Abstract
Objectives:
To analyze the change in circulating angiogenic factor levels after transarterial radioembolization (TARE) for colorectal cancer liver metastases (CRCLMs) and its prognostic significance
Methods:
Blood samples immediately before TARE and on 1 day, 1 week and 6 weeks after were collected for angiogenic factor analysis in 23 patients.
Results:
Patients with elevated serum basic fibroblast growth factor and platelet-derived growth factor levels in the 1st week and vascular endothelial growth factor (VEGF) levels in the 6th week after TARE had significantly shorter median overall survival (OS) times.
Conclusion:
Some early increases in serum angiogenic factor levels and in serum VEGF in the 6th week after TARE for CRCLMs are related to short OS and progression-free survival.
Keywords: Colorectal cancer, liver metastasis, transarterial radioembolization, serum angiogenic factors
Abstract
Amaç:
Kolorektal kanser metastazları için transarteriyel radyoembolizasyon (TARE) sonrası dolaşımda anjiyojenik faktörlerin seviyelerindeki değişikliklerin analiz edilmesidir.
Yöntem:
Anjiyojenik faktör analizi için 23 hastada TARE’den hemen önce, 1. günde, 1. haftada ve 6 hafta sonra kan örnekleri toplandı.
Bulgular:
TARE sonrası 1. haftada bazik fibroblast büyüme faktörü ve platelet kaynaklı büyüme faktörü seviyelerinde ve 6. haftada vasküler endotelyal büyüme faktörü (VEGF) seviyelerinde artış olan hastalarda medyan genel sağkalım süreleri istatistiksel olarak daha kısaydı.
Sonuç:
Bazı anjiyojenik faktör seviyelerinde erken yükselişler ve kolorektal kanser metastazları için TARE sonrası 6. haftada serum VEGF seviyelerinde artış olması kısa genel sağkalım ve progresyonsuz sağkalım ile ilişkilidir.
Introduction
The liver is the most common metastasis site of colorectal cancer (CRC) and a major cause of death (1). The only curative treatment choice is surgery; however, it is impossible for most patients, and palliative options such as systemic treatments may be administered instead (2). Local treatment options should be considered for patients for whom systemic treatments fail. Specifically, transarterial radioembolization (TARE) might be an alternative for these patient groups (3).
Ideal candidates for TARE for colorectal cancer liver metastases (CRCLMs) are those with liver-dominant, unresectable, and chemorefractory tumors (4,5). Resin microspheres with diameters of 30-40 mm embedded with Yttrium-90 (Y-90) are delivered to the hepatic artery via a catheter. The microspheres become lodged in the arteriolar system of the tumor and cause necrosis due to radiation and embolic effects (6,7,8). Despite the promising outcomes for CRCLM, not all patients show a good response to TARE. Moreover, some patients experience rapid progression of extrahepatic disease following TARE. One of the possible explanations is an increase in circulating angiogenic factor levels after TARE and their effects on extrahepatic progression. Because both radiation and embolization promote angiogenesis, it has been hypothesized that increases in proangiogenic cytokines or decreases in cytokines that inhibit angiogenesis may affect the response to TARE (9,10,11). Measuring these markers might therefore have predictive value for treatment response to TARE. If increases in circulating angiogenic factor levels can be proven to be related to prognosis, concomitant use of anti-angiogenic treatments with TARE may improve patient outcomes.
To date, only three studies have focused on angiogenic markers after TARE (9,12,13,14), and one included only hepatocellular cancer (HCC) patients (12). Considering the limited data on this topic, in our pilot study, we included patients with CRCLM and measured circulating angiogenic factors and baseline levels at different time points after TARE. The primary goal of this study was to determine whether there is a change in circulating angiogenic factor levels after TARE with resin microspheres and to investigate possible prognostic importance. We also compared the baseline circulating angiogenic factor levels of patients with and without extrahepatic disease as a secondary objective.
