Abstract
BACKGROUND
Spontaneous spinal subdural hematomas (SSDHs) are unusual. Among their probable etiologies, an association with ruptured brain aneurysms has been described in an extraordinary way. The underlying pathophysiological mechanism is not conclusively described in the literature.
OBSERVATIONS
The authors reported an exceptional case of a 59-year-old woman admitted for a condition that included sudden headache, stiff neck, and vomiting associated with pain in the left flank area that radiated to the leg. Computed tomography (CT) of the brain evidenced acute subarachnoid hemorrhage distributed in the bilateral posterior parieto-occipital fossa and occipital horns of the ventricles. CT angiography detected a dissecting aneurysm in the left vertebral artery (V4) that was treated urgently via the endovascular route. In the next hours, the patient’s symptoms worsened, with paraplegia of the lower extremities. Magnetic resonance imaging showed SSDH at T4–6 and extensive associated myelopathy.
LESSONS
The origin of the spinal hematoma may be the rupture of the aneurysm of the V4 segment in the dura mater of the foramen magnum and subsequent rostrocaudal migration of the hemorrhage to the spinal subdural space, enhanced by an intracranial pressure increase. This hypothesis is discussed, as is a brief literature review.
Keywords: angiography, intradural aneurysm, spontaneous spinal subdural hematoma, subarachnoid hemorrhage, transarterial embolization
ABBREVIATIONS : CT = computed tomography, MRI = magnetic resonance imaging, SAH = subarachnoid hemorrhage, SSDH = spinal subdural hematoma
Intraspinal hematomas are uncommon. They fall into three categories: intramedullary, subdural, and extradural. The most uncommon are hematomas located in the spinal subdural space, which account for less than 5% of the total.1 According to their etiology, spinal subdural hematomas (SSDHs) can be classified as traumatic, secondary, or idiopathic. The secondary ones have a variety of causes, such as vasculitis, coagulation disorders, anticoagulants, lumbar punctures, surgeries, vascular malformations, and tumors.2 We report an exceptional clinical case in which the presence of an SSDH is associated with intracranial vertebral artery aneurysm rupture and discuss its probable relationship.
Illustrative Case
A 59-year-old female patient with hypertension and dyslipidemia presented to the emergency department with headache and vomiting that had started 3 days earlier. On the day of admission, the patient reported severe left dorsal pain of metameric distribution. On initial examination, she had high blood pressure levels (175/99 mm Hg), stiff neck, and left Babinski’s sign.
Baseline computed tomography (CT) of the brain evidenced subarachnoid hemorrhage (SAH) of infratentorial predominance, bilateral parieto-occipital sulci, and slight hemoventricle. In addition, it was associated with a mega cisterna magna as a variant of normality (Fig. 1). Her Hunt and Hess scale score was 1 and the modified Fisher scale score was 2. Intracranial and supraaortic trunk CT angiography demonstrated the presence of a dissecting aneurysm in the left vertebral artery (V4), which was confirmed on angiography (Fig. 2) and was treated urgently via endovascular embolization with two coils. During the procedure, the origin of the posterior inferior cerebellar artery was preserved, and no incidents or contrast extravasation was recorded. No anticoagulation drugs were administered during the procedure or the postoperative period.
FIG. 1.
