Abstract
Complementary and alternative medicine (CAM) encompasses a wide range of different non-mainstream therapies that have been increasingly used for the treatment or adjunct treatment of various ailments, with premature ovarian failure (POF) being one of the most common conditions treated with CAM. This review updates the progress of CAM in the treatment of POF, and we focus specifically on reviewing the evidence for the efficacy and mechanisms of a range of CAM treatments in POF, including single herbal medicines and their active ingredients, compound Chinese medicines, acupuncture and moxibustion, psychotherapy, exercise, vitamins, massage, and dietary supplements. According to the literature, CAM is very helpful for improving POF symptoms, and we hope to provide some instructive suggestions for clinical treatment and experimental research in the future. However, more clinical trials are needed to prove the safety of CAM.
1. Introduction
Premature ovarian failure (POF) is a common endocrine disease leading to female amenorrhea and infertility. It is characterized by high expression of gonadotropin (follicle-stimulating hormone (FSH) ≥ 40 mIU/ml), low expression of estradiol (E2), and poor follicular development in women under 40 years old. Clinical symptoms are also accompanied by perimenopausal symptoms such as hot flashes, sweating, mood swings, sleep disorders, and low sexual desire [1–3]. At present, it is considered that the occurrence and development of POF are closely related to gonadotropin-related disorders [4], immune factors [5, 6], infectious factors [7, 8], iatrogenic factors [9], lack of metabolism-related enzymes [10], environmental factors [11], socio-psychological factors [12], and genetic factors [13] (Figure 1). The incidence of POF is about 1.0% globally, while in China, it is 1%–3.8%. Primary amenorrhea accounts for 20%–28% of POF cases, secondary amenorrhea accounts for about 4%–20% of cases, and about 74%–90% of POF cases have unknown etiology. The incidence of POF has been increasing in recent years with the development of the economy, changes in social relationships, and unhealthy lifestyles [14–16].
Figure 1.
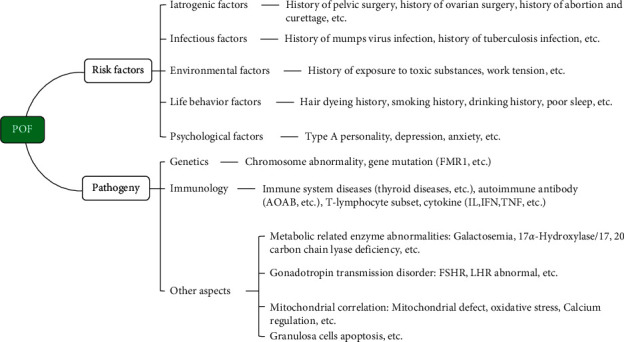
Risk factors and etiology of POF.
At present, the most common clinical treatment for POF is still hormone replacement therapy (HRT), but other therapies include in vitro activation, stem cell therapy, tissue engineering, and regenerative medicine. HRT is considered to reduce the risk of infection, osteoporosis, cardiovascular disease, and urogenital atrophy and improve the quality of life of women with POF. However, HRT does not fully restore ovarian function, and some studies have reported that HRT is a predisposing factor for breast cancer [17]. Therefore, clinicians are still looking for a new method to treat POF through complementary and alternative medicine (CAM). CAM is usually defined as “non-traditional” medicine according to the recommendations of the National Center for Comprehensive and Integrative Health (NCCIH). If unconventional methods or products are used together with conventional drugs, it is called complementary medicine, and if an unconventional method is used instead of standard treatment, it is considered an alternative method [18]. CAM includes many products and medical practices that are not conventional therapies in western countries, including not only traditional medicines and folk therapies, but also many new therapies that cannot be covered by medical insurance, such as traditional Chinese medicine (TCM; including Chinese herbal medicine, acupuncture, qigong, etc.), Indian medicine, medicinal food, health food, aromatherapy, vitamin therapy, dietary therapy, psychotherapy, spa therapy, and oxygen therapy [19, 20]. CAM is favored by many countries and nationalities because of its natural ingredients and methods, its convenience, and its low costs. It is also an effective strategy to alleviate the pain related to many diseases. Reports have suggested that the rate of CAM application has reached 9.8%–76.0% globally and that roughly 40% of adults use at least one type of CAM to treat a wide range of conditions in the USA [21, 22]. This article updates the progress in the research and application of CAM in the treatment of POF.
2. Single Herbal Medicines and Their Active Ingredients
Chinese herbal medicines have excellent efficacy in the treatment of POF, and many compound Chinese medicines have been widely used in the clinical treatment of POF due to their many advantages. Single herbal medicines are the basis for the research into compound Chinese medicines, and some of their active ingredients provide indications for the use of different Chinese herbal medicines in the treatment of POF. Current studies have found that the potential mechanisms of single herbal medicines and their active ingredients include estrogen-like effects, promoting DNA damage repair, enhancing anti-inflammatory and antioxidant capacity, regulating the expression of related pathways and proteins, and affecting prostaglandin biosynthesis, apoptosis, aging-associated, autophagy, etc., to delay POF.
2.1. Epimedium and Icariin
Epimedium, a representative of Chinese herbal medicines, has the ability to tonify the kidney and is commonly used to treat female infertility, irregular menstruation, amenorrhea, POF, and other diseases. One of the main active ingredients of Epimedium is icariin. Studies have shown that icariin has an obvious estrogen-like effect that can significantly increase the uterine coefficient, endometrial epithelial thickness, and serum E2 levels in ovariectomized mice [23]. In a rat model of POF, icariin could significantly increase the serum level of anti-Müllerian hormone (AMH), possibly by promoting the secretion of AMH in ovarian granulosa cells (GCs) and restoring normal follicular recruitment and maturation to maintain the ovarian reserve [24]. Li et al. found that icariin was effective in reducing ovarian damage by promoting DNA damage repair, suggesting that icariin might be used as a protective agent against POF [25].
2.2. Semen Cuscutae and TFSC/Cuscuta Flavonoids
Semen cuscutae is an important tonic for kidney yang and is commonly used in the treatment of gynecological diseases. Its main active chemical ingredient is Cuscuta flavonoids, which have significant effects on improving and enhancing the function of the human reproductive endocrine system. In a rat model of POF, total flavonoids from Semen cuscutae (TFSC) had a significant restorative effect on the estrous cycle and ovarian endocrine function and promoted follicular development and GCs proliferation in the ovary, indicating that they had estrogen-like effects [26]. Huang Changsheng believed that quercetin might be one of the main effective ingredients in Cuscuta flavonoids for the treatment of POF, and in a rat model of POF, both Cuscuta flavonoids and quercetin alone could inhibit the process of POF through activation of the phosphatidylinositol 3-kinase (PI3K)/protein kinase B (Akt) signaling pathway [27, 28].
2.3. Pueraria Lobata and Puerarin
The main active ingredients in Pueraria lobata are isoflavones and compound isoflavones. Puerarin is a 4,7-dihydroxy-8-β-D-glucosyl isoflavone and is the most important active ingredient of Pueraria lobata, and it has different degrees of estrogen-like effects [29]. Bcl-2-associated X protein (Bax) and B-cell lymphoma 2 (Bcl-2) play important roles in the anti-apoptotic effect in the Bcl-2 family, and Zhang et al. [30] found that puerarin could regulate the activity of Bax and Bcl-2 and inhibit apoptosis in ovarian tissue in a mouse model of POF and thus restore ovarian function. The expression of mouse vasa homolog (Mvh) and octamer-binding transcription factor 4 (OCT4) maintain the activity of female germline stem cells, and Chen et al. [31] found that puerarin not only activated the Wnt/β-catenin signaling pathway but also increased the expression of the antioxidant factors superoxide dismutase 2 (SOD2) and nuclear factor erythroid 2-related factor (Nrf2) to reduce oxidative stress.
2.4. Ginseng and Rg1
Ginseng is a traditional anti-aging drug, and its active ingredients are mainly composed of ginsenosides. The ginsenosides can be divided into three categories, namely ginseng diols (e.g., Rb1, Rb2, Rc, Rd, F2, etc.), ginseng triols (e.g., Re, Rg1, Rg2, Rf, Rh1, etc.), and pentacyclic triterpenoid saponins such as Ro [32]. The p16 and p53–p21–p19 pathways play an important role in the aging process, and Rg1 not only upregulates the expression of follicle-stimulating hormone receptor (FSHR) in the GCs of POF mice but also downregulates aging-associated proteins in the p19–p53–p21–p16 pathway and enhances the anti-aging capacity and fertility of POF mice by improving the anti-inflammatory and antioxidant capacity of the ovary [33]. Another experiment has shown that Rg1 effectively regulates the physiological status of the ovary, induces the expression of light-chain 3 (LC3)-II to increase autophagy levels, and may delay POF by activating the PI3K/Akt/mammalian target of rapamycin (mTOR) autophagy pathway [34].
2.5. Other Single Herbal Medicines
Hematopoietic prostaglandin D synthase (HPGDS), phospholipase A2-IVA (PLA2G4A), and prostaglandin-endoperoxide synthase 1 (PTGS1) are involved in prostaglandin biosynthesis in the body, and American ginseng affects the transformation of prostaglandin H2 (PGH2) into prostaglandin D2 (PGD2) by downregulating the expression of HPGDS and PTGS1 in the ovary and thus participates in the regulation of the reproductive system [35]. Animal models have shown that American ginseng plays a role in regulating prostaglandin biosynthesis, promoting ovulation, and preventing ovarian aging, which expands our understanding of the pharmacological activity of American ginseng as an anti-POF drug [36]. The expression of PLA2G4A is positively correlated with POF, while the expression levels of pregnancy-associated plasma protein-A, stanniocalcin-2, C-C motif chemokine ligand 2, and NEL-like protein 1 are negatively correlated with POF, and Ge et al. [37] confirmed in animal models that American ginseng can prevent and alleviate POF in rats by altering the expression levels of POF-related genes in ovarian tissues. These studies indicate that American ginseng is a potential clinical treatment for the prevention of POF.
The preparation made from Cistanche formulas can improve the clinical symptoms of menopausal syndrome, and follicle-promoting and luteinizing effects of Cistanche can regulate the endocrine function of female mice with kidney deficiency. Experiments have shown that Cistanche polysaccharide significantly improves the endocrine regulatory mechanisms of the body and has an inhibitory effect on POF by affecting the expression of tumor necrosis factor-alpha (TNF-α), interferon-gamma (IFN-γ), and the apoptosis-related protein Bcl-2/Bax [38, 39].
Angelica is an important gynecological medicine commonly used in Chinese herbal preparations, and Angelica polysaccharide is the main active ingredient. Animal experiments have found that Angelica polysaccharide can increase the activity of SOD and inhibit the level of malondialdehyde in the blood of mice with POF and that it promotes both oxidative stress and antioxidant capacity through the Akt/Forkhead box subgroup O3 (FOXO3) pathway, thus providing a novel approach for the treatment of immune-related POF [40].
Lycium barbarum polysaccharides are one of the main ingredients isolated from Lycium barbarum, a characteristic plant in Ningxia. These polysaccharides regulate endocrine production and maintain ovarian function in mice by slowing down ovarian damage caused by anti-zona pellucida antibody, possibly through both direct actions on immunoreactive cells and indirect actions on the hypothalamic pathway [41].
A study showed that high-dose maca powder could restore ovarian function and the abnormal estrous cycle, and improve the ovarian index and serum reproductive hormone levels of POF rats with kidney yang deficiency syndrome and that it has certain conservation effects on the ovary [42]. Oyster polypeptide plays an anti-oxidative role through the SIRT1-FOXO3a-SOD2 axis and protects against POF by reducing apoptosis [43]. The effectiveness of single herbal medicines and their active ingredients in the treatment of POF is summarized in Table 1.
Table 1.