Materials and Methods
This prospective study was approved by the Ankara University Faculty of Medicine, Local Institutional Ethical Committee (decision number: 01-14-16) and supported by a research grant from the Nevin Baykent Health and the Education Foundation. Inclusion criteria were as follows: Older than 18 years, the existence of inoperable CRCLM, fit the criteria for TARE, and provided informed consent for the trial. The exclusion criteria were as follows: Younger than 18 years, prior history of bevacizumab therapy, coexistence of a secondary malignancy, and any contraindications for TARE. Written informed consent was obtained from all participants. All patients who fitted the inclusion criteria and received TARE between March 2016 and May 2019 for the treatment of CRCLM were included in the analysis. Pretreatment tumor load of the liver was evaluated by computed tomography (CT) or magnetic resonance imaging of the liver. Pretreatment 18fluorine-fluorodeoxyglucose (18F-FDG) positron emission tomography (PET)/CT was performed to assess the extrahepatic tumor load. After the TARE, none of the patients received additional treatment until the 6th week. Treatment response and extrahepatic disease progression were evaluated using 18F-FDG PET/CT using the PERCIST 1.1 criteria, which is based on the percent change in metabolic activity at the 6th week of follow-up. The outline of the study design is given in Figure 1.
Figure 1.
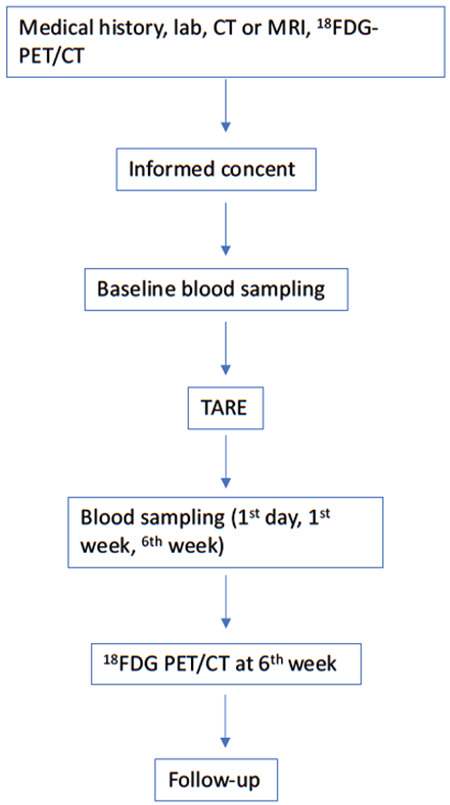
Outline of the clinical evaluations and study procedures
CT: Computed tomography, MRI: Magnetic resonance imaging, 18F-FDG: 18Fluorine-fluorodeoxyglucose, PET: Positron emission tomography, TARE: Transarterial radioembolization
Transarterial Radioembolization
The widely accepted parameters of liver reserve, bone marrow reserve (granulocytes >1500/µL, platelets >60000/µL), and hepatic vascularity were used as inclusion and exclusion criteria for TARE. Liver reserve was assessed on serum bilirubin, aspartate transaminase (AST), alanine transaminase (ALT), gamma glutamyl transferase (GGT), and alkaline phosphatase (ALP) levels. For radioembolization, bilirubin levels below 2 mg/dL AST, ALT and ALP levels less than five times the standard upper limit was required. The candidate patient provided written informed consent. The Y-90 dose was adjusted according to the following body surface area (BSA) method: Activity (GBq) = (BSA -0.2) + tumor volume/total liver volume. Tumor and liver volumes were calculated from CT images. The lung shunt fraction was calculated from hepatic artery perfusion scintigraphic images. Mean absorbed dose thresholds were accepted as 120 Gy for tumors, 50 Gy for non-tumorous liver tissue and 20 Gy for the lung. The Y-90 resin microspheres (Sirtex Medical) were injected through selective catheterization of the hepatic artery catheter under intermittent fluoroscopic visualization. A right femoral puncture was performed using the landmark technique, where the maximal pulse was palpated; left femoral puncture was performed if right femoral access could not be achieved because of underlying vascular pathology. For hepatic arterial catheterizations, either the celiac truncus or superior mesenteric artery was selectively catheterized with an appropriate 5 F catheter (Sim2, C2, RDC, or sim 1; Imager II Boston Scientific Corp., Natick, MA, USA or Terumo Medical Corp., Tokyo, Japan). After selective catheterization of the artery, a 2.7 F microcatheter set with a 0.021-inch guidewire (Progreat; Terumo Medical Corp., Tokyo, Japan) was used for superselective catheterization of the tumor feeders coaxial. Subsegmental, selective right, or selective left hepatic arterial catheterization decisions were made according to the vascularity patterns of the tumors on DSA images. If <2 hepatic segments were involved in diagnostic images, subsegmental catheterization was performed for ablative purposes. Within 1-24 hours after microsphere infusion, Bremsstrahlung images were obtained to confirm that Y-90 was deposited only in the liver. For patients with bilobar disease, TARE was applied in two separate sequences. All patients were hospitalized overnight, and medications (e.g., analgesics, antiemetic, H2 antagonists) were administered if necessary. All patients were closely monitored until acute or late toxicities were resolved.
