better resolution of the results [48].
Modification of DNA methylation by air pollution
DNA methylation is influenced by both environmental and genetic factors. It has been documented that DNA methylation alterations are resulting from a wide range of different environmental exposures such as smoking, physical activity, stress, diet, and toxins [49–55]. Thus, the epigenome is increasingly being proposed as a vital link between environmental exposures and gene expression modifications. A growing body of evidence now shows that air pollution influences DNA methylation [56–64].
Rossnerova et al. compared the methylation profiles in 200 blood samples of children from two regions with different levels of air pollution. Air pollution measurement was performed by the Czech Hydrometeorological Institute in a highly polluted region and a control region in the Czech Republic. Using the Human Methylation 27 K BeadChip with 27,578 CpG sites, they found ~ 36% (9,916) of CpG sites had significantly different methylation levels. A total of 58 out of 9,916 CpG sites had > 10% lower methylation levels in children from polluted area, associated with higher gene expression in comparison with the control region in the children from the polluted region compared to the children from the control region [65].
Below, we review the available evidence for the association of a number of specific air pollutants with DNA methylation, namely PM, O3, NO2, and PAH.
Particulate matter and DNA methylation
Particulate matter (PM) constitutes a complex mixture of very small particles and liquid droplets that get into the air. These small particles, regardless of their chemical composition, can cause serious health effects as they can pass biological barriers. Airborne PM may induce epigenetic changes. Several studies have linked short- and mid-term PM exposure to global and gene-specific DNA methylation [66–72]. Some studies found that exposure to PM2.5 may affect DNA methylation of certain candidate genes related to coagulation and inflammation [73–78]. Likewise, a randomized, double-blind crossover trial showed that short-term exposure to PM2.5 was associated with rapid global DNA hypomethylation [68]. A recent EWAS on 2,956 participants from three cohorts of European ancestry studied the association between DNA methylation and cumulative PM2.5 exposure averaged over 2 days up to 4 weeks using the Illumina 450 k BeadChip [79]. Applying a stringent genome-wide Bonferroni significance level (p ≤ 7.5E−8), revealed 12 CpG sites (ACVR2B-AS1, ACYP2, C1orf212, F2, MN1, MSGN1, NEURL4, NSMAF, NXN, SERBP1, TSPYL6, and ZMIZ1). Applying a more lenient false discovery rate significance level increased the number of associated CpG sites to more than 1,800. Although the results still need replication in an independent study population, this study provides evidence of the effect of PM2.5 pollution on DNA methylation. Based on the identified CpG sites, this study suggests biological pathways that might mediate associations between PM2.5 and health outcomes such as glucose metabolism [79]. A later EWAS on 646 participants using the Illumina 450 k BeadChip array showed that long-term exposures to some PM2.5 species (Fe, Ni, V), mostly combustion emitted particles, were associated with alterations in DNA methylation in immune response genes. In this study, 20 Bonferroni significant (P value < 9.4 × 10–9) CpGs were found for Fe, 8 for Ni, and 1 for V [80].
In addition to PM2.5, several lines of evidence show PM10 (particulate matter ≤ 10 μm) is associated with DNA methylation of some candidate genes related to cardiovascular and respiratory diseases as well as inflammatory immune responses and oxidative stress [51, 61, 74, 81]. A recent EWAS provides evidence for association of PM10 exposure and altered DNA methylation of multiple loci [81]. Moreover, animal studies have also investigated the effects of particulate matter on DNA methylation [58, 72], but the focus of this review is mostly on human studies.
Ozone and DNA methylation
Ozone (O3) is created by chemical reactions between oxides of nitrogen (NOx) and volatile organic compounds in the presence of sunlight. There is evidence that ozone air pollution is associated with global DNA methylation and interferon gamma (IFN-γ) hyper-methylation, as well as its protein level [82]. IFN-γ has an important role in immune responses to a foreign compound. Ozone exposures (2–4 weeks) were also negatively related to intercellular adhesion molecule 1 (ICAM-1) methylation [75].
Another study showed that acute exposure to ambient ozone was associated with higher blood pressure and with increased serum levels of angiotensin-converting enzyme (ACE) and endothelin-1 (ET-1) as biomarkers of blood pressure. Results of this study supported an instant hypomethylation response of the ACE and EDN1 genes due to ozone exposure, but there was no significant mediation of DNA methylation in the effects of ozone on blood pressure [83].
NO2 and DNA methylation
Nitrogen dioxide (NO2) is formed and released into the air from burning of fuel, for example from car emissions, and is related to a wide range of adverse health effects [84]. A recent study shows that short-term exposure to NO2 is associated with DNA methylation of two respiratory function related genes, i.e., arginase (ARG2) hypermethylation and inducible nitric oxide synthase (NOS2A) hypomethylation [85].
A recent large-scale EWAS on 1508 newborns from four European and North American birth cohort studies investigated the association between maternal NO2 exposure during pregnancy and DNA methylation in newborns using the Illumina 450 k BeadChip. Three CpG sites in mitochondria-related genes (LONP1, HIBADH, and SLC25A28) became significant after correcting for multiple testing (FDR < 0.05) [86]. In another more recent large-scale EWAS on 1,017 subjects from the Lifelines cohort study using the Illumina 450 k BeadChip, significant associations were found between long-term NO2 exposure and DNA methylation for seven CpG sites (Bonferroni-corrected threshold p < 1.19 × 10−7) or for 4980 CpG sites (FDR < 0.05). Furthermore, two Bonferroni-corrected significant CpG sites significantly mediated the association between NO2 and lung function [87].
A recent EWAS investigating whether NO2 during pregnancy is associated with differences in placental DNA methylation levels showed that methylation level of 2 CpGs located in the ADORA2B gene, whose expression is associated with hypoxia and pre-eclampsia, were significantly associated with NO2 exposure during the pregnancy (FDR < 0.05) [88]. These two studies show that maternal exposure to air pollution can lead to modification of DNA methylation patterns—and potential adverse health outcomes—in the offspring.
Another EWAS in a Korean chronic obstructive pulmonary disease cohort investigated association with long-term ambient air pollution exposure and found 45 CpGs related to NO2 (FDR < 0.05). Enriched networks based on these results were related to outcomes associated with air pollution such as cardiovascular and respiratory diseases as well as inflammatory and immune responses [81].
PAHs and DNA methylation
PAHs are highly lipid soluble and could have a role in obesity and development of MetS and its components [30, 89]. These chemicals can form or bind to small particles in the air. Exposure to PAHs might have epigenetic effects so that DNA methylation is considered to provide a novel marker of the environmental impact of PAH exposure on gene function [90]. Several lines of evidence showed an association of PAHs and DNA methylation in both global methylation and candidate genes studies [90–94]. Moreover, a recent study using the 450 k array reported the association of PAHs with an epigenetic predictor of accelerated aging [95].
Methylation and its effect on MetS
It is believed that chronic diseases are complex consequences of long-term exposures to risk factors before clinical onset of the diseases. According to the Developmental Origins of Health and Disease (DOHaD) hypothesis, intrauterine or postnatal adaptations to adverse environmental exposures might cause several physiologic or metabolic alterations affecting health later in life. This hypothesis proposes an association of suboptimal intrauterine development with risk of chronic disorders, including MetS, in adult life [64, 96–98]. The mechanisms through which fetal programming as well as early-life exposures may affect physiologic or metabolic status in later life is still to be elucidated, but epigenetic variation may offer a good explanation [99–102]. Epigenetic variation, either early or late in life, may play an important role in the complex interplay between genetic susceptibility and environmental exposures which can eventually result in metabolic alterations. In a comparison between normal infants and those with intrauterine growth restriction (IUGR), Williams et al. reported a global shift toward hypermethylation in IUGR infants [103]. In a recent meta-analysis of EWASs totaling 8825 neonates from 24 birth cohorts in the PACE (Pregnancy And Childhood Epigenetics) Consortium, we found that DNA methylation in neonatal blood is genome-wide significantly associated with birthweight at 914 sites, with a difference in birthweight ranging from −183 to 178 g per 10% increase in methylation [102].
