Abstract
Background
There are multiple hematological and other entities (metastases, infections) that can affect the bone marrow (BM). The gold standard imaging technique for BM examination is magnetic resonance imaging (MRI). Technological advances have made it possible to digitalize image files and create applications that help to produce higher quality structured reports, facilitating the analysis of data and unifying the criteria collected, making it possible to fill an existing gap. The aim of this study is to present a structured report model applicable to BM studies by MRI.
Methods
We have carried out a systematic review following the recommendations of the PRISMA checklist report to explore previous publications applying structured BM MRI reporting. Eligibility criteria: the selection of articles carried out by MeSH thesaurus. Original or review articles of BM pathology assessed by MRI. Our group with a wide experience in the evaluation of BM by MRI have designed a model for BM report using eight items: demographic data, diagnostic suspicion, technical data, type of exam initial or control, distribution and patterns involvement, complications and location, total assessment comments.
Results
We have not found articles that reflect the existence of a structured report of BM examination by MRI. Only one descriptive article has been identified on guidelines for acquisition, interpretation and reporting which refers to a single entity. With the selected parameters, a software has been developed that allows to fill in the sections of the structured report with ease and immediacy and to send the result directly to the clinician.
Discussion
Structured reports are the result of applying a logical structure to the radiological report, and the rules of elaboration comprise several criteria: (I) using a uniform language. The standardization of terminology avoids ambiguity in reporting and makes it easier to compare reports. (II) Accurately describe the radiological findings, following a prescribed order with review questions and answers. (III) Drafting using diagnostic screening tables. (IV) Respect the radiologists’ workflow by facilitating the work and not hindering it. The final report of this work has been the product of the clinical-radiological collaboration in our working group.
Keywords: Template report, structured form, magnetic resonance imaging (MRI), bone marrow patterns
Introduction
The bone marrow (BM) is a large organ that has remained hidden from diagnostic imaging; its study is dependent on biopsy puncture, which provides a limited view at the point of collection and does not allow to have an overview of the extent of involvement or the diversity of the pattern distribution (1).
The introduction of magnetic resonance imaging (MRI) as a tool for assessing tissue relaxation has made it possible to differentiate between the BM content. MRI allows the assessment of maturation and different pathophysiological mechanisms of medullary involvement (infiltration, ischemia, aplasia, edema, medullary reconversion), but given the enormous variability in its normality patterns, it requires training and uniformity in the description of its assessment by the radiologist (2).
BM involvement requires a precise and detailed assessment in the MRI report; a structured report allows the descriptive information in both situations in the initial diagnosis and in the follow-up controls to evaluate the response to therapy. This information is an essential part of specifying the staging and evolution of the patient with different hematological diseases, metastases and other entities that affect this organ, as well as lysosomal diseases (2,3).
The radiology report is the main communication tool between radiologists and clinicians and is the most important contribution of the radiologist in assisting in the evaluation of the patient (4,5). There are different types of radiological report, the most important being the free report, or traditional report, and the structured report. The free-text radiology report has a great variability in structure, content and style. It is simple and spontaneous, but sometimes abstract outside the radiological world and difficult to enter into a database for computer handling (6).
Traditionally the radiological report cycle consists of several phases, which can be summarized as (I) acceptance of the request and planning of the examination, (II) performance and quality control, (III) image processing and analysis, (IV) report writing and validation, and (V) transmission of the report and associated images together with their subsequent archiving (7).
The lack of unified criteria in free radiological reports makes it difficult to compare and transfer data on a day-to-day basis. Technological advances in the last few decades have enabled the digitalization of image archives and various applications have been developed to help to interpret and communicate examination results in a standardized way to produce higher quality structured reports (8).
An example of this are structured reporting systems that include text modules with specialized terminology from different organ systems and allow for risk characterization and stratification through scoring systems in different pathologies, such as, BI-RADS, TI-RADS, LI-RADS, PI-RADS and in recent months the CO-RADS in the COVID-19 disease (9,10).
The aim of this study is to present a structured report model applicable to BM studies by MRI. We present the following article in accordance with the PRISMA reporting checklist (available at https://qims.amegroups.com/article/view/10.21037/qims-21-1191/rc) (11).
Methods
A literature search was conducted from the earliest record until October 2021 to identify studies published using the PubMed, EMBASE, Science Open, Mendeley and Web of Science.
