Abstract
Objective: In wheelchair rugby (WR) athletes with tetraplegia, wheelchair performance may be impaired due to (partial) loss of innervation of upper extremity and trunk muscles, and low blood pressure (BP). The objective was to assess the effects of electrical stimulation (ES)-induced co-contraction of trunk muscles on trunk stability, arm force/power, BP, and WR performance.
Design: Cross-sectional study.
Setting: Rehabilitation research laboratory and WR court.
Participants: Eleven WR athletes with tetraplegia.
Interventions: ES was applied to the rectus abdominis, obliquus externus abdominis and erector spinae muscles. For every test, the ES condition was compared to the non-ES condition.
Outcome measures: Stability was assessed with reaching tasks, arm force/power with an isokinetic test on a dynamometer, BP during an ES protocol and WR skill performance with the USA Wheelchair Rugby Skill Assessment.
Results: Overall reaching distance (ES 14.6 ± 7.5 cm, non-ES 13.4 ± 8.2 cm), and BP showed a significant increase with ES. Arm force (ES 154 ± 106 N, non-ES 148 ± 102 N) and power (ES 37 ± 26 W, non-ES 36 ± 25 W), and WR skills were not significantly improved.
Conclusion: ES-induced trunk muscle activation positively affects trunk stability and BP, but not arm force/power. No effects were found in WR skill performance, probably due to abdominal strapping. More research is needed to assess different ES (training) protocols and longitudinal effects.
Keywords: Trunk control, Exercise, Tetraplegia, Electrical stimulation, Rehabilitation
Introduction
Wheelchair rugby (WR) is a dynamic sport, originally designed for athletes with high spinal cord injury (SCI). In recent years it has quickly evolved as athletes with other disabilities are allowed to play the game.1 Important aspects are quick wheelchair turning, braking, acceleration from standstill, and ball handling.2,3 These aspects largely depend on trunk stability and upper extremity power,3–5 which are impaired in most athletes with high SCI, due to the (partial) loss of innervation of upper extremity and trunk muscles.
To compensate for this loss of stability, WR athletes with high SCI in general have a different postural strategy, with a more backward tilted pelvis during sitting,6–10 using different muscles to restore balance 6,7,9–11 and using adjusted wheelchairs with a deep seating position and abdominal strapping.11–14 However, trunk range of motion is greatly decreased by these adjustments.12,13
Next to limited stability and strength, loss of sympathetic innervation under the lesion level is another important factor that impairs performance in WR athletes with high SCI. There is less vasoconstriction in the nonworking muscles of the legs and trunk, resulting in venous pooling and a lower venous return to the heart.15–17 Therefore, blood pressure (BP) is generally low and less capable of rising in response to exercise. Moreover, there is a direct effect on heart rate in high SCI lesions.16–19 Due to loss of sympathetic innervation, heart rate is only moderately capable of rising in response to exercise by decreasing parasympathetic input. As loss of sympathetic innervation is not part of the classification criteria, athletes with a high SCI have a disadvantage compared to athletes with other disabilities with the same motor impairment19–22; they will have a lower maximum heart rate, lower aerobic power and peak power output.19,23
To improve arm and trunk performance in patients with high SCI, application of electrical stimulation (ES) has been studied.17,24–26 Surface ES on the erector spinae and rectus abdominis muscles increases trunk stiffness significantly in healthy participants during sitting.26 Moreover, implanted ES with effect on the trunk muscles in high SCI showed to have a significantly positive effect on stability and reaching,27,28 and on wheelchair propulsion mechanics.29
These limiting factors in WR performance together with the promising effects of ES have led to the objective of this study, which was to assess the effects of ES-induced co-contraction of trunk muscles on WR performance in athletes with tetraplegia. The first hypothesis was that co-contraction of the trunk muscles would lead to more stability,26,28 and therefore increased reaching distance. The second hypothesis was that co-contraction of the trunk muscles would lead to a firmer trunk position, and therefore would lead to a higher peak force and peak power during an arm push. The third hypothesis was that BP would rise in response to ES, as co-contraction of the trunk muscles might also lead to an increase in intra-abdominal pressure, leading to more venous return. The fourth hypothesis was that WR skill performance would improve due to the combination of increased trunk stability, arm force and power and increased BP.
Methods
Participants
Eleven WR athletes with a tetraplegia participated (Table 1). Exclusion criteria comprised: active rehabilitation treatment at the time of study, autonomic dysreflexia in response to previous ES, other diseases and conditions that could interfere with the study such as pressure sores, fever or cardiac and pulmonary disease, and usage of medication interfering with one of the outcome parameters such as beta blockers. Participants were recruited from elite WR teams in the Netherlands. This study was approved by the ethics committee of the Faculty of Behavioural and Movement Sciences at the Vrije Universiteit Amsterdam. All participants voluntarily signed informed consent.