A growing body of evidence supports the role of methylation changes in metabolic dysregulation including MetS [66, 104]. A review on the subject concluded that modifications in DNA methylation may contribute to MetS susceptibility [42]. Epigenetics could have a role in affecting obesity and cardiometabolic diseases, by activating or silencing the relevant genes. Scientific evidence has suggested that LINE-1 methylation is associated with obesity-related diseases, as well as insulin resistance, type 2 diabetes mellitus, and cardiovascular disease [105]. A recent epigenome-wide study in African-American adults with high prevalence of MetS showed that MetS was consistently associated with increased methylation in the ABCG1 gene [106]. Other epigenome-wide investigations showed methylation sites associated with components of MetS, including central obesity, insulin responsiveness, and type 2 diabetes, as well as lipid profiles in different populations [107–109].
Elevated blood pressure is another component of MetS. An early pilot study conducted by us already showed difference in a single blood leukocyte DNA methylation site between hypertensives and controls [70]. In a more recent study, the CHARGE (Cohorts for Heart and Aging Research in Genomic Epidemiology) consortium conducted a meta-analysis of EWASs investigating cross-sectional associations with systolic and diastolic blood pressure and found 13 CpGs replicated after Bonferroni correction. In a later study, they found and cross-validated 34 CpG sites for blood pressure using two large datasets of over 4000 and 17,000 individuals. Six of the identified CpG sites also showed significant association (FDR < 0.05) with gene expression (PHGDH, ABCG1, LMNA, RBPMS2, and SLC1A5). Further investigation of these CpG sites in a meta-analysis of twin cohorts suggested that the majority of correlation between DNA methylation and blood pressure can be explained by shared environmental factors. Findings of these studies showed that heritable DNA methylation may play a role in regulating blood pressure [110, 111].
Recently, we performed a systematic review and replication to test the association between DNA methylation and glycemic traits including type 2 diabetes. We showed that a number of EWAS signals of type 2 diabetes in the literature can be significantly replicated providing confidence in the association between DNA methylation and type 2 diabetes [112]. Moreover, a number of recent EWASs of obesity-related traits provide convincing evidence for association with DNA methylation at numerous CpG sites [113–116]. However, the direction of association has been a matter of debate. Although Wahl et al. report changes in DNA methylation at 187 genetic loci to be associated with BMI, their analyses indicate that DNA methylation changes are more likely the effect of obesity rather than the cause [115].
In animal studies, increasing the diversity of environmental interventions in the study of metabolic health will provide a more complete picture of the interactions between environment, epigenetic and genetic background, and metabolic health. Both global and locus-specific differential DNA methylation have been observed in rodent models of metabolic syndrome [117].
DNA methylation may mediate the effect of air pollution on MetS
MetS is one of the major challenges worldwide. The association between MetS and air pollution is of great concern. Epigenetic modifications, including DNA methylation, have been identified as one mechanism by which the environment interacts with the genome with alterations in DNA methylation potentially contributing to the development of metabolic diseases [118, 119].
A systematic review of studies in children concluded that exposure to environmental pollutants may have an important role in the origin of various disorders including MetS. Environmental pollutants trigger epigenetic imbalances, which may lead to increasing risk of MetS [50]. The epigenome is increasingly being proposed as a vital link between environmental exposures and gene expression modifications [120]. Epigenetic markers can be modified by environmental factors and may constitute an underlying biological mechanism affecting an individual's predisposition to almost all MetS components [121].
A recent, large epigenome-wide meta-analysis across 13 cohorts of the PACE consortium showed the effect of maternal exposure to tobacco smoke on newborn DNA methylation [31]. In an earlier study, we further showed that DNA methylation may mediate the effect of maternal smoking on the birth weight of the neonate. DNA methylation of only a few CpG sites explained 12–19% of the lower birth weight of the neonate of smoking mothers [122]. The mediating effect of DNA methylation between air pollution and cardiovascular phenotypes such as carotid intima–media thickness and blood pressure has been reported [123]. Besides, there is evidence that the effect of ambient air pollutants on blood glucose might be mediated by DNA methylation [69] and that there is a mediating effect of DNA methylation on other human complex traits such as inflammation and thrombosis [75] and neurodevelopmental disorders [124].
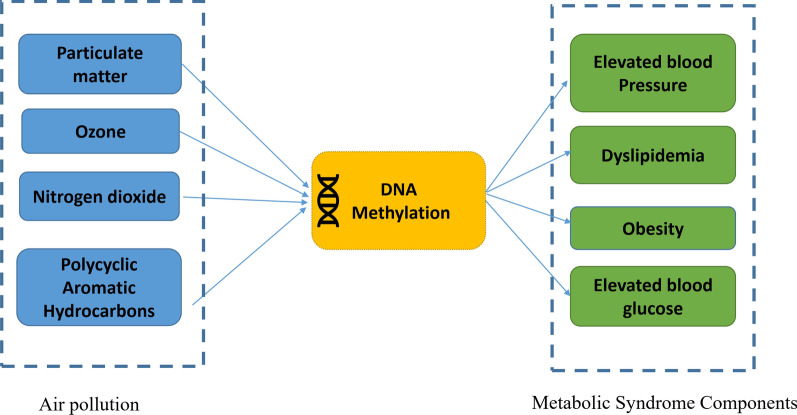
Based on the combined evidence presented, we propose that alterations in DNA methylation may mediate adverse effects of environmental pollutants on MetS and its components (Fig. 2). We also summarized the overlapping genes reported in independent epigenetic studies of air pollution and MetS components in Additional file 1: Table S3. The direction of effects seems to be supportive of our main hypothesis, as for most of the sites (98%) consistent direction of association of DNA methylation with air pollution and MetS is observed. Thus, DNA methylation could play an important role as an underlying explanatory mechanism. A few locus-specific example mechanisms from Additional file 1: Table S3 are discussed below:
Fig. 2.
Hypothetical paths that might link criteria air pollutants exposures we discussed here to metabolic syndrome components through DNA methylation
Air pollution, including NO2 and PM, affects DNA methylation at the NXN gene, at which DNA methylation is also associated with obesity, glucose level, and blood pressure. This gene encodes nucleoredoxin, a regulator of Wnt signaling pathway and in utero embryonic development [125, 126]. Whether the mediating role of epigenetics occurs through effects on the embryonic environment and metabolic dysregulation proceeds with embryonic development is to be elucidated by further longitudinal studies. NO2 and PM also affect DNA methylation at the protein kinase C zeta gene (PRKCZ), at which differential methylation is also associated with obesity and fasting glucose levels. The involvement of this protein in the insulin signaling pathway [127] may describe another mechanism by which air pollution affects metabolic dysregulation, through epigenetic modifications. Another differentially methylated gene in relation to NO2 exposure is zinc finger MIZ domain-containing protein 1 (ZMIZ1), which is involved in androgen receptor signaling. This pathway has been studied in the context of sex differences in lipid profile and blood pressure [128–130]. Epigenetic regulation of this pathway may explain another mechanism by which air pollution affects metabolic complications.
