Abstract
Objective
We examined the relationship of team and leadership attributes with clinician feelings of burnout over time during the corona virus disease 2019 (COVID‐19) pandemic.
Methods
We surveyed emergency medicine personnel at 2 California hospitals at 3 time points: July 2020, December 2020, and November 2021. We assessed 3 team and leadership attributes using previously validated psychological scales (joint problem‐solving, process clarity, and leader inclusiveness) and burnout using a validated scale. Using logistic regression models we determined the associations between team and leadership attributes and burnout, controlling for covariates.
Results
We obtained responses from 328, 356, and 260 respondents in waves 1, 2, and 3, respectively (mean response rate = 49.52%). The median response for feelings of burnout increased over time (2.0, interquartile range [IQR] = 2.0–3.0 in wave 1 to 3.0, IQR = 2.0–3.0 in wave 3). At all time points, greater process clarity was associated with lower odds of feeling burnout (odds ratio [OR] [95% confidence interval (CI) = 0.36 [0.19, 0.66] in wave 1 to 0.24 [0.10, 0.61] in wave 3). In waves 2 and 3, greater joint problem‐solving was associated with lower odds of feeling burnout (OR [95% CI] = 0.61 [0.42, 0.89], 0.54 [0.33, 0.88]). Leader inclusiveness was also associated with lower odds of feeling burnout (OR [95% CI] = 0.45 [0.27, 0.74] in wave 1 to 0.41 [0.24, 0.69] in wave 3).
Conclusions
Process clarity, joint problem‐solving, and leader inclusiveness are associated with less clinician burnout during the COVID‐19 pandemic, pointing to potential benefits of focusing on team and leadership factors during crisis. Leader inclusiveness may wane over time, requiring effort to sustain.
1. INTRODUCTION
1.1. Background
Emergency medicine has faced one of the highest incidences of burnout in healthcare for many years, 1 and being on the frontlines of patient care during the coronavirus disease 2019 (COVID‐19) pandemic has brought this important challenge into focus. A growing body of research has documented the severity of burnout in emergency medicine during the pandemic, citing added workload, fear of being infected or infecting others, and trauma from delivering care amid a pandemic, with estimates close to 50% of emergency medicine personnel reporting moderate to severe burnout. 2 Recent research has sought to pinpoint modifiable factors that could help to alleviate burnout in this setting, identifying several individual and structural factors, such as offering viral testing, 3 and there is growing recognition that multi‐faceted responses to this complex issue are likely warranted. 4
1.2. Importance
Research to date has focused on individual and structural factors to alleviate burnout and has paid less attention to the potential role of team‐level attributes, despite past research documenting the importance of teamwork and leadership in healthcare workers’ daily experience. 5 Interpersonal leadership and team factors are relevant to burnout because leaders and teammates are the primary entities that inform, provide resources to, seek input from and recognize the efforts of frontline healthcare workers. 6 Early evidence during COVID‐19 supported this idea, finding that feeling part of a team buffered against burnout among emergency medicine staff. 7 Yet, little is known about the aspects of leadership and teamwork that may protect emergency medicine staff against burnout, particularly over time in a prolonged crisis. Longitudinal research in this context is important, because leadership and team factors may be the first to fray amid high stress and uncertainty. 8
1.3. Goals of this investigation
Expanding on prior healthcare research on both burnout and COVID‐19, we sought to determine interpersonal team and leadership factors associated with burnout over time in the emergency medicine setting during COVID‐19.
2. METHODS
2.1. Study design and setting
We used a 3‐wave cross‐sectional survey of emergency department (ED) clinicians and staff to examine the association between validated measures of team and leadership attributes and self‐reported feelings of burnout over 17 months of the COVID‐19 pandemic. We administered the survey electronically at 2 EDs affiliated with the University of California, San Francisco from June 2020 to July 2020, December 2020 to January 2021, and October 2021 to November 2021. The survey instrument was developed to measure a broad set of experiences related to the pandemic, of which we focus on a subset in this study; it took approximately 10 minutes to complete. Participants received a $5 gift card as remuneration for each survey.
The Bottom Line.