Table 1. Participants characteristics.
| Participant | Age (yr) | Sex | Lesion Level | Motor Complete | Time Since Injury (yr) | Wheelchair Rugby Experience (yr) | Classification | FES Amplitude Back (mA) | FES Amplitude Abdomen (mA) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 47 | M | C6 | Complete | 28 | 22 | 0,5 | 65 | 65 |
| 2 | 30 | M | C4-5 | Complete | 8 | 5 | 0,5 | 70 | 70 |
| 3 | 29 | M | C6 | Incomplete | 13 | 12 | 1 | 100 | 70 |
| 4 | 27 | M | C6 | Incomplete | 4 | 1,5 | 1,5 | 75 | 65 |
| 5 | 33 | M | C5-6 | Incomplete | 5 | 4 | 1,5 | 50 | 55 |
| 6 | 46 | M | C6 | Complete | 17 | 15 | 1,5 | 60 | 60 |
| 7 | 60 | M | C4-5 | Incomplete | 47 | 20 | 2 | 60 | 30 |
| 8 | 51 | M | C7 | Incomplete | 34 | 22 | 2,5 | 55 | 75 |
| 9 | 45 | F | C4 | Incomplete | 14 | 2 | 2,5 | 90 | 90 |
| 10 | 46 | M | C7 | Incomplete | 13 | 12 | 3 | 90 | 90 |
| 11 | 44 | M | C4 | Incomplete | 10 | 3 | 3 | 50 | 30 |
Study design
Trunk stability, arm force, arm power and BP were measured on the same day. On a second day, WR skills were measured. Each test was performed with and without ES. Not all participants could perform all tests due to the large number of tests and logistical constraints. The order of testing (i.e. ES or non-ES) was randomized. Participants were asked to void their bladder to minimize the chance of autonomic dysreflexia,16 not to use performance-influencing means 24 h before testing.
Electrical stimulation
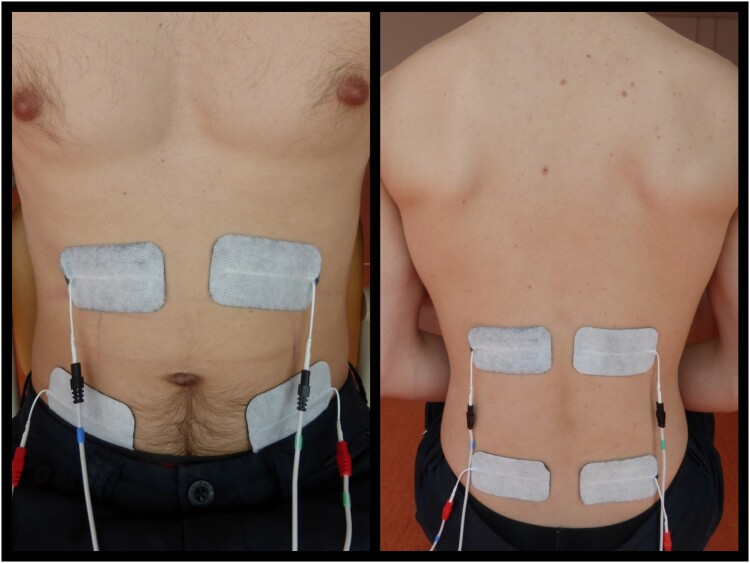
ES was applied using a portable electrical stimulator with four channels (Compex 3 Professional, CefarCompex, DJO Benelux) and eight self-adhesive electrodes (Enraf Nonius, EN-Trode, 50 × 90 mm rect, Axelgaard Mfg. Co., Ltd.). The rectus abdominis, obliquus externus abdominis and erector spinae muscle were stimulated simultaneously to create co-contraction. Electrodes of an electrode pair were placed proximal and distal over the muscle and in line with the muscle fiber direction (Fig. 1). A continuous protocol with biphasic pulses was used. Frequency and pulse duration were fixed at 30 Hz and 300 μs, respectively, and current amplitude was determined individually. Amplitude (mA) level was increased until at least a tetanic muscle contraction was visible and palpable, and was further increased to the highest level tolerable for the participant (i.e. without strong discomfort or signs of autonomic dysreflexia). Amplitude values varied between 30 and 100 mA (Table 1).
Figure 1.
Electrode placement on the rectus abdominis muscle, obliquus externus abdominis muscle (left) and erector spinae muscle (right).
Trunk stability
Trunk stability was measured in nine participants and assessed with a reaching task (Fig. 2). The participant sat in his/her own daily wheelchair without any strappings. The purpose was to push away a tube as far as possible. Participants had to reach forward, laterally (90 degrees) and diagonally (45 degrees). In forward reaching, both arms were extended in 90 degrees shoulder anteflexion. In lateral and diagonal direction the tested arm (both dominant and non-dominant arm were tested) was abducted in a horizontal position and the opposite arm was placed on the chest or contralateral shoulder. The distance at which the participant was able to return to the original position (and not fall to the side or front) was counted valid and measured in millimeters. All directions were tested twice and scores were averaged for analysis. For each reaching direction, ES was compared with non-ES. In addition, scores of all directions together (total reaching) were averaged and compared between ES and non-ES conditions.
Figure 2.
Reaching diagonal with dominant arm.
Arm force and arm power
Arm force and arm power were measured in five participants with a Biodex dynamometer (Biodex System 3 ProTM Biodex Medical Systems, New York, NY). An isokinetic protocol (i.e. movement at a constant speed) with closed-chain attachment was used. The participant sat on the Biodex chair, with the handgrip in resting position just lateral to the iliac crest and elbow in ninety degrees flexion. The purpose was to push the handgrip away (0.24 m/s) and then pull back (0.61 m/s) until starting position, both as forcefully as possible. Participants had six attempts per arm both with and without ES. Before the first set a practice round was conducted.