Our study highlights the need and potential for large-scale genome-wide consortium meta-analysis on human samples with air pollution measures, DNA methylation levels, and MetS components being measured on the same samples preferably in the context of a prospective cohort design. Alternatively, there are large amounts of summary-level results available from very large-scale EWASs and air pollution measures and MetS components. One may think of integrating summary-level data from independent EWAS, gene expression studies, and epidemiologic studies to test the mediating effect of DNA methylation on the link between air pollution and MetS. Such analyses are based on summary-level results from large-scale epidemiological studies and hence may provide sufficient power to detect subtle mediating effects. However, methodological issues should be carefully considered [75, 120, 124]. Obviously, statistical significance is not equivalent to causality. An increasingly popular approach, Mendelian Randomization, uses genetically informed instrumental variables (IVs) to test whether the association of two traits is due to real causation. Mendelian Randomization may be extended to the field of epigenomics to dig into the causality of the associations [131]. While the statistical links between air pollution and MetS-related disorders, between air pollution and DNA methylation, and between DNA methylation and MetS have separately been established, here we integrated the evidence suggesting that the link between air pollution and Mets may be partly explained by DNA methylation. This sheds light on the design and conduct of future epidemiological and laboratory studies aiming to prevent MetS and its tragic consequences. This review provides evidence for the mediating role of DNA methylation explaining the effects of air pollution on the development of MetS. Further studies are necessary to provide the clinical impact of these associations.
Epigenomics—beyond DNA methylation
Beyond DNA methylation, epigenetic regulation also includes histone modifications [132]. Upon the type and site of modification, this will lead to a decrease or increase in their nearby gene’s expression [133]. There is evidence of air pollution-induced histone modifications [134, 135], some of which are also observed in metabolic syndrome versus health [133, 136]. Studying these epigenetic marks together with their interplay with non-protein coding RNA transcripts (ncRNAs) will elucidate mediatory mechanisms from air pollution to metabolic syndrome [137]. Additional file 1: Table S3 is also suggestive of such interplay, where many ncRNA genes are among targets of DNA methylation in air pollution and MetS. Further research is required to elucidate the possible mediatory role of these mechanisms in linking air pollution to MetS, which is beyond the scope of this article.
Limitations of the current state of the science
The available evidence on environment–methylation–disease patterns is mostly derived from blood methylation investigations. This choice of preferred tissue may be reasonable as typical exposure routes for air pollution are from inhalation, ingestion, and dermal exposure. However, one of the limitations of epigenetic investigations is the unavailability of data from disease/exposure-relevant tissues. On the other side, the tissue-specific pathogenesis of metabolic syndrome remains debated. When clarified and with increased availability of tissue-specific epigenetic data, deeper investigations of tissue-specific effects will be worthwhile.
Future perspectives
Since there is no known level of air pollution exposure that is risk free, strategies to lessen daily exposures can always be effective. Global awareness of air pollution is increasing, and it is necessary to provide recommendations for reducing air pollution levels as well as human exposure to it. Public policy has a key role in reducing air pollution, and exposures can be mitigated by providing education to the community and support people to limit their exposure to harmful levels of air pollution. Recommendations in this regard include using filtering face masks, shifting from car and public transport to active transport, i.e., cycling or walking, maintaining vehicle ventilation, and avoiding rapid accelerations and decelerations. Moreover, household air pollution should be considered. Household exposure could be minimized by using clean fuels, enhancing household ventilation, and using efficient cookstoves [138–140].
In terms of epigenetic research, longitudinal measurements of DNA methylation alongside with different health outcomes could provide beneficial and informative resources [141]. Comparative analysis of methylation changes due to air pollution and/or other lifestyle habits can be of help. Moreover, it is essential to improve our understanding of the molecular mechanisms which mediate the effect of the environmental exposure on NCD prevalence and incidence. To ascertain the mediating molecular mechanisms from air pollution to MetS, a first step would be to investigate whether methylation alterations, in methylation regions that overlap between air pollution and MetS, result in actual changes in gene expression and corresponding protein levels. Then, we need to examine if these alterations eventually yield MetS or its components. The best strategy would be to study all three data levels of air pollution, DNA methylation, and MetS (components) in a single population, though integrative studies on different data levels could also provide clues to potential mechanisms by which different kinds of air pollutants contribute to morbidity and mortality. At the intervention side, assuming ROS causes epigenetic changes due to air pollution exposure, antioxidants and carotenoids can potentially reduce the harmful effects of air pollution on global epigenetic changes which leads to MetS and other types of diseases. Vitamin B supplementation is also observed to attenuate air pollution-induced epigenetic changes [1]. Targeted interventions based on air pollution-induced epigenetic modifications require a more complete and robust knowledge of the impacted loci and subsequently involved mechanisms.
Conclusions
Current evidence supports the possible mediation of air pollution effects on metabolic syndrome by epigenetic regulation. This warrants further research to investigate the causality of associations with DNA methylation and the biological mechanisms involved.
Supplementary Information
Additional file 1. Supplementary Tables 1–3.
Acknowledgements
Not applicable.
Abbreviations
- ACE
Angiotensin-converting enzyme
- AQI
Air quality index
- ARG2
Arginase
- CHARGE
Cohorts for Heart and Aging Research in Genomic Epidemiology
- CO
Carbon monoxide
- CpG
Cytosine–guanine dinucleotide
- DALY
Deaths and disability-adjusted life years
- DOHaD
Developmental Origins of Health and Disease
- ET-1
Endothelin-1
- EWAS
Epigenome-wide association study
- GBD
Global Burden of Disease
- IARC
International Agency for Research on Cancer
- ICAM-1
Intercellular adhesion molecule 1
- IUGR
Intrauterine growth restriction
- IVs
Instrumental variables
- MetS
Metabolic syndrome
- NCDs
Non-communicable disease
- NO2
Nitrogen dioxide
- NOS2A
Nitric oxide synthase
- O3
Ozone
- PACE
Pregnancy And Childhood Epigenetics
- PAHs
Polycyclic aromatic hydrocarbons
- PM
Particulate matter
- PM2.5
Particulate matter with a diameter ≤ 2.5 μm
- SO2
Sulfur dioxide
Author contributions
All authors wrote and edited the manuscript. All authors read and approved the final manuscript.
Funding
ZK and AV are financially supported by Isfahan University of Medical Sciences, Isfahan, Iran.
Availability of data and materials
All papers reviewed and described in this manuscript are available online in the relevant publications.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors have contributed to this study and approve its submission.
Competing interests
The authors declare that they have no competing interest.
Footnotes
Shared first authors: Parinaz Poursafa and Zoha Kamali.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Professor H. Marike Boezen passed away in October 2021
Contributor Information
Ahmad Vaez, Email: a.vaez@umcg.nl.
Harold Snieder, Email: h.snieder@umcg.nl.
