Abstract
Context: Primary leiomyosarcomas are malignant tumors of smooth muscles, with few reported cases occurring in the cervical spine. The authors report a case involving a 29-year-old man with primary leiomyosarcoma in the spinal canal posterior to the C3–C5 vertebrae.
Findings: No obvious osteolytic lesions could be found in neither X-ray nor computed tomography scan. Because of the confusion of nontypical imaging findings, a decompressive surgery of anterior cervical corpectomy of C4 and reconstruction with a mesh cage filled with allogenic bone grafts were performed. The patient refused a second operation and then was advised to receive the radiotherapy. No recurrence of the symptoms was evident 6 months after surgery.
Conclusion: When a patient suffers from upper cervical tumor, the leiomyosarcoma should be kept in mind as possible diagnoses despite its low occurring ratio. Early detection, early diagnosis, and early treatment must be the goal of the strategy.
Keywords: Cervical spine, Leiomyosarcoma, Smooth muscle, Osteoclasia, Corpectomy
Introduction
Primary leiomyosarcomas are rare malignant tumors of smooth muscles. Patients with leiomyosarcoma usually suffered from poor prognosis for the high metastatic recurrence rate and relative resistivity to radiotherapy and chemotherapy.1 In most cases, leiomyosarcoma arise in the retroperitoneum, subcutaneous tissue of the extremities, and intra-abdominal space such as gastrointestinal tract and uterus. Primary leiomyosarcoma of bone is quite rare, among which most cases occur in the femur and tibia. Primary leiomyosarcomas located in the cervical spinal regions were much scarcer. To our knowledge, only three relevant cases with obvious osteoclasia have been reported.1–3 In this report, we want to describe a case of primary leiomyosarcoma in the spinal canal which have invaded the C4 vertebra but did not exhibit obvious osteoclasia.
Case report
A 29-year-old male complaining about neck pain radiating into the left shoulder which had persisted for one month was admitted to our hospital. The progressively increased pain feeling and unresponsiveness to analgesics or traditional Chinese medicine made him seek medical advice in our hospital. The patient's medical history included the surgical enucleation of the left eye for retinoblastoma in his 5-year-old. No obviously positive symptom was found in physical examination.
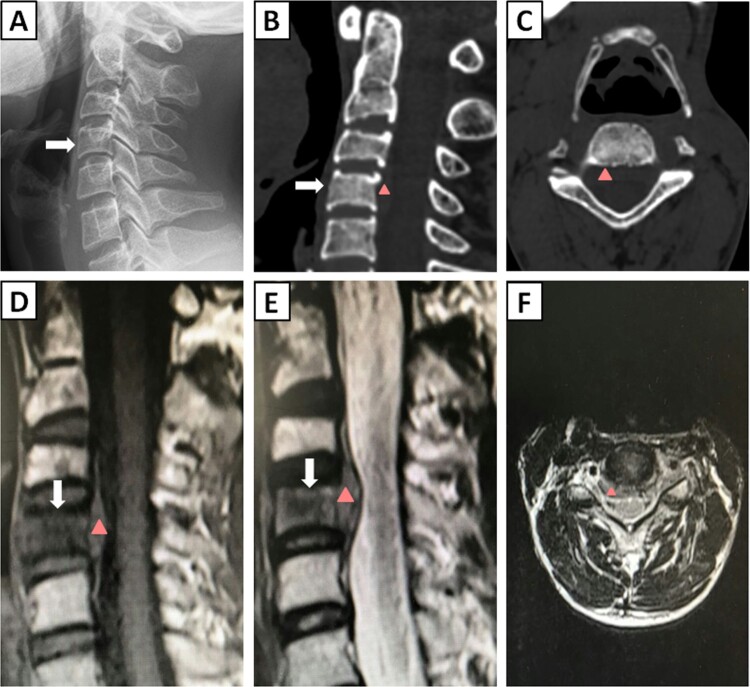
No abnormal findings were revealed in laboratory examinations and the X-ray (Fig. 1A). Computed tomography (CT) scans showed soft-tissue mass in the spinal canal posterior to the C3–C5 vertebrae without obvious osteoclasia (Fig. 1B and C). Magnetic resonance imaging (MRI) showed that the spinal cord at the level of the C3–C5 spine was compressed by a soft-tissue mass, which was mostly isointense on T1-weighted MRI scans, of mixed is a low signal on T2-weighted MRI scans. The signal of C4 vertebra was isointense to that of posterior soft-tissue mass and showed as hypointense compared with other vertebrae on both T1 and T2-weighted MRI scans (Fig. 1D–F). The positron emission tomography/computed tomography (PET-CT) was also conducted for a systemic evaluation, in which high fluorodeoxyglucose (FDG) uptake could only be found in the area of C3–C5 level spinal canal and left intervertebral foramens, further demonstrating the primary tumor.