Emergency worker burnout has been a major concern throughout the corona virus disease 2019 (COVID‐19) pandemic. In this multi‐wave survey of emergency department personnel at 2 California hospitals, leadership and teamwork attributes (process clarity, join problem‐solving, and leader inclusiveness) were associated with lower rates of self‐reported burnout. Training or interventions focused on leadership and teamwork may potentially mitigate worker burnout.
2.2. Selection of participants
We surveyed all personnel in the EDs across the following roles: attending physicians, residents and fellows, advanced practice providers (physician assistants and nurse practitioners), pharmacists, respiratory therapists, greeters, technicians, and social workers. The survey was administered electronically in English via Qualtrics; it was accessible through an email link and by QR code on posters in the units. The response rate was determined by dividing the responses for each role by the number of employees on record for that role in both departments.
2.3. Measurements
For this analysis, we focus on 3 team and leadership attributes that satisfied 2 criteria: (1) having a validated measurement scale from past research, and (2) having conceptual relevance to the problem of burnout in emergency medicine during COVID‐19. The selected measures include process clarity, joint problem‐solving, and leader inclusiveness.
Process clarity, a scale validated in past psychological research, provides a measurement of the extent to which staff is clear about how to do their jobs and has been found to be an antecedent of team effectiveness. 9 , 10 We selected it because it may be particularly important for maintaining the emotional and physical resources that limit stress during crisis, when there is great uncertainty about what to do and typical ways of working together are disrupted. 11 , 12
Joint problem‐solving among teammates was developed and validated to measure collaboration in fluid teamwork settings, as team members change and goals or tasks shift. 13 This measure may have particular relevance to emergency medicine during the COVID‐19 pandemic because it can capture the ability of multi‐disciplinary, distributed teams to respond to problems emerging as the crisis unfolds.
Leader inclusiveness is a scale that has been shown to be an important factor in healthcare for helping people on the frontlines of care to speak up with concerns and questions, 14 and recent research has suggested that feeling that one can speak up and be heard is associated with lower burnout. 15 Leader inclusiveness offers a modifiable factor that may influence feelings of burnout through increasing feelings that people can speak up and be heard.
All survey items were measured using 5‐point Likert agreement scales, where 1 was “strongly disagree” and 5 was “strongly agree” (see the Supporting Information Appendix for survey measures verbatim). Negatively worded items were reverse coded to establish positive directionality. We measured demographics by self‐report, including age, gender, race, location, role, tenure, and shift. Survey item wordings were minimally adapted for appropriateness in the ED during the pandemic and cognitively tested with 3 organizational insiders, and wording was modified for clarity through iterative discussions among the authors with multi‐disciplinary expertise.
Our research focus was the emergency medicine clinician experience throughout a prolonged pandemic, and to examine this robustly, we administered the survey repetitively at 3 time points as the pandemic spiked in relevance for staff, once early in the pandemic, June 2020, about half a year later as another spike arose in December 2020, and approximately a year later in October 2021, following another spike in July–August 2021 and as the total number of vaccinated individuals plateaued. The 7‐day rolling average of daily new COVID‐19 cases in San Francisco for each wave were as follows: when wave 1 began, it was 62 and increased to 122 by the wave end; for wave 2, it began at 278 and ended at a high of 370; for wave 3, it began at 86 and fell to 60. 16
2.4. Outcomes
The 2 outcome measures were self‐reported perceptions of burnout and perceived change in burnout during the COVID‐19 pandemic. Perceptions of burnout were assessed using a previously validated single‐item scale developed by Dolan et al 17 for parsimonious use among healthcare workers: “Overall, based on your definition of burnout, how would you rate your level of burnout?” Perception of the extent to which burnout was worsening during the crisis was ascertained with a single‐item created for this study: “Compared to your level of burnout prior to COVID‐19, to what extent is your current level of burnout worse, improved or the same?” (see the Supporting Information Appendix for survey measures). Outcome measures were coded as binary variables to indicate whether respondents experienced burnout (i.e., if they reported experiencing any symptoms of burnout) and worsening burnout (i.e., if they reported experiencing any worsening symptoms of burnout since the COVID‐19 pandemic began).
