Objectives
This was a retrospective analysis of the epidemiological features of pediatric intussusception, the effects of different management strategies and the factors affecting successful reduction.
Methods
Using our hospital database, data on pediatric intussusception from January 2019 to December 2020 were extracted for analysis, including demographic data, size of intussusception, treatment method, and effects.
Results
The number of children diagnosed with intussusception was 726 (782 episodes). In all, 394 (54.27%) of these children were male. The male to female ratio was 1.19:1. The peak of the onset age was between 3 and 4 years. In the single intussusception group, the successful reduction rate of cleansing enemas was 65.25%, that of air enemas was 95.80%, and that of B-ultrasound–guided hydrostatic enemas (B-USGHEs) was 96.04%. In the multiple intussusceptions group, the successful reduction rate of cleansing enemas was 43.9%, air enemas were 75%, and B-USGHE was 57.6%. There were no significant differences between the air enema and B-USGHE groups. The diameter and length were related factors influencing successful reduction (P ≤ 0.05). Fifty-three (7.53%) children had recurrent intussusception within 4 years, and all of them were following successful enemas. Thirty-one (3.40%) episodes were found to have spontaneously reduced. Five patients (0.7%) underwent surgery after the failure of air enemas or B-USGHE.
Conclusions
Pediatric intussusception in our region showed a sex ratio difference and age difference of onset. For single intussusceptions and multiple intussusceptions, the successful reduction rate of cleansing enemas means that some children may avoid radiation exposure. The diameter and length of intussusception were related factors influencing successful reduction in cleansing enema. There were no significant differences in successful reduction between air enemas and B-USGHE. Most recurrent intussusceptions can still be reduced, avoiding surgery.
Key Words: intussusception, epidemiology, enema, diameter
Intussusception is one of the most common causes of abdominal pain and vomiting in infants and children. Its etiology and management have changed significantly over the last decades. Hypertrophic Peyer patches, polyps, seasonality, viral factors and postnatal changes in the enteric nervous system have been considered responsible. Nonsurgical treatment is the first-line management at present, with a high reduction rate. Currently, there are numerous methods of treatment for intussusception management. The purpose of the study is to analyze the characteristics of intussusception in children and to evaluate the effects of different management strategies, to initiate appropriate treatment as early as possible and to protect intussuscepted children from medicinal injury.
METHODS
Study Design
The flowchart (Fig. 1) for the management of pediatric intussusception was performed in our hospital for 3 years. This retrospective study reviewed data of younger than 12 years from our hospital database who were diagnosed with intussusception and managed with cleansing enemas, air enemas, or B-ultrasound–guided hydrostatic enemas (B-USGHE) from January 2019 to December 2020. Children who were given a detailed B-ultrasound description of the ultrasound parameters of intussusception were categorized into 4 groups based on the reduction methods. The data extracted included demographic data (sex, age, date of onset, and date of birth), size of intussusception (transverse diameter and longitudinal length of the involved segment), treatment method, and effects. The diagnosis of intussusception was determined by high-frequency ultrasound, with a descriptive report given in our hospital that included transverse diameter, length of involved segment, number and location of the intussusception, but these data may lack in other hospitals. Single intussusception means that only 1 intussusception was found by B-ultrasound. Multiple intussusceptions refer to the discovery of more than 2 intussusceptions at a time. Recurrent intussusception refers to children with repeated attacks within an uncertain time, and age statistics were evaluated according to the time of first attack. Children with peritonitis and ileus and delayed symptoms for more than 48 hours were prohibited from undergoing any enema treatment.
FIGURE 1.
