Introduction
The COVID-19 pandemic has caused at least 508,827,830 infections and is associated with a 1.2% mortality rate worldwide (1). New SARS-CoV-2 variants have driven new waves of the pandemic as a result of their increased transmissibility and ability to evade the immune response (2). The post-acute sequelae of SARS-CoV-2 infection (PASC) is an important but underestimated public health issue that can have a long-term impact on pulmonary and multiple extrapulmonary tissues and organs through several potential mechanisms (3, 4). Recent studies demonstrate that approximately 4–69% of patients (including children, adolescents, adults, and senior) suffer from PASC (5–11). There is considerable evidence concerning post-acute sequelae that will likely outlast the current pandemic and need to be addressed. This article reviews the clinical sequelae of COVID-19 survivors and provides valuable insights required to fill the gaps in medical knowledge.
Pulmonary and Extrapulmonary Organ Sequelae
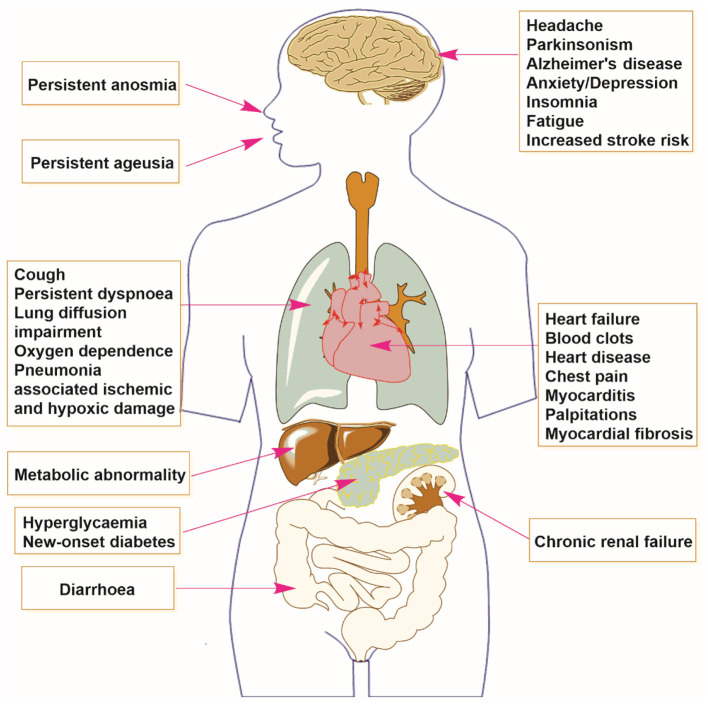
There are several persistent sequelae occurring among COVID-19 survivors (see Figure 1). A longitudinal cohort study from Wuhan, China found that 1 year after COVID-19 diagnosis, 26% (313/1,185) and 30% (380/1,271) of survivors experienced dyspnea, or persistent breathlessness, at 6 and 12 months, respectively (12). The same study found that lung diffusion impairment was common among critically ill patients at 12 months (12). In a multicenter UK study, Evans et al. (13) found that of 1,077 hospitalized patients, 41% experienced dyspnea and 21–28% experienced palpitations and chest pain 5.9 months after discharge. A random-effect meta-analysis of 257,348 patients revealed that 25, 21, and 31% of survivors displayed persistent dyspnea at 6–8, 9–12, and >12 months follow-up, respectively (14).
Figure 1.
Multiple organ sequelae of SARS-CoV-2 infection.
There is an increased long-term risk of cardiovascular complications such as heart failure among patients with SARS-CoV-2 infection, even among mild cases (15). A large-scale study including a cohort of 153,760 COVID-19 survivors, an age-matched control group of 5,637,647 individuals, and a historical comparison group of 5,859,411 individuals, was conducted by Al-Aly et al. (16) to estimate the risk of cardiovascular sequelae. COVID-19 survivors had a significantly increased risk of cardiovascular disease within 1 year, including a 52% and a 72% increased risk of stroke and heart failure, respectively (16). SARS-CoV-2 infection is correlated with “new-onset” cardiovascular disease following infection (17). Rizvi et al. (18) independently reported that SARS-CoV-2-infected golden Syrian hamsters had cardiovascular complications such as ventricular wall thickening and interstitial fibrosis with elevated cardiac troponin I during the late phase of infection. Maio et al. (19) reported that the risk of thromboembolic events 8.5 months after the follow-up of COVID survivors (1.53%, n = 6,937) was five times higher than among population controls (0.31%, n = 435,104). An online survey showed that 53 and 68% of patients reported chest pain and palpitations 7 months after COVID-19 infection (20).
