Abstract
A 54-year-old man, with previous history of neurogenic heterotopic ossification (HO) in muscles around the left hip following a spinal cord injury ten months earlier, was referred to our nuclear medicine center for an 18fluorine-fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) to rule out a spondylodiscitis. No sign of spondylodiscitis was found on 18F-FDG PET/CT, but images revealed an increased 18F-FDG uptake in HO areas, matching with ongoing osteoblastic activity on a following bone scan.
Keywords: Heterotopic ossification, bone scan, 18F-FDG PET/CT
Abstract
On ay önce omurilik yaralanmasını takiben sol kalça çevresindeki kaslarda nörojenik heterotopik ossifikasyon (HO) öyküsü olan 54 yaşında bir erkek hasta, spondilodiskiti ekarte etmek için 18flor-florodeoksiglukoz (18F-FDG) pozitron emisyon tomografisi/bilgisayarlı tomografi (PET/BT) için nükleer tıp merkezimize sevk edildi. 18F-FDG PET/BT’de spondilodiskit belirtisi bulunmadı, ancak görüntüler, sonraki kemik taramasında devam eden osteoblastik aktivite ile eşleşen, HO alanlarında 18F-FDG tutulumunun arttığını ortaya koydu.
Figure 1.
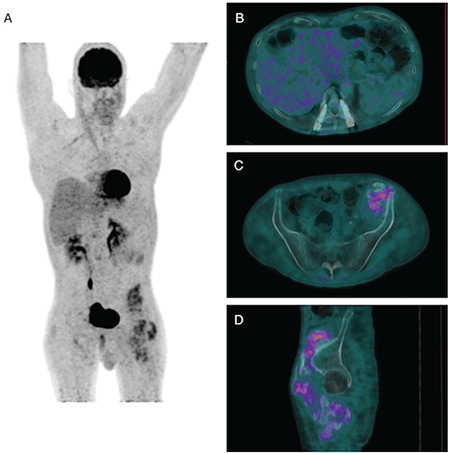
A 54-year-old man was referred to our nuclear medicine center for a combined 18fluorine-fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) to rule out a spondylodiscitis. He had a previous history ten months earlier of a thoracolumbar fracture complicated with paraplegia, treated with anterolateral decompression and fixation. He presented unexplained persistent lumbar pain and C-reactive protein level above the normal range after two successfully treated obstructive pyelonephritis, and a suspicion of spondylodiscitis was waived. The patient was known to present heterotopic ossification (HO) associated with the spinal cord injury with multiple areas of dense calcifications in the muscles around the left hip, as the anterior compartment of the thigh and iliopsoas muscle. No sign of spondylodiscitis was found on 18F-FDG PET/CT (maximum intensity projection 18F-FDG PET/CT image A, axial fused PET/CT image B), but images revealed a diffuse increased 18F-FDG uptake in a few of HO areas (axial and sagittal fused PET/CT images C and D).
Figure 2.