Angiogenic Factor Measurements
Blood samples immediately before TARE and on 1day, 1 week and 6 weeks after were collected for angiogenic factor analysis. Serum vascular endothelial growth factor (VEGF), angiopoietin-2 (Ang-2), basic fibroblast growth factor (bFGF), hepatocyte growth factor (HGF) and platelet-derived growth factor (PDGF) measurements were performed by ELISA using the quantitative sandwich enzyme immunoassay technique.
Statistical Analysis
Descriptive data are expressed as median [minimum (min)-maximum (max)] or mean ± standard deviation (SD) values. The Mann-Whitney U test was used to compare the difference between the two groups in terms of non-normally distributed variables. Differences among the four time points for circulating angiogenic factor levels were evaluated by the Friedman test. When the p value from the Friedman test showed statistical significance, Bonferroni correction was applied for multiple comparisons. Nominal variables were tested by Fisher’s Exact test. Survival estimations were performed using the Kaplan-Meier algorithm, and comparison between groups was evaluated with the log-rank test. A p value less than 0.05 was considered significant. SPSS version 20.0 (IBM, Chicago, Illinois, USA) was used for the statistical analysis.
Results
Patients
Twenty-three patients (median age: 64, min-max: 45-78; 3 female and 20 male) with inoperable CRCLM were included in the study. All patients had inoperable liver-dominant or liver-only metastases and fitted the inclusion criteria. While the primary tumor was operable in 21 patients, it was inoperable in 2 patients. All patients had received chemotherapy and had chemorefractory or recurrent disease before TARE. Primary tumors were located in the right, left colon and rectum in 12 (52%), 8 (35%) and 3 (13%) patients, respectively. Surgical liver resection was performed in 4 (17%) patients; transarterial chemoembolization (TACE) was applied in 16 (70%) cases before the TARE. All patients had received one-line systemic chemotherapy for liver metastases before consideration for TARE; 16 (70%) patients received FOLFOX and 7 (30%) the FOLFIRI regimen. The median time between the last cycle of chemotherapy and TARE was (3 months, min-max: 1-5 months). The number of liver tumors was 1-5 in 5 (22%), 6-10 in 8 (35%) and >10 in 10 (43%) patients. The mean tumor diameter was calculated as 34.6±12.7 mm. The pretreatment mean levels of serum ALT, AST, GGT and ALP were 44.13±37.7 IU/L, 35.56±29.3 IU/L, 217.5±264.5IU/L, and 231.86±182.1IU/L, respectively. Before the TARE, extrahepatic disease was detected in 12 (52%) patients, located in the lymph nodes, lungs and bones in 8 (35%), 3 (13%) and 1 (4%), respectively. TARE was administered to both the right and left liver lobes in 5 (22%), 15 (65%) and 3 (13%) patients, respectively.
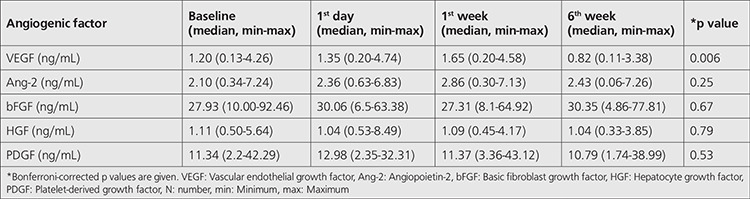
Angiogenic Factor Analyses
Baseline measurements of median serum angiogenic factor levels of patients with and without extrahepatic disease were not significant (Table 1). In the entire patient group, a slight increase in the median values of several angiogenic factors in the 1st day or in the 1st week after TARE was observed. While at the 1st day median values of all angiogenic factors except HGF were elevated, at the 1st week only median values of VEGF and Ang-2 were done. By the 6th week, serum VEGF levels were significantly decreased compared to on the 1st day and in the 1st week (Figure 2). An increase in any angiogenic factor level was seen in 21 (91%) patients on the 1st day, and increases were found in 21 (91%) and 17 (74%) patients in the 1st and 6th weeks. In three patients, all of the angiogenic factor levels were elevated on the 1st day and in the 1st week. Changes in the median values of serum angiogenic factor levels are summarized in Table 2.
Table 1. Descriptive data of baseline angiogenic factor levels of patients with and without extrahepatic disease.

Figure 2.