SARS-CoV-2 infection even among those with mild symptoms can cause severe cognitive and neurological defects (21). Recent studies have demonstrated that >10% of patients experience COVID-19-associated anosmia (21). A large UK-based community cohort study with 4,999 participants conducted from June 2021 to January 2022 found that patients infected with the omicron variant more frequently possessed a loss of smell than those infected with the delta variant (52.7 vs. 16.7%, respectively; p < 0.001) (22). Zazhytska et al. (23) found non-cell-autonomous disruption of olfactory sensory neuron nuclear architecture and down-regulation of olfactory receptors and signaling genes in SARS-CoV-2-infected hamster and human autopsies. These findings provide a potential pathophysiological mechanism linking COVID-19 and anosmia. Kraus et al. (24) provided an alternate mechanism by which the intranasal receptor-binding domain of SARS-CoV-2 spike protein causes olfactory receptor damage and olfactory system dysfunction in SARS-CoV-2-infected zebrafish. This finding has potential implications for the intranasal treatment of PASC. Douaud et al. (25) conducted a large-scale longitudinal neuroimaging cohort study of the brain images from 401 COVID-19 cases 51 to 81 years of age and 384 age-matched controls to estimate how changes to brain structure and function correlate with the taste and smell of infected patients. COVID-19 survivors showed a greater reduction in the gray matter thickness of the parahippocampal gyrus and entorhinal cortex, ranging from ~0.2 to ~2%, and a greater reduction in the global brain volume than controls (25).
To date, from anosmia, headaches, to Parkinsonism, Alzheimer's have been attributed to SARS-CoV-2 infection (26). A clinical study indicated that the risk of dementia was 2–3-fold higher among SARS-CoV-2-infected individuals than healthy controls (27). Semerdzhiev et al. (28) found that Parkinsonism is caused by a direct interaction between the SARS-CoV-2 N-protein and α-synuclein. Lang et al. (29) indicated that hypoxemia, or respiratory compromise, along with potential virus-specific endothelial mechanisms may account for post-infectious Parkinsonism. Revere et al. (30) found that Alzheimer's is associated with a higher expression of Angiotensin-Converting Enzyme 2 in the brains of COVID-19 survivors, and Shen et al. (31) showed that SARS-CoV-2 enters the brain, induces an Alzheimer's-like gene program in healthy neurons and exacerbates disease-related neuropathology. Fernández-de-las-Peñas et al. (32) found that 8.4–15% of COVID-19 survivors suffer from post-COVID headaches 6 months after infection.
“Long COVID” can cause metabolic abnormalities and immunological dysfunction (33–35). For example, in a cohort study of 551 discharged COVID-19 survivors in Italy, 35 and 2% had hyperglycemia and “new-onset diabetes,” respectively, after 6 months (33). In another retrospective England-based cohort study of 47,780 COVID-19 patients with a mean of 65 years of age, 2.9% had “new-onset diabetes” 4.6 months following infection (34). Thus, SARS-CoV-2 infection can cause multiple organ failure and induce long-lasting post-COVID sequelae that are of great concern.
Discussion
The COVID-19 pandemic is ongoing and promising curative treatments do not yet exist (36, 37). Meanwhile, the sequelae of this infection have posed a considerable threat to global health and economic development. Considering the available evidence, additional preventive and treatment strategies are needed.
Current prophylactic measures, such as wearing masks and increasing vaccination coverage, are still necessary. Vaccination is associated with a lower risk of several COVID-19 sequelae and remains the most practical approach to preventing the further spread of the virus (38). After 2 years, 11,438,720,838 doses of the COVID-19 vaccine have been administered globally to combat SARS-CoV-2 infection (1). Third and even fourth vaccine booster doses are being administered in many countries to improve immunity (39). However, many low-income nations are still waiting to offer the initial doses (1). Vaccine inequity has enabled SARS-CoV-2 to spread rapidly, increasing the incidence of sequelae, and undermining global COVID-19 recovery efforts (40). Fair allocation of vaccines is critical for effective COVID-19 control and elimination in resource-limited settings. Fortunately, more countries are taking further action. In November 2021, President Xi announced that China would provide 1.0 billion, including 600 million donated, COVID-19 vaccine doses to African countries to help reach its goal of vaccinating 60% of its population by 2022 (41). Countries will need to collaborate to create a fairer vaccination environment required to bolster worldwide immunity.