2.5. Exposures
We examined these outcomes in relation to the 3 interpersonal leadership and team measures described in the measurement section above. Each of these measures has been studied as an aspect of employee experience and exhibited conceptual relevance to burnout during COVID‐19, but to our knowledge had not previously been associated with burnout in emergency medicine.
2.6. Analysis
We conducted descriptive analyses of demographic characteristics, the 2 outcome measures, and the 3 predictors of interest for each survey wave. We assessed each predictor measure's internal consistency across all 3 waves. We conducted multivariate analyses using a series of logistic regression models to estimate the relationships of each team and leadership scale with burnout and worsening burnout in each wave, while controlling for demographic covariates. All models included a single predictor of interest (i.e., joint problem‐solving, process clarity, or leader inclusiveness) and controlled for demographic factors (gender, race, ED location, role, tenure, and shift). We presented odds ratios (ORs) in each time point. Statistical analyses were performed with Stata SE 16.1. The study was approved by institutional review boards at Harvard University and the University of California San Francisco.
3. RESULTS
3.1. Characteristics of study subjects
A total of 328, 356, and 260 people responded to wave 1, 2, and 3, respectively (average response rate = 49.52%). Respondent characteristics were similar across the 3 survey waves (Table 1). Across the survey waves, respondents included 26–39 attendings (13.4%–16.4%), 16–31 residents/fellows (8.0%–11.5%), 18–21 advance practice providers (7.4%–11.2%), 86–113 registered nurses (45.7%–50.6%), and 39–44 other ED personnel (respiratory therapists, social workers, etc.: 17.1%–20.7%).
TABLE 1.
Sample characteristics, waves 1, 2, and 3
| Characteristics | No. (%) | ||
|---|---|---|---|
| Wave 1 (n = 328) | Wave 2 (n = 356) | Wave 3 (n = 260) | |
| Age (mean [SD]), y | 39.3 (8.91) | 39.6 (9.37) | 40.1 (8.94) |
| Sex | |||
| Male | 81 (34.2%) | 84 (31.2%) | 56 (29.8%) |
| Female | 138 (58.2%) | 167 (62.1%) | 116 (61.7%) |
| Trans, non‐binary, and prefer not to answer | 18 (7.6%) | 18 (6.7%) | 16 (8.5%) |
| Race | |||
| White | 131 (59.6%) | 153 (60.0%) | 107 (60.8%) |
| Black | 12 (5.4%) | 15 (5.9%) | 7 (4.0%) |
| Asian | 34 (15.4%) | 43 (16.9%) | 23 (13.1%) |
| Other (Native American, Pacific Islander, or more than one race) | 43 (19.6%) | 44 (17.2%) | 39 (22.2%) |
| Emergency department site | |||
| Site 1 | 195 (62.1%) | 209 (61.3%) | 158 (62.4%) |
| Site 2 | 119 (37.9%) | 132 (38.7%) | 95 (37.6%) |
| Role | |||
| Attending | 39 (16.4%) | 36 (13.4%) | 26 (13.8%) |
| Resident/Fellow | 19 (8.0%) | 31 (11.5%) | 16 (8.5%) |
| APP | 18 (7.6%) | 20 (7.4%) | 21 (11.2%) |
| RN | 118 (49.6%) | 136 (50.6%) | 86 (45.7%) |
| Other (respiratory therapists, social workers, pharmacists, techs) | 44 (18.5%) | 46 (17.1%) | 39 (20.7%) |
| Tenure | |||
| <2 y | 44 (18.3%) | 59 (21.9%) | 37 (19.7%) |
| 2‐5 y | 64 (26.7%) | 71 (26.4%) | 44 (23.4%) |
| >5 y | 132 (55.0%) | 139 (51.7%) | 107 (56.9%) |
| Shift | |||
| Night | 54 (22.8%) | 65 (24.2%) | 44 (23.4%) |
| Day | 89 (37.6%) | 85 (31.6%) | 62 (33.0%) |
| Mixed | 94 (38.7%) | 119 (44.2%) | 82 (43.6%) |
Note: The percentages across categories do not total to 100% due to some missingness or rounding.