Eligibility criteria
The inclusion and exclusion criteria are listed in Table 1. The inclusion criteria used for the selection of articles has been carried out by MeSH thesaurus: all published original or review articles, the object of study was BM pathology assessed by MRI and the use of structured radiological reports. Isolated case reports were excluded. Files were selected and narrowed down to those that met the eligibility criteria.
Table 1. Inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria |
|---|---|
| The selection of articles has been carried out by MeSH thesaurus | Isolated case reports |
| Original or review articles of bone marrow pathology assessed by magnetic resonance imaging | Non-MRI exam included |
| Structured radiological reports used | Non-bone marrow articles |
All articles in any language but with abstract available in English.
In no case was an article identified that included a structured BM report, so we extended the search to those articles that included systems for assessing BM involvement.
Search strategy
The PubMed, Embase, Science Open, Mendeley and Web of Science databases were electronically searched for relevant papers published up to October 2021, without language limitations. English descriptors were adapted according to the database. The following search strategy were entered into the database, (“radiology structured reporting” OR “radiology structured form” OR “radiology templates report” OR “radiology information systems”) AND (“magnetic resonance imaging”) AND (“bone marrow”). Three independent reviewers collected data searching in the databases and read all the summaries included in an excel file independently and then exchanged their evaluations, according the eligibility criteria detailed in Table 1.
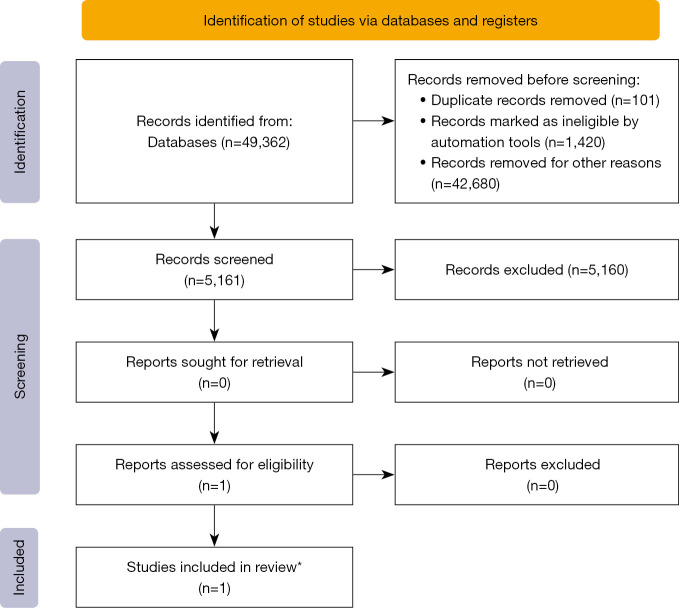
A secondary manual search of the reference lists of the relevant articles was also carried out. In addition to these database searches, numerous permutations of our search terms (Keywords: bone marrow patterns, MRI, structured reporting, template report, structured form) were entered into Google Scholar and thoroughly searched for any additional articles not found in the database searches. In total, we identified 49,362 studies of which met the eligibility criteria 5,161 (Figure 1).
Figure 1.
PRISMA flowchart of study selection. *, it is not a structured reporting template because the objective is to establish the extent of disease in a single entity.
Based on the need for a structured BM report for MRI study and on the experience accumulated over more than 25 years in the evaluation of BM using MRI, a report has been prepared taking into account the items reflected in Table 2.
Table 2. The preparation of a structured bone marrow report takes into account.
| (I) Demographic data |
| (II) Diagnostic suspicion |
| (III) Technical data |
| (IV) Initial or control examination |
| (V) The distribution and patterns of involvement of the BM according to the development and maturation related to the age and sex of the patient |
| (VI) The existence of complications defined as the phenomena of ischemia, edema, fracture and joint degeneration |
| (VII) Location |
| (VIII) Total assessment: diagnostic impression, comparative evolution |
Results
These searches returned no articles that reflect the existence of a structured BM report; only one descriptive article has been found on guidelines for acquisition, interpretation and reporting by means of whole-body MRI in Multiple Myeloma (12), which refers to a single entity Multiple Myeloma and the usefulness of MY-RADS for the diagnosis of extension and its therapeutic implication (Figure 1). Other articles refer to a semi-quantitative assessment of BM involvement by MRI by entities or by locations, but do not include a semiological description of the patterns of BM involvement required in a radiological report (13-17).