Figure 1.
Images of preoperative radiological examinations. (A) Plain cervical spine radiograph. (B) Sagittal view of CT scan. (C) Axial view of CT scan (C4). (D) Sagittal T1-weighted MRI. (E) Sagittal T2-weighted MRI. (F) Axial T2-weighted MRI of C4. The white arrow indicates the C4 vertebra, and the red triangles indicate the tumor tissue posterior to the C3–C5 vertebrae.
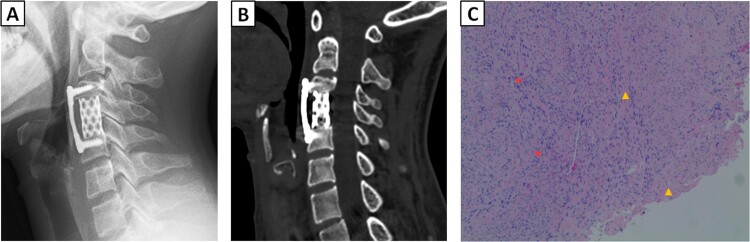
After general anesthesia, the patient was placed in the supine position with the neck slightly extended. A right-sided transverse skin incision was used to expose the cervical spine. Following discectomies of C3/C4 and C4/C5 intervertebral discs, a C4 corpectomy was performed. No obvious abnormity could be observed or felt during biting away the C4 vertebra. The excision of vertebral posterior margin and posterior soft tissue were performed under the microscope. After removing the posterior longitudinal ligament, dural sacs were found to be pressed by the grayish-white tumor tissue. Then the tumor tissue was removed for a total decompression, and a titanium mesh cage full filled with allogenic bone grafts was placed between the C3 and C5 vertebrae. The titanium mesh cage was further covered by a locking plate (Fig. 2A and B).
Figure 2.
Images of radiological examinations obtained 1 week after surgery and pathological examination. (A) Postoperative plain cervical spine radiograph. (B) Postoperative sagittal view of CT scan, revealing that tumor tissue could no longer be found in spinal canal posterior to the C3–C5 vertebrae. (C) Result of pathological examination (C4 vertebra, stained with haemotoxylin and eosin, magnification × 40): yellow triangles indicate the bone tissue, and red stars show leiomyosarcoma cells.
Through the pathological examination of soft-tissue mass and resected bone, spindle-shaped cells were found invading the C4 vertebra (Fig. 2C). The immunohistochemical staining was positive for CD34 (vessel), SMA, Vimentin, EMA (partly), Ki67 (20–50%), Calponin, Desmin, but negative for Lysozyme, PGP9.5, S-100, SOX10, NF, MyoD1. Based on these results, a diagnosis of well-differentiated leiomyosarcoma aggressing vertebra was finally identified. We recognized that the excision extension might be insufficient. However, the patient refused the second operation, and then he was advised to receive the radiotherapy.
Discussion
Leiomyosarcoma is a kind of soft-tissue sarcoma. Their aggressive nature and hematogenous spreading propensity lead to their definition of malignant neoplasm, which also contribute to the poor prognosis. The 5-year survival rate for leiomyosarcomas is about 38–60%, with metastases occurring in at least 50%. Leiomyosarcoma usually occurs in soft tissues of extremities and trunk. Primary leiomyosarcoma of head and neck is rare, with a ratio of only approximately 3%.4 Furthermore, primary leiomyosarcoma of the cervical spine is extremely rare. To our knowledge, there are only three reported cases of primary leiomyosarcoma in cervical spine invading the spinal canal and vertebra before.1–3 The characteristics of these three cases of primary cervical spine leiomyosarcoma are summarized in Table 1.