Summary of the curative effects of single herbal medicines in POF.
| Single herbal medicine | Active ingredients | Outcomes | References |
|---|---|---|---|
| Epimedium | Icariin | FSH, LH↓; E2, AMH↑. | [24, 25] |
| Semen cuscutae | TFSC/cuscuta flavonoids | TFSC processing: E2↑. Cuscuta flavonoids processing: FSH↓; E2, AMH↑. |
[26, 27] |
| Pueraria lobata | Puerarin | FSH↓; E2, AMH↑; Bcl-2↑; Bax, cleaved caspase-3↓; β-catenin, SOD2, Nrf2↑. | [30, 31] |
| Ginseng | Rg1 | FSH↓; E2, AMH↑; IL-1b, IL-6, TNF-α↓; aging-associated proteins in the p19-p53-p21-p16 pathway↓, LC3-II↑. | [33, 34] |
| American ginseng | / | FSH↓; E2↑; HPGDS, PLA2G4A, PTGS1↓; PAPPA, STC2, CCL2, NELL1↑. | [34–37] |
| Cistanche | / | FSH↓; E2, AMH↑; IFN-γ and TNF-α↓; Bcl-2↑; Bax↓; Bcl-2/Bax ratio↑. | [39] |
| Angelica | AP | SOD↑; MDA↓; IL-1β, IL-6↓. | [40] |
| Lycium barbarum | LBP | FSH↓; E2↑; serum anti-zona pellucida antibody↓. | [41] |
| Maca | / | FSH, LH↓; E2↑. | [42] |
| Oyster | Oyster polypeptide | FSH↓; P↑; P53, Bad↓. | [43] |
TFSC: total flavonoids from Semen cuscutae; AP: Angelica polysaccharide; LBP: Lycium barbarum polysaccharides. FSH: follicle-stimulating hormone; LH: luteinizing hormone; E2: estradiol; AMH: anti-Mullerian hormone; Bcl-2: B-cell lymphoma 2; Bax: Bcl-2-associated X protein; SOD2: superoxide dismutase 2; Nrf2: nuclear factor erythroid 2-related factor; IL-1b: interleukin-1b; IL-6: interleukin-6; TNF-α: tumor necrosis factor-alpha; LC3-II: light-chain 3 (LC3)-II; HPGDS: hematopoietic prostaglandin D synthase; PLA2G4A: phospholipase A2-IVA; PTGS1: prostaglandin-endoperoxide synthase 1; PAPPA: pregnancy-associated plasma protein A; STC2: stanniocalcin-2; CCL2 : C-C motif chemokine ligand 2; NELL1: NEL-like protein 1; IFN-γ: interferon-gamma; SOD: superoxide dismutase; MDA: malondialdehyde; IL-1β: interleukin-1beta.
3. Compound Chinese Medicines
Compound Chinese medicines are composed of two or more kinds of herbs that are boiled in water, and the residue is removed to obtain a clear liquid for Chinese medicine decoctions or is further processed into other dosage forms such as Chinese patent medicines, pills, powders, or creams [19]. Compound Chinese medicines have been used to treat diseases for thousands of years and have formed their own materia medica that is separate from traditional western medical practice. More and more studies have shown that compound Chinese medicines have overall advantages in the treatments of diseases due to their ability to simultaneously affect multiple targets and pathways, and this has attracted more and more attention in the treatment of POF compared with the efficacy and side effects of pharmaceutical drugs. Several studies have shown that compound Chinese medicines have a positive effect on POF, and the side effects are significantly less than for pharmaceutical drugs. Compounds extracted from Chinese herbal medicines can significantly reduce oxidative stress in the ovary and reduce apoptosis in ovarian GCs and oocytes. Thus, they play an important role in the treatment of POF by delaying apoptosis and regulating the secretory function of ovarian GCs and have significant advantages in increasing serum E2, reducing serum FSH levels, and improving clinical symptoms [44–47].
3.1. Chinese Medicine Decoctions
Chinese medicine decoctions, known in ancient times as “Tang Ye,” are important traditional preparations in TCM due to their ease of consumption, fast absorption, large drug load, and remarkable curative effect. The decoctions can be fully adapted to the needs of syndrome differentiation and treatment in TCM because of their flexibility, simplicity, low cost, quick effect, and the use of water as the solvent [48]. Chinese medicine decoctions that are commonly used in the clinical treatment of POF include Zuogui pill (ZGP), Bushen Huoxue decoction (BHD), Erxian decoction (EXD), and Yulin decoction.
3.1.1. ZGP
ZGP, from Jingyue Quanshu, is a classic prescription for nourishing yin and tonifying the kidney and is widely used in the treatment of POF. According to TCM, women are kidney-based and POF is responsible for kidney deficiency. By nourishing yin and tonifying the kidney, filling the lean marrow, improving perimenopausal symptoms of POF, correcting sexual hormone disorders, and promoting the recovery of ovarian function, ZGP can not only improve the curative effects of western medicine but can also reduce side effects caused by hormone drugs without any serious adverse events [49–51]. Zeng et al. [52] showed that after ZGP treatment female rats showed an increase in ovarian volume, the ratio of total ovarian weight to body weight, and serum AMH and E2 levels and a decrease in serum FSH levels. Peng et al. [53] established a control group, model group, three ZGP groups (high-dose, medium-dose, and low-dose), and a triptorelin group to study ZGP's inhibition of mitochondrial-dependent apoptosis of follicles in POF rats. They found that ZGP inhibited follicle loss after exposure to chemotherapeutic drugs and improved the estrous cycle in rats. Further mechanistic studies showed that the protective effect of ZGP is related to the inhibition of the activation of the mitochondrial-dependent apoptosis cascade at the gene and protein levels. By inhibiting the expression of the pro-apoptotic molecule Bax and increasing the expression of the anti-apoptotic molecule Bcl-2, ZGP can reduce the level of serum FSH and increase the level of serum E2. It has also been shown that ZGP upregulates the protein expression of growth differentiation factor-9 and its signal transduction protein Smad2 in POF mouse ovaries, and thus ZGP can promote the recruitment of primordial follicles, promote follicular development, and inhibit follicular atresia [54].
3.1.2. BHD
BHD [55–57] is a prescription developed by Professor Zhu Nansun, a master of Chinese medicine, and it exerts its therapeutic effects by tonifying the kidney and invigorating the blood, which benefits the kidney and fills the essence, fills the qi and blood, promotes blood circulation, and unblocks the collaterals to promote normal menstruation. Song et al. [58] verified the clinical efficacy of BHD in the treatment of POF patients by comparing the oral BHD group and the oral estradiol or estradiol dydrogesterone tablets group. Their results showed that BHD in the treatment of POF could significantly improve the TCM symptoms of patients—including hot flashes, night sweats, and other clinical manifestations—reduce the levels of serum FSH, mir-23a, and ovarian artery resistance index, and increase the level of AMH. Liu et al. [59] studied the effect of BHD on immune-related POF mice and found that compared with the model group, there was a significant increase in the number of mature ovarian follicles and a decrease in the number of atretic follicles in the high-dose group, medium-dose group, low-dose group, and estradiol valerate group of BHD, demonstrating that BHD can improve ovarian function by upregulating the protein expression of transforming growth factor-beta 1 (TGF-β1), transforming growth factor-beta receptor II (TGF-β RII), and Smad2/3 in GCs. BHD can promote normal levels of ovarian hormone secretion and promote the increase in mature follicles and the formation of primordial follicles and a large number of primary follicles through the upregulation of PI3K, Akt, and Bcl-2 protein expression in GCs [60].
3.1.3. EXD
EXD is derived from the clinical manual of TCM formulations, and it warms the kidney, fills the essence, and reconciles the Chong Ren. In recent years, clinical observations and research on EXD in the treatment of POF have shown that the decoction has a clear effect on POF [61, 62]. Studies have shown that EXD has an effect on serum inflammatory factors and related growth factors in a rat model of POF. Compared with the low EXD dose group and the medium EXD dose group, the high-dose group showed significantly decreased serum levels of TNF-α, IFN-γ, FSH, and LH, significantly increased protein expression of vascular endothelial growth factor and basic fibroblastic growth factor in ovarian tissue, and increased levels of E2, showing that EXD could improve the level of sex hormone in a rat model of POF and promote the recovery of ovarian function [63]. In another study [64], treating POF mice with EXD restored the ovarian cycle to near or above the normal ovarian index, brought serum E2, FSH, and LH levels close to normal, the increased the numbers of CD3+ T-cells, CD4+ T-cells, and the CD4+ T-cell/CD8+ T-cell ratio, decreased the number of CD8+ T-cells, and increased the expression of BMP15 and Akt.
3.1.4. Other TCM Decoctions
Based on the “liver and kidney theory” [65], Longjiang Han's Department of Gynecology applies Jiawei Yuyin decoction for tonifying the kidney and soothing the liver to provide symptomatic treatment for liver depression and kidney deficiency related to POF, and the patients' perimenopausal symptoms are significantly relieved and the serum levels of sex hormones return to normal. Modified mulberry decoction (MMD) has the effects of tonifying the liver and kidney, nourishing the blood and essence, and harmonizing Chong Ren. Wang et al. used estradiol valerate and cyproterone tablets as their control group and MMD as their treatment group. The results showed that the effective rate of the control group was 66.67% while that of the treatment group was 86.67%, and after treatment, the TCM syndrome scores and FSH and LH levels in the treatment group were lower than those in the control group and the E2 level was higher than in the control group. Their study showed that MMD could effectively improve the clinical symptoms of patients with POF, regulate the level of serum hormones, and promote menstrual regularity [66]. Modified Bazhen Decoction (MBD) [67] is effective in the treatment of POF. Professor Li [68] used the empirical formula “Yangshu Bazhen Decoction,” which was modified from the ancient formula “Bazhen decoction,” to treat POF by emphasizing the harmony of liver and kidney, paying attention to emotional treatment, balancing yin and yang, and regulating Chong Ren, which achieved good curative effects. In addition, Danggui Buxue decoction [69], Siwu decoction [70], Wenjing decoction [71], Bushen Jianpi formula [72], and other TCM decoctions have good effects in the treatment of POF, and these emphasize the flexible composition and good curative effect of TCM decoctions and fully demonstrate the theory of disease differentiation and treatment using TCM. The effect of TCM decoctions on POF is summarized in Table 2.
Table 2.
Summary of the curative effects of TCM decoctions on POF.
| Chinese medicine decoction | Ingredients | Sample size | Interventions | Model used | Outcomes | References |
|---|---|---|---|---|---|---|
| Zuogui pill (ZGP) | Rehmanniae radix praeparata, cornel, yam, semen cuscutae, Chinese wolfberry fruit, radix achyranthis bidentatae, colla carapacis et plastri testudinis, and antler gelatin | N = 114 | Control group, model group, low-ZGP group, high-ZGP group, low-dose estradiol valerate, high-dose estradiol valerate, DAPT group, and DAPT + low-ZGP group | SD rats | FSH↓; E2, AMH↑; ovarian volume↑; ratio of total ovary weight to body weight↑. | [52] |
|
| ||||||
| Bushen huoxue decoction (BHD) | Panax notoginseng powder, rhizoma cyperi, licorice, spatholobus suberectus stem, psoralea corylifolia, rhizoma curculiginis, semen cuscutae, cornel, angelica, epimedium, salvia miltiorrhiza, ligusticum wallichii, codonopsis pilosula, rehmanniae radix praeparata, and radix paeoniae alba. | N = 73 | BHD group and western medicine group (estradiol or estradiol didroxyprogesterone tablets) | Human study | FSH↓; AMH↑; TCM syndrome score↓; mir-23a, ovarian artery RI↓. | [58] |
|
| ||||||
| Erxian decoction (EXD) | Rhizoma curculiginis, epimedium, morinda officinalis, anemarrhena, phellodendron amurense, and angelica. | N = 60 | Normal group, model group, bujiale group, low-EXD group, medium-EXD group, and high-EXD group | SD rats | FSH, LH↓; E2↑; TNF-α, IFN-γ↓; VEGF, bFGF↑. | [63] |
|
| ||||||
| Modified mulberry decoction (MMD) | Fructus mori, lilium brownii, angelica, rehmanniae radix praeparata, radix paeoniae alba, epimedium, cistanche, and licorice. | N = 60 | Control group: climen tablets treatment group: MMD | Human study | FSH, LH↓; E2↑; TCM syndrome score↓. | [66] |
|
| ||||||
| Modified bazhen decoction (MBD) | Bupleurum, angelica, ligusticum wallichii, radix paeoniae alba, glutinous rehmannia, codonopsis pilosula, atractylodes, poria cocos, licorice, antlers, radix achyranthis bidentatae, and rhizoma cyperi | N = 24 | Control group, POF group, MBD group, and FES group | SD rats | XIAP↑; mir-23a, mir-27a↓. | [67] |
|
| ||||||
| Danggui buxue decoction (DBD) | Angelica and astragalus mongholicus | N = 50 | Control group, model group, DBD group, quercetin group, and kaempferol group | SD rats | FSH, LH↓; E2, AMH↑; cytochrome c, Bax, p53 and IL6↓; ,ESR1, AR, Bcl-2↑. | [69] |
|
| ||||||
| Si-Wu-Tang (SWT) | Rehmanniae radix praeparata, angelica, paeonia lactiflora pall, and ligusticum wallichii | N = 36 | Control group, model group, low-SWT group, medium-SWT group, high-SWT group, and DHEA group | Six C57BLmice | FSH, LH↓; E2, AMH↑; TCM syndrome score↓. | [70] |
|
| ||||||
| Wenjing decoction (WJD) | Evodia rutaecarpa, cassia twig, radix paeoniae alba, angelica, ligusticum wallichii, donkey-hide gelatin, ophiopogon japonicus, ginger, rhizoma pinelliae, moutan bark, ginseng, and licorice | N = 119 | Control group: HRT (progynat + progesterone capsules) observation group: HRT (progynat + progesterone capsules), WJD, and acupuncture | Human study | FSH, LH↓; E2, AMH↑; TCM syndrome score↓. | [71] |
DAPT: dual antiplatelet therapy; FES: Fufang Ejiao Syrup; DHEA: dehydroepiandrosterone; FSH: follicle-stimulating hormone; LH: luteinizing hormone; E2: estrogen; AMH: anti-Müllerian hormone; RI: resistance index; TNF-α: tumor necrosis factor-alpha; IFN-γ: interferon-gamma; VEGF: vascular endothelial growth factor; bFGF: basic fibroblastic growth factor; XIAP: X-linked inhibitor of apoptosis protein; IL6: interleukin-6; ESR1: estrogen receptor 1; AR: androgen receptor.