In the report (Figure S1), the sections numbered 1–5 corresponding to demographic data, time of study and technical characteristics. The sections 6–8 (Figure S1) correspond to the physiological distribution of the BM according to age and sex and the pathological patterns of focal or diffuse distribution described by Moulopoulos et al. (2). Section 9 (Figure S1) refers to the presence of possible complications secondary to the involvement such as infarcts, fractures, necrosis, secondary arthropathy, etc. Finally, Sections 10,11 (Figure S1) summarizes the final diagnosis with the findings detailed above.
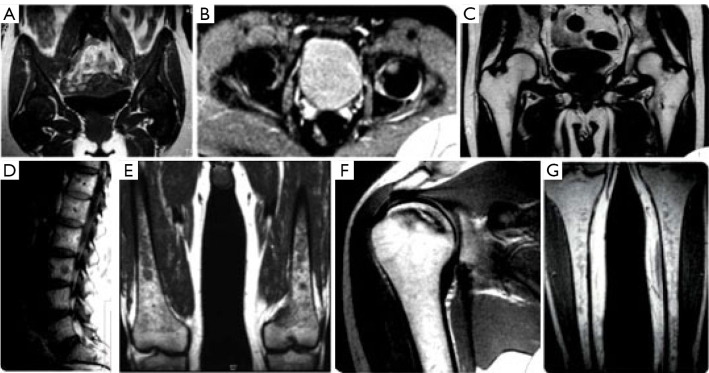
Imaging examples of parameters included in the structured MRI bone marrow assessment report are shown in Figure 2. The bone areas with the highest hematopoietic richness (lumbar spine, pelvis, femurs) are selected for the analysis of the infiltration pattern (18). For evaluation of sagittal spinal images, coronal pelvic images and both femurs, the following parameters are used: T1-WI (TR 600 ms TE 20 ms) and T2-WI (TR 2,500 ms TE 80 ms). The slice thickness was 3–5 mm, and the field of view 45 cm. The extension of involvement is reflected in section 7 of the report. Three MRI patterns and apply a point system in each location were defined: normal, 0; non-homogeneous infiltration subtypes reticular, 1; mottled, 2; diffuse, 3; and homogeneous infiltration 4. In addition, the types of complications are detailed, assigning an extra score of 4 for each type. The outline of the skeleton is used to detail the location and specify whether they are single or multiple.
Figure 2.
MRI images diversity of infiltration patterns and complications in bone marrow. [The images are provided by Dr. Mercedes Roca and are part of her publications “Magnetic Resonance Imaging of Bone Involvement in Gaucher Disease” ISBN 978-84-945315-7-6 (18) & “Resonancia Magnética en Enfermedades Hematológicas” ISBN 84-7885-275-1) (3). The publication of these books was her own initiative and that the images are of their property and they were not ceded to the publishers who published these books, with whom she had not signed any copyright agreement because the books were not copies for sale.] (A) SE T1 WI Coronal pelvis: Homogeneous pattern. No sign of fatty marrow. (B) SE T2 WI axial hips. Initial ischemic focus on the left femoral head. (C) SE T1WI Coronal hips: small foci of hematopoietic marrow around the lesser trochanter, in pelvis with abundant fatty marrow. (D) SE T1 WI Sagittal lumbar. Low signal infiltrative foci. Melanoma metastasis. (E) SE T1 WI Coronal distal femur. Medullary infiltration as mottled foci with preserved epiphyses. (F) SE T1 WI Coronal T1 shoulder: Bone infarction. Intramedullary ischemic area. (G) SE T1 WI Coronal tibias. Non-homogeneous reticular pattern. MRI, magnetic resonance imaging; SE, spin echo; T1 WI, T1 weighted imaging; T2WI, T2 weighted imaging.
The total sum reflects the overall assessment of the infiltration in the areas studied and the presence of complications is added to this score.
The result has been the creation of a structured radiological report document for the study of bone marrow pathology by MRI. A sample test in Spanish is included on the website of the Spanish Society of Musculoskeletal Radiology (SERME). The model is included as Figure S1.
Discussion
Traditionally, the radiology report has been a free text based on personal experience and sub-specialties, characterized by a lack of uniformity in writing. This gives it a wide variability in content and style and makes it difficult to integrate it into databases for subsequent comparison between studies or entities. Currently, the generalization of digital tools and systems in the radiological field has generated the need for a common radiological language applicable to the different organ-systems, which facilitates the sharing of information (19).
The aim of the structured report is to standardize information following a logical orderly protocol to increase the quality of radiological reports and provide better guidance to clinicians for daily clinical practice. In addition, the sharing of a common language between radiologists and between clinicians facilitates the comparison and analysis of data from registries for research purposes (20). Among the many strengths of the structured report is the minimization of errors and omissions in the description of radiological exams (21).