Raw data were analyzed in Matlab (Mathworks Inc., Natick, MA R2015a). The main power of the signal was observed at frequencies below 15 Hz. The data were filtered with a low-pass Butterworth filter (2nd order, 20-Hz cut-off frequency) to remove noise. Power output (W) was calculated by multiplying the filtered force signal (N) with the corresponding speed (m/s). Peak force and peak power were determined as the highest score in each attempt. Peak scores of all six attempts of both the dominant and non-dominant arm were used to compare between ES and non-ES conditions.
Blood pressure
Systolic (SBP) and diastolic blood pressure (DBP) were measured in ten participants with an automatic electronic sphygmomanometer (Omron, M6 (Hem-7001-E(v))) around the left upper arm. The participants were in rest, sitting in their daily wheelchair. BP was first measured without ES, then after one and two minutes with ES, directly after stopping ES and after one minute without ES. The participant was instructed not to talk or move during the measurements.
Wheelchair rugby skills
WR skills were measured with the USA Wheelchair Rugby Skill Assessment2,30 in seven participants. This assessment includes five field performance tests, and was performed in the participant’s personal rugby wheelchair including abdominal strapping. All tests were conducted with and without ES.
Ball handling was tested with the Passing Skill Test. The aim was to throw a ball to the center of a target on the wall. Three, two or one point was awarded when hitting the center, middle or outer square, respectively. Participants had three attempts from six different positions. Target distance depended on the classification of the athlete and was 3 and 4.5 meters for low-point players (classification 0.5–1.5), and 4.5 and 6 meters for high-point players (classification 2.0–3.5).
The other four WR skills assessed speed and wheelchair handling, measured in time. Participants had to conduct a sprint over twenty meters (two attempts), an endurance sprint (one attempt) around an indoor court (13.4 × 28 meter), ups & backs (one attempt) and a slalom (two attempts). For the ups & backs, seven lines were placed with 90 cm in between in which participants had to propel to the first line and then return backwards to the starting position, then to the second line and so forth. The slalom was performed between eight cones with 120 cm distance in between. In the ES condition, ES was turned off between all subtests.
At the start and end of the test, timing gates with accelerometers (Delsys Trigno Wireless EMG system, Natick, MA) were used to measure time. By riding through the timing gates, a peak in the z-direction of the accelerometer signal was registered. These signals were analyzed with Matlab. The first twenty samples of the data were removed because of noise, and every signal was corrected for offset. Thereafter, start and end time were set automatically when acceleration in the z-direction was >0.2 m/s2. In the time-based subtests, every attempt was used for analysis. For the Passing Skill Test, all three scores for each position were summed. All scores were compared between the ES and non-ES condition.
Statistical analysis
Statistical analysis was performed with SPSS (IBM SPSS Statistics 22, SPSS, Inc., Chicago, IL). The data were tested for normality using Kolmogorov–Smirnov tests with Lilliefors Significance Correction and Shapiro–Wilk tests. Additionally, z-scores for skewness and kurtosis were calculated. For the scores of the reaching distance the assumptions for normality of the differences were not met. Therefore, the nonparametric Wilcoxon signed rank test was used for analysis. Two repeated-measures ANOVA with Bonferroni correction for pairwise comparisons were used to test the effect of ES on arm force and arm power. ES condition (2), arm (2), and attempts (6) were used as within-subject factors. To test the effect of ES on BP, a repeated-measures ANOVA was used. Mauchly’s test showed that the assumption of sphericity had been met, indicating a normal distribution of the variances of differences. A Bonferroni correction was used for pairwise comparisons. For the WR skills the difference between ES and non-ES within the Passing Skill Test was tested with a paired t-test. For the time-based subtests of the WR skills, a repeated measures ANOVA with Bonferroni correction for pairwise comparisons was used. ES condition (2) and subtests (6) were used as within-subject factors. In all statistic procedures, the significance level was set at P < .05. In significant test results, Pearson’s r effect sizes were calculated: r = 0.1 was considered a small effect; r = 0.3 a medium effect; and r = 0.5 or above as a large effect.31
Results
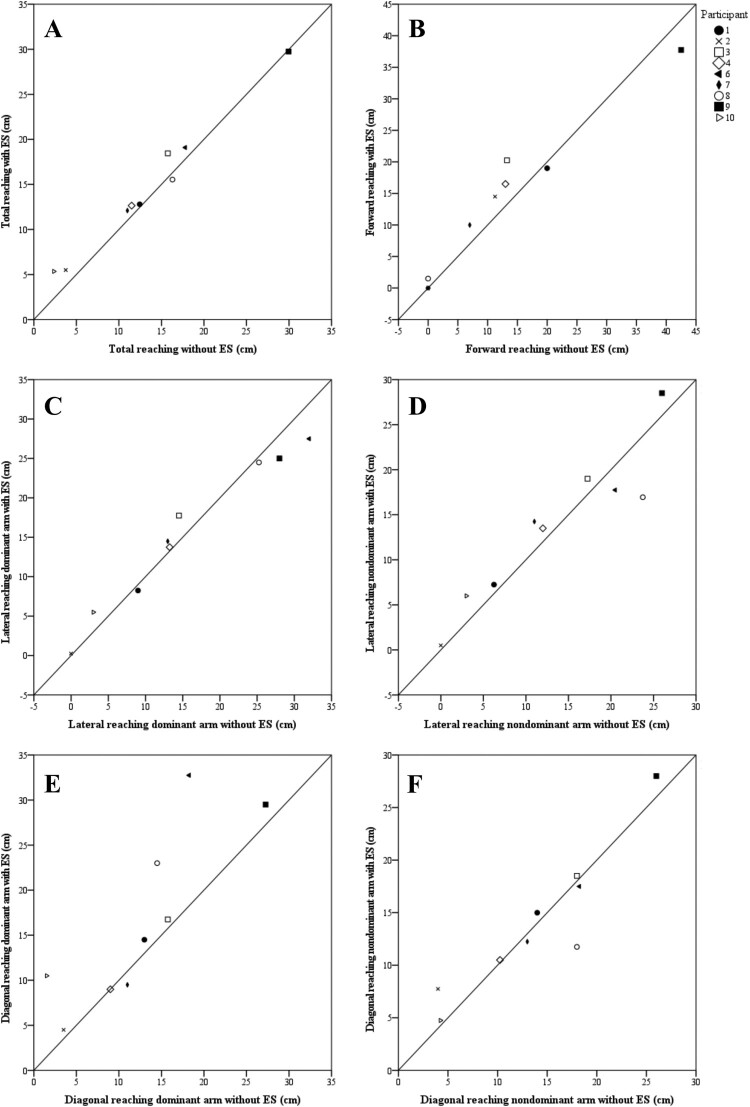
The results for trunk stability are shown in Table 2 and Fig. 3. Total reaching with ES was significantly higher (9%, large effect size) compared with the non-ES condition. Of the individual reaching directions, the diagonal direction with dominant arm was the only task that scored significantly higher with ES (33%, medium effect size) compared with the non-ES condition.