3.2. Chinese Patent Medicines
Chinese patent medicines use Chinese herbs as raw materials, and these are processed into a certain dosage form according to the specified prescription and preparation process. They have the characteristics of stable nature, definite curative effects, relatively weak side effects, and convenience of consumption, transport, and storage [73–75].
3.2.1. Kuntai Capsule (KTC)
KTC is made according to the ancient prescription found in the Treatise on Febrile Diseases. It can effectively regulate women's endocrine levels, improve ovarian function, and prevent the decline of ovarian function. It can be used either alone or in combination with sex hormones to treat POF [76, 77]. Zhang et al. [78] found that KTC can regulate the estrous cycle, increase hormone secretion, improve fertility, and significantly reduce follicular atresia in the case of impaired ovarian function. Transmission electron microscopy showed that KTC could effectively maintain the ultrastructure of the mouse ovary, terminal deoxynucleotidyl transferase dUTP Nick end labeling (TUNEL) staining confirmed that KTC decreased apoptosis, and Western blot showed that KTC could reduce the expression of AMH, SOD2, Bcl-2, and Bax.
3.2.2. Kunbao Pill (KBP)
KBP [79, 80] has the effects of restoring deficiency of qi and blood, weakness of kidney qi, and imbalance of yin and yang, nourishing the liver, kidney, and blood, calming the nerves, and dredging the collaterals, and it is widely used in the treatment of POF in the clinic. Li et al. explored the effects of KBP on the prevention and treatment of a rat model of POF and showed that the serum FSH, LH, and ovarian TGF-β1 levels were significantly decreased in the low-, medium-, and high-dose groups of KBP and combined estrogen group. They also found that serum E2 levels significantly increased and that stem cell factor expression levels significantly decreased in the medium- and high-dose KBP groups and combined estrogen group, and the connective tissue growth factor expression in ovarian tissue significantly decreased in the high-dose KBP group and combined estrogen group. Together, these results indicate that KBP has the effect of regulating the hormone levels of POF, which can reduce the expression of connective tissue growth factor, TGF-β1, and stem cell factor in ovarian tissues to relieve ovarian fibrosis damage and to promote the growth and development of early follicles and thus prevent the occurrence of POF [81].
3.2.3. Other Chinese Patent Medicines
Chinese patent medicines can improve the clinical symptoms of POF and regulate the serum levels of hormones. Zishen Yutai pill (ZYP) has the effects of tonifying the kidney and spleen, nourishing blood, calming the fetus, supplementing qi, and nourishing yuan. It can effectively promote the blood supply to the female sexual organs and promote follicular development and progesterone secretion. The prescription has a good effect on promoting ovarian function. In one study, 78 patients with POF were randomly divided into a control group who took estradiol valerate tablets orally and an observation group who took estradiol valerate tablets combined with ZYP orally. The improvement in FSH, LH, and E2 contents in the observation group was significantly better than in the control group [82, 83]. Fuke Yangrong capsule is a compound preparation of TCM, and it has the effects of promoting blood circulation and menstruation, supplementing qi, nourishing the blood, tonifying the kidney, and soothing the liver. It can promote the development of the corpus luteum, accelerate the excretion of follicles, and improve ovarian function. Xiong treated patients using a sequential artificial cycle of estrogen and progesterone in the control group and a sequential artificial cycle of estrogen and progesterone combined with Fuke Yangrong capsule in the study group. The results showed that the levels of E2, FSH, and LH in the study group were significantly better than those in the control group, and this led to a significant increase in the number of sinus follicles and endometrial thickness and improved the level of sex hormones and the quality of sexual life, and thus is worthy of clinical promotion [84, 85]. Qilin pill has the functions of tonifying the kidney and essence, supplementing qi, and nourishing blood, and studies have shown that Qilin pill combined with estradiol valerate tablets can quickly and significantly reduce the serum levels of FSH and LH, increase the level of E2, and restore menstruation [86, 87].
3.3. Other Forms of Compound Chinese Medicine
Chinese medicine cream formulas are good at tonifying deficiencies. They are a commonly used TCM preparation in the gynecological clinic and are widely used because of their characteristics of slow onset of action and safety for long-term use, which is suitable for the diagnosis and treatment of POF. Moreover, the taste of Chinese medicine creams is better than Chinese medicine decoctions, which greatly improves the medication compliance of patients and thus is favored by doctors and patients [88]. To verify the efficacy of Bushen Tiaojing cream formula (BTCF) in the treatment of POF, Lu et al. [89] randomly divided 120 patients into a cream formula group, a Chinese medicine group, and a Western medicine group. In the cream formula group, the BTCF was prepared and decocted for oral administration. In the Chinese medicine group, self-prepared herbal medicine was used, and in the western medicine group, HRT was applied. After three courses of treatment, the results showed that the improvement of clinical symptoms in the cream formula group was better than that in the Western medicine group and Chinese medicine group. Compared with the Western medicine group, the cream formula group had clear advantages in treatment effect, the serum levels of E2 in the cream formula group and Chinese medicine group were higher than in the western medicine group, and the levels of FSH and LH were lower than in the western medicine group. BTCF has a significant clinical effect in the treatment of POF, and it improves clinical symptoms such as irregular menstruation, and it effectively regulates sex hormone levels and immune function [90, 91]. Yunkang oral solution (YKos) [92] has the effects of strengthening the spleen, nourishing the blood, and calming the fetus. A rat model of POF was prepared by giving cyclophosphamide. Compared with the model group, the serum E2 level of rats in the YKos group increased significantly, the FSH content decreased significantly, the ovarian and uterine coefficients increased significantly, the pathological changes of ovarian and uterine tissues improved significantly, and the expression of gonadotropin-releasing hormone receptor (GnRHR) and FSHR protein in the ovary increased significantly, indicating that YKos can effectively repair the damage to the reproductive system and can restore ovarian function through the regulation of the GnRHR-FSHR signaling pathway. The efficacy of Chinese patent medicines and other forms of compound Chinese medicines in the treatment of POF is summarized in Table 3. In addition, Ren et al. searched the Chinese science and technology journal database (VIP), the Wanfang Digital Journal Full-text Database, the China National Knowledge Infrastructure (CNKI), and other TCM literature on POF over the past 10 years and identified a total of 180 articles that met the inclusion criteria to summarize the Chinese herbal medicines with a high frequency of use in the treatment of POF as shown in Table 4 [93].
Table 3.
Summary of the efficacy of Chinese patent medicines on POF.
| Chinese patent medicine | Ingredients | Sample size | Interventions | Model used | Outcomes | References |
|---|---|---|---|---|---|---|
| Kuntai capsule (KTC) | Rehmanniae radix praeparata, rhizoma coptidis, donkey-hide gelatin, radix paeonia alba, poria cocos, and radix scutellariae. | / | / | / | FSH, LH↓; E2, AMH↑; Kupperman score↓. | [77] |
|
| ||||||
| Kunbao pills (KBP) | Fructus ligustri lucidi, raspberry, semen cuscutae, Chinese wolfberry fruit, fleeceflower root, tortoise shell, Chinese wolfberry root bark, adenophora tetraphylla, ophiopogon japonicus, wild jujube kernel, glutinous rehmannia, radix paeoniae alba, radix paeoniae rubra, angelica, spatholobus suberectus stem, nacre mother of pearl, dendrobium nobile, chrysanthemum, eclipta, folium mori, radix cynanchi atrati, anemarrhena, and radix scutellariae. | N = 60 | Blank group, model group, low-KBP group, medium-KBP group, high-KBP group, and estrogen combination group | SD rats | FSH, LH↓; E2↑; TGF-β1↓; SCF↓. | [81] |
|
| ||||||
| Zishen yutai pill (ZYP) | Semen cuscutae, fructus amomi, rehmanniae radix praeparata, ginseng, parasitic loranthus, donkey-hide gelatin, fleeceflower root, folium artemisiae argyi, morinda officinalis, bighead atractylodes rhizome, codonopsis pilosula, cornu cervi degelatinatum, Chinese wolfberry fruit, teasel root, eucommia ulmoides | N = 80 | The control group (estradiol valerate tablets), the observation group (estradiol valerate tablets combined with ZYP) | Human study | FSH, LH↓; E2↑; Kupperman score↓. | [82] |
|
| ||||||
| Fuke yangrong capsule (FYC) | Angelica, bighead atractylodes rhizome, rehmanniae radix praeparata, ligusticum wallichii, radix paeoniae alba, rhizome cyperi, motherwort, astragalus mongholicus, eucommia ulmoides, folium artemisiae argyi, ophiopogon japonicus, donkey-hide gelatin, licorice, dried tangerine peel, poria cocos, fructus amomi | N = 80 | The control group (sequential artificial cycle of estrogen and progesterone) and the observation group (sequential artificial cycle of estrogen and progesterone combined with FYC) | Human study | FSH, LH↓; E2↑; TCM syndrome score↓. | [85] |
|
| ||||||
| Qilin pill (QLP) | Prepared fleeceflower root, eclipta, epimedium, semen cuscutae, cynomorium songaricum, codonopsis pilosula, radix curcumae, raspberry, Chinese wolfberry fruit, yam, red-rooted salvia root, astragalus mongholicus, radix paeoniae alba, pericarpium citri reticulatae viride, and fructus mori | N = 72 | Climen tablet group and climen tablets combined with QLP group | Human study | FSH, LH↓; E2↑. | [87] |
|
| ||||||
| Bushen Tiaojing cream formula (BTCF) | Rehmanniae radix praeparata, yam, cornel, chinese wolfberry fruit, semen cuscutae, angelica, radix cyathulae, donkey-hide gelatin, motherwort, poria cocos, and moutan bark | N = 110 | The control group (HRT) and the observation group (HRT combined with BTCF) | Human study | FSH, LH↓; E2↑; GDF-9, BMP-15↑. | [90] |
|
| ||||||
| Yunkang oral solution (YKos) | Yam, teasel root, astragalus mongholicus, angelica, rhizoma cibotii, semen cuscutae, parasitic loranthus, eucommia ulmoides, psoralea corylifolia, codonopsis pilosula, poria cocos, bighead atractylodes rhizome, donkey-hide gelatin, glutinous rehmannia, cornel, Chinese wolfberry fruit, smoked plum, radix paeoniae alba, fructus amomi, alpinia oxyphylla, radix boehmeriae, radix scutellariae, and folium artemisiae argyi | N = 108 | Control group, CTX model group, positive control group and high-YKos, medium-YKos and low-YKos groups | SD rats | FSH↓; E2↑; ovarian coefficient, uterine coefficient↑; GnRHR, FSHR↑. | [92] |
CTX: cyclophosphamide; FSH: follicle-stimulating hormone; LH: luteinizing hormone; E2: estrogen; AMH: anti-Müllerian hormone; TGF-β1: transforming growth factor beta1; SCF: stem cell factor; GDF-9: growth differentiation factor 9; BMP15: bone morphogenetic protein 15; GnRHR: gonadotropin-releasing hormone receptor; FSHR: follicle-stimulating hormone receptor.
Table 4.
