Abstract
Background:
Low retention is a persistent challenge in the delivery of buprenorphine treatment for opioid use disorder (OUD). The goal of this study was to identify provider factors that could drive differences in treatment retention while accounting for the contribution of patient characteristics to retention.
Methods:
We developed a novel a mixed-methods approach to explore provider factors that could drive retention while accounting for patient characteristics. We used Medicaid claims data from North Carolina in the United States to identify patient characteristics associated with higher retention. We then identified providers who achieved high and low retention rates. We matched high- and low-retention providers on their patients’ characteristics. This matching created high- and low-retention provider groups whose patients had similar characteristics. We then interviewed providers while blinded to which belonged in the high- and low-retention groups on aspects of their practice that could affect retention rates, such as treatment criteria, treatment cost, and services offered.
Results:
Less than half of patients achieved 180-day treatment retention with large differences by race and ethnicity. We did not find evidence that providers who achieved higher retention consistently did so by providing more comprehensive services or selecting for more stable patients. Rather, our findings suggest use of “high-threshold” clinical approaches, such as requiring participation in psychosocial services or strictly limiting dosages, explain differences in retention rates between providers whose patients have similar characteristics. All low-retention providers interviewed used a high-threshold practice compared to half of high-retention providers interviewed. Requiring patients to participate in psychosocial services, which were often paid out-of-pocket, appeared to be especially important in limiting retention.
Conclusion:
Providers who adopt low-threshold approaches to treatment may achiever higher retention rates than those who adopt high-threshold approaches. Addressing cost barriers and systemic racism are likely also necessary for improving buprenorphine treatment retention.
Keywords: buprenorphine, retention, mixed methods, low-threshold treatment
Introduction
A persistent challenge in the delivery of buprenorphine treatment for opioid use disorder (OUD) is low treatment retention (Martin et al., 2019; Williams et al., 2019). Despite longer retention in buprenorphine treatment being associated with lower mortality (Sordo et al., 2017), clinical studies yield highly variable buprenorphine retention rates (Timko et al., 2016). The National Quality Forum endorses retention in OUD pharmacotherapy for at least 180 days as a quality measure (National Quality Forum, 2017), but studies from real-world practice settings find relatively few patients attain this metric, ranging from 21% to 65% of patients (Gertner et al., 2020; Miotto et al., 2012; Neumann et al., 2013; Samples et al., 2018).
Both patient and provider characteristics likely contribute to differing retention rates across treatment settings and populations (Simpson, 2004). A multi-state study of Medicaid data in the United States (USA) found that patients with OUD who had an overdose history, recent inpatient care, hepatitis, and additional comorbid substance use disorders had higher risk of discontinuing buprenorphine treatment compared to those without these risk factors (Samples et al., 2018). These associations suggest patients with more severe OUD and comorbid conditions are less likely to be retained in treatment. Further, Black and Hispanic patients had higher risk of discontinuing than non-Hispanic White patients. Differences in social support, financial resources, and discriminatory systems, such as systemic racism, likely explain much of this variation by race and ethnicity (Jordan et al., 2020; Kunins, 2020).
By contrast, there is scant evidence of what provider factors are associated with improved retention. In a prior study, we used Medicaid claims data from North Carolina in the USA to find that primary care providers achieved similar retention rates as behavioral health providers but higher retention than pain specialists (Gertner et al., 2020). Retention differences between these provider groups could be driven by differences in patients’ characteristics (e.g., pain specialists treat sicker or more marginalized patients). Alternatively, some providers may achieve higher retention because they offer more comprehensive services or have superior clinical approaches to treatment. Several studies have documented substantial variation in buprenorphine providers’ treatment practices including urine drug testing frequency, office visit frequency, and buprenorphine dosages prescribed (Baxter et al., 2015; Knudsen et al., 2019; Yang et al., 2013). Regular office visits and receipt of any psychosocial treatment is associated in lower mortality in buprenorphine treatment, but it’s unclear if these relationships are causal (Watkins et al., 2017). Identifying the source of provider-level variation in patient retention could provide insight into how to increase retention rates; however, this cannot be accomplished using claims data alone.
The USA exerts strict regulatory control over buprenorphine in the treatment of OUD.(Kresina et al., 2009) While buprenorphine can be prescribed to treat pain by any provider licensed to prescribe controlled substances, providers have historically had to undergo additional training to obtain a waiver to prescribe buprenorphine for OUD. Buprenorphine can also be directly dispensed to patients for OUD treatment by federally regulated opioid treatment programs (OTPs). Only OTPs can dispense methadone for OUD treatment, typically requiring patients to travel to OTPs daily for dosing. Methadone cannot be prescribed to be picked up in a pharmacy for OUD treatment. For this reason, buprenorphine is far more accessible in the US than methadone.
In this study, we sought to identify provider factors, such as clinical approaches, policies, or services, that lead to improved retention. A challenge in studying how providers factors affect retention is that different types of providers may treat different groups of patients. Providers who offer more psychosocial support, for instance, may treat patients with fewer comorbid conditions, presenting a problem of confounding. The objective of this study was to explore factors that may drive differences in retention between providers while accounting for differences in their patients’ characteristics. We accomplished this through an innovative mixed-methods study design combining claims data analysis and provider interviews.
Methods
We conducted a mixed methods study using North Carolina Medicaid claims data and interviews with providers. North Carolina Medicaid is a joint state and federal program that covers medical costs for low-income individuals who are pregnant, disabled, elderly, or responsible for minors. Under the 2010 Affordable Care Act, US states had the option of expanding Medicaid to most low-income individuals living under 138% of the federal poverty line. North Carolina is among 12 US states that have opted not to expand Medicaid eligibility.(Kaiser Family Foundation, 2022) For this reason, the population in this study likely largely represents people with very low incomes who qualified for Medicaid through disability or by being parents of minors. During the study period, North Carolina Medicaid covered buprenorphine prescriptions, visits for OUD treatment, and behavioral health counseling. Healthcare providers are not required to accept Medicaid. Medicaid patients may pay out of pocket to see non-Medicaid providers, and prescriptions written by these providers for Medicaid enrollees could be paid for by Medicaid.
We accessed Medicaid claims and encounter data from North Carolina through the Carolina Cost and Quality Initiative from January 2014 to July 2018 for individuals 18 and older (The Carolina Cost and Quality Initiative, 2019). We used Medicaid claims to identify patient and provider characteristics associated with 180-day retention in treatment, as further described below. We then identified providers who achieved high and low retention in buprenorphine treatment. Using a purposeful sampling approach (Palinkas et al., 2015), we selected subgroups of high- and low-retention providers whose patients had similar characteristics. We did this to ensure that differences in retention between providers weren’t driven by observable patient characteristics. We interviewed providers from these groups to identify factors that could affect retention. We considered several hypotheses for how providers achieve higher retention, including that some providers select for more stable patients, offer more comprehensive services, deliver more intensive treatment, are more skilled clinicians, deliver lower-cost care, or offer more flexible treatment services.
We termed our mixed-methods approach of using quantitative methods to match a sub-group of our sample for subsequent qualitative inquiry “matched subgroup analysis” (see Supplementary Material 1). Our mixed-methods approach followed a quan → QUAL structure wherein there is sequential collection and analysis of quantitative and qualitative data (Palinkas, Aarons, et al., 2011; Palinkas, Horwitz, et al., 2011). The mixed-methods approach served the functions of complementarity, expansion, and sampling (Palinkas, Aarons, et al., 2011). That is, the methods used answered related questions, the qualitative methods provided insights into results from quantitative methods, and the quantitative methods provided a sampling basis for the qualitative methods. For combined analysis of quantitative and qualitative data, we followed a connecting process where qualitative data elaborated on quantitative data (Palinkas, Aarons, et al., 2011). This study was approved by the University of North Carolina Institutional Review Board for Human Subjects Research (17–2434).
Buprenorphine Treatment and Retention
We identified Medicaid enrollees with claims for buprenorphine formulations for OUD treatment. We defined buprenorphine treatment episodes as periods of continuous buprenorphine prescription coverage without more than a 30-day gap. We included in our analyses only the first observed treatment episode for each patient, so there is only one treatment episode per patient. Multiple providers may prescribe buprenorphine to a patient within an episode, so we assigned each episode to the provider prescribing the most buprenorphine prescriptions for the episode. As such, the provider sample represents the most-frequent buprenorphine prescribers for our patients treated with buprenorphine. We employed a binary measure of treatment retention as continuous receipt of buprenorphine for at least 180 days. We included in our analyses only treatment episodes that began between January 1, 2015 and December 31, 2017 to allow for 12-months of observation before episodes and 6 months of follow-up observation. We required patients to be Medicaid enrolled for at least 8 of the 12 months prior to the start of an episode and for all 6 months after the start of an episode, to ensure differences in prior healthcare use and retention between groups were not driven by differences in length of enrollment. We thus identified 7,956 buprenorphine patients and 513 prescribers in the claims data.