In addition, therapeutic regimens, including small-molecule inhibitors and traditional medicine, are still needed. Small-molecule inhibitors are being widely studied and play an essential function in COVID-19 treatment. Gilead's controversial drug, Veklury®, was conditionally approved by the Food and Drug Administration (FDA) to combat the pandemic (42, 43) and Pfizer's oral broad-spectrum candidate, Paxlovid®, and Merck's oral prodrug, Lagevrio®, provide new hope for a COVID-19 cure (44). Even with promising clinical results, however, widespread use of these treatments may increase the virus' resistance to inhibitors. Researchers will need to carefully design more aggressive and effective strategies to address therapeutic limitations and uncertainties. For example, multi-target drug combination therapy (PF-07321332 + Remdesivir, Linoleic acid + Remdesivir, PF-07321332 + Molnupiravir), could enhance synergistic anti-COVID-19 efficacy while also reducing drug resistance (45). Traditional medicine is another valuable tool that should be considered for COVID-19 treatment. Many studies have shown that herbal medicine offers multi-organ protection against SARS-CoV-2 (46). Ye et al. (47) illustrated that licorice-saponin A3 and glycyrrhetinic acid, triterpenoids isolated from Gan-Cao, have strong inhibitory potency against SARS-CoV-2 infection at EC50 values of 75 nM against the SARS-CoV-2 nsp7 protein and 3.17 μM against the Spike protein. In the COVID-19 era, small-molecule inhibitors and traditional medicine have a distinct advantage and should be shared between laboratories.
PASC rehabilitation measures, such as multi-disciplinary PASC collaboration, are also critical. A database that includes the physiology, serological, clinical imaging, and epidemiological characteristics of PASC is required to better understand the condition. In addition, fundamental science research, including an understanding of the mechanisms of viral replication, disease pathogenesis, and host immunity is required to direct the earlier evaluation and future rehabilitation of survivors. Healthcare professionals will need to recognize and document pulmonary complications to improve mental and physical health by providing timely team-based, high-quality rehabilitation nursing to survivors. In short, clinical trials of the PASC and additional anti-PASC treatment options are required to fully understand and address this medical issue.
Author Contributions
ZW: conceptualization, writing—original draft, writing—review and editing, visualization, and funding acquisition. LY: conceptualization, writing—review and editing, and funding acquisition. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the project of the Ph.D. research start-up fund of Qufu Normal University, China (Grant Nos. 614901 and 615201).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.World Health Organization . WHO Coronavirus (COVID-19) Dashboard. Available online at: https://covid19.who.int/ (assessed April 28, 2022).
- 2.Wang Z, Yang L. In the age of omicron variant: paxlovid raises new hopes of COVID-19 recovery. J Med Virol. (2022) 94:1766–7. 10.1002/jmv.27540 [DOI] [PubMed] [Google Scholar]
- 3.Sidik SM. Heart-disease risk soars after COVID—even with a mild case. Nature. (2022) 602:560. 10.1038/d41586-022-00403-0 [DOI] [PubMed] [Google Scholar]
- 4.Writing Committee, Gluckman TJ, Bhave NM, Allen LA, Chung EH, Spatz ES, et al. ACC expert consensus decision pathway on cardiovascular sequelae of COVID-19 in adults: myocarditis and other myocardial involvement, post-acute sequelae of SARS-CoV-2 infection, and return to play: a report of the American college of cardiology solution set oversight committee. J Am Coll Cardiol. (2022) 79:1717–56. 10.1016/j.jacc.2022.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Su Y, Yuan D, Chen DG, Ng RH, Wang K, Choi J, et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell. (2022) 185:881–95. 10.1016/j.cell.2022.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen K, Ren S, Heath K, Dasmariñas MC, Jubilo KG, Guo Y, et al. Risk of persistent and new clinical sequelae among adults aged 65 years and older during the post-acute phase of SARS-CoV-2 infection: retrospective cohort study. BMJ. (2022) 376:e068414. 10.1136/bmj-2021-068414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buonsenso D, Di Giuda D, Sigfrid L, Pizzuto DA, Di Sante G, De Rose C, et al. Evidence of lung perfusion defects and ongoing inflammation in an adolescent with post-acute sequelae of SARS-CoV-2 infection. Lancet Child Adolesc Health. (2021) 5:677–80. 