The frequency of use of Chinese herbal medicines for the treatment of POF.
| Drug efficacy | Number | Percentage (%) | Chinese herbal medicines and frequency |
|---|---|---|---|
| Tonic drug | 21 | 67.86 | Rehmanniae radix praeparata 164, angelica 164, semen cuscutae 163, yam 109, Chinese wolfberry fruit 106, radix paeoniae alba 76, licorice 67, fructus ligustri lucidi 66, epimedium 87, eucommia ulmoides 54, dried human placenta 46, morinda officinalis 43, bighead atractylodes rhizome 38, antler gelatin 38, radix glehniae 13, fructus mori 13, donkey hide gelatin 11, amethyst 10, ginseng 10, radix pseudostellariae 9, ophiopogon japonicus 9 |
| Drug for promoting blood circulation and removing stasis | 11 | 11.77 | Salvia miltiorrhiza 57, ligusticum wallichii 50, radix achyranthis bidentatae 28, radix cyathulae 24, safflower carthamus 24, spatholobus suberectus stem 23, motherwort 20, peach kernel 19, eupatorium 16, radix curcumae 10, motherwort fruit 10 |
| Astringent drug | 3 | 6.30 | Cornus officinalis 110, raspberry 24, schisandra chinensis 17 |
| Antipyretic drug | 5 | 5.09 | Moutan bark 39, phellodendron amurense 22, anemarrhena 21, rehmannia glutinosa 20, radix paeoniae rubra 20 |
| Diuretic and hygroscopic drug | 2 | 3.38 | Poria cocos 67, alisma orientalis 14 |
| Qi regulating drug | 2 | 2.84 | Rhizoma cyperi 48, dried tangerine peel 20 |
| Drug for treating external syndromes | 1 | 1.59 | Bupleurum 38 |
| Interior-warming drug | 2 | 1.17 | Cinnamomum cassia 17, radix aconiti carmichaeli 11 |
4. Acupuncture and Moxibustion
Acupuncture and moxibustion are widely used and have a variety of treatment forms. In addition to manual acupuncture and electroacupuncture stimulation, acupoint embedding and auricular acupoint pressure have also attracted much attention because of their simple operation and prolonged acupoint stimulation. Moxibustion combined with Chinese medicine decoctions can also achieve a remarkable therapeutic effect. Acupuncture and moxibustion therapy can adjust the balance of qi, blood, yin, and yang by stimulating acupoints. This has the characteristics of simple operation, safety, efficiency, and good efficacy and has been widely used in the treatment of POF. In addition, the combination of acupuncture and moxibustion with Chinese medicine and western medicine can have synergistic therapeutic effects, so such combinations are often used in clinical practice. In clinical treatment, the selection of acupoints is crucial for the therapeutic effect on the disease. Zhang et al. [94] summarized the commonly used therapeutic acupoints through a literature review of acupuncture treatments of POF, and this provides a useful reference for the clinical treatment of the disease (Table 5).
Table 5.
Modern acupuncture selection for the treatment of POF.
| Acupoint | International code | Meridians | Frequency of use | Percentage (%) |
|---|---|---|---|---|
| Guanyuan | RN4 | Ren | 34 | 73.91 |
| Shenshu | BL23 | Bladder | 29 | 63.04 |
| Sanyinjiao | SP6 | Spleen | 28 | 60.87 |
| Zhongji | RN3 | Ren | 21 | 45.65 |
| Zusanli | ST36 | Stomach | 19 | 41.30 |
| Zigong | EX-CA1 | Extra points | 18 | 39.13 |
| Pishu | BL20 | Bladder | 18 | 39.13 |
| Taixi | KI3 | Kidney | 17 | 36.96 |
| Taichong | LR3 | Liver | 16 | 34.78 |
| Ganshu | BL18 | Bladder | 16 | 34.78 |
| Xuehai | SP10 | Spleen | 15 | 32.61 |
| Qihai | RN6 | Ren | 14 | 30.43 |
| Guilai | ST29 | Stomach | 9 | 19.57 |
| Dahe | KI12 | Kidney | 7 | 15.22 |
| Ciliao | BL32 | Bladder | 7 | 15.22 |
4.1. Acupuncture
In a rat model of POF, it was found that acupuncture regulated the expression levels of genes and proteins related to the PI3K/Akt/mTOR signaling pathway, promoted an increase in serum E2 level, and restored ovarian function [4, 95]. Clinical studies have shown that acupuncture can not only actively adjust ovarian status in the early stage of POF but can also improve the menstrual situation, perimenopausal symptoms, and serum sex hormone levels, increase clinical efficiency, and create better conditions for pregnancy [96, 97]. Yao et al. [98] needled the Guanyuan (RN4), Guilai (ST29), Taichong (LR3), Taixi (KI3), Xuehai (SP10), Sanyinjiao (SP6), Zigong (EX-CA1), Yinlingquan (SP9), Zusanli (ST36), Shuidao (ST28), Dahe (KI12), and Tianshu (ST25) acupoints prior to ovulation and needled the Ciliao (BL32), Shiqizhui (EX-B7), Ganshu (BL18), Shenshu (BL23), Geshu (BL17), and Pishu (BL20) acupoints after ovulation and compared the effects to HRT. The results showed that the total effective rate of the acupuncture group was 90.4% and the expression levels of IFN-γ and TNF-α decreased while the levels of LH, FSH, and E2 improved. The umbilical cord is an important orifice in the human body and is the hub of qi movement flow in the whole body. Professor Zhang Yongchen [99] developed the clinical treatment of acupuncture combined with umbilical cord therapy in the treatment of POF and used blood prick therapy to dredge the local qi and blood to treat both the symptoms and the root cause, and this had a significant curative effect and reduced patients' pain and side effects and thus is worthy of clinical promotion and application.
4.2. Moxibustion
Moxibustion therapy regulates the body's disordered physical and chemical functions by regulating the flow of qi and blood to prevent and treat disease [100]. Experiments in animal models showed that moxibustion of RN4 and SP6 can restore ovarian function and hormone levels, reduce the content of inflammatory factors IL-6 and IL-1β, and downregulate the expression levels of phosphorylated P-PI3K, P-Akt, and P-MTOR in ovarian tissues [101]. The toll-like receptor 4 (TLR4)/nuclear factor kappa B (NF-κB) signaling pathway is the initial signal of inflammatory response. Moxibustion not only inhibits the TLR4/myeloid differentiation factor 88 (MyD88)/NF-κB signaling pathway but also indirectly decreases nod-like receptor protein-3 (NLRP3), the precursor of IL1β (Pro-IL1β), and the precursor of IL18 (Pro-IL18). It can also directly inhibit pyroptosis induced by the thioredoxin-interacting protein (TXNIP)/NLRP3/Caspase1 signaling pathway and can regulate cell death through pyroptosis to alleviate ovarian failure in POF [102]. In addition, Liu [103] used Shenque moxibustion, Guanyuan moxibustion, and fire-dragon moxibustion to treat patients with POF and found that moxibustion improved patients' menstrual activity, clinical symptoms, and serum sex hormone levels and that it was easy to perform and accept and is a safe and effective method for the clinical treatment of POF.
4.3. Electroacupuncture Stimulation
Electroacupuncture stimulation of acupoints can effectively activate the functions of relevant organs. Through different intensities of electrical stimulation, it can not only increase the blood supply and nutrition of the treatment site and improve microcirculation but can also regulate neuroendocrine function [100, 104]. In a rat model of POF, it was found that electroacupuncture could improve the local morphology of the ovary, inhibit follicular atresia, promote follicular development, and improve ovarian function [105]. It protects the ovary by upregulating the expression of the apoptosis suppressor Bcl-2 protein and downregulating the expression of the pro-apoptotic factor Bax protein in ovarian GCs, and it improves POF by mediating the PI3K/AKT/mTOR pathway [106, 107]. Other animal model experiments have shown that electroacupuncture has a good therapeutic effect on POF, which is achieved by inhibiting ferroptosis and apoptosis that are induced by glutathione peroxidase 4 (GPX4) targeting the xC-system [108]. In addition, Zhang et al. found that warm acupuncture at “RN4” combined with electroacupuncture at “SP6” could regulate the serum sex hormone levels, improve the reproductive endocrine environment, and reduce the inflammatory response of the ovary in a rat model of POF [109].
4.4. Clinical Application of Combined Acupuncture and Moxibustion
Acupuncture and moxibustion therapy are often used in combination in clinical application. Wang et al. [110] used abdominal acupuncture combined with moxibustion to treat POF, and Yu et al. [111] used umbilical needle therapy combined with mixed moxibustion to treat POF. In addition, Wu et al. [112] randomly divided 50 patients with POF into an acupuncture group and a western medicine group. The acupuncture group used ST36 and RN4 warm acupuncture combined with Baliao (BL31, BL32, BL33, and BL34) ginger moxibustion, and the western medicine group was given oral climen. The results showed that in the acupuncture group, FSH and FSH/LH decreased, E2 increased, the peak systolic velocity of ovarian artery blood flow signal increased, the artery resistance index and pulsatility index decreased, the ovarian volume increased, and the AFC increased. The total effective rate was 92.0%, which was higher than that of the western medicine group (88%). In addition, Tian et al. [113] applied electroacupuncture combined with heat-sensitive moxibustion to treat 60 patients with POF, and its total effective rate reached 93.3% with the improved menstrual cycle and symptom scores.
4.5. Acupuncture and Moxibustion Combined with Drugs
Acupuncture is often used as an auxiliary treatment method in TCM and western medicine to adjust endocrine levels and improve the clinical symptoms and the pregnancy rate of infertility patients with POF [114–116]. Lai et al. [117] proposed the clinical use of “Tongyuan acupuncture” combined with TCM in the treatment of POF. Studies have found that moxibustion combined with artificial cycle therapy in the treatment of POF can adjust the levels of sex hormones and improve clinical indicators compared with the effect of artificial cycle therapy alone [118, 119]. In addition, Chi [120] used Yougui pills, acupuncture, and moxibustion combined with sequential therapy to treat POF, and the results showed that the effective rate was up to 90.48%, the TCM syndrome score and Kupperman score significantly reduced, and the ovarian function index, hemodynamic index, and sex hormone levels significantly improved. Acupuncture and moxibustion combined with Chinese and western medicine can not only reduce the incidence of adverse reactions and improve the safety of treatment but can also increase the clinical efficacy and is thus worth promoting [121–123]. Some studies have shown that electroacupuncture combined with compound Chinese medicines has good efficacy in the treatment of POF, but the sample sizes in the studies were small, and the mechanism of action and long-term efficacy need to be further observed and studied [124, 125].
4.6. Acupoint Catgut-Embedding
Acupoint catgut-embedding therapy is an improved acupuncture method in which biodegradable medical sutures are embedded into specific acupoints and regions of the body. This can stimulate the meridians and harmonize qi and blood and has the advantages of simple operation and long stimulation effect, and thus it has become important in the treatment of gynecological diseases and can be used for the treatment of POF with good efficacy [126, 127]. Chen et al. [128] used Chinese medicine for tonifying the kidney and nourishing the liver combined with acupoint catgut-embedding to treat POF, and the total effective rate of clinical efficacy reached 86.67% and significantly improved clinical symptoms such as menstrual cycle, vaginal dryness, and loss of sexual desire, and it increased serum sex hormone levels, endometrial thickness, and ovarian volume. In addition, studies on acupoint catgut-embedding combined with Chinese patent medicines, Chinese medicine decoctions, and western medicine have shown that acupoint catgut-embedding combination therapy can improve and restore ovarian function of patients, thus providing strong evidence for its clinical promotion [129–131].
4.7. Auricular Acupoint Pressure
Ear acupoints are closely related to the Zang-Fu organs and meridians, and stimulating specific acupoints of ear acupoints can regulate autonomic nerve function and relieve the uncomfortable symptoms caused by autonomic nerve dysfunction in patients with POF [132]. Shen [133] compared Modified Guishen Pill combined with auricular acupoint therapy (the combined treatment group) with sequential estrogen-progesterone therapy (the artificial cycle group) and observed the efficacy after 3 months of treatment. The results showed that the total effective rate of the combined treatment group was 93.3% and the TCM symptom score, FSH, and LH levels were significantly lower than those of the artificial cycle group, while the E2 level was significantly increased in the combined treatment group. Ye et al. [134] treated POF using Qingxin Jianpi decoction combined with auricular acupoint pressure, with a total clinical effective rate of 82.9% and proposed that regulating the heart and spleen is an important link that cannot be ignored in the treatment of POF. In conclusion, auricular acupoint pressure therapy is often used as an auxiliary therapy for the treatment of POF. Selecting auricular acupoints according to the results of TCM syndrome differentiation can not only enhance the pertinence of clinical treatment but can also reduce the adverse reactions of drug treatment and achieve better therapeutic effects.
5. Other Treatments
In clinical studies, psychotherapy, exercise therapy, oral vitamins, massage, and other methods have been shown to have good therapeutic effects in the treatment of gynecological diseases. These methods are often used in combination with hormones and Chinese herbal medicines, which can improve the therapeutic effect and the quality of life of patients.
5.1. Psychotherapy
POF causes a great deal of physical and psychological stress in women, so psychological nursing is essential in the treatment of this disease. Psychological suggestion, targeted care, strengthening communication with patients about the disease, and enhancing communication with family members [135, 136] are commonly used in the treatment of POF and can improve anxiety, depression, and quality of life and can increase treatment compliance and treatment effect in patients with POF [137]. Cui et al. [138] proposed a psychosomatic treatment with TCM for POF that is based on regulating the movement of qi. Clinical studies have shown that combination therapy such as the psychosomatic treatment of TCM and estrogen-progesterone combined with psychological counseling has clinical promotion and application value by improving the happiness index of patients with good clinical efficacy [139–143].