Patient and Provider Characteristics
Our selection of patient and provider characteristics was informed by Simpson’s conceptual framework for drug treatment process and outcomes (Simpson, 2004). Using claims data, we identified patients’ demographic characteristics including age, gender, race, ethnicity, and rural county of residence based on the United Stated Department of Agriculture categories for completely rural counties (United States Department of Agriculture, 2013). We identified whether patients had other comorbidities identified using non-diagnostic service claims for key physical, mental health, and substance use conditions using ICD codes in the 12-months before the start of treatment episodes. Inpatient or specialty service use may indicate more severe illnesses. We used Current Procedure Terminology (CPT) and revenue codes to quantify patients’ use of specialty substance use services, behavioral health (BH) services, inpatient medical services, and emergency services in the 12 months prior to the start of buprenorphine treatment episodes (see Supplementary Material 2 for codes) (American Medical Association, 2021).
We merged claims data with the National Plan & Provider Enumeration System (NPPES) to identify providers’ specialty, grouping providers as primary care providers (PCPs), BH specialists, pain specialists, and other providers. Primary care providers included general practitioners, family medicine physicians, non-specialized internal medicine physicians, non-specialized nurse practitioners, and non-specialized physician assistants. Regardless of providers’ primary specialty, we created a binary variable of whether the provider was identified as an addiction specialist in claims or NPPES. We determined providers’ gender using NPPES and whether they were in a rural county using claims data.
We also identified the treatment setting where providers delivered most services for people with OUD, including office settings, hospital-based clinics, or BH centers. BH centers included OTPs, federally or state certified community behavioral health clinics, or clinics specializing in mental health services. We also designed whether providers billed for services from a Medicaid patient-centered medical home (PCMH) when treating people with OUD. PCMHs may have additional resources compared to other primary care offices, such as case management, that may help patients remain in treatment.
Providers’ prior experience prescribing buprenorphine for OUD may affect the probability of a treatment episode reaching 180-day retention. As measures of provider experience, we counted how many patients providers treated with buprenorphine prior to each episode and how many days providers has been prescribing buprenorphine prior to each episode. We identified receipt of certain services during treatment episodes such as evaluation & management (E&M) visits, BH visits, and toxicology testing using approaches described elsewhere (Gertner et al., 2020).
Statistical Analysis
Our analytic dataset was comprised of buprenorphine treatment episodes starting between January 1, 2015 and December 31, 2017. Each episode represented a single patient and was associated with that patient’s characteristics. Similarly, every episode was associated with a prescribing provider’s characteristics. We used generalized estimation equations (GEE) to model the association between 180-day retention and patient characteristics or provider characteristics. GEE models allowed us to account for clustering of patients at the provider level in estimating standard errors. We used a logit link function, binomial distribution, and exchangeable correlation structure at the provider level for all models. We present average marginal effects with 95% confidence interval from delta method standard errors with two significant figures for statistical precision. To determine how well patient and provider characteristics predicted retention, we generated predicted probabilities of retention from our GEE models. We estimated the optimal cut-points for predicting retention using Liu’s method for maximizing the product of the sensitivity and specificity (Clayton, 2013; Liu, 2012). This procedure measures how well the predicted probabilities of our GEE model performs in accurately predicting sample retention. Analyses were performed using Stata 15 (College Station, TX).
Interview Sampling
We used a purposive sampling approach to identify high-retention and low-retention providers (Figure 1) (Palinkas et al., 2015). We identified 513 unique buprenorphine prescribers in our Medicaid claims data. To accurately observe providers’ retention rates, we dropped 106 providers who treated fewer than 5 patients. To focus on providers who were more likely to be actively prescribing, we dropped 75 providers who we did not observe prescribing buprenorphine in 2017. We divided providers into thirds by the percent of their patients who were retained in treatment for at least 180 days. We designated the bottom third of 111 providers as low-retention and the top third of 107 providers as high-retention.
Figure 1.
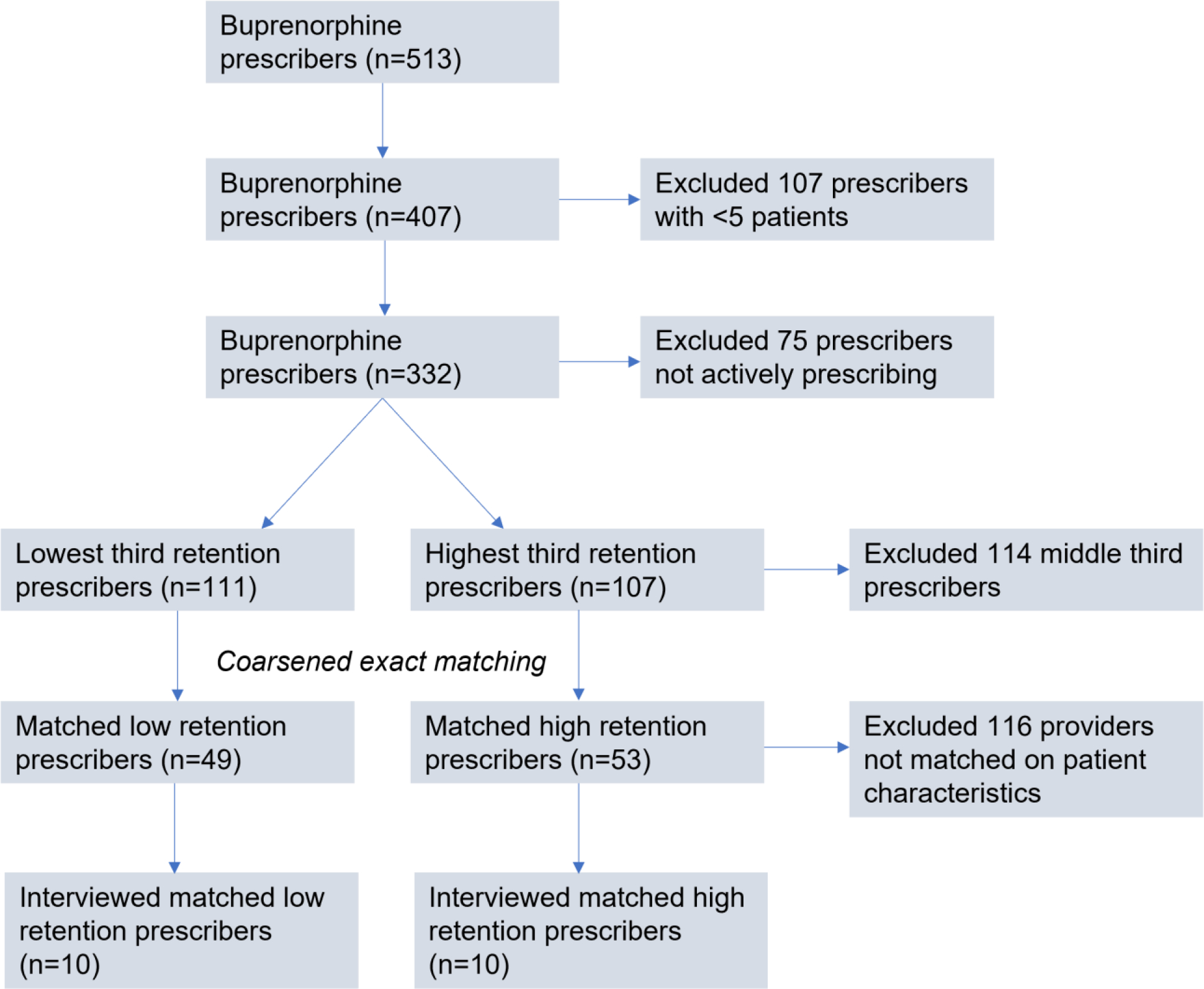
Interview sampling approach
Unsurprisingly, patient characteristics differed between high- and low-retention providers. To minimize the extent to which differences in retention rates were driven by patient characteristics, we identified subgroups of high- and low-retention providers whose patients had similar characteristics. We identified these subgroups using coarsened exact matching, a method for creating subgroups within samples that have similar characteristics for specified variables (Blackwell et al., 2009). Coarsened exact matching coarsens variables using a binning algorithm and then selects for observations from each group that fit into a stratum, dropping observations whose stratum does not contain one unit from each group. We treated patient characteristics as variables describing providers. The patient characteristics variables were coarsened using Sturge’s Rule (k = 1 + 3.322 log n, where k = the number of bins and n = the number of observations in the data set), and then providers from high and low retention groups were binned into strata of the coarsened variables. The excluded providers are those for whom patient characteristics may explain their differences in retention.
