Abstract
Introduction
Laparoscopy is used in as many as 95% of adult appendicectomies. There is level I evidence showing that it reduces wound infection, postoperative ileus and length of inpatient stay in children compared with the open approach. The aim of this study was to report the uptake of laparoscopy for paediatric appendicectomy in England and to determine whether this was similar for general surgeons (GS) and specialist paediatric surgeons (SPS).
Methods
Hospital Episode Statistics data were obtained for all children aged <16 years who had an OPCS 4.6 code for emergency appendicectomy from 1997 to 2015 (18 years). Data are analysed to compare rate of laparoscopic vs open procedures for GS and SPS over time and to investigate factors associated with the use of laparoscopy.
Results
There were 196,987 appendicectomies and where specialty was available, 133,709 (79%) cases were undertaken by GS and 35,141 (21%) by SPS. The rate of cases undertaken with laparoscopy for both specialties combined increased from 0.8% in 1998 to 50% in 2014 (p<0.0001). In 2014, this rate was 41% for GS compared with 71% for SPS (p<0.0001). Female gender (odds ratio (OR)=1.84, 95% confidence interval (CI) 1.80–1.90), increasing age (OR=1.18, 95% CI 1.18–1.19 per year) and treatment by SPS (OR=3.71, 95% CI 3.60–3.82) were all factors positively associated with use of laparoscopy in multivariate analysis.
Conclusions
There has been a vast increase in the proportion of appendicectomies undertaken laparoscopically in children. Despite adjusting for patient factors, laparoscopy was used significantly less by GS when compared with SPS. This difference is most apparent in younger children.
Keywords: Appendicitis, Laparoscopy, Paediatric surgery, Outcomes
Introduction
In the United Kingdom (UK) paediatric appendicitis is managed by both general surgeons (GS) and specialist paediatric surgeons (SPS) but in practice transfer to a tertiary paediatric surgical centre is common in younger children owing to anaesthetic limitations outside a specialist centre.1 Conventional treatment for appendicitis in children consists of appendicectomy via an open or laparoscopic approach. Meta-analyses have shown that the laparoscopic approach is superior in children with reduced inpatient stay, postoperative ileus and wound infection rate.2 In adult appendicitis, laparoscopy has long been adopted with some studies reporting completion of up to 95% of appendicectomies via this approach.3 A previous study of paediatric appendicectomy in a selection of centres during a short time frame indicated that laparoscopy is utilised more by SPS than GS but it is unclear whether this holds true nationally or whether patient age is contributory.4
The aim of this study was to report the use of laparoscopy in paediatric appendicectomy over time and to determine whether there is a difference in approach when comparing GS with SPS and when taking into account other patient factors such as age and gender.
Methods
Data collection and case identification
Hospital Episode Statistics (HES) data were obtained from National Health Service (NHS) Digital to include an 18-year period from April 1997 to April 2015, for all patients aged less than 16 years. This included all hospital admissions for any child who had an appendicectomy in England except for those undertaken by private providers. The Royal College of Surgeons of England commissioning guide for paediatric emergency appendicectomy was used to identify codes for emergency appendicectomy using established and accepted methodology.1,5 This consisted of using the Office of Population, Census and Surveys – Classification of surgical operations and procedures, 4th revision (OPCS 4.6) code of H01 (emergency excision of appendix) without reference to the (International Classification of Disease 10th edition (ICD-10)) code or H02 (other excision of appendix) or H03 (other operations on appendix) with a ICD-10 code of R10, K35, K36, K37 or K38 (see Appendix 1 for more detail). Cases were excluded if they did not meet this strict criteria or were above 16 years of age on hospital admission. Laparoscopic procedures were identified with the addition of OPCS code of Y75 on the same day as the OPCS code of appendicectomy.
Specialty coding
Specialties were identified in the HES database using specialty codes ‘100’ for GS and ‘171’ for SPS. Where specialty was neither of these codes it was considered as missing. To test the impact of missing specialty data on results, a sensitivity analysis was carried out. This took all children with missing specialty and placed them first in the GS group and then in the SPS group, with results in each scenario reported.