Table 1. Reported primary leiomyosarcomas in cervical spine invading the spinal canal and vertebra.
| Study | Site | Age (years) | Sex | Follow-up (months) | Presenting symptoms | Duration of symptom | Osteoclasia | Surgical strategy | Postoperative treatment |
|---|---|---|---|---|---|---|---|---|---|
| Marshman et al. | C3–C5 | 61 | Female | Lost follow-up | Progressive spastic quadriparesis and acute urinary retention | NR | Bone erosion and infiltration within the posterior elements of C4 | First operation: decompressive laminectomy from C3 to C5 and soft-tissue tumor subtotal excision Second operation: complete macroscopic tumor excision incorporating posterior stabilization with the use of C2 pedicle and C3–C6 lateral mass screws coupled to contour rods |
None |
| Ochiai et al. | C7 | 69 | Male | 6 (dead) | Dysesthesia of both hands | 2 months | C7 compression fracture | Biopsy of the tumor | None |
| Sucu et al. | C2 | 25 | Female | 12 (alive) | Neck and left upper extremity pain | 6 months | Infiltrative lesion in the left C2 region | Left-sided partial spondylectomy plus expandable titanium prosthesis reconstruction and posterior craniocervical fixation | Radiotherapy |
| Current study | C3–C5 | 29 | Male | 6 (alive) | Neck pain radiating into the left shoulder | 1 month | None | Anterior C4 corpectomy and reconstruction with a mesh cage filled with allogenic bone grafts | Radiotherapy |
NR: not reported.
Because of its aggressive nature, leiomyosarcoma adjacent to the bone is usually combined with extensive infiltration of the trabecular bone. These tumors are usually initially diagnosed with X-ray or CT, the principal feature of which consists in a solitary osteolytic lesion with indistinct margins and cortical destruction with no presence of bone matrix production, with about 15% patients presenting with a pathological fracture. All the three previously reported cases reported the osteolytic lesion of vertebra: one reported the compression fracture of the vertebra,2 one reported the infiltrative lesion in the left C2 region,3 and one reported the bone erosion and infiltration within the posterior elements of C4.1 However, in our case no obvious bone destruction could be found in X-ray, CT scan, PET-CT, or even under direct vision, which disturbed our primary diagnosis of the tumor at the initial stage. We inferred the reason could be that the tumor was in its early stage, who just invaded to the vertebra without destructing the structure of bone.
As for the similar imaging findings in some cases, it might be hard to distinguish other tumors such as leiomyoma, fibrosarcoma, rhabdomyosarcoma, schwannmoas, spindle-cell carcinoma, schwannoma, neurofibroma, meningioma, and ependymoma from leiomyosarcomas by imageological examinations. So, the pathological examination is required for a more specific diagnosis. Under the microscope the specimen usually reveals prominent interlacing bundles and fascicles of elongated spindle cells with elongated cigar-shaped blunt-ended nuclei, prominent nucleoli, and abundant eosinophilic cytoplasm. Additionally, immunohistochemical studies are also important for the correct diagnosis of smooth muscle cell origin. The leiomyosarcoma is usually positive for smooth muscle actin, weakly positive for desmin, and negative for S-100.
Surgical excision is still the primary recommendation for the treatment of leiomyosarcoma. Despite most surgeons emphasizing the long survival is associated with the total resection of the tumor, some studies revealed that the limit of tumor resection only correlated to the local recurrence rate rather than the survival rate. There was no standard surgical procedure for the leiomyosarcoma of the cervical spine, as different cases have different occurring sites and infiltration regions. In the three previous reported cases, Sucu et al. treat the leiomyosarcoma locating on the left side of C2 with a left-sided partial spondylectomy plus expandable titanium prosthesis reconstruction and posterior craniocervical fixation.3 The patient in the case of Marshman et al. presented with progressive spastic quadriparesis and acute urinary retention, so she received a decompressive laminectomy from C3 to C5 and soft-tissue tumor subtotal excision for the first operation.1 Four weeks later the patient regained independent walking and normal sphincter function, and received the second operation with complete macroscopic tumor excision incorporating posterior stabilization with the use of C2 pedicle and C3–C6 lateral mass screws coupled to contour rods. In general, the surgical strategy of cervical spine leiomyosarcoma should be trying best to completely excise the tumor with rigidly rebuilding the construction.