Table 2. Reaching task (N = 9).
| Non-ES | ES | |||||||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Median | Mean ± SD | Median | Δ ± SD | z-score | P value | Effect size r | |
| Total (cm) | 13.4 ± 8.2 | 12.5 | 14.6 ± 7.5 | 12.8 | 1.2 ± 1.2 | 2.19 | 0.03* | 0.52 |
| Forward (cm) | 11.9 ± 13.5 | 11.3 | 13.3 ± 12.2 | 14.5 | 1.4 ± 3.3 | 1.18 | 0.24 | ns |
| Lateral – Dominant arm (cm) | 15.3 ± 11.0 | 13.3 | 15.2 ± 9.4 | 14.5 | −0.1 ± 2.5 | −0.06 | 0.95 | ns |
| Lateral – Non-dominant arm (cm) | 13.3 ± 9.2 | 12.0 | 13.7 ± 8.3 | 14.3 | 0.4 ± 3.2 | 0.89 | 0.37 | ns |
| Diagonal – Dominant arm (cm) | 12.6 ± 7.8 | 13.0 | 16.7 ± 9.8 | 14.5 | 4.0 ± 5.4 | 2.04 | 0.04* | 0.48 |
| Diagonal – Non-dominant arm (cm) | 14.0 ± 7.1 | 14.0 | 14.0 ± 6.8 | 12.3 | 0.0 ± 2.7 | 0.53 | 0.59 | ns |
Figure 3.
Scatterplot with line of identity. All values above the line of identity indicate a higher value in the ES condition compared to the non-ES condition. Each symbol represents a participant. A. Total reaching direction. B. Forward reaching direction. C. Lateral reaching direction with dominant arm. D. Lateral reaching direction with nondominant arm. E. Diagonal reaching direction with dominant arm. F. Diagonal reaching direction with nondominant arm.
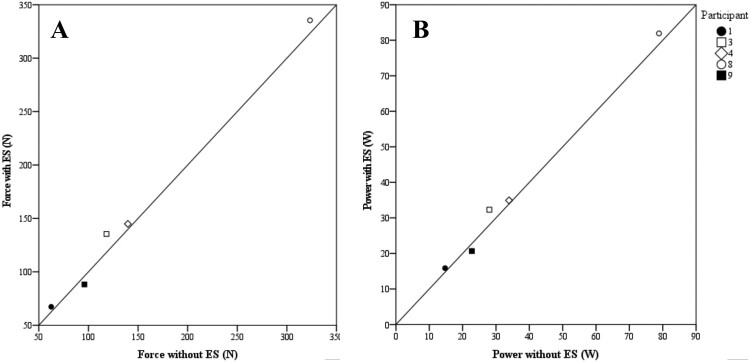
Arm force was 4.1% higher in the ES condition compared with the non-ES condition. This effect was, however, not significant (Mean ± SD: 154 ± 106 N, vs. 148 ± 102 N, P = 0.21). Arm power was 2.8% higher in the ES condition compared with the non-ES condition, but not significantly different (37 ± 26 W vs. 36 ± 25 W, P = 0.24). Figure 4(A,B) show the average values per participant in both ES conditions.
Figure 4.
Scatterplot with line of identity. All values above the line of identity indicate a higher value in the ES condition compared to the non-ES condition. Each symbol represents a participant. A. Arm force. B. Arm power.