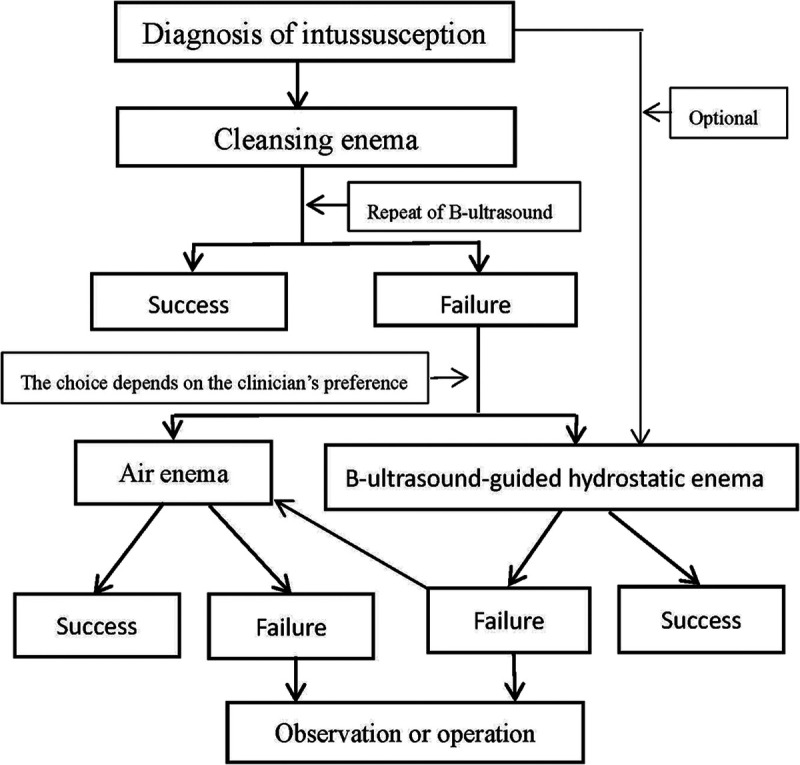
Flowchart of pediatric intussusception treatment.
Therapeutic Method
The cleansing enema was used as routine bowel preparation before performing an air enema without imaging guidance. We found that some pediatric intussusceptions had been reduced after cleansing enema on repeat of the B-ultrasound. Thus, we have taken it as one of the routine methods of intussusception reduction. The cleansing enema was performed by a nurse. First, using glycerin (10–20 mL) helps children defecate once before cleansing enemas. The child was placed in the left lateral decubitus position or lithotomy position with hips raised to 30°. The height of enema barrel from anus was 30 to 60 cm. Then, normal saline was heated to 35°C to 40°C and slowly dripped into the colon by an enema tube (12F–16F silicone catheter) with a depth of 6 to 8 cm under the influence of gravity, and the dropping rate and filling volume were adjusted according to the pressure in the rectum. The dropping time of liquid depended on the pressure in the rectum and the height of enema barrel, which usually took about 5 minutes. The enema volume should be calculated as 30 mL/kg body weight in children, and the total saline volume should not exceed 500 mL, which could be divided into approximately 200 mL each time to drop if there was a resistance in the rectum. The child was checked again by B-ultrasound after excreting liquid. Next, an air enema or B-USGHE was performed if the intussusception was still ongoing. Air enemas were performed by a radiologist under a fluoroscopic monitor. A Foley catheter (12F–16F) was inserted in the rectum of the patient and was fixed after inflation to prevent air leakage. The pressure was controlled between 6 and 10 kPa by automatic control gas injection equipment. A successful air enema depended on a radiology report, typically demonstrating reduction of the ileocolic intussusception with reflux of air into the terminal ileum and distal small bowel visualized directly by fluoroscopy. B-USGHE was performed by a sonographer under ultrasound guidance. Similarly, a Foley catheter was inserted in the rectum of the child and was fixed after inflation to prevent normal saline leakage. The height of enema barrel from anus was 60 to 100 cm (converted to pressure, 6–10 kPa), and the height and filling volume were adjusted according to the movement of intussusception head under the B-ultrasonic monitoring. The temperature of normal saline was heated to 35°C to 40°C. A successful reduction was considered when the fluid administered was seen to have passed the cecum and been distributed in the small intestine, and no intussusception was found again by B-ultrasound examination. Also, abdominal pain and vomiting abated.