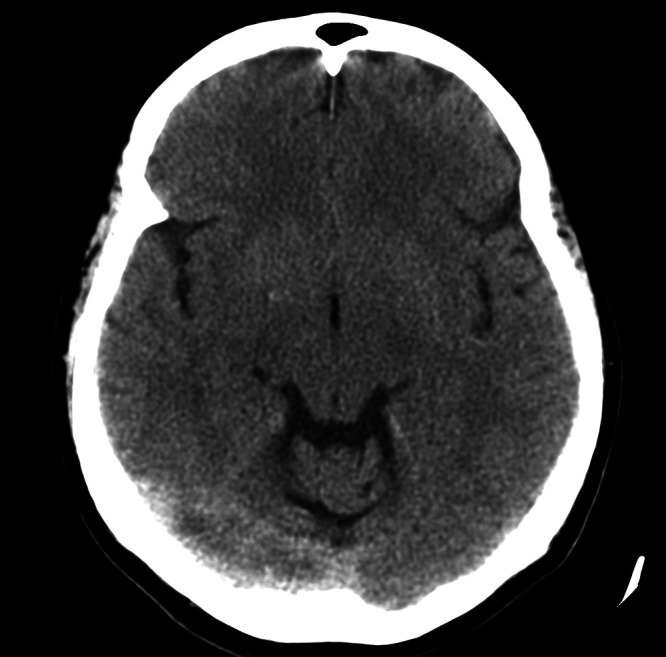
CT of the brain. Axial section. Diffuse SAH of right infratentorial predominance is visible.
FIG. 2.
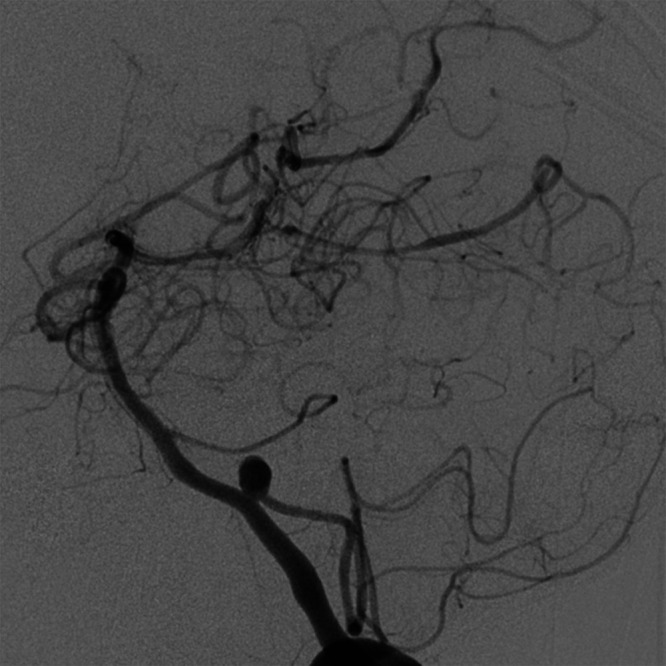
Brain arteriography before treatment. Work projection. A 4.5-mm dissecting aneurysm of the left vertebral artery gives origin to the right posterior inferior cerebellar artery.
The patient was extubated in the ward and admitted to the intensive care unit, where rapidly progressive flaccid paraparesis of the lower extremities was established at 12 hours. It progressed to complete paraplegia, associated with the sensory level at T6, anesthesia in the lower extremities, global sphincter incontinence, atony of the anal sphincter, and abolition of abdominal-cutaneous reflexes. No lumbar puncture or any other type of dural puncture was performed during this period. Because acute spinal cord syndrome was suspected, spinal magnetic resonance imaging (MRI) was requested. It showed SSDH from the cervical level to T6, with extensive myelopathy (Fig. 3). The patient underwent emergency surgery in which we performed a laminectomy and drained the hematoma. Complete spinal cord arteriography performed 7 days later did not show other vascular lesions. Extensive laboratory tests were performed to rule out other described causes of SSDH, such as collagen diseases or coagulation disorders.
FIG. 3.