5.2. Exercise
There is a close causal relationship between exercise and human physical and mental health. Physical exercise can improve body functions, and regular exercise can reduce stress, improve negative moods such as anxiety and depression, support sleep, and reduce chronic stress-related diseases [144]. Animal experiments have also shown that exercise can improve depression-like behavior in ovariectomized rats [145]. In a clinical study, Wu et al. [146] found that Baduan Jin exercises improved ovarian function, increased ovulation rates, and improved the quality of life of patients with low ovarian reserve function. Exercise therapy is simple, easy to implement, and does not increase the patient's financial burden, and it has a high acceptance among patients and strong operability, which make it highly applicable to patients with POF [147].
5.3. Vitamins
Vitamin E is a fat-soluble vitamin with strong antioxidant effects. Reasonable supplementation of vitamin E can enhance the antioxidant protection of the ovary and can increase ovarian reserve. Vitamin E combined with HRT is often used in the clinical treatment of POF [148, 149]. Zou et al. [150] further suggested that coenzyme Q10 combined with vitamin E can enhance the protective antioxidant effect on the ovaries in elderly women, improve ovarian reserve, and increase ovarian responsiveness. It has been shown that POF is a high-risk factor for osteoporosis, and the combination of calcium tablets, calcitriol, and vitamin D has definite efficacy in the treatment of POF with osteoporosis [151].
5.4. Massage
Massage, which can relax tendons, invigorate blood, improve fitness, and prevent disease, is often used clinically in combination with Chinese herbal medicine in patients with POF. Such combined therapy can improve the levels of various serum sex hormones and has good efficacy in the treatment of POF [152, 153]. In addition, Feng et al. [154] adopted electroacupuncture combined with pelvic floor muscle massage, which can not only improve the local blood flow of the ovary but can also adjust the clinical symptoms and endocrine levels of the patients as a whole to treat POF.
5.5. Diet
TCM has always held to the concept of the homology between medicine and food. Studies have shown that a high-calorie diet may contribute to metabolic disorders including diabetes, obesity, and hyperlipidemia and may also affect female fertility by directly impairing oocyte health and differentiation or by indirectly interfering with the pituitary-hypothalamic axis [155]. Chen et al. [156] explored the relationship between dietary nutrition and POF by comparing different daily intakes of protein, carbohydrate, and dietary fiber in two groups of POF patients, and they proposed the view that a deficiency of carbohydrate and dietary fiber is associated with POF. However, there is still a lack of studies examining the relationship between dietary nutrition and POF, which needs to be explored further.
6. Conclusions
In recent years, clinical and scientific researchers have paid more attention to POF and its associated symptoms such as amenorrhea and infertility. As the research has progressed, more and more CAM therapies have become widely accepted and well used, including herbal medicine, acupuncture, psychology, exercise, vitamins, massage, diet, etc. These therapies can significantly improve the patient's symptoms and hormone levels and can be used in combination with other treatments to enhance their efficacy. However, to increase the benefits of these alternative medical interventions for POF patients worldwide, the standardization of effective CAM treatments, larger sample sizes, and more randomized controlled trials are still needed to confirm the effectiveness and safety of CAM for POF.
Acknowledgments
The study was supported by the National Natural Science Foundation of China (82074484).
Data Availability
No data were used to support the findings of this study.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Authors' Contributions
Yue Li conducted the research, wrote the article, collected, and organized the data; Feng-juan Han conceived and designed the study; Meng-yu Yan, Qiao-chu Chen, Ya-ya Xie, and Chen-yu Li amended the article.
References
- 1.Fu Y. X., Ji J., Shan F., Li J., Hu R. Human mesenchymal stem cell treatment of premature ovarian failure: new challenges and opportunities. Stem Cell Research & Therapy . 2021;12:p. 161. doi: 10.1186/s13287-021-02212-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu X. L., Hu C. Y., Liu G., Guo Q. Recent research progress in the pathogenesis and related therapeutic mechanisms of premature ovarian failure. Journal of Jiangsu University (Medicine Edition) . 2021;31:541–548. doi: 10.13312/j.issn.1671-7783.y210061. [DOI] [Google Scholar]
- 3.Grossmann B., Saur S., Rall K., et al. Prevalence of autoimmune disease in women with premature ovarian failure. The European Journal of Contraception and Reproductive Health Care . 2020;25(1):72–75. doi: 10.1080/13625187.2019.1702638. [DOI] [PubMed] [Google Scholar]
- 4.Zhang Y. M., Yu B., Chen J., et al. Effects of acupuncture on PI3K/Akt/mTOR signaling pathway in rats with premature ovarian failure. Zhongguo Zhen Jiu = Chinese Acupuncture & Moxibustion . 2015;35(1):53–58. doi: 10.13703/j.0255-2930.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 5.Ceccarelli F., Orefice V., Perrone G., et al. Premature ovarian failure in patients affected by systemic lupus erythematosus: a cross-sectional study. Clinical & Experimental Rheumatology . 2020;38(3):450–454. [PubMed] [Google Scholar]
- 6.Gong T., Liu L., Jiang W., Zhou R. DAMP-sensing receptors in sterile inflammation and inflammatory diseases. Nature Reviews Immunology . 2020;20(2):95–112. doi: 10.1038/s41577-019-0215-7. [DOI] [PubMed] [Google Scholar]
- 7.Du Q., He D., Zeng H. L., et al. Siwu paste protects bone marrow hematopoietic function in rats with blood deficiency syndrome by regulating TLR4/NF-κB/NLRP3 signaling pathway. Journal of Ethnopharmacology . 2020;262 doi: 10.1016/j.jep.2020.113160.113160 [DOI] [PubMed] [Google Scholar]
- 8.Li Y., Xu P., Wang Y., et al. Different intensity exercise preconditions affect cardiac function of exhausted rats through regulating TXNIP/TRX/NF-κBp65/NLRP3 inflammatory pathways. Evidence-Based Complementary and Alternative Medicine . 2020;2020:9. doi: 10.1155/2020/5809298.5809298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yoo M., Tanaka T., Konishi H., et al. The protective effect of testosterone on the ovarian reserve during cyclophosphamide treatment. OncoTargets and Therapy . 2020;13:2987–2995. doi: 10.2147/OTT.S242703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li J., Xu L., Gao Y. Research progress and current status of etiological mechanism and treatment of premature ovarian failure. China Medicine and Pharmacy . 2021;11:58–61. [Google Scholar]
- 11.Liao B. Q., Liu C. B., Xie S. J., et al. Effects of fine particulate matter (PM 2.5) on ovarian function and embryo quality in mice. Environment International . 2020;135 doi: 10.1016/j.envint.2019.105338.105338 [DOI] [PubMed] [Google Scholar]
- 12.Fu X. Y., Chen H. H., Zhang N., et al. Effects of chronic unpredictable mild stress on ovarian reserve in female rats: feasibility analysis of a rat model of premature ovarian failure. Molecular Medicine Reports . 2018;18(1):532–540. doi: 10.3892/mmr.2018.8989. [DOI] [PubMed] [Google Scholar]
- 13.Barros F., Carvalho F., Barros A., Dória S. Premature ovarian insufficiency: clinical orientations for genetic testing and genetic counseling. Porto Biomedical Journal . 2020;5 doi: 10.1097/j.pbj.0000000000000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yin N., Wang Y., Lu X., et al. hPMSC transplantation restoring ovarian function in premature ovarian failure mice is associated with change of Th17/Tc17 and Th17/Treg cell ratios through the PI3K/Akt signal pathway. Stem Cell Research & Therapy . 2018;9(1) doi: 10.1186/s13287-018-0772-x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 15.Wang L. L., Peng Y. J., You W., Liu L. H. Bushen Shugan decoction combined with hormone replacement therapy in the treatment of premature ovarian failure patients with negative emotions and the effect on sex hormone levels. Modern Journal of Integrated Traditional Chinese and Western Medicine . 2022;31:243–247. [Google Scholar]
- 16.Tatang C., Arredondo Bisonó T., Bergamasco A., Salvo F., Costa Clemens S. A., Moride Y. Human papillomavirus vaccination and premature ovarian failure: a disproportionality analysis using the vaccine adverse event reporting system. Drugs - Real World Outcomes . 2022;9:79–90. doi: 10.1007/s40801-021-00271-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ghahremani-Nasab M., Ghanbari E., Jahanbani Y., Mehdizadeh A., Yousefi M. Premature ovarian failure and tissue engineering. Journal of Cellular Physiology . 2020;235(5):4217–4226. doi: 10.1002/jcp.29376. [DOI] [PubMed] [Google Scholar]
- 18.Kasprzycka K., Kurzawa M., Kucharz M., et al. Complementary and alternative medicine use in hospitalized cancer patients-study from Silesia, Poland. International Journal of Environmental Research and Public Health . 2022;19 doi: 10.3390/ijerph19031600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guo Y., Liu F. Y., Shen Y., et al. Complementary and alternative medicine for dysmenorrhea caused by endometriosis: a review of utilization and mechanism. Evidence-Based Complementary and Alternative Medicine . 2021;2021:14. doi: 10.1155/2021/6663602.6663602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feng J., Wang J., Zhang Y., et al. The efficacy of complementary and alternative medicine in the treatment of female infertility. Evidence-Based Complementary and Alternative Medicine . 2021;2021:21. doi: 10.1155/2021/6634309.6634309 [DOI] [Google Scholar]
- 21.Ng J. Y., Jomy J., Vacca A. Evaluation of the quality of online patient information at the intersection of complementary and alternative medicine and hypertension. Clinical Hypertension . 2022;28(1) doi: 10.1186/s40885-021-00193-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang D., Jiang Y., Feng J., et al. Evidence for the use of complementary and alternative medicine for pelvic inflammatory disease: a literature review. Evidence-Based Complementary and Alternative Medicine . 2022;2022:20. doi: 10.1155/2022/1364297.1364297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu J. S., Zhang Y., Wen Y., Zhang J. J. Effect of icariin on serum estradiol level in ovariectomized mice. Guizhou Medical Journal . 2010;34(1):79–80. [Google Scholar]
- 24.Dong R. X., Zhu X. D., Fan B. Z., et al. Research on effects of icariin on ovarian reserve in Cisplatin-induced premature ovarian failure rats. Zhejiang Medical Journal . 2019;41:230–233. [Google Scholar]
- 25.Li N., Wang J., Wang X., Sun J., Li Z. Icariin exerts a protective effect against d-galactose induced premature ovarian failure via promoting DNA damage repair. Biomedicine & Pharmacotherapy . 2019;118 doi: 10.1016/j.biopha.2019.109218.109218 [DOI] [PubMed] [Google Scholar]
- 26.Wang Y. X., Ma N., Zhong X. M., Cui R., Miao Z. L. Research on effects of total flavonoids of dodder seed on ovarian function in rats with premature ovarian failure. Medical Recapitulate . 2019;25:2695–2699. [Google Scholar]
- 27.Huang C. S., He S. D., Guan Y. C., et al. Effects of flavonoid of dodder seed and quercetin on ovarian function in rats with premature ovarian failure induced by tripterygium glycosides. The Chinese Journal of Clinical Pharmacology . 2020;36(6):667–670. doi: 10.13699/j.cnki.1001-6821.2020.06.021. [DOI] [Google Scholar]