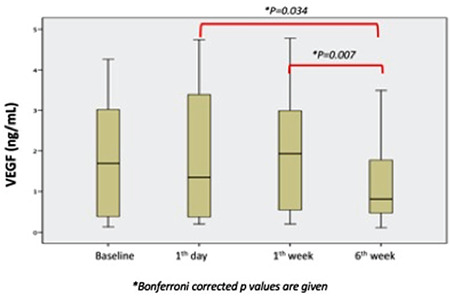
Boxplots of median serum VEGF levels after transarterial radioembolization for different time points
VEGF: Vascular endothelial growth factor, ng/mL: Nanogram per milliliter
Table 2. Change in median serum levels of different angiogenic factors at different time points.
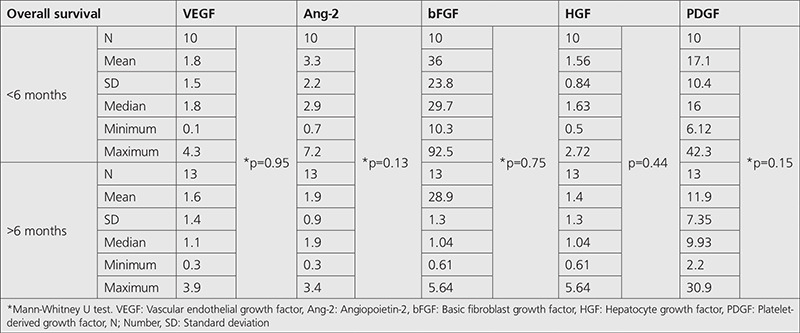
Follow-up and Survival Analyses
The survivors in this study had a minimum follow-up time of 4 months. There was an insignificant difference between baseline median angiogenic factor levels of those patients with overall survival (OS) longer than 6 months and those with OS shorter than 6 months (Table 3).
Table 3. Descriptive data of baseline angiogenic factor levels of patients who did or did not have overall survival longer than 6 months.
By the 6th week of follow-up, disease progression in the treated liver lobe was seen in 7 (30%) patients, and extrahepatic metastases were detected in 12 (52%). Some of the mean ± SD values of circulating angiogenic factor levels of the patients with and without progression in the treated liver lobe in the 6th week of follow-up were significantly different (Table 4, Figure 3); mean ± SD Ang-2 levels on the 1st day for patients with and without extrahepatic disease progression in the 6th week also differed significantly (Figure 4).
Table 4. Significant difference in circulating angiogenic factor levels of patients with and without progression of the treated liver lobe at the 6th week of follow-up.
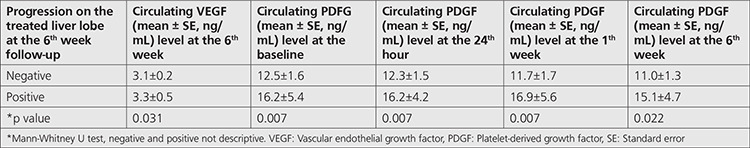
Figure 3.
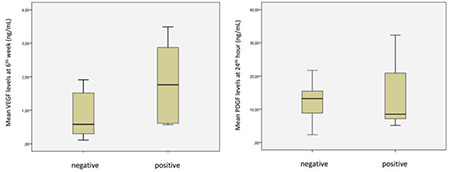
Boxplots representing significant distributions of median serum VEGF and PDGF levels of patients who had progression on treated liver lobe in the 6th week of follow-up
VEGF: Vascular endothelial growth factor, PDGF: Platelet-derived growth factor, Negative: No progression, Positive: Progression
Figure 4.
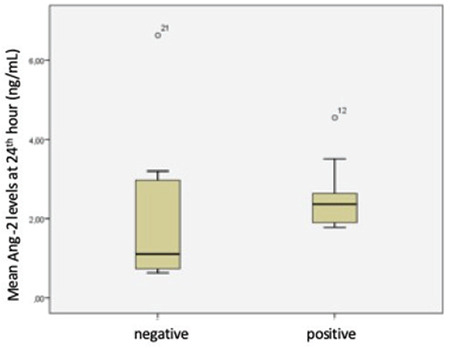
Boxplots representing significant distributions of mean Ang-2 levels of patients who had extrahepatic disease progession in the 6th week of follow-up
Ang-2: Angiopoietin-2, Negative: No progression, Positive: Progression
In the follow-up period, 16 (70%) patients had died by the median 20 months follow-up period (min: 3, max: 43). Patients with elevated serum bFGF and PDGF levels in the 1st week after TARE had significantly shorter median OS times than those without elevated levels [for FGF; 5.0±0.7 (95% confidance interval (CI); 3.7-6.3) months vs. 11.0±2.1 (95% CI; 7.0-15.0) months, p=0.004; for PGDF; 5.0±2.2 (95% CI; 0.8-9.2) months vs. 16.0±3.3 (95% CI: 9.4-22.6) months, p=0.013] (Figure 5). Patients who had elevated serum VEGF levels in the 6th week also had significantly shorter median OS times than those who did not [11.0±0.0 months vs. 16.0±1.2 (95% CI; 13.7-18.3) months, p=0.034] (Figure 5). Moreover, patients with elevations of all of the angiogenic factors in the 1st week had shorter median OS times than those who did not [5.0±0.0 months vs. 11.0±0.8 (95% CI; 9.5-12.5) months, p=0.007] (Figure 5).