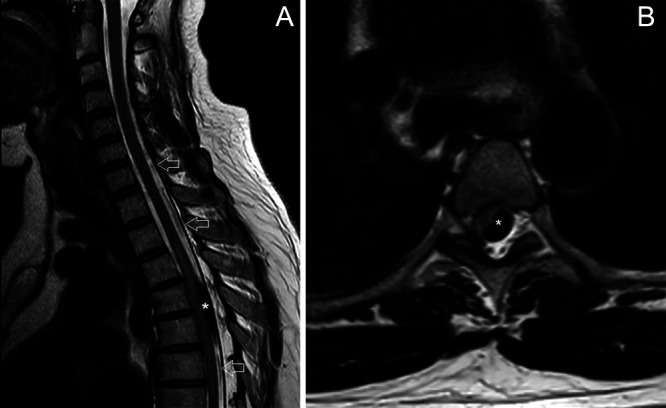
Spinal MRI. Sagittal (A) and axial (B) sections. A subdural hematoma (asterisks) that caused significant displacement of the spinal cord and hyperintense spinal area at T3–6 levels is shown. Continuity of the hematoma is seen several levels above and below the hematoma (white arrows).
The patient, who had experienced sudden-onset back pain since the start of the condition and had Babinski’s sign on examination, was likely to have concomitant or sequential SAH and SSDH. However, treatment of the brain aneurysm was prioritized and the spinal injury went unnoticed in the first hours. The patient was subsequently admitted to a center that specialized in spinal injuries, and her condition improved progressively. After 12 months of rehabilitation therapy, she could walk with aid, and the sensitivity of her lower extremities and sphincter disorder had improved remarkably (modified Rankin scale score of 3). New complete brain arteriography was then performed, which evidenced stability of the embolized aneurysm (Fig. 4) with no other associated vascular lesions. Finally, the rupture of the V4 aneurysmal lesion was considered to be responsible for the brain SAH and the SSDH.
FIG. 4.
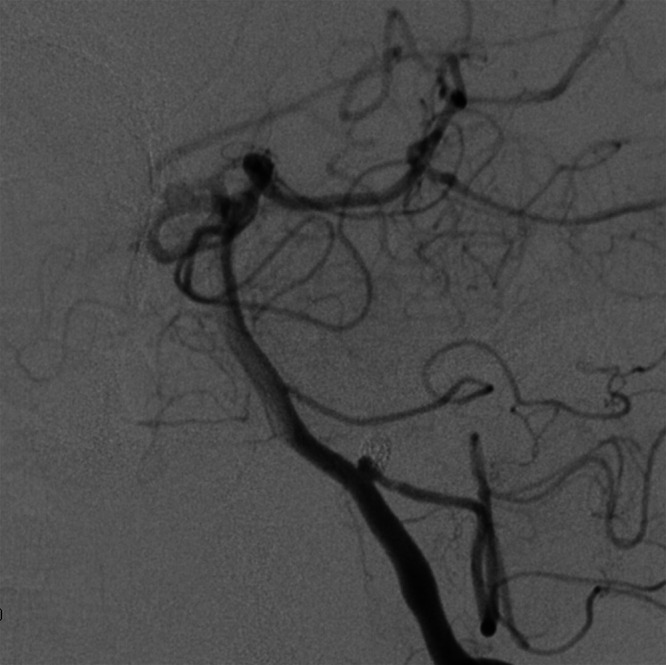
Control arteriography of the brain at 12 months. Work projection. Coil embolization of vertebral aneurysm shows minimum residual neck and complete patency of the right posterior inferior cerebellar artery.
Discussion
Spinal hematomas are an uncommon condition and require early diagnosis to prevent a spinal cord compression syndrome that causes irreversible injuries. The most common form of spontaneous intraspinal hemorrhage occurs in the extradural space, whereas SSDH is much rarer because, unlike the intracranial space, the spinal subdural space is completely avascular.3 A hemorrhage can expand from the subarachnoid space to the subdural space as a result of rupture of the subarachnoid membrane, which takes place in approximately 0.5% to 7.9% of cases.4 Several mechanisms have been proposed to explain the occurrence of this event after rupture of an aneurysm:5 adhesion of the aneurysm to arachnoid granulations, which causes lacerations in it due to repeated microbleeding and allows blood to enter the subdural space, and a tear of the pia-arachnoid due to a pressure increase, with blood extravasation to the subdural space.