References
- 1.Rider CF, Carlsten C. Air pollution and DNA methylation: effects of exposure in humans. Clin Epigenetics. 2019;11:131. doi: 10.1186/s13148-019-0713-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hall ES, Kaushik SM, Vanderpool RW, Duvall RM, Beaver MR, Long RW, et al. Integrating sensor monitoring technology into the current air pollution regulatory support paradigm: practical considerations. Am J Environ Eng. 2014;4:147–154. [Google Scholar]
- 3.Srogi K. Monitoring of environmental exposure to polycyclic aromatic hydrocarbons: a review. Environ Chem Lett. 2007;5:169–195. doi: 10.1007/s10311-007-0095-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.IARC Working Group on the Evaluation of Carcinogenic Risk to Humans. Outdoor air pollution measurement methods. Outdoor Air Pollut. International Agency for Research on Cancer; 2016 [cited 2021 Oct 21]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK368020/
- 5.Krall JR, Chang HH, Sarnat SE, Peng RD, Waller LA. Current methods and challenges for epidemiological studies of the associations between chemical constituents of particulate matter and health. Curr Environ Health Rep. 2015;2:388–398. doi: 10.1007/s40572-015-0071-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO, GBD Compare. Burden of disease from ambient air pollution for 2016: Description of method. Seattle, WA: IHME, University of Washington: Institute for Health Metrics and Evaluation (IHME); 2018 May. Available from: https://www.who.int/airpollution/data/AAP_BoD_methods_Apr2018_final.pdf
- 7.Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet Lond Engl. 2017;389:1907–1918. doi: 10.1016/S0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clay K, Muller N. Recent Increases in Air Pollution: Evidence and Implications for Mortality. Cambridge, MA 02138: National Bureau of Economic Research; 2019 Oct. Report No.: w26381. Available from: https://www-nber-org.proxy-ub.rug.nl/system/files/working_papers/w26381/w26381.pdf
- 9.Shaddick G, Thomas ML, Mudu P, Ruggeri G, Gumy S. Half the world’s population are exposed to increasing air pollution. Npj Clim Atmospheric Sci. 2020;3:1–5. doi: 10.1038/s41612-019-0105-5. [DOI] [Google Scholar]
- 10.Popovich N. America’s air quality worsens, ending years of gains, study says. N Y Times. 2019 Oct 24 [cited 2021 Oct 21]; Available from: https://www.nytimes.com/interactive/2019/10/24/climate/air-pollution-increase.html
- 11.Tong S. Air pollution and disease burden. Lancet Planet Health. 2019;3:e49–50. doi: 10.1016/S2542-5196(18)30288-2. [DOI] [PubMed] [Google Scholar]
- 12.de Ferranti SD, Gauvreau K, Ludwig DS, Neufeld EJ, Newburger JW, Rifai N. Prevalence of the metabolic syndrome in American adolescents: findings from the Third National Health and Nutrition Examination Survey. Circulation. 2004;110:2494–2497. doi: 10.1161/01.CIR.0000145117.40114.C7. [DOI] [PubMed] [Google Scholar]
- 13.Cook S, Auinger P, Li C, Ford ES. Metabolic syndrome rates in United States adolescents, from the National Health and Nutrition Examination Survey, 1999–2002. J Pediatr. 2008;152:165–170. doi: 10.1016/j.jpeds.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 14.Brambilla P, Lissau I, Flodmark C-E, Moreno LA, Widhalm K, Wabitsch M, et al. Metabolic risk-factor clustering estimation in children: to draw a line across pediatric metabolic syndrome. Int J Obes. 2005;2007(31):591–600. doi: 10.1038/sj.ijo.0803581. [DOI] [PubMed] [Google Scholar]
- 15.Wallwork RS, Colicino E, Zhong J, Kloog I, Coull BA, Vokonas P, et al. Ambient fine particulate matter, outdoor temperature, and risk of metabolic syndrome. Am J Epidemiol. 2017;185:30–39. doi: 10.1093/aje/kww157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flores-Viveros KL, Aguilar-Galarza BA, Ordóñez-Sánchez ML, Anaya-Loyola MA, Moreno-Celis U, Vázquez-Cárdenas P, et al. Contribution of genetic, biochemical and environmental factors on insulin resistance and obesity in Mexican young adults. Obes Res Clin Pract. 2019;13:533–540. doi: 10.1016/j.orcp.2019.10.012. [DOI] [PubMed] [Google Scholar]
- 17.Kelishadi R, Mirghaffari N, Poursafa P, Gidding SS. Lifestyle and environmental factors associated with inflammation, oxidative stress and insulin resistance in children. Atherosclerosis. 2009;203:311–319. doi: 10.1016/j.atherosclerosis.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 18.Jiang S, Bo L, Gong C, Du X, Kan H, Xie Y, et al. Traffic-related air pollution is associated with cardio-metabolic biomarkers in general residents. Int Arch Occup Environ Health. 2016;89:911–921. doi: 10.1007/s00420-016-1129-3. [DOI] [PubMed] [Google Scholar]
- 19.Wei Y, Zhang JJ, Li Z, Gow A, Chung KF, Hu M, et al. Chronic exposure to air pollution particles increases the risk of obesity and metabolic syndrome: findings from a natural experiment in Beijing. FASEB J Off Publ Fed Am Soc Exp Biol. 2016;30:2115–2122. doi: 10.1096/fj.201500142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hajat A, Hsia C, O’Neill MS. Socioeconomic disparities and air pollution exposure: a global review. Curr Environ Health Rep. 2015;2:440–450. doi: 10.1007/s40572-015-0069-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.European Commission. Directorate General for the Environment., University of the West of England (UWE). Science Communication Unit. Links between noise and air pollution and socioeconomic status. LU: Publications Office; 2016 [cited 2022 Apr 15]. Available from: 10.2779/200217
- 22.Jiao K, Xu M, Liu M. Health status and air pollution related socioeconomic concerns in urban China. Int J Equity Health. 2018;17:18. doi: 10.1186/s12939-018-0719-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chi GC, Hajat A, Bird CE, Cullen MR, Griffin BA, Miller KA, et al. Individual and neighborhood socioeconomic status and the association between air pollution and cardiovascular disease. Environ Health Perspect Environ Health Perspect. 2016;124:1840–1847. doi: 10.1289/EHP199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang W, Wang L, Li J, Liu M, Xu H, Liu S, et al. Short-term blood pressure responses to ambient fine particulate matter exposures at the extremes of global air pollution concentrations. Am J Hypertens. 2018;31:590–599. doi: 10.1093/ajh/hpx216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bowe B, Xie Y, Li T, Yan Y, Xian H, Al-Aly Z. The 2016 global and national burden of diabetes mellitus attributable to PM 2·5 air pollution. Lancet Planet Health. 2018;2:e301–e312. doi: 10.1016/S2542-5196(18)30140-2. [DOI] [PubMed] [Google Scholar]
- 26.Clementi EA, Talusan A, Vaidyanathan S, Veerappan A, Mikhail M, Ostrofsky D, et al. Metabolic syndrome and air pollution: a narrative review of their cardiopulmonary effects. Toxics. 2019 [cited 2021 Apr 25];7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6468691/ [DOI] [PMC free article] [PubMed]
- 27.Eze IC, Schaffner E, Foraster M, Imboden M, von Eckardstein A, Gerbase MW, et al. Long-term exposure to ambient air pollution and metabolic syndrome in adults. PLoS ONE. 2015;10:e0130337. doi: 10.1371/journal.pone.0130337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brook RD, Sun Z, Brook JR, Zhao X, Ruan Y, Yan J, et al. Extreme air pollution conditions adversely affect blood pressure and insulin resistance: the air pollution and cardiometabolic disease study. Hypertens Dallas Tex. 1979;2016(67):77–85. doi: 10.1161/HYPERTENSIONAHA.115.06237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Poursafa P, Mansourian M, Motlagh M-E, Ardalan G, Kelishadi R. Is air quality index associated with cardiometabolic risk factors in adolescents? The CASPIAN-III Study. Environ Res. 2014;134:105–109. doi: 10.1016/j.envres.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 30.Poursafa P, Dadvand P, Amin MM, Hajizadeh Y, Ebrahimpour K, Mansourian M, et al. Association of polycyclic aromatic hydrocarbons with cardiometabolic risk factors and obesity in children. Environ Int. 2018;118:203–210. doi: 10.1016/j.envint.2018.05.048. [DOI] [PubMed] [Google Scholar]