Outcomes
The main outcome of interest was the proportion of all appendicectomies performed laparoscopically by each specialty of surgeon. Secondary outcomes were variations in the proportion of laparoscopic appendicectomy over time and across age groups. Finally, we identified which factors were associated with a laparoscopic (as opposed to open) approach.
Ethical approval
Approval to access and use HES data for this study was obtained during the application process to NHS Digital. Ethical approval was not required because this study uses existing data which is fully anonymised.
Statistical analysis
Statistical analysis was undertaken using StataSE v.15 (StataCorp LLC, College Station, TX, USA). Chi-squared was used for categorical data (2×2 analysis) and Mann–Whitney U-test was used for non-parametric continuous data. Chi-squared for trend was used to compare number of cases undertaken over time. Data are reported as median with interquartile range, or number with percentage, as appropriate. Multivariate logistic regression was used to identify the relative contribution of age, gender and treating specialty as factors associated with a laparoscopic approach. First, this was undertaken using the whole data set and second, using cases from the year 2013 onwards in children aged 5 years or older, to focus on contemporary data which represent a caseload common to GS and SPS. A p-value of <0.05 was considered significant. Graphs have been created using GraphPad Prism v.8 (GraphPad Software, La Jolla, CA, USA).
Results
Case demographics
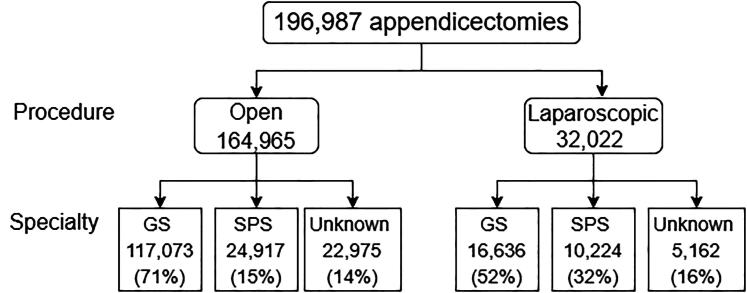
During the 18-year study period, there were 196,987 appendicectomies in children aged less than 16 years for suspected acute appendicitis. Appendix 1 details number of cases identified using each OPCS code and ICD-10 code if the OPCS code was H02 or H03. The median age was 11 (9–14) years and 110,153 (56%) children were male. Where specialty was available (n=168,850; 86%), 133,709 (79%) cases were undertaken by GS and 35,141 (21%) by SPS (Figure 1).
Figure 1 .
Flow chart of children included in the study showing operative technique and specialty of treating surgeon. GS = general surgeons; SPS = specialist paediatric surgeons.
Laparoscopy uptake
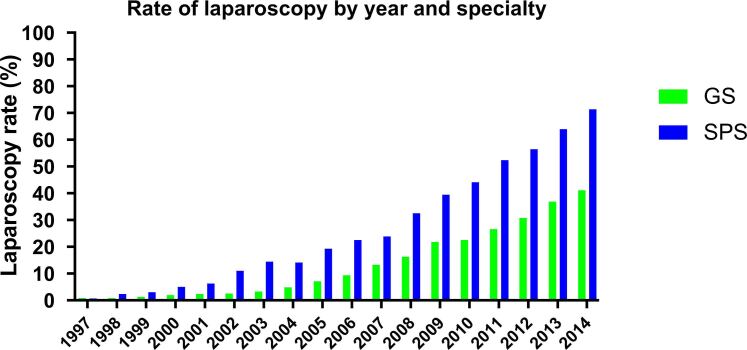
In total, 32,022 (16%) cases were performed with laparoscopy over the whole study period. The rate of cases undertaken with laparoscopy for both specialties increased from 0.8% in 1998 to 50% in 2014 (p<0.0001). Females were more likely to have a laparoscopic procedure than males (18,180 vs 13,839, 57% vs 43%; p<0.001). Overall, across both genders, in the most recent complete year of data, 41% of cases were undertaken using laparoscopy by GS compared with 71% of cases undertaken by SPS (p<0.0001) (Figure 2).