3.2. Main results
The median response to the self‐reported burnout scale increased from wave 1 to wave 2 and plateaued in wave 3 (median of 2.0 in wave 1 to 3.0 in waves 2 and 3); reaching a median of 3.0 indicated that half of respondents reported that they were at least “definitely burning out” (Table 2). Reports of worsening burnout as compared to before COVID‐19 remained consistent, with a median of 4.0 in all 3 waves (a response of 4 indicated that feelings of burnout had gotten “a little worse” since before the COVID‐19 pandemic).
TABLE 2.
Burnout outcomes, teamwork, and leadership factors, waves 1, 2, and 3
| Measure descriptives | Median (IQR) | ||
|---|---|---|---|
| Wave 1 | Wave 2 | Wave 3 | |
| Outcomes | |||
| Overall burnout | 2.0 (2.0–3.0) | 3.0 (2.0–3.0) | 3.0 (2.0–3.0) |
| Worsening burnout | 4.0 (3.0–4.0) | 4.0 (4.0–5.0) | 4.0 (4.0–5.0) |
| Teamwork factors | |||
| Joint problem‐solving | 4.0 (3.0–4.0) | 4.0 (3.0–4.0) | 4.0 (3.0–4.0) |
| Leadership factors | |||
| Process clarity | 3.5 (3.3–4.0) | 3.5 (3.3–3.8) | 3.5 (3.0–3.8) |
| Leader inclusiveness | 3.5 (3.0–4.0) | 3.5 (2.8–4.0) | 3.3 (2.8–4.0) |
Note: IQR, interquartile range. Overall burnout was assessed with the following scale: (1) “I enjoy my work. I have no symptoms of burnout;” (2) “Occasionally I am under stress, and I don't always have as much energy as I once did, but I don't feel burned out;” (3) “I am definitely burning out and have one or more symptoms of burnout, such as physical and emotional exhaustion;” (4) “The symptoms of burnout that I'm experiencing won't go away. I think about frustration at work a lot;” (5) “I feel completely burned out and often wonder if I can go on. I am at the point where I may need some changes or may need to seek some sort of help.” Worsening burnout was reverse‐coded and assessed with the following scale as burnout that had: (1) “Gotten much worse;” (2) “Gotten a little worse;” (3) “Stayed the same;” (4) “Gotten a little better;” and (5) “Gotten much better.”
The scores for the team and leadership measures were reported as follows in wave 1, where a higher score between 1 and 5 indicated stronger perceptions of that measure: median joint problem‐solving = 4.0; process clarity = 3.5; leader inclusiveness = 3.5. These remained mostly stable across the three measurement time points, except leader inclusiveness declined in wave 3, from a median of 3.5–3.2. The survey scales for the 3 team and leadership attributes all exhibited scale reliability (Cronbach's α ranged from 0.70 to 0.83).
All 3 team and leadership attributes were associated with lower odds of feeling burnout, though with differing magnitudes and patterns of statistical significance across the 3 reporting time points (Figure 1). Process clarity was associated with lower odds of feeling burnout in all 3 waves, and the magnitude of this relationship increased over time. For example, a 1‐point increase in process clarity was associated with 64% lower odds of feeling burnout in wave 1 (OR = 0.36; 95% confidence interval [CI] = 0.19, 0.66) and this grew to 76% by wave 3 (OR = 0.24; 95% CI = 0.10, 0.61). Leader inclusiveness was associated with lower odds of burnout in all time points. Greater joint problem‐solving was associated with lower odds of burnout in waves 2 and 3.
FIGURE 1.