We matched the subgroups of high- and low-retention providers using the patient characteristics that were independently associated with retention in our GEE model of patient characteristics (Table 2 – column 1). This approach allowed us to focus interviews on providers whose differences in retention were likely not explained by observable differences in patient characteristics. We identified 49 low-retention and 53 high-retention providers whose patients had similar characteristics. Current contact information for three providers could not be found. We contacted the remaining 99 providers for interviews at least once but not more than twice by phone or email, offering $100 gift cards for participation.
Table 2.
Association of Patient and Provider Characteristics with 180-Day Retention
| Patient model | Provider model | Combined model | |
|---|---|---|---|
| Patient characteristics | |||
|
| |||
| Age | 0.00079 [−0.00051,0.0021] | 0.00078 [−0.00051,0.0021] | |
| Female | 0.052*** [0.026,0.078] | 0.052*** [0.026,0.078] | |
| Race (white ref) | |||
| Black | −0.11*** [−0.15,−0.067] | −0.11*** [−0.15,−0.064] | |
| Asian | −0.053 [−0.39,0.29] | −0.049 [−0.39,0.29] | |
| Two or more | 0.081 [−0.055,0.22] | 0.079 [−0.056,0.21] | |
| Unknown | −0.036 [−0.079,0.0076] | −0.029 [−0.072,0.014] | |
| Ethnicity (not Latino ref) | |||
| Latino | −0.11* [−0.21,−0.0097] | −0.11* [−0.21,−0.011] | |
| Unknown | −0.065* [−0.12,−0.012] | −0.065* [−0.12,−0.013] | |
| Rural | 0.025 [−0.0019,0.052] | 0.020 [−0.0074,0.048] | |
| Comorbidities | |||
| Opioid poisoning | −0.090*** [−0.12,−0.056] | −0.089*** [−0.12,−0.055] | |
| Depression | 0.0041 [−0.022,0.030] | 0.0048 [−0.021,0.031] | |
| Anxiety | 0.022 [−0.0068,0.051] | 0.020 [−0.0084,0.049] | |
| Bipolar disorder | −0.024 [−0.049,0.00068] | −0.025* [−0.049,−0.00027] | |
| Schizophrenia | −0.054** [−0.090,−0.018] | −0.052** [−0.088,−0.017] | |
| Alcohol use disorder | −0.021 [−0.047,0.0047] | −0.021 [−0.047,0.0048] | |
| Other substance use disorder | 0.018 [−0.013,0.049] | 0.016 [−0.015,0.047] | |
| HIV infection | −0.035 [−0.16,0.089] | −0.039 [−0.16,0.083] | |
| HCV infection | −0.023 [−0.052,0.0064] | −0.022 [−0.051,0.0064] | |
| Chronic pain | −0.0035 [−0.035,0.028] | −0.0043 [−0.035,0.026] | |
| Diabetes | 0.028 [−0.00075,0.056] | 0.028 [−0.00036,0.056] | |
| COPD | 0.018 [−0.0084,0.045] | 0.018 [−0.0079,0.045] | |
| CAD | −0.014 [−0.062,0.033] | −0.015 [−0.062,0.032] | |
| Healthcare use | |||
| Specialty SUD visits | 0.00030** [0.000083,0.00052] | 0.00031** [0.000096,0.00052] | |
| BH visits | 0.00045 [−0.00084,0.0017] | 0.00053 [−0.00074,0.0018] | |
| Emergency department visits | −0.0059*** [−0.0085,−0.0033] | −0.0057*** [−0.0083,−0.0031] | |
| Inpatient psychiatric stays | −0.0039 [−0.013,0.0050] | −0.0045 [−0.013,0.0043] | |
| Inpatient medical stays | 0.0051 [−0.0070,0.017] | 0.0060 [−0.0061,0.018] | |
| Provider Characteristics | |||
| Provider specialty (PCP ref) | |||
| BH specialist | −0.069** [−0.12,−0.021] | −0.069** [−0.12,−0.022] | |
| Pain specialist | −0.10** [−0.18,−0.024] | −0.095* [−0.17,−0.017] | |
| Other provider | −0.0093 [−0.088,0.069] | −0.0044 [−0.082,0.074] | |
| Female | −0.036 [−0.080,0.0078] | −0.037 [−0.081,0.0066] | |
| Setting (office ref) | |||
| Hospital | −0.13*** [−0.20,−0.067] | −0.12*** [−0.19,−0.051] | |
| BH center | −0.0077 [−0.064,0.049] | 0.00014 [−0.056,0.057] | |
| FQHC | 0.0024 [−0.080,0.085] | 0.021 [−0.061,0.10] | |
| Other setting | 0.12 [−0.030,0.26] | 0.11 [−0.038,0.25] | |
| Unknown | −0.0092 [−0.12,0.099] | −0.013 [−0.12,0.094] | |
| Addiction specialist | −0.00044 [−0.056,0.055] | 0.00065 [−0.054,0.056] | |
| PCMH | −0.031 [−0.075,0.013] | −0.032 [−0.076,0.012] | |
| Rural | 0.060* [0.0066,0.11] | 0.040 [−0.015,0.095] | |
| Days providing buprenorphine (100) | −0.00041 [−0.0049,0.0041] | −0.0013 [−0.0058,0.0032] | |
| Patients treated (100) | −0.015 [−0.040,0.010] | −0.012 [−0.037,0.013] | |
|
| |||
| Observations | 7953 | 7956 | 7953 |
Estimates are from generalized estimation equations models with logit link function, binomial distribution, and exchangeable correlation structure at the provider level. Marginal effects are presented with 95% confidence interval from delta method standard errors.
Provider Interviews
In developing our interview guide, we used Simpson’s conceptual framework for drug treatment process and outcomes to identify key constructs that could affect retention (Simpson, 2004). We then used our treatment guidelines and our knowledge of treatment to develop questions about specific program characteristics, provider practices, and provider beliefs that could affect retention (American Society of Addiction Medicine, 2015; Martin et al., 2018; Substance Abuse Mental Health Services Administration, n.d.). We piloted the interview guide with two addiction providers who were not in our study sample, making adjustments to ensure the guide’s comprehensiveness and clarity. The final interview guide addressed aspects of providers’ practice that could affect retention, including their criteria for prescribing buprenorphine, the psychosocial services they provided to buprenorphine patients, aspects of their clinical practice, their attitudes towards buprenorphine treatment, the cost of care, and their patients’ reasons for stopping buprenorphine (see Supplementary Material 3).
Some providers have proposed “low-threshold” buprenorphine treatment models that emphasize flexibility to improve accessibility and retention. However, consensus on what constitutes low-threshold treatment is lacking. To compare provider practices that may create barriers to retention, we identified five key high-threshold treatment practices based on Jakubowsky and Fox’s framework (Jakubowski & Fox, 2019). We counted whether providers engaged in any of these five high-threshold practices: conducting office or facility-based inductions, requiring psychosocial treatment as part of buprenorphine treatment, discharging patients in response to positive drug tests, discharging patients in response to missed visits, and encouraging shorter treatment duration.
We conducted interviews from September to November 2019 to investigate factors that may be driving different retention rates between providers. To guard against bias, authors were blinded to which group of providers were high and low retention. Interviews consisted of closed- and open-ended questions (see Supplementary Material 3 for interview questionnaire). All interviews were conducted by AKG in a structured manner emphasizing consistent presentation of questions to improve comparability between interviews. Follow-up questions were primarily pre-planned based on answers. Unplanned follow-up questions were used to seek clarification of answers. AKG was a graduate student at the time of interview with experience in interviewing addiction providers. No providers were known to AKG prior to interviews. AKG did not collect provider characteristics other than those listed in the interview questionnaire. Interviews were recorded and transcribed for analysis. Analysis took place concurrently with interviews. No new themes emerged by the 7th interview in each group, suggesting thematic saturation was reached. We continued contacting providers for interviews until we conducted 3 additional interviews with each group to ensure no additional themes arose (Guest, 2006). Of the 99 providers eligible for interviews, 20 participated, making the participate rate 20%.