Statistical Analysis
All data handling and statistical analyses were performed using SPSS 23.0 (IBM, Chicago, IL). Statistical significance was set at a P value of 0.05 or less. Continuous variables are presented as the mean ± standard deviation. An independent-samples t test and one-way analysis of variance (ANOVA) were applied for continuous variables. Categorical variables were compared with χ2 and Fisher exact tests.
This was a retrospective study that did not involve clinical trial. It was exempted by the institutional review board of the hospital because of the retrospective nature of the study.
RESULTS
Demographics and Characteristics of Sex and Age
A retrospective study was performed with a total of 726 children (782 episodes) managed for intussusception between January 2019 and December 2020. Most children came to the hospital within 24 hours of symptom onset. In all, 394 (54.27%) children were boys. The male-to-female ratio was 1.19:1. The mean age of all children was 3.86 ± 1.85 years (range, 2 months to 12 years). The majority of cases were younger than 4 years. Of them, the highest percentage occurred in children aged between 3 and 4 years (n = 332; 42.46%), and only 8.7% of children were younger than 1 year. The basic characteristics of the children are shown in Table 1.
TABLE 1.
Basic Characteristics of the Children Studied
| Characteristics | Children, n (%) | Episodes, n (%) |
|---|---|---|
| Sex | ||
| Male | 394 (54.27) | 434 (55.50) |
| Female | 332 (45.73) | 348 (44.50) |
| Total | 726 | 782 |
| 0–1 y | 65 (8.95) | 68 (8.70) |
| 2 y | 113 (15.56) | 126 (16.11) |
| 3 y | 145 (19.97) | 157 (20.08) |
| 4 y | 162 (22.31) | 175 (22.38) |
| 5+ y | 241 (33.20) | 256 (32.74) |
| Single intussusceptions | 678 (93.39) | 731 (93.48) |
| Multiple intussusceptions | 48 (6.61) | 51 (6.52) |
| Recurrent children | 53 (7.30) | 117 (14.96) |
| Detail size of intussusceptions | ||
| Single intussusceptions | 476 (90.84) | 519 (91.05) |
| Multiple intussusceptions | 48 (9.16) | 51 (8.95) |
| Total | 524 | 570 |
| Treatment | ||
| Cleansing enema | 683 | 728 |
| Air enema | 113 | 119 |
| B-USGHE | 97 | 101 |
| Spontaneous reduction | 31 (4.53) | 31 (3.40) |
| Operation | 5 (0.7) | |
Reduction Effects of Different Procedures
Single intussusception represented 731 (93.48%) of the total episodes of intussusception. Among them, 728 episodes had a cleansing enema, with a successful reduction rate of 65.25% (475/728); 119 episodes had an air enema, with a successful reduction rate of 95.80% (114/119); and 101 episodes had a B-USGHE, with a successful reduction rate of 96.04% (97/101). The χ2 test showed that there were significant differences between the cleansing enema, air enema, and B-USGHE groups (P = 0.000). There were no significant differences between the air enema and B-USGHE groups.
Multiple intussusceptions represented 51 (6.52%) of the total episodes of intussusception. Among them, 41 episodes had a cleansing enema, with a successful reduction rate of 43.9% (18/41); 16 episodes had an air enema, with a successful reduction rate of 75% (12/16); and 9 episodes had a B-USGHE, with a successful reduction rate of 88.88% (8/9). The χ2 test showed that there were significant differences between the cleansing enema, air enema, and B-USGHE groups (P = 0.02). There were no significant differences between the air enema and B-USGHE groups.
The successful reduction rate of cleansing enemas in single intussusception was higher than that in multiple intussusceptions. There was a significant difference between them (P = 0.01).