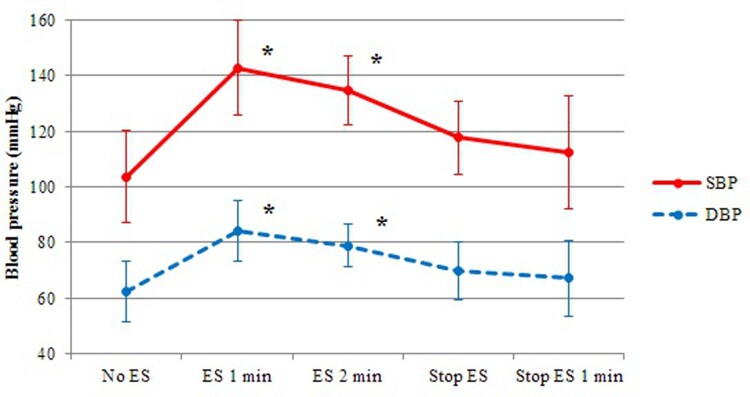
SBP and DBP (Fig. 5) were significantly different in the five test conditions, F(4, 36) = 23.57, P < .001 and F(4, 36) = 18.77, P < .001 respectively. After one minute with ES, SBP and DBP were significantly higher (SBP: P = .001, DBP: P = .005) compared with the SBP and DBP at the beginning of the test without ES (SBP: Δ 39.2 ± 18.04 mmHg, DBP: Δ 21.80 ± 12.95 mmHg). After two minutes with ES, both SBP and DBP were still significantly higher (SBP: P = .001, DBP: P = .002) compared with the beginning of the test without ES (SBP: Δ 31.30 ± 15.13 mmHg, DBP: Δ 16.50 ± 8.75 mmHg). Directly after stopping ES, both SBP and DBP decreased and were not significantly different (SBP: P = .08, DBP: P = .15) from the values at the beginning of the test without ES (SBP: Δ 14.00 ± 12.93 mmHg, DBP: Δ 7.60 ± 7.96 mmHg).
Figure 5.
Blood pressure over different ES conditions in time. *indicates significant difference compared to non-ES at the beginning of the protocol.
For the Passing Skill Test, there was no significant difference between the ES condition and non-ES condition (M = 14 ± SD 10 points vs. 13 ± 10 points, P = 0.45). For the time-based subtest, there was no significant difference between the ES condition and the non-ES condition (M = 23.3 ± SE 1.1 s, M = 23.7 ± SE 1.2 s, P = 0.16): sprint M = 7.9 ± SD 1.1 s vs. 7.8 ± 1.1 s; endurance sprint M = 33.3 ± SD 5.4 s vs. 33.4 ± 5.1 s; ups & backs M = 45.1 ± SD 4.4 s vs. 46.6 ± 6.3 s; slalom M = 22.9 ± SD 3.1 s vs. 23.3 ± 3.4 s.
Discussion
With ES it was possible to create co-contraction of the trunk muscles in WR athletes with high SCI, inducing more trunk stability, depicted by a higher measured reaching distance. The increased stability probably caused a more stable base to deliver arm force on, but this did not result in a significantly higher arm force and arm power. In addition, stimulation of the trunk muscles significantly increased SBP and DBP. However, WR skills were not significantly improved with the use of ES.
The created co-contraction with ES led to increased trunk stability, reflected by the increased reaching distance. Although the increase in reaching distance with ES was in an absolute sense small (total distance Δ 1.2 cm, diagonal dominant arm Δ 4.0 cm), in a relative sense it was quite large (9–33%), an increase that can make an important difference in ball possession during a WR match. For the different reaching directions, only the diagonal dominant-arm direction significantly improved with ES. This is in concordance with previous studies that found the oblique reaching directions to be the most sensitive to investigate dynamic stability.7,32 Moreover, athletes might be more used to perform controlled reaching movements with their dominant arm.15,32,33 Although there was not a significant effect in the forward direction, a functional useful effect was observed in several participants; some participants were not able to lift both arms to 90 degrees without falling forward. However, with ES they were all able to make this movement and sit stable. This effect was observed several times. Nevertheless, in both conditions reaching distance was zero and therefore no difference was measured.
Arm force and power both increased with ES (4.1% and 2.5%, respectively). This effect was, however, not significant. A reduced statistical power might be an explanation. Figure 4(A,B) show that one of five participants had a decrease in arm force and power with ES. This participant had a motor incomplete SCI.
Another important effect of co-contraction of the trunk muscles is the influence on BP. The impaired vasoconstriction under the lesion level results in venous pooling and therefore less venous return and a lower BP.16–18,21,23,34 Co-contraction of the trunk muscles can lead to an increased intra-abdominal pressure, resulting in an increase in mean vascular pressure, which facilitates venous return and therefore increases BP.35,36 Another mechanism causing an increase in BP is autonomic dysreflexia.17,35 As the BP increase in this study was quite high after one minute, this mechanism could play an additional role. However, as no other signs of autonomic dysreflexia were apparent (e.g. headache, nausea), BP showed already a slight decrease during ES, and the fast return to normal levels after ES cessation, this mechanism is a less likely explanation for the rise in BP in our study. The slight decrease in BP during ES could be explained by rapid fatigue of the trunk muscles. Because of this fatigue, there will be a less forceful co-contraction and intra-abdominal pressure will slightly decrease over time. Future longitudinal studies need to be performed to investigate whether different ES settings and several successive sessions with ES may lead to a more sustained BP increase.
A combined effect of above-mentioned results was hypothesized to improve WR skills. WR skills were, however, not significantly improved. This might be explained by the fact that abdominal strapping was used during these tests and that the tests were executed in their own adjusted wheelchairs with a deep seating position. In our view it was important to keep the tests as sport specific as possible, so the athletes were instructed to perform the tests in their normal rugby gear including abdominal strapping. However, these adjustments can positively affect stability and wheelchair acceleration and deceleration,11,14 and could, therefore, overshadow the effect of ES. Nevertheless, athletes mentioned to experience more stability in their trunk with the addition of ES in this study. They felt ES was beneficial, however sometimes also contra-intuitive because they were not used to this feeling and it required different propulsion coordination. In future studies it would be interesting to perform a longitudinal study where individuals are able to practice and train with ES.