- 31.Kapiotis S, Holzer G, Schaller G, Haumer M, Widhalm H, Weghuber D, et al. A proinflammatory state is detectable in obese children and is accompanied by functional and morphological vascular changes. Arterioscler Thromb Vasc Biol. 2006;26:2541–2546. doi: 10.1161/01.ATV.0000245795.08139.70. [DOI] [PubMed] [Google Scholar]
- 32.Poursafa P, Kelishadi R, Lahijanzadeh A, Modaresi M, Javanmard SH, Assari R, et al. The relationship of air pollution and surrogate markers of endothelial dysfunction in a population-based sample of children. BMC Public Health. 2011;11:115. doi: 10.1186/1471-2458-11-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bourdrel T, Bind M-A, Béjot Y, Morel O, Argacha J-F. Cardiovascular effects of air pollution. Arch Cardiovasc Dis. 2017;110:634–642. doi: 10.1016/j.acvd.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pope CA, Bhatnagar A, McCracken JP, Abplanalp W, Conklin DJ, O’Toole T. Exposure to fine particulate air pollution is associated with endothelial injury and systemic inflammation. Circ Res. 2016;119:1204–1214. doi: 10.1161/CIRCRESAHA.116.309279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kelishadi R, Hashemi M, Javanmard SH, Mansourian M, Afshani M, Poursafa P, et al. Effect of particulate air pollution and passive smoking on surrogate biomarkers of endothelial dysfunction in healthy children. Paediatr Int Child Health. 2014;34:165–169. doi: 10.1179/2046905513Y.0000000104. [DOI] [PubMed] [Google Scholar]
- 36.Poursafa P, Baradaran-Mahdavi S, Moradi B, Haghjooy Javanmard S, Tajadini M, Mehrabian F, et al. The relationship of exposure to air pollutants in pregnancy with surrogate markers of endothelial dysfunction in umbilical cord. Environ Res. 2016;146:154–160. doi: 10.1016/j.envres.2015.12.018. [DOI] [PubMed] [Google Scholar]
- 37.Xu M-X, Ge C-X, Qin Y-T, Gu T-T, Lou D-S, Li Q, et al. Prolonged PM2.5 exposure elevates risk of oxidative stress-driven nonalcoholic fatty liver disease by triggering increase of dyslipidemia. Free Radic Biol Med. United States; 2019;130:542–56. [DOI] [PubMed]
- 38.Hahad O, Lelieveld J, Birklein F, Lieb K, Daiber A, Münzel T. Ambient air pollution increases the risk of cerebrovascular and neuropsychiatric disorders through induction of inflammation and oxidative stress. Int J Mol Sci. 2020;21:E4306. doi: 10.3390/ijms21124306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Goldberg AD, Allis CD, Bernstein E. Epigenetics: a landscape takes shape. Cell. 2007;128:635–638. doi: 10.1016/j.cell.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 40.Gluckman PD, Hanson MA. Developmental and epigenetic pathways to obesity: an evolutionary-developmental perspective. Int J Obes. 2005;2008(32 Suppl 7):S62–71. doi: 10.1038/ijo.2008.240. [DOI] [PubMed] [Google Scholar]
- 41.Bell JT, Spector TD. A twin approach to unraveling epigenetics. Trends Genet TIG. 2011;27:116–125. doi: 10.1016/j.tig.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yara S, Lavoie J-C, Levy E. Oxidative stress and DNA methylation regulation in the metabolic syndrome. Epigenomics. 2015;7:283–300. doi: 10.2217/epi.14.84. [DOI] [PubMed] [Google Scholar]
- 43.Newell-Price J, Clark AJ, King P. DNA methylation and silencing of gene expression. Trends Endocrinol Metab TEM. 2000;11:142–148. doi: 10.1016/S1043-2760(00)00248-4. [DOI] [PubMed] [Google Scholar]
- 44.Smith ZD, Meissner A. DNA methylation: roles in mammalian development. Nat Rev Genet. 2013;14:204–220. doi: 10.1038/nrg3354. [DOI] [PubMed] [Google Scholar]
- 45.Cookson W, Liang L, Abecasis G, Moffatt M, Lathrop M. Mapping complex disease traits with global gene expression. Nat Rev Genet. 2009;10:184–194. doi: 10.1038/nrg2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Visscher PM, Wray NR, Zhang Q, Sklar P, McCarthy MI, Brown MA, et al. 10 Years of GWAS discovery: biology, function, and translation. Am J Hum Genet. 2017;101:5–22. doi: 10.1016/j.ajhg.2017.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bibikova M, Le J, Barnes B, Saedinia-Melnyk S, Zhou L, Shen R, et al. Genome-wide DNA methylation profiling using Infinium® assay. Epigenomics. 2009;1:177–200. doi: 10.2217/epi.09.14. [DOI] [PubMed] [Google Scholar]
- 48.Moran S, Arribas C, Esteller M. Validation of a DNA methylation microarray for 850,000 CpG sites of the human genome enriched in enhancer sequences. Epigenomics. 2016;8:389–399. doi: 10.2217/epi.15.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.van Vliet-Ostaptchouk JV, Snieder H, Lagou V. Gene-lifestyle interactions in obesity. Curr Nutr Rep. 2012;1:184–196. doi: 10.1007/s13668-012-0022-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alvarado-Cruz I, Alegría-Torres JA, Montes-Castro N, Jiménez-Garza O, Quintanilla-Vega B. Environmental epigenetic changes, as risk factors for the development of diseases in children: a systematic review. Ann Glob Health. 2018;84:212–224. doi: 10.29024/aogh.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cantone L, Iodice S, Tarantini L, Albetti B, Restelli I, Vigna L, et al. Particulate matter exposure is associated with inflammatory gene methylation in obese subjects. Environ Res. 2017;152:478–484. doi: 10.1016/j.envres.2016.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ouidir M, Mendola P, Buck Louis GM, Kannan K, Zhang C, Tekola-Ayele F. Concentrations of persistent organic pollutants in maternal plasma and epigenome-wide placental DNA methylation. Clin Epigenetics. 2020;12:103. doi: 10.1186/s13148-020-00894-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zakarya R, Adcock I, Oliver BG. Epigenetic impacts of maternal tobacco and e-vapour exposure on the offspring lung. Clin Epigenetics. 2019;11:32. doi: 10.1186/s13148-019-0631-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Li S, Chen M, Li Y, Tollefsbol TO. Prenatal epigenetics diets play protective roles against environmental pollution. Clin Epigenetics. 2019;11:82. doi: 10.1186/s13148-019-0659-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Van Cauwenbergh O, Di Serafino A, Tytgat J, Soubry A. Transgenerational epigenetic effects from male exposure to endocrine-disrupting compounds: a systematic review on research in mammals. Clin Epigenetics. 2020;12:65. doi: 10.1186/s13148-020-00845-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bind M-A, Baccarelli A, Zanobetti A, Tarantini L, Suh H, Vokonas P, et al. Air pollution and markers of coagulation, inflammation, and endothelial function: associations and epigene-environment interactions in an elderly cohort. Epidemiol Camb Mass. 2012;23:332–340. doi: 10.1097/EDE.0b013e31824523f0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bind M-AC, Coull BA, Peters A, Baccarelli AA, Tarantini L, Cantone L, et al. Beyond the mean: quantile regression to explore the association of air pollution with gene-specific methylation in the normative aging study. Environ Health Perspect. 2015;123:759–65. [DOI] [PMC free article] [PubMed]