Figure 2 .
Rate of all appendicectomies undertaken with laparoscopy by both general surgeons (GS) and specialist paediatric surgeons (SPS) from 1997 to 2014.
A sensitivity analysis was undertaken to determine whether these findings hold true with re-classification of children with missing specialty coding (n=28,137). The specialty codes other than those for GS or SPS present in the data set are shown in Appendix 1. When these children with missing specialty were included in the GS group or SPS group, there was still a statistically significant difference between the two groups of children when comparing rate of laparoscopic cases overtime (Supplementary Table 1).
Age
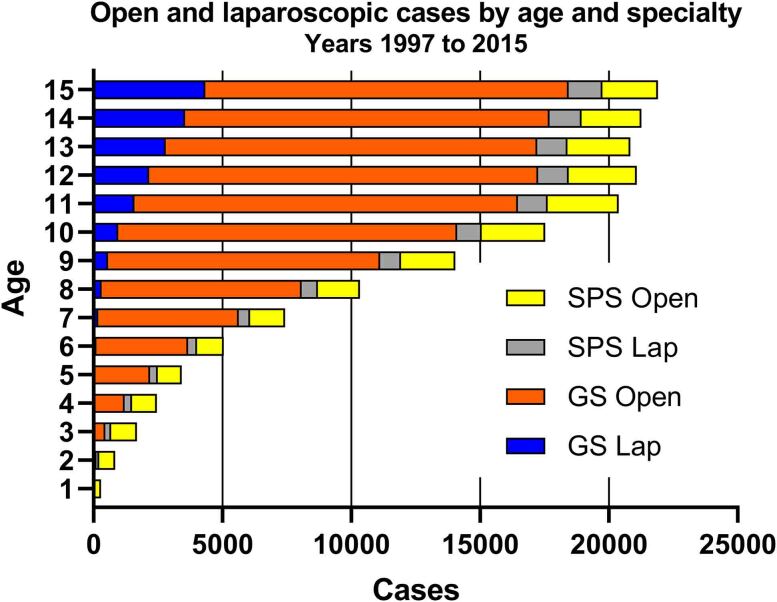
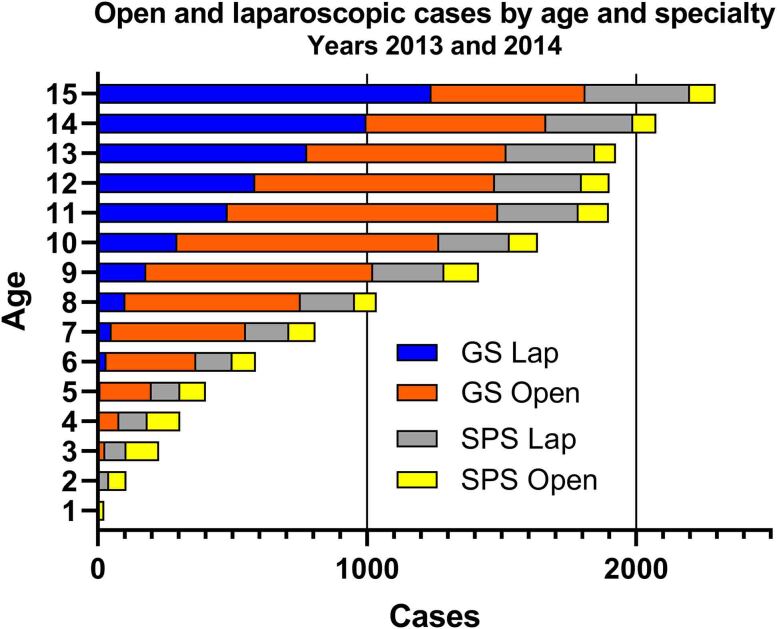
The median age of a child at appendicectomy via a laparoscopic procedure was higher than for an open procedure (13 (11–14) vs 11 (9–13) years; p<0.001). The number of cases undertaken open and with laparoscopy by child age across the whole study period is shown in Figure 3 and separated by specialty. We focused on the two most recent complete years of data, 2013 and 2014, to explore whether age was associated with use of laparoscopy in both specialties (Figure 4). In younger children (aged 2–10 years), 680/4,275 (16%) cases undertaken by a GS were performed laparoscopically compared with 1,350/2,276 (59%) of cases undertaken by SPS (p<0.0001). In children aged 11–15 years, the laparoscopy rate was also lower in GS compared with SPS (4,084/7,959 (51%) vs 1,664/2,140 (77%); p<0.0001). The median age of a child at appendicectomy by GS was higher than SPS (12 (10–14) vs 11 (8–13) years; p<0.001).