- 28.Huang C. S., Ning Y., Guan Y. C., et al. Quercetin and flavonoids from cuscuta chinensis lam. inhibit tripterygium glycoside-induced premature ovarian failure progression via PI3K-AKT signaling pathway. Pharmacognosy Magazine . 2021;17 doi: 10.4103/PM.PM_25_20. [DOI] [Google Scholar]
- 29.Chu J. M., Ma S. Y., Li H. F., Xu L. Research progress of active ingredients and pharmacological action of kudzuvine root. Food and Drug . 2015;17:142–146. [Google Scholar]
- 30.Zhang H. Y., Liang R., Cao C. S., et al. Effect of puerarin on premature ovarian failure induced by cisplatin in mice. China Journal of Modern Medicine . 2021;31:67–73. [Google Scholar]
- 31.Chen C., Li S., Hu C., et al. Protective effects of puerarin on premature ovarian failure via regulation of Wnt/β-catenin signaling pathway and oxidative stress. Reproductive Sciences . 2021;28:982–990. doi: 10.1007/s43032-020-00325-0. [DOI] [PubMed] [Google Scholar]
- 32.Yang J. L., Gao L. L., Zhu P. Research progress of ginsenoside biosynthesis. Acta Pharmaceutica Sinica . 2013;48:170–178. doi: 10.16438/j.0513-4870.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 33.He L., Ling L., Wei T., Wang Y., Xiong Z. Ginsenoside Rg1 improves fertility and reduces ovarian pathological damages in premature ovarian failure model of mice. Experimental Biology and Medicine . 2017;242:683–691. doi: 10.1177/1535370217693323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu X. H., Zhao Z. H., Zhou Y., Wang C. L., Han Y. J., Zhou W. Effect of ginsenoside Rg1 in delaying premature ovarian failure induced by D-gal in mice through PI3K/Akt/mTOR autophagy pathway. Zhongguo Zhong Yao Za Zhi = Zhongguo Zhongyao Zazhi = China Journal of Chinese Materia Medica . 2020;45:6036–6042. doi: 10.19540/j.cnki.cjcmm.20200901.405. [DOI] [PubMed] [Google Scholar]
- 35.Liang Y., Wu D. Effect of american ginseng on the expression of HPGDS, PLA2G4A, and PTGS1 genes in ovary of rats with premature ovarian failure. Chinese Journal of Traditional Medical Science and Technology . 2016;23:166–167. [Google Scholar]
- 36.Zhu L., Li J., Xing N., Han D., Kuang H., Ge P. American ginseng regulates gene expression to protect against premature ovarian failure in rats. BioMed Research International . 2015;2015:8. doi: 10.1155/2015/767124.767124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ge P., Xing N., Ren Y., et al. Preventive effect of American ginseng against premature ovarian failure in a rat model. Drug Development Research . 2014;75(8):521–528. doi: 10.1002/ddr.21234. [DOI] [PubMed] [Google Scholar]
- 38.Zhang N. N. Study on the regulation of desertliving cistanche polysaccharide on endocrine function in menopausal hypertensive rats with dryness syndrome. Acta Chinese Medicine and Pharmacology . 2018;46(1):65–69. doi: 10.19664/j.cnki.1002-2392.180016. [DOI] [Google Scholar]
- 39.Liu T., Yin S. N., Luan X. Effect of desertliving cistanche on immune factors and apoptosis-related proteins in rats with premature ovarian failure. The Chinese Journal of Clinical Pharmacology . 2019;35:3084–3087. doi: 10.13699/j.cnki.1001-6821.2019.23.036. [DOI] [Google Scholar]
- 40.Li L., Lu P., Gao X. Chinese Angelica polysaccharide regulates endocrine function in mice with immune premature ovarian failure through AKT/FOXO3 pathway. Genomics and Applied Biology . 2019;38:3268–3272. doi: 10.13417/j.gab.038.003268. [DOI] [Google Scholar]
- 41.Huang T., Zheng X. X., Qiu X. H., Wang Y. Protective effect of lycium barbarum polysaccharide on autoimmune premature ovarian failure model mice. Journal of Pharmaceutical Research . 2014;33:437–440. doi: 10.13506/j.cnki.jpr.2014.08.002. [DOI] [Google Scholar]
- 42.Wang K., Liu S. S., Guo Q. Y., Lin J. W., Wu Z. F., Sun X. S. Study on the ovarian maintenance effect of maca powder on premature ovarian failure model rats with Kidney Yang deficiency syndrome. China Pharmacy . 2016;27:3929–3932. [Google Scholar]
- 43.Li Y., Qiu W., Zhang Z., et al. Oral oyster polypeptides protect ovary against d-galactose-induced premature ovarian failure in C57BL/6 mice. Journal of the Science of Food and Agriculture . 2020;100(1):92–101. doi: 10.1002/jsfa.9997. [DOI] [PubMed] [Google Scholar]
- 44.Li L., Zhong D. Y., Yang K. F., Xiao X. Q. To explore the regularity of medication for premature ovarian failure based on the medical records of famous doctors. China Medical Herald . 2020;17:165–168. [Google Scholar]
- 45.Fan S. Effect of Supplemented Bushen Decoction on Lipoprotein Residue and Endometrium in Model Rats with POF Hyperlipidemia . Nanchang, China: Jiangxi University of Chinese Medicine; 2019. [Google Scholar]
- 46.Rao C. C. Protective Effects of Two-Immortals Decoction and Medicine Pair Common Curculigo Rhizome-Epimedium Herb on Ovarian Oxidative Damage Induced by Cisplatin . Beijing, China: Beijing University of Chinese Medicine; 2019. [Google Scholar]
- 47.Chen J. Y., Feng L., Tong G. Q., Li L. Traditional Chinese medicine reverses resistance to epidermal growth factor receptor tyrosine kinase inhibitors in advanced non-small cell lung cancer: a narrative review. Journal of traditional Chinese medicine = Chung i tsa Chih Ying Wen Pan . 2021;41(4):650–656. doi: 10.19852/j.cnki.jtcm.2021.03.017. [DOI] [PubMed] [Google Scholar]
- 48.Jiang Z., Jiang L. X., Li Z. T., et al. Progress in decoction methods and influencing factors of traditional Chinese medicine decoction. Journal of Guangzhou University of Traditional Chinese Medicine . 2022;39(2):458–462. doi: 10.13359/j.cnki.gzxbtcm.2022.02.040. [DOI] [Google Scholar]
- 49.Zhao F. Q., Zhao Y., Liu J. Y., et al. Left-restoring pill on apoptosis and p53 protein expression in ovarian tissue of rats injured by 6 0 Gyγ-ray. Global Traditional Chinese Medicine . 2022;15:378–383. [Google Scholar]
- 50.Zhang F. F., Cui X. P., Zhao P. T., Zhang X. Y., Xiao X. C. Experience of Cui Xiaoping, chief physician in the treatment of premature ovarian failure. Western Journal of Traditional Chinese Medicine . 2022;35:48–51. [Google Scholar]
- 51.Wu X. Y., Cui X. P., Fan M. L., Liu L. Clinical and experimental research progress of left-restoring pill in the treatment of premature ovarian failure. Acta Chinese Medicine . 2020;35:568–572. doi: 10.16368/j.issn.1674-8999.2020.03.129. [DOI] [Google Scholar]
- 52.Zeng L., Ye J., Zhang Z., et al. Zuogui pills maintain the stemness of oogonial stem cells and alleviate cyclophosphamide-induced ovarian aging through notch signaling pathway. Phytomedicine . 2022;99 doi: 10.1016/j.phymed.2022.153975. [DOI] [PubMed] [Google Scholar]
- 53.Peng H., Zeng L., Zhu L., et al. Zuogui pills inhibit mitochondria-dependent apoptosis of follicles in a rat model of premature ovarian failure. Journal of Ethnopharmacology . 2019;238 doi: 10.1016/j.jep.2019.111855.111855 [DOI] [PubMed] [Google Scholar]
- 54.Zhu L., Zhang Y. Q., Peng Y. L., Ren J. J. Effect of left-restoring pill on GDF-9/Smad2 signal transduction in ovary of immune premature ovarian failure model mice. Chinese Journal of Integrated Traditional and Western Medicine . 2017;37:1367–1371. [Google Scholar]
- 55.Dong Y. L., Dong L. Clinical observation of Bushen Huoxue decoction in treating premature ovarian failure and its effect on ANA-ACA-AOA pathway. Shanghai Journal of Traditional Chinese Medicine . 2020;54:61–65. doi: 10.16305/j.1007-1334.2020.08.011. [DOI] [Google Scholar]
- 56.Wang P., Lu Y., Chen S., Chen Y., Hu C., Zuo Y. Protective function of Bu Shen Huo Xue formula on the immunity of B6AF1 mice with experimental autoimmune premature ovarian failure. Experimental and Therapeutic Medicine . 2018;15(4):3302–3310. doi: 10.3892/etm.2018.5804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Song K. K., Ma W. W., Huang C., et al. Effect and mechanism of Bushen Huoxue recipe on ovarian reserve in mice with premature ovarian failure. Journal of Huazhong University of Science and Technology. Medical Sciences=Hua Zhong ke ji da Xue Xue Bao. Yi Xue Ying De Wen Ban=Huazhong Keji Daxue Xuebao. Yixue Yingdewen Ban . 2016;36:571–575. doi: 10.1007/s11596-016-1627-2. [DOI] [PubMed] [Google Scholar]
- 58.Song J. Y., Xia Y. Q., Dong L. To investigate the effect of Zhu’s Bushen Huoxue decoction on premature ovarian failure based on the correlation between AMH and microRNA-23a. Shanghai Journal of Traditional Chinese Medicine . 2021;55:41–45. doi: 10.16305/j.1007-1334.2021.1907166. [DOI] [Google Scholar]
- 59.Liu H. P., Zeng L. T., Hu L. J., Wang C., Yang K. L., Zhang G. M. Effect of Bushen Huoxue decoction on the expression of TGF-β1, TGF-βRII, and Smad2/3 in granulosa cells of mice with premature ovarian failure. Chinese Traditional Patent Medicine . 2017;39:1782–1788. [Google Scholar]
- 60.Hu L. J., Liu H. P., Zeng L. T., Liao H. Y., Zhang G. M., Yang K. L. Effect of Bushen Huoxue recipe on PI3, Akt, and Bcl2 protein in immune premature ovarian failure mice. Chinese Archives of Traditional Chinese Medicine . 2017;35:2282–2284. doi: 10.13193/j.issn.1673-7717.2017.09.021. [DOI] [Google Scholar]
- 61.Li Y., Li X. B., Cao X. J. To investigate the mechanism of two-immortals decoction in treating premature ovarian failure based on network pharmacology and molecular docking. Journal of Hainan Medical University . 2021. [DOI]
- 62.Du B., Liu L. H., Lv Y. J., Ai H. Systems pharmacology uncovers multiple mechanisms of Erxian decoction for treatment of premature ovarian failure. Chinese Journal of Integrative Medicine . 2020;26(2):106–113. doi: 10.1007/s11655-019-3201-9. [DOI] [PubMed] [Google Scholar]
- 63.Zhou M. L., Yu X. L., Mao H. The effect of two-immortals decoction on the levels of serum inflammatory factors, related growth factors and sex hormones in rats with premature ovarian failure. Chinese Archives of Traditional Chinese Medicine . 2021;39:240–243. doi: 10.13193/j.issn.1673-7717.2021.09.060. [DOI] [Google Scholar]
- 64.Zhang X. L., Li J., Zhou X. L., Chen Q. L. Effect of Er-Xian decoction on autoimmune premature ovarian failure in mice. Journal of traditional Chinese medicine=Chung i tsa Chih Ying Wen Pan . 2021;41:725–731. doi: 10.19852/j.cnki.jtcm.2021.05.007. [DOI] [PubMed] [Google Scholar]
- 65.Han Y. H., Geng T. T., Han Y. G. Han’s gynecology experience in the treatment of premature ovarian failure based on the theory of liver and kidney theory. China Journal of Traditional Chinese Medicine and Pharmacy . 2021;36:7177–7179. [Google Scholar]
- 66.Wang W. P., Liu Q. H., Fang Y. Treatment of 30 cases of premature ovarian failure with supplemented Sangshen decoction. Henan Traditional Chinese Medicine . 2020;40:1074–1076. doi: 10.16367/j.issn.1003-5028.2020.07.0272. [DOI] [Google Scholar]
- 67.Liu C., Li Q., Yang Y. Effects of the modified Bazhen decoction in the treatment of premature ovarian failure in rats. Annals of Clinical and Laboratory Science . 2019;49(1):16–22. [PubMed] [Google Scholar]
- 68.Liu M. M., Yu X. H., Li W. L. Li Weili treats premature ovarian failure. Journal of Changchun University of Traditional Chinese Medicine . 2021;37:538–540. doi: 10.13463/j.cnki.cczyy.2021.03.018. [DOI] [Google Scholar]
- 69.Liu H., Yang H., Qin Z., et al. Exploration of the Danggui Buxue decoction mechanism regulating the balance of ESR and AR in the TP53-AKT signaling pathway in the prevention and treatment of POF. Evidence-Based Complementary and Alternative Medicine . 2021;2021:16. doi: 10.1155/2021/4862164.4862164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhou F., Song Y., Liu X., et al. Si-Wu-Tang facilitates ovarian function through improving ovarian microenvironment and angiogenesis in a mouse model of premature ovarian failure. Journal of Ethnopharmacology . 2021;280 doi: 10.1016/j.jep.2021.114431.114431 [DOI] [PubMed] [Google Scholar]