Practical applications and future studies
Rules around ES application during WR games are undefined and therefore the question if ES is allowed during games is unanswered.32 ES did not directly improve WR skills in this study and is therefore, in this stage, not of added value during the game. Nevertheless, benefits of increased reaching distance and BP are also applicable in daily life in patients with SCI. For example, increased reaching distance could enhance reaching for tools and could ease self-care. Moreover, increasing BP could minimize the negative effects of hypotension and elevate concentration levels or alertness.37 These cross-sectional results show a new application of ES and could be a building block for further research. A longitudinal approach with successive sessions with ES on trunk muscles will give insight into the relative shift from low fatigue resistance muscle fibers to high fatigue resistance fibers in individuals with SCI.38 This effect might potentially lead to longer periods of trunk stabilization and BP increase than measured in the present study. Secondly, a 30-Hz frequency, moderate pulse duration (300 μs) and high individually set amplitude were used in this study. These settings were in line with other studies 22,25,26 and chosen to make sure that the values were high enough to create a tetanic contraction 39 but not too high so the effect of fatigue could be minimized.40 With these settings it was possible to create co-contraction in all our participants. However, little is known about the optimal settings for these variables. Future studies should focus on different ES settings and protocols to induce co-contraction and high trunk stability with relatively low muscle fatigue. Lastly, the effect of abdominal ES on respiratory function was not investigated in the present study. Previous studies have shown that abdominal ES might have an acute effect on cough peak flow and maximum expiratory pressure.41–43 One could imagine that the effect of continuous abdominal ES on respiratory function might also influence wheelchair performance. Future studies should pay attention to this aspect.
Limitations
The first limitation of this study was that the tests were performed in a small group of participants. Therefore, the statistical power was reduced. Another limitation of this small group was that it was not possible to distinguish different subgroups to explain variability in the results, for example, possible differences between individuals with complete SCI compared with incomplete SCI. A second limitation was the immeasurable effect we found in the forward reaching task. Some other studies investigated stability with measurement of the center of pressure or by recording movement with sensors or camera’s, which do not have this limitation.11,44,45
Conclusion
This study shows that ES on trunk muscles has a clear positive effect on different performance measures in athletes with high SCI. Trunk stability and BP increased. No significant effects could be found in arm force and power, and WR skills. More longitudinal research is needed to assess different ES (training) protocols and settings. This study shows that ES is a promising intervention in sport, rehabilitation and daily life.
Acknowledgements
The authors would like to thank Viola Altmann, Sint Maartenskliniek, Nijmegen, the Netherlands; Karin Gerrits, Department of Human Movement Sciences, Faculty of Behavioural and Human Movement Sciences, Vrije Universiteit Amsterdam, Amsterdam Movement Sciences, the Netherlands; and Linda van Vliet and Suzanne Romviel, Amsterdam Rehabilitation Research Center | Reade Amsterdam, the Netherlands for their support with the research protocol.
Disclaimer statements
Contributors None.
Funding None.
Conflicts of interest Authors have no conflict of interests to declare.
References
- 1.International Wheelchair Rugby Classification Manual 3rd edition, revised 2015. [cited 2016 November 25]. Available from https://www.iwrf.com/?page=classification.
- 2.Orr K, Malone LA.. Wheelchair rugby. In: Goosey-tolfrey VL, (ed.) Wheelchair sport. Champaign, IL: Human Kinetics; 2010. p. 151–66. [Google Scholar]
- 3.Vanlandewijck Y, Theisen D, Daly D.. Wheelchair propulsion biomechanics. Implications for wheelchair sports. Sport Med 2001;31(5):339–67. doi: 10.2165/00007256-200131050-00005 [DOI] [PubMed] [Google Scholar]
- 4.Chow JW, Millikan TA, Carlton LG, Chae W, Lim Y, Morse MI.. Kinematic and electromyographic analysis of wheelchair propulsion on ramps of different slopes for young men with paraplegia. Arch Phys Med Rehabil 2009;90(2):271–8. doi: 10.1016/j.apmr.2008.07.019 [DOI] [PubMed] [Google Scholar]
- 5.Altmann VC, Groen BE, Hart AL, Vanlandewijck YC, van Limbeek J, Keijsers NLW.. The impact of trunk impairment on performance-determining activities in wheelchair rugby. Scand J Med Sci Sport 2017;27(9):1005–14. doi: 10.1111/sms.12720 [DOI] [PubMed] [Google Scholar]