In our case, as no obvious bone destruction and distant metastasis could be found in the imageological examinations, the tumor was considered as benign preoperatively after the consultation of Nuclear Medicine Department and Radiology Department. We initially advised the patient to receive aspiration biopsy or incisional biopsy for a more accurate diagnosis. The patient, however, refused and was more desired for an operation to release his symptom. Additionally, considering the whole involvement of the C4 vertebra, a decompressive surgery of anterior cervical corpectomy and fusion was finally selected as the therapeutic strategy. After obtaining the diagnosis of pathological examination and immunohistochemical staining we recognized that the excision extension might be insufficient. Unfortunately, the patient refused the second operation. So in its early stage, the leiomyosarcoma can be atypical on imageological examinations, which may affect the scheme of treatment and emphasize the significance of early accurate diagnosis. We introspected that biopsy or intra-operative frozen section analysis might be good choices. However, intra-operative frozen section analysis is sometimes difficult to make an accurate diagnosis in the musculoskeletal tumor. So we consider that the tumor should be resected as widely as possible during the primary operation, otherwise once postoperatively confirming the leiomyosarcoma a second surgery is still recommended.
No clear survival benefit has been demonstrated with the use of adjuvant chemotherapy or radiotherapy. However, as there may be differences in biological behavior, radiotherapy and/or chemotherapy are still recommended especially for the cases failed to obtain the total resection of the lesion. In the present case, the patient was referred for further radiotherapy after we confirmed the pathology of the tumor, and no recurrence of the symptoms was exhibited during the 6-month phone call follow-up as the patient lack of compliance. Nevertheless, more detailed evaluation with a longer follow-up period is still required.
The patient in this case had past medical history of retinoblastoma. Similarly, several cases reported secondary leiomyosarcoma of the urogenital system in patients with retinoblastoma. The mechanism remained unclear. Holzmann et al. found that uterine leiomyosarcoma revealed multiple genetic aberrations including bi-allelic deletions of the RB1 gene, the mutation of which also played an important role in the occurrence of retinoblastoma.5 In general, most authors believed that patients with retinoblastoma are at a highly increased risk of developing subsequent second malignancies due to genetic mutations, long-term survival, and effects of radiation and chemotherapy. So when treating the patient with a previous history of retinoblastoma the doctor should be aware of the second malignancy risks.
Conclusions
To the best of our knowledge, this is the first case of a primary leiomyosarcoma in the cervical spine without obvious osteolytic lesions in neither X-ray nor CT scan. Despite its low occurring ratio, leiomyosarcoma should be kept in mind as possible diagnoses for patients suffer from the upper cervical tumor. Early detection, early diagnosis, and early treatment must be the goal of the strategy.
Disclaimer statements
Contributors None.
Funding None.
Conflicts of interest The authors declare no conflicts of interest.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
References
- 1.Marshman LA, Pollock JR, King A, Chawda SJ.. Primary extradural epithelioid leiomyosarcoma of the cervical spine: case report and literature review. Neurosurgery. 2005;57(2):372. doi: 10.1227/01.NEU.0000166695.89757.A4 [DOI] [PubMed] [Google Scholar]
- 2.Ochiai H, Yamakawa Y, Fukushima T, Yamada H, Hayashi T.. Primary leiomyosarcoma of the cervical spine causing spontaneous compression fracture: report of an autopsy case. Neuropathology. 2000;20(1):60–4. doi: 10.1046/j.1440-1789.2000.00279.x [DOI] [PubMed] [Google Scholar]
- 3.Sucu HK, Bezircioglu H, Rezanko T.. Partial spondylectomy for primary leiomyosarcoma of c2 vertebra. Spine (Phila Pa 1976). 2011;36(21):E1422–E1426. doi: 10.1097/BRS.0b013e31820a79c6 [DOI] [PubMed] [Google Scholar]
- 4.Takahashi T, Higo R, Nakata H, Sugasawa M.. Leiomyosarcoma of the hypopharynx: a case report. Auris Nasus Larynx. 2008;35(2):304–7. doi: 10.1016/j.anl.2007.10.002 [DOI] [PubMed] [Google Scholar]
- 5.Holzmann C, Koczan D, Loening T, Rommel B, Bullerdiek J.. Case report: a low-grade uterine leiomyosarcoma showing multiple genetic aberrations including a bi-allelic loss of the retinoblastoma gene locus, as well as germ-line uniparental disomy for part of the long arm of chromosome 22. Anticancer Res. 2017;37(5):2233–37. doi: 10.21873/anticanres.11559 [DOI] [PubMed] [Google Scholar]