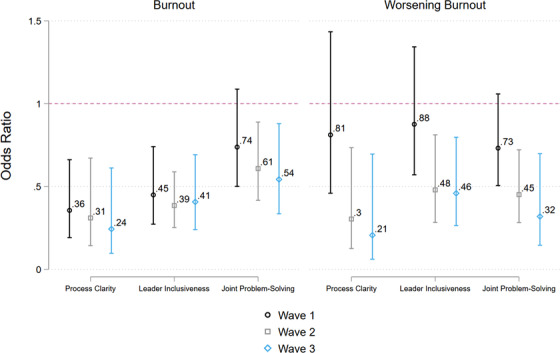
Associations of team and leadership attributes with burnout over time. Notes: Analytic N = 216 for wave 1; 253 for burnout and 251 for worsening burnout in wave 2; 174 in wave 3. The values reported are odds ratio coefficients generated using logistic regression models. Not presented in this figure are the controlling variables, gender, race, emergency department location, role, tenure, and shift, the coefficients for which can be found in Supporting Information Appendix Tables S1–S3. Standard errors are robust. Burnout and worsening burnout were redefined as binary outcomes, where burnout was reported as “I am definitely burning out and have one or more symptoms of burnout, such as physical and emotional exhaustion” or worse, and worsening burnout was burnout that had gotten “a little worse,” or “much worse” since before the pandemic.
4. LIMITATIONS
There are limitations in this analysis. First, the measures examined in this study were self‐reported and could be affected by measurement error. In a dynamic environment such as emergency medicine during a pandemic, feelings of burnout or teamwork may vary day‐to‐day, and any single time‐point may not represent an overarching feeling. However, this particular concern was mitigated by the consistency in the observed team and leadership factors across the 3 time points in this study. Nonetheless, individual reports for each measure are likely to include some degree of personal discretion and interpretation. Second, the survey measures were collected using the same survey instrument and could be subject to common source bias; for example, respondents who are more likely to rate team and leadership factors highly may also be those who are least likely to report feelings of burnout due to a general tendency toward optimism or another psychological trait. Future research can address this limitation by gathering team and leadership measures from sources separate from the same survey through which burnout is measured. Third, although our combined response rate reflects typical response rates in clinician surveys, 18 staff who were feeling particularly high burnout may not have participated in the survey due to stress and competing demands, which would lead our overall estimates to underestimate the reality. Fourth, the cross‐sectional study design cannot examine causality, and some degree of recursive relationship is likely—for example, it is possible not only that strong teamwork helps alleviate feelings of burnout but also that less burned‐out teams find it easier to collaborate. Future research with granular multi‐method data can help to uncover this nuanced interplay. Last, the survey was administered to a limited population of ED personnel in California during a pandemic; generalizability to other time points and contexts needs exploration.
5. DISCUSSION
This study aligns with other recent studies that have observed a high degree of emergency medicine healthcare worker burnout during the coronavirus pandemic. 3 Our longitudinal design further highlights that both the degree of burnout and its alleviating factors may change over time in a sustained crisis. Moreover, we observed that individuals who reported higher levels of teamwork and inclusive leadership experienced less burnout. Efforts to strengthen teamwork, clarify processes, and enhance staff inclusivity may offer additional pathways to alleviating burnout.
Much of the existing literature on burnout in emergency medicine has focused on individual “methods of coping,” such as calling the hospital's COVID‐19 hotline for psychological help or participating in meditation and yoga, as described in a recent multi‐center study of emergency medicine. 2 Although this focus may offer some potentially helpful methods, it places the responsibility for burnout on the shoulders of the individuals experiencing it, often asking them to do even more (eg, calling a hotline) exactly when they feel they have little left. 19 Our study offers an important contrast; that organizational aspects of teamwork and leadership may help to alleviate feelings of burnout. Our findings point to organizational interventions to improve teamwork and leadership as a potentially underused resource in alleviating burnout. For example, efforts to measure perceptions of teamwork and leadership among clinicians via repeated pulse surveys during a crisis could help organizations rapidly identify units in need of focused support.
Our longitudinal research on self‐reported burnout during the pandemic shows the importance of tracking these factors over time. For instance, we observe that leader inclusiveness decreased over time (by contrast, process clarity and joint problem‐solving were notably consistent). This accords with previous research that leadership in crisis can fray, 8 and emphasizes the need for healthcare organizations to attend to leader inclusiveness over time—for example, by initiating renewed efforts to support leaders in modeling these behaviors over time. 20 At the same time, we found that joint problem‐solving was not significantly related to lower odds of feeling burnout in the first survey wave, but this changed in later waves. Team members may offer a particular resource to one another as sustained crises continue.