Our analysis aimed to identify possible provider-level drivers of retention by comparing high- and low-retention providers. We followed a qualitative content analysis approach to analyzing interviews divided into immersion, reduction, and interpretation (Coffey & Atkinson, 1996; Forman & Damschroder, 2007). Immersion involves becoming deeply familiar with the data, reduction involves identifying essential information in the data, and interpretation involves making sense of the essential information. We developed some themes deductively based on known areas of common divergence in buprenorphine treatment practice, such as requiring psychosocial treatment components and frequency of urine drug testing. We developed other themes inductively based on providers’ answers, such as their motivations for providing buprenorphine treatment and their attitudes towards treatment effectiveness. We iteratively revised codes as interviews proceeded. AKG and HMC double-coded all interviews, resolving discrepancies through consensus (Forman & Damschroder, 2007; Harris et al., 2006). AKG and HMC also kept unstructured notes that were reviewed at each meeting to identify and clarify themes. To guard against bias, AKG and HMC were blinded as to which group was high and low retention while coding. Researchers were unblinded to the groups after coding was completed. We then organized data into code reports to develop matrices and interpretive summaries of the data (Forman & Damschroder, 2007; Miles & Huberman, 1994).
As noted above, we followed a connecting process for combined analysis of quantitative and qualitative data (Palinkas, Aarons, et al., 2011). We sought from the interviews insights that might explain the quantitative associations. We also noted factors that appeared linked to retention in interviews that could not be measured in the quantitative data.
Results
Characteristics Associated with Retention
The overall 180-day retention rate was 48% (see Supplementary Material 5 for distribution of episode lenthgs). Treatment episodes achieving 180-day retention differed from those that did not in numerous patient and provider characteristics (Table 1). In addition, treatment episodes that achieved 180-day retention had higher starting buprenorphine doses, more frequent urine drug testing, and less frequent BH visits (Table 1). Patients who achieved 180-day retention had on average 1.6 (SD 3.3) BH visits in the first 30 days of treatment compared to 1.9 (SD 3.6) among patient who did not achieved retention.
Table 1.
Patient, Provider and Treatment Episode Characteristics by 180-Day Retention
| Not Retained (4115) | Retained (3841) | p-value | |
|---|---|---|---|
| Patient demographics | |||
| Age | 35 (10) | 35 (9.6) | 0.16 |
| Female | 2956 (72%) | 2952 (77%) | <0.001 |
| Race | |||
| White | 3385 (82%) | 3319 (86%) | <0.001 |
| Black | 379 (9.2%) | 206 (5.4%) | |
| Asian | 5 (.12%) | 3 (.078%) | |
| Two or more | 23 (.56%) | 27 (.7%) | |
| Unknown | 323 (7.8%) | 286 (7.4%) | |
| Ethnicity | |||
| Not Hispanic | 3839 (93%) | 3670 (96%) | <0.001 |
| Hispanic | 54 (1.3%) | 31 (.81%) | |
| Unknown | 222 (5.4%) | 140 (3.6%) | |
| Rural | 1224 (30%) | 1303 (34%) | <0.001 |
| Co-morbidities (pre 12 months) | |||
| Opioid overdose | 579 (14%) | 340 (8.9%) | <0.001 |
| Depression | 2927 (71%) | 2712 (71%) | 0.61 |
| Anxiety | 3168 (77%) | 3013 (78%) | 0.12 |
| Bipolar disorder | 1474 (36%) | 1266 (33%) | 0.007 |
| Schizophrenia | 597 (15%) | 386 (10%) | <0.001 |
| Alcohol use disorder | 1156 (28%) | 900 (23%) | <0.001 |
| Other substance use disorder | 3490 (85%) | 3258 (85%) | 0.99 |
| HIV | 43 (1%) | 24 (.62%) | 0.040 |
| Hepatitis C | 789 (19%) | 637 (17%) | 0.003 |
| Chronic pain | 3505 (85%) | 3216 (84%) | 0.089 |
| Diabetes | 864 (21%) | 787 (20%) | 0.58 |
| Chronic obstructive pulmonary disease | 1125 (27%) | 1030 (27%) | 0.60 |
| Coronary artery disease | 296 (7.2%) | 219 (5.7%) | 0.007 |
| Healthcare Use (pre 12 months) | |||
| Specialty SUD visits | 14 (47) | 17 (57) | 0.004 |
| Behavioral health visits | 3.7 (9.9) | 3.5 (8.1) | 0.34 |
| Emergency visits | 3.5 (5.7) | 2.7 (4.1) | <0.001 |
| Inpatient psych stays | .41 (2.9) | .26 (3.1) | 0.030 |
| Inpatient med stays | .34 (1.8) | .25 (2.4) | 0.064 |
| Buprenorphine prescriber | |||
| Specialty | |||
| Primary care | 1919 (47%) | 1934 (50%) | <0.001 |
| Behavioral health | 1458 (35%) | 1275 (33%) | |
| Pain | 509 (12%) | 371 (9.7%) | |
| Other | 229 (5.6%) | 261 (6.8%) | |
| Addiction Specialist | 974 (23.7%) | 854 (22.2%) | 0.13 |
| Setting | |||
| Office | 2918 (70.9%) | 2808 (73.1%) | <0.001 |
| Hospital | 305 (7.4%) | 190 (4.9%) | |
| Behavioral health center | 623 (15.1%) | 535 (13.9%) | |
| Federally qualified health center | 166 (4.0%) | 177 (4.6%) | |
| Other | 33 (0.8%) | 56 (1.5%) | |
| Unknown | 70 (1.7%) | 75 (2.0%) | |
| Patient-centered medical home | 1761 (43%) | 1733 (45%) | 0.037 |
| Rural | 610 (15%) | 676 (18%) | <0.001 |
| Female | 1169 (28%) | 973 (25%) | 0.002 |
| Days provider observed prescribing buprenorphine prior to a treatment episode (100 days) | 8.7 (3.7) | 8.8 (3.6) | 0.17 |
| Numbers of patients treatment with buprenorphine prior to a treatment episode (100 patients) | 1.1 (1.1) | 1 (99) | 0.024 |
| Episode characteristics a | |||
| Starting daily dose (mg) | 14 (8.7) | 15 (6.5) | <0.001 |
| Visit frequency 30 day | 3.3 (3.5) | 3.2 (3.2) | 0.56 |
| Tox frequency 30 day | 2.5 (2.8) | 2.7 (2.9) | 0.005 |
| BH visit frequency 30 day | 1.9 (3.6) | 1.6 (3.3) | 0.003 |
Means, standard deviations, and Wald p-values are presented for continuous variables while counts, percentages, and chi-squared p-values are presented for categorical values.
Starting daily dose is the daily dose for the first buprenorphine prescription of the treatment episode. E&M visit frequency, toxicology frequency, and BH visits is the number of visits or tests in the first 30 days of an episode. These variables excluded episodes that lasted less than 30 days, but no other variables or analyses excluded such episodes.
Some of patient and provider characteristics remained independently associated with retention in adjusted analyses (Table 2). When controlling for other patient characteristics, Black and Hispanic patients had 11 percentage points lower probability of reaching 180-day retention compared to White and non-Hispanic patients, respectively (95% CI −0.15 to −0.067 and −0.21 to −0.0097, respectively) (Table 2 – Column 1). Female patients had a 5.2 percentage point (95% CI 0.026 to 0.078) higher probability of 180-day retention compared to male patients. Receiving care for opioid poisoning in the 12 months prior to starting buprenorphine was associated with a 9-percentage point (95% CI −0.12 to −0.056) lower probability of 180-day retention. Similarly, having a schizophrenia diagnosis in the 12 months prior to buprenorphine initiation was associated with a 5.4 percentage point (95% CI −0.090 to −0.018) lower probability of 180-day retention. Having more ED visits in the 12 months before treatment was associated with lower retention, while having more specialty SUD visits before treatment was associated with higher retention.
PCPs, office-based providers, and rural providers were more likely to have episodes that achieved 180-day retention when controlling for provider characteristics (Table 2 – column 2). When simultaneously controlling for all patient and provider characteristics, rural providers were no longer associated with higher retention, but all other associations from the previous models remained statistically significant with similar coefficients (Table 2 – column 3). Optimal cut points for predicted probabilities from Liu’s method correctly identified 180-day retention with 57% sensitivity and 55% specificity using the patient characteristics model, 53% sensitivity and 57% specificity using the provider characteristics model, and 56% sensitivity and 59% specificity using the combined model.
The coarsened exact matching procedure was successful in eliminating statistically significant differences between high- and low-retention providers for all patient characteristics except rates of anxiety disorder and chronic pain (Supplementary Material 4), neither of which were independently associated with retention. We identified 49 low-retention and 53 high-retention matched providers. High-retention providers were still more likely to be PCPs after matching on patient characteristics. High-retention providers’ episodes also had fewer BH visits in the first 30 days.