10.1016/S2352-4642(21)00196-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lund LC, Hallas J, Nielsen H, Koch A, Mogensen SH, Brun NC, et al. Post-acute effects of SARS-CoV-2 infection in individuals not requiring hospital admission: a Danish population-based cohort study. Lancet Infect Dis. (2021) 21:1373–82. 10.1016/S1473-3099(21)00211-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fabbri L, Moss S, Khan FA, Chi W, Xia J, Robinson K, et al. Parenchymal lung abnormalities following hospitalisation for COVID-19 and viral pneumonitis: a systematic review and meta-analysis. Thorax. (2022). 10.1101/2021.03.15.21253593. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 10.Long Q, Li J, Hu X, Bai Y, Zheng Y, Gao Z. Follow-ups on persistent symptoms and pulmonary function among post-acute COVID-19 patients: a systematic review and meta-analysis. Front Med. (2021) 8:702635. 10.3389/fmed.2021.702635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Han Q, Zheng B, Daines L, Sheikh A. Long-term sequelae of COVID-19: a systematic review and meta-analysis of one-year follow-up studies on post-COVID symptoms. Pathogens. (2022) 11:269. 10.3390/pathogens11020269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang L, Yao Q, Gu X, Wang Q, Ren L, Wang Y, et al. 1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study. Lancet. (2021) 398:747–58. 10.1016/S0140-6736(21)01755-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Evans RA, McAuley H, Harrison EM, Shikotra A, Singapuri A, Sereno M, et al. Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): a UK multicentre, prospective cohort study. Lancet Respir Med. (2021) 9:1275–87. 10.1016/S2213-2600(21)00383-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alkodaymi MS, Omrani OA, Fawzy NA, Abou Shaar B, Almamlouk R, Riaz M, et al. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: a systematic review and meta-analysis. Clin Microbiol Infect. (2022) 28:657–66. 10.1016/j.cmi.2022.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature. (2021) 594:259–64. 10.1038/s41586-021-03553-9 [DOI] [PubMed] [Google Scholar]
- 16.Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. (2022) 28:583–90. 10.1038/s41591-022-01689-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abbasi J. The COVID heart—one year after SARS-CoV-2 infection, patients have an array of increased cardiovascular risks. JAMA. (2022) 327:1113–4. 10.1001/jama.2022.2411 [DOI] [PubMed] [Google Scholar]
- 18.Rizvi ZA, Dalal R, Sadhu S, Binayke A, Dandotiya J, Kumar Y, et al. Golden Syrian hamster as a model to study cardiovascular complications associated with SARS-CoV-2 infection. eLife. (2022) 11:e73522. 10.7554/eLife.73522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maio SD, Lamina C, Coassin S, Forer L, Würzner R, Schönherr S, et al. Lipoprotein (a) and SARS-CoV-2 infections: susceptibility to infections, ischemic heart disease and thromboembolic events. J Intern Med. (2022) 291:101–7. 10.1111/joim.13338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ, Re'em Y, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. eClinicalMedicine. (2021) 38:101019. 10.1016/j.eclinm.2021.101019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.York A. SARS-CoV-2 sensory loss. Nat Rev Microbiol. (2022) 20:190. 10.1038/s41579-022-00707-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Menni C, Valdes AM, Polidori L, Antonelli M, Penamakuri S, Nogal A, et al. Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: a prospective observational study from the ZOE COVID study. Lancet. (2022) 399:1618–24. 10.1016/S0140-6736(22)00327-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zazhytska M, Kodra A, Hoagland DA, Frere J, Fullard JF, Shayya H, et al. Non-cell-autonomous disruption of nuclear architecture as a potential cause of COVID-19-induced anosmia. Cell. (2022) 185:1052–64. 10.1016/j.cell.2022.01.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kraus A, Huertas M, Ellis L, Boudinot P, Levraud JP, Salinas I. Intranasal delivery of SARS-CoV-2 Spike protein is sufficient to cause olfactory damage, inflammation and olfactory dysfunction in zebrafish. Brain Behav Immun. (2022) 102:341–59. 10.1016/j.bbi.2022.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Douaud G, Lee S, Alfaro-Almagro F, Arthofer C, Wang C, McCarthy P, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. (2022) 604:697–707. 10.1038/s41586-022-04569-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gollub RL. Brain changes after COVID revealed by imaging. Nature. (2022) 604:633–4. 10.1038/d41586-022-00503-x [DOI] [PubMed] [Google Scholar]