These aspects have long been discussed, with publications evaluating and discussing the need for quality standards in radiological reports dating back to the 1980s (22). The aim of these early publications was to define quality criteria for radiological reports (23). In 2007, the American College of Radiology (ACR) was one of the first major societies to publish the results of a consensus calling for more structured reporting. At the same time, the Radiological Society of North America (RSNA) developed and published RadLex, in order to unify the terms used in radiological reports (24,25). A few years later, different international societies have promoted the development of standardized templates allowing the integration and logical presentation of information, to facilitate the classification of different pathologies and increase the quality of radiological reports (26,27).
To date, we have not found any specific structured radiology report template for bone marrow MRI in the systematic review carried out. We have only identified one article dedicated to a specific bone marrow (Multiple Myeloma) disease with the aim of assessing the extent of the disease, so it is not possible to establish a discussion focused on the objective of our project, which is the standardization of the radiological report of bone marrow by MRI.
Standardized templates minimize variations in reports and avoid ambiguous terminology (28) and produce a relevant improvement in quality with more complete and accurate data especially in oncological pathology but also in different studies such as plain chest X-ray, shoulder MRI, pulmonary angiography and MRI in multiple sclerosis (29,30).
The report and data systems (RADS) are guidelines for the evaluation and interpretation of disease-oriented imaging studies such as BI-RADS. Recently has been published CO-RADS in COVID-19 disease, which has facilitated the stratification of disease severity and therapeutic management (31,32).
Structured reports are the result of applying a logical structure to the radiological report, and the rules of elaboration comprise several criteria: (I) using a uniform language, avoiding personal styles or existing institutional templates. The standardization of terminology avoids ambiguity in reporting and makes it easier to compare reports with each other. (II) Accurately describe the radiological findings, following a prescribed order with review of a list of questions and answers. (III) Drafting using diagnostic screening tables. (IV) Respect the radiologists' workflow by facilitating the work and not hindering it.
It is essential that radiologists understand the importance and added value of structured information, especially in order to be able to store report data and compare variables more objectively (2).
MRI has proved to be a useful tool for obtaining a global map of the contents of the bone marrow cavity and the applications of the technique to the study of different processes affecting the bone marrow. Assessment is often complex due to the presence of multiple patterns and their evolutionary change with age and disease. MRI allows distinguishing differences and abnormalities in different tissues reflecting the balance between the fat component and medullary hematopoietic cell component, providing a picture of the variations between these components within the bone cavity (33). This provides an answer in daily clinical practice, where situations of uncertainty are generated due to the lack of knowledge of the radiological semiology of the bone marrow, technical limitations in an extensive organ and variability in the maturation of the bone marrow tissue and its pathological affectation. This involves both diagnosis and follow-up in the face of differentiated therapeutic approaches.
The creation of structured radiological reports for the study of bone marrow is of great relevance in order to unify terms and provide the most objective assessment possible. Our experience is based on a long history of assessing bone marrow involvement in different hematological entities (see Table S1 with references the articles related our experience in bone marrow MRI) and the previous design of scores for assessing bone marrow infiltration applied mainly to bone involvement in Gaucher disease as a starting point for the preparation of this structured report (16).
We have developed this specific structured report for the assessment of bone marrow involvement which we have applied in a cohort of 430 studies of patients with Gaucher disease. This structured report is applicable to any bone marrow pathology allowing the characterization of the different patterns of marrow infiltration, description and localization of complications and differentiation between single and multiple lesions.
In general, the elaboration of a structured report template in a specific disease requires that all radiologists and clinicians involved in that pathology can participate in its elaboration in order to address the needs and key points. The final report of this work has been the product of the clinical-radiological collaboration of our working group (GEEDL).
In addition, radiological societies should be involved in the use of these structured reports and encouraged to use them as part of the quality audits in radiology services. A sample test of the report in Spanish is included on the website of the Spanish Society of Musculoskeletal Radiology (SERME) (34).
Conclusions
We present a structured report template for the preparation of bone marrow MRI studies that serves to standardize the information provided by the exam, increasing the quality of radiology reports, and facilitating professional networking and knowledge dissemination in the era of digitalization of medicine.
Acknowledgments
Funding: The Spanish Foundation (FEETEG) supported the infrastructure to perform the review and the structured model (No. 21/003).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Footnotes
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://qims.amegroups.com/article/view/10.21037/qims-21-1191/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-21-1191/coif). PG reports that this study received grants from Sanofi and honoraria from Takeda for educational events, but all amounts are received for Spanish Foundation to study and therapy of Gaucher disease and other lysosomal disorders to contribute to research activities. The other authors have no conflicts of interest to declare.