- 6.Van Breukelen K. Rolstoel performance. Moordrecht: Double Performance; 2014. p. 75–79. [Google Scholar]
- 7.Gauthier C, Gagnon D, Grangeon M, Jacquemin G, Nadeau S, Masani K, et al. Comparison of multidirectional seated postural stability between individuals with spinal cord injury and able-bodied individuals. J Rehabil Med 2013;45(1):47–54. doi: 10.2340/16501977-1066 [DOI] [PubMed] [Google Scholar]
- 8.Hobson DA, Tooms RE.. Seated lumbar/pelvic alignment. A comparison between spinal cord-injured and noninjured groups. Spine 1992;17(3):293–8. doi: 10.1097/00007632-199203000-00009 [DOI] [PubMed] [Google Scholar]
- 9.Potten YJM, Seelen HAM, Drukker J, Reulen JPH, Drost MR.. Postural muscle responses in the spinal cord injured persons during forward reaching. Ergonomics 1999;42(9):1200–15. doi: 10.1080/001401399185081 [DOI] [PubMed] [Google Scholar]
- 10.Seelen HAM, Potten YJM, Huson A, Spaans F, Reulen JPH.. Impaired balance control in paraplegic subjects. J Electromyogr Kinesiol 1997;7(2):149–60. doi: 10.1016/S1050-6411(97)88884-0 [DOI] [PubMed] [Google Scholar]
- 11.Curtis KA, Kindlin CM, Reich KM, White DE.. Functional reach in wheelchair users: the effects of trunk and lower extremity stabilization. Arch Phys Med Rehabil 1995;76(4):360–7. doi: 10.1016/S0003-9993(95)80662-8 [DOI] [PubMed] [Google Scholar]
- 12.Kerk JK, Clifford PS, Snyder AC, Prieto TE, O'Hagan KP, Schot PK, et al. Effect of an abdominal binder during wheelchair exercise. Med Sci Sport Exerc 1995;27(6):913–9. doi: 10.1249/00005768-199506000-00018 [DOI] [PubMed] [Google Scholar]
- 13.Vanlandewijck YC, Verellen J, Tweedy SM.. Towards evidence-based classification in wheelchair sports: impact of seating position on wheelchair acceleration. J Sports Sci 2011;29(10):1089–96. doi: 10.1080/02640414.2011.576694 [DOI] [PubMed] [Google Scholar]
- 14.West CR, Campbell IG, Goosey-tolfrey VL, Mason BS, Romer LM.. Effects of abdominal binding on field-based exercise responses in Paralympic athletes with cervical spinal cord injury. J Sci Med Sport 2014;17(4):351–5. doi: 10.1016/j.jsams.2013.06.001 [DOI] [PubMed] [Google Scholar]
- 15.Goosey-Tolfrey VL, Leicht CA.. Field-based physiological testing of wheelchair athletes. Sport Med 2013;43(2):77–91. doi: 10.1007/s40279-012-0009-6 [DOI] [PubMed] [Google Scholar]
- 16.Krassioukov A. Autonomic function following cervical spinal cord injury. Respir Physiol Neurobiol 2009;169(2):157–64. doi: 10.1016/j.resp.2009.08.003 [DOI] [PubMed] [Google Scholar]
- 17.Phillips WT, Kiratli BJ, Sarkarati M, Weraarchakul G, Myers J, Franklin BA, et al. Effect of spinal cord injury on the heart and cardiovascular fitness. Curr Probl Cardiol 1998;23(11):641–716. doi: 10.1016/S0146-2806(98)80003-0 [DOI] [PubMed] [Google Scholar]
- 18.Bhambhani Y. Physiology of wheelchair racing in athletes with spinal cord injury. Sport Med 2002;32(1):23–51. doi: 10.2165/00007256-200232010-00002 [DOI] [PubMed] [Google Scholar]
- 19.Mills PB, Krassioukov A.. Autonomic function as a missing piece of the classification of Paralympic athletes with spinal cord injury. Spinal Cord 2011;49(7):768–76. doi: 10.1038/sc.2011.2 [DOI] [PubMed] [Google Scholar]
- 20.West CR, Krassioukov A.. Autonomic cardiovascular control and sports classification in Paralympic athletes with spinal cord injury. Disabil Rehabil 2017;39(2):127–34. doi: 10.3109/09638288.2015.1118161 [DOI] [PubMed] [Google Scholar]
- 21.West CR, Romer LM, Krassioukov A.. Autonomic function and exercise performance in elite athletes with cervical spinal cord injury. Med Sci Sport Exerc 2013;45(2):261–7. doi: 10.1249/MSS.0b013e31826f5099 [DOI] [PubMed] [Google Scholar]
- 22.Yang Y, Koontz AM, Triolo RJ, Cooper RA, Boninger ML.. Biomechanical analysis of functional electrical stimulation on trunk musculature during wheelchair propulsion. Neurorehabil Neural Repair 2009;23(7):717–25. doi: 10.1177/1545968308331145 [DOI] [PubMed] [Google Scholar]
- 23.Haas F, Axen K, Pineda H.. Aerobic capacity in spinal cord injured people. Cent Nerv Syst Trauma 1986;3(1):77–91. doi: 10.1089/cns.1986.3.77 [DOI] [PubMed] [Google Scholar]
- 24.Janssen TWJ, Glaser RM, Shuster DB.. Clinical efficacy of electrical stimulation exercise training: effects on health, fitness, and function. Top Spinal Cord Inj Rehabil 1998;3(3):33–49. [Google Scholar]
- 25.Ragnarsson KT. Functional electrical stimulation after spinal cord injury: current use, therapeutic effects and future directions. Spinal Cord 2008;46(4):255–74. doi: 10.1038/sj.sc.3102091 [DOI] [PubMed] [Google Scholar]
- 26.Vette AH, Wu N, Masani K, Popovic MR.. Low-intensity functional electrical stimulation can increase multidirectional trunk stiffness in able-bodied individuals during sitting. Med Eng Phys 2015;37(8):777–82. doi: 10.1016/j.medengphy.2015.05.008 [DOI] [PubMed] [Google Scholar]