These findings also have important implications for practice. Healthcare leaders seeking to mitigate feelings of burnout should consider team and leadership factors alongside individual and structural approaches. Process clarity can be achieved through deliberate efforts to share information by leadership; for instance, clear communication of protocols has been found to reduce physician anxiety in emergency medicine. 21 Although this is an essential first step, the vicissitudes of crisis may also call for more rapid and flexible adaptation through joint problem‐solving; it is not enough to set a process, people also need interpersonal tools and time to solve the many problems that arise thereafter Joint problem‐solving can be fostered through processes of asking questions and offering solutions to joint problems—and these processes can be quick and time‐limited, such as in a brief huddle. 6 For leaders addressing concerns of uncertainty and distress, providing staff with opportunities to be heard, no matter their rank or role, and reinforcing camaraderie may be vital and require careful stewardship over time.
Using a 3‐wave cross‐sectional survey of ED clinicians and staff, we find that process clarity, leader inclusiveness, and joint problem‐solving were associated with reduced feelings of burnout over 1.5 years of the COVID‐19 pandemic. Amid a sustained crisis, an emphasis on teamwork and inclusive leadership may offer a powerful avenue for resilience.
CONFLICTS OF INTEREST
C.R.P. is a consultant for FujiFilm SonoSite and Ceribell. N.S. is a consultant for Inflammatix.
AUTHOR CONTRIBUTIONS
Aditi Bhanja, Tuna Hayirli, Nicholas Stark, James Hardy, Christopher R. Peabody, and Michaela Kerrissey conceived the study and designed the trial. Aditi Bhanja, Tuna Hayirli, Nicholas Stark, James Hardy, Christopher R. Peabody, and Michaela Kerrissey supervised the conduct of the trial and data collection. Aditi Bhanja, Tuna Hayirli, Nicholas Stark, James Hardy, Christopher R. Peabody, and Michaela Kerrissey undertook recruitment of participants and managed the data, including quality control. Aditi Bhanja and Michaela Kerrissey provided statistical advice and analyzed the data. Aditi Bhanja drafted the manuscript, and all authors contributed substantially to its revision. All authors take responsibility for the paper as a whole.
Supporting information
Supporting Information
Biography
Aditi Bhanja is a Research Advisor for the Women's Refugee Commission in New York, New York.

Bhanja A, Hayirli T, Stark N, Hardy J, Peabody CR, Kerrissey M. Team and leadership factors and their relationship to burnout in emergency medicine during COVID‐19: A 3‐wave cross‐sectional study. JACEP Open. 2022;3:e12761. 10.1002/emp2.12761
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Henry Wang, MD, MS.
REFERENCES
- 1. Lin M, Battaglioli N, Melamed M, Mott SE, Chung AS, Robinson DW. High prevalence of burnout among US Emergency Medicine Residents: results from the 2017 National Emergency Medicine Wellness Survey. Ann Emerg Med. 2019;74(5):682‐690. 10.1016/j.annemergmed.2019.01.037 [DOI] [PubMed] [Google Scholar]
- 2. Chor WPD, Ng WM, Cheng L, et al. Burnout amongst emergency healthcare workers during the COVID‐19 pandemic: a multi‐center study. Am J Emerg Med. 2021;46:700‐702. 10.1016/j.ajem.2020.10.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rodriguez RM, Montoy JCC, Hoth KF, et al. Symptoms of anxiety, burnout, and PTSD and the mitigation effect of serologic testing in emergency department personnel during the COVID‐19 pandemic. Ann Emerg Med. 2021;78(1):35‐43.e2. 10.1016/j.annemergmed.2021.01.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gualano MR, Sinigaglia T, Lo Moro G, et al. The burden of burnout among healthcare professionals of intensive care units and emergency departments during the COVID‐19 pandemic: a systematic review. Int J Environ Res Public Health. 2021;18(15):8172. 10.3390/ijerph18158172. Published 2021 Aug 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kerrissey MJ, Singer SJ, Leading frontline COVID‐19 teams: research‐informed strategies. NEJM Catal Innov Care Deliv. 2020. [Google Scholar]