Treatment Experience and Services
We interviewed 10 high-retention and 10 low-retention providers regarding factors that could explain differences in retention (Table 3). We asked providers about their experience providing buprenorphine treatment and characteristics of their treatment programs that could affect retention. Providers with more treatment experience may be more skilled in retaining patients. However, we found that high-retention providers on average started prescribing buprenorphine more recently than low-retention prescribers (4.5 years vs. 8 years). Both groups on average reported currently treating a similar number of patients (120 for high-retention and 110 for low-retention providers).
Table 3.
Provider responses to key constructs by provider subgroup
| Low-retention providers (n=10) | High-retention providers (n=10) | |
|---|---|---|
| Treatment Experience and Services | ||
| Time providing treatment | 8 years | 4.5 years |
| Number of patients treating | 110 patients | 120 patients |
| On-site psychological services | 8 | 5 |
| Peer support or case-management | 4 | 2 |
| Accept Medicaid | 8 | 5 |
| Motivated by need for treatment | 4 | 8 |
| Motivated by professional opportunities | 7 | 4 |
| Clinical practices | ||
| Select for stable patients | 5 | 5 |
| Urine testing every visit | 8 | 5 |
| Max 16 mg dose | 6 | 3 |
| Used any high-threshold practice | 10 | 5 |
| Office or facility-based induction | 5 | 3 |
| Required counseling | 7 | 4 |
| Discharged for positive urine | 3 | 1 |
| Discharged for missed visit | 2 | 0 |
| Encouraged shorter treatment | 6 | 2 |
| Attitudes and Experiences | ||
| Emphasized psychosocial factors | 6 | 6 |
| Reported patients self-discharge | 5 | 2 |
| Mentioned conflicts with patients | 5 | 3 |
We considered whether providers may have achieved higher retention by offering more comprehensive services. However, we found eight low-retention providers worked in programs that offered on-site psychosocial services, typically individual or group counseling, compared to only five high-retention providers. Similarly, four low-retention and two high-retention providers reported offering some level of peer support or case management services.
We also considered that that providers with lower cost services may have achieved higher retention. Again, however, our results did not support this supposition. Eight low-retention providers accepted payments from Medicaid and private insurance, compared to only five high-retention providers. The providers who did not accept Medicaid or private insurance only took direct payments from patients for services.
Even among providers who accepted Medicaid, Medicaid did not always cover counseling services that programs required patients receive, so patients had to pay out-of-pocket for these. One provider explained that weekly counseling was typically required but Medicaid patients could come to counseling less than weekly to minimize costs, “The patients pay out of pocket $25 for the counseling session, and that’s why they have to be at the two weeks or four weeks. We don’t want to be a financial burden for those patients.” Some providers that did not accept insurance said that they used sliding-scale fees and adjusted visit frequency to avoid burdening patients financially. One provider who did not accept insurance said, “I do have a sliding scale. From time to time I’ll see somebody for $25 a visit if I feel like they’re genuinely destitute and they’re genuinely trying as hard as they can.”
Providers’ motivations to deliver buprenorphine treatment may affect their approaches to care. We found differences in motivations for providing treatment between groups. Eight high-retention and four low-retention providers reported that they started prescribing buprenorphine in response to a perceived need for treatment. “I saw a need for it,” one provider said, “One of my best friend’s son died of a heroin overdose, which sort of got me particularly interested in it.” In contrast, seven low-retention and four high-retention providers described starting buprenorphine for employment opportunities, professional development, or income.
Clinical Practices
We asked providers about numerous aspects of their clinical practice that could affect retention. Providers may have achieved high patient retention by selecting to treat only stable patients who were likely to adhere to treatment, but we did not find evidence of this. Five low-retention and four high-retention providers said they might not initiate buprenorphine for a patient with co-occurring psychiatric illness, another co-occurring substance use disorder, or lacking social stability. As one provider said, “Most of the time I do not put a person that is homeless or mentally ill [on buprenorphine].” Other providers required only diagnosed OUD and interest in treatment: “That [patients] meet criteria for opioid use disorder and that they would like to try buprenorphine. Those are probably my two criteria.”
As described above, we counted whether providers used any of five key higher-threshold practices that could reduce retention: conducting office or facility-based inductions, requiring psychosocial treatment as part of buprenorphine treatment, discharging patients in response to positive drug tests, discharging patients in response to missed visits, and encouraging shorter treatment duration. We found that both high- and low-retention providers engaged in high-threshold practices, but these practices were more common among low-retention providers. All ten low-retention providers used at least one high-threshold practice, compared to only five out of ten high-retention providers. For every high-threshold practice, low-retention providers more often reported using the practice than high-retention providers. The average number of high-threshold practices was 2.3 in the low-retention group and 1.1 in the high-retention group.
Five low-retention and three high-retention providers required some patients to undergo office or facility-based induction that typically required remaining under clinical observation for several hours. Some providers that required office-based induction said this practice was becoming less frequent, in part because so many patients had previously used buprenorphine illicitly or in treatment. As a provider explained, “I think more and more nowadays we’re just letting them take it at home because they have had experience with Suboxone, but if they’ve never had any experience with Suboxone or they’re coming off of methadone, or there’s something else that we’re concerned about then, we’ll watch them for an hour or two.”
Seven low-retention providers required counseling as part of treatment, compared to four high-retention providers. Providers that did not require counseling pointed to evidence that it did not improve outcomes and expressed skepticism about the benefit of mandated therapy: “You can’t make people do therapy. I mean, that’s ridiculous. I mean, therapy’s a whole process that requires buy-in.” Providers that required counseling saw it as a crucial component of recovery, at times viewing buprenorphine as the less significant component: “If you just have somebody come to an office and you hand them a [buprenorphine] strip and that’s all they get, I don’t think that’s really helping him. I believe the combination of the group therapy, one on one counseling, the one on one with me, all of that is an important component to getting people better.”
No providers strictly limited treatment to a certain length of time. Six low-retention and two high-retention providers encouraged patients to stop buprenorphine treatment at some point, though they typically emphasized that this was a gradual process: “If they’d been in the program for a while and they appear to be stable on recovery, I start talking to them about, gradually and slowly starting to lean down, but they have to be mentally prepared for that.” The remaining providers flexibly approached treatment length, often emphasizing patients’ choice: “That’s an individual choice… We have a conversation that’s based on their goals, and if it’s one of their goals to come off [buprenorphine], we work with it. If it’s not, then we don’t.”
Eight low-retention providers reported conducting urine drug tests every visit, compared to only five high-retention providers. Providers generally reported that they responded to positive drug tests by discussing the result with patients and by increasing visit frequency. Three low-retention providers and one high-retention provider mentioned discharge as a possible response to positive urine drug tests.
Providers offered diverging views about the importance of cessation of non-opioid illicit drug use as a condition for continued treatment. A provider who conducted urine drug testing at every visit said: “I’m not going to let you smoke weed and I’m not going to let you do this stuff and say, ‘Oh, this is just a little bit better.’ So I’m very strict and I have a no tolerance policy in my clinics.” By contrast, a provider who individualized testing frequency said: “The reality is, if you test people a lot, a lot of what you find is pot, which I don’t care about, or you find out who did a bump of coke at their cousin’s bachelor party. You just get a lot of information that is really not super clinically significant.” This provider noted nonetheless that patients who frequently used stimulants were particularly challenging to treat, a view echoed by other providers.
Nearly all providers reported seeing patients for weekly visits for a time after induction and gradually moving to four- or six-week visits, though there were variations in how long patients remained on weekly visits and what the conditions were for moving to less frequent visits. Two lower retention providers and no high-retention providers mentioned discharge as a possible consequence of missing visits. Some providers made decreasing visit frequency contingent on urine drug tests demonstrating cessation of drug use: “So I have folks come in weekly until they pass a urine drug test for all substances. And then they can gain a week up to six weeks.” If patients had a positive drug test, this provider would return them to weekly visits at which point they could again begin to earn additional weeks by passing drug tests.
Differences in retention could also be driven in part by differences in dosing practices. Providers varied in how quickly they increased dosage at initiation, with several reporting that patients were often already on illicit buprenorphine when they arrived to start treatment. Six high-retention and two low-retention providers said they asked patients what dosage worked for them: “I’ll ask them, historically, how have you taken this? Whether it’s a previous healthcare provider has prescribed it or if it’s been taken off the street.” Six low-retention providers and three high-retention providers said they did not prescribe more than 16mg of buprenorphine per day for maintenance treatment.