Influencing Factors of Intussusception Reduction
Of 782 episodes of intussusception, there were 570 episodes with a descriptive report that included the diameter, length of involved segment, and number of intussusceptions. Statistical analysis was performed on the relationship between the reduction rate and size of intussusception among the different groups (Table 2). There were 519 episodes of single intussusception that were categorized into 4 groups based on the reduction method, which included cleansing enema, air enema, B-USGHE, and spontaneous reduction groups. The mean diameter of intussusception with successful reduction was smaller than that with failed reduction in the cleansing enema group, air enema group, and B-USGHE group. There were significant differences between them in the cleansing enema group and B-USGHE group (P < 0.001), but not in air enema group (P ≤ 0.05). The mean length of intussusception with successful reduction was smaller than that with failed reduction in the cleansing enema group, air enema group, and B-USGHE group. There were significant differences between them in the cleansing enema group (P < 0.001), but not in air enema group and B-USGHE group (P ≤ 0.05). One-way ANOVA and t test showed that diameter, length, and different enema methods were related factors influencing successful reduction (P ≤ 0.05). There were no significant differences in failed reduction (P > 0.05). The mean diameter of air enemas with successful reduction was larger than that of cleansing enemas, B-USGHE, and spontaneous reduction, and there were significant differences between them (P ≤ 0.05). There was no significant difference in diameter between spontaneous reduction, B-USGHE, and cleansing enemas (P > 0.05). The mean length in air enemas with successful reduction was larger than that in cleansing enemas, B-USGHE, and spontaneous reduction, and there was a significant difference between them (P ≤ 0.05). There was no significant difference between cleansing enemas, B-USGHE, and spontaneous reduction (P > 0.05).
TABLE 2.
Size Comparisons of Single Intussusceptions
| Cleansing enema | Air enema | B-UGHE | Spontaneous Reduction | |||||
|---|---|---|---|---|---|---|---|---|
| Diameter (519) | Length (369) | Diameter (113) | Length (93) | Diameter (71) | Length (54) | Diameter (25) | Length (25) | |
| Reduction | 20.30 ± 5.36 (311) | 30.20 ± 10.22 (208) | 27.55 ± 7.93 (109) | 39.52 ± 13.43 (89) | 23.75 ± 7.76 (68) | 33.47 ± 11.72 (51) | 20.84 ± 5.66 (25) | 33.92 ± 7.76 (25) |
| No reduction | 25.66 ± 8.22 (208) | 37.48 ± 12.78 (161) | 32.5 ± 10.4 (4) | 43.25 ± 14.36 (4) | 35 ± 16.7 (3) | 44.00 ± 21.00 (3) | ||
| t Test | t = 84.76 P = 0.000 | t = 5.74, P = 0.000 | t = 0.15 P = 0.23 | t = 0.000 P = 0.59 | t = 4,199 P = 0.02 | t = 1.165 P = 0.15 | ||
| Reduction | One-way ANOVA: diameter, Tamhane T α = 36.83, P = 0.00. Length: Tamhane T α = 14.62, P = 0.000 | |||||||
| No reduction | One-way ANOVA: diameter, LSD α 3.10, P = 0.05. Length: LSD α = 0.74, P = 0.48 | |||||||
There were 51 episodes of multiple intussusceptions, and the number of intussusceptions was 105 in total. For successful reduction, the mean diameter of single intussusception was 22.45 ± 7.15 mm and that of multiple intussusceptions was 20.60 ± 4.96 mm. There was a significant difference between them (P = 0.002). The mean length of single intussusception was 33.41 ± 11.95 mm and that of multiple intussusceptions was 32.12 ± 10.17 mm. There was no significant difference between them (P = 0.467).
Recurrent Intussusception and Surgery
Fifty-three (7.53%) children, with 117 (14.96%) episodes, had recurrent intussusception, and all of them were following successful reduction enemas. The age of 53 patients at the first intussusception ranged from 10 months to 8 years (median, 33.06 ± 17.86 months), and the interval between attacks ranged 1 day to 21 months. Thirty-one (3.40%) episodes were found to have spontaneously reduced. Five patients (0.7%) underwent surgery after the failure of an air enema or B-USGHE. There was neither perforation nor mortality (Table 1).