References
- 1.Hernandez Nieto L. Biopsia de la medula ósea. Perspectiva clínica-patológica. 2º Edición. Sociedad Española de Hematología y Hemoterapia. Madrid 2017. ISBN: 978-84-697-6855-6. [Google Scholar]
- 2.Moulopoulos LA, Dimopoulos MA. Magnetic resonance imaging of the bone marrow in hematologic malignancies. Blood 1997;90:2127-47. 10.1182/blood.V90.6.2127 [DOI] [PubMed] [Google Scholar]
- 3.Giraldo P, Roca M, Rubio-Felix D. Resonancia Magnética en enfermedades hematológicas. Aula Medica Ediciones. Madrid 2001. ISBN: 84-7885-275-1. [Google Scholar]
- 4.European Society of Radiology (ESR) . ESR paper on structured reporting in radiology. Insights Imaging 2018;9:1-7. 10.1007/s13244-017-0588-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nobel JM, van Geel K, Robben SGF. Structured reporting in radiology: a systematic review to explore its potential. Eur Radiol 2022;32:2837-54. 10.1007/s00330-021-08327-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nobel JM, Kok EM, Robben SGF. Redefining the structure of structured reporting in radiology. Insights Imaging 2020;11:10. 10.1186/s13244-019-0831-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Caicedo Montaño CA, Martínez de los Ríos RA, Mantilla Espinosa R, Dávila Valdés CP. How and Why to Migrate to Radiology Structured and Contextualized Report? Rev. Colomb. Radiol 2019; 30: 5194-98 [Google Scholar]
- 8.Aiello M, Esposito G, Pagliari G, et al. How does DICOM support big data management? Investigating its use in medical imaging community. Insights Imaging 2021;12:164. 10.1186/s13244-021-01081-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Segrelles JD, Medina R, Blanquer I, et al. Increasing the Efficiency on Producing Radiology Reports for Breast Cancer Diagnosis by Means of Structured Reports. A Comparative Study. Methods Inf Med 2017;56:248-60. 10.3414/ME16-01-0091 [DOI] [PubMed] [Google Scholar]
- 10.Rubin GD, Ryerson CJ, Haramati LB, et al. The Role of Chest Imaging in Patient Management During the COVID-19 Pandemic: A Multinational Consensus Statement From the Fleischner Society. Chest 2020;158:106-16. 10.1016/j.chest.2020.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. J Clin Epidemiol 2021;134:178-89. 10.1016/j.jclinepi.2021.03.001 [DOI] [PubMed] [Google Scholar]
- 12.Messiou C, Hillengass J, Delorme S, et al. Guidelines for Acquisition, Interpretation, and Reporting of Whole-Body MRI in Myeloma: Myeloma Response Assessment and Diagnosis System (MY-RADS). Radiology 2019;291:5-13. 10.1148/radiol.2019181949 [DOI] [PubMed] [Google Scholar]
- 13.Rosenthal DI, Scott JA, Barranger J, et al. Evaluation of Gaucher disease using magnetic resonance imaging. J Bone Joint Surg Am 1986;68:802-8. 10.2106/00004623-198668060-00002 [DOI] [PubMed] [Google Scholar]
- 14.Terk MR, Esplin J, Lee K, et al. MR imaging of patients with type 1 Gaucher's disease: relationship between bone and visceral changes. AJR Am J Roentgenol 1995;165:599-604. 10.2214/ajr.165.3.7645477 [DOI] [PubMed] [Google Scholar]
- 15.Maas M, Poll LW, Terk MR. Imaging and quantifying skeletal involvement in Gaucher disease. Br J Radiol 2002;75 Suppl 1:A13-24. 10.1259/bjr.75.suppl_1.750013 [DOI] [PubMed] [Google Scholar]
- 16.Roca M, Mota J, Alfonso P, et al. S-MRI score: A simple method for assessing bone marrow involvement in Gaucher disease. Eur J Radiol 2007;62:132-7. 10.1016/j.ejrad.2006.11.024 [DOI] [PubMed] [Google Scholar]
- 17.Poll LW, Cox ML, Godehardt E, et al. Whole body MRI in type I Gaucher patients: evaluation of skeletal involvement. Blood Cells Mol Dis 2011;46:53-9. 10.1016/j.bcmd.2010.10.005 [DOI] [PubMed] [Google Scholar]