Attitudes and Experiences
Differences in provider attitudes and experiences may inform practices that affect retention. As noted above, high-retention providers less often offered co-located psychosocial services or required counseling as part of treatment. However, this difference was not apparently based on lack of appreciation for psychosocial factors in OUD treatment. When discussing the causes of OUD, six providers in each group emphasized the role of psychosocial factors, including trauma, in combination with opioid exposure. A provider at a treatment program for women said: “I think [OUD] is multi-factorial. I think that for a lot of the women that I take care of, the majority, not all, have pretty significant trauma histories. And then they’ll have sort of early introduction to use substances.” The remaining providers emphasized opioid exposure, at times mentioning genetics: “I think genetic vulnerability is always going to be there, but the early exposure from dentists and primary care doctors is killing us. I’ve had many, many patients who were given opioids for menstrual cramps, or for migraines when they were teenagers.”
There were not clear differences in the reasons providers reported patients stopped treatment between high- and low-retention providers. The most frequent reasons providers gave were recurrent drug use, cost of treatment, other barriers to treatment such as transportation, and stigma, often related to lack of support from family. One provider explained why patients typically stopped treatment, “Financial reasons are one. Maybe they’re getting pressure from family members or a spouse. There’s definitely a lot of misinformation out there about [medication treatment].” Though high-retention providers less often accepted insurance, four providers in each group mentioned cost as a reason that patients stopped treatment.
Differences in retention may be driven by patient preferences. Indeed, five low-retention providers and only two high-retention providers mentioned that patients at times stopped treatment because they choose to. However, some providers emphasized that this was a rare occurrence and these patients often returned to drug use. One provider who encouraged shorter treatment length acknowledged the peril of stopping treatment early, noting that people often stopped to pursue jobs where prescription buprenorphine use was not permitted: “Unfortunately, most of the people that stopped treatment on their own have relapsed if they stop early. I have had some people who wanted to accelerate and get back into school or yeah get a job as a truck driver or whatever, you know, things that buprenorphine wasn’t compatible with.”
Finally, high-retention providers may be providers that achieved better therapeutic relationships with their patients. While we could not assess this directly, we noted that five low-retention and three high-retention providers mentioned conflicts or mistrust with patients as challenges of treatment: “Setting limits. Barriers, barriers, barriers. That’s the biggest challenge. These are people that are not used to people saying no to them.” Generalizations regarding people who use drugs may suggest stigmatized views of this population, a possible contributor to retention that we were unable to directly assess. Despite conflicts with patients, providers from both groups spoke positively about their experiences providing buprenorphine: “Before I started using buprenorphine and learning about addiction, I didn’t know how to relate to these patients, and I didn’t know the best way to care for them. And once I learned more about that, it really helped those relationships grow. And I’ve seen it change people’s lives.”
Discussion
We summarized our qualitative and quantitative findings regarding key hypotheses along with our interpretation of findings in Table 4. Our findings suggest use of high-threshold clinical approaches may explain differences in retention between providers whose patients have similar characteristics. All the low-retention providers used high-threshold practices compared to half of high-retention providers. Every high-threshold practice was used more often by low-retention providers compared to high-retention providers. We did not find evidence that providers who achieved higher retention consistently did so by providing more comprehensive services, delivering lower-cost care, or selecting for more stable patients.
Table 4.
Summary of qualitative and quantitative findings regarding key hypotheses
| Hypothesis | Quantitative results | Qualitative results | Interpretation |
|---|---|---|---|
| Providers achieve high retention by offering “low-threshold” care. | Supported: higher starting buprenorphine dose and fewer BH visits were more common among treatment episodes achieving retention (Table 1); matched high-retention providers had treatment episodes with fewer BH visits (Supplementary Material 4). | Supported: all low-retention providers used high-threshold practices compared to half of high-retention providers, with the requirement to participate in psychosocial services being the most frequently used high-threshold practice (Table 3). | This hypothesis was supported by our quantitative and qualitative findings. The requirement to participate in psychosocial services appeared especially important in limiting buprenorphine treatment retention. |
| Providers achieve high retention by offering more comprehensive services. | Not supported: in adjusted models, there was no difference in retention between care delivered in office or BH settings (Table 2); matched high retention providers were more often located in office settings, but this difference wasn’t statistically significant (Supplementary Material 4). | Opposed: more low-retention providers reported offering on-site psychological, peer support, or case management services (Table 3). | High-retention providers less frequently offered psychosocial services. This may be explained by the fact that participation in psychosocial services where available was often mandatory, creating a barrier to retention. |
| Providers achieve high retention by offering lower cost care. | Not assessed: the Medicaid claims data we used represent Medicaid payments but do not offer direct insights into out-of-pocket costs for patients. | Equivocal: more low-retention providers accepted Medicaid, but some of these providers required patients pay out-of-pocket for psychosocial services (Table 3); providers generally cited cost as a barrier to treatment retention. | The relationship between cost and retention is confounded by the fact that providers who accepted Medicaid also frequently required participation in services that required out-of-pocket spending. Cost is likely a barrier to retention, as providers generally mentioned it being, but we could not determine that offering lower cost care was reliably employed by providers in our sample to improve retention. |
| Providers achieve high retention because their patients prefer longer treatment. | Not assessed: patient preferences could not be assessed with claims. | Supported: More low-retention providers mentioned that patients at times chose to stop treatment (Table 3). | We could not rule out this hypothesis. However, we believe that low-retention providers’ use of burdensome high-threshold practices likely explains why they more often reported that their patients stopped treatment. |
| Providers achieve high retention through better therapeutic relationships. | Not assessed: the quality of therapeutic relationships could not be assessed with claims. | Not assessed: the quality of therapeutic relationships could not be directly assessed but more low-retention providers mentioned conflicts with patients (Table 3). | We could not directly assess this hypothesis, but low-retention providers more often mentioned conflicts with patients. This may be because these providers used more high-threshold practices that led to conflicts with patients, or because these providers were otherwise unable to form as therapeutic relationships with patients. |
| Providers achieve high retention by selecting more stable patients. | Not supported: sicker patients had lower retention in adjusted models (Table 2) but coarsened exact matching balanced groups on measures of OUD severity and comorbidity (Supplementary Material 4). | Not supported: the same number of high- and low-retention providers indicated selecting for more stable patients (Table 3). | We could not rule out that this practice takes place out of our sample, but we did not find evidence to support this hypothesis among our matched group of providers. |
For each hypothesis of how providers may achieve high retention, the table summarizes whether quantitative and qualitative methods did not assess, did not support, supported, were equivocal, or opposed the hypothesis. “Opposed” is used to designated findings that suggest an opposite relationship than the hypothesis, in contrast to “not supported,” which merely designates absence of support.
Compared to low-retention providers, high-retention providers generally began providing buprenorphine treatment more recently. This difference in time providing treatment may be critical in explaining differing approaches to treatment. Providers who began delivering buprenorphine treatment more recently may be more informed by recent shifts in recommended treatment practices that emphasize individualization over strict regimented approaches that may create barriers to retention (Martin et al., 2018).
Required participation in counseling may represent a particularly important barrier to treatment retention. Treatment episodes that achieved 180-day retention had fewer BH visits in their first 30 days compared to episodes that did not achieved retention. Even after coarsened exact matching, high-retention providers’ episodes had fewer BH visits in the first 30 days of treatment. In provider interviews, low-retention providers more often offered on-site psychosocial services and required participation for treatment. The added time, cost, and energy required to participate in these services may pose barriers to treatment retention. Not requiring counseling could explain why PCPs and office-based providers were associated with higher retention, since these providers may be less likely to have on-site psychosocial services. These results mirror evidence from methadone programs that requiring counseling is associated with lower retention (Hochheimer & Unick, 2022). There is no evidence that requiring behavioral health interventions improves outcomes in buprenorphine treatment (Carroll & Weiss, 2017). Another particularly important barrier to retention may be low buprenorphine doses. Treatment episodes that achieved 180-day retention had higher initial buprenorphine doses compared to episode that did not achieve retention. testing
The fact that high-retention providers less frequently accepted insurance should not be taken to mean cost is not a barrier to retention, as several providers indicated it was a frequent reason that patients stopped treatment. Though our study used Medicaid data, we found that many provider treating Medicaid patients did not accept Medicaid, suggesting these patients were paying out-of-pocket for treatment. Patients may be faced with a choice of low-threshold providers at higher costs and high-threshold providers at lower costs. Some patients may choose higher cost providers who use lower threshold approaches so they can continue income-generating practices, trading off cost of care with time to accommodate work or other activities.