Figure 5.
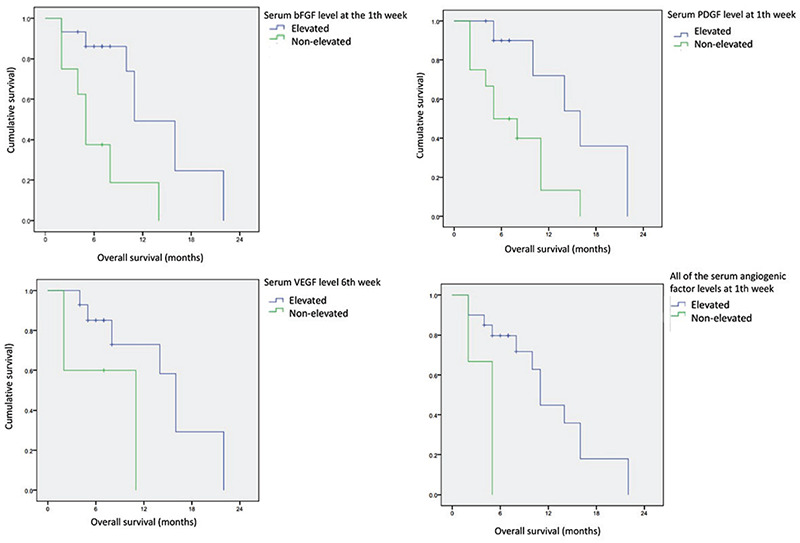
Kaplan-Meier survival curves of patient groups with significant overall survival differences according to elevated and non-elevated levels of different angiogenic factors at different time points. You have studied 5 angiogenic factors, but why only 2 parameters are included. why some week 1 and some week 6. It might be more descriptive if you elaborate more in the results section
bFGF: Basic fibroblast growth factor, VEGF: Vascular endothelial growth factor, PDGF: Platelet-derived growth factor
Disease progression occurred in 16 (70%) patients. Patients with elevated bFGF levels in the 1st week after TARE had significantly shorter median progression-free survival (PFS) than those without elevated bFGF levels [2.0±0.1 (95% CI, 2.0-2.1) months vs. 5.2±1.5 (95% CI, 1.6-9.0) months, p=0.050].
Discussion
Angiogenesis is a complex process that is still not fully understood. Antiangiogenic drugs have been developed for cancer treatment because the activation of the angiogenic process responds to hypoxia. Several studies have focused on angiogenic factors after transarterial treatments of liver tumors (9,14,15,16,17,18,19). However, most of them have been designed to evaluate the angiogenic response after TACE for HCC (16,17,18,19). In contrast, data on the angiogenic response after TARE for CRC liver metastases are limited to two studies (9,13). For this reason, in this pilot study, we analyzed the angiogenic response after TARE in CRCLM patients.
First, we evaluated the change in circulating angiogenic factor levels after TARE. An increase in most of the angiogenic factor levels was observed on the 1st day or in the 1st week after TARE. Moreover, in 91% of patients, at least one angiogenic factor level was increased on the 1st day and in the 1st week after treatment. Additionally, serum levels of circulating VEGF and PDGF for different time points were significantly different among patients who responded and did not respond to treatment. Similarly, Rosenbaum et al. (13) found a significant increase in serum VEGF, HGF and Ang-2 levels after TARE in 42 CRCLM patients. Carpizo et al. (9) also reported an increase >50% over the baseline in serum angiogenic factor levels in patients who received TARE for HCC and CRCLMs. Consideration of the results of these three studies reveals that an angiogenic response after TARE is observed in at least one group of patients, and it seems to be related to treatment response. Antiangiogenic treatment combinations might be a valuable option for these patients. Antiangiogenic treatment may help prevent early progression by increasing oxygenation of the tumor via the normalization of the blood supply. In three large prospective trials, TARE was combined with antiangiogenic treatments in subgroups of patients (20,21). However, subgroup analysis of patients who received or did not receive bevacizumab has not yet been reported. Moreover, when considering the elevation of different angiogenic factor levels, multitarget agents might be more beneficial than bevacizumab.