Expansion of the hemorrhage to the spinal subdural space is extremely rare, and its physiopathogenesis has not been completely elucidated because only a few cases have been described in the literature. One of the mechanisms involved is a sudden increase in intraspinal vessel pressure due to an increase in intraabdominal or intrathoracic pressure, which causes rupture of the venous structures that cross the spinal subarachnoid space, resulting in leakage into the subdural space.6 A series describing four cases of SSDH associated with brain aneurysm surgery has been reported. It argues that this relationship can be due to overdrainage of cerebrospinal fluid during the procedure and caudal migration for severity of the blood collections.7
Observations
Authors have described approximately 10 cases of concomitant SAH and SSDH8 that can occur with no vascular malformation9–11 in the context of brain aneurysm rupture and other vascular diseases.8,12–14 In the case of supratentorial aneurysms, the theory proposed by Yamaguchi et al.13 consists of an infratentorial projection of the hemorrhage, with dissection of the subdural space under the tentorium and migration due to gravity to the spinal canal. The SAHs caused by dissecting lesions of the vertebral arteries14–16 could promote direct invasion of the hemorrhage to the dura mater located in the craniocervical transition.
Similar to other cases described in the literature,17 from the onset of the clinical onset our patient had symptoms consistent with spinal involvement. In fact, MRI showed the trajectory of the blood collection from the cervical area to the dorsal area, which supports the possibility that the hematoma migrated by expanding from the intracranial compartment instead of being the result of a local effect caused by an increase in intraabdominal or intrathoracic pressure. The presence of a mega cisterna magna could also enhance the passage of a higher amount of blood.
Lessons
Intradural aneurysms can occasionally cause hemorrhages to open to the subdural space, generally due to rupture of the arachnoid membrane and direct invasion. There is anatomical continuity between the brain and spinal subdural spaces,9 so SAH can occur together with an SSDH. We report on an exceptional case in which the most probable mechanism is hemorrhage due to the vertebral aneurysm that reached the subdural space and subsequent rostrocaudal migration, enhanced by the intracranial pressure increase. The presence of symptoms or signs of spinal involvement, together with intracranial SAH, must raise this diagnostic suspicion.
Acknowledgments
We thank the patient and her family, who consented to the publication of this work. We thank Drs. Hernán Sandoval Valencia and Juan Campos for the clinical and neurosurgical management of the patient.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Hernández-Fernández. Acquisition of data: all authors. Analysis and interpretation of data: Hernández-Fernández, Cámara-González. Drafting the article: Hernández-Fernández, Cámara-González, Alcahut-Rodríguez. Critically revising the article: Hernández-Fernández, Pedrosa-Jiménez. Reviewed submitted version of manuscript: Hernández-Fernández. Approved the final version of the manuscript on behalf of all authors: Hernández-Fernández. Administrative/technical/material support: Hernández-Fernández. Study supervision: Hernández-Fernández.
Supplemental Information
Previous Presentations
Portions of this work were presented at the LXIX Reunión Anual Sociedad Española de Neurología, Valencia, Spain, November 21–25, 2017.