- 6. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516‐529. 10.1111/joim.12752 [DOI] [PubMed] [Google Scholar]
- 7. Sangal RB, Wrzesniewski A, DiBenigno J, et al. Work team identification associated with less stress and burnout among front‐line emergency department staff amid the COVID‐19 pandemic. BMJ leader. 2021;5(1):51‐54. 10.1136/leader-2020-000331 [DOI] [Google Scholar]
- 8. Teo WL, Lee M, Lim W‐S, The relational activation of resilience model: how leadership activates resilience in an organizational crisis. J Contingencies Crisis Manag. 2017;25(3):136‐147. 10.1111/1468-5973.12179 [DOI] [Google Scholar]
- 9. Hu J, Liden R, Antecedents of team potency and team effectiveness: an examination of goal and process clarity and servant leadership. J Appl Psychol. 2011;96:851‐862. 10.1037/a0022465 [DOI] [PubMed] [Google Scholar]
- 10. Sawyer JE. Goal and process clarity: specification of multiple constructs of role ambiguity and a structural equation model of their antecedents and consequences. J Appl Psychol. 1992;77(2):130‐142. 10.1037/0021-9010.77.2.130 [DOI] [Google Scholar]
- 11. Stark N, Kerrissey M, Grade M, Berrean B, Peabody C. Streamlining care in crisis: rapid creation and implementation of a digital support tool for COVID‐19. West J Emerg Med. 2020;21(5):1095‐1101. 10.5811/westjem.2020.7.48537. Published 2020 Aug 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hayirli TC, Stark N, Bhanja A, Hardy J, Peabody CR, Kerrissey MJ. Masked and distanced: a qualitative study of how personal protective equipment and distancing affect teamwork in emergency care. Int J Qual Health Care. 2021;33(2):mzab069. 10.1093/intqhc/mzab069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kerrissey MJ, Mayo AT, Edmondson AC. Joint problem‐solving orientation in fluid cross‐boundary teams. Academy of Management Discoveries; 2021. 10.5465/amd.2019.0105 [DOI] [Google Scholar]
- 14. Nembhard IM, Edmondson AC. Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J Organ Behav. 2006;27(7):941‐966. 10.1002/job.413 [DOI] [Google Scholar]
- 15. Kerrissey MJ, Hayirli TC, Bhanja A, Stark N, Hardy J, Peabody CR. How psychological safety and feeling heard relate to burnout and adaptation amid uncertainty. Health Care Manage Rev. 2022. 10.1097/HMR.0000000000000338. [published online ahead of print, 2022 Feb 7]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. San Francisco Public Health Department; 2020–2021; COVD‐19 Cases and Deaths; https://sf.gov/data/covid‐19‐cases‐and‐deaths
- 17. Dolan ED, Mohr D, Lempa M, et al. Using a single item to measure burnout in primary care staff: a psychometric evaluation. J Gen Intern Med. 2015;30(5):582‐587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kellerman SE, Herold J. Physician response to surveys: a review of the literature. Am J Prev Med. 2001;20(1):61‐67. 10.1016/S0749-3797(00)00258-0 [DOI] [PubMed] [Google Scholar]
- 19. DiBenigno J, Kerrissey M. Structuring mental health support for frontline caregivers during COVID‐19: lessons from organisational scholarship on unit‐aligned support. BMJ Leader. 2020;4(3):124. 10.1136/leader-2020-000279 [DOI] [Google Scholar]
- 20. Ahmed F, Zhao F, Faraz NA, Qin YJ. How inclusive leadership paves way for psychological well‐being of employees during trauma and crisis: a three‐wave longitudinal mediation study. J Adv Nurs. 2021;77(2):819‐831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rodriguez RM, Medak AJ, Baumann BM, et al. Academic emergency medicine physicians' anxiety levels, stressors, and potential stress mitigation measures during the acceleration phase of the COVID‐19 pandemic. Acad Emerg Med. 2020;27(8):700‐707. 10.1111/acem.14065 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