Similar to our study, Carpizo et al. (9) evaluated the prognostic importance of circulating angiogenic factors in CRCLM patients and found that baseline cytokine levels in patients with OS <6 months differed significantly from those with longer survival. In our analysis, we did not find any difference between baseline angiogenic factor levels of patients with longer and shorter (<6 months) OS. In contrast to a previous report, we performed Kaplan-Meier analysis of patient groups based on the elevation of angiogenic factor levels after TARE. We observed that the elevation of serum bFGF and PDGF levels in the 1st week and in serum VEGF levels in the 6th week of treatment has a prognostic value in the prediction of OS after TARE. Moreover, we performed PFS analysis and found that the elevation of serum bFGF levels in the 1st week seemed to predict PFS after TARE.
Lastly, we analyzed the difference in baseline circulating angiogenic factor levels of patients with and without extrahepatic disease. Although the finding was not statistically significant, some of the baseline levels of circulating angiogenic factors were higher in patients with extrahepatic disease; this difference in baseline VEGF and bFGF levels was nearly significant. A small number of patients included in our analysis might account for the low significance; therefore, a larger patient population may improve the significance of these differences.
Study Limitations
A major limitation of our study was the relatively small number of patients included. Some calculated values that did not reach the significance level may have been proven to be significant if applied to data for a larger study population. Additionally, if the frequency of blood samples collected was higher, the trend of the angiogenic response depending on time might be demonstrated more precisely. We cannot reach the details of the previously given TACE procedures. compared with the TARE, TACE has significant hypoxic effects, especially if larger particles are used; furthermore, some professionals attempt to achieve complete arterial blockage for success. Therefore, previous procedures might have affected the baseline levels of angiogenic factor levels. Last, additional different angiogenic factors should be examined to allow for documentation of a wide profile of angiogenic factor changes following TARE.
Despite its limitations; differently from previous analyses, our study demonstrated a relationship between elevation of different serum angiogenic factor levels and overall and progression free survival times after TARE in patients with CRCLMs. Based on the results of our analysis, which contributes to the limited data in the literature, various circulating angiogenic factors seem to have prognostic importance for patients who receive TARE for CRCLMs. An early elevation of circulating angiogenic factor levels was found in most of the patients after treatment. Some of these elevations seem to be related to treatment response, OS and PFS. Future larger prospective studies would help clarify the relationship between angiogenic response and prognosis of patients with CRCLMs. Combined treatment with antiangiogenic agents and TARE might be a suitable option to improve patient outcomes in the future.
Conclusion
Some early increases in serum PDGF, bFGF and Ang-2 levels and increases in serum VEGF in the 6th week after TARE are related to a poor treatment response and short overall and progression-free survival times for patients with CRCLMs. If outcomes of our analyses would be supported with further studies, combined treatment options would be standardized to improve survival of patients with CRCLMs.
Footnotes
Ethics
Ethics Committee Approval: This prospective study was approved by the Ankara University Faculty of Medicine, Local Institutional Ethical Committee (decision number: 01-14-16).
Informed Consent: Written informed consent was obtained from all participants.
Peer-review: Externally peer-reviewed.
Authorship Contributions
Surgical and Medical Practices: İ.E.G., S.B., N.Ö.K., E.Ö., Concept: İ.E.G., Ç.S., N.Ö.K., S.B., Design: Ç.S., Data Collection or Processing: M.D., B.İ.E., Analysis or Interpretation: Ç.S., A.H.E., Literature Search: Ç.S., Writing: Ç.S., M.A.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The author declared that this study has received no financial support.