References
- 1. Jung HS, Jeon I, Kim SW. Spontaneous spinal subdural hematoma with simultaneous cranial subarachnoid hemorrhage. J Korean Neurosurg Soc. 2015;57(5):371–375. doi: 10.3340/jkns.2015.57.5.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Russell NA, Benoit BG. Spinal subdural hematoma. A review. Surg Neurol. 1983;20(2):133–137. doi: 10.1016/0090-3019(83)90464-0. [DOI] [PubMed] [Google Scholar]
- 3. Gillilan LA. Veins of the spinal cord. Anatomic details; suggested clinical applications. Neurology. 1970;20(9):860–868. doi: 10.1212/wnl.20.9.860. [DOI] [PubMed] [Google Scholar]
- 4. Boop WC, Jr, Chou SN, French LA. Ruptured intracranial aneurysm complicated by subdural hematoma. J Neurosurg. 1961;18:834–836. doi: 10.3171/jns.1961.18.6.0834. [DOI] [PubMed] [Google Scholar]
- 5. Koerbel A, Ernemann U, Freudenstein D. Acute subdural haematoma without subarachnoid haemorrhage caused by rupture of an internal carotid artery bifurcation aneurysm: case report and review of literature. Br J Radiol. 2005;78(931):646–650. doi: 10.1259/bjr/60601877. [DOI] [PubMed] [Google Scholar]
- 6. Rader JP. Chronic subdural hematoma of the spinal cord: report of a case. N Engl J Med. 1955;253(9):374–376. doi: 10.1056/NEJM195509012530906. [DOI] [PubMed] [Google Scholar]
- 7. Kim MS, Lee CH, Lee SJ, Rhee JJ. Spinal subdural hematoma following intracranial aneurysm surgery: four case reports. Neurol Med Chir (Tokyo) 2007;47(1):22–25. doi: 10.2176/nmc.47.22. [DOI] [PubMed] [Google Scholar]
- 8. Rothrock RJ, Li AY, Rumsey J, et al. Aneurysmal subarachnoid hemorrhage with spinal subdural hematoma: a case report and systematic review of the literature. World Neurosurg. 2019;128:240–247. doi: 10.1016/j.wneu.2019.05.069. [DOI] [PubMed] [Google Scholar]
- 9. Wang US, Ju CI, Kim SW, Kim SH. Spontaneous concomitant intracranial and spinal subdural hematomas in association with anticoagulation therapy. J Korean Neurosurg Soc. 2012;51(4):237–239. doi: 10.3340/jkns.2012.51.4.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kim HY, Ju CI, Kim SW. Acute cervical spinal subdural hematoma not related to head injury. J Korean Neurosurg Soc. 2010;47(6):467–469. doi: 10.3340/jkns.2010.47.6.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lee Y, Lim J, Han S, et al. Spontaneous spinal subdural and subarachnoid hemorrhage with concomitant intracerebral hemorrhage: a case report. Korean J Neurotrauma. 2019;15(1):34–37. doi: 10.13004/kjnt.2019.15.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gilad R, Fatterpekar GM, Johnson DM, Patel AB. Migrating subdural hematoma without subarachnoid hemorrhage in the case of a patient with a ruptured aneurysm in the intrasellar anterior communicating artery. AJNR Am J Neuroradiol. 2007;28(10):2014–2016. doi: 10.3174/ajnr.A0726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yamaguchi S, Hida K, Akino M, et al. Spinal subdural hematoma: a sequela of a ruptured intracranial aneurysm? Surg Neurol. 2003;59(5):408–412. doi: 10.1016/s0090-3019(03)00016-8. [DOI] [PubMed] [Google Scholar]
- 14. Ovalı GY, Adam G, Çınar C, et al. Symptomatic spinal migration of subarachnoid hemorrhage due to ruptured intradural vertebral artery aneurysm. J Neuroimaging. 2015;25(4):668–670. doi: 10.1111/jon.12189. [DOI] [PubMed] [Google Scholar]
- 15. Steele L, Raza MH, Perry R, et al. Subarachnoid haemorrhage due to intracranial vertebral artery dissection presenting with atypical cauda equina syndrome features: case report. BMC Neurol. 2019;19(1):262. doi: 10.1186/s12883-019-1487-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Neto L, Moura Guedes M, Campos J. Spinal subarachnoid hemorrhage mimicking an acute abdomen. Neuroradiol J. 2012;25(2):217–221. doi: 10.1177/197140091202500211. [DOI] [PubMed] [Google Scholar]
- 17. Swann KW, Ropper AH, New PF, Poletti CE. Spontaneous spinal subarachnoid hemorrhage and subdural hematoma. Report of two cases. J Neurosurg. 1984;61(5):975–980. doi: 10.3171/jns.1984.61.5.0975. [DOI] [PubMed] [Google Scholar]