- 27.Szabo MP, Iba M, Nath A, Masliah E, Kim C. Does SARS-CoV-2 affect neurodegenerative disorders? TLR2, a potential receptor for SARS-CoV-2 in the CNS. Exp Mol Med. (2022) 54:447–54. 10.1038/s12276-022-00755-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Semerdzhiev SA, Fakhree M A, Segers-Nolten I, Blum C, Claessens MM. Interactions between SARS-CoV-2 N-protein and α-synuclein accelerate amyloid formation. ACS Chem Neurosci. (2022) 13:143–50. 10.1021/acschemneuro.1c00666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fearon C, Mikulis DJ, Lang AE. Parkinsonism as a sequela of SARS-CoV-2 infection: pure hypoxic injury or additional COVID-19-related response? Movement Disord. (2021) 36:1483–4. 10.1002/mds.28656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reveret L, Leclerc M, Emond V, Loiselle A, Bourassa P, Tremblay C, et al. Higher ACE2 expression in the brains of individuals with Alzheimer's disease. Alzheimers Dement. (2021) 17:e055278. 10.1002/alz.055278 [DOI] [Google Scholar]
- 31.Shen WB, Logue J, Yang P, Baracco L, Elahi M, Reece EA, et al. SARS-CoV-2 invades cognitive centers of the brain and induces Alzheimer's-like neuropathology. bioRxiv. [Preprint]. (2022). 10.1101/2022.01.31.478476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fernandez-de-Las-Peñas C, Navarro-Santana M, Gomez-Mayordomo V, Cuadrado ML, García-Azorín D, et al. Headache as an acute and post-COVID-19 symptom in COVID-19 survivors: a meta-analysis of the current literature. Eur J Neurol. (2021) 28:3820–5. 10.1111/ene.15040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Montefusco L, Ben Nasr M, D'Addio F, Loretelli C, Rossi A, Pastore I, et al. Acute and long-term disruption of glycometabolic control after SARS-CoV-2 infection. Nat Metab. (2021) 3:774–85. 10.1038/s42255-021-00407-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ayoubkhani D, Khunti K, Nafilyan V, Maddox T, Humberstone B, Diamond I, et al. Post-covid syndrome in individuals admitted to hospital with covid-19: retrospective cohort study. BMJ. (2021) 372:n693. 10.1136/bmj.n693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Phetsouphanh C, Darley DR, Wilson DB, Howe A, Munier C, Patel SK, et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat immunol. (2022) 23:210–6. 10.1038/s41590-021-01113-x [DOI] [PubMed] [Google Scholar]
- 36.Wang Z, Yang L. Broad-spectrum prodrugs with anti-SARS-CoV-2 activities: strategies, benefits, and challenges. J Med Virol. (2022) 94:1373–90. 10.1002/jmv.27517 [DOI] [PubMed] [Google Scholar]
- 37.Kozlov M. Merck's COVID pill loses its lustre: what that means for the pandemic. Nature. (2022). 10.1038/d41586-021-03667-0. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 38.Du Y, Chen L, Shi Y. Safety, immunogenicity, and efficacy of COVID-19 vaccines in adolescents, children, and infants: a systematic review and meta-analysis. Front Public Health. (2022) 10:829176. 10.3389/fpubh.2022.829176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tanne JH. Covid 19: US cases rise amid omicron fears but booster shots offer protection, experts say. BMJ. (2021) 375:n3098. 10.1136/bmj.n3098 [DOI] [PubMed] [Google Scholar]
- 40.Hassan F, London L, Gonsalves G. Unequal global vaccine coverage is at the heart of the current covid-19 crisis. BMJ. (2021) 375:n3074. 10.1136/bmj.n3074 [DOI] [PubMed] [Google Scholar]
- 41.Xu W. Xi: China to Provide 1b More Vaccine Doses to Africa. Available online at: http://www.chinadaily.com.cn/a/202111/29/WS61a4c26aa310cdd39bc782ff.html
- 42.Schwartz IS, Heil EL, McCreary EK. Remdesivir: a pendulum in a pandemic. BMJ. (2020) 371:m4560. 10.1136/bmj.m4560 [DOI] [PubMed] [Google Scholar]
- 43.Wang Z, Yang L. GS-5734: a potentially approved drug by FDA against SARS-CoV-2. N J Chem. (2020) 44:12417–29. 10.1039/D0NJ02656E [DOI] [Google Scholar]
- 44.Cully M. A tale of two antiviral targets — and the COVID-19 drugs that bind them. Nat Rev Drug Discov. (2022) 21:3–5. 10.1038/d41573-021-00202-8 [DOI] [PubMed] [Google Scholar]
- 45.Yang L, Wang Z. Natural products, alone or in combination with FDA-approved drugs, to treat COVID-19 and lung cancer. Biomedicines. (2021) 9:689. 10.3390/biomedicines9060689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang Z, Yang L. Chinese herbal medicine: fighting SARS-CoV-2 infection on all fronts. J Ethnopharmacol. (2021) 270:113869. 10.1016/j.jep.2021.113869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yi Y, Li J, Lai X, Zhang M, Kuang Y, Bao YO, et al. Natural triterpenoids from licorice potently inhibit SARS-CoV-2 infection. J Adv Res. (2022) 36:201–10. 10.1016/j.jare.2021.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]