References
- 1.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 2.Silberhumer GR, Paty PB, Temple LK, Araujo RL, Denton B, Gonen M, Nash GM, Allen PJ, DeMatteo RP, Guillem J, Weiser MR, D’Angelica MI, Jarnagin WR, Wong DW, Fong Y. Simultaneous resection for rectal cancer with synchronous liver metastasis is a safe procedure. Am J Surg. 2015;209:935–942. doi: 10.1016/j.amjsurg.2014.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Cutsem E, Cervantes A, Adam R, Sobrero A, Van Krieken JH, Aderka D, Aranda Aguilar E, Bardelli A, Benson A, Bodoky G, Ciardiello F, D’Hoore A, Diaz-Rubio E, Douillard JY, Ducreux M, Falcone A, Grothey A, Gruenberger T, Haustermans K, Heinemann V, Hoff P, Köhne CH, Labianca R, Laurent-Puig P, Ma B, Maughan T, Muro K, Normanno N, Österlund P, Oyen WJ, Papamichael D, Pentheroudakis G, Pfeiffer P, Price TJ, Punt C, Ricke J, Roth A, Salazar R, Scheithauer W, Schmoll HJ, Tabernero J, Taïeb J, Tejpar S, Wasan H, Yoshino T, Zaanan A, Arnold D. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016;27:1386–1422. doi: 10.1093/annonc/mdw235. [DOI] [PubMed] [Google Scholar]
- 4.Tsitskari M, Filippiadis D, Kostantos C, Palialexis K, Zavridis P, Kelekis N, Brountzos E. The role of interventional oncology in the treatment of colorectal cancer liver metastases. Ann Gastroenterol. 2019;32:147–155. doi: 10.20524/aog.2018.0338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boas FE, Bodei L, Sofocleous CT. Radioembolization of colorectal liver metastases: indications, technique, and outcomes. J Nucl Med. 2017;58(Suppl 2):104S–111S. doi: 10.2967/jnumed.116.187229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gray B, Van Hazel G, Hope M, Burton M, Moroz P, Anderson J, Gebski V. Randomised trial of SIR-Spheres plus chemotherapy vs. chemotherapy alone for treating patients with liver metastases from primary large bowel cancer. Ann Oncol. 2001;12:1711–1720. doi: 10.1023/a:1013569329846. [DOI] [PubMed] [Google Scholar]
- 7.Hendlisz A, Van den Eynde M, Peeters M, Maleux G, Lambert B, Vannoote J, De Keukeleire K, Verslype C, Defreyne L, Van Cutsem E, Delatte P, Delaunoit T, Personeni N, Paesmans M, Van Laethem JL, Flamen P. Phase III trial comparing protracted intravenous fluorouracil infusion alone or with Yttrium-90 resin microspheres radioembolization for liver-limited metastatic colorectal cancer refractory to standard chemotherapy. J Clin Oncol. 2010;28:3687–3694. doi: 10.1200/JCO.2010.28.5643. [DOI] [PubMed] [Google Scholar]
- 8.Van Hazel G, Blackwell A, Anderson J, Price D, Moroz P, Bower G, Cardaci G, Gray B. Randomised phase 2 trial of SIR-Spheres plus fluorouracil/leucovorin chemotherapy versus fluorouracil/leucovorin chemotherapy alone in advanced colorectal cancer. J Surg Oncol. 2004;88:78–85. doi: 10.1002/jso.20141. [DOI] [PubMed] [Google Scholar]
- 9.Carpizo DR, Gensure RH, Yu X, Gendel VM, Greene SJ, Moore DF, Jabbour SK, Nosher JL. Pilot study of angiogenic response to yttrium-90 radioembolization with resin microspheres. J Vasc Interv Radiol. 2014;25:297–306.e1. doi: 10.1016/j.jvir.2013.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gorski DH, Beckett MA, Jaskowiak NT, Calvin DP, Mauceri HJ, Salloum RM, Seetharam S, Koons A, Hari DM, Kufe DW, Weichselbaum RR. Blockage of the vascular endothelial growth factor stress response increases the antitumor effects of ionizing radiation. Cancer Res. 1999;59:3374–3378. [PubMed] [Google Scholar]
- 11.Korse CM, Bonfrer JM, Prevoo W, Baas P, Taal BG. Increase of angiogenic growth factors after hepatic artery embolization in patients with neuroendocrine tumours. Tumour Biol. 2011;32:647–652. doi: 10.1007/s13277-011-0164-7. [DOI] [PubMed] [Google Scholar]
- 12.Lewandowski RJ, Andreoli JM, Hickey R, Kallini JR, Gabr A, Baker T, Kircher S, Salem R, Kulik L. Angiogenic response following radioembolization: results from a randomized pilot study of Yttrium-90 with or without sorafenib. J Vasc Interv Radiol. 2016;27:1329–1336. doi: 10.1016/j.jvir.2016.03.043. [DOI] [PubMed] [Google Scholar]