- 71.Yi A., Qin X., Du Z., Wang T., Liu F. Clinical observation on the improvement of serum sex hormone and ovarian function in premature ovarian failure patients with deficiency-cold syndrome by combining Wenjing decoction with tiaobu Chongren acupuncture and moxibustion. Evidence-Based Complementary and Alternative Medicine . 2021;2021:9. doi: 10.1155/2021/3926822.3926822 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 72.Guilin F., Meijiao L., Xiaolin Z., Lihong Z., Jing L., Jingfeng O. Efficacy of Bushenjianpi prescription on autoimmune premature ovarian failure in mice. Journal of Traditional Chinese Medicine . 2017;37(5):667–674. doi: 10.1016/s0254-6272(17)30321-7. [DOI] [PubMed] [Google Scholar]
- 73.Pang Q., Yang Y. N., Wu Q., Ni Q., Liao X. Overview of clinical research evidence of oral Chinese patent medicine in the treatment of hyperlipidemia. Chinese Journal of Experimental Traditional Medical Formulae . 2022;28:214–221. doi: 10.13422/j.cnki.syfjx.20220892. [DOI] [Google Scholar]
- 74.Peng D. H., Qiang X. Y., Hu H. Y., et al. Clinical evidence analysis report of Chinese patent medicine in 2020. Zhongguo Zhong Yao Za Zhi=Zhongguo Zhongyao Zazhi=China Journal of Chinese Materia Medica . 2022;47(9):2315–2321. doi: 10.19540/j.cnki.cjcmm.20220209.502. [DOI] [PubMed] [Google Scholar]
- 75.Geng Z., Duan L. Q., Yi H., Wu S. Q., Peng Y. J. Consideration of controllable mass proportion in Chinese patent medicine standard. Lishizhen Medicine and Materia Medica Research . 2021;32:2983–2985. [Google Scholar]
- 76.Sun W. Application effect of Kun Tai Capsule in the treatment of decline in ovarian reserve and premature ovarian failure. Guide of China Medicine . 2021;19:108–109. doi: 10.15912/j.cnki.gocm.2021.08.051. [DOI] [Google Scholar]
- 77.Liu W., Nguyen T. N., Tran Thi T. V., Zhou S. Kuntai capsule plus hormone therapy vs. hormone therapy alone in patients with premature ovarian failure: a systematic review and meta-analysis. Evidence-Based Complementary and Alternative Medicine . 2019;2019:9. doi: 10.1155/2019/2085804.2085804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhang J., Fang L., Shi L., et al. Protective effects and mechanisms investigation of Kuntai capsule on the ovarian function of a novel model with accelerated aging ovaries. Journal of Ethnopharmacology . 2017;195:173–181. doi: 10.1016/j.jep.2016.11.014. [DOI] [PubMed] [Google Scholar]
- 79.Yang J. T. Clinical study on the therapeutic effect and adverse reactions of Kunbao pills on climacteric syndrome. Strait Pharmaceutical Journal . 2021;33:108–110. [Google Scholar]
- 80.Li H. Y., Li Y. Y., Fan L. L., Cao Y. H. Clinical observation of Kuntai capsule combined with Kunbao pills in the treatment of perimenopausal cardiovascular disease. World Journal of Integrated Traditional and Western Medicine . 2020;15:119–122. doi: 10.13935/j.cnki.sjzx.200125. [DOI] [Google Scholar]
- 81.Li X., Li J. Effect of Kunbao pills on experimental premature ovarian failure model in rats. Journal of Guangzhou University of Traditional Chinese Medicine . 2021;38(09):1949–1954. doi: 10.13359/j.cnki.gzxbtcm.2021.09.028. [DOI] [Google Scholar]
- 82.Yang J. H., Tang L. H., Wei H., Song X. Efficacy of Zishen Yutai pills combined with estradiol valerate in the treatment of female premature ovarian failure and its effect on serum estrogen level. Chongqing Medicine . 2020;49:3803–3806. [Google Scholar]
- 83.Xie J., Chen M. F. Clinical observation of Zishen Yutai pills combined with climen in treatment of premature ovarian failure. Journal of Hunan University of Chinese Medicine . 2017;37:1396–1399. [Google Scholar]
- 84.Xiong R. R. Effect of Fuke Yangrong capsule combined with drospirone eynestradiol on endometrial thickness and sexual quality in patients with premature ovarian failure. Journal of Medical Forum . 2019;40:145–148. [Google Scholar]
- 85.Liu H. Y. Effect of Fuke Yangrong capsule combined with estrogen and progesterone in artificial cycle sequential treatment of premature ovarian failure. Medical Journal of Chinese People’s Health . 2021;33:73–75. [Google Scholar]
- 86.Lv S. M. Clinical observation of Qili pills combined with foot bath in the treatment of premature ovarian failure (kidney deficiency syndrome) Biped and Health . 2019;28:181–182. doi: 10.19589/j.cnki.issn1004-6569.2019.14.181. [DOI] [Google Scholar]
- 87.Liang B. Clinical analysis of 72 cases of premature ovarian failure treated with Qilin Pills and Climen. China’s Naturopathy . 2017;25:56–57. doi: 10.19621/j.cnki.11-3555/r.2017.05.048. [DOI] [Google Scholar]
- 88.Liu W. L., Gao J., Luo S. P. The embodiment of Yang transforming Qi while Yin constituting form in the diagnosis and treatment of premature ovarian failure. Modern Chinese Clinical Medicine . 2021;28:73–76. [Google Scholar]
- 89.Lu Y. L., Li J., Han L. Clinical study on the treatment of premature ovarian failure with kidney deficiency syndrome by Bushen Tiaojing cream formula. World Journal of Integrated Traditional and Western Medicine . 2019;14:388–391. doi: 10.13935/j.cnki.sjzx.190323. [DOI] [Google Scholar]
- 90.Wang J., Liu B. Effect of Bushen Tiaojing cream formula on the levels of sex hormones, GDF-9 and BMP-15 in patients with premature ovarian failure of kidney deficiency syndrome. Modern Journal of Integrated Traditional Chinese and Western Medicine . 2018;27 [Google Scholar]
- 91.Zhao X. Y., Xie Y. H., Zheng H. Z., Chen H. B. Therapeutic effect of Bushen Tiaojing cream formula on premature ovarian failure of kidney deficiency syndrome and its influence on sex hormones and immune function. Chinese Archives of Traditional Chinese Medicine . 2019;37(01):192–196. doi: 10.13193/j.issn.1673-7717.2019.01.048. [DOI] [Google Scholar]
- 92.Xia W., Liu X. W., Wang X. Q., Jiang D. J., Li X. R. Yunkang Oral solution ameliorates cyclophosphamide-induced premature ovarian failure in rats and its mechanism. Chinese Journal of Pharmacology and Toxicology . 2020;34:591–596. [Google Scholar]
- 93.Ren H. X., Si F., Zhu K., Zhu X. X., Wang C. H. Study on the regularity of traditional Chinese medicine compound in the treatment of premature ovarian failure based on data mining technology. Chinese Medicine Modern Distance Education of China . 2022;20:45–48. [Google Scholar]
- 94.Zhang J., Huang H. L., Zhang Y. C., Jia H. L. Study on acupoint selection rule of modern acupuncture and moxibustion treatment for premature ovarian failure. Shandong Journal of Traditional Chinese Medicine . 2019;38:534–538. doi: 10.16295/j.cnki.0257-358x.2019.06.008. [DOI] [Google Scholar]
- 95.Wang S., Lin S., Zhu M., et al. Acupuncture reduces apoptosis of granulosa cells in rats with premature ovarian failure via restoring the PI3K/Akt signaling pathway. International Journal of Molecular Sciences . 2019;20:p. 6311. doi: 10.3390/ijms20246311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fang Y. G., Chen Y. R., Wang F., Yang L. Preacupuncture intervention in 24 cases of premature ovarian failure. Chinese Acupuncture & Moxibustion . 2017;37:256–258. doi: 10.13703/j.0255-2930.2017.03.009. [DOI] [Google Scholar]
- 97.Guo Y. J. Guangzhou, China: Guangzhou University of Chinese Medicine; 2017. clinical study on the treatment of premature ovarian failure with regulating conception vessel and dredging governor vessel. M.A thesis. [Google Scholar]
- 98.Yao M., Wang Q., Pan H. L., Xu Z. M., Song A. Q. Effect of acupuncture on the expressions of TNF-α and IFN-γ in patients with premature ovarian failure. Zhongguo Zhen Jiu=Chinese Acupuncture & Moxibustion . 2019;39:1181–1184. doi: 10.13703/j.0255-2930.2019.11.012. [DOI] [PubMed] [Google Scholar]
- 99.Zhang H. F., Zhu Y. Z., Jia H. L., Zhang Y. C. Professor Zhang Yongchen’s experience of acupuncture combined with umbilical therapy in treating premature ovarian failure. Journal of Zhejiang Chinese Medical University . 2017;41:339–341. doi: 10.16466/j.issn1005-5509.2017.04.020. [DOI] [Google Scholar]
- 100.Xu F. H., Hou Y. N., Ge P. L., Chen H. Z., Zhu X. L. Characteristics of TCM treatment of premature ovarian failure. Journal of Liaoning University of Traditional Chinese Medicine . 2020;22:25–28. doi: 10.13194/j.issn.1673-842x.2020.01.008. [DOI] [Google Scholar]
- 101.Zhang C. R., Deng J. L., Zhu W. N., et al. Involvement of PI 3 K/Akt/mTOR signaling in protective effects of moxibustion for premature ovarian failure in rats. Zhen Ci Yan Jiu=Acupuncture Research . 2018;43:75–79. doi: 10.13702/j.1000-0607.170857. [DOI] [PubMed] [Google Scholar]
- 102.Zhang C. R., Zhu W. N., Tao W., et al. Moxibustion against cyclophosphamide-induced premature ovarian failure in rats through inhibiting NLRP3-/Caspase-1-/GSDMD-dependent pyroptosis. Evidence-Based Complementary and Alternative Medicine . 2021;2021:9. doi: 10.1155/2021/8874757.8874757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Liu L. J. Jinan, China: Shandong University of Traditional Chinese Medicine; 2018. comparative observation on the clinical efficacy of different moxibustion methods in the treatment of premature ovarian failure. M.A thesis. [Google Scholar]
- 104.Xu M. B., Tian H. Y. Comparative observation on the therapeutic effect of electroacupuncture combined with thermal moxibustion and Western medicine on premature ovarian failure. World Journal of Acupuncture-Moxibustion . 2017;27:9–14. [Google Scholar]
- 105.Yu X. Q., Li Y. J. Study on the effect of Chinese herbs for Tonifying kidney and soothing liver combined with acupuncture on ovarian reserve in rats with premature ovarian failure. Jiangsu Journal of Traditional Chinese Medicine . 2019;51:83–87. [Google Scholar]
- 106.Wang W. M., Wang Y., Wu J. N., Yang L. K., Liu Z. S. Protective effects of electroacupuncture pretreatment on ovarian in rats with premature ovarian insufficiency. Zhongguo Zhen Jiu=Chinese Acupuncture & Moxibustion . 2018;38(4):405–411. doi: 10.13703/j.0255-2930.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 107.Zhang H., Qin F., Liu A., et al. Electro-acupuncture attenuates the mice premature ovarian failure via mediating PI3K/Akt/mTOR pathway. Life Sciences . 2019;217:169–175. doi: 10.1016/j.lfs.2018.11.059. [DOI] [PubMed] [Google Scholar]
- 108.Geng Z. X., Nie X. L., Liu P., et al. Effect of electroacupuncture on iron death in mice with premature ovarian failure. Shanghai Journal of Acupuncture and Moxibustion . 2022. pp. 1–8. [DOI]
- 109.Zhang Q., Ji B., Xie Y. N., et al. Effect of warm acupuncture combined with electroacupuncture on serum sex hormones and inflammatory factors in rats with premature ovarian failure. Chinese Journal of Information on Traditional Chinese Medicine . 2021;28:62–67. doi: 10.19879/j.cnki.1005-5304.202103029. [DOI] [Google Scholar]
- 110.Wang Q., Huang W., Gao F., Liao H. Y., Yao M. Effect of abdominal acupuncture combined with governor vessel moxibustion on levels of sex hormones and immune cells in patients with premature ovarian failure. Journal of Yunnan University of Traditional Chinese Medicine . 2020;43:60–64. doi: 10.19288/j.cnki.issn.1000-2723.2020.02.012. [DOI] [Google Scholar]
- 111.Yu X. J., Zhu X. Y., Hua S. S. Clinical observation on umbilical acupuncture combined with mixed moxibustion in treating premature ovarian failure. Guangming Journal of Chinese Medicine . 2019;34:2035–2037. [Google Scholar]
- 112.Wu S., Yan J. T. Clinical observation on premature ovarian failure by warming acupuncture at Zusanli (ST 36) and Guanyuan (CV 4) combined with ginger moxibustion at Baliao points. Zhongguo Zhen Jiu=Chinese Acupuncture & Moxibustion . 2018;38:1267–1271. doi: 10.13703/j.0255-2930.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 113.Tian H. Y., Wu D., Zhang G. F. 60 cases of premature ovarian failure of kidney deficiency and liver depression syndrome treated by electroacupuncture combined with thermal moxibustion. Chinese Acupuncture & Moxibustion . 2016;36:1069–1070. doi: 10.13703/j.0255-2930.2016.10.017. [DOI] [Google Scholar]