- 27.Triolo RJ, Boggs L, Miller ME, Nemunaitis G, Nafy J, Nogan Bailey S.. Implanted electrical stimulation of the trunk for seated postural stability and function after cervical spinal cord injury: a single case study. Arch Phys Med Rehabil 2009;90(2):340–7. doi: 10.1016/j.apmr.2008.07.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Triolo RJ, Nogan Bailey S, Miller ME, Lombardo LM, Audu ML.. Effects of stimulating hip and trunk muscles on seated stability, posture, and reach after spinal cord injury. Arch Phys Med Rehabil 2013;94(9):1766–75. doi: 10.1016/j.apmr.2013.02.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Triolo RJ, Nogan Bailey S, Lombardo LM, Miller ME, Foglyano K, Audu ML.. Effects of intramuscular trunk stimulation on manual wheelchair propulsion mechanics in 6 subjects with spinal cord injury. Arch Phys Med Rehabil 2013;94(10):1997–2005. doi: 10.1016/j.apmr.2013.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barfield J-P, Malone LA.. Performance test differences and Paralympic Team selection: pilot study of the United States National wheelchair rugby team. Int J Sports Sci Coach 2012;7(4):715–20. doi: 10.1260/1747-9541.7.4.715 [DOI] [Google Scholar]
- 31.Rosenthal R. Effect sizes: Pearson’s correlation, its display via the BESD, and alternative indices. Am Psychol 1991;46(10):1086–7. doi: 10.1037/0003-066X.46.10.1086 [DOI] [Google Scholar]
- 32.Altmann VC, Hart AL, Vanlandewijck YC, van Limbeek J, van Hooff ML.. The impact of trunk impairment on performance of wheelchair activities with a focus on wheelchair court sports: a systematic review. Sport Med – Open 2015;1(22):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stephens CL, Engsberg JR.. Comparison of overground and treadmill propulsion patterns of manual wheelchair users with tetraplegia. Disabil Rehabil Assist Technol 2010;5(6):420–7. doi: 10.3109/17483101003793420 [DOI] [PubMed] [Google Scholar]
- 34.Glaser RM. Physiologic aspects of spinal cord injury and functional neuromuscular stimulation. Cent Nerv Syst Trauma 1986;3(1):49–62. doi: 10.1089/cns.1986.3.49 [DOI] [PubMed] [Google Scholar]
- 35.Taylor P, Tromans AM, Harris KR, Swain ID.. Electrical stimulation of abdominal muscles for control of blood pressure and augmentation of cough in a C3 / 4 level tetraplegic. Spinal Cord 2002;40(1):34–36. doi: 10.1038/sj.sc.3101250 [DOI] [PubMed] [Google Scholar]
- 36.West CR, Goosey-Tolfrey VL, Campbell IG, Romer LM.. Effect of abdominal binding on respiratory mechanics during exercise in athletes with cervical spinal cord injury. J Appl Physiol 2014;117(1):36–45. doi: 10.1152/japplphysiol.00218.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wecht JM, Bauman WA.. Decentralized cardiovascular autonomic control and cognitive deficits in persons with spinal cord injury. J Spinal Cord Med 2013;36(2):74–81. doi: 10.1179/2045772312Y.0000000056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pette D, Vrbova G.. What does chronic electrical stimulation teach us about muscle plasticity? Muscle Nerve 1999;22(6):666–77. doi: [DOI] [PubMed] [Google Scholar]
- 39.Muccio P, Andrews B, Byron Marsolais E.. Electronic orthoses: technology, prototypes, and practices. J Prosthetics Orthot 1988;1(1):3–17. doi: 10.1097/00008526-198810000-00004 [DOI] [Google Scholar]
- 40.Gorgey AS, Black CD, Elder CP, Dudley GA.. Effects of electrical stimulation parameters on fatigue in skeletal muscle. J Orthop Sport Phys Ther 2009;39(9):684–92. doi: 10.2519/jospt.2009.3045 [DOI] [PubMed] [Google Scholar]
- 41.McCaughey EJ, Borotkanics RJ, Gollee H, Folz RJ, McLachlan AJ.. Abdominal functional electrical stimulation to improve respiratory function after spinal cord injury: a systematic review and meta-analysis. Spinal Cord 2016;54(9):628–39. doi: 10.1038/sc.2016.31 [DOI] [PubMed] [Google Scholar]
- 42.Linder SH. Functional electrical stimulation to enhance cough in quadriplegia. Chest 1993;103(1):166–9. doi: 10.1378/chest.103.1.166 [DOI] [PubMed] [Google Scholar]
- 43.Langbein WE, Maloney C, Kandare F, Stanic U, Nemchausky B, Jaeger RJ.. Pulmonary function testing in spinal cord injury: effects of abdominal muscle stimulation. J Rehabil Res Dev 2001;38(5):591–7. [PubMed] [Google Scholar]
- 44.Chen C, Yeung K, Bih L, Wang CH, Chen MI, Chien JC.. The relationship between sitting stability and functional performance in patients with paraplegia. Arch Phys Med Rehabil 2003;84(9):1276–81. doi: 10.1016/S0003-9993(03)00200-4 [DOI] [PubMed] [Google Scholar]
- 45.Field-Fote EC, Ray SS.. Seated reach distance and trunk excursion accurately reflect dynamic postural control in individuals with motor-incomplete spinal cord injury. Spinal Cord 2010;48(10):745–9. doi: 10.1038/sc.2010.11 [DOI] [PMC free article] [PubMed] [Google Scholar]