- 58.Ding R, Jin Y, Liu X, Ye H, Zhu Z, Zhang Y, et al. Dose- and time- effect responses of DNA methylation and histone H3K9 acetylation changes induced by traffic-related air pollution. Sci Rep. 2017;7:43737. doi: 10.1038/srep43737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hou L, Zhang X, Wang D, Baccarelli A. Environmental chemical exposures and human epigenetics. Int J Epidemiol. 2012;41:79–105. doi: 10.1093/ije/dyr154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chi GC, Liu Y, MacDonald JW, Barr RG, Donohue KM, Hensley MD, et al. Long-term outdoor air pollution and DNA methylation in circulating monocytes: results from the Multi-Ethnic Study of Atherosclerosis (MESA) Environ Health Glob Access Sci Source. 2016;15:119. doi: 10.1186/s12940-016-0202-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Plusquin M, Chadeau-Hyam M, Ghantous A, Alfano R, Bustamante M, Chatzi L, et al. DNA methylome marks of exposure to particulate matter at three time points in early life. Environ Sci Technol. 2018;52:5427–5437. doi: 10.1021/acs.est.7b06447. [DOI] [PubMed] [Google Scholar]
- 62.Sayols-Baixeras S, Fernández-Sanlés A, Prats-Uribe A, Subirana I, Plusquin M, Künzli N, et al. Association between long-term air pollution exposure and DNA methylation: the REGICOR study. Environ Res. 2019;176:108550. doi: 10.1016/j.envres.2019.108550. [DOI] [PubMed] [Google Scholar]
- 63.Gondalia R, Baldassari A, Holliday KM, Justice AE, Méndez-Giráldez R, Stewart JD, et al. Methylome-wide association study provides evidence of particulate matter air pollution-associated DNA methylation. Environ Int. 2019;132:104723. doi: 10.1016/j.envint.2019.03.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Saenen ND, Martens DS, Neven KY, Alfano R, Bové H, Janssen BG, et al. Air pollution-induced placental alterations: an interplay of oxidative stress, epigenetics, and the aging phenotype? Clin Epigenetics. 2019;11:124. doi: 10.1186/s13148-019-0688-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rossnerova A, Tulupova E, Tabashidze N, Schmuczerova J, Dostal M, Rossner P, et al. Factors affecting the 27K DNA methylation pattern in asthmatic and healthy children from locations with various environments. Mutat Res. 2013;741–742:18–26. doi: 10.1016/j.mrfmmm.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 66.Baccarelli A, Wright R, Bollati V, Litonjua A, Zanobetti A, Tarantini L, et al. Ischemic heart disease and stroke in relation to blood DNA methylation. Epidemiol Camb Mass. 2010;21:819–828. doi: 10.1097/EDE.0b013e3181f20457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bellavia A, Urch B, Speck M, Brook RD, Scott JA, Albetti B, et al. DNA hypomethylation, ambient particulate matter, and increased blood pressure: findings from controlled human exposure experiments. J Am Heart Assoc. 2013;2:e000212. doi: 10.1161/JAHA.113.000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chen R, Meng X, Zhao A, Wang C, Yang C, Li H, et al. DNA hypomethylation and its mediation in the effects of fine particulate air pollution on cardiovascular biomarkers: a randomized crossover trial. Environ Int. 2016;94:614–619. doi: 10.1016/j.envint.2016.06.026. [DOI] [PubMed] [Google Scholar]
- 69.Peng C, Bind M-AC, Colicino E, Kloog I, Byun H-M, Cantone L, et al. Particulate air pollution and fasting blood glucose in nondiabetic individuals: associations and epigenetic mediation in the normative aging study, 2000–2011. Environ Health Perspect. 2016;124:1715–21. [DOI] [PMC free article] [PubMed]
- 70.Wang X, Falkner B, Zhu H, Shi H, Su S, Xu X, et al. A genome-wide methylation study on essential hypertension in young African American males. PLoS ONE. 2013;8:e53938. doi: 10.1371/journal.pone.0053938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Saenen ND, Vrijens K, Janssen BG, Roels HA, Neven KY, Vanden Berghe W, et al. Lower placental leptin promoter methylation in association with fine particulate matter air pollution during pregnancy and placental nitrosative stress at birth in the ENVIRONAGE cohort. Environ Health Perspect. 2017;125:262–268. doi: 10.1289/EHP38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ferrari L, Carugno M, Bollati V. Particulate matter exposure shapes DNA methylation through the lifespan. Clin Epigenetics. 2019;11:129. doi: 10.1186/s13148-019-0726-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Salam MT, Byun H-M, Lurmann F, Breton CV, Wang X, Eckel SP, et al. Genetic and epigenetic variations in inducible nitric oxide synthase promoter, particulate pollution, and exhaled nitric oxide levels in children. J Allergy Clin Immunol. 2012;129:232–239. doi: 10.1016/j.jaci.2011.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tarantini L, Bonzini M, Tripodi A, Angelici L, Nordio F, Cantone L, et al. Blood hypomethylation of inflammatory genes mediates the effects of metal-rich airborne pollutants on blood coagulation. Occup Environ Med. 2013;70:418–425. doi: 10.1136/oemed-2012-101079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bind M-A, Lepeule J, Zanobetti A, Gasparrini A, Baccarelli A, Coull BA, et al. Air pollution and gene-specific methylation in the Normative Aging Study: association, effect modification, and mediation analysis. Epigenetics. 2014;9:448–458. doi: 10.4161/epi.27584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chen R, Qiao L, Li H, Zhao Y, Zhang Y, Xu W, et al. Fine Particulate matter constituents, nitric oxide synthase DNA methylation and exhaled nitric oxide. Environ Sci Technol. 2015;49:11859–11865. doi: 10.1021/acs.est.5b02527. [DOI] [PubMed] [Google Scholar]
- 77.Shi Y, Zhao T, Yang X, Sun B, Li Y, Duan J, et al. PM2.5-induced alteration of DNA methylation and RNA-transcription are associated with inflammatory response and lung injury. Sci Total Environ. 2019;650:908–21. [DOI] [PubMed]
- 78.Tantoh DM, Wu M-C, Chuang C-C, Chen P-H, Tyan YS, Nfor ON, et al. AHRR cg05575921 methylation in relation to smoking and PM2.5 exposure among Taiwanese men and women. Clin Epigenetics. 2020;12:117. [DOI] [PMC free article] [PubMed]
- 79.Panni T, Aj M, Jd S, Aa B, Ac J, K W, et al. Genome-wide analysis of DNA methylation and fine particulate matter air pollution in three study populations: KORA F3, KORA F4, and the normative aging study. environ health perspect. environ health perspect; 2016 [cited 2021 Oct 21];124. Available from: http://pubmed.ncbi.nlm.nih.gov/26731791/ [DOI] [PMC free article] [PubMed]
- 80.Dai L, Mehta A, Mordukhovich I, Just AC, Shen J, Hou L, et al. Differential DNA methylation and PM2.5 species in a 450K epigenome-wide association study. Epigenetics. 2017;12:139–48. [DOI] [PMC free article] [PubMed]
- 81.Lee MK, Xu C-J, Carnes MU, Nichols CE, Ward JM, BIOS consortium, et al. Genome-wide DNA methylation and long-term ambient air pollution exposure in Korean adults. Clin Epigenetics. 2019;11:37. [DOI] [PMC free article] [PubMed]
- 82.De Prins S, Koppen G, Jacobs G, Dons E, Van de Mieroop E, Nelen V, et al. Influence of ambient air pollution on global DNA methylation in healthy adults: a seasonal follow-up. Environ Int. 2013;59:418–424. doi: 10.1016/j.envint.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 83.Xia Y, Niu Y, Cai J, Lin Z, Liu C, Li H, et al. Effects of personal short-term exposure to ambient ozone on blood pressure and vascular endothelial function: a mechanistic study based on DNA methylation and metabolomics. Environ Sci Technol. 2018;52:12774–12782. doi: 10.1021/acs.est.8b03044. [DOI] [PubMed] [Google Scholar]
- 84.Fiorito G, Vlaanderen J, Polidoro S, Gulliver J, Galassi C, Ranzi A, et al. Oxidative stress and inflammation mediate the effect of air pollution on cardio- and cerebrovascular disease: a prospective study in nonsmokers. Environ Mol Mutagen. 2018;59:234–246. doi: 10.1002/em.22153. [DOI] [PubMed] [Google Scholar]