- 13.Rosenbaum CE, van den Hoven AF, Braat MN, Koopman M, Lam MG, Zonnenberg BA, Verkooijen HM, van den Bosch MA. Yttrium-90 radioembolization for colorectal cancer liver metastases: a prospective cohort study on circulating angiogenic factors and treatment response. EJNMMI Res. 2016;6:92. doi: 10.1186/s13550-016-0236-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alsultan AA, Barentsz MW, Smits MLJ, Koopman M, Lam MGEH, Rosenbaum CENM. Angiogenesis in 90Y-radioembolization of colorectal liver metastases. Semin Nucl Med. 2019;49:204–210. doi: 10.1053/j.semnuclmed.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 15.Sergio A, Cristofori C, Cardin R, Pivetta G, Ragazzi R, Baldan A, Girardi L, Cillo U, Burra P, Giacomin A, Farinati F. Transcatheter arterial chemoembolization (TACE) in hepatocellular carcinoma (HCC): the role of angiogenesis and invasiveness. Am J Gastroenterol. 2008;103:914–921. doi: 10.1111/j.1572-0241.2007.01712.x. [DOI] [PubMed] [Google Scholar]
- 16.Shim JH, Park JW, Kim JH, An M, Kong SY, Nam BH, Choi JI, Kim HB, Lee WJ, Kim CM. Association between increment of serum VEGF level and prognosis after transcatheter arterial chemoembolization in hepatocellular carcinoma patients. Cancer Sci. 2008;99:2037–2044. doi: 10.1111/j.1349-7006.2008.00909.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li X, Feng GS, Zheng CS, Zhuo CK, Liu X. Expression of plasma vascular endothelial growth factor in patients with hepatocellular carcinoma and effect of transcatheter arterial chemoembolization therapy on plasma vascular endothelial growth factor level. World J Gastroenterol. 2004;10:2878–2882. doi: 10.3748/wjg.v10.i19.2878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suzuki H, Mori M, Kawaguchi C, Adachi M, Miura S, Ishii H. Serum vascular endothelial growth factor in the course of transcatheter arterial embolization of hepatocellular carcinoma. Int J Oncol. 1999;14:1087–1090. doi: 10.3892/ijo.14.6.1087. [DOI] [PubMed] [Google Scholar]
- 19.Rahbari NN, Reissfelder C, Mühlbayer M, Weidmann K, Kahlert C, Büchler MW, Weitz J, Koch M. Correlation of circulating angiogenic factors with circulating tumor cells and disease recurrence in patients undergoing curative resection for colorectal liver metastases. Ann Surg Oncol. 2011;18:2182–2191. doi: 10.1245/s10434-011-1761-9. [DOI] [PubMed] [Google Scholar]
- 20.van Hazel GA, Heinemann V, Sharma NK, Findlay MP, Ricke J, Peeters M, Perez D, Robinson BA, Strickland AH, Ferguson T, Rodríguez J, Kröning H, Wolf I, Ganju V, Walpole E, Boucher E, Tichler T, Shacham-Shmueli E, Powell A, Eliadis P, Isaacs R, Price D, Moeslein F, Taieb J, Bower G, Gebski V, Van Buskirk M, Cade DN, Thurston K, Gibbs P. SIRFLOX: Randomized phase III trial comparing first-line mFOLFOX6 (plus or minus bevacizumab) versus mFOLFOX6 (plus or minus bevacizumab) plus selective internal radiation therapy in patients with metastatic colorectal cancer. J Clin Oncol. 2016;34:1723–1731. doi: 10.1200/JCO.2015.66.1181. [DOI] [PubMed] [Google Scholar]
- 21.Wasan HS, Gibbs P, Sharma NK, Taieb J, Heinemann V, Ricke J, Peeters M, Findlay M, Weaver A, Mills J, Wilson C, Adams R, Francis A, Moschandreas J, Virdee PS, Dutton P, Love S, Gebski V, Gray A; FOXFIRE trial investigators; SIRFLOX trial investigators; FOXFIRE-Global trial investigators, van Hazel G, Sharma RA. First-line selective internal radiotherapy plus chemotherapy versus chemotherapy alone in patients with liver metastases from colorectal cancer (FOXFIRE, SIRFLOX, and FOXFIRE-Global): a combined analysis of three multicentre, randomised, phase 3 trials. Lancet Oncol. 2017;18:1159–1171. doi: 10.1016/S1470-2045(17)30457-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