High-threshold practices may be, in part, financially motivated. Low-retention providers more often accepted insurance, but also more often required participation in counseling that was not always covered by Medicaid. For providers who accept Medicaid for buprenorphine visits, and likely receive low compensation per visit, requiring patient participation in psychosocial services may be an important revenue strategy. Similarly, requiring patients to have more frequent visits or dismissing patients who miss visits may be seen as financially necessary.
We found large differences in probability of retention by patient race and ethnicity, even when controlling for co-morbidities and prior health service use. These findings mirror those in previous papers that have found large racial disparities in both buprenorphine treatment access and retention.(Schuler et al., 2021; Weinstein et al., 2017) This finding suggests differences in retention by race and ethnicity are not explainable only by measured comorbidities and prior service use in our study. According to providers, treatment cost, logistical barriers such as transportation, and stigma were important reasons for why patients left treatment early. These factors likely differentially affect racial and ethnic groups. Providers may also be more likely to discharge these patients because of overt or implicit racism that is widespread in healthcare and can affect treatment adherence (Ben et al., 2017; Fitzgerald & Hurst, n.d.). Addressing systematic racism is critical to reducing racial and ethnic disparities in OUD treatment through policies such as targeted grant funding, criminal legal reform, and changes to regulation of medications treatment for MOUD (Andraka-Christou, 2021; Jordan et al., 2020).
We termed the mixed-methods approach used in this paper matched subgroup analysis. Matched subgroup analysis bears resemblance to systematic anomalous case analysis in that quantitative methods are used to identify cases of interest that may then be explored using a variety of qualitative approaches to explain quantitative finding (Pearce, 2002). Matched subgroup analysis is useful when comparing units that achieve different outcomes while acting on different populations for the purpose of identifying unit characteristics or approaches that drive outcomes. In this case, the units are providers, the outcome is retention, and the populations are patients. In other instances, the units may be teachers or managers, while the populations may be students or clients. The analysis of data on the matched units may be undertaken with various methodologies. In this case, qualitative content analysis was used, but this stage of analysis may lend itself to causal analyses with configurational comparative approaches (Haesebrouck & Thomann, 2021; Yakovchenko et al., 2020).
Our provider sample was limited to providers with high number of buprenorphine patients enrolled in Medicaid in North Carolina, so generalizability may be limited to similar provider groups. Our study was limited to capturing data from North Carolina Medicaid enrollees, so we could not observe outcomes for non-Medicaid individuals. We could not rule out that patients appeared lost to retention because they switched from prescribed buprenorphine to daily dispensed methadone at an OTP, though this is uncommon based on our knowledge of practice in North Carolina, in part because there are relatively few OTPs. For providers who did not accept Medicaid, we may have underestimated their rates retention for all patients, since low-income Medicaid patients may have faced higher costs for care compared to other patients. That said, we found more of these providers in the high-retention group, so this underestimation would not change the direction of our findings. Our study was also limited in that we could not interview patients, so we presented providers’ perspective on why patients were not retained in treatment. We also cannot be certain that the interview results are representative of the groups samples. While we used matching to minimized differences between, we cannot rule out the possibilities that unobserved differences in patient populations remain.
Predicted probabilities from our regression models performed poorly in identifying patients retained in treatment. This result suggests retention that is likely driven by factors that are not observed in secondary data. We present evidence that high-threshold treatment practices is an important one of this factors that is unobserved in secondary data. An alternative or complementary explanation to our findings is that low-retention providers had patients who preferred shorter treatment durations, as several indicated. There are many reasons why patients may prefer shorter treatment durations, such as burden of attending treatment or stigma related to treatment.(Madden et al., 2021) We think it is likely that high threshold practices contribute to preferences for shorter treatment because high threshold practices can make treatment more burdensome. Previous research has found that treatment program inflexibility to accommodate patients’ other obligations is a leading cause of discharge (Gryczynski et al., 2014). Similarly, it is possible that patients who attended high-retention providers had more social support that allowed them to bear the financial and time costs of treatment.
Our study suggests low-threshold approaches to buprenorphine treatment may contribute to higher retention, but that other factors, such as treatment cost and systemic racism, are also likely involved. Strategies to reduce the time and logistical burden of buprenorphine treatment for patients while serving patients’ psychosocial needs could hold promise for improving retention. Addressing provider factors that limit treatment retention will require a combination of research, education, and policy. Additional research is needed to clarify optimal frequency of visits and use of urine drug testing in OUD treatment. Professional societies and training programs should ensure providers know current evidence and guidelines that required counseling or frequent urine drug testing do not improve retention, that treatment length should be individualized, and that 16 mg is an insufficient treatment dose for many patients. Payers should ensure that reimbursement levels for buprenorphine visits are adequate to avoid incentivizing providers mandating use of non-covered services.
Supplementary Material
Highlights.
Less than half of patients achieved 180-day treatment retention
There were large differences in retention by race and ethnicity.
High-threshold practices best explained differences in retention
Acknowledgments
A.K.G. was supported by the National Institute on Drug Abuse of the National Institutes of Health under award number F30DA044668. The database infrastructure used for this project was supported in part by the Cecil G. Sheps Center for Health Services Research and the CER Strategic Initiative of UNC’s Clinical and Translational Science Award (UL1TR001111). The authors are grateful to the Carolina Cost and Quality Initiative for assistance accessing North Carolina Medicaid claims data for this analysis. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the North Carolina Department of Health and Human Services.
REFERENCES
- American Medical Association. (2021). CPT overview and code approval. https://www.ama-assn.org/practice-management/cpt/cpt-overview-and-code-approval
- American Society of Addiction Medicine. (2015). The ASAM National Practice Guideline for the Use of Medications in the Treatment of Addiction Involving Opioid Use. https://www.asam.org/docs/default-source/practice-support/guidelines-and-consensus-docs/asam-national-practice-guideline-pocketguide.pdf?sfvrsn=35ee6fc2_0 [DOI] [PMC free article] [PubMed]
- Andraka-Christou B (2021). Addressing Racial And Ethnic Disparities In The Use Of Medications For Opioid Use Disorder. Health Affairs, 40(6), 920–927. 10.1377/hlthaff.2020.02261 [DOI] [PubMed] [Google Scholar]
- Baxter JD, Clark RE, Samnaliev M, Aweh G, & O’Connell E (2015). Adherence to buprenorphine treatment guidelines in a Medicaid program. Substance Abuse, 36(2), 174–182. 10.1080/08897077.2014.991469 [DOI] [PubMed] [Google Scholar]
- Ben J, Cormack D, Harris R, & Paradies Y (2017). Racism and health service utilisation: A systematic review and meta-analysis. PLOS ONE, 12(12), e0189900. 10.1371/journal.pone.0189900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackwell M, Iacus S, King G, & Porro G (2009). Cem: Coarsened exact matching in Stata. Stata Journal. [DOI] [Google Scholar]
- Carroll KM, & Weiss RD (2017). The Role of Behavioral Interventions in Buprenorphine Maintenance Treatment: A Review. American Journal of Psychiatry, 174(8), 738–747. 10.1176/appi.ajp.2016.16070792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clayton P (2013). CUTPT: Stata module for empirical estimation of cutpoint for a diagnostic test. In Statistical Software Components S457719. Boston College Department of Economics. https://ideas.repec.org/c/boc/bocode/s457719.html [Google Scholar]