- 114.Teng X. X., Liu D., Yao H. Y., Liu Z. Z. A small sample prospective clinical study on acupuncture combined with modified Yulin decoction in the treatment of premature ovarian failure with spleen-kidney yang deficiency syndrome. Chinese Journal for Clinicians . 2018;46:1372–1375. [Google Scholar]
- 115.Hou S. L., Zhao P., Shi Y. L. Observation on therapeutic effect of acupuncture combined with western medicine on infertility caused by premature ovarian failure. Shanghai Journal of Acupuncture and Moxibustion . 2019;38(01):82–85. doi: 10.13460/j.issn.1005-0957.2019.01.0082. [DOI] [Google Scholar]
- 116.Wu J. M., Ning Y., Chen Y., Tang M., Zhuo Y. Y. Clinical observation on treatment of premature ovarian failure with acupuncture for regulating meridians and promoting pregnancy. Lishizhen Medicine and Materia Medica Research . 2019;30:1422–1423. [Google Scholar]
- 117.Li X. Z., Zhang S. J. Professor LAI Xinsheng’s clinical experience in the treatment of premature ovarian failure with Tongyuan acupuncture technique and Chinese herbal medicine. Zhongguo Zhen Jiu=Chinese Acupuncture & Moxibustion . 2017;37:303–306. doi: 10.13703/j.0255-2930.2017.03.023. [DOI] [PubMed] [Google Scholar]
- 118.Yang X., Kang J. S., Yang S. L., Wang R. L. Clinical observation on thermal moxibustion combined with artificial cycle in treating premature ovarian failure of and spleen-kidney Yang deficiency syndrome. Shanghai Journal of Acupuncture and Moxibustion . 2021;40:715–720. doi: 10.13460/j.issn.1005-0957.2021.06.0715. [DOI] [Google Scholar]
- 119.Feng C. Q., Shen Y. J., Qin X. Z. Clinical curative observation on thunder-fire moxibustion combined with estradiol valerate and medroxyprogesterone in the treatment of premature ovarian failure with spleen-kidney Yang weakness and blood stasis syndrome. Journal of Guangxi Medical University . 2019;36:1619–1622. doi: 10.16190/j.cnki.45-1211/r.2019.10.016. [DOI] [Google Scholar]
- 120.Chi Y. Y. Clinical observation on premature ovarian failure treated by modified right-restoring pill, acupuncture and moxibustion combined with sequential therapy. World Chinese Medicine . 2019;14:2474–2478. [Google Scholar]
- 121.Wang Y., Yu H. M. Observation on the therapeutic effect of acupuncture and moxibustion combined with Chinese and western medicine on premature ovarian failure. Shanghai Journal of Acupuncture and Moxibustion . 2018;37(09):1042–1046. doi: 10.13460/j.issn.1005-0957.2018.09.1042. [DOI] [Google Scholar]
- 122.Xie Y., Cheng F., Shi W. H., et al. Clinical observation on acupuncture combined with governor vessel moxibustion in treating premature ovarian failure of liver-kidney Yin deficiency syndrome. World Journal of Integrated Traditional and Western Medicine . 2020;15:943–945. doi: 10.13935/j.cnki.sjzx.200537. [DOI] [Google Scholar]
- 123.Hu J. L., Xiao S. F., Zhu L. J. Analysis of the clinical effect of Chinese herbs for Tonifying kidney and liver combined with acupuncture and sex hormone sequential therapy on premature ovarian failure. Jiangxi Journal of Traditional Chinese Medicine . 2021;52:55–57. [Google Scholar]
- 124.Luo J. J., Li H., Liu D. Z. Clinical observation on electroacupuncture combined with Bushen Huoxue recipe in treating 30 cases of premature ovarian failure of kidney deficiency and blood stasis syndrome. Guiding Journal of Traditional Chinese Medicine and Pharmacy . 2015;21:46–48. doi: 10.13862/j.cnki.cn43-1446/r.2015.06.015. [DOI] [Google Scholar]
- 125.Fang Q. X., Zou P., Chen R. X., Chen D. Q. Clinical study of Bushen Shugan decoction combined with electroacupuncture on 32 cases of premature ovarian failure with kidney deficiency and liver depression syndrome. Shandong Journal of Traditional Chinese Medicine . 2016;35:294–296. doi: 10.16295/j.cnki.0257-358x.2016.04.008. [DOI] [Google Scholar]
- 126.Chen M., Chen L. H., Tian X. P., Chen X. L. Clinical observation on acupoint catgut embedding therapy for premature ovarian failure. Shanghai Journal of Acupuncture and Moxibustion . 2017;36:697–701. doi: 10.13460/j.issn.1005-0957.2017.06.0697. [DOI] [Google Scholar]
- 127.Bian X. H., An Y., Chen J. J. Clinical observation on acupoint catgut embedding therapy for premature ovarian failure. Journal of Guangxi University of Chinese Medicine . 2016;19:19–21. [Google Scholar]
- 128.Chen J., Tang G. J., Tang H. Y., et al. Clinical study on Chinese herbs for Tonifying kidney and soothing liver combined with acupoint catgut embedding in treating premature ovarian failure. Acta Chinese Medicine and Pharmacology . 2019;47(02):112–115. doi: 10.19664/j.cnki.1002-2392.190063. [DOI] [Google Scholar]
- 129.Luo W. X., Xu M. J., Zhu X. P., et al. Clinical observation on acupoint catgut embedding combined with kuntai capsule in treating premature ovarian failure. Journal of North Sichuan Medical College . 2020;35(02):264–266. [Google Scholar]
- 130.Yu G. Y., Chen J. Observation on the therapeutic effect of Bushen Yanggan decoction combined with catgut embedding at acupoint on premature ovarian failure and its influence on serum follicle-stimulating hormone and estradiol levels. Chinese Journal of Primary Medicine and Pharmacy . 2019;26(01):65–69. [Google Scholar]
- 131.Tan X. M., Fei L. B., Yu C. C., Lan S. Z. Clinical observation on acupoint catgut embedding combined with western medicine in treating premature ovarian failure. Hebei Journal of Traditional Chinese Medicine . 2017;39:1089–1092. [Google Scholar]
- 132.Zhong H. Y., Yang L. L., Shen S. M., Xiao X. F. Clinical study on auricular point combined with traditional Chinese medicine in treating premature ovarian failure. Guangming Journal of Chinese Medicine . 2018;33:2369–2371. [Google Scholar]
- 133.Shen X. P. Clinical observation on auricular point combined with modified guishen pills in treating premature ovarian failure. Journal of Hubei University of Chinese Medicine . 2019;21:83–85. [Google Scholar]
- 134.Ye J. L., Xing T. L. Clinical observation on Qingxin Jianpi decoction combined with auricular point pill pressing in treating premature ovarian failure. Chinese Journal of Traditional Medical Science and Technology . 2018;25(01):69–70. [Google Scholar]
- 135.Huang C. L. Effect of targeted nursing on adverse mood of patients with premature ovarian failure. Electronic Journal of Practical Gynecological Endocrinology . 2019;6:p. 158. doi: 10.16484/j.cnki.issn2095-8803.2019.24.119. [DOI] [Google Scholar]
- 136.He J. Q. Analysis of the role of psychological nursing in the clinical nursing of patients with premature ovarian failure. Electronic Journal of Practical Gynecological Endocrinology . 2019;6 doi: 10.16484/j.cnki.issn2095-8803.2019.10.107. [DOI] [Google Scholar]
- 137.Wu L. Q. Value of psychological nursing in nursing care of patients with premature ovarian failure. Guide of China Medicine . 2021;19:160–161. doi: 10.15912/j.cnki.gocm.2021.35.067. [DOI] [Google Scholar]
- 138.Cui X. R., Li M. R., Qin Z. To explore the traditional Chinese medicine psychosomatic treatment of premature ovarian failure based on the idea of regulating Qi. Yunnan Journal of Traditional Chinese Medicine and Materia Medica . 2021;42:9–12. doi: 10.16254/j.cnki.53-1120/r.2021.10.004. [DOI] [Google Scholar]
- 139.Chen L., Wang X. Y. Clinical effect of psychosomatic therapy on menstrual disorder in women with decreased ovarian reserve. Journal of Guangdong Pharmaceutical University . 2014;30:514–516. [Google Scholar]
- 140.Cao J. H. Clinical effect of traditional Chinese medicine psychosomatic therapy on menstrual disorder in women with decreased ovarian reserve. China Continuing Medical Education . 2016;8:180–181. [Google Scholar]
- 141.Wang B. Y. Evaluation of the effect of estrogen and progestogen combined with psychological counseling in the treatment of premature ovarian failure. Practical Clinical Journal of Integrated Traditional Chinese and Western Medicine . 2016;16:68–70. doi: 10.13638/j.issn.1671-4040.2016.09.037. [DOI] [Google Scholar]
- 142.Ma X. Y., Feng M. Y., Li Y. F. Effect research of estrogen and progestogen combined with psychological counseling in the treatment of premature ovarian failure. Electronic Journal of Practical Gynecological Endocrinology . 2019;6:p. 74. doi: 10.16484/j.cnki.issn2095-8803.2019.27.056. [DOI] [Google Scholar]
- 143.Yu F., Jiang T., Zhao J. J. Effect of estrogen and progestogen combined with psychological counseling in the treatment of premature ovarian failure. China Medical Herald . 2015;12:65–69. [Google Scholar]
- 144.Xu R. P., Zhang X. W., Zhao G. C. Research progress of exercise in improving physical and mental health. Gansu Medical Journal . 2013;32:422–424. doi: 10.15975/j.cnki.gsyy.2013.06.001. [DOI] [Google Scholar]
- 145.Wang Z. L., Cui J. M., Zhou C. F., et al. Effects of treadmill running on depression-like behavior, hippocampal inflammatory factors and nNOS expression in CA1 and CA3 regions of hippocampus in ovariectomized rats. Sports Research and Education . 2021;36:91–96. doi: 10.16207/j.cnki.2095-235x.2021.06.016. [DOI] [Google Scholar]
- 146.Wu S. Z., Chen Y., Xu H. Y. Clinical study of Baduanjin exercise prescription in the treatment of ovarian reserve hypofunction. Journal of External Therapy of Traditional Chinese Medicine . 2020;29:3–5. [Google Scholar]
- 147.Qin Y. T., Wei L. X. Effect of exercise intervention combined with progressive relaxation training on psychological status of patients with premature ovarian failure. Nursing Practice and Research . 2017;14:77–78. [Google Scholar]
- 148.Hou Y. Effect of vitamin E combined with hormone supplementation therapy on endocrine function in patients with premature ovarian failure. Electronic Journal of Practical Gynecological Endocrinology . 2020;7:10–11. doi: 10.16484/j.cnki.issn2095-8803.2020.03.008. [DOI] [Google Scholar]
- 149.Wang H. B., Li Y. W., Ding Y. L. Effect of vitamin E combined with hormone supplement therapy on endocrine and reproductive function in patients with premature ovarian failure. Chinese Journal of Coal Industry Medicine . 2021;2:204–208. [Google Scholar]
- 150.Zou Y. J., Yin T. L., Li J., Wang Y. Q., Xu W. M., Yang J. Effect of coenzyme Q10 combined with vitamin E on ovarian function and IVF outcome in elderly women. Journal of Reproductive Medicine . 2017;26:1028–1034. [Google Scholar]
- 151.Wang Q. K., Wu L. H., Liu H. R. Investigation of osteoporosis in patients with premature ovarian failure of different ages and analysis of combined prevention and treatment of calcium tablets, calcitriol and vitamin D. Maternal and Child Health Care of China . 2018;33:3289–3291. [Google Scholar]
- 152.Liu Y. To evaluate the effect of Bushen Tiaojing decoction combined with acupoint massage in the treatment of 30 patients with kidney deficiency syndrome premature ovarian failure. Contemporary Medical Symposium . 2017;15:188–189. [Google Scholar]
- 153.Wu Z. X., Li C. D., Zhang L. H. 59 cases of premature ovarian failure treated by Yishen Huoxue decoction combined with massage. Liaoning Journal of Traditional Chinese Medicine . 2010;37(08):1533–1534. doi: 10.13192/j.ljtcm.2010.08.130.wuchx.031. [DOI] [Google Scholar]
- 154.Feng X. J., Sun W., Wang L. Observation on therapeutic effect of electroacupuncture combined with pelvic floor muscle massage on premature ovarian failure. Journal of Shandong University of Traditional Chinese Medicine . 2011;35(01):43–44. doi: 10.16294/j.cnki.1007-659x.2011.01.012. [DOI] [Google Scholar]
- 155.Silvestris E., Lovero D., Palmirotta R. Nutrition and female fertility: an interdependent correlation. Frontiers in Endocrinology . 2019;10 doi: 10.3389/fendo.2019.00346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Chen H., Cheng R., Xu L. Z. Correlation between dietary nutrition and premature ovarian failure. Sichuan da Xue Xue Bao. Yi Xue Ban=Journal of Sichuan University. Medical Science Edition . 2017;48(4):575–578. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data were used to support the findings of this study.