DISCUSSION
Most pediatric intussusceptions are primary intussusceptions and are usually classified into 6 types: ileocolic, ileo-ileocolic, colocolic, ileo-colo-colic, ileo-ileal, and jejuno-jejunum. The ileocolic type is the most common intussusception. Intussusception can be divided into single intussusception and multiple intussusceptions according to the number. Most of the single intussusceptions are considered to be the ileocolic, ileo-ileocolic, or colocolic type, and a few may be the ileo-ileal or jejuno-jejunum type. Most multiple intussusceptions are considered to be ileo-ileal or jejuno-jejunum type, and some of them may be mixed with ileocolic intussusception. Abdominal pain is the most frequent presenting symptom of intussusception, and it is not always accompanied by vomiting. Sometimes, vomiting is the only symptom.
There were great significant differences in age and sex composition with regard to the onset of intussusception. In Chinese documents, it is usually considered that more than half of intussusceptions occur in infants younger than 1 year old (32–83%), with a peak at 4 to 10 months, and the incidence is rare in infants younger than 3 months and in children older than 5 years. The male-to-female ratio is approximately 1.7 to 1.9:1.1,2 In Korea, male to females was recently reported to be 1.4 to 1.8:1, and the highest percentage was in infants aged between 2 and 36 months.3,4 Previous studies have shown that there are great differences between different races and regions. In foreign countries, range was from 1.6 to 2.1:1.5 In the current data, the male to female ratio was 1.19:1; only 8.95% of patients were younger than 1 year, and 36.19% of patients were between 1 and 3 years old, with a peak at 3 to 4 years old. The mean age of all children was 3.85 ± 1.84 years. In our district, all children with abdominal pain or vomiting were checked by high-frequency B-ultrasound. It is not clear whether the incidence of intussusception is increasing in older children or whether more intussusception is found by B-ultrasound routine use. Some studies had the same understanding due to an increase in the routine use of ultrasound for children with abdominal pain.6,7
The recurrence rate of intussusception varies greatly, with reported rates of 2% to 20%. The incidence of pathological lead point (PLP) in all children with intussusception was 3.9% to 10%. PLP was present in 14% of the children who had 2 or more recurrences compared with 4% of those children who had only 1 recurrence.5,8–12 There is universal consensus that PLP is a risk factor for recurrence. Instead, some documents think that the rates of PLP among children with 1 or more episodes of intussusception is similar, and there is no association between recurrent intussusceptions and PLP.9 The enema success rate of recurrent intussusceptions was 96% to 100%.11,13,14 In the current data, 53 (7.53%) children had recurrent intussusception within the age from 10 months to 8 years, all of which were after successful enema or conservative treatment. Nonoperative treatment was still the first choice, regardless of which treatment they have previously received.9,14
Nonoperative reduction should be attempted in most patients with acute primary intussusception. Air enema reduction under fluoroscopy or B-USGHE has been the main procedure. The reduction success rate based on published literature achieved at least 80% and even as high as 100%.5,12,14–16 In our data, there was a cleansing enema for intussusception reduction that was initially used for intestinal preparation before an air enema. We occasionally found that some intussusceptions were reduced after cleansing enema on repeat B-ultrasound. For single intussusception, the success rate of cleansing enema was 65.25%, that of air enema was 95.80% and that of B-USGHE was 96.04%, meanwhile, the success rate of cleansing enema was 43.90%, the of air enema was 75.00% and that of B-USGFE was 57.60% for multiple intussusceptions. There was no difference in success rate between the air enema group and the B-USGHE group. Although the success rate in the cleansing enema group was lower than that in the air enema and B-USGHE groups, it had great significance in protecting some children from radiation exposure and avoiding unnecessary suffering.