- Coffey A, & Atkinson P (1996). Making Sense of Qualitative Data: Complementary Research Strategies and Social Thought. SAGE Publications. [Google Scholar]
- Fitzgerald C, & Hurst S (n.d.). Implicit bias in healthcare professionals: a systematic review. 10.1186/s12910-017-0179-8 [DOI] [PMC free article] [PubMed]
- Forman J, & Damschroder LJ (2007). Qualitative Content Analysis. In Jacoby L & Siminoff LA (Eds.), Empirical Methods for Bioethics: A Primer (Advances i, pp. 39–62). Emerald Group Publishing Limited. [Google Scholar]
- Gertner AK, Robertson AG, Powell BJ, Jones H, Silberman P, & Domino ME (2020). Primary Care Providers And Specialists Deliver Comparable Buprenorphine Treatment Quality. Health Affairs, 39(8), 1395–1404. 10.1377/hlthaff.2019.01559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gryczynski J, Mitchell SG, Jaffe JH, O’Grady KE, Olsen YK, & Schwartz RP (2014). Leaving buprenorphine treatment: Patients’ reasons for cessation of care. Journal of Substance Abuse Treatment, 46(3), 356–361. 10.1016/j.jsat.2013.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guest G (2006). How Many Interviews Are Enough?: An Experiment with Data Saturation and Variability. Field Methods, 18(1), 59–82. 10.1177/1525822X05279903 [DOI] [Google Scholar]
- Haesebrouck T, & Thomann E (2021). Introduction: Causation, inferences, and solution types in configurational comparative methods. Quality and Quantity, 0123456789. 10.1007/s11135-021-01209-4 [DOI] [Google Scholar]
- Harris J, Pryor J, & Adams S (2006). The challenge of intercoder agreement in qualitative inquiry. http://emissary.wm.edu/templates/content/
- Hochheimer M, & Unick GJ (2022). Systematic review and meta-analysis of retention in treatment using medications for opioid use disorder by medication, race/ethnicity, and gender in the United States. Addictive Behaviors, 124(September 2021), 107113. 10.1016/j.addbeh.2021.107113 [DOI] [PubMed] [Google Scholar]
- Jakubowski A, & Fox A (2019). Defining Low-threshold Buprenorphine Treatment. Journal of Addiction Medicine, 00(00), 1–4. 10.1097/ADM.0000000000000555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan A, Mathis ML, & Isom J (2020). Achieving Mental Health Equity: Addictions. Psychiatric Clinics of North America, 43(3), 487–500. 10.1016/j.psc.2020.05.007 [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation. (2022). Status of State Action on the Medicaid Expansion Decision | The Henry J. Kaiser Family Foundation. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/ [Google Scholar]
- Knudsen HK, Lofwall MR, Lin L, Walsh SL, & Studts JL (2019). US physicians’ decision-making during buprenorphine-naloxone treatment: Conjoint analyses of dose and office visit adjustments based on patient progress. Drug and Alcohol Dependence. 10.1016/j.drugalcdep.2019.05.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kresina TF, Litwin A, Marion I, Lubran R, & Clark HW (2009). United States Government Oversight and Regulation of Medication Assisted Treatment for the Treatment of Opioid Dependence. Journal of Drug Policy Analysis, 2(1), 1–23. 10.2202/1941-2851.1007 [DOI] [Google Scholar]
- Kunins HV (2020). Structural Racism and the Opioid Overdose Epidemic: The Need for Antiracist Public Health Practice. Journal of Public Health Management and Practice, 26(3), 201–205. 10.1097/PHH.0000000000001168 [DOI] [PubMed] [Google Scholar]
- Liu X (2012). Classification accuracy and cut point selection. Statistics in Medicine, 31(23), 2676–2686. 10.1002/sim.4509 [DOI] [PubMed] [Google Scholar]
- Madden EF, Prevedel S, Light T, & Sulzer SH (2021). Intervention Stigma toward Medications for Opioid Use Disorder: A Systematic Review. Substance Use & Misuse, 56(14), 2181–2201. 10.1080/10826084.2021.1975749 [DOI] [PubMed] [Google Scholar]
- Martin SA, Chido L, Bosse JD, & Amanda W (2018). The Next Stage of Buprenorphine Care for Opioid Use Disorder: A Special Article. Annals of Internal Medicine. 10.7326/M18-1652 [DOI] [PubMed] [Google Scholar]
- Martin SA, Chiodo LM, & Wilson A (2019). Retention in care as a quality measure for opioid use disorder. Substance Abuse, 1–6. 10.1080/08897077.2019.1635969 [DOI] [PubMed] [Google Scholar]
- Miles MB, & Huberman AM (1994). Qualitative data analysis: A sourcebook (2nd ed.). SAGE Publications. [Google Scholar]
- Miotto K, Hillhouse M, Donovick R, Cunningham-Rathner J, Charuvastra C, Torrington M, Esagoff AE, & Ling W (2012). Comparison of Buprenorphine Treatment for Opioid Dependence in 3 Settings. Journal of Addiction Medicine, 6(1), 68–76. 10.1097/ADM.0b013e318233d621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Quality Forum. (2017). Continuity of Pharmacotherapy for Opioid Use Disorder 3175. http://www.qualityforum.org
- Neumann AM, Blondell RD, Azadfard M, Nathan G, & Homish GG (2013). Primary care patient characteristics associated with completion of 6-month buprenorphine treatment. Addictive Behaviors, 38(11), 2724–2728. 10.1016/j.addbeh.2013.07.007 [DOI] [PubMed] [Google Scholar]
- Palinkas LA, Aarons GA, Horwitz S, Chamberlain P, Hurlburt M, & Landsverk J (2011). Mixed Method Designs in Implementation Research. Administration and Policy in Mental Health and Mental Health Services Research, 38(1), 44–53. 10.1007/s10488-010-0314-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palinkas LA, Horwitz SM, Chamberlain P, Hurlburt MS, & Landsverk J (2011). Mixed-Methods Designs in Mental Health Services Research: A Review. Psychiatric Services, 62(3), 255–263. 10.1176/ps.62.3.pss6203_0255 [DOI] [PubMed] [Google Scholar]
- Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, & Hoagwood K (2015). Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm. Policy Ment. Health, 42(5), 533–544. 10.1007/s10488-013-0528-y.Purposeful [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce LD (2002). 3. Integrating Survey and Ethnographic Methods for Systematic Anomalous Case Analysis. Sociological Methodology, 32(1), 103–132. 10.1111/1467-9531.00113 [DOI] [Google Scholar]
- Samples H, Williams AR, Olfson M, & Crystal S (2018). Risk factors for discontinuation of buprenorphine treatment for opioid use disorders in a multi-state sample of Medicaid enrollees. Journal of Substance Abuse Treatment, 95, 9–17. 10.1016/j.jsat.2018.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler MS, Dick AW, & Stein BD (2021). Growing racial/ethnic disparities in buprenorphine distribution in the United States, 2007–2017. Drug and Alcohol Dependence, 223(April), 108710. 10.1016/j.drugalcdep.2021.108710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson DD (2004). A conceptual framework for drug treatment process and outcomes. Journal of Substance Abuse Treatment, 27(2), 99–121. 10.1016/j.jsat.2004.06.001 [DOI] [PubMed] [Google Scholar]
- Sordo L, Barrio G, Bravo MJ, Indave I, Degenhardt L, Wiessing L, Ferri M, Pastor-Barriuso R, Indave BI, Degenhardt L, Wiessing L, Ferri M, & Pastor-Barriuso R (2017). Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ (Clinical Research Ed.), 357, j1550. 10.1136/bmj.j1550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse Mental Health Services Administration. (n.d.). Medication for opiod use disorder (OUD). In Tip 63. Retrieved August 23, 2018, from https://www.surveymonkey.com/r/KAPPFS [Google Scholar]
- The Carolina Cost and Quality Initiative. (2019). https://www.shepscenter.unc.edu/data/bcbsnc-claims-data-ccqi/
- Timko C, Schultz NR, Cucciare MA, Vittorio L, & Garrison-Diehn C (2016). Retention in medication-assisted treatment for opiate dependence: A systematic review. Journal of Addictive Diseases, 35(1), 22–35. 10.1080/10550887.2016.1100960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Agriculture. (2013). Rural-Urban Continuum Codes. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx#.UYJuVEpZRvY
- Watkins KE, Paddock SM, Hudson TJ, Ounpraseuth S, Schrader AM, Hepner KA, & Stein BD (2017). Association between process measures and mortality in individuals with opioid use disorders. Drug and Alcohol Dependence, 177(March), 307–314. 10.1016/j.drugalcdep.2017.03.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein ZM, Kim HW, Cheng DM, Quinn E, Hui D, Labelle CT, Drainoni M-L, Bachman SS, & Samet JH (2017). Long-term retention in Office Based Opioid Treatment with buprenorphine. Journal of Substance Abuse Treatment, 74, 65–70. 10.1016/j.jsat.2016.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams AR, Nunes EV, Bisaga A, Levin FR, & Olfson M (2019). Development of a Cascade of Care for responding to the opioid epidemic. American Journal of Drug and Alcohol Abuse, 45(1), 1–10. 10.1080/00952990.2018.1546862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yakovchenko V, Miech EJ, Chinman MJ, Chartier M, Gonzalez R, Kirchner JE, Morgan TR, Park A, Powell BJ, Proctor EK, Ross D, Waltz TJ, & Rogal SS (2020). Strategy Configurations Directly Linked to Higher Hepatitis C Virus Treatment Starts. Medical Care, 58(5), e31–e38. 10.1097/mlr.0000000000001319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang A, Arfken CL, & Johanson CE (2013). Steps Physicians Report Taking to Reduce Diversion of Buprenorphine. The American Journal on Addictions, 22(3), 184–187. 10.1111/J.1521-0391.2012.00335.X [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