Figure 3 .
Number of appendicectomies undertaken using open and laparoscopic approach by general surgeons (GS) and specialist paediatric surgeons (SPS) by age of child from 1997 to 2015. Laparoscopic cases by GS are denoted as 'GS Lap', open cases by GS as 'GS Open', laparoscopic cases by SPS as 'SPS Lap' and open SPS cases as 'SPS Open'.
Figure 4 .
Number of appendicectomies undertaken using open and laparoscopic approach by general surgeons (GS) and specialist paediatric surgeons (SPS) by age of child in 2013 and 2014. Laparoscopic cases by GS are denoted as ‘GS Lap', open cases by GS as ‘GS Open', laparoscopic cases by SPS as ‘SPS Lap' and open SPS cases as ‘SPS Open'.
Multivariate analysis
A multivariate model was created to explore factors associated with a laparoscopic procedure. Surgeon specialty, age and gender were entered into the model. Across the whole period, surgeon specialty was the factor most closely associated with a laparoscopic procedure. Gender and age were also significantly associated in this model (Table 1). In a restricted data set (containing 17,805/196,987 (9%) children) for years 2013 and 2014, and children aged 5 years or more, all three of these variables were significantly associated with use of laparoscopy, again with specialty of treating surgeon carrying the strongest association (Table 1).
Table 1 .
Multivariate logistic regression analysis of factors associated with laparoscopy use
| Odds ratio (95% CI) | p-value | |
|---|---|---|
| All children | ||
| Female | 1.84 (1.80–1.90) | <0.001 |
| Increase in age per year | 1.18 (1.18–1.19) | <0.001 |
| Specialist paediatric surgeon | 3.71 (3.60–3.82) | <0.001 |
| Years 2013 onwards and age 5 years or more only | ||
| Female | 2.11 (1.97–2.26) | <0.001 |
| Increase in age per year | 1.34 (1.33–1.36) | <0.001 |
| Specialist paediatric surgeon | 6.62 (6.07–7.22) | <0.001 |
Odds ratios are compared with a reference group who are male with appendicectomy undertaken by GS. To focus on contemporary data that represent a caseload common to GS and SPS the lower part of Table 1 includes only cases from 2013 onwards aged 5 years or older.
Discussion
In this study of national trends in use of laparoscopy for paediatric appendicectomy over an 18-year period, we found that the overall rate of laparoscopic appendicectomy has increased year on year. We also found that patient age and gender were significantly associated with surgical approach and that SPS used laparoscopy significantly more frequently than GS in children (even adjusting for age and gender). The gap between the two specialties was largest in the group of children aged 2–10 years, where the rate of laparoscopy was four times greater in the SPS group compared with GS. When focusing on children aged more than 5 years, from 2013 to 2015 (representing the most recent data), the odds of having a laparoscopic procedure were more than six times greater if surgery was undertaken by a SPS.