What is the association between the diameter, length of intussusception and the successful reduction rate? Ultrasound has a high sensitivity of 95% to 100% and specificity of 78% to 100%.5,17 Spontaneous reduction of intussusception, which is usually limited to the small bowel, has been frequently found by high-frequency ultrasound. Ultrasound plays an important role in the management of intussusception. In the current data, the diameter and length were the factors affecting the success rate in the cleansing enema. One-way ANOVA showed that the diameter and length were not significant differences between spontaneous reduction, B-USGHE and cleansing enemas. So, the hydrostatic pressure were the factors affecting the success rate between B-USGHE and cleansing enemas. Intussusception with a diameter of approximately 20 mm was more easily reduced spontaneously. The cleansing enema was effective because the warm normal saline (35–40°C) used for it may play an important role, except for hydrostatic pressure, which helped intussusception to reduce spontaneously by relieving spasm of the intestinal smooth muscle. Therefore, cleansing enemas might exert therapeutic effects in both single and multiple intussusceptions. Some multiple intussusceptions might become single intussusceptions after cleansing enema in practice and then be reduced by air or B-USGHE. Length was not the factor affecting the success rate in the air enema and B-USGHE groups. Diameter was the factor affecting the success rate in the B-USGHE groups, but not in air enema. Although the mean diameter and length of intussusception in air enemas were larger than that in the B-USGHE, there may be a deviation because of the nature of the retrospective studies. A further prospective study is needed to confirm the observation and improve the evidence.
The mean diameter of single intussusception was larger than that of multiple intussusceptions. This means that multiple intussusceptions may be mainly small intussusceptions. Park et al6 reported that the mean diameter was 16.8 ± 5.2 mm with small bowel intussusception and 27.4 ± 4.3 mm with ileocolic intussusception. Demirel et al13 reported that the mean length of spontaneously reduced intussusception was 23 ± 3.02 mm, and the median length of successful hydrostatic reduced intussusception was 45 mm (range, 27–160 mm). Rajagopal et al18 reported that the mean diameter of intussusception requiring surgical reduction was 33 mm (range, 29–54 mm), and the length was 56 mm (range, 23–78 mm). The mean diameter of transient small bowel intussusception was 12 mm (range, 8–23 mm), and the length was 22.5 mm (range, 18–45 mm). The assessment of the intussusception size by B-ultrasound examination may be useful in the management of intussusception.
There is not much evidence to support that air enemas may be more effective than hydrostatic enemas for reducing intussusception in children.19 The greatest advantage of B-USGHE is that it does not involve radiation exposure in children; therefore, reduction can be attempted repeatedly and patiently. The successful reduction rate is determined by local management patterns, selection criteria, and the skill of operators. In the current data, only 5 (0.7%) children underwent emergency surgery after failed reduction, and we did not determine how many children underwent surgery due to underlying causes in a later period of time by follow-up.
CONCLUSIONS
Pediatric intussusception in our region showed a sex ratio difference and age difference of onset. More and more intussusception in children with abdominal pain might be found by B-ultrasound examination. Not all pediatric intussusceptions must be reduced by air enema or B-USGHE. For single and multiple intussusceptions, the successful reduction rate of cleansing enemas with warm saline meant that some children may avoid radiation exposure and unnecessary suffering. The diameter and length of intussusception were related factors influencing successful reduction in the cleansing enema. There might be no statistically significant differences in the successful reduction between air enemas and B-USGHE. The length was not the factor affecting the success rate in the air enema and B-USGHE. Whether the diameter is a factor affecting intussusception reduction needs to be confirmed by a further prospective study. Most recurrent intussusceptions can still be reduced by nonoperative methods. This study was limited by the nature of retrospective studies and the single-center design.
Footnotes
Disclosure: The authors declare no conflict of interest.
Contributor Information
Guoxin Song, Email: sgxx2005@126.com.
Dandan Lian, Email: liandandan@hotmail.com.
Qingsong Zhang, Email: 46227927@qq.com.
Lei Dong, Email: leid1030@163.com.