- 85.Jiang Y, Niu Y, Xia Y, Liu C, Lin Z, Wang W, et al. Effects of personal nitrogen dioxide exposure on airway inflammation and lung function. Environ Res. 2019;177:108620. doi: 10.1016/j.envres.2019.108620. [DOI] [PubMed] [Google Scholar]
- 86.Gruzieva O, Xu C-J, Breton CV, Annesi-Maesano I, Antó JM, Auffray C, et al. Epigenome-wide meta-analysis of methylation in children related to prenatal NO2 air pollution exposure. Environ Health Perspect. 2017;125:104–110. doi: 10.1289/EHP36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.de F C Lichtenfels AJ, van der Plaat DA, de Jong K, van Diemen CC, Postma DS, Nedeljkovic I, et al. Long-term air pollution exposure, genome-wide DNA methylation and lung function in the lifelines cohort study. Environ Health Perspect. 2018;126:027004. [DOI] [PMC free article] [PubMed]
- 88.Abraham E, Rousseaux S, Agier L, Giorgis-Allemand L, Tost J, Galineau J, et al. Pregnancy exposure to atmospheric pollution and meteorological conditions and placental DNA methylation. Environ Int. 2018;118:334–347. doi: 10.1016/j.envint.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 89.Scinicariello F, Buser MC. Urinary polycyclic aromatic hydrocarbons and childhood obesity: NHANES (2001–2006) Environ Health Perspect. 2014;122:299–303. doi: 10.1289/ehp.1307234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Alegría-Torres JA, Barretta F, Batres-Esquivel LE, Carrizales-Yáñez L, Pérez-Maldonado IN, Baccarelli A, et al. Epigenetic markers of exposure to polycyclic aromatic hydrocarbons in Mexican brickmakers: a pilot study. Chemosphere. 2013;91:475–480. doi: 10.1016/j.chemosphere.2012.11.077. [DOI] [PubMed] [Google Scholar]
- 91.Alvarado-Cruz I, Sánchez-Guerra M, Hernández-Cadena L, De Vizcaya-Ruiz A, Mugica V, Pelallo-Martínez NA, et al. Increased methylation of repetitive elements and DNA repair genes is associated with higher DNA oxidation in children in an urbanized, industrial environment. Mutat Res Genet Toxicol Environ Mutagen. 2017;813:27–36. doi: 10.1016/j.mrgentox.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 92.Herbstman J, D T, D Z, L Q, A S, Z L, et al. Prenatal exposure to polycyclic aromatic hydrocarbons, benzo[a]pyrene-DNA adducts, and genomic DNA methylation in cord blood. Environ Health Perspect. Environ Health Perspect; 2012 [cited 2021 Oct 22];120. Available from: http://pubmed.ncbi.nlm.nih.gov/22256332/ [DOI] [PMC free article] [PubMed]
- 93.Kim YH, Lee YS, Lee DH, Kim DS. Polycyclic aromatic hydrocarbons are associated with insulin receptor substrate 2 methylation in adipose tissues of Korean women. Environ Res. 2016;150:47–51. doi: 10.1016/j.envres.2016.05.043. [DOI] [PubMed] [Google Scholar]
- 94.Lin S, Ren A, Wang L, Santos C, Huang Y, Jin L, et al. Aberrant methylation of Pax3 gene and neural tube defects in association with exposure to polycyclic aromatic hydrocarbons. Clin Epigenetics. 2019;11:13. doi: 10.1186/s13148-019-0611-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Li J, Zhu X, Yu K, Jiang H, Zhang Y, Wang B, et al. Exposure to polycyclic aromatic hydrocarbons and accelerated DNA methylation aging. Environ Health Perspect. 2018;126:067005. doi: 10.1289/EHP2773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Latini G, De Mitri B, Del Vecchio A, Chitano G, De Felice C, Zetterström R. Foetal growth of kidneys, liver and spleen in intrauterine growth restriction: “programming” causing “metabolic syndrome” in adult age. Acta Paediatr Oslo Nor. 1992;2004(93):1635–1639. doi: 10.1080/08035250410023106. [DOI] [PubMed] [Google Scholar]
- 97.Wadhwa PD, Buss C, Entringer S, Swanson JM. Developmental origins of health and disease: brief history of the approach and current focus on epigenetic mechanisms. Semin Reprod Med. 2009;27:358–368. doi: 10.1055/s-0029-1237424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Xita N, Tsatsoulis A. Fetal origins of the metabolic syndrome. Ann N Y Acad Sci. 2010;1205:148–155. doi: 10.1111/j.1749-6632.2010.05658.x. [DOI] [PubMed] [Google Scholar]
- 99.Saffery R, Novakovic B. Epigenetics as the mediator of fetal programming of adult onset disease: what is the evidence? Acta Obstet Gynecol Scand. 2014;93:1090–1098. doi: 10.1111/aogs.12431. [DOI] [PubMed] [Google Scholar]
- 100.Felix JF, Joubert BR, Baccarelli AA, Sharp GC, Almqvist C, Annesi-Maesano I, et al. Cohort profile: pregnancy and childhood epigenetics (PACE) consortium. Int J Epidemiol. 2018;47:22–23u. doi: 10.1093/ije/dyx190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Godfrey KM, Sheppard A, Gluckman PD, Lillycrop KA, Burdge GC, McLean C, et al. Epigenetic gene promoter methylation at birth is associated with child’s later adiposity. Diabetes. 2011;60:1528–1534. doi: 10.2337/db10-0979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Küpers LK, Monnereau C, Sharp GC, Yousefi P, Salas LA, Ghantous A, et al. Meta-analysis of epigenome-wide association studies in neonates reveals widespread differential DNA methylation associated with birthweight. Nat Commun. 2019;10:1893. doi: 10.1038/s41467-019-09671-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Williams L, Seki Y, Delahaye F, Cheng A, Fuloria M, Hughes Einstein F, et al. DNA hypermethylation of CD3(+) T cells from cord blood of infants exposed to intrauterine growth restriction. Diabetologia. 2016;59:1714–1723. doi: 10.1007/s00125-016-3983-7. [DOI] [PubMed] [Google Scholar]
- 104.Luttmer R, Spijkerman AM, Kok RM, Jakobs C, Blom HJ, Serne EH, et al. Metabolic syndrome components are associated with DNA hypomethylation. Obes Res Clin Pract. 2013;7:e106–e115. doi: 10.1016/j.orcp.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 105.Lopes LL, Bressan J, Peluzio M do CG, Hermsdorff HHM. LINE-1 in Obesity and Cardiometabolic Diseases: A Systematic Review. J Am Coll Nutr. 2019;38:478–84. [DOI] [PubMed]
- 106.Akinyemiju T, Do AN, Patki A, Aslibekyan S, Zhi D, Hidalgo B, et al. Epigenome-wide association study of metabolic syndrome in African-American adults. Clin Epigenetics. 2018;10:49. doi: 10.1186/s13148-018-0483-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Das M, Sha J, Hidalgo B, Aslibekyan S, Do AN, Zhi D, et al. Association of DNA methylation at CPT1A locus with metabolic syndrome in the genetics of lipid lowering drugs and diet network (GOLDN) study. PLoS ONE. 2016;11:e0145789. doi: 10.1371/journal.pone.0145789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hidalgo B, Irvin MR, Sha J, Zhi D, Aslibekyan S, Absher D, et al. Epigenome-wide association study of fasting measures of glucose, insulin, and HOMA-IR in the Genetics of Lipid Lowering Drugs and Diet Network study. Diabetes. 2014;63:801–807. doi: 10.2337/db13-1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kulkarni H, Kos MZ, Neary J, Dyer TD, Kent JW, Göring HHH, et al. Novel epigenetic determinants of type 2 diabetes in Mexican-American families. Hum Mol Genet. 2015;24:5330–5344. doi: 10.1093/hmg/ddv232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Richard MA, Huan T, Ligthart S, Gondalia R, Jhun MA, Brody JA, et al. DNA methylation analysis identifies loci for blood pressure regulation. Am J Hum Genet. 2017;101:888–902. doi: 10.1016/j.ajhg.2017.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Huang Y, Ollikainen M, Muniandy M, Zhang T, van Dongen J, Hao G, et al. Identification, heritability, and relation with gene expression of novel DNA methylation loci for blood pressure. Hypertens Dallas Tex. 1979;2020(76):195–205. doi: 10.1161/HYPERTENSIONAHA.120.14973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Walaszczyk E, Luijten M, Spijkerman AMW, Bonder MJ, Lutgers HL, Snieder H, et al. DNA methylation markers associated with type 2 diabetes, fasting glucose and HbA1c levels: a systematic review and replication in a case-control sample of the Lifelines study. Diabetologia. 