Laparoscopy was first introduced for appendicectomy in 1983 and numerous studies have compared laparoscopic and open procedures in children. Meta-analysis including a Cochrane review found convincing evidence of benefit with laparoscopy including reduced incidence of wound infection, reduced postoperative ileus and shorter inpatient stay using laparoscopy in children.2,6 A recent survey of European SPS identified that laparoscopy is the preferred surgical approach for both simple (89%) and perforated appendicitis (81%).7 The benefits may be even greater for complicated appendicitis with meta-analysis showing that laparoscopy is associated with shorter inpatient stay, reduced wound infection incidence, lower rates of readmission and postoperative ileus, as well as lower rates of reoperation.8 Despite this, it is clear that some are not yet convinced by the literature which may be due to the scarcity of high-quality randomised prospective studies on this topic. In a 2018 survey of Irish surgical practice, 71% felt that there is no advantage of laparoscopic appendicectomy other than improved cosmesis.9
The implementation of laparoscopy for paediatric appendicectomy has been reported in both the USA and Canada over a similar time frame10–12 and largely follows a similar pattern to that reported here. In a Canadian10 population-based data set also using administrative data, the rate of laparoscopy increased from 29% in 2004 to 66% in 2010. This is similar to a national report from the USA12 showing an increased rate from 41% in 2004 to 73% in 2011. Uptake of laparoscopy for appendicectomy was more rapid in North America than in England because even in 2014 the laparoscopic rate in England had only reached 50% in our study.
In England, children with appendicitis may be treated by either GS or SPS, dependent in part on which hospital they present to, but also on their age and the availability of local expertise. It is commonplace for children less than 5 years old presenting to a district general hospital to be transferred to a specialist paediatric surgical centre for surgery.13 Our data reflect this in that the median age of child treated by SPS is lower than that treated by GS. However, age alone does not fully account for the differing use of laparoscopy by GS and SPS in children. In children of all ages, laparoscopy is more common in girls and also in children treated by SPS. Laparoscopy may be used more commonly in girls due to the possibility of an alternative diagnosis as previous study has shown that normal appendicectomy is more likely in girls than boys.4
Although there was wide uptake of laparoscopy in general by GS in the last decades of the 21st century, SPS were much slower to learn these skills.14 Conversely, for appendicectomy in children, SPS are more likely than GS to perform the procedure laparoscopically. These data suggest that either GS believe there is no clear benefit to laparoscopic appendicectomy in most ages of children or there are barriers to its implementation. If the former was true, we may expect the data to show a clear age cut-off below which laparoscopy is not used, rather than the observed gradual increase in use with increasing age. Barriers to more widespread use of laparoscopy by GS may include GS unfamiliarity working in small abdomens compared with the adult patients who dominate their practice, resistance from anaesthetists to undertake laparoscopy in children outside specialist centres, and the extent of consultant presence during appendicectomy. Regarding patient size, we note that even among 11–13 year olds, who are much closer in size and weight to adult patients, laparoscopy was used in fewer than half of all cases by GS. Previous work has shown that SPS consultants are more likely to be present in theatre compared with GS consultants for paediatric appendicectomies, which may be another factor responsible for the difference in laparoscopy utilisation although we do not have data to investigate this association in the current study.4 Surprisingly, a recent Irish study showed large variation of laparoscopy use in appendicectomy depending on which county the child was treated in but with overall rates comparable with England.15 There may be centre-to-centre variation within England too although we are unable to explore this further in the current study.
Strengths and limitations
This study had the benefit of reporting a large number of cases from an entire population but is limited by use of administrative data that includes the ability to correctly identify cases based on clinical coding. There is also the risk that some laparoscopic procedures were coded as open procedures if the laparoscopic OPCS code (Y75) was missing; however, previous studies using HES data have used this method of identifying laparoscopic procedures.1,16 It is also a possibility that the rate of laparoscopy has increased as HES coding has improved; however, rates reported in this study are similar to other studies using different methodology.4 In addition, we focused solely on reporting practice rather than outcomes given the large amount of existing evidence and the limitations of HES to accurately report outcomes that do not require repeat surgery.
Conclusion
This work has shown a significant difference in laparoscopy use in paediatric appendicectomy between GS and SPS. In addition, it is clear that in England our overall figures are lower than those reported in the USA and Canada, although similar to Ireland. Further work is needed to clearly define barriers to the use of laparoscopy by GS and to determine whether further robust research is needed to determine whether outcomes are better with either technique. In the short term, the use of paediatric surgical networks regionally may be able to offer training to support both GS consultants and trainees.