REFERENCES
- 1.Tang XB Hu DY Mu XQ, et al. Association of air temperature with pediatric intussusception in northeastern China: a 10-year retrospective study. Am J Emerg Med. 2021;42:211–216. [DOI] [PubMed] [Google Scholar]
- 2.Guo WL Zhang SF Li JE, et al. Association of meteorological factors with pediatric intussusception in subtropical China: a 5-year analysis. PLoS One. 2014;9:e90521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jo S Lim IS Chae SA, et al. Characteristics of intussusception among children in Korea: a nationwide epidemiological study. BMC Pediatr. 2019;19:211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hwang S Kim J Jung JY, et al. The epidemiology of childhood intussusception in South Korea: an observational study. PLoS One. 2019;14:e0219286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ito Y Kusakawa I Murata Y, et al. Japanese guidelines for the management of intussusception in children, 2011. Pediatr Int. 2012;54:948–958. [DOI] [PubMed] [Google Scholar]
- 6.Park BL, Rabiner JE, Tsung JW. Point-of-care ultrasound diagnosis of small bowel-small bowel vs ileocolic intussusception. Am J Emerg Med. 2019;37:1746–1750. [DOI] [PubMed] [Google Scholar]
- 7.Levinson H Capua T Scolnik D, et al. Comparison between small and large bowel intussusception in children: the experience of a large tertiary care pediatric hospital. Pediatr Emerg Care. 2020;36:e189–e191. [DOI] [PubMed] [Google Scholar]
- 8.Özcan R Hüseynov M Emre Ş, et al. A review of intussusception cases involving failed pneumatic reduction and re-intussusception. Ulus Travma Acil Cerrahi Derg. 2016;22:259–264. [DOI] [PubMed] [Google Scholar]
- 9.Cho MJ Nam CW Choi SH, et al. Management of recurrent ileocolic intussusception. J Pediatr Surg. 2020;55:2150–2153. [DOI] [PubMed] [Google Scholar]
- 10.Shen G Liu H Guan Z, et al. Clinical features and factors leading to early recurrence of intussusception after saline reduction. J Pak Med Assoc. 2020;70:1727–1730. [DOI] [PubMed] [Google Scholar]
- 11.Ma GMY, Lillehei C, Callahan MJ. Air contrast enema reduction of single and recurrent ileocolic intussusceptions in children: patterns, management and outcomes. Pediatr Radiol. 2020;50:664–672. [DOI] [PubMed] [Google Scholar]
- 12.Talabi AO Famurewa OC Bamigbola KT, et al. Sonographic guided hydrostatic saline enema reduction of childhood intussusception: a prospective study. BMC Emerg Med. 2018;18:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Demirel BD Hancioğlu S Dağdemir B, et al. Ultrasound-guided hydrostatic reduction of ileo-colic intussusception in childhood: first-line management for both primary and recurrent cases. Acta Chir Belg. 2021;1–5. [DOI] [PubMed] [Google Scholar]
- 14.Simon NM Joseph J Philip RR, et al. Intussusception: single center experience of 10 years. Indian Pediatr. 2019;56:29–32. [PubMed] [Google Scholar]
- 15.Xiaolong X Yang W Qi W, et al. Risk factors for failure of hydrostatic reduction of intussusception in pediatric patients: a retrospective study. Medicine (Baltimore). 2019;98:e13826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xie X Wu Y Wang Q, et al. A randomized trial of pneumatic reduction versus hydrostatic reduction for intussusception in pediatric patients. J Pediatr Surg. 2018;53:1464–1468. [DOI] [PubMed] [Google Scholar]
- 17.Bines JE Ivanoff B Justice F, et al. Clinical case definition for the diagnosis of acute intussusception. J Pediatr Gastroenterol Nutr. 2004;39:511–518. [DOI] [PubMed] [Google Scholar]
- 18.Rajagopal R Mishra N Yadav N, et al. Transient versus surgically managed small bowel intussusception in children: role of ultrasound. Afr J Paediatr Surg. 2015;12:140–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gluckman S Karpelowsky J Webster AC, et al. Management for intussusception in children. Cochrane Database Syst Rev. 2017;6:CD006476. [DOI] [PMC free article] [PubMed] [Google Scholar]