2018;61:354–368. doi: 10.1007/s00125-017-4497-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Demerath EW, Guan W, Grove ML, Aslibekyan S, Mendelson M, Zhou Y-H, et al. Epigenome-wide association study (EWAS) of BMI, BMI change and waist circumference in African American adults identifies multiple replicated loci. Hum Mol Genet. 2015;24:4464–4479. doi: 10.1093/hmg/ddv161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ali O, Cerjak D, Kent JW, James R, Blangero J, Carless MA, et al. Methylation of SOCS3 is inversely associated with metabolic syndrome in an epigenome-wide association study of obesity. Epigenetics. 2016;11:699–707. doi: 10.1080/15592294.2016.1216284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wahl S, Drong A, Lehne B, Loh M, Scott WR, Kunze S, et al. Epigenome-wide association study of body mass index, and the adverse outcomes of adiposity. Nature. 2017;541:81–86. doi: 10.1038/nature20784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wang X, Pan Y, Zhu H, Hao G, Huang Y, Barnes V, et al. An epigenome-wide study of obesity in African American youth and young adults: novel findings, replication in neutrophils, and relationship with gene expression. Clin Epigenetics. 2018;10:3. doi: 10.1186/s13148-017-0435-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Carson C, Lawson HA. Epigenetics of metabolic syndrome. Physiol Genomics. 2018;50:947–955. doi: 10.1152/physiolgenomics.00072.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bansal A, Pinney SE. DNA methylation and its role in the pathogenesis of diabetes. Pediatr Diabetes. 2017;18:167–177. doi: 10.1111/pedi.12521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Liang M. Epigenetic mechanisms and hypertension. Hypertens Dallas Tex. 1979;2018(72):1244–1254. doi: 10.1161/HYPERTENSIONAHA.118.11171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Mostafavi N, Vlaanderen J, Portengen L, Chadeau-Hyam M, Modig L, Palli D, et al. Associations between genome-wide gene expression and ambient nitrogen oxides. Epidemiol Camb Mass. 2017;28:320–328. doi: 10.1097/EDE.0000000000000628. [DOI] [PubMed] [Google Scholar]
- 121.Raftopoulos L, Katsi V, Makris T, Tousoulis D, Stefanadis C, Kallikazaros I. Epigenetics, the missing link in hypertension. Life Sci. 2015;129:22–26. doi: 10.1016/j.lfs.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 122.Küpers LK, Xu X, Jankipersadsing SA, Vaez A, la Bastide-van GS, Scholtens S, et al. DNA methylation mediates the effect of maternal smoking during pregnancy on birthweight of the offspring. Int J Epidemiol. 2015;44:1224–1237. doi: 10.1093/ije/dyv048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Breton CV, Yao J, Millstein J, Gao L, Siegmund KD, Mack W, et al. Prenatal air pollution exposures, DNA methyl transferase genotypes, and associations with newborn LINE1 and Alu methylation and childhood blood pressure and carotid intima-media thickness in the children’s health study. Environ Health Perspect. 2016;124:1905–1912. doi: 10.1289/EHP181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Wei H, Liang F, Meng G, Nie Z, Zhou R, Cheng W, et al. Redox/methylation mediated abnormal DNA methylation as regulators of ambient fine particulate matter-induced neurodevelopment related impairment in human neuronal cells. Sci Rep. 2016;6:33402. doi: 10.1038/srep33402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Stelzer G, Rosen N, Plaschkes I, Zimmerman S, Twik M, Fishilevich S, et al. The GeneCards suite: from gene data mining to disease genome sequence analyses. Curr Protoc Bioinforma. 2016;54:1.30.1–1.30.33. [DOI] [PubMed]
- 126.Battram T, Yousefi P, Crawford G, Prince C, Babei MS, Sharp G, et al. The EWAS Catalog: a database of epigenome-wide association studies. OSF Preprints; 2021 [cited 2021 May 5]. Available from: https://osf.io/837wn/ [DOI] [PMC free article] [PubMed]
- 127.Zou L, Yan S, Guan X, Pan Y, Qu X. Hypermethylation of the PRKCZ gene in type 2 diabetes mellitus. J Diabetes Res. 2013;2013:721493. doi: 10.1155/2013/721493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Dubey RK, Oparil S, Imthurn B, Jackson EK. Sex hormones and hypertension. Cardiovasc Res. 2002;53:688–708. doi: 10.1016/S0008-6363(01)00527-2. [DOI] [PubMed] [Google Scholar]
- 129.Hughes GS, Mathur RS, Margolius HS. Sex steroid hormones are altered in essential hypertension. J Hypertens. 1989;7:181–187. doi: 10.1097/00004872-198903000-00003. [DOI] [PubMed] [Google Scholar]
- 130.Reckelhoff JF. Androgens and blood pressure control: sex differences and mechanisms. Mayo Clin Proc Elsevier. 2019;94:536–543. doi: 10.1016/j.mayocp.2018.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Relton CL, Davey SG. Epigenetic epidemiology of common complex disease: prospects for prediction, prevention, and treatment. PLoS Med. 2010;7:e1000356. doi: 10.1371/journal.pmed.1000356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Epigenetics. Wikipedia. 2022 [cited 2022 Apr 14]. Available from: https://en.wikipedia.org/w/index.php?title=Epigenetics&oldid=1082239772
- 133.Ramzan F, Vickers MH, Mithen RF. Epigenetics, microRNA and metabolic syndrome: a comprehensive review. Int J Mol Sci. 2021;22:5047. doi: 10.3390/ijms22095047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Suhaimi NF, Jalaludin J, Abu BS. The influence of traffic-related air pollution (TRAP) in primary schools and residential proximity to traffic sources on histone H3 level in selected Malaysian children. Int J Environ Res Public Health. 2021;18:7995. doi: 10.3390/ijerph18157995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zheng Y, Sanchez-Guerra M, Zhang Z, Joyce BT, Zhong J, Kresovich JK, et al. Traffic-derived particulate matter exposure and histone H3 modification: a repeated measures study. Environ Res. 2017;153:112–119. doi: 10.1016/j.envres.2016.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kresovich JK, Zhang Z, Fang F, Zheng Y, Sanchez-Guerra M, Joyce BT, et al. Histone 3 modifications and blood pressure in the Beijing Truck Driver Air Pollution Study. Biomark Biochem Indic Expo Response Susceptibility Chem. 2017;22:584–593. doi: 10.1080/1354750X.2017.1347961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Buitrago D, Labrador M, Arcon JP, Lema R, Flores O, Esteve-Codina A, et al. Impact of DNA methylation on 3D genome structure. Nat Commun. Nature Publishing Group; 2021;12:3243. [DOI] [PMC free article] [PubMed]
- 138.US EPA R 01. Actions You Can Take to Reduce Air Pollution | Ground-level Ozone | New England | US EPA. [cited 2022 Feb 5]. Available from: https://www3.epa.gov/region1/airquality/reducepollution.html
- 139.Household air pollution and health. [cited 2022 Feb 5]. Available from: https://www.who.int/news-room/fact-sheets/detail/household-air-pollution-and-health
- 140.10 things you can do to help reduce air pollution today. Sustrans. [cited 2022 Feb 5]. Available from: https://www.sustrans.org.uk/our-blog/get-active/2020/in-your-community/10-things-you-can-do-to-help-reduce-air-pollution-today
- 141.Campagna MP, Xavier A, Lechner-Scott J, Maltby V, Scott RJ, Butzkueven H, et al. Epigenome-wide association studies: current knowledge, strategies and recommendations. Clin Epigenetics. 2021;13:214. doi: 10.1186/s13148-021-01200-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Supplementary Tables 1–3.
Data Availability Statement
All papers reviewed and described in this manuscript are available online in the relevant publications.