Funding
The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. George Bethell is funded by the National Institute of Health Research Academic Clinical Fellow programme. The fee for obtaining the data from NHS Digital was funded by the University of Southampton.
References
- 1.Giuliani S, Cecil EV, Apelt Net al. Pediatric emergency appendectomy and 30-day postoperative outcomes in district general hospitals and specialist pediatric surgical centers in England, April 2001 to March 2012: retrospective cohort study. Ann Surg 2016; 263: 184–190. [DOI] [PubMed] [Google Scholar]
- 2.Aziz O, Athanasiou T, Tekkis PPet al. Laparoscopic versus open appendectomy in children: a meta-analysis. Ann Surg 2006; 243: 17–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Collaborative RSGobotWMR. Evaluation of appendicitis risk prediction models in adults with suspected appendicitis. Br J Surg 2020; 107: 73–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tiboni S, Bhangu A, Hall NJ, Collaborative PSTRNatNSR. Outcome of appendicectomy in children performed in paediatric surgery units compared with general surgery units. Br J Surg 2014; 101: 707–714. [DOI] [PubMed] [Google Scholar]
- 5.Royal College of Surgeons of England. Commissioning guide: paediatric emergency appendicectomy. rcseng.ac.uk/library-and-publications/rcs-publications/docs/paediatric-emergency-appendicectomy/ (cited February 2021).
- 6.Jaschinski T, Mosch CG, Eikermann Met al. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev 2018; 11: CD001546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zani A, Hall NJ, Rahman Aet al. European paediatric surgeons’ association survey on the management of pediatric appendicitis. Eur J Pediatr Surg 2019; 29: 53–61. [DOI] [PubMed] [Google Scholar]
- 8.Low ZX, Bonney GK, So JBYet al. Laparoscopic versus open appendectomy in pediatric patients with complicated appendicitis: a meta-analysis. Surg Endosc 2019; 33: 4066–4077. [DOI] [PubMed] [Google Scholar]
- 9.Bhatt NR, Dunne E, Faraz Met al. Trends in the Use of laparoscopic versus open paediatric appendicectomy: A regional 12-year study and a national survey. World J Surg 2018; 42: 3792–3802. [DOI] [PubMed] [Google Scholar]
- 10.Cheong LH, Emil S. Pediatric laparoscopic appendectomy: a population-based study of trends, associations, and outcomes. J Pediatr Surg 2014; 49: 1714–1718. [DOI] [PubMed] [Google Scholar]
- 11.Sattarova V, Eaton S, Hall NJet al. Laparoscopy in pediatric surgery: implementation in Canada and supporting evidence. J Pediatr Surg 2016; 51: 822–827. [DOI] [PubMed] [Google Scholar]
- 12.Masoomi H, Nguyen NT, Dolich MOet al. Laparoscopic appendectomy trends and outcomes in the United States: data from the nationwide inpatient sample (NIS), 2004-2011. Am Surg 2014; 80: 1074–1077. [PubMed] [Google Scholar]
- 13.Pye JK, AoSoGBa I. Survey of general paediatric surgery provision in England, Wales and Northern Ireland. Ann R Coll Surg Engl 2008; 90: 193–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gilchrist BF, Lobe TE, Schropp KPet al. Is there a role for laparoscopic appendectomy in pediatric surgery? J Pediatr Surg 1992; 27: 209–212; discussion 12-4. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed O, Mealy K, Sorensen J. Exploring geographic variation in acute appendectomy in Ireland: results from a national registry study. BMJ Open 2019; 9: e025231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wiggins T, Markar SR, MacKenzie Het al. Optimum timing of emergency cholecystectomy for acute cholecystitis in England: population-based cohort study. Surg Endosc 2019; 33: 2495–2502. [DOI] [PMC free article] [PubMed] [Google Scholar]