- 18.Roca-Espiau M. Magnetic Resonance Imaging of Bone Involvement in Gaucher Disease. YOU&US, S.A. Edit. Madrid 2016. ISBN: 978-84-945315-7-6. [Google Scholar]
- 19.Ganeshan D, Duong PT, Probyn L, et al. Structured Reporting in Radiology. Acad Radiol 2018;25:66-73. 10.1016/j.acra.2017.08.005 [DOI] [PubMed] [Google Scholar]
- 20.Boland GW, Duszak R, Jr. Structured Reporting and Communication. J Am Coll Radiol 2015;12:1286-8. 10.1016/j.jacr.2015.08.001 [DOI] [PubMed] [Google Scholar]
- 21.Sarwar A, Boland G, Monks A, et al. Metrics for Radiologists in the Era of Value-based Health Care Delivery. Radiographics 2015;35:866-76. 10.1148/rg.2015140221 [DOI] [PubMed] [Google Scholar]
- 22.Clinger NJ, Hunter TB, Hillman BJ. Radiology reporting: attitudes of referring physicians. Radiology 1988;169:825-6. 10.1148/radiology.169.3.3187005 [DOI] [PubMed] [Google Scholar]
- 23.Hall FM. Language of the radiology report: primer for residents and wayward radiologists. AJR Am J Roentgenol 2000;175:1239-42. 10.2214/ajr.175.5.1751239 [DOI] [PubMed] [Google Scholar]
- 24.Dunnick NR, Langlotz CP. The radiology report of the future: a summary of the 2007 Intersociety Conference. J Am Coll Radiol 2008;5:626-9. 10.1016/j.jacr.2007.12.015 [DOI] [PubMed] [Google Scholar]
- 25.Rubin DL. Creating and curating a terminology for radiology: ontology modeling and analysis. J Digit Imaging 2008;21:355-62. 10.1007/s10278-007-9073-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morgan TA, Helibrun ME, Kahn CE, Jr. Reporting initiative of the Radiological Society of North America: progress and new directions. Radiology 2014;273:642-5. 10.1148/radiol.14141227 [DOI] [PubMed] [Google Scholar]
- 27.European Society of Radiology (ESR) . Good practice for radiological reporting. Guidelines from the European Society of Radiology (ESR). Insights Imaging 2011;2:93-6. 10.1007/s13244-011-0066-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.An JY, Unsdorfer KML, Weinreb JC. BI-RADS, C-RADS, CAD-RADS, LI-RADS, Lung-RADS, NI-RADS, O-RADS, PI-RADS, TI-RADS: Reporting and Data Systems. Radiographics 2019;39:1435-6. 10.1148/rg.2019190087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Flusberg M, Ganeles J, Ekinci T, et al. Impact of a Structured Report Template on the Quality of CT and MRI Reports for Hepatocellular Carcinoma Diagnosis. J Am Coll Radiol 2017;14:1206-11. 10.1016/j.jacr.2017.02.050 [DOI] [PubMed] [Google Scholar]
- 30.Marcovici PA, Taylor GA. Journal Club: Structured radiology reports are more complete and more effective than unstructured reports. AJR Am J Roentgenol 2014;203:1265-71. 10.2214/AJR.14.12636 [DOI] [PubMed] [Google Scholar]
- 31.Lieveld AWE, Azijli K, Teunissen BP, et al. Chest CT in COVID-19 at the ED: Validation of the COVID-19 Reporting and Data System (CO-RADS) and CT Severity Score: A Prospective, Multicenter, Observational Study. Chest 2021;159:1126-35. 10.1016/j.chest.2020.11.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Verdú-Díaz J, Alonso-Pérez J, Nuñez-Peralta C, et al. Accuracy of a machine learning muscle MRI-based tool for the diagnosis of muscular dystrophies. Neurology 2020;94:e1094-102. 10.1212/WNL.0000000000009068 [DOI] [PubMed] [Google Scholar]
- 33.Giraldo P, Roca-Espiau M. La resonancia magnética frente a la biopsia medular cómo método de estudio de la médula ósea en diferentes situaciones. En Biopsia de la médula ósea. Perspectiva clínico-patológica. L Hernandez-Nieto Ed. Fundación Española de Hematología y Hemoterapia. Madrid, 2017:187-203. [Google Scholar]
- 34.Available online: www.serme.es/wp-content/uploads/2020/11/INFORME-ESTRUCTURADO-MO-Gaucher-1.pdf. Access 11 February 2022.