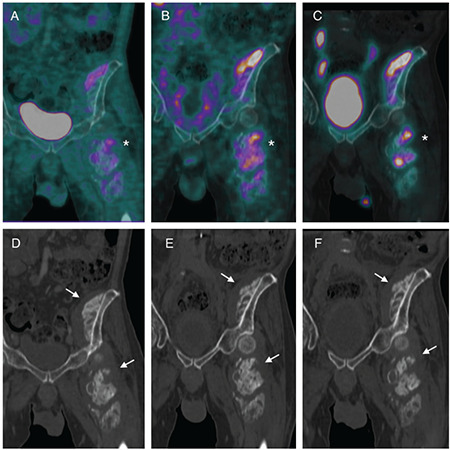
A complementary 3-phase bone scan was secondly performed. The bone scan showed extra-osseous extensive accumulations of technetium-99m (Tc-99m) hydroxymethylene diphosphonate matching with increased 18F-FDG uptake areas. Coronal fused PET/CT image (A), coronal fused single photon emission computed tomography/CT images on soft-tissue phase (B) and on delayed phase (C), showing a matching tracer uptake between the two modalities in HO areas around the left hip (asterisks). On CT images, multiple areas of dense calcifications were seen (arrows, coronal CT images D, E, and F). HO is a diverse pathologic process, defined as the formation of extraskeletal bone in muscle and soft tissues, usually between the muscle and the joint capsule. The reported incidence of HO in patients with spinal cord injury is approximately 20% (1). Such development of neurogenic HO generally occurs within a few months after spinal cord injury and progresses over a period of years (2). Clinically, neurogenic HO may cause severe pain during the process of formation and adversely affecting quality of life (3). Three-phase bone scanning is a highly sensitive method for the assessment of progression, maturation process and extent of HO. An increased vascularity on angiographic flow and soft-tissue phases is the earlier sign. Then occurs Tc-99m methyl diphosphonate (MDP) accumulation on delayed-phase, which is often seen 4 to 6 weeks earlier than ossification (4). Threephase bone scanning could be required for the clinical management of HO. Indeed, conservative treatment such as medication or local radiotherapy could be performed over surgical excision in case of high Tc-99m MDP accumulation (5). 18F-FDG uptake in HO, suggestive of active inflammation, is known as a pitfall of 18F-FDG PET/CT imaging. The concern, especially in early cases is that the imaging findings on FDG PET/CT could mimic that of aggressive sarcomas (6,7,8). Elucidating the antecedent history becomes important in making the current diagnosis in these patients.
Footnotes
Ethics
Informed Consent: A written informed consent was obtained.
Peer-review: Externally peer-reviewed.
Authorship Contributions
Concept: J.T., Design: J.T., Data Collection or Processing: M.D., J.T., Analysis or Interpretation: M.D., J.T., Literature Search: M.D., Writing: M.D., J.T.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.
References
- 1.Wittenberg RH, Peschke U, Bötel U. Heterotopic ossification after spinal cord injury. Epidemiology and risk factors. J Bone Joint Surg Br. 1992;74:215–218. doi: 10.1302/0301-620X.74B2.1544955. [DOI] [PubMed] [Google Scholar]
- 2.Meyers C, Lisiecki J, Miller S, Levin A, Fayad L, Ding C, Sono T, McCarthy E, Levi B, James AW. Heterotopic ossification: a comprehensive review. JBMR Plus. 2019;3:e10172. doi: 10.1002/jbm4.10172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cipriano CA, Pill SG, Keenan MA. Heterotopic ossification following traumatic brain injury and spinal cord injury. J Am Acad Orthop Surg. 2009;17:689–697. doi: 10.5435/00124635-200911000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Freed JH, Hahn H, Menter R, Dillon T. The use of three-phase bone scan in the early diagnosis of heterotopic ossification (HO) and in the evaluation of Didronel therapy. Paraplegia. 1982;20:208–216. doi: 10.1038/sc.1982.39. [DOI] [PubMed] [Google Scholar]
- 5.Lin Y, Lin WY, Kao CH, Tsai SC. Easy interpretation of heterotopic ossification demonstrated on bone SPECT/CT. Clin Nucl Med. 2014;39:62–63. doi: 10.1097/RLU.0b013e318286824f. [DOI] [PubMed] [Google Scholar]
- 6.Koob M, Durckel J, Dosch JC, Entz-Werle N, Dietemann JL. Intercostal myositis ossificans misdiagnosed as osteosarcoma in a 10-year-old child. Pediatr Radiol. 2010;40:S34–37. doi: 10.1007/s00247-010-1769-5. [DOI] [PubMed] [Google Scholar]
- 7.Clarençon F, Larousserie F, Babinet A, Zylbersztein C, Talbot JN, Kerrou K. FDG PET/CT findings in a case of myositis ossificans circumscripta of the forearm. Clin Nucl Med. 2011;36:40–42. doi: 10.1097/RLU.0b013e3181feed95. [DOI] [PubMed] [Google Scholar]
- 8.Costelloe CM, Murphy WA Jr, Chasen BA. Musculoskeletal pitfalls in 18F-FDG PET/CT: pictorial review. AJR Am J Roentgenol. 2009;193:WS1–WS13. doi: 10.2214/AJR.07.7138. [DOI] [PubMed] [Google Scholar]


